Abstract
The purpose of this review is to provide (1) a synopsis on relations of mindfulness with cardiovascular disease (CVD) and major CVD risk factors, and (2) an initial consensus-based overview of mechanisms and theoretical framework by which mindfulness might influence CVD. Initial evidence, often of limited methodological quality, suggests possible impacts of mindfulness on CVD risk factors including physical activity, smoking, diet, obesity, blood pressure, and diabetes regulation. Plausible mechanisms include (1) improved attention control (e.g., ability to hold attention on experiences related to CVD risk, such as smoking, diet, physical activity, and medication adherence), (2) emotion regulation (e.g., improved stress response, self-efficacy, and skills to manage craving for cigarettes, palatable foods, and sedentary activities), and (3) self-awareness (e.g., self-referential processing and awareness of physical sensations due to CVD risk factors). Understanding mechanisms and theoretical framework should improve etiologic knowledge, providing customized mindfulness intervention targets that could enable greater mindfulness intervention efficacy.
Keywords: Mindfulness, Cardiovascular disease, Etiology
Introduction
Scientific findings on the role of mindfulness in health are becoming clearer as larger numbers of increasingly methodologically rigorous studies are published [1••, 2••]. Systematic reviews and meta-analyses of randomized controlled trials suggest protective effects of mindfulness practices on depression relapse and non-clinical anxiety symptoms [1••, 3, 4]. Research about the impacts of mindfulness on cardiovascular disease (CVD) risk is in a much more nascent phase, but recent systematic reviews and meta-analyses suggest possible benefits for obesity, blood pressure, and smoking [5, 6, 7•, 8]. CVD remains the primary cause of mortality worldwide [9]. However, mindfulness studies on CVD risk are relatively few, and many are of fairly low methodological quality, often utilizing small sample sizes and brief follow-up times. Furthermore, the mechanisms and theoretical framework by which mindfulness may influence CVD have been minimally explored or discussed. Understanding the mechanisms, and delineating a theoretical framework, will not only allow for improved etiologic knowledge but will also provide targets that mindfulness interventions can be tailored to better engage with [10••]. More specifically, identifying the mechanisms of change through which mindfulness interventions could influence CVD risk is critical for developing the most effective and simple interventions, as recommended in the National Institutes of Health Stage Model for Intervention Development [10••]. If we understand the mechanisms through which an intervention is working, we can then better customize the intervention to act on those mechanisms. By knowing which plausible mechanisms are not important, those can be trimmed out of interventions to make them more cost-effective [10••].
The purpose of this review is to provide (1) an overview on the relationship of mindfulness with CVD and major CVD risk factors including smoking, diet, physical activity, obesity, lipids, blood pressure, and diabetes, and (2) an initial consensus-based overview of the mechanisms and theoretical framework by which mindfulness might influence CVD.
What Is Mindfulness?
Mindfulness is often defined as the ability to attend in a non-judgmental way to one’s own physical and mental processes during ordinary, everyday tasks [11]. A consensus two-component mindfulness definition stated that “The first component involves the self-regulation of attention so that it is maintained on immediate experience, thereby allowing for increased recognition of mental events in the present moment. The second component involves adopting a particular orientation toward one’s experiences in the present moment, an orientation that is characterized by curiosity, openness, and acceptance” [12]. Other traditional versions of mindfulness definitions include elements of “remembering” or “holding something in mind,” which could be important if what is held in mind are aspects that can positively influence well-being [13, 14••]. “Dispositional mindfulness” represents an inherent, yet modifiable, trait, where all people have varying capacities to attend and to be aware of what is occurring in the present moment [15].
The current review included studies that evaluated either mindfulness interventions or dispositional mindfulness. As there is an increasing variety of mindfulness interventions, we attempt to state the types of interventions when possible. For example, mindfulness-based interventions derived from mindfulness-based stress reduction (MBSR) have strong emphases on meditation [16]. MBSR is a multicomponent intervention providing systematic training in formal mindfulness meditation practices, and the informal application of mindfulness in daily life. It also includes gentle stretching and mindful yoga, as well as psychoeducation about the applications of mindfulness to support improved health, health-enhancing behaviors, and stress reduction. Subsequent adaptations of MBSR have been developed for a variety of conditions such as preventing relapse of recurrent depression, named mindfulness-based cognitive therapy (MBCT) [17]. Other mindfulness interventions such as acceptance and commitment therapy (ACT) overlap a reasonable amount theoretically with mindfulness-based interventions such as MBSR but have less emphasis on formal meditation practice [18]. There have been almost no explanatory studies in the cardiovascular literature to identify active components of mindfulness interventions [19••, 20••]. Consequently, we present interventions that address any type of mindfulness in order to be inclusive of the range of possible approaches. We also include studies that evaluated dispositional mindfulness assessed via questionnaires with validation evidence. There is current debate on the accuracy of self-reported mindfulness [21•, 22•]. Readers are referred to a systematic review of self-reported mindfulness questionnaires for further information on validity and reliability [22•]. We aim to clearly distinguish between these categories of evidence to allow readers to evaluate findings according to distinct mindfulness measures and interventions.
Is Mindfulness Predictive of CVD Risk or Cardiovascular Health?
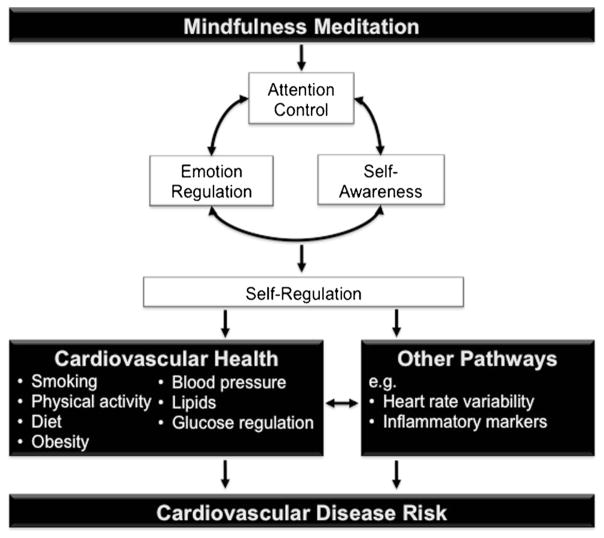
There is some evidence that dispositional mindfulness may be related to cardiovascular health, based on a cross-sectional study of 382 US participants who showed a 86 % higher likelihood (prevalence ratio 1.86; 95 % confidence interval (CI) 1.08, 3.19) of having good cardiovascular health with high versus low dispositional mindfulness levels [23•]. However, there is virtually no evidence on whether mindfulness is related to cardiovascular events. Despite this, there is a small but growing body of evidence on the relation between mindfulness and CVD risk factors. This review focuses on conventional CVD risk factors and components of cardiovascular health including physical activity, smoking, diet, obesity, blood pressure, lipids, and diabetes, described below and shown in Fig. 1.
Fig. 1.
Conceptual framework suggesting plausible mechanisms by which mindfulness meditation may influence cardiovascular disease risk
Physical Activity
Mindfulness-based interventions have potential to positively influence physical activity; however, there has been relatively little research in this area. To date, cross-sectional observational studies typically demonstrate that higher levels of dispositional mindfulness are associated with greater physical activity levels [23•, 24, 25]. A prospective observational study demonstrated that individuals with higher levels of dispositional mindfulness were more likely to follow through with baseline intentions to be physically active at 5 weeks follow-up [26]. A few ACT randomized controlled trials (RCTs) showed promising effects on increasing physical activity after 1 h to 6 months of follow-up time [27–30]. A recent observational study showed that mindfulness was associated with physical activity levels only in participants with weak habits for regularly doing physical activity [31]. These findings need to be replicated in intervention studies but suggest early evidence for possible ceiling effects, where mindfulness may be most effective in those with lower physical activity levels.
