Abstract
Background and Purpose
Fatigue is common after stroke but has no effective treatments. Psychological interventions improve fatigue in other conditions by targeting psychological factors such as mood. If psychological factors correlate with fatigue in stroke, this would justify the development of similar interventions for poststroke fatigue (PSF). We used systematic review and meta-analysis to determine psychological associations of PSF.
Methods
We systematically searched for studies that reported psychological associations of PSF. We used odds ratios (ORs) to estimate the strength of associations and random-effects modeling to calculate summary estimates of ORs. We used stratified meta-analysis to investigate the impact of study design and conducted sensitivity analyses limited to studies that excluded patients with clinical depression and to studies that used depression scales without fatigue items.
Results
Thirty-five studies (n=9268) reported the association between PSF and ≥1 psychological factor. For PSF and depressive symptoms, we identified 19 studies (n=6712; pooled OR=4.14; 95% confidence interval, 2.73–6.27); this association existed in patients without clinical depression (pooled OR=1.39; 95% confidence interval, 1.27–1.53) and in studies using depression scales without fatigue items (pooled OR=5.41; 95% confidence interval, 1.54–18.93). For PSF and anxiety, we identified 4 studies (n=3884; pooled OR=2.34; 95% confidence interval, 0.98–5.58). Two studies (n=123) found an association with poor coping styles and 1 study (n=167) with loss of control. Six studies (n=1978) reported other emotional or behavioral associations.
Conclusions
PSF is associated with depressive symptoms, anxiety, poor coping, loss of control, emotional, and behavioral symptoms. These factors are potential targets for treatment of PSF. (Stroke. 2014;45:1778-1783.)
Keywords: behavior, fatigue, rehabilitation, stroke
Poststroke fatigue (PSF) is a distressing symptom that affects more than a third of stroke survivors.1 Currently, there is insufficient evidence to guide treatment.2 Psychological interventions improve fatigue in cancer, multiple sclerosis, and chronic fatigue syndrome by targeting thoughts, mood, and behavior. To determine whether to develop and test similar interventions for PSF, we need evidence about associations between PSF and those factors that could be targeted as part of a psychological intervention.
Although several narrative reviews have reported psychological factors associated with PSF,1,3–10 their results are conflicting, for example, 3 reviews concluded that PSF was associated with depression1,5,9 and 6 reported that PSF could occur independently of depression.3,4,6–8,10 Three reviews reported that PSF was associated with anxiety1,3,9 and 1 review reported no association.4 One review reported that fatigue was associated with lower expectations for self-efficacy in performing physical activity.11 Importantly, none of these reviews used meta-analysis to estimate the strength of associations. Thus, we need more evidence about the nature of the association between PSF and psychological factors, including, but not limited to, depressive symptoms, anxiety, sense of control, and coping styles.
This systematic review and meta-analysis aimed to determine whether PSF is associated with psychological factors that could be targets for a psychological intervention.
Methods
We systematically searched electronic databases (MEDLINE, EMBASE, CINAHL Plus, AMED, and PsycINFO) using key words stroke and fatigue and their synonyms adapted from a Cochrane review of interventions for PSF.2
One author (S.W.) screened all titles and abstracts on 2 separate occasions (to ensure that eligible studies were not missed) and obtained full texts of potentially eligible studies. S.W. read all full texts and 2 authors (G.M., A.B.) each read half of the full texts, independently of the first author. Any disagreement was discussed between authors. Reference lists of included articles and previous reviews were screened, and potentially relevant full texts were obtained.
We included observational studies reporting measures of both PSF and ≥1 psychological factor either as dichotomous variables (eg, the presence or absence of depressive symptoms) or as a continuous variable (eg, depression scales). For studies in which only qualitative data for the association were available, we included studies in the review but not in the meta-analysis. Studies were excluded if they (1) contained insufficient data to allow reporting of any association, (2) included any patients aged <18 years, (3) used unstructured assessment for PSF, or (4) provided data for patients with stroke that could not be disaggregated from other types of patients.
Two authors (S.W., A.B.) independently extracted data on demographics, presence of prestroke fatigue, how PSF and psychological factors were assessed, whether patients with a clinical diagnosis of depression were included or excluded, and statistics for associations. They independently applied the Strengthening the Reporting of Observational Studies in Epidemiology checklist12 to assess study quality.
