Abstract
Introduction
Basic health care is beyond the reach of many families, partly due to lack of health insurance. Many of those with insurance also experience unmet need and limited access. In this study, low-income parents illuminate barriers to obtaining health care services for their children.
Methods
We surveyed a random sample of families from Oregon’s food stamp population with children eligible for public insurance, based on household income. Mixed-methods included: (1) multivariable analysis of data from 2,681 completed surveys, and (2) qualitative study of written narratives from 722 parents.
Results
Lack of health insurance was the most consistent predictor of unmet health care needs in the quantitative analysis. Qualitatively, health insurance instability, lack of access to services despite having insurance, and unaffordable costs were major concerns.
Conclusions
Parents in this low-income population view insurance coverage as different from access to services, and reported a hierarchy of needs. Insurance was the primary concern; access and costs were secondary.
Keywords: Insurance coverage, access to health care, primary health care, Medicaid, children’s health, underserved populations
Ideally, all children in the United States would have stable access to high-quality health care, but many barriers make this goal presently unattainable. These barriers have been described as voltage drops, or resistance points, where children drop from the health care system like voltage from an electrical current.1 There is a wealth of information describing the multitude of barriers for low-income children, who often experience several barriers simultaneously1–6 but a clear hierarchical framework to define the relative importance of each barrier is lacking.
Uninsurance, known to inhibit access to care,7–11 significantly affects U.S. children: among the nearly 47 million uninsured Americans, over 9 million are uninsured children.12,13 A majority of these uninsured children qualify for publicly-funded insurance programs, such as Medicaid and the State Children’s Health Insurance Programs (SCHIP), but have either lost coverage or become disenrolled due to various barriers.13–16 Oregon has a high rate of uninsured children,13,17 and over 60% of uninsured Oregon children appeared to be eligible for some form of public coverage in 2004—a higher percentage than is estimated for uninsured children nationally.11,18 As struggles to reauthorize SCHIP continue,19–22 Oregon and several other states are focused on enrolling uninsured but eligible low-income children.
In this context, it is important to step back and examine the role that insurance plays in helping low-income children obtain necessary health care and to consider how it compares with other factors affecting access. Past research has concluded that most low-income parents are familiar with Medicaid and SCHIP, but restrictive regulations and confusing organizational structures keep public health insurance out of reach for some low-income families and contribute to coverage instabilities for others.14,17,23–41 Less is known about how parents feel about public insurance offerings and whether they believe that getting and maintaining coverage is worth the effort required. Despite the wealth of evidence linking insurance to better health care outcomes, how much does health insurance matter to poor families? Also, beyond health insurance coverage, what factors do low-income parents identify as major influences on whether their children’s health care needs are met or not?
Most previous studies of factors influencing children’s health care access have focused on patterns of insurance enrollment and service utilization.14,17,40,42,43 Study methods often include the use of administrative data, claims data, secondary analysis of national surveys, and key informant interviews, all of which are several steps removed from the actual life experiences of poor and underserved families. We collected information directly from low-income parents about the importance of health insurance and other possible factors affecting access to health care for their children. This study was part of a larger effort, the Oregon Children’s Access to Health Care Survey (CAHS), which was launched in 2005, shortly affer Medicaid reforms. In the early 1990s, the Oregon Health Plan (OHP) was a national model for innovative Medicaid program expansions that facilitated more comprehensive insurance coverage for entire families.44 As happened in many states, a fiscal crisis in Oregon at the turn of the century led to the implementation of cost containment policies for the OHP starting in 2003, including benefit reductions and increased premiums.45 These changes have been associated with the loss of insurance for thousands of adults in Oregon’s low-income families.46–48
Although Oregon’s cutbacks were targeted at adults, children may have been indirectly affected. The CAHS collected cross-sectional, statewide data from low-income families in Oregon’s food stamp population to assess the potential impacts of Medicaid policy changes on children. For this paper, we conducted a quantitative analysis of factors associated with children’s unmet health care needs from all survey respondents and a qualitative analysis of written comments from responses to a concluding open-ended survey question that asked, “Is there anything else you would like to tell us?” With this mixed-methods approach, we had two primary aims: (1) to examine, both quantitatively and qualitatively, whether parents from this low-income population believed health insurance coverage for their children was important; and (2) to learn more from parents about factors that affect their efforts to obtain necessary care for their children.
