This and Related “Classic” Articles Appear on Prsjournal.Com for Journal Club Discussions.
Summary:
This article is a 42-year history of the development of a comprehensive face-lift technique by the author. It describes how the composite rhytidectomy has been constructed, anatomical area by anatomical area, over the author’s lifetime career as a plastic surgeon. Over the course of these years, beginning with Skoog’s 1973 description of using the platysma muscle of the lower face, it describes how progressively the other significant structures of anatomy necessary to be used in achieving significant rejuvenation have been analyzed by the author and in turn surgically repositioned. The theory was based on creating a composite flap of the face, keeping the orbicularis oculi muscle, facial platysma muscle, and cheek fat in their normal anatomical and intimate relationship with each other by using the skin as the carriage. In addition, differences of vectors between the composite rhytidectomy and traditional techniques are demonstrated. The gradual and persistent pursuit of periorbital rejuvenation using the lower eyelid fat and the septal orbitale is described. Each of the anatomical structures involved and the description of their importance and surgical execution have been published over the surgical career of the author, including use of the same principles for reversing suboptimal face-lift results.
My lifetime in plastic surgery is a mirror image of my pursuit of the face-lift technique that has consumed my time and energy for 42 years. As every plastic surgeon can attest, the advancing of any procedure of interest must be viewed in the context of the past, the present, and the future. The past belongs to the many surgeons whose contributions have provided all of us with the knowledge and experiences essential in our training and understanding of each surgical procedure. The present belongs to the current and time-honored philosophies practiced by contemporary surgeons who provide the deliverance of aesthetic surgery to the world at large. The future of aesthetic surgical techniques, although unwritten today, will determine the ultimate destiny of every operation we perform today. As an aesthetic plastic surgeon, I honor the past and remain in awe of the extraordinary surgeons who created the groundwork for modern facial rejuvenation techniques. In contrast, for many reasons, I was never totally satisfied with what were the “present” traditional procedures and continually thought about what innovations could be made available in search of the “perfect face lift.” Unlike nasal surgery and breast surgery, which allow surgeons individual license and opinions concerning size and shape, I have always thought that the ultimate goal of facial rejuvenation is essentially predetermined by nature, which is the anatomy of youth that every human once possessed before the aging process began. This philosophy simplified this pursuit of the desired result. In contrast, this philosophy did not provide the surgical maneuvers necessary to acquire the desired result. This article describes my own personal journey throughout my professional career with each documented step along the way.
HISTORY
From 1970 to 1973, my early exposure to face-lift surgery was in my residency at New York University. There was an extraordinarily high exposure to face-lift surgery compared with most plastic surgery teaching programs. This was because several of the faculty had achieved international acclaim and had large face-lift practices, because New York City was one of the few cities in the world where aesthetic surgery was firmly established at that time. The basic face-lift procedure was a subcutaneous undermine and redrape of the skin. The incisions were usually pretragal and retroauricular. Cervical changes were minimal, as submental incisions were rare and the undermined cervical skin was advanced behind the ear and the excess excised. Forehead lifts were rare, although they were being performed in Europe and South America. This residency provided not only many hours assisting these accomplished aesthetic surgeons, but it also allowed all the residents to independently perform face lifts. The blepharoplasties that were being performed at that time were standard upper blepharoplasties with skin and fat removal, and lower blepharoplasties with either skin only or skin-muscle flaps preceding lower eyelid fat removal. As residents in all training programs, the results we saw were very short-term and we rarely if ever saw the long-term results of our teachers.
