Abstract
Background & objectives:
Preventing unintended pregnancies among people living with HIV (PLHIV) is one of the strategies of WHO for preventing parent-to-child transmission (PPTCT). Given the limitation of only condom use, the objective of this study was to improve use of dual contraceptive methods among HIV infected women.
Methods:
An experimental study among HIV positive women was conducted at two tertiary care level hospitals in Mumbai. Linking HIV with family planning services was the focus of intervention at one site and standard level of care was maintained at the control site. At each site, 150 HIV+ve women attending counselling and testing centres, who did not intend to get pregnant in the next one year and were eligible to use dual methods, were enrolled and followed up to one year.
Results:
At the end of one year, 60 per cent women in the intervention group reached Family Planning Centres compared to eight per cent in the control group. There was three times more acceptance and continuation of use of dual methods along with increase in consistent use of condoms and less number of unplanned pregnancies in the intervention group than the control group.
Interpretation & conclusions:
The study findings demonstrate that linking HIV and family planning services may facilitate the uptake of dual methods of contraception without reducing consistent condom use among HIV infected women. The PPTCT programmes need to focus on the component of Prong 2 of PPTCT which aims to prevent unintended pregnancies among HIV positive women.
Keywords: Contraceptive, dual method, dual protection, family planning, HIV, linkages
The World Health Organization's PMTCT (prevention of mother-to-Child transmission) strategic Vision 2010-20151 outlines four approaches: (i) Primary prevention of HIV infection among women of childbearing age; (ii) Preventing unintended pregnancies among women living with HIV; (iii) Preventing HIV transmission from a woman living with HIV to her infant; and (iv) Providing appropriate treatment, care and support to mothers living with HIV and their children and families. Most PMTCT programmes focus on the third approach. In India, with an estimated HIV prevalence rate of 0.22 per cent among women, approximately 38,000 HIV+ve pregnant women needed prevention of parent-to-child transmission (PPTCT) in 20112. However, as per 2012 technical report estimates of National AIDS Control Organization (NACO) current PPTCT regimen reaches to only 32 per cent of pregnant women needing it2. The National PPTCT programme has introduced in 2014 Option B plus multidrug anti-retroviral regimen to reduce transmission rates3 which is being scaled up in a phased manner.
However, the programme lacks focus on fertile non-pregnant women who are at risk of unwanted pregnancies. Most HIV/AIDS service delivery settings typically focus on condoms as a method for preventing the spread of sexually transmitted infections (STIs), HIV and miss opportunities to acknowledge the importance of dual methods of contraception or contraceptive benefits of condoms and backup methods in case of contraceptive failure. Studies have demonstrated that a reduction of only 16 per cent in unintended pregnancy rates among HIV-infected women would reduce rates of HIV-positive births as much as would current PPTCT efforts coupled with a range of health benefits to all women and their families4,5,6,7.
A review of studies offering sexual and reproductive health (SRH) services to people living with HIV (PLHIV) have identified a number of positive effects of condom and contraceptive use along with improved quality of services, health outcomes and cost-effectiveness especially in African settings7,8,9,10,11,12,13,14. At the global level, policy support for the integration of reproductive health, especially family planning into PPTCT programmes, has been established15. Essential services for preventing unintended pregnancies among women living with HIV have been defined16. There are still gaps in the know-how of which interventions are most successful and cost-effective to meet sexual and reproductive health needs of PLHIV in different settings with varying HIV prevalence17,18. Making contraceptive services more widely available would make it easier for these women to coordinate their HIV-related care with their pregnancy prevention goals, and at the same time, help prevent mother-to-child HIV transmission. It is this aspect of linkages that has been historically underappreciated. With evidence from literature revealing repeat unintended pregnancies among HIV positive women in India19,20, the present study was undertaken with an objective to improve dual method use among HIV+ve women availing counselling and testing services at two tertiary hospitals in Mumbai, Maharashtra by linking HIV counselling and testing centres with family planning services.
Material & Methods
This study was conducted from July 2011 to December 2013 in two tertiary care level hospitals of Municipal Corporation of Greater Mumbai (B.Y.L. Nair Hospital and Lokmanya Tilak Municipal General Hospital), with identical set-ups (both in terms of infrastructure and services provided) which were randomly selected from the four such hospitals. One of the two was assigned as intervention and another as control site. The two sites were located at a distance of 10 km from each other catering individually to a large population. Within the hospital set-up, the study was conducted at the HIV testing centres known as Integrated Counselling and Testing Centers (ICTC) and PPTCT centres where all antenatal clinic (ANC) attendees were counselled, and tested for HIV and finally these women delivered.
The inclusion criteria were (i) HIV positive women in childbearing age (18-40 yr), (ii) currently married, sexually active and non-pregnant, (iii) had not undergone permanent sterilization, (iv) not using any family planning method or were using only condom, (v) those who did not want to have a child for at least one year, (vi) willing to participate in the study and give written consent, (vii) would be residing in Mumbai for at least next one year.
