Abstract
The disparate effects of social determinants of health (SDOH) on cardiovascular (CV) health status and health care have been extensively documented by epidemiology. Yet, very little attention has been paid to how understanding and addressing SDOH might improve the quality of clinical interactions, especially by improving patients’ adherence to recommended therapies. We present a case and suggested approach to illustrate how cardiovascular clinicians can use patient-centered approaches to identify and address SDOH barriers to adherence and reduce the impact of unconscious clinician biases. We propose that CV clinicians 1) Recognize that patients may have different belief systems about illnesses’ cause and treatment, which may influence their actions, and not to assume they share one’s experiences or explanatory model; 2) Endeavor to Understand the individual patient before you; 3) Based on that understanding, Tailor your approach to that individual. We suggest a previously-developed mnemonic for an approach to RESPECT the patient: First, show Respect; then elicit patients’ understandings of their illness by asking about their Explanatory model. Ask about the patient’s Social context, share Power in the interaction, show Empathy, ask about Concerns or fears, and work to develop Trust by building the relationship over time. We provide additional clinical resources to support these efforts, including lay descriptions of cardiovascular conditions, challenges to adherence and suggested strategies to address them.
Keywords: Adherence, Patient-centered Care, Disparities, Treatment disparities, Social determinants of health, Socioeconomic position, Race and ethnicity
Introduction: Social determinants of health (SDOH) drive health and health care disparities
Disparities in health status and health care processes, related to patients’ social and demographic characteristics and associated life experiences (e.g., socioeconomic position (wealth, income, education, employment status), race/ethnicity, social support, access to care, residential environment, and discrimination), remain pervasive in American society, and contribute to significant disparities in disability and death from cardiovascular disease (CVD) 1. Disparities in health care are those variations which are not attributable to treatment eligibility, clinical contraindications, patient preferences, or confounding by other clinical factors 2,3, which are associated with adverse consequences in health outcomes, and are of national public health concern,4. Racial and ethnic disparities in health status also have a striking and disparate impact on public health. For example, racial and ethnic disparities in hypertension are associated with 15% of black/white disparities in mortality due to income5, and cardiovascular disease is the largest cause of the 14-year sociodemographic gap in life expectancy in the Eight Americas Study, which defined 8 sub-populations of the United States based on race and county-level demographic characteristics 6, 7.
The 2015 American Heart Association Scientific Statement on the social determinants of risk and outcomes for cardiovascular disease (CVD) asserted: “…at present, the most significant opportunities for reducing death and disability from CVD in the United States lie with addressing the social determinants of cardiovascular outcomes.” [italics ours; 1]. Social determinants of CVD include the direct effects of personal characteristics, such as those listed above1. In addition, there are indirect psychological, behavioral, and biological mechanisms by which social determinants lead to or exacerbate CVD, with one of the most significant being adherence to recommended lifestyle or therapeutic prevention, or to secondary prevention after a cardiovascular event 1.
Cardiovascular Epidemiology has incorporated a ‘life-course’ approach to understanding SDOH risk factors for adult CVD 1, 8, 9, recognizing that life experiences and conditions are critical, and cumulative, determinants of health. This approach “accounts for the simultaneous and cumulative consideration of social and environmental health risks that burden socially disadvantaged communities” (8, page 1897). Put more concisely, deprivation and bad things that happen to people starting early in life have strong, cumulative and multiplicative effects on them physically and psychologically, leading to worse educational, occupational and health outcomes, and earlier death.
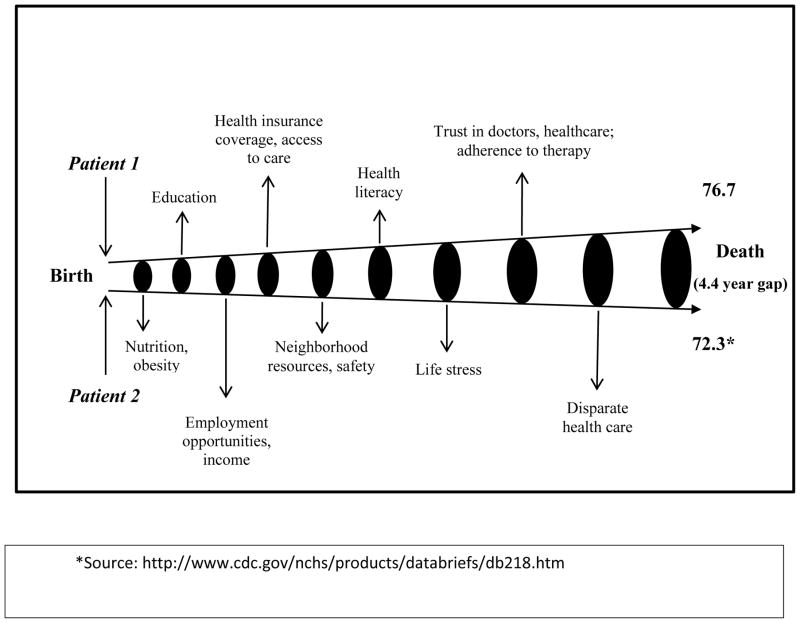
Thus, significant descriptive work in cardiovascular epidemiology has characterized the associations between disadvantage and the incidence of cardiovascular disease 1. Such disparities begin in the intra-uterine environment10, negatively affecting use of pre-natal care11, low birth weight12, infant mortality13, breastfeeding14 and early childhood nutrition15. They continue with differential access to preschool, kindergarten readiness16, and elementary school success17, later affecting high school graduation rates and access to higher education18, which in turn influences occupational opportunities, income19 and access to health insurance 20. Disadvantage may also include housing segregation, with associated disparities in exposure to community violence, housing quality, toxic chemicals and air pollution 21, and experiences of racial or other discrimination22. Such disadvantage also affects nutrition, obesity, food availability, and the odds of incident cardiovascular disease1, and access to high quality health care 23. Figure 1 illustrates the multitude of ways in which two lives of ‘disparate’ experiences and access to resources can result in wide gaps in outcomes including mortality.
Figure 1.
A lifetime of disparities.
The life-course approach illustrated here demonstrates the cumulative and progressive impact of the direct and indirect social determinants of cardiovascular disease. Each dimension (e.g., nutrition, education) listed can be a positive or negative influence, depending on a person’s access to resources or exposure to disadvantage. In this example, Patient 1 has had consistent advantages, while Patient 2 has had consistent disadvantage; the net result is a 4.4 year difference in life span in two hypothetical men, one black and the other, white, as per the Centers for Disease Control’s 2013 mortality data.
Along disparate pathways from birth to death, most individuals interact with the healthcare system (Table 1). There, already-disadvantaged patients may experience further disparities – unequal treatment, by virtue of their sociodemographic characteristics–in healthcare and resulting outcomes 2, 3, 24, 25,26–28
Table 1.