In 1973, I completed my residency and joined Dr. Mark Lemmon in Dallas, Texas, which by all criteria was a very fortunate and unexpected episode in my face-lift career. In February of 1973, Dr. Lemmon had attended the Baker Gordon symposium in Miami, Florida, where the guest surgeon was Dr. Tord Skoog. Dr. Skoog, a brilliant innovative surgeon from Sweden, had developed the first face lift using deep tissue to enhance the results. Rather than undermining the skin from the platysma muscle of the lower face, he lifted that muscle en bloc with the skin and continued that unique elevation into the neck. The procedure was performed with local anesthesia provided by nerve blocks. Up to that point, Dr. Lemmon had performed the subcutaneous type face lifts, but was unhappy with the short-term improvements. After seeing the one demonstration by Dr. Skoog, Dr. Lemmon bravely adopted the technique in spite of the fact that the textbook by Dr. Skoog1 had not yet been published. When I joined Dr. Lemmon in September of 1973, I was shocked and a bit frightened to observe him perform the operation because, when he elevated the “Skoog flap” off of the subplatysma tissue, the facial nerves that were unanesthetized would cause facial movement when the blunt dissection was performed. However, after observing the minimal ecchymosis and edema of the face with his face lifts, and the absence of facial nerve problems with impressive facial contour, I became an enthusiastic convert in an era before publication of the superficial musculoaponeurotic system (SMAS) technique in 1976. Skoog published his impressive textbook in 1974 and died at approximately the same time, before he could publish his technique in a plastic surgery journal. Dr. Lemmon and I presented our series in San Francisco in 1978 and published it in 1980 in Plastic and Reconstructive Surgery,2 which became the first and only series on the Skoog technique. In fact, I was so enthusiastic about it, I was asked to demonstrate this operation for Drs. Aston and Casson at New York University in 1975 before the SMAS article3 was published. The SMAS was in fact a term for the operation created by Dr. Paul Tessier, the great craniofacial surgeon. He told me that because he was familiar with Skoog and his innovation, he first lifted the subcutaneous tissue, and then elevated the platysma, calling it the superficial musculoaponeurotic system. This was published before our publication on the Skoog procedure was mentioned in a journal. Because surgeons could, as they had always done, lift the skin first, the SMAS technique of variable extensiveness became and remains the universally accepted procedure of choice for most surgeons around the world. To this day, this same technique persists and is taught and discussed at most symposia almost 40 years later.
In the late 1970s, the “era of the neck” was beginning because of the influence of surgeons in Mexico and California. I then incorporated the neck dissection into the Skoog procedure. This variation created three distinct planes. The neck dissection was preplatysmal, the Skoog part was “sub-SMAS,” and the upper face continued to be subcutaneous. This was published in 1984 and was entitled the “tri-plane rhytidectomy.”4 In keeping with the accepted cervical rejuvenation, the excessive fat was excised, and the cervical platysma was transected, regretfully, as a window-shade deformity commonly followed.
THE DEEP PLANE RHYTIDECTOMY
The triplane approach was used until 1985. As the postoperative results were observed, there were complaints from patients about the unchanged nasolabial fold; thus, I began reading anatomy, having never dissected a cadaver. I found that the cheek fat, the fat overlying the zygomaticus muscles, was totally cranial to the SMAS, and in fact there was a normal dissection plane between the cheek fat and the zygomaticus muscles, as the zygomaticus major was the junction between the fat and the SMAS. This led me to begin attempting to elevate the fat with the skin but continuing to keep the Skoog flap in continuity with this dissection. It was easy to visualize the zygomaticus muscles, which made it easier to be sure that all of this cheek fat was elevated to improve the nasolabial fold. Early photographs were impressive. As a follow-up to the triplane name, I called this the “deep plane rhytidectomy” and presented it for the first time in Santa Barbara in 19895 at the winter American Society for Aesthetic Plastic Surgery face-lift symposium. The audience was very receptive, as this was the first advance since the SMAS technique in 1976. I was invited to demonstrate it at symposia in New York, San Francisco, and Miami months later. All three hosts adopted and incorporated the principle6–8 and in fact still use it and teach it today, 25 years later. It was published in 1990.9
The deep plane dissection continued to be used and is in fact still an integral maneuver in the composite face lift. However, I followed many deep plane patients for years and was a bit disappointed in many of the 10-year results, because the cheek fat repositioning had no superior vertical anchor and therefore, with aging, whatever improvement initially gained appeared minimally maintained. To be honest, I felt an obligation to publish an article describing short-term improvement but long-term disappointment.10 To this day, I still perform the deep plane dissection with an open neck dissection with muscle approximation on every composite face lift, but almost never perform a pure lateral vector rhytidectomy.