Smoking
A small number of RCTs evaluated efficacy of mindfulness training for smoking cessation [8]. For example, mindfulness training for smoking cessation was significantly more efficacious than the American Lung Association’s Freedom From Smoking for abstinence at a 4-month follow-up (31 vs 5 % abstinence, respectively) [32]. More recently, a mindfulness intervention called “Mindfulness Training for Smokers” reported significant differences in abstinence between treatment initiators and controls in a disadvantaged population (39 vs 21 %), but no difference in a more generalizable population (25 vs 18 %) [33]. There is very recent early evidence that expansion into app- and web-based delivery may be effective [34–36]. The intervention findings are supported by a meta-analysis of 11 observational studies that showed significant inverse associations between dispositional mindfulness and smoking (aggregate r=−0.14; p<0.001) [37]. Overall, recent review articles suggest that mindfulness may have promise as a treatment for smoking cessation, but also highlight the need for more adequately powered and controlled trials, replication of findings, and identifying the important active components of the mindfulness interventions that may be most effective for long-term smoking cessation [8, 38, 39].
Diet
The evidence for mindfulness approaches to changing dietary intake is preliminary but promising. RCTs of mindfulness interventions showed reduced caloric intake in diabetic participants (using the Mindfulness-Based Eating Awareness Training for Diabetes intervention) [40] and improved dietary composition in men with prostate cancer (using a diet intervention that incorporated mindfulness training) [41]. A prospective evaluation of MBSR in a general community population showed increased fruit and vegetable intake, and reduced consumption of desserts and other sweets, at program completion versus baseline assessments, in a study without a control group [42]. Another uncontrolled prospective MBSR study, in a sample comprising of war veterans, showed no changes in dietary patterns at preprogram versus postprogram completion [43]. Higher levels of dispositional mindfulness have been associated with more restrained eating, and less emotional and external eating behavior, in morbidly obese adults and diabetics [44, 45]. Evidence to date on effects of mindfulness on dietary patterns related to CVD is preliminary but offers an early signal of potential effects. Well-designed observational studies and RCTs of mindfulness interventions targeting dietary patterns that influence CVD have potential to show effects.
Obesity
Several systematic reviews evaluated mindfulness interventions for weight loss and obesity-related eating behaviors [5, 6, 46, 47]. One review consisting of nine weight loss studies used a narrow definition of mindfulness-based interventions requiring that mindfulness practices be a component of every session [47]. Overall, effects on weight loss post-intervention were small or non-significant, but significant effects were observed in the three studies focusing on weight loss as a primary outcome [47]. Two other systematic reviews used broader definitions of mindfulness interventions that included any study in which at least one session focused on mindfulness skills training. One review focusing on weight loss as the primary outcome found that weight loss was documented in 13 of 19 studies [48]. The other review, which focused on interventions for eating behaviors associated with weight gain [5], found that weight loss or maintenance was demonstrated in 9 of 10 studies, with a small effect size (Cohen’s d=0.19). Intervention findings are consistent with other observational study data showing those with higher dispositional mindfulness significantly more likely to have healthy BMI levels (≥18.5 and <25.0 kg/m2) [23•]. The role of mindfulness interventions in weight loss has been reviewed in greater detail by our group elsewhere [49]. Future directions include the need for more rigorous, fully powered randomized trials with longer follow-up periods, and inclusion of diverse populations.
Blood Pressure
A recent systematic review and meta-analysis of four mindfulness-based interventions found significant but heterogeneous effects on blood pressure [7•]. The overall effect was statistically significant (standardized mean difference for mindfulness intervention versus control: −0.78 for systolic blood pressure, p=0.03; −0.67 for diastolic blood pressure, p=0.03) [7•]. Methodological rigor for several of the studies was limited, including fairly high loss-to-follow-up for some studies, and brief follow-up periods with the exception of one study that had a 1-year follow-up period [50]. Reasons for differences in effect size between studies may be floor effects, where the largest effects were seen in the study that had participants with the highest blood pressure (unmedicated stage 1 or 2 hypertension) [51] versus other studies that included participants with unmedicated stage 1 hypertension [50] or prehypertension [52] or those who did not have blood pressure level inclusion criteria [53]. Other reasons may be that analyses showing greater effects used resting blood pressure as the outcome [51–53] instead of ambulatory blood pressure [50, 52]. The field will be helped with methodologically rigorous, well-powered RCTs evaluating impacts of standardized and customized mindfulness interventions for blood pressure reduction [54].
Lipids
One cross-sectional observational study in 346 middle-aged participants showed no associations between dispositional mindfulness and total cholesterol [23•]. The relation between mindfulness and lipids remains almost completely unexplored.
Diabetes and Glucose Regulation
Several studies investigated contributions of mindfulness interventions to glucose regulation in diabetic patients. Of the five RCTs to our knowledge, two demonstrated significant reductions in glucose regulation measures including HbA1C and fasting glucose [55, 56], and three showed null findings [53, 57, 58]. Both interventions that demonstrated significant improvements in glucose regulation specifically trained participants in mindfulness as well as behaviors that improve glucose regulation, such as diet, physical activity, glucose monitoring, and diabetes medication use (using the mindfulness interventions ACT or mindful eating/yoga) [55, 56]. Studies failing to show improvements in glucose regulation tested standardized mindfulness-based interventions, specifically MBCT [57, 58] and MBSR [53]. These standardized interventions provide some training in mindful eating and mindful movements but do not deliberately link the importance of these factors to diabetes control and do not address diabetes medication adherence or glucose monitoring [59, 60•]. Mindfulness interventions targeted toward improving mindfulness skills for glucose regulation may increase effect sizes. With regard to dispositional mindfulness, one study showed that participants with high versus low mindfulness were significantly more likely to have normal glucose levels, but these findings need replication [23•].
Other Pathways
Other CVD risk markers and risk factors may also be important in explaining mechanisms by which mindfulness interventions could influence CVD risk (Fig. 1). For example, a number of studies have explored the role of mindfulness interventions to influence heart rate variability [61, 62] and inflammatory markers [63–65]; however, in order to allow some depth of exploration into specific CVD risk factors, the current review is focused on conventional independent CVD risk factors.
How Could Mindfulness Influence CVD Risk?
The mechanisms and theoretical framework proposed herein build on important foundational work of others, particularly Holzel et al. [66•], Vago and Silberstein [67], and Tang et al. [2••] who focused reviews on mechanisms by which mindfulness could influence mental health. As shown in Fig. 1, preliminary evidence suggests that mindfulness meditation may influence health particularly through improved self-regulation, via enhancing (1) attention control, (2) emotion regulation, and (3) self-awareness [2••, 66•, 67]. These pathways are explored below in relation to CVD risk.
It should be noted that these plausible mechanisms are presented with the invitation to rigorously test them using methods such as RCTs and prospective observational studies, incorporating formal mediation analyses [68•] to evaluate if they truly are mediators between mindfulness and CVD risk. At the current time, there is limited quantitative evidence. However, based on theoretical underpinnings and evidence to date of mechanisms of mindfulness on health [2••, 66•, 67, 69•], and determinants of CVD [70, 71], these are likely some of the strongest candidates. Understanding mechanisms will not only improve etiologic knowledge but also greatly assist in identifying targets for customized mindfulness interventions, described above [10••].
Attention Control
Attention control is emphasized in mindfulness meditation and improves as a result of meditation practices [66•, 72]. In mindfulness-based interventions, attention control is frequently trained through bringing awareness to a single object, such as the breath [66•]. Through this technique, it appears that brain regions such as the anterior cingulate cortex are altered, facilitating executive attention and control [2••]. Attention can also be directed toward more emotionally challenging objects. Related to CVD risk, improved abilities to hold attention to positive, and often predominantly negative, sensations associated with risk factors such as smoking, overeating, sedentary activities, or medication adherence could be important [6, 8, 31]. Often the mind has some aversion to emotionally strong objects (particularly negative emotions), and attention can be diverted to more emotionally neutral sensations. However, theoretical underpinnings of mindfulness meditation support the benefits of bringing gentle, non-judgmental, curious attention to difficult emotions and thoughts, to explore their characteristics and roots [16]. For example, a smoker can hold attention to each moment associated with cigarette smoking, both enjoyable (e.g., having a break from work) and difficult (e.g., chronic cough due to smoking, and other health effects). Training the mind to hold each and every moment in awareness can start to highlight the short- and longer-term effects of smoking, or other CVD risk behaviors such as overeating, sedentary activities, and medication adherence, thereby helping people see more clearly, creating cognitive dissonance [73], enhancing intrinsic motivation [74] and internalization [75]. This can allow a more informed decision to be made about the personal value of engaging in CVD-related behaviors.