Statistical Analysis
For each study in which raw data were provided, odds ratios (ORs) and 95% confidence intervals (95% CIs) were calculated for associations between PSF and each psychological factor. ORs reported by study authors were accepted if raw data were unavailable. If studies reported only correlation coefficient, we used established methods to convert to ORs.13 If ORs could not be obtained by these methods, we summarized these studies qualitatively not quantitatively. Publication bias was assessed by funnel plotting.13
For associations of PSF with depressive symptoms and with anxiety, we determined summary estimates of ORs using random-effects modeling.14 Between-study heterogeneity was assessed using the Cochran Q statistic,13 in which P<0.05 implies significant heterogeneity. We had intended to perform meta-analysis for psychological associations other than mood, but this was not possible because these studies only reported regression coefficients and P values for the associations.
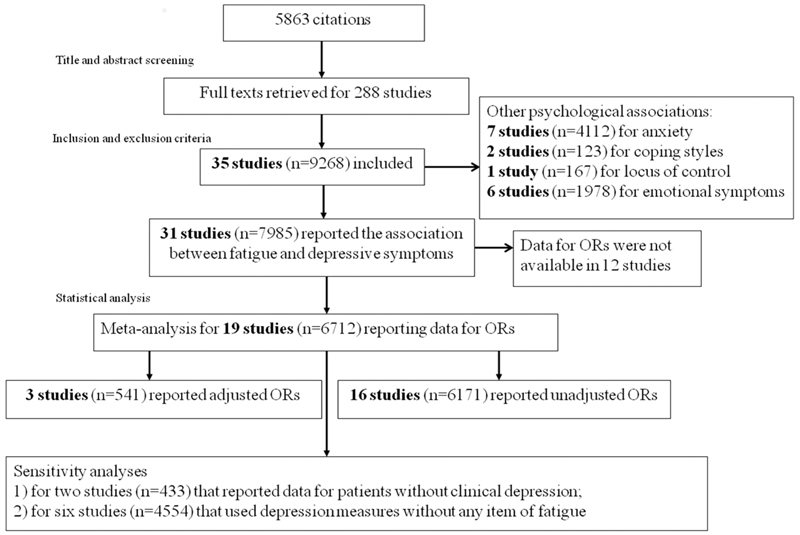
We used partitioning of heterogeneity13 to compare studies that reported adjusted ORs with those that reported unadjusted ORs. For the association with depressive symptoms, only 3 studies reported adjusted ORs by controlling for potential confounders (age, sex, lesion site, and dependence in daily life) for PSF in multiple logistic regression, whereas the remaining 16 studies reported unadjusted ORs (Figure 1). We conducted sensitivity analyses (1) for studies that had excluded people with a clinical diagnosis of depression and (2) by excluding studies that had used a depression measure that contained an item of fatigue.
Figure 1.
Electronic search, study selection, and data analysis. ORs indicates odds ratios.
Results
A total of 5863 citations were identified, and 288 full texts were retrieved. Three studies (2 conference abstracts and 1 not published in English)15–17 were excluded because they contained insufficient data for analysis and study authors did not provide further data on our request. Thirty-five studies fulfilled inclusion criteria (Figure 1).
Mean age of patients ranged from 5118 to 75 years.19 The proportion of women ranged from 19%18 to 67%.20 Five studies recruited patients with ischemic stroke,21–25 2 with subarachnoid hemorrhage,26,27 18 studies included both ischemic and hemorrhagic stroke,18–20,28–42 and the other 10 studies did not specify stroke type.43–52
The median number of Strengthening the Reporting of Observational Studies in Epidemiology checklist items scored (out of 22) was 19 (interquartile range, 18–20). No study provided sample size calculations. Other common weaknesses included not describing details of recruitment, not addressing potential bias, or not declaring sources of funding.
Depressive Symptoms
Overall Meta-Analysis
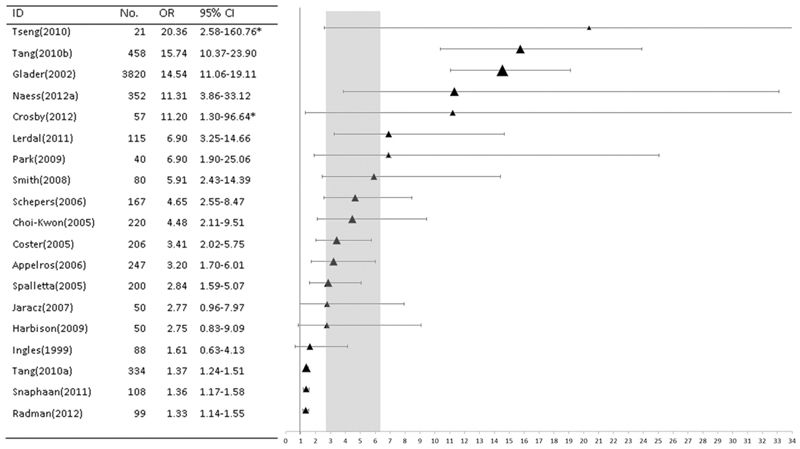
Of 31 studies that provided data on the association between PSF and depressive symptoms, ORs could be obtained, and used in meta-analysis, from 19 studies; from these we calculated ORs from raw data of 7 studies,20,36,37,39,43,44,49 extracted ORs from 4 studies,19,23,24,33 and converted ORs from correlation coefficients from 8 studies.22,25,30,32,34,45,47,48 Summary estimate of OR was 4.14 (95% CI, 2.73–6.27; Figure 2), with no significant between-study heterogeneity (Q=15.58; df=18; P=0.62).