THE COMPOSITE FACE LIFT
Although the deep plane procedure seemed at first to be satisfactory and certainly an improvement over SMAS techniques, I was still a bit unhappy with the overall improvement in the facial rejuvenation I thought should be so much more impressive. It appeared that the lower face and neck were too improved compared with the eyes and forehead; thus, I decided that I had created the disharmonious facial appearance that was always obvious and unattractive. I then saw a patient who previously had a deep plane face lift performed by me with such an appearance (Fig. 1) that caused me to decide to perform an isolated orbicularis repositioning combined with an isolated forehead lift. Suddenly, for the first time in my surgical career, I saw what I thought was the nearest I had come to creating an appearance of harmony unseen in publications or at symposia. From that day forward, the orbicularis oculi muscle was always a part of the deep plane flap, which now contained the orbicularis, the cheek fat, and the platysma. I wanted to differentiate this operation from a deep plane face lift and decided (Fig. 2) to publish it and name it a “composite face lift,” because the word “composite” means “made of many parts.” Surgeons were already familiar with the term, having used composite grafts from the ear to the nose that contained skin, fat, and cartilage. From observing the results, it became obvious that this unique surgical maneuver had shortened the lower eyelid and elevated the eyelid-cheek junction. It was at this point in my career that my goal was finally in sight. For the first time in my experience, the endpoint of a face lift had become crystal clear. My only guideline was youth that I observed in mother and daughter lookalikes. I published a book in 1993 entitled Composite Rhytidectomy11 and included many mothers and daughters with very similar features to prove my point of created youth. It was not until years later that I could demonstrate, with the same patient in youth and in age, a postoperative result where each patient’s youthful anatomy could be recreated. Having been in practice many years and having excellent photographs of many patients who had cosmetic surgery when young, I at last could see my dream of a true facial rejuvenation including facial areas never significantly changed with conventional face-lift techniques.
Fig. 1.

(Left) Following a deep plane rhytidectomy. (Center) Areas previously unaddressed. (Right) After orbicularis repositioning and forehead lift. (Reprinted from Hamra ST. Lower eyelid-cheek junction rejuvenation. In: Farhadieh RD, Bulstrode NW, Cugno S, eds. Plastic and Reconstructive Surgery: Approaches and Techniques. 1st ed. London: Wiley-Blackwell; 2015:976–991.)
Fig. 2.
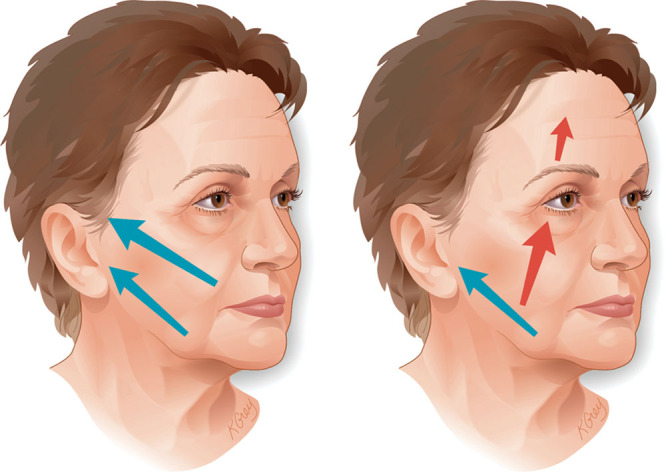
(Left) Conventional face lift. (Right) Composite face lift. (Adapted from Hamra ST. Prevention and correction of the “face-lifted” appearance. Facial Plast Surg. 2000;16:215–229.)
I then published two articles,12,13 one on the composite face lift and the second on elevation of the orbicularis muscle. I felt the latter was worthy of a separate article because it was the first demonstration of the shortened lower eyelid and the elevated eyelid-cheek junction. At the time, I was still performing lower eyelid fat removal, which had been the universally accepted procedure since 1928.14
ARCUS MARGINALIS RELEASE
In spite of results that were improved markedly over traditional techniques, the lower eyelids, regardless of improvement with the orbicularis elevation, still did not have a truly youthful appearance and in fact often remained too hollow in spite of a shortened lower eyelid. I found no answer until I read a little-known book by Loeb, who had taken the most medial fat pad of the lower eyelid and transposed it into the nasojugal groove.15 Although he did not elevate the orbicularis and he continued to remove the middle and lateral fat, it made sense. I then decided to preserve all of the fat pads under the repositioned orbicularis muscle. To keep all of the fat, I incised the arcus marginalis, which is the junction between the septum orbitale and the orbital rim. Releasing this junction would allow visualization of all of the fat that could exit the orbit most directly and fall inferiorly so it could be sutured to the soft tissue inferior to the orbital rim. The septum orbitale was otherwise untouched because of the traditional thinking that manipulation of the septum may create lower eyelid malposition. This procedure was published and was entitled the “arcus marginalis release.”16,17