Emotion Regulation
Stress Response
A systematic review and meta-analysis of 118,696 participants demonstrated a risk ratio of 1.27 (95 % CI 1.12, 1.45) for the relation of high versus low perceived stress with incident CVD [76]. A meta-analysis of 197,473 participants demonstrated that those with job strain versus those with no job strain had 1.17 (95 % CI 1.05, 1.31) higher hazard ratio for incident CVD, after adjusting for age, sex, and socioeconomic status, with a fairly small population attributable risk of 3.4 % [77•]. A systematic review and meta-analysis of 31 cohorts found that laboratory-induced stress reactivity was significantly associated with resting systolic (r=0.12, 95 % CI 0.08, 0.16) and diastolic blood pressure (r=0.08, 95 % CI: 0.05, 0.11), but not with subclinical measures of CVD such as coronary artery calcification (r=0.01, 95 % CI −0.01, 0.03) [78]. Furthermore, slow recovery from laboratory-induced stress was significantly associated with resting systolic (r=0.08, 95 % CI 0.01, 0.15) and diastolic blood pressure (r=0.08, 95 % CI 0.03, 0.13), and coronary artery calcification (r= 0.14, 95 % CI 0.05, 0.23) [78].
Mindfulness-based interventions often explicitly address stress, particularly through normalizing stress experiences, and enhancing awareness of how one responds to stress [59, 60•]. Often stress reactions can evoke additional stress through persistent negative thinking or rumination about the event for sustained time periods [69•]. Mindfulness-based interventions often emphasize bringing awareness to the stress-or, noticing inner drives for reacting, and allowing some space in between the stressor and response, to allow for a more careful response to the stress rather than a reaction [59, 60•]. Certain types of meditations can also focus in on stressors themselves, allowing for a form of exposure therapy, to allow the stressors to be experienced in controlled ways, thereby practicing more effective responses to frequently experienced stressors [2••]. Acute stress can involve rapid activation of the amygdala to allow for immediate responses that can be lifesaving [79]. The prefrontal cortex, responsible for executive function and control, modulates amygdala activity, allowing for top-down regulation of limbic information processing [79]. The impact of mindfulness training on stress response in the brain is supported by neurophysiological evidence demonstrating reduced amygdala activation, increased prefrontal cortex activation, and increased hippocampal gray matter density following mindfulness interventions [2••]. A recent systematic review and meta-analyses of nine RCTs showed evidence that mindfulness mediation programs may reduce stress compared to non-specific active control groups; however, the strength of evidence to date was considered low [1••]. Overall, evidence suggests stress as a plausible pathway; however, stronger evidence is needed on the population attributable risk of stress reactivity and stress recovery for CVD, as well as higher-quality studies evaluating if mindfulness interventions impact stress, including stress response and recovery.
Craving
Evolutionarily, humans have had good cause to crave high caloric palatable foods and physical rest [80, 81]. In many current industrialized societies, this craving no longer achieves the same adaptive benefits due to much greater food availability, and sedentary occupations and pastimes [80]. Craving and resulting behaviors can lead to excessive food consumption, obesity, and poor physical conditioning [80, 81]. Mindfulness has been positively associated with greater self-regulation and ability to notice cravings without acting on them [32, 82]. Treating emotions and physical sensations as passing events can help people tolerate cravings and overcome addictions, whether it is for cigarettes [32] or potentially for high caloric palatable foods, or sedentary activities such as electronic screen use [6, 83]. In the mindfulness training for smoking cessation RCT, mindfulness practice was found to moderate decoupling of the link between craving and smoking [84]. Neurophysiological studies showed that regions of the prefrontal cortex, including the dorsolateral prefrontal cortex and anterior cingulate cortex, are implicated in self-regulation and inhibitory control related to limiting excessive hedonic (i.e., pleasure-focused) feeding behavior [80]. Mindfulness meditation has been shown to influence these same regions [2••].
Self-Efficacy and Sense of Control
Self-efficacy is the extent or strength of belief in one’s own ability to complete tasks and reach goals. Sense of control is a related concept, often operationalized as personal mastery (a person’s sense of efficacy or effectiveness in carrying out goals) and perceived constraints (the extent to which one believes there are obstacles or factors beyond one’s control that interfere with reaching goals) [85]. Deciding to initiate a health behavior change depends on interactions between motivation and confidence about successful change [86]. Confidence about making change is often related to self-efficacy [87] and perceived behavioral control [88–90]. Self-efficacy and sense of control have been linked to CVD mortality and CVD risk behaviors, although replication of findings in high-quality prospective studies is needed [91, 92]. A trial of a mindfulness-oriented intervention for addictive disorders demonstrated enhanced perceived control over motor activity related to impulsive behavior [93]. Patients with chronic pain, chronic illness, or stress-related problems taking MBSR were shown to have significantly higher self-efficacy, related to their confidence to manage conditions on a regular basis, at 1-year follow-up compared to baseline [94]. A recent cross-sectional mediation analysis showed preliminary evidence that sense of control may be a mediator between dispositional mindfulness and cardiovascular health [23•].
Self-Kindness and Self-Compassion
Self-kindness and self-compassion are interrelated plausible pathways that could link mindfulness to CVD risk. During MBSR and MBCT, group leaders often convey implicit messages about the importance of being kind and gentle with oneself, encouraging strong determination in meeting practice goals while also emphasizing self-kindness when goals are not met [95]. Mindfulness-based interventions, such as MBSR and MBCT, may enhance participants’ self-compassion [95]. One study found self-compassion to be a mediator of the effects of MBCT on depression [96], although replication is needed. Self-compassion may be particularly effective for patients with CVD risk factors that have societal stigma such as obesity [97] and tobacco dependence [98]. Self-compassion is associated with increased motivation and persistence after task failure [99] and healthier behaviors such as physical activity and regular doctor visits [100].
Social Support
Social support and related inverse constructs such as social isolation and loneliness are potentially important for CVD and mortality [101–103]. For example, in a systematic review of prospective studies on participants with existing coronary heart disease, 9 of 10 studies showed significant associations between social support and incidence of fatal coronary heart disease, non-fatal myocardial infarction, or all-cause mortality [102]. Associations in healthy participants are more heterogeneous, where five of eight studies showed significant inverse associations between social support and incidence of coronary heart disease [102]. Mindfulness meditation is often practiced in meditation groups [65]. The group support may be an important component of meditation training, and for providing continued meditation practice support afterward, similar to behavioral change programs for alcohol abstinence (e.g., Alcoholics Anonymous) and weight loss (e.g., Weight Watchers) [104, 105]. A study that randomized 170 participants trying to lose weight to practice mindfulness meditation for 6 weeks within a group versus practicing alone demonstrated, using intent-to-treat analyses, that the group setting produced significantly (p<0.001) greater weight loss (mean 1.66 kg) than the individual setting (mean 0.45 kg) [104]. Another randomized controlled trial (n=40) demonstrated significant reductions in loneliness in the group randomized to MBSR versus waist-list control [65].
Self-Awareness
Self-Referential Processing
Self-referential processing is defined as self-reflection about internal thoughts and feelings, in the absence of external stimulus processing [106, 107]. Brain networks that have most consistently been implicated in self-referential processing include the default-mode network [106, 108]. Importantly, the main hubs of this network, including the medial prefrontal cortex and posterior cingulate cortex, have been shown to be specifically deactivated in experienced meditators relative to novices, across several different types of meditation [109]. More recently, direct links have been made between increased activation in midline brain regions such as the posterior cingulate cortex and the experience of being “caught up” in self-related states that may be related to CVD risk, such as craving [110]. Mindfulness meditation training has been directly associated with decreased activity in this same brain region [111–113].