The following operational definitions were used for the study:
Dual method - use of condom along with other available contraceptives such as intrauterine device (IUD), oral pills, injectable contraceptive (2-monthly NetEn), permanent sterilization (e.g. Tubectomy/vasectomy).
Experimental group - study site where a set of interventions were implemented to improve use of dual method and link HIV and Family Planning services.
Control group - study site with no interventions and the women received the routine standard care.
Based on the average statistics of HIV positive women attending ICTC services at public hospital settings in Mumbai, it was estimated that there would be approximately 120 eligible women in one year. Assuming a 20 per cent loss to follow up rate, the final sample size was calculated to be 150 at each site.
Among approximately 530-550 HIV positive women who attended ICTC/PPTCT centers, 150 consecutive eligible women were enrolled over nine months at each site. At the end of the study, 142 and 141 of the participants were retained in the study and were available for all follow ups in control and experimental groups, respectively (Fig. 1).
Fig. 1.
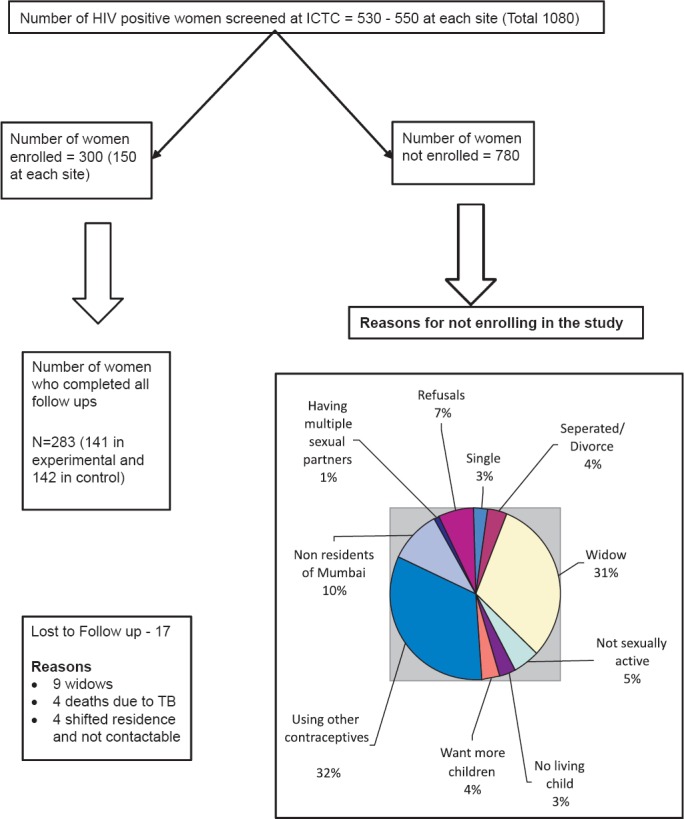
Flow chart describing numbers screened, enrolled, followed up and dropouts.
Situation analysis: Findings on existing standard of care revealed that HIV positive people were not routinely informed of other methods of contraception at ICTC and condoms were promoted mainly for infection control. There was no established referral linkage to family planning centres and PLHIVs were referred only on demand. There was no documentation and recording system on contraceptive use or pregnancy/abortion related details of the PLHIV seeking services at counselling and testing centres.
Intervention: An intervention package was introduced at the experimental site based on the gaps identified. This package included (i) one day training of service providers of ICTC/PPTCTC and family planning on promoting use of dual protection/dual method use and assessing medical eligibility for use of a particular method using WHO guidelines21 followed by a follow up training after 3 months, (ii) development and display of posters on dual methods at the respective sites and provision of counselling charts on family planning including emergency contraception by counsellors, (iii) providing counselling about dual method use and dual protection to HIV positive eligible couples by counsellors at ICTC/PPTCT and by the research team during every quarterly follow up with emphasis on consistent condom use, (iv) operationalizing a referral mechanism from ICTC/PPTCT centres to family planning clinics within the hospital set-up (Fig. 2) with a colour coded referral slip accompanied by a staff of research team to reduce administrative delays in seeking OPD registration for family planning services, (v) documenting variables such as number of children, current contraceptive use, fertility desires in the routine recording registers to identify a potential dual method user, (vi) sharing of information between ICTC/PPTCT and family planning providers, and (vii) repeated counselling by research team during quarterly follow ups.
Fig 2.