THE ZYGOMATICUS-ORBICULAR FLAP AND THE SEPTAL RESET
Even though I felt that the lower eyelid rejuvenation was greatly improved by suturing the fat over the orbital rim and elevating the orbicularis oculi muscle, I continued to observe results that were not optimal. I felt that the tension I could place on the orbicularis muscle alone was inadequate. On occasion, I attempted a subperiosteal dissection, but the thickness of the flap and the removal of the periosteum inferior to the orbital rim presented difficulty in many cases. I then discovered that I could leave the orbicularis muscle in normal continuity to the zygomaticus muscles and thereby create a flap that was more supple and flexible, and allowed what I thought was more effective redraping of the upper cheek. I discovered I could undermine the orbicularis lateral to the origin of the zygomaticus muscles and enter the area medial to the zygomaticus muscles, thereby creating a flap with the orbicularis, zygomaticus, skin, and cheek fat. This allowed me to apply more and in fact extraordinary tension compared to the simple orbicularis repositioning when securing it to the periorbital periosteum. Because the origin of the zygomaticus muscles was not displaced, the intramalar distance remained normal. The cheek fat within the repositioned flap was elevated over the malar eminence, thereby creating the high cheek mass, which is the normal anatomy of youth. For simplicity, I entitled this maneuver a “zygorbicular” flap, which is a contraction of zygomaticus-orbicularis, and published it in 199818 as an ideal midface plane. Many years later, it was described in published anatomical cadaver dissections.19
THE SEPTAL RESET
In the years preceding the process of developing the zygorbicular flap, I observed that the fat transposed over the orbital rim did not always have a predictable result. Although small sutures were used to secure the fat to the underlying soft tissue, the suture placement was often difficult because sutures passed with the needle through the fat would not always hold. Throughout my residency and for years afterward, it was always taught that manipulation of the septum may ultimately produce an ectropion. In spite of this fear, I decided that if the fat remained attached to the septum, it can easily be brought over the orbital rim safely. After incising the arcus marginalis, the newly incised inferior border of the septum was essentially reset over the orbital rim, and thus the term “septal reset” was created (Fig. 3). Although it was included in the 1998 article on the zygorbicular dissection, it was not emphasized enough in spite of its invaluable use to me in orbital rejuvenation. I had demonstrated it at the Dallas aesthetic symposium. In 2004, I published the septal reset article in a more extensive fashion with a clearer description than the 1998 article.20 This article was accompanied by an article by Barton et al.,21 who verified its reproducibility, having seen it demonstrated at the symposium.
Fig. 3.
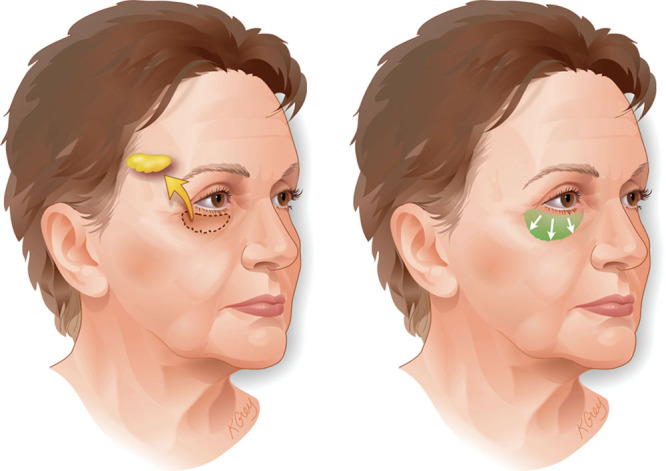
(Left) Conventional blepharoplasty. (Right) Composite blepharoplasty with septal reset. (Adapted from Hamra ST. Prevention and correction of the “face-lifted” appearance. Facial Plast Surg. 2000;16:215–229.)
When the fat is sutured without the septum over the orbital rim, the overlying orbicularis muscle and skin rest on a very soft cushion, often reflecting less than smooth skin of the lower eyelid. The septal reset, in contrast, provides a very firm foundation for the overlying muscle-skin flap. This clearly simulates the anatomy of the youthful lower eyelid and provides also for the absence of the eyelid-cheek junction. The sine qua non of a youthful face is a high cheek mass and an absent eyelid-cheek junction, which is what can be achieved with a septal reset and zygorbicular combination.