Mindfulness interventions appear to strengthen a metacognitive ability to step back from getting caught up in emotional reactivity, habitual behaviors, and self-narratives, in a process referred to as decentering [114–117]. Decentering is typically defined as the process of observing one’s thoughts and feelings as passing events in the mind, rather than as valid reflections of reality or central aspects of the self [115–117]. Individuals high in decentering tend to exhibit lower blood pressure reactivity [118]. Studies that formally evaluate whether decentering is a risk factor for CVD, and if it mediates the relation between mindfulness practices and CVD risk, would provide important information.
Values Clarification
Values clarification, or the recognition and delineation of what is truly meaningful or valuable in one’s life, is another potential mechanism of mindfulness interventions [18, 119]. Individuals tend to be more motivated and likely to engage in behaviors consistent with their values, especially clearly identified values [120]. Since mindfulness is associated with greater ability to identify and discriminate between different emotions (i.e., emotional clarity), mindfulness might also help to clarify values, and therefore enhance motivation for valued behaviors [121–123]. Studies suggest that meditation practice is associated with increases in values clarification and purpose and that values clarification is associated with positive psychological states and sense of control [124, 125]. Furthermore, observational studies demonstrated that higher values clarification levels were associated with lower temptation to drink alcohol and lower drinking frequency and drinking-related consequences [126], and that values clarification mediated associations between dispositional mindfulness and alcohol-related problems [127].
Awareness of Present-Moment Experiences
Present-moment experiences are felt through physical sensations, thoughts, and emotions [59]. In many mindfulness interventions that bring curious, non-judgmental awareness to thoughts, emotions, and physical sensations, the resulting improvements in interoception shift self-processing away from narrative toward experiential self-processing in part by favoring body-based sensory experiences [128]. Interoceptive body awareness is the ability to notice subtle bodily sensations [129, 130] and is reported to be enhanced with meditation [66•, 131, 132]. Awareness to body sensations may be particularly important for CVD risk reduction, especially enhancing awareness related to body-specific positive experiences (e.g., eating healthy palatable foods and physical exercise completion) and negative experiences (e.g., physical limitations due to inadequate physical activity, lethargy following sugar consumption, joint pain associated with obesity, and cigarette craving) [130, 133–135]. Through enhancing awareness to each moment, participants can be trained to clearly feel the short- and longer-term effects of CVD risk behaviors and potentially make healthier behavior decisions as a result.
Conclusions and Future Directions
Overall, studies to date suggest promising but still inconclusive evidence of associations of mindfulness with cardiovascular health [23•], and CVD risk factors, specifically smoking, blood pressure, diabetes, physical activity, obesity, and diet [5, 6, 7•, 8, 23•, 24–32, 37, 38, 40–43, 46, 47, 53, 55–58]. Areas needing further work include performing adequately powered RCTs adhering to CONSORT guidelines [136–138], careful consideration of control groups for pragmatic versus explanatory trials [19••, 20••, 105], longer-term follow-up [50, 58], and comparative effectiveness of tailored versus standardized general mindfulness interventions. It is important to identify which participants are most likely to benefit from mindfulness interventions, and to explore customizing mindfulness interventions to target populations [33]. The theoretical framework described here suggests that three main components may be active processes by which mindfulness interventions can exert cardiovascular effects, specifically (1) attention control (e.g., ability to hold attention on experiences related to CVD risk, such as smoking, diet, physical activity, and medication adherence), (2) emotion regulation (e.g., improved stress response, self-efficacy, and skills to manage craving for cigarettes, palatable foods, and sedentary activities), and (3) self-awareness (e.g., self-referential processing and awareness of physical sensations due to CVD risk factors). These proposed pathways need much further testing to determine which, if any, are particularly important. Customized mindfulness interventions may want to consider engaging with these plausible mechanisms of change to evaluate if doing so increases intervention effectiveness on CVD risk.
Acknowledgments
This publication was supported by grant number UH2AT009145 from the National Institutes of Health (NIH), specifically the National Center for Complementary and Integrative Health (NCCIH) and the Office of Behavioral and Social Sciences Research (OBSSR). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NCCIH, OBSSR, or the NIH.
Footnotes
Conflict of interest Eric B. Loucks, Zev Schuman-Olivier, Willoughby B. Britton, David M. Fresco, Gaelle Desbordes, Judson A. Brewer, and Carl Fulwiler declare that they have no conflict of interest.
Compliance with Ethical Standards
Human and Animal Rights and Informed Consent This article does not contain any studies with human or animal subjects performed by any of the authors.
This article is part of the Topical Collection on Psychological Aspects of Cardiovascular Diseases
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1••.Goyal M, Singh S, Sibinga EM, et al. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Intern Med. 2014;174(3):357–68. doi: 10.1001/jamainternmed.2013.13018. US Government Agency for Health Care Research and Qualty (AHRQ)-commissioned systematic review including mindfulness meditation RCTs with active control groups. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2••.Tang YY, Holzel BK, Posner MI. The neuroscience of mindfulness meditation. Nat Rev Neurosci. 2015;16(4):213–25. doi: 10.1038/nrn3916. Thorough review on mechanims by which mindfulness can influence mental health. [DOI] [PubMed] [Google Scholar]
- 3.Khoury B, Lecomte T, Fortin G, et al. Mindfulness-based therapy: a comprehensive meta-analysis. Clin Psychol Rev. 2013;33(6):763–71. doi: 10.1016/j.cpr.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 4.Strauss C, Cavanagh K, Oliver A, Pettman D. Mindfulness-based interventions for people diagnosed with a current episode of an anxiety or depressive disorder: a meta-analysis of randomised controlled trials. PLoS ONE. 2014;9(4):e96110. doi: 10.1371/journal.pone.0096110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O’Reilly GA, Cook L, Spruijt-Metz D, Black DS. Mindfulness-based interventions for obesity-related eating behaviours: a literature review. Obes Rev. 2014;15(6):453–61. doi: 10.1111/obr.12156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Olson KL, Emery CF. Mindfulness and weight loss: a systematic review. Psychosom Med. 2015;77(1):59–67. doi: 10.1097/PSY.0000000000000127. [DOI] [PubMed] [Google Scholar]
- 7•.Abbott RA, Whear R, Rodgers LR, et al. Effectiveness of mindfulness-based stress reduction and mindfulness based cognitive therapy in vascular disease: a systematic review and meta-analysis of randomised controlled trials. J Psychosom Res. 2014;76(5):341–51. doi: 10.1016/j.jpsychores.2014.02.012. Methodologically well-performed systematic review and meta-analysis on mindfulness interventions and blood pressure. [DOI] [PubMed] [Google Scholar]
- 8.de Souza IC, de Barros VV, Gomide HP, et al. Mindfulness-based interventions for the treatment of smoking: a systematic literature review. J Altern Complement Med. 2015;21(3):129–40. doi: 10.1089/acm.2013.0471. [DOI] [PubMed] [Google Scholar]