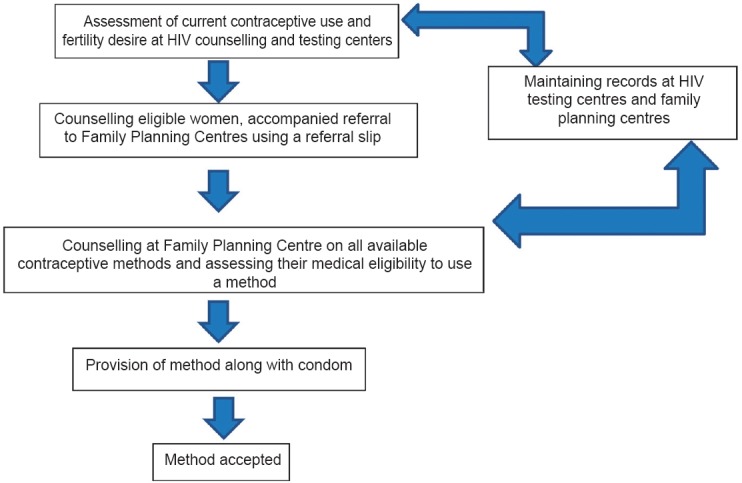
Flow of participants from ICTC/PPTCT centres to Family Planning Centres.
No intervention was introduced at the control site and women were offered standard level of care. The study protocol was approved by the ethics committee of the National Institute for Research in Reproductive Health, Mumbai. Written informed consent was obtained from every participant before enrolment.
Using a semi structured questionnaire, all enrolled women were assessed regarding their knowledge on contraception and safe sex, and details regarding their pregnancies/abortion related events during the study, type of contraceptives used and regularity in condom use at baseline and during every follow up were recorded.
Statistical analysis: The data were analysed using SPSS version 19 (SPSS, Inc., Chicago, USA). Information obtained at enrolment was considered as baseline or pre-intervention and that obtained during the fourth follow up was considered as end-line or post-intervention information. McNemar test was used to assess the differences between pre- and post-intervention in both study groups and chi-square test was used to find out the differences between the two groups post-intervention. Differences in mean values were assessed by paired t test. Knowledge based questions had a ‘Yes’ and ‘No’ response. Each correct answer was coded as 1. The cumulative scores were derived for each of the issues explored and mean scores were used to assess the change in knowledge pre- and post-intervention. The association of acceptance of dual methods with a number of identified independent variables was measured by odds ratio and their 95% confidence intervals (CI). All variables significant at P<0.05 in univariate analysis were entered in multivariate analysis using step-up method, to identify factors determining acceptance of dual methods in the intervention group. Risk of pregnancy in one year of contraceptive use was derived as a product of known contraceptive failure rate of each method (perfect use and typical use for condom only)22 and number of women using a particular method in each group. The cumulative failure rate depicts the number of women who are at risk of unintended pregnancy in each group in one year of contraceptive use.
Results
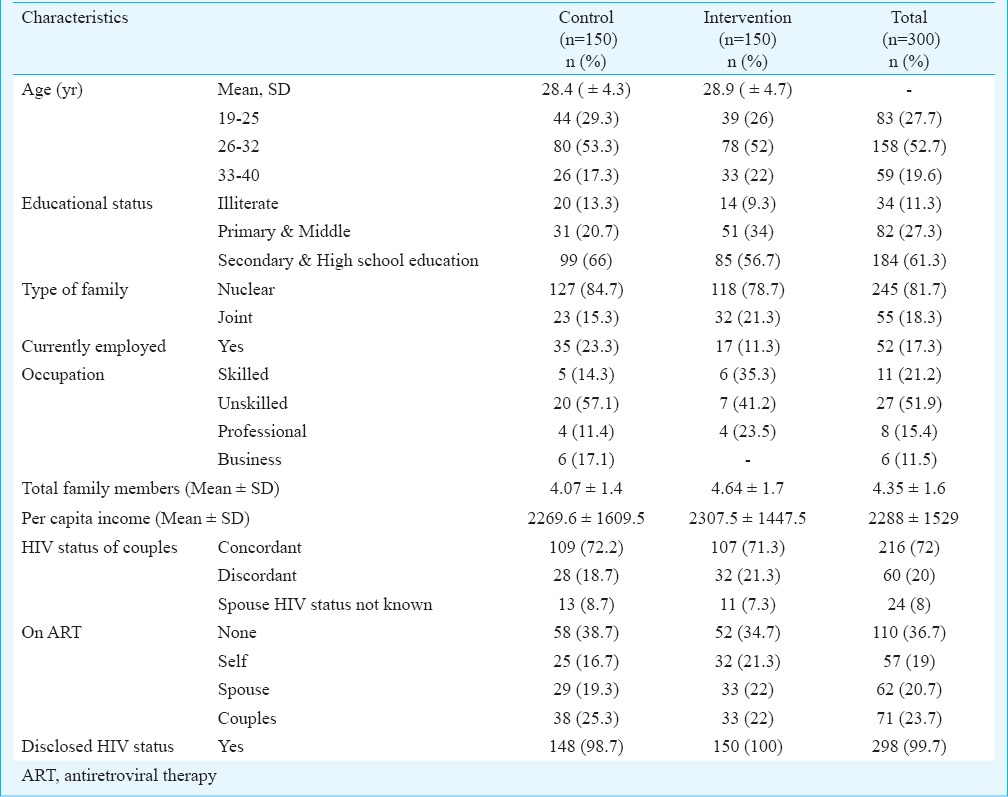
Profile of women: The two groups had matched background characteristics. The mean age of participants in both the groups was 28 (±4) yr with almost half of them belonging to 26-32 yr age group. About 11 per cent were illiterate in both the groups and about 81 per cent resided in nuclear families with a mean family size of 4.35 ± 1.6. Less than a quarter of the women were employed and the mean per capita income was  2288±1529. Each group had equal number of concordant couples (72%) and more than 99 per cent had disclosed their status to spouses (Table I).