Case Presentation
| Overview | |
| A 55-year-old man with a history of hypertension, hyperlipidemia, tobacco dependence and obesity presented to the Emergency Department with chest pressure. NSTEMI was confirmed and the workup resulted in placement of a bare metal stent. Appropriate medications were initiated that included dual antiplatelet therapy, high-intensity statin and a beta blocker. For blood pressure control, the patient was started on a thiazide and ACE inhibitor. | |
| Medication therapy and lifestyle counseling were discussed during his inpatient stay. A two week follow-up visit with the cardiologist was scheduled. | |
| Patient 1 | Patient 2 |
| He has been adherent to his prescribed med regimen. | He misses the scheduled 2 wk cardiology appointment due to his work schedule |
| He is curious about his blood pressure reading which is above goal. | With outreach from the cardiologist’s office he does present for an appointment 2 wk later. |
| He has gone on-line and has questions about an article he read about obesity and heart disease. He is interested in an exercise regimen and wonders when it will be ok to exercise again. | He expresses concern about taking so many medications. On review, he has been taking his blood pressure medication and aspirin only when he has a headache. TV commercials regarding statins’ side effects dissuaded his use. |
| He admits he is worried that this could happen again. Of note, he hasn’t smoked a cigarette since his hospitalization. | Everyone around him smokes so he has found it hard to cut down. |
| These two patients are clinically similar and the same therapy is appropriate for both. Yet, there are differences in their adherence. How might you approach each of them to ensure the best outcomes for both? Picture each patient in your mind; what kind of a person are they? What do they look like? | |
Clinician bias – whether conscious or unconscious – is a potential contributor to disparities, through differential clinical decisions, its effect on clinical interactions and communication, or on patients’ anticipation of discriminatory or stereotypical treatment1. Regardless of conscious intent, social psychology has amply demonstrated that we all make unconscious judgments about others, based on their social, physical and other characteristics, which may in turn drive our behaviors toward them. Thus, even well-meaning clinicians may make and act upon unconscious assumptions about patients, based on their race/ethnicity, social class, education, etc., which may lead to disparate care. We found, for example, that cardiologists anticipated significantly greater treatment adherence from white (versus black) patients29. Other evidence from social psychology, however, supports the value of several strategies for reducing the effects of unconscious biases. It is important to recognize that such biases may exist, accept that they are a natural part of human cognitive functioning that helps us make sense of the world 30, yet be vigilant in detecting biases in our own thinking, and develop tactics and systems that foster more conscious patterns of interactions to reduce racial and other biases to help to address them 31. Thus, increasing clinicians’ skills in developing empathy with patients, and enhancing clinicians’ ability to take patients’ perspectives and to build partnerships with them, can mitigate bias 32. In turn, such activities may increase clinicians’ (and patients’) positive emotions in clinical encounters, which can simultaneously mitigate bias and enhance physicians’ satisfaction with their work 33.
Successful organization-level efforts to reduce healthcare disparities have recognized, identified and addressed disparities in processes of care, often through quality improvement methods 26–28. Other promising approaches include cultural and patient-centered tailoring, use of multidisciplinary clinical teams, and interventions aimed at multiple leverage points28. However, despite some successes, many outcomes remain stubbornly disparate34,25,6; even as CVD mortality has declined overall, disparities (especially by race/ethnicity) in such mortality have remained constant35, 36.
How Can the Epidemiological Evidence About Social Determinants of Health Inform the Provision of Clinical Care?
A lifetime of disparities in social determinants of health leads to disparate risk for CVD, as has been extensively described by cardiovascular epidemiology. 1, 37, 38 Yet, many cardiologists’ initial encounters with sociodemographically disadvantaged patients occur only in the acute care setting following a CV event. The Case suggests such an encounter and illustrates the adverse contributions of social and demographic factors in CVD care and secondary prevention, as well as the ways in which physicians’ recognition of and ability to address the social realities of their patients, and their own unconscious biases, may affect care and outcomes. It is of course not possible for clinicians to address or counteract the disparate life experiences that occurred prior to a patients’ CV event. Yet, clinicians are still faced with patients whose life experiences may have led to this point and which will influence their willingness, ability, or means to utilize or adhere to recommended healthcare now. At this juncture, the goal of care is to minimize further risk through ongoing medical therapy and lifestyle change. Thus, patients’ acceptance and adoption of recommended therapy pose a crucial gateway to opportunities for maximizing adherence and minimizing disparities in future outcomes 39, 40. Cardiologists’ ability to recognize and act upon the sociodemographic factors contributing to their patients’ health and health-related behaviors is crucial to bending the curve of disparities. Recognition and understanding of the social determinants of disease can then guide patient-centered care strategies and bolster patient adherence41–43.
Central to enhancing adherence is patient-centered care, one of the six pillars of quality care in the Institute of Medicine’s report, Crossing the Quality Chasm44. Patient-centered care is defined as “respecting and responding to patients’ wants, needs and preferences, so that they can make choices in their care that best fit their individual circumstances”(p 48–50). Key to a patient-centered approach is good communication, based on an understanding of patients’ life experiences, values, and identity. The evidence is clear that patient-centered communication leads to improved outcomes, including self-management of chronic conditions, adherence to recommended therapy, and patient satisfaction 45, 46.
Adherence to therapy is a function of many factors, according to the World Health Organization 47, including patients’ sociodemographic characteristics and clinician-patient relationships 48,39, 49. Multi-level interventions are most effective at improving adherence 50,51, 52 yet healthcare systems are not always able to implement them. Individual clinicians can address adherence in their own practices through a deepened understanding of individual patients, and by providing counseling and accountability 53. However, few physicians directly inquire about adherence 48, 54, missing a key opportunity to identify patients in need of further support.
Clinicians may be concerned that addressing social determinants of health in the clinical setting will negatively impact efficiency, by requiring excessive time. This view may be a ‘false economy’, in that saving time in the short run by not addressing social determinants of health or how they might affect adherence can lead to nonadherence and worse outcomes, including hospital readmission and additional events. In fact, evidence indicates that patient centered approaches can actually help doctors obtain better information more efficiently, which can be used to enhance adherence55–58. Systematic screening for social determinants of health, accompanied by referrals to address gaps, results in greater connections to community resources 59, which may in turn enhance patients’ ability to adhere or otherwise care for their own health.
Further supporting the critical importance of adherence is the fact that the Centers for Medicaid and Medicare and other organizations’ performance metrics are increasingly focusing on clinicians’ ability to help patients adhere to recommended CVD therapies, including antihypertensive medications, and lipid-lowering agents 60, 61. Thus, it is progressively more important for clinicians to hone their skills in helping patients maximize adherence, to improve outcomes and to maximize reimbursements for such care.