Figure 2.
Random-effects meta-analysis for the association between poststroke fatigue and depressive symptoms. The horizontal axis is the odds ratio (OR) comparing the occurrence of depressive symptoms in patients with and without fatigue after stroke. Horizontal error bars represent the 95% confidence interval (CI) of OR in individual studies, and vertical gray bar represents the 95% CI of the summary estimate of OR. Symbol size represents the log of the number of participants in that study. *The upper limit of the 95% CI of OR beyond 34 did not show in the plot.
Stratified Meta-Analysis
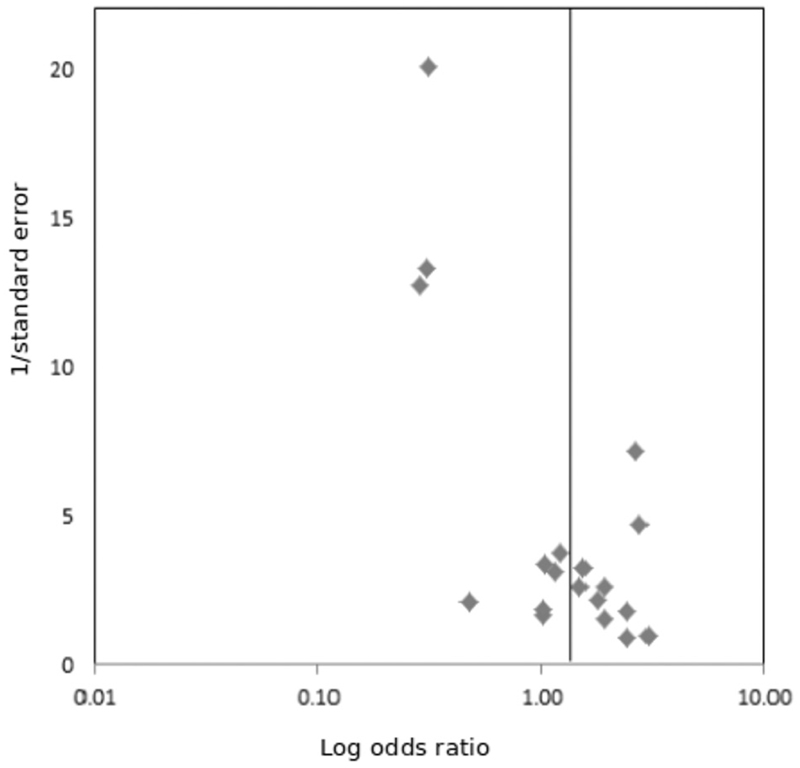
The use of adjusted ORs or unadjusted ORs explained a significant portion of heterogeneity between studies (Q=4.91; df=1; P=0.03). The strength of the association in 16 studies of unadjusted ORs (n=6171; pooled OR=5.46; 95% CI, 3.58–8.32) was higher (P<0.01) than the association in 3 studies in which ORs were adjusted (541 patients; pooled OR=1.36; 95% CI, 1.26–1.46). This heterogeneity might have contributed to an asymmetrical funnel plot (Figure 3) because the 3 studies reporting adjusted ORs were located in the upper left-hand corner of the plot away from the other 16 studies.
Figure 3.
Funnel plot for publication bias. The horizontal axis represents the log odds ratios (ORs) for the association between poststroke fatigue and depressive symptoms, and the vertical axis represents the inverse SE. The vertical bar represents the pooled estimate of ORs.
Sensitivity Analyses
Of the 19 studies included in meta-analysis, one study (n=334) excluded patients with major depression at recruitment24 and another study (n=99) provided data for patients without depression33; pooled estimate of these 2 adjusted ORs was 1.39 (95% CI, 1.27–1.53, which was not statistically different from the summary estimate of all 3 adjusted ORs; P=0.91). The other 17 studies did not specify whether they had distinguished patients with current clinical depression.