HOLLOW EYES AND THE LATERAL SWEEP
In the course of always performing the zygorbicular dissection and the septal reset, I saw many patients who had previous face-lift surgery and often showed the typical recognizable stigmata of previous face lifts. As I applied the principles of the new technique to these patients, I was excited to discover that most unfortunate signs of previous surgery could be effectively corrected. It then became obvious to me that the appearance of these patients, many of whom were mine from previous years, was attributable to conventional techniques, most commonly SMAS-type procedures and lower eyelid fat removal. Because the aggressively repositioned SMAS effectively straightened out the jawline, it would actually stay longer than the upper portion of the face-lift dissection. The jawline tension was superolateral and only a short distance. The vector from the upper nasolabial fold to the helical area was a longer distance and almost parallel. This was the vector of the deep plane and all lateral vector techniques. This portion of the face frequently would drop on top of the firm lower face and jawline. For years, the lay public had described these patients as appearing as though they are “in a wind tunnel.” In addition to this appearance, many patients exhibited a very hollow lower eyelid that was deeper than normally seen in the unoperated person. Because lower eyelid fat removal had always been the modus operandi in lower eyelid rejuvenation, I began using the septal reset on all secondary face-lift and eyelid patients and could almost always recruit some fat from the lower eyelid, regardless of how hollow it appeared. These two signs of previous aesthetic surgery then became clearer, because I could reverse both signs with the new techniques. Because the appearance of the operated face was invariably pulled laterally, I called this the “lateral sweep” and published the 1998 article entitled “Frequent Face Lift Sequelae: Hollow Eyes and the Lateral Sweep: Cause and Repair.”22 In a sense, this became very gratifying, because patients who had acquired this appearance often found that it had a negative impact on their lives. Certainly, it was clear that the surgeons did not intend this to occur, as the problem occurred only because of the use of time-honored techniques. Obviously, every patient who undergoes conventional techniques does not acquire this appearance but, without question, those who do have this appearance more often previously were operated on with conventional face-lift and blepharoplasty procedures. These could almost always be markedly improved, erasing the typical appearance of previous face-lift surgery. There is, however, a consistent anatomical area that surgeons always attempted to treat, usually unsuccessfully. This area was described in the composite face-lift article in 1992 as the “malar crescent” (Fig. 4). The composite face-lift dissection exposed this to be the normal inferior border of the orbicularis muscle. Attempts to improve it had included liposuction, steroid injection, and excision. I discovered while elevating the cheek toward the eye in a superior medial vector that this deformity, often called festoons, could be successfully made to disappear. It worked whether the deformity existed before a primary face lift or it was an outcome of the lateral vector face lift that made the crescent even more obvious.
Fig. 4.
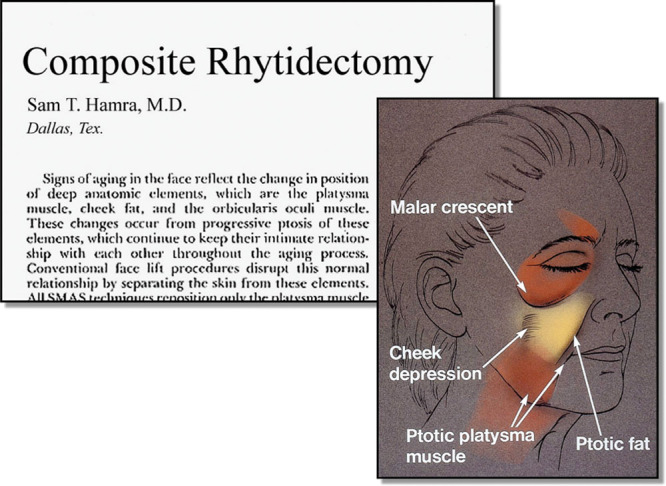
Identification of the malar crescent. (Reprinted from Hamra ST. Composite rhytidectomy. Plast Reconstr Surg. 1992;90:1–13.)
THE MEDIAL VECTOR FOREHEAD LIFT
The forehead lift in traditional face-lift techniques is optional and in fact is performed only in a minority of face lifts performed throughout the world. Frequently, the patient elects not to have it performed, and often many surgeons prefer not to perform it, as it extends the procedure and is thought to prolong the recovery. Because of the nature of the lateral vector face lifts, whether SMAS, subcutaneous, high SMAS, or deep plane, there is no true necessity for a forehead lift. However, when performing a composite lift, the superomedial vector of the upper face obligates the surgeon to perform a medial vector forehead lift to prevent an obvious deformity of “bunching.” Because most secondary face-lift requests are from patients who did not have a forehead lift the first time, one can reestablish harmony for these patients by including the obligatory forehead lift with the composite face lift.
