Medical school curricula, mentorship, infectious diseases (ID) exposure, and salary were identified as significant factors influencing internal medicine resident perceptions of ID. Understanding these factors and how they fit into career decision-making constructs is central to increasing interest in ID.
Keywords: career choice, microbiology curriculum, infectious diseases education, mentorship, perception of infectious diseases
Abstract
Background. Only 49% of infectious diseases (ID) fellowship programs were filled in 2015 through the national match, but little is known about internal medicine (IM) resident perceptions of ID and factors related to IM resident career choice.
Methods. We conducted 25 interviews and disseminated a Web-based survey to graduating IM residents in the United States utilizing a 2-stage sampling strategy. Participants were categorized into 3 groups based on interest in ID: (1) applied/intended to apply to ID; (2) interested in ID but did not apply; (3) never interested in ID. We conducted all analysis using poststratification adjustment weights with survey data analysis procedures.
Results. Of the 590 participants, 42 (7%) selected category 1, 188 (32%) category 2, and 360 (61%) category 3. Most (65%) developed an interest in their ultimate career before residency. Of those interested in ID, >52% rated their ID medical school curriculum as very good and influential on their interest in ID. Ninety-one percent of category 2 participants felt mentorship was influential on career choice, although 43% identified an ID mentor. Category 2 chose salary as the most dissuading factor and the most likely intervention to increase ID interest.
Conclusions. In this nationally representative sample of graduating IM residents, most develop an interest in their ultimate career before residency. Factors influencing this decision reside in both medical school and residency, which is consistent with career decision-making constructs. By identifying career determining factors and understanding how they fit into medical training frameworks, we can develop targeted initiatives to reinvigorate interest in ID.
(See the Major Article by Melber, Teherani, and Schwartz on pages 164–8, and the Editorial Commentary by Chida, Melia, and Ghanem on pages 169–71.)
The number of internal medicine (IM) residents applying to infectious diseases (ID) fellowship programs through the national match has declined disproportionately compared with other medicine subspecialties over the last 5 years [1, 2]. Despite a relative increase in the number of medical students matching into IM residency positions in 2015, only 240 residents applied to ID through the National Resident Match Program, whereas 344 applied in 2008 [1, 3]. Furthermore, 51% of ID fellowship programs did not fill through the match for 2015, and the ratio of applicants per ID fellowship position decreased from 1.2 in 2008 to 0.7 in 2015 [1].
The steady downtrend in applicants to ID has led to speculation that low remuneration, poor ID exposure during training, and work-life balance represent prominent factors [4–6]. However, published data examining these hypotheses are lacking. A clear understanding of the factors behind this trend and how they fit into career decision-making constructs is essential. We hypothesize that several factors related to ID curricula, ID exposure, and perceptions of the ID physician's career influence IM residents' decision to pursue a career in ID. To identify and explore possible explanations for the downward trend in ID fellowship applications, we surveyed graduating IM residents regarding their perceptions of ID and factors that influenced their career choices.
METHODS
Study Design and Population
We conducted a national cross-sectional mixed-methods study of IM residents graduating from United States Accreditation Council for Graduate Medical Education (ACGME) programs in the spring and fall of 2014. Graduating residents included primary care and categorical residents completing their IM training in the postgraduate year (PGY) 3 or 4, or PGY-2 if the trainee was enrolled in the physician-scientist research pathway. Each interview and survey participant received a financial incentive. The Oregon Health & Science University Institutional Review Board approved this study.
Qualitative Design
Two authors (E. M. B., W. S. A.) interviewed 20 residents and 5 program directors (PDs) from 8 unique IM residency training programs using a standard script prior to questionnaire development to identify key themes hypothesized to play a role in IM resident career decisions and to uncover unknown themes. A diverse sample of PDs and residents from their programs participated in semistructured interviews. PD interviews focused on ID exposure, perception of ID physicians, perception of resident interest, and applications to ID. Resident interviews focused on perceptions of ID careers, career decision-making processes, preclinical ID education, clinical ID exposure, and mentorship. Each interview concluded with general thoughts about the declining numbers of resident applications to ID. Interviews were analyzed using qualitative methods, and findings were applied to questionnaire development.
Sampling Design
We sampled 2 graduating resident cohorts with a 2-stage design intended to provide a nationally representative sample, minimize confounding of a single graduating class or a particular program size, and assure adequate numbers in the dataset. In the first stage, we defined 5 strata based on program size from the ACGME directory and FREIDA Online (the American Medical Association Residency and Fellowship Database), using total first-year positions available as a proxy for third-year residents. We selected 160 residency programs with probability proportional to program size, varying the sampling ratio from 1:5 in the stratum of the smallest programs to 1:1 in the largest programs and systematically sampling to balance program type and region. In the second stage, sampling ratios ranged from 1:1 to 1:5 to achieve an overall sampling rate of 20% in each stratum. We confirmed the contact information for all IM PDs using the ACGME Directory, FREIDA Online, and institution-published information, then contacted PDs to request consent for study participation and resident solicitation.