Thirteen studies assessed depression using a measure that contained a single item for fatigue,19,22,24,25,30,32–34,36,43,45,48,49 and 2 of them also assessed fatigue using this fatigue item of the depression measure.22,49 For the remaining 6 studies (n=4554) that used depression measures without any fatigue item, the pooled OR was 5.41 (95% CI, 1.54–18.93), which was not significantly different from either the summary estimate for the other 13 studies (pooled OR=3.45; 95% CI, 1.82–6.57; P=0.53) or from that of the total 19 studies (pooled OR=4.14; 95% CI, 2.73–6.27; P=0.84).
Qualitative Analysis
Twelve studies did not report sufficient data to be included in meta-analysis. Nine studies (n=1043) reported an association between PSF and depression,18,21,28,31,38,41,42,51,52 whereas one study (n=32) reported no significant difference in depression scores between fatigued and nonfatigued groups35; another study (n=100) reported that depressive symptoms were associated with mental fatigue but not with other fatigue domains50; and one further study (n=88) used 2 measures for PSF and 2 measures for depression, but reported 4 conflicting results of the association.29
Anxiety
Seven studies reported the association between PSF and anxiety,23,29,31,33,39,44,52 and data from 4 studies (n=3934)23,33,39,44 could be included in meta-analysis. The summary estimate of the OR was 2.34 (95% CI, 0.98–5.58) with no significant between-study heterogeneity (Q=2.36; df=3; P=0.50). Stratified meta-analysis indicated that the strength of association between PSF and anxiety in 2 studies23,33 not controlling the effect of depression (n=217; pooled OR=5.34; 95% CI, 4.70–6.07) was higher (P<0.01) than that in the other 2 studies39,44 having controlled the effect of depression (n=3717; pooled OR=1.25; 95% CI, 1.14–1.38).
Of the 3 studies that provided insufficient data to be included in the meta-analysis, 2 (n=90) reported a significant association between fatigue and anxiety,31,52 whereas 1 (n=88) excluded patients with depression at recruitment and found a nonsignificant association between PSF and anxiety.29
Sense of Control and Coping Styles
One study (n=167) reported that patients who were not confident in their own ability to control their health had more severe fatigue (P=0.002).47 Associations between PSF and coping styles were investigated by 2 studies. One (n=50) reported that patients focusing on personal emotions and self-blame were more likely to have a higher level of PSF (P<0.01).30 Another study (n=73) found that maladaptive coping (eg, denial and self-distraction) was the main cause of post-traumatic stress disorder (P<0.0001), and the latter was associated with PSF (P<0.0001).27
Other Psychological Factors
Six studies reported other psychological associations of PSF. Three studies (n=1527) assessed mental health and emotional role by Short Form-36, and all reported that poor outcomes of mental or emotional subscales were associated with PSF.25,40,46 Such an association was also reported by another study (n=141) using the emotional subscale of stroke-specific quality of life.26 PSF was also associated with inappropriate laughing (1 study, n=220)43 and alertness behavior (measured by Sickness Impact Scale in 1 study, n=90).51
Discussion
This is, to our knowledge, the first meta-analysis to report associations between PSF and mood or other psychological factors. We found a statistically significant association between PSF and depressive symptoms and a trend toward an association between PSF and anxiety. Two studies reported associations with inadequate coping styles, 1 study with loss of control, and 6 studies with emotional or behavioral symptoms. The named psychological factors, that is, depressive symptoms, anxiety, locus of control and coping, have already been targeted by psychological interventions for fatigue in other conditions such as cancer and multiple sclerosis. This review provides the necessary evidence to justify the development of a similar intervention for fatigue in stroke survivors. However, our findings should be interpreted with caution because only a small number of studies investigated each factor except for depressive symptoms. Also, there are some weaknesses in the quality of the included studies in that most of them did not report how patients were recruited and how study size was achieved; thus, it is difficult to determine whether the sample is representative of the entire stroke population.
PSF is associated with depressive symptoms, even in patients not meeting clinical criteria for depression. A previous study reported the presence of depressive symptoms in patients with stroke without clinical depression, where 41% of the patients reported depressed mood but only half of them met clinical criteria for depression.53 This suggests that clinicians should be aware of depressive symptoms in patients with stroke and screen for them in patients with PSF, even in those without a clinical depression. We also noticed that some of the included studies had measured depression by using scales or criteria that contain a single item of fatigue. We therefore performed a sensitivity analysis to determine whether this might result in an overestimation of the strength of association between fatigue and depression. The result indicated that this association remained significant even after excluding studies that had used a depression measure containing a fatigue item. In fact, in these depression measures, fatigue only contributes a small proportion to the total score of depression (from 1/9 to 1/66). Thus, the association that we identified was not because of the overlap between fatigue and depression measures.