2288±1529. Each group had equal number of concordant couples (72%) and more than 99 per cent had disclosed their status to spouses (Table I).
Table I.
Characteristics of participants
Change in awareness and knowledge: Overall knowledge on modern contraceptives was above 90 per cent for male condoms, IUD and female sterilization in both groups. A large number of infected women in both groups (42.7%) considered use of any modern contraceptive methods to be harmful especially the ones used for spacing such as IUD (32.7%), oral contraceptive pills (OCP, 19.3%) and injectables (2.7%). They also reported that the use of contraceptives depended on their sexual partner (90%) and other family members (11.3%).
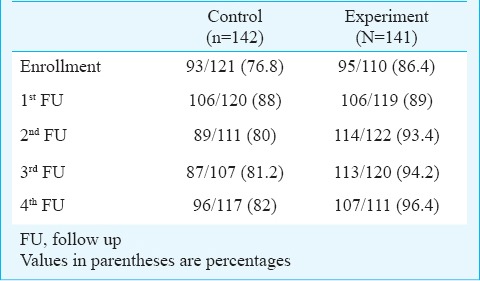
Significant differences (P<0.001) were observed post-intervention, in the intervention group compared to control group pertaining to knowledge on injectable contraceptives (96.5 vs 53%), female condoms (44 vs 18%) and emergency contraceptive (EC) pills (81.6 vs 30%). No significant difference was observed regarding knowledge of other methods as those were already above 90 per cent in both groups pre-intervention. A 10 per cent increase in awareness on dual protection was noted in control compared to 30 per cent in intervention group (Fig. 3). Similarly, 25 per cent improvement in knowledge about the need to use condom by concordant couples was observed in intervention group (73.7 to 99.3%) compared to only eight per cent increase in the control (65.3 to 73.2%) group (Fig. 4). These differences between intervention and control groups were significant (P<0.001).
Fig. 3.
Awareness on dual protection among enrolled HIV position women.
Fig. 4.
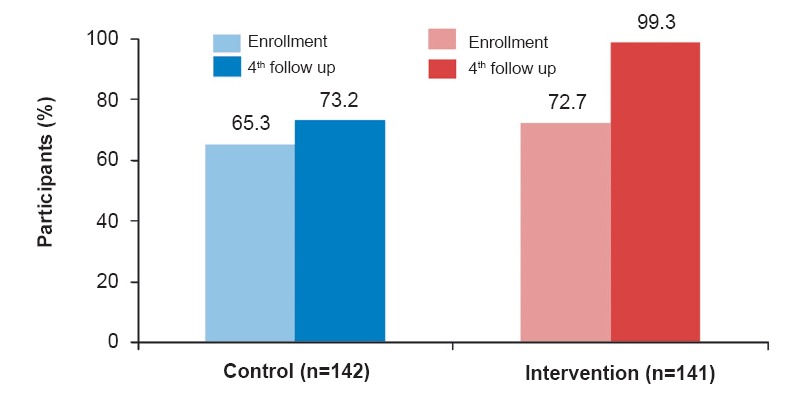
Awareness among HIV positive women about need to use condom if spouse is also HIV positive.
Accessed family planning services: Sixty per cent of participants in intervention group reached the family planning centres after they were referred from ICTC/PPTCT centres as against only eight per cent in the control group (P<0.001). At these centres, apart from the medical and paramedical staff, PPTCT counsellors also attended to them and provided information and counselling on family planning. The main reasons for women not reaching family planning centre were if they were psychologically not prepared to think of family planning after hearing their test result for the first time (13.7%); if they had already received all information on family planning at ICTC/PPTCT centre and needed time to decide (32.6%); if they were happy with only condom use/having infrequent sexual act (20%) and their priority was illness and medicines (2%); their decision depended on spouse or other family members (15.7%) or if they felt it was not ideal time of menstrual cycle to start using contraceptives (5%). A few preferred to visit health facilities close to their homes due to time and financial constraints (11%).