Although the basic design was self-weighting, we conducted all analyses using adjustment weights with survey data analysis procedures in Stata to compensate for nonresponse bias related to program size and region. Because we obtained numbers of first-year positions for all programs in our frame, but third-year positions only for responding programs, we estimated the size of the national graduating class by calculating the ratio of actual to listed positions in programs that did respond, then applied that ratio to nonresponding programs.
Questionnaire Development and Statistical Analysis
The questionnaire items were grouped into the following areas: demographics, career interest, mentorship, scholarship, conferences, undergraduate medical education, graduate medical education, and potential interventions to increase ID interest (Supplementary Data). Participants were divided into 3 categories: Category 1 residents indicated they applied or planned to apply to ID fellowship; category 2 residents were interested in ID at one time but ultimately decided not to apply; and category 3 residents were never interested in ID. This delineation enabled us to compare responses according to interest in the field of ID.
All estimates were calculated with poststratification weights using survey procedures in Stata 13.1. We calculated relative risk ratios using multinomial logistic regression. Because international medical graduates (IMGs) have different training experiences, we controlled for IMG status in some analyses, as indicated in the results, and tested for interactions; none were statistically significant and they were omitted from final analyses.
RESULTS
Project Flow and Participant Demographics
We contacted 160 IM PDs to solicit participation of their programs in the study (Figure 1). Of these, 45 programs participated in the spring and 60 in the fall. We received complete responses from a total of 590 unique IM residents, 230 in the spring of 2014 (55% response rate), and 360 in the fall (63% response rate). The final response rate, a combination of program participation and resident response, equaled 27%–30%.
Figure 1.
Flowchart of project.
Of the 590 residents who responded, 42 applied/planned to apply to ID for fellowship training (category 1), 188 were interested in ID but did not apply (category 2), and 360 were never interested in ID (category 3) (Table 1). Participants from Northeastern programs represented 39% of the total, and participants from programs with <15 positions contributed 9% of the total. Although IMGs represented 41% of the responding residents, they comprised the majority of respondents in category 1.
Table 1.
Demographics by Level of Interest in Infectious Diseases as a Career Among Graduating Medical Residents
| Characteristic | Infectious Diseases Career Category |
Total (N = 590) | P Value* | ||
|---|---|---|---|---|---|
| (1) Applied (n = 42) | (2) Considered (n = 188) | (3) Uninterested (n = 360) | |||
| Female sex | 47.7 | 42.1 | 47.4 | 45.6 | .703 |
| International medical school graduate | 64.2 | 49.0 | 33.5 | 41.6 | .001 |
| Will be family's primary wage earner | 74.0 | 72.0 | 68.9 | 70.5 | .806 |
| Took ≥1 y off | 37.6 | 39.5 | 44.8 | 42.3 | .615 |
| Program type | |||||
| Community | 62.4 | 47.3 | 32.6 | 40.4 | .004 |
| University/military | 37.6 | 52.7 | 67.4 | 59.6 | |
| Program size | |||||
| <15 positions | 4.8 | 17.5 | 4.3 | 9.0 | .038 |
| 15–24 | 20.2 | 21.5 | 20.5 | 20.8 | |
| 25–34 | 41.1 | 19.0 | 27.6 | 25.8 | |
| 35–49 | 17.7 | 20.2 | 25.2 | 22.8 | |
| ≥50 | 16.2 | 21.9 | 22.3 | 21.6 | |
| Region | |||||
| Northeast | 53.5 | 44.5 | 33.8 | 39.3 | .136 |
| Midwest | 8.3 | 19.2 | 24.5 | 21.2 | |
| South | 32.5 | 22.7 | 25.4 | 25.1 | |
| West | 5.7 | 13.6 | 16.3 | 14.5 | |
| Chosen career field | |||||
| Internal medicine primary care | 22.6 | 26.1 | 15.3 | 19.8 | .043** |
| Hospitalist medicine | … | 15.9 | 19.3 | 16.3 | |
| Cardiovascular disease | … | 9.5 | 16.8 | 12.6 | |
| Gastroenterology | … | 7.4 | 13.1 | 9.8 | |
| Hematology/oncology | … | 10.1 | 10.0 | 9.1 | |
| Pulmonary/critical care medicine | 3.3 | 10.3 | 8.7 | 8.8 | |
| Infectious diseases | 74.1 | … | … | 6.9 | |
| Endocrinology, diabetes, and metabolism | … | 4.1 | 5.9 | 4.7 | |
| Other clinical or nonclinical work | … | 4.9 | 3.8 | 3.8 | |
| Nephrology | … | 7.7 | 1.3 | 3.5 | |
| Rheumatology | … | 2.3 | 3.7 | 2.8 | |
| Allergy and immunology | … | 1.7 | 2.2 | 1.8 | |
| When did you first develop an interest in your chosen career field? | |||||
| Before medical school | 24.3 | 17.7 | 22.6 | 21.0 | .469 |
| In medical school | 48.1 | 48.2 | 41.1 | 44.2 | |
| In residency | 27.5 | 34.2 | 36.2 | 34.7 | |
Data are presented as percentage.