In some of the included studies, age, sex, lesion site, and dependence in daily life were considered as confounders for the association between PSF and depressive symptoms. Based on the current data, however, we could not analyze the effect of each individual factor on the association. Previous studies reported that age and sex are associated with fatigue40 but not with depression.54 There is insufficient evidence for the association between lesion site and either fatigue55 or depression.56 The association between PSF and dependence has been widely reported in the studies included in this review. Dependence was also reported to be associated with poststroke depression.57 Future research is expected to investigate the effect of these confounders.
There is a trend toward an association between PSF and anxiety, but the association was weaker after controlling the effect of depressive symptoms. One study (included in our systematic review but not in meta-analysis) that had excluded patients with depression reported no significant association between PSF and anxiety.29 It is reported that anxiety is strongly correlated with depression after stroke.58 To better clarify whether depressive symptoms are confounders, the association between PSF and anxiety needs to be compared between patients with stroke with and without depressive symptoms.
Our study has several strengths. It is the first systematic review to pool the results from studies that reported the associations between PSF and depressive symptoms or anxiety. We performed a comprehensive search, had a prespecified protocol, and used a well-established statistical approach. We also used a funnel plot to detect publication bias, in which the asymmetrical plot might indicate certain publication bias caused by the missing studies in the bottom left-hand corner of the plot. These studies are likely to be of small sample size and reported less significant results. A possible source for this publication bias might be the exclusion of conference abstracts and studies not published in English, although we have attempted to obtain further data by contacting the study authors but did not get a reply. One limitation of our study is that only 1 author read all the abstracts to identify potentially eligible studies. However, this was done on 2 separate occasions to reduce the possibility of missing any relevant studies.
Conclusions
This review provides robust evidence for the association between PSF and depressive symptoms. This implies the screening and treatment of PSF in patients with stroke needs to integrate strategies targeting mood. PSF is also associated, either directly or indirectly, with anxiety, loss of control, poor coping styles, emotional, and behavioral symptoms; these factors are potential targets for treatment of PSF.
Sources of Funding
S. Wu was funded by the China Scholarship Council/University of Edinburgh Joint Scholarship. A. Barugh was supported by the Dunhill Medical Trust (grant No. RTF17/0111).
Footnotes
Disclosures
None.
References
- 1.Lerdal A, Bakken LN, Kouwenhoven SE, Pedersen G, Kirkevold M, Finset A, et al. Poststroke fatigue–a review. J Pain Symptom Manage. 2009;38:928–949. doi: 10.1016/j.jpainsymman.2009.04.028. [DOI] [PubMed] [Google Scholar]
- 2.McGeough E, Pollock A, Smith LN, Dennis M, Sharpe M, Lewis S, et al. Interventions for post-stroke fatigue. Cochrane Database Syst Rev. 2009:CD007030. doi: 10.1002/14651858.CD007030.pub2. [DOI] [PubMed] [Google Scholar]
- 3.Annoni JM, Staub F, Bogousslavsky J, Brioschi A. Frequency, characterisation and therapies of fatigue after stroke. Neurol Sci. 2008;29(suppl 2):S244–S246. doi: 10.1007/s10072-008-0951-0. [DOI] [PubMed] [Google Scholar]
- 4.Barker-Collo S, Feigin VL, Dudley M. Post stroke fatigue–where is the evidence to guide practice? N Z Med J. 2007;120:U2780. [PubMed] [Google Scholar]
- 5.Barritt AW, Smithard DG. Targeting fatigue in stroke patients. ISRN Neurol. 2011;2011:805646. doi: 10.5402/2011/805646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choi-Kwon S, Kim JS. Poststroke fatigue: an emerging, critical issue in stroke medicine. Int J Stroke. 2011;6:328–336. doi: 10.1111/j.1747-4949.2011.00624.x. [DOI] [PubMed] [Google Scholar]