- 9.Mendis S, Puska P, Norrving B. Global atlas on cardiovascular disease prevention and control. Geneva: World Health Organization; 2011. [Google Scholar]
- 10••.Onken LS, Carroll KM, Shoham V, Cuthbert BN, Riddle M. Reenvisioning clinical science: unifying the discipline to improve the public health. Clin Psychol Sci. 2014;2(1):22–34. doi: 10.1177/2167702613497932. Article reconceptualizing the importance of understanding mechanisms when developing behavioral intervention studies. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Epstein RM. Mindful practice. JAMA. 1999;282(9):833–9. doi: 10.1001/jama.282.9.833. [DOI] [PubMed] [Google Scholar]
- 12.Bishop SR, Lau M, Shapiro S, et al. Mindfulness: a proposed operational definition. Clin Psychol-Sci Pr. 2004;11(3):230–41. [Google Scholar]
- 13.Dreyfus G. Is mindfulness present-centred and non-judgmental? A discussion of the cognitive dimensions of mindfulness. Contemp Buddhism. 2011;12:41–54. [Google Scholar]
- 14••.Gethin R. Buddhist conceptualizations of mindfulness. In: Brown KW, Creswell JD, Ryan RM, editors. Handbook of mindfulness. New York: The Guilford Press; 2015. This is a chapter from a recently published textbook on mindfulness; the textbook includes a well-done overview of mindfulness theory and associations with health. [Google Scholar]
- 15.Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Personal Soc Psychol. 2003;84(4):822–48. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 16.Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry. 1982;4(1):33–47. doi: 10.1016/0163-8343(82)90026-3. [DOI] [PubMed] [Google Scholar]
- 17.Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression: a new approach to preventing relapse. New York: Guilford Press; 2002. [Google Scholar]
- 18.Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: an experiential approach to behavior change. 1999 [Google Scholar]
- 19••.Freedland KE. Demanding attention: reconsidering the role of attention control groups in behavioral intervention research. Psychosom Med. 2013;75(2):100–2. doi: 10.1097/PSY.0b013e3182851b75. This article provides important information to aid selection of ideal control groups, relevent to mindfulness research. [DOI] [PubMed] [Google Scholar]
- 20••.Freedland KE, Mohr DC, Davidson KW, Schwartz JE. Usual and unusual care: existing practice control groups in randomized controlled trials of behavioral interventions. Psychosom Med. 2011;73(4):323–35. doi: 10.1097/PSY.0b013e318218e1fb. This article also provides important information to aid selection of ideal control groups, relevent to mindfulness research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21•.Visted E, Jollestad J, Nielsen MB, Nielsen GH. The impact of group-based mindfulness training on self-reported mindfulness: a systematic review and meta-analysis. Mindfulness. 2014 Feb; Article providing systematic review that informs validity and reliabliity of dispositional mindfulness measures. [Google Scholar]
- 22•.Park T, Reilly-Spong M, Gross CR. Mindfulness: a systematic review of instruments to measure an emergent patient-reported outcome (PRO) Qual Life Res. 2013;22(10):2639–59. doi: 10.1007/s11136-013-0395-8. Article providing systematic review that informs validity and reliabliity of dispositional mindfulness measures. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23•.Loucks EB, Britton WB, Howe CJ, Eaton CB, Buka SL. Positive associations of dispositional mindfulness with cardiovascular health: the New England Family Study. Int J Behav Med. 2015;22(4):540–50. doi: 10.1007/s12529-014-9448-9. This is the first observational study to evaluate associations of dipositional mindfulness with cardiovascular health. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Salmoirago-Blotcher E, Husinger M, Morgan L, Fischer D, Carmody J. Mindfulness-based stress reduction and change in health-related behaviors. J Evid Based Complement Altern Med. 2013;18(4):243–7. [Google Scholar]
- 25.Ulmer CS, Stetson BA, Salmon PG. Mindfulness and acceptance are associated with exercise maintenance in YMCA exercisers. Behav Res Ther. 2010;48(8):805–9. doi: 10.1016/j.brat.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 26.Chatzisarantis NL, Hagger MS. Mindfulness and the intention-behavior relationship within the theory of planned behavior. Personal Soc Psychol Bull. 2007;33(5):663–76. doi: 10.1177/0146167206297401. [DOI] [PubMed] [Google Scholar]
- 27.Tapper K, Shaw C, Ilsley J, Hill AJ, Bond FW, Moore L. Exploratory randomised controlled trial of a mindfulness-based weight loss intervention for women. Appetite. 2009;52(2):396–404. doi: 10.1016/j.appet.2008.11.012. [DOI] [PubMed] [Google Scholar]
- 28.Moffitt R, Mohr P. The efficacy of a self-managed Acceptance and Commitment Therapy intervention DVD for physical activity initiation. Br J Health Psychol. 2015;20(1):115–29. doi: 10.1111/bjhp.12098. [DOI] [PubMed] [Google Scholar]
- 29.Ivanova E, Jensen D, Cassoff J, Gu F, Knauper B. Acceptance and commitment therapy improves exercise tolerance in sedentary women. Med Sci Sports Exerc. 2015;47(6):1251–8. doi: 10.1249/MSS.0000000000000536. [DOI] [PubMed] [Google Scholar]
- 30.Kangasniemi AM, Lappalainen R, Kankaanpaa A, Tolvanen A, Tammelin T. Towards a physically more active lifestyle based on one’s own values: the results of a randomized controlled trial among physically inactive adults. BMC Public Health. 2015;15:260. doi: 10.1186/s12889-015-1604-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tsafou KE, De Ridder DT, van Ee R, Lacroix JP. Mindfulness and satisfaction in physical activity: a cross-sectional study in the Dutch population. J Health Psychol. 2015 doi: 10.1177/1359105314567207. [DOI] [PubMed] [Google Scholar]
- 32.Brewer JA, Mallik S, Babuscio TA, et al. Mindfulness training for smoking cessation: results from a randomized controlled trial. Drug Alc Depend. 2011;119(1–2):72–80. doi: 10.1016/j.drugalcdep.2011.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Davis JM, Goldberg SB, Anderson MC, Manley AR, Smith SS, Baker TB. Randomized trial on mindfulness training for smokers targeted to a disadvantaged population. Subst Use Misuse. 2014;49(5):571–85. doi: 10.3109/10826084.2013.770025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Davis JM, Manley AR, Goldberg SB, Stankevitz KA, Smith SS. Mindfulness training for smokers via web-based video instruction with phone support: a prospective observational study. BMC Complement Alt Med. 2015;15:95. doi: 10.1186/s12906-015-0618-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ruscio AC, Muench C, Brede E, Waters AJ. Effect of brief mindfulness practice on self-reported affect, craving, and smoking: a pilot randomized controlled trial using ecological momentary assessment. Nicotine Tobac Res. 2015 doi: 10.1093/ntr/ntv074. [DOI] [PubMed] [Google Scholar]
- 36.Garrison KA, Pal P, Rojiani R, Dallery J, O’Malley SS, Brewer JA. A randomized controlled trial of smartphone-based mindfulness training for smoking cessation: a study protocol. BMC Psychiatr. 2015;15:83. doi: 10.1186/s12888-015-0468-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Karyadi KA, VanderVeen JD, Cyders MA. A meta-analysis of the relationship between trait mindfulness and substance use behaviors. Drug Alc Depend. 2014 doi: 10.1016/j.drugalcdep.2014.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Carim-Todd L, Mitchell SH, Oken BS. Mind-body practices: an alternative, drug-free treatment for smoking cessation? A systematic review of the literature. Drug Alc Depend. 2013;132(3):399–410. doi: 10.1016/j.drugalcdep.2013.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schuman-Olivier Z, Hoeppner BB, Evins AE, Brewer JA. Finding the right match: mindfulness training may potentiate the therapeutic effect of nonjudgment of inner experience on smoking cessation. Subst Use Misuse. 2014;49(5):586–94. doi: 10.3109/10826084.2014.850254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Miller CK, Kristeller JL, Headings A, Nagaraja H. Comparison of a mindful eating intervention to a diabetes self-management intervention among adults with type 2 diabetes: a randomized controlled trial. Health Ed Behav. 2014;41:145–54. doi: 10.1177/1090198113493092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Carmody JF, Olendzki BC, Merriam PA, Liu Q, Qiao Y, Ma Y. A novel measure of dietary change in a prostate cancer dietary program incorporating mindfulness training. J Acad Nutr Dietetics. 2012;112:1822–7. doi: 10.1016/j.jand.2012.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Salmoirago-Blotcher E, Morgan L, Fischer D, Carmody J. Mindfulness-based stress reduction and change in health-related behaviors. J Evid-Based Complement Altern Med. 2013;18:243–7. [Google Scholar]