* P value from Pearson χ2 test performed with survey poststratification weights.
** P value comparing categories 2 and 3 only.
All participants identified their chosen field. In category 1, the majority (74%) selected ID, whereas 23% selected IM. In category 2, 26% chose IM (general or primary care), 16% chose hospital medicine, and 10% chose pulmonary/critical care. For category 3 residents, the top 3 chosen careers were hospital medicine, cardiology, and IM. Overall, 65% of all residents and 72% of those who chose ID as a career developed their interest in their chosen field in medical school or earlier.
When queried about areas of ID which were most interesting to them, residents pursuing ID fellowship selected human immunodeficiency virus (HIV) as their top field of interest (36%), followed by general ID and global health. Among category 2 participants, 28% selected general ID followed by HIV (19%) and global health (17%). Among all participants, intellectual stimulation was chosen as the primary attraction to either ID or their chosen field. For category 3 participants, the option to do procedures was also an important factor in their career choice.
Medical School and Residency Experiences
The majority of participants (63%) graduated from medical schools that employed a traditional curricular structure consisting of blocks of time dedicated to specific concepts (eg, microbiology, physiology) (Table 2). For 80% of participants, the primary pedagogical method for ID material was traditional didactics with learning by memorization. Those who experienced case-based learning and nonmemorization learning had an increased likelihood of choosing ID (relative risk ratio, 3.7–3.89; Table 3).
Table 2.
Medical School Training and Interest in Infectious Diseases (Categories 1 and 2) or Ultimate Career Choice (Category 3)
| Training | Infectious Diseases Career Category |
|||
|---|---|---|---|---|
| (1) Applied (n = 42) | (2) Considered (n = 188) | (3) Uninterested (n = 360) | Total (N = 590) | |
| Rated quality of medical school ID/microbiology curriculum | ||||
| Very good | 52.6 (42.0–62.9) | 52.1 (39.1–64.9) | 33.1 (26.9–40.0) | 41.4 (33.5–49.8) |
| Good | 33.1 (19.6–50.1) | 34.1 (23.9–46.0) | 40.5 (33.8–47.6) | 37.6 (31.2–44.6) |
| Poor/acceptable | 14.3 (4.6–36.8) | 13.8 (9.3–19.9) | 26.3 (19.3–34.8) | 20.9 (16.0–26.9) |
| Influence of the quality of preclinical training on your level of interest in ID | ||||
| Very influential | 49.9 (25.2–74.7) | 35.4 (22.6–50.7) | 11.6 (6.6–19.8) | 24.9 (16.6–35.6) |
| Somewhat influential | 40.6 (20.5–64.5) | 49.7 (35.8–63.6) | 31.4 (25.7–37.7) | 39.6 (31.9–47.7) |
| Not influential | 9.4 (3.1–25.1) | 14.9 (8.4–25.2) | 56.9 (48.5–65.0) | 35.5 (29.2–42.4) |
| Structure of medical school curriculum | ||||
| Traditional | 60.4 (48.5–71.1) | 64.9 (57.4–71.8) | 61.8 (55.5–67.7) | 62.8 (58.0–67.2) |
| Organ-based | 38.2 (27.3–50.3) | 32.6 (24.8–41.6) | 33.9 (27.6–40.8) | 33.8 (28.8–39.3) |
| Structure of medical school ID learning sessions | ||||
| Traditional lectures | 47.5 (26.1–69.9) | 79.9 (71.7–86.2) | 84.7 (77.5–89.9) | 79.7 (72.0–85.8) |
| Case-based discussion | 40.2 (16.2–70.1) | 13.2 (7.7–21.5) | 10.8 (6.3–17.9) | 14.3 (8.3–23.4) |
| Team-based learning | 2.1 (.5–8.6) | 5.3 (2.1–12.5) | 3.3 (1.9–5.6) | 3.9 (2.2–6.5) |
| Laboratory-based | 10.2 (2.9–30.2) | 1.6 (.5–5.8) | 0.8 (.2–3.5) | 2.0 (.8–4.4) |
| Flipped classroom | … | … | 0.3 (.0–2.5) | 0.2 (.0–1.4) |
| Typical ID pedagogy in medical school | ||||
| Memorization | 33.2 (14.6–59.1) | 64.7 (57.1–71.6) | 77.9 (69.5–84.5) | 69.3 (61.5–76.2) |
| Concept maps and frameworks | 21.2 (8.8–42.6) | 21.4 (15.5–28.7) | 11.3 (7.3–17.0) | 15.7 (11.5–20.9) |
| Patient encounters | 29.7 (16.7–47.1) | 9.7 (5.2–17.5) | 5.1 (2.3–11.0) | 8.9 (5.5–14.1) |
| Algorithms | 16.0 (5.8–36.9) | 4.2 (2.1–8.2) | 5.7 (3.6–8.9) | 6.1 (4.5–8.3) |
| Teacher(s) for ID/microbiology in medical school | ||||
| Basic science faculty | 48.4 (21.5–76.3) | 59.7 (46.2–71.9) | 63.2 (55.1–70.6) | 60.6 (50.8–69.6) |
| ID clinical faculty | 46.9 (20.0–75.7) | 35.7 (24.1–49.3) | 30.3 (23.4–38.1) | 33.7 (25.3–43.2) |
Data are presented as percentage (95% confidence interval).