- 7.Colle F, Bonan I, Gellez Leman MC, Bradai N, Yelnik A. Fatigue after stroke. Ann Readapt Med Phys. 2006;49:361–364. doi: 10.1016/j.annrmp.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 8.De Groot MH, Phillips SJ, Eskes GA. Fatigue associated with stroke and other neurologic conditions: implications for stroke rehabilitation. Arch Phys Med Rehabil. 2003;84:1714–1720. doi: 10.1053/s0003-9993(03)00346-0. [DOI] [PubMed] [Google Scholar]
- 9.Duncan F, Wu S, Mead GE. Frequency and natural history of fatigue after stroke: a systematic review of longitudinal studies. J Psychosom Res. 2012;73:18–27. doi: 10.1016/j.jpsychores.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 10.Staub F, Bogousslavsky J. Fatigue after stroke: a major but neglected issue. Cerebrovasc Dis. 2001;12:75–81. doi: 10.1159/000047685. [DOI] [PubMed] [Google Scholar]
- 11.Duncan F, Kutlubaev MA, Dennis MS, Greig C, Mead GE. Fatigue after stroke: a systematic review of associations with impaired physical fitness. Int J Stroke. 2012;7:157–162. doi: 10.1111/j.1747-4949.2011.00741.x. [DOI] [PubMed] [Google Scholar]
- 12.Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med. 2007;4:e297. doi: 10.1371/journal.pmed.0040297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Borenstein M, Hedges LV, Higgins JP, Rothstein HR. Introduction to Meta-Analysis. 1st ed. West Sussex, England: Wiley; 2009. pp. 45–50.pp. 107–112.pp. 277–293. [Google Scholar]
- 14.Hedges LV, Vevea JL. Fixed- and random-effects models in meta-analysis. Psychol Methods. 1998;3:486–504. [Google Scholar]
- 15.Fourtassi M, Wajszczak I, Riffo P, Jacquin-Courtois S, Luaute J, Rode G. Post-stroke fatigue. Ann Phys Rehab Med. 2011;54:e242–e243. Conference Abstract. [Google Scholar]
- 16.Rossi C, Cordonnier C, Popescu V, Dequatre N, Leys D, Henon H. Prevalence and determinants of fatigue 1 year after spontaneous intracerebral haemorrhage. Eur J Neurol. 2011;8:52. Conference Abstract. [Google Scholar]
- 17.Soyuer F, Unalan D, Ozturk A. Fatigue in stroke patients [Turkish] Turk Serebrovaskuler Hastaliklar Dergisi. 2008;14:73–77. [Google Scholar]
- 18.Hubacher M, Calabrese P, Bassetti C, Carota A, Stöcklin M, Penner IK. Assessment of post-stroke fatigue: the fatigue scale for motor and cognitive functions. Eur Neurol. 2012;67:377–384. doi: 10.1159/000336736. [DOI] [PubMed] [Google Scholar]
- 19.Appelros P. Prevalence and predictors of pain and fatigue after stroke: a population-based study. Int J Rehabil Res. 2006;29:329–333. doi: 10.1097/MRR.0b013e328010c7b8. [DOI] [PubMed] [Google Scholar]
- 20.Crosby GA, Munshi S, Karat AS, Worthington E, Lincoln NB. Fatigue after stroke: frequency and effect on daily life. Disabil Rehabil. 2012;34:633–637. doi: 10.3109/09638288.2011.613517. [DOI] [PubMed] [Google Scholar]
- 21.Parks NE, Eskes GA, Gubitz GJ, Reidy Y, Christian C, Phillips SJ. Fatigue impact scale demonstrates greater fatigue in younger stroke survivors. Can J Neurol Sci. 2012;39:619–625. doi: 10.1017/s0317167100015353. [DOI] [PubMed] [Google Scholar]
- 22.de Coster L, Leentjens AF, Lodder J, Verhey FR. The sensitivity of somatic symptoms in post-stroke depression: a discriminant analytic approach. Int J Geriatr Psychiatry. 2005;20:358–362. doi: 10.1002/gps.1290. [DOI] [PubMed] [Google Scholar]
- 23.Snaphaan L, van der Werf S, de Leeuw FE. Time course and risk factors of post-stroke fatigue: a prospective cohort study. Eur J Neurol. 2011;18:611–617. doi: 10.1111/j.1468-1331.2010.03217.x. [DOI] [PubMed] [Google Scholar]
- 24.Tang WK, Chen YK, Mok V, Chu WC, Ungvari GS, Ahuja AT, et al. Acute basal ganglia infarcts in poststroke fatigue: an MRI study. J Neurol. 2010;257:178–182. doi: 10.1007/s00415-009-5284-2. [DOI] [PubMed] [Google Scholar]
- 25.Tang WK, Lu JY, Chen YK, Mok VC, Ungvari GS, Wong KS. Is fatigue associated with short-term health-related quality of life in stroke? Arch Phys Med Rehabil. 2010;91:1511–1515. doi: 10.1016/j.apmr.2010.06.026. [DOI] [PubMed] [Google Scholar]