Methods
Study population and data collection
To identify a large group of families with children who were likely eligible for public insurance coverage, the study sample was drawn from all 84,087 Oregon families enrolled in the federal food stamp program at the end of January 2005 with children between the ages of 1 and 18 years of age. At that time, both the public insurance and food stamp programs required a household income less than 185% of the federal poverty level and proof of the child’s U.S. citizenship. (Families with only children under one year of age were excluded due to different public insurance enrollment procedures for these infants.) A stratified, random sample of 10,175 food stamp families was drawn with purposeful oversampling to ensure adequate representation from rural areas and uninsured families. A focal child was then randomly selected from each household, and parents were clearly instructed to answer survey questions about only this child. After four-waves of mailing from March–May 2005, we excluded 1,539 families who had moved out of state or to another location with no forwarding address information available. Completed surveys were received from 2,681 of the 8,636 eligible households in the random sample (for a 31% response rate). This response rate is consistent with other similar surveys of Medicaid-eligible populations.3,48,49
Data from the 2,681 completed surveys were used in the quantitative analysis. The additional written comments from 722 parents were used in the qualitative analysis. Demographic characteristics of the original sample were similar to those responding to the survey and those contributing additional written narratives. (Data available from lead author upon request.) For the quantitative analysis, we assigned individual response weights depending on the probability of original selection into the random sample. To account for non-response, final weights assigned to each respondent case were further adjusted using a raking ratio estimation process.50,51 All reported quantitative results have been weighted back to the overall study population of 84,087 households, unless otherwise described. (More information about the raking ratio estimation process available from the lead author upon request.)
Survey instrument
The Oregon Children’s Access to Health Care Survey was developed to allow parents to report about various health-related issues for one randomly-selected focal child during the previous year. Survey questions were grouped into four major sections: child’s health insurance status, child’s access to various health care services, child’s demographic information, and family information (primarily demographics and parental insurance information, collected only from the parent/guardian who completed the survey). Most survey questions were adapted from widely accepted and validated national surveys.52–55 Written at a fifth grade reading level, the mail-return survey instrument contained 62 questions with multiple-choice response options and a final open-ended question: “Is there anything else you would like to tell us?” For validity testing of the self-administered instrument, cognitive interviews were conducted during a pilot test phase with a small sample of low-income parents. Surveys were translated into Spanish and Russian (the two most common non-English languages among this population) and then independently back-translated to ensure fidelity of translation. The Oregon Health & Science University Institutional Review Board approved the survey and all aspects of the study protocol (OHSU eIRB# 1717).
Quantitative analysis
The quantitative analysis used a standard bivariate and multivariate analytical approach. Five outcome variables were measured pertaining to access that measured unmet health care needs (medical, prescription and dental), delayed urgent care, and ambulatory care visits (see Appendix for details on these variables). In addition to children’s health insurance status as the main predictor variable, chi-square bivariate analyses facilitated the identification of several other independent variables significantly associated with at least one of the outcome variables among the low-income study population (p<.05). These covariates included age, race/ethnicity, parental employment, household income, parental insurance status, place of residence, and whether or not the child had a usual source of care. Because Oregon’s predominant minority population is Hispanic and a large number of Hispanics in the sample reported Hispanic as their race, we created a combination race/ethnicity covariate (White, non-Hispanic; Hispanic, any race; non-White, non-Hispanic). Rural residence was determined based on ZIP code designations from the Oregon Office of Rural Health. These covariates are consistent with conceptual models of health services utilization described previously by Aday, Andersen, and others.56 No significant (p<.05) interactions between the primary children’s health insurance predictor variable and the other covariates were noted.