Abbreviation: ID, infectious diseases.
Table 3.
Characteristics of Preclinical Training Reported by Final-Year Residents Who Applied to Infectious Diseases, Considered but Did Not Apply, or Were Uninterested, Controlling for International Medical Graduate Status
| Characteristic | Applied vs Considered |
Applied vs Uninterested |
||
|---|---|---|---|---|
| RRRa | 95% CI | RRRa | 95% CI | |
| Case-based learning | 3.89** | 1.46–10.31 | 3.70* | 1.34–10.31 |
| Nonmemorization pedagogyb | 3.30* | 1.16–9.43 | 5.43** | 2.19–13.51 |
| Taught by ID faculty | 1.44 | .50–4.18 | 1.69 | .53–5.38 |
| International medical graduate | 1.87 | .76–4.59 | 3.57** | 1.57–8.13 |
Abbreviations: CI, confidence interval; ID, infectious diseases; RRR, relative risk ratio.
a Similar to odds ratio, from multinomial logistic model simultaneously comparing applied, considered, and uninterested groups, controlling for international medical graduate status.
b Non-memorization pedagogy includes algorithms, concept maps, and patient encounters.
* P < .05.
** P < .01.
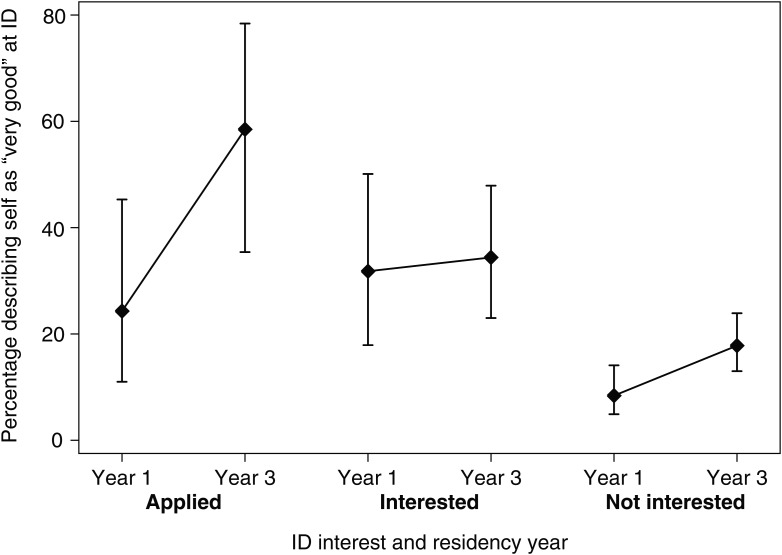
Those who indicated an interest in ID at the end of residency (categories 1 and 2) were more likely to rate their medical school curricula as very good (53% and 52%, respectively), compared with only 33% of those never interested in ID. In another potential measure of curriculum effectiveness, 71% of those who chose ID rated their ID knowledge as good or very good at the end of medical school, compared with 64% in category 2 and only 45% in category 3 (Figure 2). Self-rated knowledge was significantly associated with perception of the quality of the medical school curriculum at the beginning and the end of residency (P < .001).
Figure 2.
Self-efficacy: perception of infectious diseases (ID) knowledge at the end of medical school/transition to postgraduate year (PGY) 1 and the end of residency (PGY-3) according to categories of interest in ID (categories 1–3).
Once in residency, 95.5% of category 1 participants rotated in ID, compared with 72% and 70% of category 2 and 3 participants, respectively. Of those who rotated in ID, 85% experienced inpatient consults whereas only 23%–38% experienced an outpatient clinic. Although the timing of a resident's first ID rotation varied, >70% occurred in the first 2 years.
Mentorship and Scholarship
Regardless of career choice, respondents overwhelmingly indicated that mentorship, scholarship, and/or conference attendance positively influenced entry into a chosen field (Table 4). Among category 1, 80% identified an ID mentor compared with only 43% of category 2 participants. Less than 25% of all category 2 respondents participated in ID scholarship, compared with 76% in category 1. More than half of all respondents attended a regional or national conference. Of those who attended a conference, 84% in category 1 attended an ID conference compared with 18% of category 2 participants. The majority of respondents in all categories indicated that mentorship relationships, scholarship, and conference attendance opportunities occurred during residency.