- 43.Kearney DJ, Milton ML, Malte CA, McDermott KA, Martinez M, Simpson TL. Participation in mindfulness-based stress reduction is not associated with reductions in emotional eating or uncontrolled eating. Nutr Res. 2012;32(6):413–20. doi: 10.1016/j.nutres.2012.05.008. [DOI] [PubMed] [Google Scholar]
- 44.Ouwens MA, Schiffer AA, Visser LI, Raeijmaekers NJ, Nyklicek I. Mindfulness and eating behaviour styles in morbidly obese males and females. Appetite. 2015;87:62–7. doi: 10.1016/j.appet.2014.11.030. [DOI] [PubMed] [Google Scholar]
- 45.Tak SR, Hendrieckx C, Nefs G, Nyklicek I, Speight J, Pouwer F. The association between types of eating behaviour and dispositional mindfulness in adults with diabetes. Results from Diabetes MILES. The Netherlands. Appetite. 2015;87:288–95. doi: 10.1016/j.appet.2015.01.006. [DOI] [PubMed] [Google Scholar]
- 46.Godsey J. The role of mindfulness based interventions in the treatment of obesity and eating disorders: an integrative review. Complement Ther Med. 2013;21(4):430–9. doi: 10.1016/j.ctim.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 47.Katterman SN, Kleinman BM, Hood MM, Nackers LM, Corsica JA. Mindfulness meditation as an intervention for binge eating, emotional eating, and weight loss: a systematic review. Eat Behav. 2014;15(2):197–204. doi: 10.1016/j.eatbeh.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 48.Olson KL, Emery CF. Mindfulness and weight loss: a systematic review. Psychosom Med. 2015;77:59–67. doi: 10.1097/PSY.0000000000000127. [DOI] [PubMed] [Google Scholar]
- 49.Fulwiler C, Brewer JA, Loucks EB. Curr Cardiovasc Dis Risk Rep. 2015 doi: 10.1007/s12170-015-0474-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Blom K, Baker B, How M, et al. Hypertension analysis of stress reduction using mindfulness meditation and yoga: results from the harmony randomized controlled trial. Am J Hypertens. 2014;27(1):122–9. doi: 10.1093/ajh/hpt134. [DOI] [PubMed] [Google Scholar]
- 51.de la Fuente M, Franco C, Salvador M. Reduction of blood pressure in a group of hypertensive teadhers through a program of mindfulness meditation. Psicol Conductual. 2010;18:533–52. [Google Scholar]
- 52.Hughes JW, Fresco DM, Myerscough R, van Dulmen M, Carlson LE, Josephson R. Randomized controlled trial of Mindfulness-Based Stress Reduction for prehypertension. Psychosom Med. 2013;75:721–8. doi: 10.1097/PSY.0b013e3182a3e4e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hartmann M, Kopf S, Kircher C, et al. Sustained effects of a mindfulness-based stress-reduction intervention in type 2 diabetic patients: design and first results of a randomized controlled trial (the Heidelberger Diabetes and Stress-study) Diabet Care. 2012;35(5):945–7. doi: 10.2337/dc11-1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Goldstein CM, Josephson R, Xie S, Hughes JW. Current perspectives on the use of meditation to reduce blood pressure. Intern J Hypertens. 2012;2012:578397. doi: 10.1155/2012/578397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gregg JA, Callaghan GM, Hayes SC, Glenn-Lawson JL. Improving diabetes self-management through acceptance, mindfulness, and values: a randomized controlled trial. J Consult Clin Psychol. 2007;75(2):336–43. doi: 10.1037/0022-006X.75.2.336. [DOI] [PubMed] [Google Scholar]
- 56.Youngwanichsetha S, Phumdoung S, Ingkathawornwong T. The effects of mindfulness eating and yoga exercise on blood sugar levels of pregnant women with gestational diabetes mellitus. Appl Nurs Res. 2014;27(4):227–30. doi: 10.1016/j.apnr.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 57.van Son J, Nyklicek I, Pop VJ, Blonk MC, Erdtsieck RJ, Pouwer F. Mindfulness-based cognitive therapy for people with diabetes and emotional problems: long-term follow-up findings from the DiaMind randomized controlled trial. J Psychosom Res. 2014;77(1):81–4. doi: 10.1016/j.jpsychores.2014.03.013. [DOI] [PubMed] [Google Scholar]
- 58.Tovote KA, Schroevers MJ, Snippe E, et al. Long-term effects of individual mindfulness-based cognitive therapy and cognitive behavior therapy for depressive symptoms in patients with diabetes: a randomized trial. Psychother Psychosom. 2015;84(3):186–7. doi: 10.1159/000375453. [DOI] [PubMed] [Google Scholar]
- 59.Segal ZV, Williams JMG, Teasdale JD, Kabat-Zinn J. Mindfulness-based cognitive therapy for depression. New York: The Guildford Press; 2012. [Google Scholar]
- 60•.Kabat-Zinn J. Full catastrophe living: using the wsidom of your body and mind to face stress, pain, and illness. New York: Bantam; 2013. Foundational book describing Mindfulness-Based Stress Reduction intervention. [Google Scholar]
- 61.Azam MA, Katz J, Fashler SR, Changoor T, Azargive S, Ritvo P. Heart rate variability is enhanced in controls but not maladaptive perfectionists during brief mindfulness meditation following stress-induction: A stratified-randomized trial. Internat J Psychophys. 2015 doi: 10.1016/j.ijpsycho.2015.06.005. [DOI] [PubMed] [Google Scholar]
- 62.Bhatnagar R, Phelps L, Rietz K, et al. The effects of mindfulness training on post-traumatic stress disorder symptoms and heart rate variability in combat veterans. J Altern Complement Med. 2013;19(11):860–1. doi: 10.1089/acm.2012.0602. [DOI] [PubMed] [Google Scholar]
- 63.Gallegos AM, Lytle MC, Moynihan JA, Talbot NL. Mindfulness-Based Stress Reduction to enhance psychological functioning and improve inflammatory biomarkers in trauma-exposed women: a pilot study. Psychol Trauma. 2015 doi: 10.1037/tra0000053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Malarkey WB, Jarjoura D, Klatt M. Workplace based mindfulness practice and inflammation: a randomized trial. Brain Behav Immun. 2013;27(1):145–54. doi: 10.1016/j.bbi.2012.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Creswell JD, Irwin MR, Burklund LJ, et al. Mindfulness-Based Stress Reduction training reduces loneliness and pro-inflammatory gene expression in older adults: a small randomized controlled trial. Brain Behav Immun. 2012;26(7):1095–101. doi: 10.1016/j.bbi.2012.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66•.Holzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspect Psychol Sci. 2011;6(6):537–59. doi: 10.1177/1745691611419671. Foundational paper describing mechanisms by which mindfulnes meditaiton could influence neurophysiology and self-regulation. [DOI] [PubMed] [Google Scholar]
- 67.Vago DR, Silbersweig DA. Self-awareness, self-regulation, and self-transcendence (S-ART): a framework for understanding the neurobiological mechanisms of mindfulness. Front Hum Neurosci. 2012;6:296. doi: 10.3389/fnhum.2012.00296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68•.Valeri L, Vanderweele TJ. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods. 2013;18(2):137–50. doi: 10.1037/a0031034. Important new innovations in statistical approaches for mediation analyses with fewer assumptions than prior methods, and now have fairly user-friendly macros. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69•.Gu J, Strauss C, Bond R, Cavanagh K. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clin Psychol Rev. 2015;37:1–12. doi: 10.1016/j.cpr.2015.01.006. One of the first papers to perform mediation analyses to evlaute evidence behind plausible mediatiors between mindfluness interventions and health. [DOI] [PubMed] [Google Scholar]