THE GOAL OF A COMPOSITE RHYTIDECTOMY
The endpoint of facial rejuvenation is the Webster’s definition of rejuvenation, which is “to make young again.” Whereas breast surgery and rhinoplasty surgery allow the surgeon a certain amount of artistic license to create what they feel and the patient feels is the desired appearance, this is not the case for facial rejuvenation. It is easy to analyze a young face and, except for inherited variations, there are areas of absolute youth that are obtainable. In the case of the aging face, surgeons forever have understood a better jawline and neckline and have sought to produce these areas with standard techniques. In general, there are two areas of anatomy hard to recreate with standard techniques. These are the high cheek mass and the absent eyelid-cheek junction seen on every young face, with rare exception.
Figure 5 shows a 75-year-old patient who exhibits all the advanced signs of the aging face. To demonstrate the vectors, the cheek fat and orbicularis muscle were painted on the face in repose and then photographed with manipulation of the face in an attempt to demonstrate the ultimate goal of surgery. The postoperative view after 1 year shows how the desired anatomical changes have in fact been obtained.
Fig. 5.
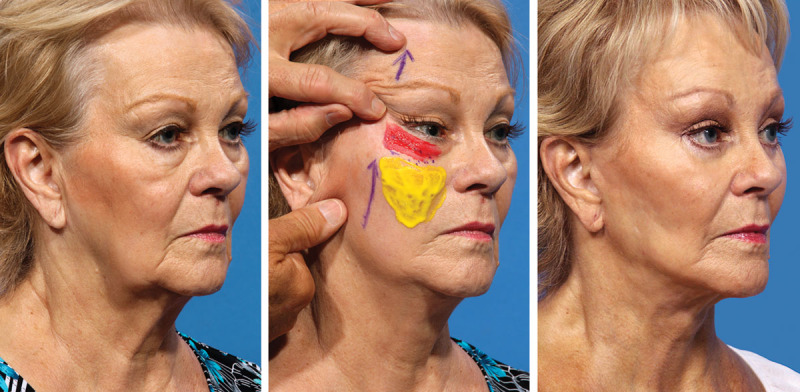
(Left) Preoperative appearance. (Center) Demonstration of the goal of surgery. (Right) One-year after composite face lift.
To demonstrate the goal of a composite face lift, the following patients can be analyzed. The patient in Figure 6 presented with all of the signs of the aging face at age 55 years. In addition to the excessive lower eyelid fat, she exhibited also the malar crescent and a high hairline. She had microgenia and a bulbous nasal tip. The postoperative result, in addition to the face, neck, and forehead rejuvenation, includes a high cheek mass and an absent eyelid-cheek junction. Figure 7 shows another example of the aging face in a 60-year-old patient. The yellow overlay represents the cheek fat that has been moved in a superomedial vector to create the high cheek mass. The septal reset has created the shortened lower eyelid with an absent eyelid-cheek junction. Because of cheek fat repositioning and a septal reset, there is never an indication when a composite face lift is performed to inject fat into the lower eyelid or midface. All patients have photographs of themselves in youth. I have been fortunate over a long career to perform surgery on young patients who were photographed carefully, including faces, and then to see them again many years later after normal aging has occurred. The patients in Figure 8 and Figure 9 are twins, shown at age 26 and then at age 52 years. The postoperative views demonstrate the high cheek mass and absent eyelid-cheek junction, quite similar to their anatomy of youth.
Fig. 6.

Before and after composite face lift.
Fig. 7.

Before and after composite face lift: creation of high cheek mass and absent eyelid-cheek junction. (Adapted from Hamra ST. Lower eyelid-cheek junction rejuvenation. In: Farhadieh RD, Bulstrode NW, Cugno S, eds. Plastic and Reconstructive Surgery: Approaches and Techniques. 1st ed. London: Wiley-Blackwell; 2015:976–991.)
Fig. 8.

(Left) Age 26 years. (Center) Preoperatively at age 52 years. (Right) After composite face lift.
Fig. 9.

(Left) Age 26 years. (Center) Preoperatively at age 52 years. (Right) After composite face lift.