Table 4.
Mentorship, Scholarship, and Conference Attendance Influence on Choosing a Career in Infectious Diseases or Other Fields
| Answer Category | Infectious Diseases Career Category |
P Value | ||
|---|---|---|---|---|
| (1) Applied (n = 42) | (2) Considered (n = 188) | (3) Uninterested (n = 360) | ||
| A mentor in a given field influences career choice | 100.0 | 91.0 | 87.7 | .365 |
| Had a mentor in ID/chosen field during training | 79.9 | 43.3 | 72.0 | <.001 |
| If yes, when developed relationship | ||||
| Before medical school | 2.8 | 7.6 | 6.9 | .908 |
| In medical school | 33.1 | 25.0 | 27.8 | |
| In residency | 64.1 | 67.4 | 65.3 | |
| Participating in scholarship in a given field influences career choice | 80.3 | 88.8 | 85.7 | .572 |
| Participated in scholarship in ID/chosen field during training | 76.2 | 23.4 | 64.4 | <.001 |
| If participated, first experience was | ||||
| Before medical school | 4.2 | 7.0 | 7.0 | .841 |
| In medical school | 32.8 | 34.3 | 27.8 | |
| In residency | 63.0 | 58.7 | 65.2 | |
| If participated, type of scholarship | ||||
| Teaching session to other learners | 25.1 | 6.8 | 28.3 | <.001 |
| Grand Rounds | 4.8 | 2.7 | 8.2 | .047 |
| Research project | 32.7 | 14.0 | 50.2 | <.001 |
| Poster presentation | 47.1 | 12.9 | 41.8 | <.001 |
| Oral presentation | 18.0 | 5.1 | 18.5 | .002 |
| Manuscript | 21.8 | 4.5 | 25.6 | <.001 |
| Attending conferences influences career choice | 83.9 | 77.0 | 78.2 | .739 |
| Attended conference during training | 59.0 | 52.5 | 59.7 | .540 |
| If attended, went to ID-themed conference | 83.8 | 17.6 | 4.1 | <.001 |
| If attended, when (first) | ||||
| Before medical school | 6.2 | 4.5 | 6.5 | .344 |
| In medical school | 36.8 | 37.1 | 24.8 | |
| In residency | 56.9 | 58.4 | 68.7 | |
Data are presented as percentage.
Abbreviation: ID, infectious diseases.
Dissuading Factors and Potential Interventions
Participants in categories 2 and 3 were asked to rate the factors that most dissuaded them from selecting ID as a career (Table 5). Among those who had an interest in ID but chose another career, the 3 main detractors from ID were salary, the desire to be a generalist, and limited job availability in ID. Those never interested (category 3) indicated less intellectual stimulation from ID, a desire to be a generalist, and ID salary concerns.
Table 5.
Which Factor Most Influenced the Decision Not to Pursue Infectious Diseases as a Career
| Factor | Infectious Diseases Career Category |
Total (N = 548) | |
|---|---|---|---|
| (2) Considered (n = 188) | (3) Uninterested (n = 360) | ||
| Salary | 19.2 (11.4–30.6) | 12.1 (7.5–19.1) | 14.9 (9.2–23.2) |
| Desire to be a generalist vs consultant | 17.6 (11.4–26.1) | 15.0 (10.9–20.3) | 16.0 (12.1–21.0) |
| Limited job availability | 13.3 (7.5–22.3) | 2.1 (.9–4.8) | 6.4 (3.9–10.5) |
| Other | 10.1 (6.3–15.8) | 9.3 (6.3–13.4) | 9.6 (7.1–12.8) |
| Lack of procedures in ID | 9.9 (5.8–16.2) | 8.0 (5.7–11.2) | 8.7 (6.5–11.7) |
| ID and microbiology are challenging subjects and mostly memorization | 6.9 (3.7–12.6) | 12.1 (8.1–17.6) | 10.1 (7.1–14.2) |
| Less opportunity for longitudinal patient care | 5.5 (2.1–13.6) | 2.8 (1.4–5.6) | 3.9 (2.1–7.1) |
| Low engagement of the ID faculty and/or fellows | 4.4 (1.6–11.6) | 0.9 (.3–2.6) | 2.2 (1.0–4.8) |
| Work-life balance | 4.2 (1.8–9.1) | 4.5 (2.2–9.1) | 4.4 (2.5–7.4) |
| ID physicians are not thought of highly | 3.7 (.8–15.3) | 1.0 (.4–2.5) | 2.1 (.7–5.7) |
| Length of ID fellowship training | 2.5 (1.0–6.2) | 0.2 (.0–1.4) | 1.1 (.5–2.4) |
| Less intellectual stimulation in ID field | 1.9 (.7–5.0) | 28.3 (22.6–34.8) | 18.1 (13.9–23.3) |
| Limited innovation possibilities and research opportunities | 0.6 (.1–2.6) | 0.6 (.2–2.0) | 0.6 (.3–1.5) |
| Limited career niche options in the ID field | 0.3 (.0–1.9) | 3.0 (1.6–5.6) | 2.0 (1.1–3.5) |
Data are presented as percentage (95% confidence interval).