The cases: Two different patients illustrate the varying influence of social determinants of health on adherence
Tables 2 and 3 present additional detail on the cases, to illustrate various social determinants of health which may influence adherence to recommended therapy, and strategies clinicians (including physicians, nurses, clinical pharmacists, nurse practicitioners and physicians’ assistants) can use to maximize adherence. We discuss the cases from both the physicians’ (Table 2) and patients’ (Table 3) perspectives, with the goals of developing a deeper understanding of the dynamics of how SDOH undergird disparities in adherence. Our objective is to provide strategies that cardiologists can use to understand and reduce disparities in their own clinical practice.
Table 2.
Case presentation, continued
| The physician’s thoughts | |
|---|---|
| Patient 1 | Patient 2 |
|
Physician thoughts (unvoiced to the patient) “This patient is appropriately concerned about his recent event. He has stopped smoking, is adhering to the medications, has made an effort to learn more about his condition, and has begun to make needed lifestyle changes. I will see him back in a month and am optimistic about his recovery and future progress.” |
Physician thoughts (unvoiced to the patient) “His blood pressure is uncontrolled, one month after an NSTEMI, and he has missed appointments. He’s only taking the antihypertensives intermittently and not taking the statin at all. It’s hard to see how we can help someone who doesn’t show up for his appointments and doesn’t take the medication we prescribe.” |
Table 3.
Case presentation, continued
| The patient’s perspective* | |
|---|---|
| Patient 1, continued | Patient 2, continued |
|
Patient thoughts (unvoiced to the physician) “That chest pain was awful, and it scared me to be in the hospital, to learn I’d had a heart attack, and to get the stent. I knew my blood pressure was a little high, but didn’t realize that 170/120 was such a big deal. This whole experience was a wake-up call and now I understand how important it is to take my blood pressure medications, as well as the statins, and other new medications they gave me, to exercise and get my weight down. The doctor said I was lucky, that the heart attack could have been much worse, and that if I take the medications he’s given me, lose some weight, and exercise more, I have a good chance of seeing my grandchildren grow up, many years from now.” |
Patient thoughts (unvoiced to the physician) “That chest pain was awful, but I still wasn’t going to go to the hospital – I figured that if I waited it out, it would go away. But my sister made me go to the emergency room. I was shocked to hear I’d had a heart attack, since I didn’t think it was my time to go. I’d been told my pressure was high several years ago, but my pressure normally runs high, and since then I’ve tried to stay calm, even though there’s a lot of stress on my job and if I miss time, I don’t get paid, and if I don’t get paid, I can’t pay the rent, and my sister depends on me for the apartment. But I haven’t had any headaches recently, so I figured I was doing all right. The doctor in the hospital (who I’d never met before) gave me prescriptions for a bunch of medicines, but I don’t know what they are all for, and even though I have insurance, they will still cost me plenty. That doctor doesn’t know me and I don’t know him. I saw a commercial that said one of the pills can give me muscle pain, and a lawyer was advertising that people can go to court over the bad effects of that medicine. I don’t need that since I do a lot of lifting at work, so I’m not taking that one at all. I feel fine now. It just wasn’t my time to go.” |
Note. We have deliberately not stated the patients’ races, in this case. Did you make an assumption about each patient’s race? Did this assumption affect your thoughts about the patients’ adherence or whether/how you could address it? Perhaps Patient 1 is white and Patient 2 is black, but the reverse is also possible. Consider why race might be important (or not), as well as the other aspects of these patients and their lives which might influence their adherence.
Some patients’ value systems are congruent with the “biomedical view”
The biomedical view holds that that illness and disease are a function of physical processes, including pathology, biochemistry or physiology, and does not take into account the role of social factors 62 62. Patient 1 demonstrates a proactive approach to understanding the nature of his disease, predisposing factors, medication treatment and risk modification strategies. Such an orientation is congruent with the biomedical model, which asserts that patients can take control over their disease through adherence to therapy and lifestyle change. This reflects an underlying sense of personal control over his fate and a perspective oriented toward the future. This man’s respect for the biomedical model is congruent with most physicians’ views and in accordance with physician expectations. This patients’ obvious respect for what his doctors have told him, his perception that he can be the master of his own fate, and his orientation toward having a healthy future reflect an endorsement of the biomedical view. Physicians may experience such an individual as a model patient.
Other patients’ value systems may differ from the biomedical view
Patient 2 demonstrates some doubt about the information and therapeutic plan he has been given, and various aspects of his life interfere with his adherence to the plan. The advice given during the hospitalization regarding aftercare and need for medication therapy seems to have been eroded by perceived side effects and information from TV commercials, as well as his own beliefs about his conditions and what might help treat them. This is not uncommon; patients often hold different views about their conditions and effective treatments than the biomedical model 63, 64. For example, our and others’ work has revealed that many patients view hypertension as a stress-induced condition which can be remedied by lifestyle changes to reduce stress 54, 63. Patients may hold beliefs about disease causality that are unrelated to biomedical explanations, and such beliefs may vary by SDOH. We found, within a primary-care based sample of white and black patients with hypertension, that African American patients were significantly more likely than white patients to believe that a germ or virus, pollution, or poor medical care caused their hypertension, 65. A potential natural consequence of such views is the belief that antihypertensive therapies will not address the perceived cause of the condition, which in turn will likely affect adherence.
Further, terminology used for CVD conditions may also affect adherence, a notion supported by the Agency for Healthcare Research and Quality’s Literacy Universal Precautions Toolkit66. For example, the term ‘hypertension’ is interpreted by many patients to mean that the condition represents excess stress, leading to views that its treatment should involve stress reduction63. We thus suggest use of the term ‘high blood pressure’, instead.64 Decreasing the use of technical terms and medical jargon is an important general communication strategy to improve patient comprehension67.
Note that patient #2 does not detect any symptoms, and he says that the high measured BP is ‘normal’ for him. In addition, his limited health literacy and/or different culturally related world view about illness and what it means has led to a non-biomedical understanding of his condition and the means to treat it 54, 63. His social context is such that taking time off from work means he will lose pay, jeopardizing his ability to pay his rent, and his sister’s living situation. His poorer quality health insurance has high prescription copayments and he will incur significant out-of- pocket costs for the prescribed medications.
Yet, upon further questioning, one begins to understand the deliberate decision making that undergirds his seeming non-adherence. This patients’ rationale for not quickly going to the ED was that he anticipated that the ‘spell’ would pass. His reasoning for not taking the BP medications is that they will interrupt his sleep due to increased need to urinate, and he has actively devised an alternative treatment strategy to decrease his stress, (and thus, he thinks, his high blood pressure) which makes sense to him given his explanatory model. Then, when high BP symptoms become detectable, he will take his antihypertensive medication. In this case, the patient is actively addressing his medical problems, albeit not in the way his doctor has prescribed. Writing this patient off as ‘non-compliant’ misses the underlying complexities of his situation and opportunities to address it. For example, could his clinic appointments be scheduled to better accommodate his work schedule so that he does not have to miss work? Could any of his care be managed by phone? Could a visit with a clinical pharmacist or health or peer educator help him understand the rationale for the medications, and help the care team to better understand the social situation or views of the patient? If the physician does not understand the patient’s model of hypertension as a stress-induced condition, then the opportunity to share information about the biomedical view and how it might benefit the patient is lost.