- 26.Visser-Meily JM, Rhebergen ML, Rinkel GJ, van Zandvoort MJ, Post MW. Long-term health-related quality of life after aneurysmal subarachnoid hemorrhage: relationship with psychological symptoms and personality characteristics. Stroke. 2009;40:1526–1529. doi: 10.1161/STROKEAHA.108.531277. [DOI] [PubMed] [Google Scholar]
- 27.Noble AJ, Baisch S, Schenk T, Mendelow AD, Allen L, Kane P. Posttraumatic stress disorder explains reduced quality of life in subarachnoid hemorrhage patients in both the short and long term. Neurosurgery. 2008;63:1095–1105. doi: 10.1227/01.NEU.0000327580.91345.78. [DOI] [PubMed] [Google Scholar]
- 28.van de Port IGL, Kwakkel G, Schepers VPM, Heinemans CTI, Lindeman E. Is fatigue an independent factor associated with activities of daily living, instrumental activities of daily living and health-related quality of life in chronic stroke? Cerebrovasc Dis. 2007;23:40–45. doi: 10.1159/000095757. [DOI] [PubMed] [Google Scholar]
- 29.Zedlitz AMEE, Visser-Meily JMA, Schepers VP, Guerts ACH, Fasotti L. Patients with severe poststroke fatigue show a psychosocial profile comparable to patients with other chronic disease: Implications for diagnosis and treatment. ISRN Neurol. 2011;2011:1–8. doi: 10.5402/2011/627081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jaracz K, Mielcarek L, Kozubski W. Clinical and psychological correlates of poststroke fatigue. Preliminary results. Neurol Neurochir Pol. 2007;41:36–43. [PubMed] [Google Scholar]
- 31.Lynch J, Mead G, Greig C, Young A, Lewis S, Sharpe M. Fatigue after stroke: the development and evaluation of a case definition. J Psychosom Res. 2007;63:539–544. doi: 10.1016/j.jpsychores.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 32.Park JY, Chun MH, Kang SH, Lee JA, Kim BR, Shin MJ. Functional outcome in poststroke patients with or without fatigue. Am J Phys Med Rehabil. 2009;88:554–558. doi: 10.1097/PHM.0b013e3181a0dae0. [DOI] [PubMed] [Google Scholar]
- 33.Radman N, Staub F, Aboulafia-Brakha T, Berney A, Bogousslavsky J, Annoni JM. Poststroke fatigue following minor infarcts: a prospective study. Neurology. 2012;79:1422–1427. doi: 10.1212/WNL.0b013e31826d5f3a. [DOI] [PubMed] [Google Scholar]
- 34.Tseng BY, Billinger SA, Gajewski BJ, Kluding PM. Exertion fatigue and chronic fatigue are two distinct constructs in people post-stroke. Stroke. 2010;41:2908–2912. doi: 10.1161/STROKEAHA.110.596064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hoang CL, Salle JY, Mandigout S, Hamonet J, Macian-Montoro F, Daviet JC. Physical factors associated with fatigue after stroke: an exploratory study. Top Stroke Rehabil. 2012;19:369–376. doi: 10.1310/tsr1905-369. [DOI] [PubMed] [Google Scholar]
- 36.Ingles JL, Eskes GA, Phillips SJ. Fatigue after stroke. Arch Phys Med Rehabil. 1999;80:173–178. doi: 10.1016/s0003-9993(99)90116-8. [DOI] [PubMed] [Google Scholar]
- 37.Naess H, Lunde L, Brogger J, Waje-Andreassen U. Fatigue among stroke patients on long-term follow-up. The Bergen Stroke Study. J Neurol Sci. 2012;312:138–141. doi: 10.1016/j.jns.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 38.Almborg AH, Ulander K, Thulin A, Berg S. Discharged after stroke - important factors for health-related quality of life. J Clin Nurs. 2010;19:2196–2206. doi: 10.1111/j.1365-2702.2010.03251.x. [DOI] [PubMed] [Google Scholar]
- 39.Glader EL, Stegmayr B, Asplund K. Poststroke fatigue: a 2-year follow-up study of stroke patients in Sweden. Stroke. 2002;33:1327–1333. doi: 10.1161/01.str.0000014248.28711.d6. [DOI] [PubMed] [Google Scholar]
- 40.Mead GE, Graham C, Dorman P, Bruins SK, Lewis SC, Dennis MS, et al. UK Collaborators of IST. Fatigue after stroke: baseline predictors and influence on survival. Analysis of data from UK patients recruited in the International Stroke Trial. PLoS One. 2011;6:e16988. doi: 10.1371/journal.pone.0016988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Skånér Y, Nilsson GH, Sundquist K, Hassler E, Krakau I. Self-rated health, symptoms of depression and general symptoms at 3 and 12 months after a first-ever stroke: a municipality-based study in Sweden. BMC Fam Pract. 2007;8:61. doi: 10.1186/1471-2296-8-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sibon I, Lassalle-Lagadec S, Renou P, Swendsen J. Evolution of depression symptoms following stroke: a prospective study using computerized ambulatory monitoring. Cerebrovasc Dis. 2012;33:280–285. doi: 10.1159/000334663. [DOI] [PubMed] [Google Scholar]