Abbreviation: ID, infectious diseases.
The most important intervention selected to increase interest in ID by those in all 3 categories was improved salary of the ID physician (Table 6). Furthermore, if the salaries were equal to their chosen career, 45% of category 2 respondents reported that they would have chosen ID instead. Despite this, 50% thought an improved ID physician salary was unlikely to increase the number of residents choosing ID as a career. Early exposure to the broad field of ID was the next most selected intervention, particularly among category 3 participants.
Table 6.
Which Factor Would You Consider the Most Important in Increasing Interest in Infectious Diseases?
| Factor | Infectious Diseases Career Category |
|||
|---|---|---|---|---|
| (1) Applied (n = 42) | (2) Considered (n = 188) | (3) Uninterested (n = 360) | Total (N = 590) | |
| Improved salary of the ID physician | 33.5 (16.7–55.9) | 32.0 (22.6–43.1) | 32.5 (26.8–38.8) | 32.4 (26.6–38.9) |
| Early exposure to the broad field of ID | 16.2 (5.1–41.3) | 14.4 (10.1–20.1) | 26.4 (20.1–33.8) | 21.3 (16.8–26.7) |
| More ID mentorship to students/residents | 2.9 (.7–11.7) | 11.7 (6.6–19.6) | 3.7 (2.1–6.5) | 6.4 (4.3–9.4) |
| Improved job availability after ID fellowship | 13.7 (4.1–37.1) | 11.3 (6.1–19.9) | 6.9 (4.6–10.2) | 9.0 (6.4–12.6) |
| Improved quality of ID curriculum in medical school | 14.4 (3.7–42.1) | 9.3 (5.0–16.4) | 8.8 (5.7–13.4) | 9.5 (7.0–12.8) |
| More enthusiastic ID faculty in medical student/resident teaching | 14.4 (4.7–36.5) | 9.0 (4.6–16.8) | 8.0 (5.4–11.6) | 8.9 (6.0–13.1) |
| Increased resident engagement in scholarship and in ID-focused conferences | 4.9 (1.0–20.7) | 7.7 (3.4–16.8) | 6.8 (3.6–12.6) | 7.0 (4.8–10.0) |
| Decreased length of ID fellowship training | … | 1.9 (.7–4.8) | 1.2 (.4–3.3) | 1.3 (.7–2.5) |
| Improved work hours of the ID physician | … | 1.5 (.4–5.6) | 3.0 (1.2–7.5) | 2.2 (1.0–5.1) |
| More ID faculty presence in residency program leadership | … | 1.3 (.4–4.9) | 2.7 (1.4–5.0) | 2.0 (1.1–3.5) |
Data are presented as percentage (95% confidence interval).
Abbreviation: ID, infectious diseases.
DISCUSSION
In this study, we found that the decision to pursue ID fellowship training is influenced by experiences beginning in and even prior to medical school, indicating that interest in a career often develops before residency. Interventions targeting these early experiences could enhance interest in ID. Examining experiences and factors that influence career choice in the context of existing frameworks for career decision making sheds light on IM resident career choices overall and facilitates the identification of areas where interventions to generate interest in ID would yield the most impact.
Thus far, studies investigating career choices among medical trainees have focused either on how medical students select their residency or on IM resident career trends away from primary care [7–12]. Although the primary aims of these studies differed from ours, we observed common themes: Exposures in medical school impact career choice [8, 12], IM residents often change their career decisions during training [10, 11], and intellectual stimulation in the field of choice is important [7, 12]. These themes are consistent with career decision-making models described outside the field of medicine. Examining the application of these themes in the context of existing career decision-making constructs not previously applied to medicine enriches our understanding of the findings.
Early theories regarding career choice described decision making based on one's understanding of self and the proposed career [13]. More recent literature suggests the process of decision making is less rational or fixed [13, 14]. One such construct is the adaptive career decision-making model described by Krieshok et al, which suggests that career choice is an iterative process between the unconscious and conscious through job experiences or “occupational engagements” [15]. Unlike many career decision makers, medical trainees experience at least 2 main occupational engagement phases, medical school and residency, each with different pressures and emphasis. These experiences shape the trainee's conscious understanding of different career fields and their own identity but also affect later decisions toward or away from possible career options in ways beyond their conscious perception [15].