Asking open-ended questions about the patient’s view of the condition’s causes and effective treatments, as well as his social context, might provide opportunities to address this patient’s concerns, reveal barriers to adherence, and potential strategies to address those concerns66. In addition, open-ended questions can convey that clinicians are truly interested in what the patient has to say, and can increase feelings of trust in the provider, which is particularly important to racial/ethnic minority patients 41, 68. Asking a yes/no question as to whether he is taking his antihypertensive medications will elicit the answer “yes”, which is true. However, a more open-ended question would lead to more and better information as to how he is taking his medications (when he gets a headache, so only infrequently), an important detail. In such an approach, the patient is appreciated as their own expert on their health care experiences and on the choices they make.
Value systems or explanatory models that are incongruent with the biomedical model might contribute to lower adherence rates 54, 69. Not all patients adopt a biomedical, numbers-based, future-oriented, linear view of illness and disease. Nor do all patients embrace the notion that they have and can exert personal control over their health. Not recognizing potentially different belief systems can cause clinicians to miss important clues as to whether and how patients are adhering, and if not, why not. Clinicians can learn about patients’ explanatory models by asking questions like, “What do you think caused your symptoms?”, and, “Why do you think this started when it did? What do you think will solve the problem?” 70 Answers to these questions can provide insights into unanticipated barriers to adherence that can potentially be addressed – but they must be identified first.
Depending on their value system, some patients will be motivated by numbers, such as the percentage decrease in mortality or recurrence of cardiac events with control of blood pressure (a number)69. Others do not relate to (or understand) such numbers but might be motivated by the quality of life and interpersonal relationship costs of non-adherence, i.e. avoiding another cardiac event so as not to disrupt family responsibilities. Some might feel individually empowered by their sense of personal control over their destiny while others might be more reliant on a higher power or an acceptance of family trends in health status (e.g. ‘my father died of a heart attack at my age, so I’ve always expected the same will happen to me’). For some patients, the establishment of a trusting relationship must occur before they will accept medical recommendations –a caring and trusting relationship might be more motivating than data about risk reduction 41, 68. Particularly for racial/ethnic minority patients, the history of unfair treatment 71, and ongoing perceptions and experiences of racial/ethnic discrimination in society and in the healthcare context72 may lead to expectations of unfair treatment by physicians, or other members of the healthcare team. Doctors can best address this by making efforts to build trust through demonstrations of empathy and concern, by listening, and through open communication.
In addition, patients’ social context undergirds their ability to understand the condition (e.g., health literacy), determines how their illness affects their life, and in turn, how their life affects the illness and ability to adhere to recommended therapies. Asking directly about social context may uncover important barriers to adherence that can be addressed – by the physician or other members of the healthcare team43.
How might a clinician efficiently tackle the process of recognizing, understanding and tailoring care, based on patients’ social determinants of health? The remainder of this article suggests strategies and tools to do so.
Principles and strategies for identifying and addressing how social determinants of health affect adherence
The fundamental principles, discussed below, are to 1) Recognize that patients may have different belief systems about illnesses’ cause and treatment, which may influence their actions, and don’t assume they share your experiences or explanatory model; 2) Endeavor to Understand the patient you are dealing with; 3) Based on that understanding, Tailor your approach to that individual.
With recognition of potential differences or biases as the starting point, one can become open to the possibility of patients having different belief systems about illness’ causes and treatment, as well as the value and purpose of adherence. Also important to recognize is that while it may seem that patients are doing ‘nothing’ in response to recommended care, they are often actively trying to determine what is wrong with them, why it happened, and what they can do to manage it. This may or may not include prescribed medical therapy.
By developing a better understanding of the individual patient before you, and the social determinants that have affected their lives and their health, you will have a better understanding of who you are dealing with and how to better help them. Understanding patients’ health literacy, life story/context, health beliefs and explanatory model provides vital information you can use to target your approach. Table 4 describes an approach to help clinicians or learners at all levels to ‘Respect’ the patient, which can enable a better understanding and mitigate potential biases 43. This approach is a mnemonic for a set of skills and behavioral approaches (including both non-verbal and verbal), for which Table 4 lists examples and suggested scripts. Starting by showing Respect for the value and autonomy of the patient, and the validity of his/her concerns, Mostow and colleagues next advocate eliciting patient’s understandings of their illness, by asking about their Explanatory model (the patient’s understanding of what causes their illness and what will help it). They next suggest asking about the patient’s Social context, including social determinants of health that impact illness and which illness will impact, including stressors, supports, strengths, and spiritual resources. Next is sharing Power in the interaction, starting by recognizing that doctors have greater status, control, resources, options, and ability to produce desired outcomes, and finding ways to share such power. Then, show Empathy, by validating patients’ emotions. Next, ask about Concerns or fears, including worries about symptoms, diagnoses, or treatments. Then, work to develop Trust by building the relationship over time, through understanding, power-sharing and empathy. Table 4 details definitions, behaviors, and suggested scripts to address each concept.
Table 4.