- 70.Artinian NT, Fletcher GF, Mozaffarian D, et al. Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: a scientific statement from the American Heart Association. Circulation. 2010;122(4):406–41. doi: 10.1161/CIR.0b013e3181e8edf1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013;127(1):e6–245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tang YY, Ma Y, Wang J, et al. Short-term meditation training improves attention and self-regulation. Proc Natl Acad Sci U S A. 2007;104(43):17152–6. doi: 10.1073/pnas.0707678104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Festinger L. Cognitive dissonance. Sci Am. 1962;207:93–102. doi: 10.1038/scientificamerican1062-93. [DOI] [PubMed] [Google Scholar]
- 74.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55(1):68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- 75.Deci EL, Eghrari H, Patrick BC, Leone DR. Facilitating internalization: the self-determination theory perspective. J Pers. 1994;62(1):119–42. doi: 10.1111/j.1467-6494.1994.tb00797.x. [DOI] [PubMed] [Google Scholar]
- 76.Richardson S, Shaffer JA, Falzon L, Krupka D, Davidson KW, Edmondson D. Meta-analysis of perceived stress and its association with incident coronary heart disease. Am J Cardiol. 2012;110(12):1711–6. doi: 10.1016/j.amjcard.2012.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77•.Kivimaki M, Nyberg ST, Batty GD, et al. Job strain as a risk factor for coronary heart disease: a collaborative meta-analysis of individual participant data. Lancet. 2012;380(9852):1491–7. doi: 10.1016/S0140-6736(12)60994-5. Important collaborative effort to merge data across many studies to evaluate associations of job strain with CVD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chida Y, Steptoe A. Greater cardiovascular responses to laboratory mental stress are associated with poor subsequent cardiovascular risk status: a meta-analysis of prospective evidence. Hypertension. 2010;55(4):1026–32. doi: 10.1161/HYPERTENSIONAHA.109.146621. [DOI] [PubMed] [Google Scholar]
- 79.Radley J, Morilak D, Viau V, Campeau S. Chronic stress and brain plasticity: mechanisms underlying adaptive and maladaptive changes and implications for stress-related CNS disorders. Neurosci Biobehav Rev. 2015 doi: 10.1016/j.neubiorev.2015.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Appelhans BM. Neurobehavioral inhibition of reward-driven feeding: implications for dieting and obesity. Obesity. 2009;17(4):640–7. doi: 10.1038/oby.2008.638. [DOI] [PubMed] [Google Scholar]
- 81.Lieberman LS. Dietary, evolutionary, and modernizing influences on the prevalence of type 2 diabetes. Annu Rev Nutr. 2003;23:345–77. doi: 10.1146/annurev.nutr.23.011702.073212. [DOI] [PubMed] [Google Scholar]
- 82.Brewer JA, Elwafi HM, Davis JH. Craving to quit: psychological models and neurobiological mechanisms of mindfulness training as treatment for addictions. Psychol Addict Behav. 2013;27(2):366–79. doi: 10.1037/a0028490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Brand M, Young KS, Laier C. Prefrontal control and internet addiction: a theoretical model and review of neuropsychological and neuroimaging findings. Front Hum Neurosci. 2014;8:375. doi: 10.3389/fnhum.2014.00375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Elwafi HM, Witkiewitz K, Mallik S, Iv TA, Brewer JA. Mindfulness training for smoking cessation: moderation of the relationship between craving and cigarette use. Drug Alc Depend. 2013;130(1–3):222–9. doi: 10.1016/j.drugalcdep.2012.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lachman ME, Weaver SL. The sense of control as a moderator of social class differences in health and well-being. J Pers Soc Psychol. 1998;74(3):763–73. doi: 10.1037//0022-3514.74.3.763. [DOI] [PubMed] [Google Scholar]
- 86.Kelly JF, Greene MC. Where there’s a will there’s a way: a longitudinal investigation of the interplay between recovery motivation and self-efficacy in predicting treatment outcome. Psychol Addictive Behav. 2013 doi: 10.1037/a0034727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 88.Ajzen I. Theories of cognitive self-regulation: the theory of planned behavior. Org Behav Hum Decis Process. 1991;50(2):179–211. [Google Scholar]
- 89.Jerant A, Moore M, Lorig K, Franks P. Perceived control moderated the self-efficacy-enhancing effects of a chronic illness self-management intervention. Chron Illness. 2008;4(3):173–82. doi: 10.1177/1742395308089057. [DOI] [PubMed] [Google Scholar]
- 90.Ajzen I. Perceived behavioral control, self-efficacy, locus of control, and the theory of planned behavior. J Appl Soc Psychol. 2002;32(4):665–83. [Google Scholar]
- 91.Surtees PG, Wainwright NW, Luben R, Khaw KT, Day NE. Mastery, sense of coherence, and mortality: evidence of independent associations from the EPIC-Norfolk Prospective Cohort Study. Health Psychol. 2006;25(1):102–10. doi: 10.1037/0278-6133.25.1.102. [DOI] [PubMed] [Google Scholar]
- 92.Steptoe A, Wardle J. Locus of control and health behaviour revisited: a multivariate analysis of young adults from 18 countries. Br J Psychol. 2001;92(Pt 4):659–72. doi: 10.1348/000712601162400. [DOI] [PubMed] [Google Scholar]
- 93.Margolin A, Schuman-Olivier Z, Beitel M, Arnold RM, Fulwiler CE, Avants SK. A preliminary study of spiritual self-schema (3-S(+)) therapy for reducing impulsivity in HIV-positive drug users. J Clin Psychol. 2007;63(10):979–99. doi: 10.1002/jclp.20407. [DOI] [PubMed] [Google Scholar]
- 94.McCubbin T, Dimidjian S, Kempe K, Glassey MS, Ross C, Beck A. Mindfulness-based stress reduction in an integrated care delivery system: one-year impacts on patient-centered outcomes and health care utilization. Permanente J. 2014;18(4):4–9. doi: 10.7812/TPP/14-014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Neff K, Dahm K. Self-Compassion: what it is, what it does, and how it relates to mindfulness. In: Robinson M, Meier B, Ostafin B, editors. Mindfulness and Self-Regulation. New York: Springer; 2015. [Google Scholar]
- 96.Kuyken W, Watkins E, Holden E, et al. How does mindfulness-based cognitive therapy work? Behav Res Therapy. 2010;48(11):1105–12. doi: 10.1016/j.brat.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 97.Lillis J, Levin ME, Hayes SC. Exploring the relationship between body mass index and health-related quality of life: a pilot study of the impact of weight self-stigma and experiential avoidance. J Health Psychol. 2011;16(5):722–7. doi: 10.1177/1359105310388321. [DOI] [PubMed] [Google Scholar]
- 98.Neff KD. The role of self-compassion in development: a healthier way to relate to oneself. Hum Dev. 2009;52(4):211–4. doi: 10.1159/000215071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Breines JG, Chen S. Self-compassion increases self-improvement motivation. Personal Soc Psychol Bull. 2012;38(9):1133–43. doi: 10.1177/0146167212445599. [DOI] [PubMed] [Google Scholar]
- 100.Terry ML, Leary MR, Mehta S, Henderson K. Self-compassionate reactions to health threats. Personal Soc Psychol Bull. 2013;39(7):911–26. doi: 10.1177/0146167213488213. [DOI] [PubMed] [Google Scholar]
- 101.Thurston RC, Kubzansky LD. Women, loneliness, and incident coronary heart disease. Psychosom Med. 2009;71(8):836–42. doi: 10.1097/PSY.0b013e3181b40efc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Hemingway H, Marmot M. Evidence based cardiology: psychosocial factors in the aetiology and prognosis of coronary heart disease. Systematic review of prospective cohort studies. BMJ. 1999;318(7196):1460–7. doi: 10.1136/bmj.318.7196.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Steptoe A, Shankar A, Demakakos P, Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc Natl Acad Sci U S A. 2013;110(15):5797–801. doi: 10.1073/pnas.1219686110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Mantzios M, Giannou K. Group vs. Single mindfulness meditation: exploring avoidance, impulsivity, and weight management in two separate mindfulness meditation settings. Appl Psychol Health Well-Being. 2014;6(2):173–91. doi: 10.1111/aphw.12023. [DOI] [PubMed] [Google Scholar]