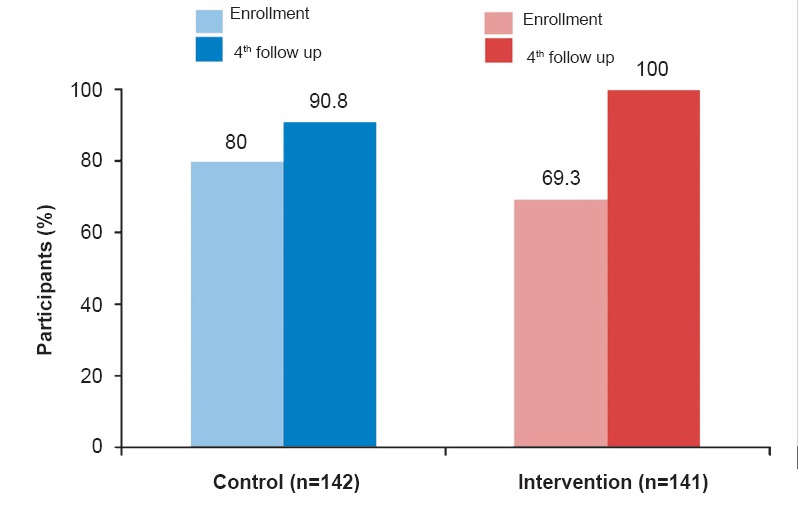
Acceptance of dual contraceptive methods: Overall 46 (32.6%, 95% CI-24.9-40.3) participants from the intervention group and 15 (10.6%, 95% CI-5.5-15.7) from the control group accepted dual contraceptive methods (Fig. 5). At the end of one year of follow up 39 (27.6%, 95% CI-20.2-35) and 12 (8.5%, CI-3.9-13.1) participants continued using family planning method from intervention and control groups, respectively. This difference was significant (P<0.001). Among those who accepted other contraceptives, spacing methods were most accepted in intervention group (n=33, 72%) compared to control (n=7, 47%). Among spacing methods, IUDs were the most accepted method.
Fig. 5.
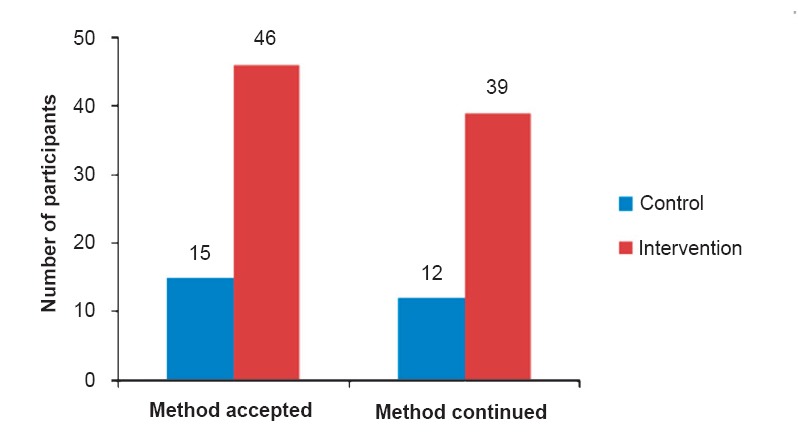
Dual methods accepted and continued by enrolled HIV positive women.
The proportion of couples using condoms was higher in the intervention group than control and this difference was significant throughout all the follow ups (Table II). Consistent use of condoms among dual method acceptors was 100 per cent in the intervention than only 50 per cent in the control group and this difference was significant (P<0.05). Five cases in control group reported non-use of condoms. Use of EC pills was limited to two cases in intervention group and none in control.
Table II.
Consistent condom use over one year by the spouses of sexually active participants
Fertility desires and reported pregnancies: Majority had one child (45%), 27 per cent had two and 25 per cent had three or more children. About three per cent were newly married and had no living child. Mean number of HIV positive children were 1.85 (±0.35) and 1.88 (±0.33) in each group, respectively.
At the time of enrolment, participants reported that they did not want to get pregnant at least for next one year. However, during the course of the study, change in fertility desire was observed in both groups. This was mainly due to their own health status, HIV status or health condition of their surviving child and due to family pressures. Reported number of pregnancies in intervention and control groups were 19 and 24, respectively. Among them, there were six planned pregnancies in intervention and four in control group. Unplanned pregnancies were higher in control (20 vs 13) compared to intervention group. However, the difference was not significant. Almost all women with unwanted pregnancies in the intervention group reported early in pregnancy and resorted to induced abortions compared to only nine among the control group. Post-abortion acceptance of various family planning methods along with regular condom use was universal in the intervention compared to only two cases in control group who underwent tubal ligation.