- 43.Choi-Kwon S, Han SW, Kwon SU, Kim JS. Poststroke fatigue: characteristics and related factors. Cerebrovasc Dis. 2005;19:84–90. doi: 10.1159/000082784. [DOI] [PubMed] [Google Scholar]
- 44.Harbison JA, Walsh S, Kenny RA. Hypertension and daytime hypotension found on ambulatory blood pressure is associated with fatigue following stroke and TIA. QJM. 2009;102:109–115. doi: 10.1093/qjmed/hcn146. [DOI] [PubMed] [Google Scholar]
- 45.Lerdal A, Bakken LN, Rasmussen EF, Beiermann C, Ryen S, Pynten S, et al. Physical impairment, depressive symptoms and pre-stroke fatigue are related to fatigue in the acute phase after stroke. Disabil Rehabil. 2011;33:334–342. doi: 10.3109/09638288.2010.490867. [DOI] [PubMed] [Google Scholar]
- 46.Lewis SJ, Barugh AJ, Greig CA, Saunders DH, Fitzsimons C, Dinan-Young S, et al. Is fatigue after stroke associated with physical deconditioning? A cross-sectional study in ambulatory stroke survivors. Arch Phys Med Rehabil. 2011;92:295–298. doi: 10.1016/j.apmr.2010.10.030. [DOI] [PubMed] [Google Scholar]
- 47.Schepers VP, Visser-Meily AM, Ketelaar M, Lindeman E. Poststroke fatigue: course and its relation to personal and stroke-related factors. Arch Phys Med Rehabil. 2006;87:184–188. doi: 10.1016/j.apmr.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 48.Smith OR, van den Broek KC, Renkens M, Denollet J. Comparison of fatigue levels in patients with stroke and patients with end-stage heart failure: application of the fatigue assessment scale. J Am Geriatr Soc. 2008;56:1915–1919. doi: 10.1111/j.1532-5415.2008.01925.x. [DOI] [PubMed] [Google Scholar]
- 49.Spalletta G, Ripa A, Caltagirone C. Symptom profile of DSM-IV major and minor depressive disorders in first-ever stroke patients. Am J Geriatr Psychiatry. 2005;13:108–115. doi: 10.1176/appi.ajgp.13.2.108. [DOI] [PubMed] [Google Scholar]
- 50.Stokes EK, O’Connell C, Murphy B. An investigation into fatigue post-stroke and its multidimensional nature. Adv Physiother. 2011;13:2–10. [Google Scholar]
- 51.van der Werf SP, van den Broek HL, Anten HW, Bleijenberg G. Experience of severe fatigue long after stroke and its relation to depressive symptoms and disease characteristics. Eur Neurol. 2001;45:28–33. doi: 10.1159/000052085. [DOI] [PubMed] [Google Scholar]
- 52.Vuletić V, Lezaić Z, Morović S. Post-stroke fatigue. Acta Clin Croat. 2011;50:341–344. [PubMed] [Google Scholar]
- 53.Fedoroff JP, Starkstein SE, Parikh RM, Price TR, Robinson RG. Are depressive symptoms nonspecific in patients with acute stroke? Am J Psychiatry. 1991;148:1172–1176. doi: 10.1176/ajp.148.9.1172. [DOI] [PubMed] [Google Scholar]
- 54.Allan LM, Rowan EN, Thomas AJ, Polvikoski TM, O’Brien JT, Kalaria RN. Long-term incidence of depression and predictors of depressive symptoms in older stroke survivors. Br J Psychiatry. 2013;203:453–460. doi: 10.1192/bjp.bp.113.128355. [DOI] [PubMed] [Google Scholar]
- 55.Kutlubaev MA, Duncan FH, Mead GE. Biological correlates of post-stroke fatigue: a systematic review. Acta Neurol Scand. 2012;125:219–227. doi: 10.1111/j.1600-0404.2011.01618.x. [DOI] [PubMed] [Google Scholar]
- 56.Carson AJ, MacHale S, Allen K, Lawrie SM, Dennis M, House A, et al. Depression after stroke and lesion location: a systematic review. Lancet. 2000;356:122–126. doi: 10.1016/S0140-6736(00)02448-X. [DOI] [PubMed] [Google Scholar]
- 57.Hackett ML, Anderson CS. Predictors of depression after stroke: a systematic review of observational studies. Stroke. 2005;36:2296–2301. doi: 10.1161/01.STR.0000183622.75135.a4. [DOI] [PubMed] [Google Scholar]
- 58.Barker-Collo SL. Depression and anxiety 3 months post stroke: prevalence and correlates. Arch Clin Neuropsychol. 2007;22:519–531. doi: 10.1016/j.acn.2007.03.002. [DOI] [PubMed] [Google Scholar]