- 105.Loucks EB. Meditation intervention reviews: selecting ideal control groups for meditation interventions. JAMA Int Med. 2014;174(7):1194–5. doi: 10.1001/jamainternmed.2014.1924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Raichle ME, MacLeod AM, Snyder AZ, Powers WJ, Gusnard DA, Shulman GL. A default mode of brain function. Proc Natl Acad Sci U S A. 2001;98(2):676–82. doi: 10.1073/pnas.98.2.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Gusnard DA, Raichle ME, Raichle ME. Searching for a baseline: functional imaging and the resting human brain. Nat Rev Neurosci. 2001;2(10):685–94. doi: 10.1038/35094500. [DOI] [PubMed] [Google Scholar]
- 108.Whitfield-Gabrieli S, Moran JM, Nieto-Castanon A, Triantafyllou C, Saxe R, Gabrieli JD. Associations and dissociations between default and self-reference networks in the human brain. NeuroImage. 2011;55(1):225–32. doi: 10.1016/j.neuroimage.2010.11.048. [DOI] [PubMed] [Google Scholar]
- 109.Brewer JA, Worhunsky PD, Gray JR, Tang YY, Weber J, Kober H. Meditation experience is associated with differences in default mode network activity and connectivity. Proc Natl Acad Sci U S A. 2011;108(50):20254–9. doi: 10.1073/pnas.1112029108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Brewer JA, Garrison KA, Whitfield-Gabrieli S. What about the “Self” is Processed in the Posterior Cingulate Cortex? Front Hum Neurosci. 2013;7:647. doi: 10.3389/fnhum.2013.00647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Garrison KA, Santoyo JF, Davis JH, Thornhill TA, Kerr CE, Brewer JA. Effortless awareness: using real time neurofeedback to investigate correlates of posterior cingulate cortex activity in meditators’ self-report. Front Hum Neurosci. 2013;7:440. doi: 10.3389/fnhum.2013.00440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Garrison KA, Scheinost D, Worhunsky PD, et al. Real-time fMRI links subjective experience with brain activity during focused attention. NeuroImage. 2013 doi: 10.1016/j.neuroimage.2013.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Garrison KA, Zeffiro TA, Scheinost D, Constable RT, Brewer JA. Meditation leads to reduced default mode network activity beyond an active task. Cog Affect Behav Neurosci. 2015 doi: 10.3758/s13415-015-0358-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kerr CE, Josyula K, Littenberg R. Developing an observing attitude: an analysis of meditation diaries in an MBSR clinical trial. Clin Psychol Psychother. 2011;18:80–93. doi: 10.1002/cpp.700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Fresco DM, Moore MT, van Dulmen MH, et al. Initial psychometric properties of the experiences questionnaire: validation of a self-report measure of decentering. Behav Ther. 2007;38(3):234–46. doi: 10.1016/j.beth.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 116.Safran J, Segal ZV. Interpersonal process in cognitive therapy. New York: Basic Books; 1990. [Google Scholar]
- 117.Bernstein A, Hadash Y, Lichtash Y, Tanay G, Shepherd K, Fresco DM. Decentering and related constructs: a critical review and meta-cognitive processes model. Perspectiv Psychol Sci. 2015 doi: 10.1177/1745691615594577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ayduk O, Kross E. From a distance: implications of spontaneous self-distancing for adaptive self-reflection. J Pers Soc Psychol. 2010;98(5):809–29. doi: 10.1037/a0019205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Shapiro SL, Carlson LE, Astin JA, Freedman B. Mechanisms of Mindfulness. J Clin Psychol. 2006;62:373–86. doi: 10.1002/jclp.20237. [DOI] [PubMed] [Google Scholar]
- 120.Miller WR. Motivational interviewing: research, practice, and puzzles. Addict Behav. 1996;21(6):835–42. doi: 10.1016/0306-4603(96)00044-5. [DOI] [PubMed] [Google Scholar]
- 121.Baer RA, Smith GT, Allen KB. Assessment of mindfulness by self-report: the Kentucky inventory of mindfulness skills. Assessment. 2004;11:191–206. doi: 10.1177/1073191104268029. [DOI] [PubMed] [Google Scholar]
- 122.Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: an experiential approach to behavior change. 1999 [Google Scholar]
- 123.Shapiro SL, Carlson LE, Astin JA, Freedman B. Mechanisms of mindfulness. J Clin Psychol. 2006;62(3):373–86. doi: 10.1002/jclp.20237. [DOI] [PubMed] [Google Scholar]
- 124.Jacobs TL, Epel ES, Lin J, et al. Intensive meditation training, immune cell telomerase activity, and psychological mediators. Psychoneuroendocrinol. 2011;36:664–81. doi: 10.1016/j.psyneuen.2010.09.010. [DOI] [PubMed] [Google Scholar]
- 125.Carmody J, Baer RA, Lykins EL, Olendzki N. An empirical study of the mechanisms of mindfulness in a mindfulness-based stress reduction program. J Clin Psychol. 2009;65:613–26. doi: 10.1002/jclp.20579. [DOI] [PubMed] [Google Scholar]
- 126.Roos CR, Kirouac M, Pearson MR, Fink BC, Witkiewitz K. Examining temptation to drink from an existential perspective: associations among temptation, purpose in life, and drinking outcomes. Psychol Addict Behav. 2015 doi: 10.1037/adb0000063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Pearson MR, Brown D, Bravo A, Witkiewitz K. Staying in the moment and inding purpose: The associations of trait mindfulness, decentering, and purpose in life with depressive symptoms, anxiety symptoms, and alcohol-related problems. Mindfulness. 2015;6 [Google Scholar]
- 128.Farb NA, Segal ZV, Mayberg H, et al. Attending to the present: mindfulness meditation reveals distinct neural modes of self-reference. Soc Cogn Affect Neurosci. 2007;2(4):313–22. doi: 10.1093/scan/nsm030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Mehling WE, Price C, Daubenmier JJ, Acree M, Bartmess E, Stewart A. The multidimensional assessment of interoceptive awareness (MAIA) PLoS ONE. 2012;7(11):e48230. doi: 10.1371/journal.pone.0048230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Mehling WE, Gopisetty V, Daubenmier J, Price CJ, Hecht FM, Stewart A. Body awareness: construct and self-report measures. PLoS ONE. 2009;4(5):e5614. doi: 10.1371/journal.pone.0005614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Silverstein RG, Brown AC, Roth HD, Britton WB. Effects of mindfulness training on body awareness to sexual stimuli: implications for female sexual dysfunction. Psychosom Med. 2011;73(9):817–25. doi: 10.1097/PSY.0b013e318234e628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Bornemann B, Herbert BM, Mehling WE, Singer T. Differential changes in self-reported aspects of interoceptive awareness through 3 months of contemplative training. Front Psychol. 2014;5:1504. doi: 10.3389/fpsyg.2014.01504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Hill DM, Craighead LW, Safer DL. Appetite-focused dialectical behavior therapy for the treatment of binge eating with purging: a preliminary trial. Int J Eat Disord. 2011;44(3):249–61. doi: 10.1002/eat.20812. [DOI] [PubMed] [Google Scholar]
- 134.Ekkekakis P, Parfitt G, Petruzzello SJ. The pleasure and displeasure people feel when they exercise at different intensities: decennial update and progress towards a tripartite rationale for exercise intensity prescription. Sports Med. 2011;41(8):641–71. doi: 10.2165/11590680-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 135.Rhodes RE, Kates A. Can the affective response to exercise predict future motives and physical activity behavior? A systematic review of published evidence. Ann Behav Med. 2015 doi: 10.1007/s12160-015-9704-5. [DOI] [PubMed] [Google Scholar]
- 136.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c332. doi: 10.1136/bmj.c332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c869. doi: 10.1136/bmj.c869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Boutron I, Moher D, Altman DG, Schulz KF, Ravaud P. Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Ann Intern Med. 2008;148(4):295–309. doi: 10.7326/0003-4819-148-4-200802190-00008. [DOI] [PubMed] [Google Scholar]