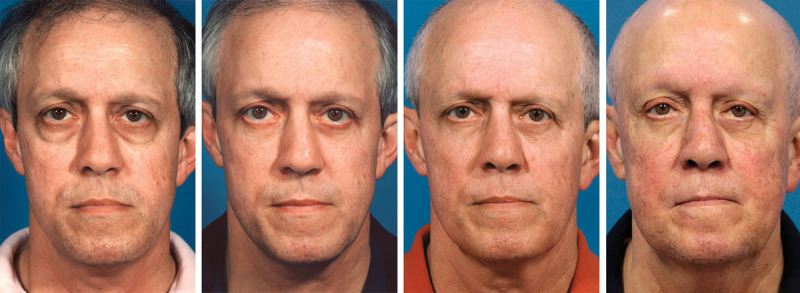
Figure 10 demonstrates the hollow eye and lateral sweep that resulted from a previous conventional rhytidectomy and blepharoplasty. Shown here is the postoperative correction of the two signs of surgery, and correction of the “pixie ear.” The patient in Figure 11 is shown with postoperative results at 1 year, 13 years, and 18 years after surgery. This demonstrates the long-term stable results of a composite face lift. Figure 12 shows a 22-year postoperative result of a septal reset. The significant improvement in the eyelid-cheek junction has been maintained.
Fig. 10.

(Left) Hollow eyes and lateral sweep. (Right) Postoperative correction.
Fig. 11.

(Left to right) Preoperatively, 1 year postoperatively, 13 years postoperatively, and 18 years postoperatively. (Far left and second from right reprinted from Hamra ST. Lower eyelid-cheek junction rejuvenation. In: Farhadieh RD, Bulstrode NW, Cugno S, eds. Plastic and Reconstructive Surgery: Approaches and Techniques, 1st ed. London: Wiley-Blackwell; 2015:976–991.)
Fig. 12.
(Left to right) Preoperatively, 1 year postoperatively, 10 years postoperatively, and 22 years postoperatively. (Left and second from left reprinted from Hamra ST. Arcus marginalis release and orbital fat preservation in midface rejuvenation. Plast Reconstr Surg. 1995:96:354–362. Second from right reprinted from Hamra, ST. Lower eyelid-cheek junction rejuvenation. In: Farhadieh RD, Bulstrode NW, Cugno S, eds. Plastic and Reconstructive Surgery: Approaches and Techniques, 1st ed. London: Wiley-Blackwell; 2015:976–991.)
CONCLUSIONS
I have attempted to describe my professional lifetime journey as I endeavored to achieve significant results in facial rejuvenation. As with every aesthetic procedure, no one can obtain a perfect result, but results will only improve if we continue to try new techniques. In spite of the reality of social and economic changes in the world today, there will always be patients who want to enhance their appearance as much as possible. Life expectancy is increasing because of improved medical advances and therefore it is only logical that patients want to continue appearing attractive and feeling healthy. I have published these articles over many years in an attempt to share the knowledge with my colleagues everywhere, because all of us have learned from our teachers through their publications. As with any advanced technique, there will always be many who reject these innovations for reasons of their own choosing. Nevertheless, I have been gratified that there are many surgeons who have incorporated many of these techniques into their practice. A recently published article23 listed the 50 most significant articles on aesthetic surgery in the past 50 years, and I was complimented that three9,12,16 of the 50 were articles described in this personal odyssey. At the end of a career, we all would like to think that we have contributed as much as we can to the well-being of our patients and to our colleagues by sharing our thoughts and experiences.
Verba volent, scripta manent. (Spoken words fly away, written words remain.)
PATIENT CONSENT
Patients provided written consent for the use of their images.
Footnotes
Disclosure: The author has no financial interest to declare in relation to the content of this article.
A “Hot Topic Video” by Editor-in-Chief Rod J. Rohrich, M.D., accompanies this article. Go to PRSJournal.com and click on “Plastic Surgery Hot Topics” in the “Videos” tab to watch. On the iPad, tap on the Hot Topics icon.