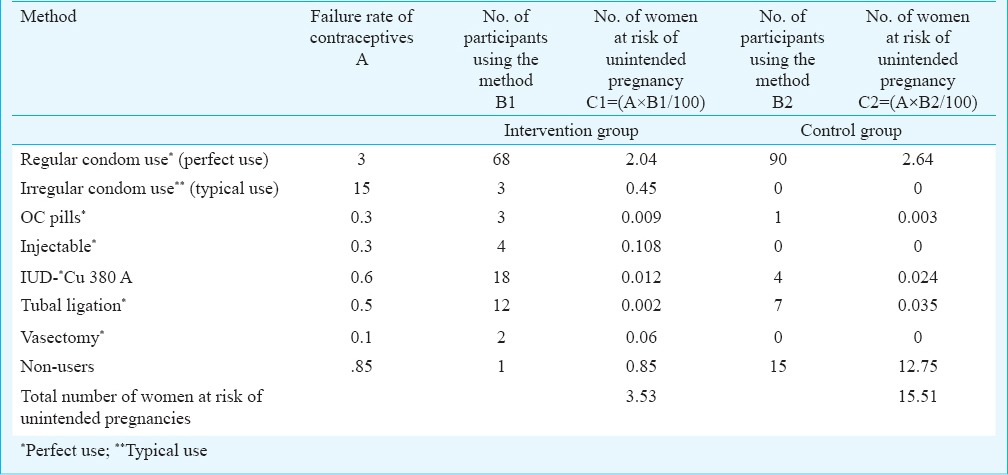
Due to increased protection offered by the use of dual method of contraception in the intervention group, the risk of unintended pregnancies in the first year of use reduced among 12 more women compared to the control group (Table III).
Table III.
Women at risk of unintended pregnancies
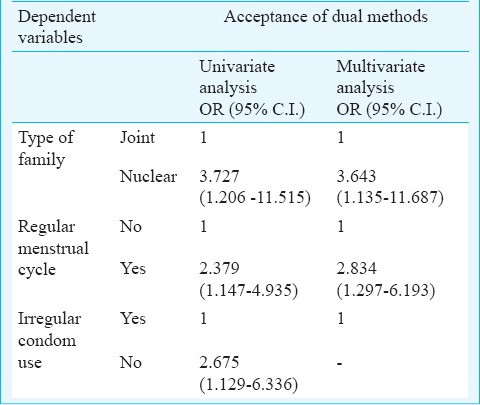
Factors associated with acceptance of dual contraceptive methods: Data from women in the intervention group (141) were analysed to find association between acceptance of dual methods (dependent variable) with a number of independent variables such as background characteristics, knowledge of contraception/dual methods, couples’ attitude towards dual contraceptive use, menstrual cycles, parity, HIV status of the couple/children, disclosure, family support and health condition of the woman. Analysis revealed significant association of acceptance of dual contraception to the following variables: residing in nuclear family (P<0.024), knowledge about limitations of condoms among women (P<0.008), if women were ready to use other methods especially injectable (P<0.034), couple was in agreement on the number of children they wished to have (P<0.083), women whose menstrual cycles were regular (P<0.010), and if positive women had comorbid TB infection (P<0.027).
Univariate analysis revealed that factors such as being in a nuclear family, women with regular menstrual cycles, history of irregular use of condoms and preference to use other contraceptive methods along with condom were significantly associated with acceptance of dual methods at 95% confidence interval (CI). All independent variables that showed significant association in univariate were considered for multivariate logistic regression using step-up method (except preference to use other contraceptive methods along with condom). The final determinants of dual method acceptance after interventions were: belonging to a nuclear family (OR 3.643, CI- 1.135-11.687) and women who had regular menstrual cycles (OR 2.834, CI-1.297-6.193) (Table IV).
Table IV.
Factors associated with acceptance of dual methods by HIV positive women
Discussion
The current PPTCT programme in India is pregnant women centric. The PPTCT guidelines are to a great extent focused on provision of prophylactic regimen to infected pregnant women. In the present study we made an effort in bringing programmatic focus on Prong 2 and testing the feasibility to provide HIV family planning linked services in tertiary settings in India. The intervention of repeated contraceptive and safe sex counselling messages during every follow up interaction has facilitated decision making in women to visit family planning centres and access contraceptive services.
It has been observed that decision of using contraception is to a large extent based on the agreement of the spouse, support from family which is also dependent on the status of disclosure and how well the couple is able to negotiate family pressure for more children or for a male child23,24. As seen in our study, nuclear family and a strong determination among women to avoid pregnancy facilitated use of dual methods. Women who had regular cycles reported higher possibility of using dual methods as it made them feel more vulnerable to get pregnant. Since most of the participants in the intervention group were regular users of condom it did not feature as an important predictor of dual method use.
As has been recommended25, it is important to incorporate fertility-related counselling, as well as contraception and advice regarding safe motherhood, as appropriate, into HIV treatment services to meet the fertility desires of HIV positive people which change overtime.
We observed good acceptance and retention of intra-uterine contraceptive device in our study. A study from Thailand revealed that long term contraceptives were less of a risk among PLHIV as these were more effective without any risk of drug interactions26. The findings of our study revealed that there was more acceptance of spacing methods than permanent methods in the intervention group compared to control. Our study also demonstrated that promotion of dual methods improved consistent condom use. This is contrary to the dual method hypothesis proposed by a Brazilian group27 which postulates that condom use reduces if PLHIVs use more effective contraception. Unlike our results, a Brazilian study demonstrated that women using an irreversible method were more likely to use condoms regularly than those using a reversible method. The same study also showed that women on ART and with a serodiscordant partner had greater odds of consistent condom use than their counterparts28. Our study did not find any such associations.