Guiding skills and principles to address disparities through RESPECT (adapted from Mostow43)
| Principle | Definition | Behavioral Description | Examples of what to say |
|---|---|---|---|
| R: RESPECT show |
a demonstrable attitude communicating the value and autonomy of the patient and the validity of his/her concerns |
Non-verbal: lean forward, maintain appropriate eye and personal contact, follow cues regarding personal space, physical contact, and appropriate greetings Verbal: welcome patient, introduce self and role on team, ask patient how they want to be addressed, recognize and affirm strengths and efforts |
“Hi Ms./Mr. XXX, I’m Doctor X, one of the heart doctors here.” “What would you like me to call you?” |
| E: EXPLANATORY MODEL ask |
The patient’s understanding of their illness, what it is called, how it works, and what will help it. |
Nonverbal: give patient space to share their ideas. Listen without judgment. Verbal: ask patient about their views |
“What do you think is causing your symptoms? What do you think will solve the problem?” |
| S: SOCIAL CONTEXT ask |
Impact of patient’s life on illness and illness on his/her life. Includes stressors, barriers to health/adherence, supports, strengths, resources that influence health or healthcare. |
Nonverbal: show interest and pay attention Verbal: ask patient how the illness affects their life and how their life affects their illness |
“What should I know about you to care for you best? What is hardest for you regarding your illness? What and who helps you keep going and do what you need to do?” |
| P: POWER share |
Access to status, control, resources, options; ability to produce desired outcomes. NOTE: the power gradient favors doctors. |
Non-verbal: Reduce physical barriers; don’t dominate the interaction. Sit, limit interruptions, and make eye contact, with an open posture Verbal: Elicit the patient’s story with open-ended questions. Invite discussion and disagreement; share information; negotiate agenda and treatment plan and elicit preferences. |
“What would make it easier to take your medications? Thanks for telling me that you don’t agree. What do you think about this?” |
| E: EMPATHY show |
Verbal and nonverbal responses that validate patients’ emotions and cause them to feel understood |
Non-verbal: Listen attentively; minimize interruptions. Verbal: Name and validate patients’ emotions. |
“That must be hard, I can see why you would feel that way” |
| C: CONCERNS/FEARS ask |
Worries about symptoms, diagnosis or treatment, often unexpressed |
Nonverbal: head nods, indications of listening Verbal: ask open-ended questions about fears/concerns |
“What worries you the most? What scares or concerns you about the medications? Are you worried about sex after your heart attack?” |
| T: TRUST Develop and build together, over time |
Relationship built on understanding, empathy and power-sharing; patient confident that doctor acts on his behalf |
Non-verbal: Notice/respond to signs of distrust. Verbal: Elicit and respond to expectations. Reassure and clarify follow-up. |
“I’m here to help you”, “I care about you” |
Using the information gathered, one can better tailor the approach to that individual. An understanding of the patients’ health literacy level will help clarify what level of terminology to use. For patients with very low literacy levels, the National Heart Lung and Blood Institute and the American Heart Associations have developed lay definitions and explanations of common cardiovascular disease-related terms, which can be used to communicate more clearly to low-literacy patients (Table 5).
Table 5. Lay descriptions of common cardiovascular conditions.
, from the American Heart Association and the National Heart, Lung and Blood Institute
| 1. High Blood pressure (this term preferred over ‘hypertension’55): Blood pressure is the force of blood pushing against the walls of the arteries as the heart pumps blood. High blood pressure, sometimes called hypertension, happens when this force is too high. (Analogy: Blood pressure is like air in a tire -- blood fills arteries to a certain capacity. Just as too much air pressure can damage a tire, too much blood pressure can threaten healthy arteries. This is what we mean by ‘high blood pressure’). Over time, if the force of the blood flow is often high, the tissue that makes up the walls of arteries gets stretched beyond its healthy limit and damage occurs. This can also damage organs in your body like your heart and kidneys, and can lead to stroke, heart failure, kidney damage, or other problems. That’s why it’s important to keep your blood pressure ‘under control’. |
| 2. High cholesterol: Cholesterol is a waxy, fat-like substance that’s found in the body. High blood cholesterol is a condition in which you have too much cholesterol in your blood. People cannot detect if they have a lot of cholesterol; a blood test is needed. Many people don’t know that their cholesterol levels are high. People who have high blood cholesterol have a greater chance of getting coronary heart disease, also called coronary artery disease. |
| 3. Atherosclerosis is a condition that develops when a substance called plaque builds up in the walls of the arteries. This buildup narrows the arteries, making it harder for blood to flow through. If a blood clot forms, it can stop the blood flow. This can cause a heart attack or stroke. |
| 4. Heart Failure: Heart failure is a condition in which the heart can’t pump enough blood to meet the body’s needs. In some cases, the heart can’t fill with enough blood. In other cases, the heart can’t pump blood to the rest of the body with enough force. Some people have both problems. The term “heart failure” doesn’t mean that your heart has stopped or is about to stop working. However, heart failure is a serious condition that requires medical care. Heart failure develops over time as the heart’s pumping action grows weaker. |
| 5. Heart Attack?. A heart attack occurs when the blood flow to a part of the heart is blocked by a blood clot. If this clot cuts off the blood flow completely, the part of the heart muscle supplied by that artery begins to die. If blood flow isn’t restored quickly, the section of heart muscle begins to die. |
| 6. Arrhythmia: This is an abnormal rhythm of the heart. There are various types of arrhythmias. The heart can beat too slow (“Bradycardia”), or too fast (Tachycardia).. An arrhythmia can affect how well the heart works. The heart may not be able to pump enough blood to meet the body’s needs. |
| 7. Heart valve problems: When heart valves don’t open enough to allow the blood to flow through as it should, it’s called stenosis. When the heart valves don’t close properly and allow blood to leak through, it’s called regurgitation. When the valve leaflets bulge or prolapse back into the upper chamber, it’s a condition called valve prolapse. When this happens, they may not close properly. This allows blood to flow backward through them. |
| (Sources: http://www.nhlbi.nih.gov/health/health-topics, and http://www.heart.org/HEARTORG/Caregiver/Resources/WhatisCardiovascularDisease/What-is-Cardiovascular-Disease_UCM_301852_Article.jsp#.VplbVKrUiig) |
Tailoring can be done according to:
Literacy. It is possible to informally assess or use formal tools to assess literacy (e.g., Rapid Estimate of Adult Literacy in Medicine (REALM)73), and with that information, target explanations of disease, etiology, and treatment. Use easily understandable lay descriptions of CVD conditions (examples provided in Table 5).
Life story/social context. Capitalize on an understanding of patients’ prior experiences and aspects of their lives that affect their ability to adhere to therapy to inform the approach to discussing care with them.
-
Health beliefs and ‘explanatory model’. Based on an understanding of the patient’s views of their illness and efficacious therapies for it, one can identify issues to address to enhance understanding.
Adherence. Inquire about willingness to take medications; discuss possible modifications, e.g. treating one condition now, wait to treat another later. If already prescribed medications, ask about adherence, saying: “Some people find it hard to take their medications. How is it for you?” (few doctors make such inquiries, so doing this alone is a significant step 74). Table 6 lists potential barriers to adherence and suggested strategies for addressing them.
Assess understanding and agreement using ‘talk-back’, or “Ask-Tell-Ask”, as suggested by the Million Hearts Initiative75. First, “Ask” permission to provide information on a specific topic. Then “Tell” patients what they need to know, using simple and understandable language (examples in Table 5). Then, “Ask” patients, “Could you explain back to me what you understand about your condition and the treatment we have discussed?”. This will help you uncover misunderstandings, so they can be addressed.
Table 6.