Under this construct, medical school represents the first engagement phase. In this study, the majority of residents indicated that their interest in their field developed before or during the first engagement phase, confirming that medical school experiences influence and inform a trainee's ultimate career choice, an observation that has been described previously [7, 8]. Careful attention to learning experiences in medical school may have a significant influence on promoting interest in a field. For students, the most prominent ID experience is the preclinical microbiology curriculum which, for most, relies heavily on didactics and memorization. These pedagogical techniques are less effective at knowledge retention than are active methods [16–19]. Interestingly, a larger proportion of those interested in ID reported a preclinical experience with active learning that correlated with perceived ID knowledge, suggestive of an effective ID curriculum (Table 2; Figure 2). In contrast, respondents in category 3 were less likely to rate their curriculum or perceived ID knowledge highly, which aligns with social cognitive career theory that people are more likely to take on tasks if they believe they have the skills to be successful [20]. Medical trainees who feel their microbiology or ID knowledge is inadequate may perceive themselves as lacking the capabilities necessary to be an ID physician and choose another field.
IM residency represents the second phase of occupational engagement with a greater emphasis on workplace learning and systems-based practices. These likely influence the trainee differently than the first phase, leading to adaptation in career choice. Data suggest that >55% of residents change career plans at least once during residency; however, specific factors that drive these decisions are unclear [11]. In our study, most respondents felt mentorship and scholarship were influential on their ultimate career decisions. However, relatively few category 2 respondents identified an ID mentor or attended an ID conference. Whether residents had a richer ID experience because they were more committed to the specialty, or if ID-associated mentorship and scholarship led residents to be more likely to choose ID cannot be determined from these data. Nevertheless, given that mentorship and scholarship were noted to be influential and that occupational experiences drive career choice in various ways, attention to ID mentorship and scholarship opportunities may represent an important intervention to encourage resident selection of ID.
While mentorship may help drive career choice, equally important is understanding factors responsible for dissuading a resident from a particular career. These factors may not be uniform across IM specialty choices. Investigators in nephrology surveyed IM non–nephrology fellows, finding that the challenging patient population and lack of role models dissuaded trainees. However, of the 25% who had considered nephrology, the majority chose another field due to enthusiasm for it [21, 22]. In our study, for those not interested in ID, the top dissuading factor was interest in another field, which is consistent with the conceptual understanding of career decision making. The group of greatest interest, category 2, reported being dissuaded by other factors (salary inequities and a desire to be a generalist). Almost 55% of this group selected a higher-remuneration specialty, yet the top career chosen was general IM, not typically considered a high-remuneration specialty. Interestingly, a greater proportion of IMGs indicated that salary was important compared with US medical graduates (UMGs). Among IMGs, 56.4% stated they would have chosen ID rather than their current field if salaries were equal, compared with only 32.9% of UMGs, and 65% of IMGs ultimately chose high-remuneration careers compared with 45% of UMGs. Financial pressures or the importance of financial success may differ between IMGs and UMGs and could explain these findings. Notably, lifestyle was not highly selected as a dissuading factor as in prior studies [7, 9]. Although all participants, regardless of career choice, highly ranked improving salary as the intervention to increase interest in ID, paradoxically most category 2 respondents did not believe improving salary would impact the number of applicants. This may reflect their perception that the decision-making process is multifactorial, which is supported by the adaptive decision-making model.
Our study has several limitations. First, response rates from small programs in the South and Northeast were lower than expected, resulting in relatively high poststratification weights, and their responses may be overly influential. Despite this, the demographics in our study closely relate to national data. IMGs represented 42% of all respondents; this matches the ACGME data for all IM residents [23]. Second, although most residents in the spring cohort likely had decided on their ultimate career plans, the fall cohort could choose to change career choices later in their final year. Because the subspecialty application due date occurred only 2 months after our survey, the number changing subspecialty choice was likely small and unlikely to significantly impact these data. Third, this study was susceptible to recall bias as graduating residents were asked about perceptions of preclinical medical school curricula. Fourth, although definitions of medical school curricular terms were provided in the survey tool, residents may have had difficulty identifying the methods used in their own curriculum. Findings did appear to correlate across resident categories, adding validity to the results.
In conclusion, we have elucidated several factors that likely impact not only the development of a pool of ID-interested medical students but also the narrowing of that pool in residency. We are the first to suggest that the adaptive career decision-making construct is applicable to career choices in medicine and may help inform our findings. Given our results, a high-quality microbiology curriculum and exposure to ID in medical school are intervention points that may be necessary to spark an interest in ID during the first engagement phase. In the second engagement phase, to maintain and recruit more interest in ID, exposure to the broad field of ID, mentorship/scholarship efforts, and improving salary represent high-yield target areas. These data identify potential interventions that will help provide guidance to the Infectious Diseases Society of America Task Force on Recruitment.
Supplementary Data
Supplementary materials are available at http://cid.oxfordjournals.org. Consisting of data provided by the author to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the author, so questions or comments should be addressed to the author.