The three times increase in acceptance and continuation of dual methods along with near 100 per cent consistent condom use in intervention group revealed that intervention was able to improve this chronic programmatic challenge. As reported in a study in Kenya28 no significant reduction in pregnancies between the two groups was observed mostly due to short period of observation of one year. However, the small number of averted pregnancies would be a significant proportion when extrapolated to the country's large eligible population wishing to prevent unintended pregnancies. The generated proof of concept needs to be tested further in an implementation research mode in larger and varied settings of the public health system.
The study concludes that linking HIV and family planning services at tertiary level of care may be feasible. This linkage led to improved use of dual methods and the consistent condom use which did not reduce even if couples accepted other modern methods of contraception. Programme directives for HIV family planning linked services need to be drafted and issued along with country-specific standard guidelines for provision of family planning among PLHIV. A strong advocacy on use of dual methods for dual protection is necessary to encourage couples make informed choices to plan pregnancies.
Acknowledgment
Authors thank ICMR for providing financial support to conduct the study, and acknowledge the cooperation extended by authorities and staff of the two study sites, Mumbai District AIDS Control Society and the study participants. Authors thank Dr Sanjay Mehendale, Director, National Institute of Epidemiology (ICMR), Chennai, India, for critically reviewing and editing the paper.
Footnotes
Conflicts of Interest: None.
References
- 1.PMTCT strategic vision 2010-2015: Preventing mother-to-child transmission of HIV to reach the UNGASS and Millenium Development Goals. Moving towards the elimination of paediatric HIV. Geneva: WHO; 2010. World Health Organization (WHO) [Google Scholar]
- 2.National Institute of Medical Statistics (ICMR); National AIDS Control Organisation, Government of India. Technical report, India 2012. HIV estimates. [accessed on February 1, 2015]. Available from: http://www.naco.gov.in/upload/Surveillance/Reports%20%26%20Publication/Technical%20Report%20-%20India%20HIV%20Estimates%202012.pdf .
- 3.Updated guidelines for prevention of parent to child transmission (PPTCT) of HIV using multi drug anti-retroviral regimen in India, December. 2013. [accessed on February 10, 2015]. Available from: http://naco.gov.in/upload/NACP%20-%20IV/18022014%20BSD/National_Guidelines_for_PPTCT.pdf .
- 4.Sweat MD, O’Reilly KR, Schmid GP, Denison J, de Zoysa I. Cost-effectiveness of nevirapine to prevent mother-to-child HIV transmission in eight African countries. AIDS. 2004;18:1661–71. doi: 10.1097/01.aids.0000131353.06784.8f. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization (WHO). Strategic approaches to the prevention of HIV infection in infants: report of a WHO meeting, March 20-22, 2002. Morges, Switzerland, Geneva, Switzerland: WHO; 2003. [Google Scholar]
- 6.Singh S, Darroch JE, Vlassoff M, Nadeau J. Adding it up, the benefits of investing in sexual and reproductive health care. New York: Alan Guttmacher Institute; 2003. [accessed on December 5, 2013]. Available from: http://www.unfpa.org/webdav/site/global/shared/documents/publications/2004/addingitup.pdf . [Google Scholar]
- 7.Reynolds HW, Steiner MJ, Cates W., Jr Contraception's proved potential to fight HIV. Sex Transm Infect. 2005;81:184–5. doi: 10.1136/sti.2004.012013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Petruney T, Minichiello SN, Wilcher R, McDowell M. Meeting the contraceptive needs of key populations affected by HIV in Asia: An unfinished agenda. AIDS Res Treat 2012. 2012 doi: 10.1155/2012/792649. 792649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McCarraher DR, Vance G, Gwarzo U, Taylor D, Chabikuli ON. Changes in contraceptive use following integration of family planning into ART Services in Cross River State, Nigeria. Stud Fam Plann. 2011;42:283–90. doi: 10.1111/j.1728-4465.2011.00291.x. [DOI] [PubMed] [Google Scholar]
- 10.Contraception cost-effective for preventing mother-tochild transmission of HIV. FHI Res Pract Bull. 2006. [accessed on February 10, 2014]. pp. 1–2. Available from: http://www.fhi360.org/sites/default/files/media/documents/Contraception for PMTCTenrh.pdf .
- 11.Hladik W, Stover J, Esiru G, Harper M, Tappero J. The contribution of family planning towards the prevention of vertical HIV transmission in Uganda. PLoS One. 2009;4:e[7691]. doi: 10.1371/journal.pone.0007691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gillespie D, Bradley H, Woldegiorgis M, Kidanu A, Karklins S. Integrating family planning into Ethiopian voluntary testing and counselling programmes. Bull World Health Organ. 2009;87:866–70. doi: 10.2471/BLT.09.065102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adair T. Desire for children and unmet need for contraception among HIV-positive women in Lesotho. USAID DHS Working papers, March 2007, No 32: 1-24. [accessed on April 14, 2014]. Available from: http://pdf.usaid.gov/pdf_docs/Pnadi792.pdf .