Predictors of nonadherence and strategies to address them, from the Million Hearts Program75
| Predictors of Non-Adherence | Possible strategies to address this predictor of nonadherence |
|---|---|
| When discussing medications, be aware if your patient demonstrates limited English language proficiency or low literacy. | Use low literacy level explanations for cardiovascular conditions, their causes and treatments (see Table 5), identify and utilize an interpreter |
| Has a history of mental health issues like depression, anxiety, or addiction. | Screen for mental health issues and refer for treatment, if necessary |
| Doesn’t believe in the benefits of treatment. | Invite patients to explain their belief system (explanatory model) and what is important to them. Based on this understanding, you may be able to address some of these different beliefs. |
| Believes medications are unnecessary or harmful. | Invite patients to explain their beliefs. By understanding them, you may be able to address their concerns. |
| Has a concern about medication side effects. | Invite patients to explain their concerns. By understanding them, you may be able to address their concerns. |
| Says he or she is tired of taking medications. | Empathize. Ask what might help. |
| Concerns about costs of medications | Prescribe generics or provide samples when appropriate, consider 90 day supply and/or bulk mail order. |
Summary
Addressing the multifactorial impact of social determinants of health on disparities in health, healthcare and outcomes remains an important national public health goal4. While epidemiology has described these associations in the population, and numerous societal and community-level interventions have been suggested,1 clinicians need to recognize the possibility of their own unconscious biases and the social determinants of health in individual patients in order to address them. Patient-centered approaches can help clinicians to better understand the effects of social factors on their patients’ lives, health and views and behaviors related to health and healthcare and address the barriers they may pose to adherence to recommended therapies. Use of the approaches and tools provided here can help concerned clinicians target their efforts by enhancing the patient centeredness of their approaches, thereby increasing adherence and decreasing disparities.
Acknowledgments
Dr. Kressin was supported in part by a Senior Research Career Scientist award from the Department of Veterans Affairs, Health Services Research & Development Service (RCS 02-066-1) and an NIH grant (1U01HL105342-01, NR Kressin, PI). Dr. Magnani is supported by Grant 2015084 from the Doris Duke Charitable Foundation. We gratefully acknowledge the thoughtful input of Tracy Wang, MD, MPH and Frederick Ruberg, MD during preparation of this manuscript.
Footnotes
Disclosures: none.
References
- 1.Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz-Flores S, Davey-Smith G, Dennison-Himmelfarb CR, Lauer MS, Lockwood DW, Rosal M, Yancy CW. Social determinants of risk and outcomes for cardiovascular disease: A scientific statement from the american heart association. Circulation. 2015;132:873–898. doi: 10.1161/CIR.0000000000000228. [DOI] [PubMed] [Google Scholar]
- 2.Smedley BD, Stith AY, Nelson AR, editors. Unequal treatment: Confronting racial and ethnic disparities in health care. 2003. [PubMed] [Google Scholar]
- 3.Rathore SS, Krumholz HM. Differences, disparities, and biases: Clarifying racial variations in health care use. Ann Intern Med. 2004;141:635–638. doi: 10.7326/0003-4819-141-8-200410190-00011. [DOI] [PubMed] [Google Scholar]
- 4.Office of Disease Prevention and Health Promotion. 2015:2016. Healthypeople.Gov.
- 5.Wong MD, Shapiro MF, Boscardin WJ, Ettner SL. Contribution of major diseases to disparities in mortality. New Engl J Med. 2002;347:1585–1592. doi: 10.1056/NEJMsa012979. [DOI] [PubMed] [Google Scholar]
- 6.Murray CJ, Kulkarni SC, Michaud C, Tomijima N, Bulzacchelli MT, Iandiorio TJ, Ezzati M. Eight americas: Investigating mortality disparities across races, counties, and race-counties in the united states. PLoS Med. 2006;3:e260. doi: 10.1371/journal.pmed.0030260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Balfour PC, Jr, Rodriguez CJ, Ferdinand KC. The role of hypertension in race-ethnic disparities in cardiovascular disease. Curr Cardiovasc Risk Rep. 2015:9. doi: 10.1007/s12170-015-0446-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hicken M, Gragg R, Hu H. How cumulative risks warrant a shift in our approach to racial health disparities: The case of lead, stress, and hypertension. Health Aff (Millwood) 2011;30:1895–1901. doi: 10.1377/hlthaff.2010.1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Halfon N, Hochstein M. Life course health development: An integrated framework for developing health, policy, and research. Milbank Q. 2002;80:433–479. doi: 10.1111/1468-0009.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kramer MS, Seguin L, Lydon J, Goulet L. Socio-economic disparities in pregnancy outcome: Why do the poor fare so poorly? Paediatr Perinat Epidemiol. 2000;14:194–210. doi: 10.1046/j.1365-3016.2000.00266.x. [DOI] [PubMed] [Google Scholar]
- 11.Park JH, Vincent D, Hastings-Tolsma M. Disparity in prenatal care among women of colour in the USA. Midwifery. 2007;23:28–37. doi: 10.1016/j.midw.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 12.Goldenberg RL, Cliver SP, Mulvihill FX, Hickey CA, Hoffman HJ, Klerman LV, Johnson MJ. Medical, psychosocial, and behavioral risk factors do not explain the increased risk for low birth weight among black women. Am J Obste Gynecol. 1996;175:1317–1324. doi: 10.1016/s0002-9378(96)70048-0. [DOI] [PubMed] [Google Scholar]
- 13.El-Sayed AM, Paczkowski M, Rutherford CG, Keyes KM, Galea S. Social environments, genetics, and black-white disparities in infant mortality. Paediatr Perinat Epidemiol. 2015;29:546–551. doi: 10.1111/ppe.12227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li R, Grummer-Strawn L. Racial and ethnic disparities in breastfeeding among united states infants: Third national health and nutrition examination survey, 1988–1994. Birth. 2002;29:251–257. doi: 10.1046/j.1523-536x.2002.00199.x. [DOI] [PubMed] [Google Scholar]
- 15.Salsberry PJ, Reagan PB. Dynamics of early childhood overweight. Pediatrics. 2005;116:1329–1338. doi: 10.1542/peds.2004-2583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Magnuson KAWJ. Early childhood care and education: Effects on ethnic and racial gaps in school readiness. The Future of Children. 2005;15:169–196. doi: 10.1353/foc.2005.0005. [DOI] [PubMed] [Google Scholar]