Notes
Acknowledgments. We gratefully acknowledge the support of the Oregon Clinical and Translational Research Institute (grant number UL1TR000128) from the National Center for Advancing Translational Sciences at the National Institutes of Health, particularly Amber Laurie, MS. We also greatly appreciate Thomas Kreishok, PhD, for his assistance in the application of career decision-making constructs to medical education.
Disclaimer. The content reflects the views of the authors. The study sponsors had no role in the design, implementation, or analysis of the study, the writing of the manuscript, or decision to submit for publication.
Financial support. This study was supported by the Infectious Diseases Society of America.
Potential conflicts of interest. All authors: No potential conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.National Resident Matching Program. Results and data: specialties matching service 2015 appointment year. Washington, DC: NRMP, 2015. [Google Scholar]
- 2.Johnson L. Resident recruitment. In: IDWeek 2013, San Francisco, CA, 2013. [Google Scholar]
- 3.National Resident Matching Program. Results and data: specialties matching service 2008 appointment year. Washington, DC: NRMP, 2008. [Google Scholar]
- 4.Chandrasekar P, Havlichek D, Johnson LB. Infectious diseases subspecialty: declining demand challenges and opportunities. Clin Infect Dis 2014; 59:1593–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tapper ML. Number of infectious disease specialists declining. Infectious Disease News. Healio. Thorofare, NJ: SLACK Inc., 2011.
- 6.Relman DA. From the President: telling the ID story. Arlington, VA: IDSAnews, Infectious Diseases Society of America, 2013.
- 7.Richard A, Garibaldi M, Popkave C, Bylsma W. Career plans for trainees in internal medicine residency programs. Acad Med 2005; 80:508–12. [DOI] [PubMed] [Google Scholar]
- 8.Hauer KE, Durning SJ, Kernan WN et al. Factors associated with medical students’ career choices regarding internal medicine. JAMA 2008; 300:1155–64. [DOI] [PubMed] [Google Scholar]
- 9.West CP, Drefahl MM, Popkave C, Kolars JC. Internal medicine resident self-report of factors associated with career decisions. J Gen Intern Med 2009; 24:946–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.West CP, Dupras DM. General medicine vs subspecialty career plans among internal medicine residents. JAMA 2012; 208:2241–7. [DOI] [PubMed] [Google Scholar]
- 11.West CP, Popkave C, Schultz H, Weinberger SE, Kolars JC. Changes in career decisions of internal medicine residents during training. Ann Intern Med 2006; 145:774–9. [DOI] [PubMed] [Google Scholar]
- 12.Ko HH, Lee TK, Leung Y, Fleming B, Vikis E, Yoshida EM. Factors influencing career choices made by medical students, residents and practising physicians. BC Med J 2007; 49:483–9. [Google Scholar]
- 13.Hartung PJ, Blustein DL. Reason, intuition and social justice: elaborating on Parson's career decision-making model. J Couns Dev 2002; 80(winter):41–7. [Google Scholar]
- 14.Nauta MM. The development, evolution, and status of Holland's theory of vocational personalities: reflections and future directions for counseling psychology. J Couns Psychol 2010; 57:11–22. [DOI] [PubMed] [Google Scholar]
- 15.Krieshok TS, Black MD, McKay RA. Career decision making: the limits of rationality and the abundance of non-conscious processes. J Vocat Behav 2009; 75:275–9. [Google Scholar]
- 16.Sousa DA. How the brain learns. 4th ed. Thousand Oaks, CA: Corwin, 2011. [Google Scholar]
- 17.Graffam B. Active learning in medical education: strategies for beginning implementation. Med Teach 2007; 29:38–42. [DOI] [PubMed] [Google Scholar]
- 18.Searle NS, Haidet P, Kelly PA, Schneider VF, Seidel CL, Richards BF. Team learning in medical education: initial experiences at ten institutions. Acad Med 2003; 78:S55–8. [DOI] [PubMed] [Google Scholar]
- 19.Koles PG, Stolfi A, Borges NJ, Nelson S, Parmelee DX. The impact of team-based learning on medical students’ academic performance. Acad Med 2010; 85:1739–45. [DOI] [PubMed] [Google Scholar]
- 20.Lent RW, Brown SD. Social cognitive model of career self-management: toward a unifying view of adaptive career behavior across the life span. J Couns Psychol 2013; 60:557–68. [DOI] [PubMed] [Google Scholar]
- 21.Jhaveri KD. Why not nephrology? A survey of US internal medicine subspecialty fellows. Am J Kidney Dis 2013; 61:540–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jhaveri KD, Shah H, Mattana J. Enhancing interest in nephrology careers during medical residency. Am J Kidney Dis 2012; 60:350–3. [DOI] [PubMed] [Google Scholar]
- 23.Accreditation Council for Graduate Medical Education. ACGME data resource book: academic year 2013–2014. Chicago, IL: ACGME, 2014. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.