- 14.Rutenberg N, Siwale M, Kankasa C, Nduati R, Ngacha DM, Oyieke J. Horizons Research Summary. Washington, D.C: Population Council; 2003. Family planning and PMTCT services: examining interrelationships, strengthening linkages. [Google Scholar]
- 15.Glion consultation on strengthening the linkages between reproductive health and HIV/AIDS: family planning and HIV/AIDS in women and children. WHO/HIV/2006. 02. Geneva: WHO; 2006. World Health Organization (WHO) [Google Scholar]
- 16.Inter-agency Task Team for Prevention and Treatment of HIV Infection in Pregnant Women, Mothers and their Children: Preventing HIV and Unintended Pregnancies, Strategic Framework UNFPA. 2011-2015. [accessed on January 5, 2014]. Available from: www.unfpa.org/…/PreventingHIV_UnintendedPregnancies_SF2011_2015 .
- 17.Brickley DB, Almers L, Kennedy CE, Spaulding AB, Mirjahangir J, Kennedy GE, et al. Sexual and reproductive healthservicesfor people living with HIV: a systematic review. AIDS Care. 2011;23:303–14. doi: 10.1080/09540121.2010.507746. [DOI] [PubMed] [Google Scholar]
- 18.Spaulding AB, Brickley DB, Kennedy C, Almers L, Packel L, Mirjahangir J, et al. Linking family planning with HIV/AIDS interventions: a systematic review of the evidence. AIDS. 2009;23(Suppl 1):S79–88. doi: 10.1097/01.aids.0000363780.42956.ff. [DOI] [PubMed] [Google Scholar]
- 19.Suryavanshi N, Erande A, Pisal H, Shankar AV, Bhosale RA, Bollinger RC, et al. Repeated pregnancy among women with known HIV status in Pune, India. AIDS Care. 2008;20:1111–8. doi: 10.1080/09540120701842753. [DOI] [PubMed] [Google Scholar]
- 20.Chakrapani V, Newman PA, Shunmugam M, Dubrow R. Prevalence and contexts of inconsistent condom use among heterosexual men and women living with HIV in India: Implications for prevention. AIDS Patient Care STDS. 2010;24:49–58. doi: 10.1089/apc.2009.0214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.WHO. Medical eligibility criteria wheel for contraceptive use - 2008 update. [accessed on February 10, 2014]. Available from: http://www.who.int/reproductivehealth/publications/family_planning/9.....789241547710/en/
- 22.Trussell J. Contraceptive efficacy. In: Hafcher RA, Trussell J, Nelson AL, Cates W, Stewart F, Kowal D, editors. Contraceptive technology. 19th ed. New York: Ardent Media; 2007. [Google Scholar]
- 23.Jayaraman A, Mishra V, Arnold F. The relationship of family size and composition to fertility desires, contraceptive adoption and method choice in South Asia. Int Perspect Sex Reprod Health. 2009;35:29–38. doi: 10.1363/ifpp.35.029.09. [DOI] [PubMed] [Google Scholar]
- 24.Myer L, Morroni C, Rebe K. Prevalence and determinants of fertility intentions of HIV-infected women and men receiving antiretroviral therapy in South Africa. AIDS Patient Care STDS. 2007;21:278–85. doi: 10.1089/apc.2006.0108. [DOI] [PubMed] [Google Scholar]
- 25.Preventing unintended pregnancies and HIV. FHI Bull Sep. 2012. [accessed on February 10, 2015]. pp. 1–6. Available from: www.fhi360.org/sites/default/files/media/documents/PMTCTbrief_0.pdf .
- 26.Landolt NK, Phanuphak N, Teeratakulpisarn N, Kriengsinyot R, Ahluwalia J, Pinyakorn S, et al. Uptake and continuous use of copper intrauterine device in a cohort ofHIV-positivewomen. The HIV Netherlands Australia Thailand Research Collaboration, Bangkok, Thailand. AIDSCare. 2013;25:710–4. doi: 10.1080/09540121.2012.752786. [DOI] [PubMed] [Google Scholar]
- 27.Tsuyuki K, Barbose RM, Pinho Ade A. Dual protection and dual methods in women living with HIV: The Brazilian context. J Sex Trans Dis 2013. 2013 doi: 10.1155/2013/540789. 540789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grossman D, Onono M, Newmann SJ, Blat C, Bukusi EA, Shade SB, et al. Integration of family planning services into HIV care and treatment in Kenya: a cluster randomised trial. AIDS. 2013;27(Suppl 1):S77–85. doi: 10.1097/QAD.0000000000000035. [DOI] [PubMed] [Google Scholar]