- 17.Farkas G. Racial disparities and discrimination in education: What do we know, how do we know it, and what do we need to know? Teachers College Record. 2003;105:1119–1146. [Google Scholar]
- 18.Roscigno V, Ainsworth-Darnell, James W. Race, cultural capital, and educational resources: Persisstent inequalities and achievement returns. Sociology of Education. 1999;72:158–178. [Google Scholar]
- 19.Grodsky Eric PD. The structure of disadvantage: Individual and occupational determinants of the black-white wage gap. Am Sociol Rev. 2001;66:542–567. [Google Scholar]
- 20.Centers for Disease Control and Prevention. Nchs data on racial and ethnic health disparities. 2013:2016. [Google Scholar]
- 21.Cubbin C, LeClere FB, Smith GS. Socioeconomic status and injury mortality: Individual and neighbourhood determinants. J Epidemiol Community Health. 2000;54:517–524. doi: 10.1136/jech.54.7.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gee GC, Walsemann KM, Brondolo E. A life course perspective on how racism may be related to health inequities. Am J Public Health. 2012;102:967–974. doi: 10.2105/AJPH.2012.300666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jha AK, Orav EJ, Epstein AM. Low-quality, high-cost hospitals, mainly in south, care for sharply higher shares of elderly black, hispanic, and medicaid patients. Health Aff. 2011;30:1904–1911. doi: 10.1377/hlthaff.2011.0027. [DOI] [PubMed] [Google Scholar]
- 24.Kressin NR, Petersen LA. Racial differences in the use of invasive cardiovascular procedures: Review of the literature and prescription for future research. Ann Intern Med. 2001;135:352–366. doi: 10.7326/0003-4819-135-5-200109040-00012. [DOI] [PubMed] [Google Scholar]
- 25.Lewey J, Choudhry NK. The current state of ethnic and racial disparities in cardiovascular care: Lessons from the past and opportunities for the future. Curr Cardiol Rep. 2014;16:530. doi: 10.1007/s11886-014-0530-3. [DOI] [PubMed] [Google Scholar]
- 26.Kelley E, Moy E, Stryer D, Burstin H, Clancy C. The national healthcare quality and disparities reports: An overview. Med Care. 2005;43:I3–8. doi: 10.1097/00005650-200503001-00002. [DOI] [PubMed] [Google Scholar]
- 27.Le Cook B, McGuire TG, Zuvekas SH. Measuring trends in racial/ethnic health care disparities. Med Care Res Rev. 2009;66:23–48. doi: 10.1177/1077558708323607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chin MH, Clarke AR, Nocon RS, Casey AA, Goddu AP, Keesecker NM, Cook SC. A roadmap and best practices for organizations to reduce racial and ethnic disparities in health care. J Gen Intern Med. 2012;27:992–1000. doi: 10.1007/s11606-012-2082-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kressin NR, Chang BH, Whittle J, Peterson ED, Clark JA, Rosen AK, Orner M, Collins TC, Alley LG, Petersen LA. Racial differences in cardiac catheterization as a function of patients’ beliefs. Am J Public Health. 2004;94:2091–2097. doi: 10.2105/ajph.94.12.2091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.LeDoux J. The emotional brain: The mysterious underpinnings of emotional life. New York, New York: Simon and Schuster; 1998. [Google Scholar]
- 31.Ross HJ. Everyday bias: Identifying and navigating unconscious judgments in our daily lives. Lanham, MD: Rowan & Littlefield; 2014. [Google Scholar]
- 32.van Ryn M, Burgess DJ, Dovidio JF, Phelan SM, Saha S, Malat J, Griffin JM, Fu SS, Perry S. The impact of racism on clinician cognition, behavior, and clinical decision making. Du Bois Rev. 2011;8:199–218. doi: 10.1017/S1742058X11000191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Horowitz CR, Suchman AL, Branch WT, Jr, Frankel RM. What do doctors find meaningful about their work? Ann Intern Med. 2003;138:772–775. doi: 10.7326/0003-4819-138-9-200305060-00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Trivedi AN, Grebla RC, Wright SM, Washington DL. Despite improved quality of care in the veterans affairs health system, racial disparity persists for important clinical outcomes. Health Aff (Millwood) 2011;30:707–715. doi: 10.1377/hlthaff.2011.0074. [DOI] [PubMed] [Google Scholar]
- 35.Kochanek KD, Arias E, Anderson RN. How did cause of death contribute to racial differences in life expectancy in the united states in 2010? NCHS Data Brief. 2013:1–8. [PubMed] [Google Scholar]
- 36.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jimenez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER, 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB. Heart disease and stroke statistics-2016 update: A report from the american heart association. Circulation. 2015 doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 37.Franklin BA, Cushman M. Recent advances in preventive cardiology and lifestyle medicine: A themed series. Circulation. 2011;123:2274–2283. doi: 10.1161/CIRCULATIONAHA.110.981613. [DOI] [PubMed] [Google Scholar]
- 38.Williams RB, Barefoot JC, Schneiderman N. Psychosocial risk factors for cardiovascular disease: More than one culprit at work. JAMA. 2003;290:2190–2192. doi: 10.1001/jama.290.16.2190. [DOI] [PubMed] [Google Scholar]
- 39.Kressin NR, Wang F, Long J, Bokhour BG, Orner MB, Rothendler J, Clark C, Reddy S, Kozak W, Kroupa LP, Berlowitz DR. Hypertensive patients’ race, health beliefs, process of care, and medication adherence. J Gen Intern Med. 2007;22:768–774. doi: 10.1007/s11606-007-0165-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ho PM, Bryson CL, Rumsfeld JS. Medication adherence: Its importance in cardiovascular outcomes. Circulation. 2009;119:3028–3035. doi: 10.1161/CIRCULATIONAHA.108.768986. [DOI] [PubMed] [Google Scholar]
- 41.Cooper LA. A 41-year-old african american man with poorly controlled hypertension: Review of patient and physician factors related to hypertension treatment adherence. JAMA. 2009;301:1260–1272. doi: 10.1001/jama.2009.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bosworth HB, Powers BJ, Oddone EZ. Patient self-management support: Novel strategies in hypertension and heart disease. Cardiol Clin. 2010;28:655–663. doi: 10.1016/j.ccl.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mostow C, Crosson J, Gordon S, Chapman S, Gonzalez P, Hardt E, Delgado L, James T, David M. Treating and precepting with respect: A relational model addressing race, ethnicity, and culture in medical training. J Gen Intern Med. 2010;25(Suppl 2):S146–154. doi: 10.1007/s11606-010-1274-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Committee on quality of health care in american, crossing the quality chasm. 2001 [Google Scholar]
- 45.Mead N, Bower P. Patient-centred consultations and outcomes in primary care: A review of the literature. Patient Educ Couns. 2002;48:51–61. doi: 10.1016/s0738-3991(02)00099-x. [DOI] [PubMed] [Google Scholar]