REFERENCES
- 1.Skoog T. Plastic Surgery: New Methods and Refinements. Philadelphia: Saunders; 1974. [Google Scholar]
- 2.Lemmon ML, Hamra ST. Skoog rhytidectomy: A five-year experience with 577 patients. Plast Reconstr Surg. 1980;65:283–297. [PubMed] [Google Scholar]
- 3.Mitz V, Peyronie M. The superficial musculo-aponeurotic system (SMAS) in the parotid and cheek area. Plast Reconstr Surg. 1976;58:80–88. doi: 10.1097/00006534-197607000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Hamra ST. The tri-plane face lift dissection. Ann Plast Surg. 1984;12:268–274. doi: 10.1097/00000637-198403000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Hamra ST. Deep plane facelift.. Paper presented at: American Society of Aesthetic Plastic Surgery Midwinter Symposium of Facial Rejuvenation; January 12–13, 1989; Santa Barbara, Calif. [Google Scholar]
- 6.Stuzin JM, Baker TJ, Gordon HL. The relationship of the superficial and deep facial fascias: Relevance to rhytidectomy and aging. Plast Reconstr Surg. 1992;89:441–449. discussion 450. [PubMed] [Google Scholar]
- 7.Owsley JQ. Lifting the malar fat pad for correction of prominent nasolabial folds. Plast Reconstr Surg. 1993;91:463–474. discussion 475. [PubMed] [Google Scholar]
- 8.Aston S. F.A.M.E. facelift Finger assisted malar elevation.. Paper presented at: Annual Meeting of the American Society for Plastic and Reconstructive Surgery; September 19–22, 1993; New Orleans, La. [Google Scholar]
- 9.Hamra ST. The deep-plane rhytidectomy. Plast Reconstr Surg. 1990;86(53) discussion 62–63. [PubMed] [Google Scholar]
- 10.Hamra ST. A study of the long term effect of malar fat repositioning in facelift surgery: Short term success but long term failure. Plas Reconstr Surg. 2002;110:940–950. doi: 10.1097/00006534-200209010-00035. discussion 952–959. [DOI] [PubMed] [Google Scholar]
- 11.Hamra ST. Composite Rhytidectomy. St. Louis: Quality Medical; 1993. [Google Scholar]
- 12.Hamra ST. Composite rhytidectomy. Plast Reconstr Surg. 1992;90:1–13. doi: 10.1097/00006534-199207000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Hamra ST. Repositioning the orbicularis oculi muscle in the composite rhytidectomy. Plast Reconstr Surg. 1992;90:14–22. doi: 10.1097/00006534-199207000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Bourget J. Les hernies graisseuses de l’orbite: Notre traitement chirurgical. Bull Acad Med (Paris) 1924;92:1270–1272. [Google Scholar]
- 15.Loeb R, editor. Aesthetic Surgery of the Eyelids. New York: Springer-Verlag; 1989. [Google Scholar]
- 16.Hamra ST. Arcus marginalis release and orbital fat preservation in midface rejuvenation. Plast Reconstr Surg. 1995;96:354–362. doi: 10.1097/00006534-199508000-00014. [DOI] [PubMed] [Google Scholar]
- 17.Hamra ST. The role of orbital fat preservation in facial aesthetic surgery: A new concept. Clin Plast Surg. 1996;23:17–28. [PubMed] [Google Scholar]
- 18.Hamra ST. The zygorbicular dissection in composite rhytidectomy: An ideal midface plane. Plast Reconstr Surg. 1998;102:1646–1657. doi: 10.1097/00006534-199810000-00051. [DOI] [PubMed] [Google Scholar]
- 19.Mendelson BC, Muzaffar AR, Adama WP. Surgical anatomy of the midcheek and malar mounds. Plast Reconstr Surg. 2002;110:885–896. doi: 10.1097/00006534-200209010-00026. discussion 897–911. [DOI] [PubMed] [Google Scholar]
- 20.Hamra ST. The role of the septal reset in creating a youthful eyelid-cheek complex in facial rejuvenation. Plast Recontstr Surg. 2004;113:2124–2141. doi: 10.1097/01.prs.0000122410.19952.e7. discussion 2142–2144. [DOI] [PubMed] [Google Scholar]
- 21.Barton FE, Jr, Ha R, Awada M. Fat extrusion and septal reset in patients with the tear trough triad: A critical appraisal. Plast Reconstr Surg. 2004;113:2115–2121. doi: 10.1097/01.prs.0000122409.00716.34. discussion 2122–2123. [DOI] [PubMed] [Google Scholar]
- 22.Hamra ST. Frequent face lift sequelae: Hollow eyes and the lateral sweep. Cause and repair. Plast Reconstr Surg. 1998;102:1658–1666. doi: 10.1097/00006534-199810000-00052. [DOI] [PubMed] [Google Scholar]
- 23.Joyce CW, Joyce KM, Kelly JC, Kelly JL, Carroll SM, Sugrue C. An analysis of the “classic” papers in aesthetic surgery. Aesthetic Plast Surg. 2015;39:8–16. doi: 10.1007/s00266-014-0414-3. [DOI] [PubMed] [Google Scholar]