- 46.Bredart A, Bouleuc C, Dolbeault S. Doctor-patient communication and satisfaction with care in oncology. Curr Opin Oncol. 2005;17:351–354. doi: 10.1097/01.cco.0000167734.26454.30. [DOI] [PubMed] [Google Scholar]
- 47.World Health Organization. Adherence to long-term therapies: Evidence for action. 2003 [Google Scholar]
- 48.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 49.Bosworth HB, Dudley T, Olsen MK, Voils CI, Powers B, Goldstein MK, Oddone EZ. Racial differences in blood pressure control: Potential explanatory factors. Am J Med. 2006;119:70 e79–15. doi: 10.1016/j.amjmed.2005.08.019. [DOI] [PubMed] [Google Scholar]
- 50.Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Interventions used to improve control of blood pressure in patients with hypertension. The Cochrane database of systematic reviews. 2010:Cd005182. doi: 10.1002/14651858.CD005182.pub4. [DOI] [PubMed] [Google Scholar]
- 51.DiMatteo MR. Variations in patients’ adherence to medical recommendations: A quantitative review of 50 years of research. Med Care. 2004;42:200–209. doi: 10.1097/01.mlr.0000114908.90348.f9. [DOI] [PubMed] [Google Scholar]
- 52.Haynes RB, McDonald H, Garg AX, Montague P. Interventions for helping patients to follow prescriptions for medications. Cochrane Database Syst Rev. 2002:Cd000011. doi: 10.1002/14651858.CD000011. [DOI] [PubMed] [Google Scholar]
- 53.Zullig LL, Peterson ED, Bosworth HB. Ingredients of successful interventions to improve medication adherence. JAMA. 2013;310:2611–2612. doi: 10.1001/jama.2013.282818. [DOI] [PubMed] [Google Scholar]
- 54.Bokhour BG, Cohn ES, Cortes DE, Solomon JL, Fix GM, Elwy AR, Mueller N, Katz LA, Haidet P, Green AR, Borzecki AM, Kressin NR. The role of patients’ explanatory models and daily-lived experience in hypertension self-management. J Gen Intern Med. 2012;27:1626–1634. doi: 10.1007/s11606-012-2141-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Haidet P, Paterniti DA. “Building” a history rather than “taking” one: A perspective on information sharing during the medical interview. Arch Intern Med. 2003;163:1134–1140. doi: 10.1001/archinte.163.10.1134. [DOI] [PubMed] [Google Scholar]
- 56.Tulsky JA. Interventions to enhance communication among patients, providers, and families. J Palliat Med. 2005;8(Suppl 1):S95–102. doi: 10.1089/jpm.2005.8.s-95. [DOI] [PubMed] [Google Scholar]
- 57.Epstein RM, Levenkron JC, Frarey L, Thompson J, Anderson K, Franks P. Improving physicians’ hiv risk-assessment skills using announced and unannounced standardized patients. J Gen Intern Med. 2001;16:176–180. doi: 10.1111/j.1525-1497.2001.02299.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Brown RF, Butow PN, Dunn SM, Tattersall MH. Promoting patient participation and shortening cancer consultations: A randomised trial. Br J Cancer. 2001;85:1273–1279. doi: 10.1054/bjoc.2001.2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Garg A, Toy S, Tripodis Y, Silverstein M, Freeman E. Addressing social determinants of health at well child care visits: A cluster rct. Pediatrics. 2015;135:e296–304. doi: 10.1542/peds.2014-2888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Schmittdiel J, Raebel M, Dyer W, STeiner JF, Goodrich GK, Karter AJ, Nichols GA. Medicare star excludes diabetes patients with poor cvd risk factor control. Am J Manag Care. 2014;20:e573–e581. [PMC free article] [PubMed] [Google Scholar]
- 61.Peterson ED, Ho PM, Barton M, Beam C, Burgess LH, Casey DE, Jr, Drozda JP, Jr, Fonarow GC, Goff D, Jr, Grady KL, King DE, King ML, Masoudi FA, Nielsen DR, Stanko S. Acc/aha/aacvpr/aafp/ana concepts for clinician-patient shared accountability in performance measures: A report of the american college of cardiology/american heart association task force on performance measures. Circulation. 2014;130:1984–1994. doi: 10.1161/CIR.0000000000000139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Engel GL. The need for a new medical model: A challenge for biomedicine. Science (New York, NY ) 1977;196:129–136. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]
- 63.Heurtin-Roberts S, Reisin E. The relation of culturally influenced lay models of hypertension to compliance with treatment. Am J Hypertens. 1992;5:787–792. doi: 10.1093/ajh/5.11.787. [DOI] [PubMed] [Google Scholar]
- 64.Bokhour BG, Kressin NR. What is in a name? How biomedical language may derail patient understanding of hypertension. Circ Cardiovasc Qual Outcomes. 2015;8:452–454. doi: 10.1161/CIRCOUTCOMES.114.001662. [DOI] [PubMed] [Google Scholar]
- 65.Kressin NR, Orner MB, Manze M, Glickman ME, Berlowitz D. Understanding contributors to racial disparities in blood pressure control. Circ Cardiovasc Qual Outcomes. 2010;3:173–180. doi: 10.1161/CIRCOUTCOMES.109.860841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Agency for Healthcare Research and Quality. Ahrq health literacy universal precautions toolkit. 2016:2016. [Google Scholar]
- 67.Oates DJ, Paasche-Orlow MK. Health literacy: Communication strategies to improve patient comprehension of cardiovascular health. Circulation. 2009;119:1049–1051. doi: 10.1161/CIRCULATIONAHA.108.818468. [DOI] [PubMed] [Google Scholar]
- 68.Collins TC, Clark JA, Petersen LA, Kressin NR. Racial differences in how patients perceive physician communication regarding cardiac testing. Med Care. 2002;40:I27–34. doi: 10.1097/00005650-200201001-00004. [DOI] [PubMed] [Google Scholar]
- 69.Bigby J. Cross-cultural medicine. Philadelphia, PA: American College of Physicians; 2003. [Google Scholar]
- 70.Kleinman A, Eisenberg L, Good B. Culture, illness, and care: Clinical lessons from anthropologic and cross-cultural research. Ann Intern Med. 1978;88:251–258. doi: 10.7326/0003-4819-88-2-251. [DOI] [PubMed] [Google Scholar]
- 71.Katz RV, Green BL, Kressin NR, Kegeles SS, Wang MQ, James SA, Russell SL, Claudio C, McCallum JM. The legacy of the tuskegee syphilis study: Assessing its impact on willingness to participate in biomedical studies. J Health Care Poor Underserved. 2008;19:1168–1180. doi: 10.1353/hpu.0.0067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.DiJulio Bianca NM, Symon Jackson, Mollyann Brodie, Kaiser Family Foundation . Kaiser family foundation/cnn survey of americans on race. 2015. [Google Scholar]
- 73.Davis TC, Long SW, Jackson RH, Mayeaux EJ, George RB, Murphy PW, Crouch MA. Rapid estimate of adult literacy in medicine: A shortened screening instrument. Fam Med. 1993;25:391–395. [PubMed] [Google Scholar]
- 74.Bokhour BG, Berlowitz DR, Long JA, Kressin NR. How do providers assess antihypertensive medication adherence in medical encounters? J Gen Intern Med. 2006;21:577–583. doi: 10.1111/j.1525-1497.2006.00397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Million hearts program. Supporting your patients with high blood pressure: visit checklist. 2016 [Google Scholar]