After selection of all significant variables, we applied a series of logistic regression models to assess independent associations between each predictor variable and each outcome variable, while controlling for all other potentially confounding factors. SPSS 14.0 software with the complex samples module was used to conduct statistical tests and make estimates with variance adjustment required for the complex sampling design of the survey (SPSS 14.0 for Windows, Chicago: SPSS Inc.).
Qualitative analysis
The qualitative analysis team included a diverse group of health services researchers including a family physician, a doctorally-prepared quantitative and qualitative senior researcher, a medical student jointly enrolled in a public health master’s program, and a research associate from our rural practice-based research network. We also received feedback during the process from two state policy researchers.
Initially, we identified our sub-sample of 722 parents who contributed narrative comments sufficient for analysis and then, aided by SPSS 14.0 software, confirmed that this sub-sample had similar demographic characteristics to those of survey respondents and those of the total eligible sample. After this preliminary review, each team member independently read the narratives and assigned themes. We then met to create a codebook of tree nodes using NVivo qualitative software 7.0 (NVivo7, Melbourne: QSR International Pty Ltd).
We repeated our individual reviews with codebook guidance and met regularly to conduct the narrative analysis using adapted immersion/crystallization techniques.57 During these meetings, we revised the codebook to reflect the multiple interpretations of all team members and policy research collaborators. We then subjected each text entry to line-by-line coding and re-reviewed it for relevance to the established nodes.
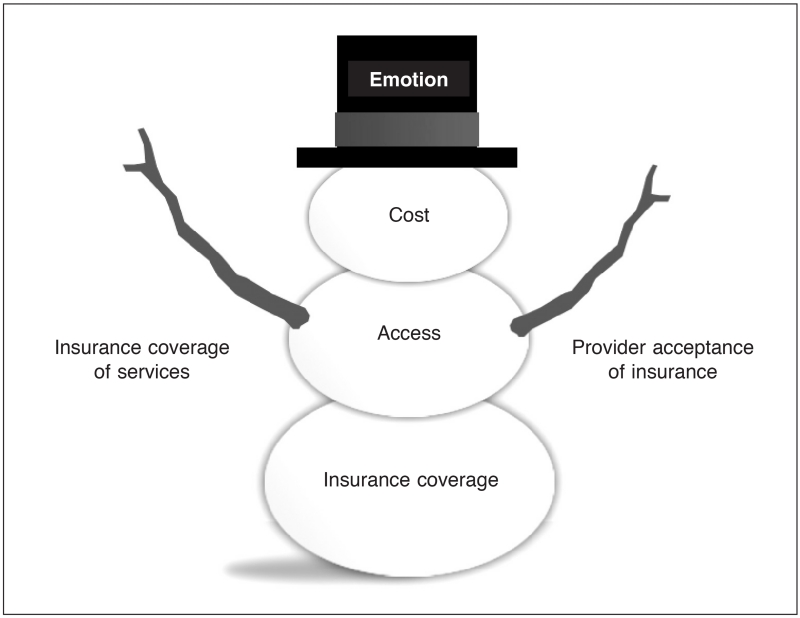
After the discovery of three major subthemes directly relevant to children’s health care access barriers, we conducted a further in-depth analysis to see if the child’s health insurance status was associated with different reporting of three subthemes. We also examined whether reports were different based on whether or not the child had a usual source of care. For this analysis, we conducted matrix-coded queries in NVivo with imported health insurance data from matched entries in the complete SPSS dataset. In a final authors’ meeting to synthesize quantitative and qualitative study findings, it became evident that families reported their needs in a hierarchical order. We designed a conceptual model—The Snowman Model—to illustrate this hierarchy of needs among this low-income population for obtaining children’s health care.
Results
Quantitative analysis
In the bivariate analyses, having health insurance and a usual source of care were the two covariates most consistently associated with better access to health care in all five outcomes measured. Racial and ethnic differences were significant in all measures; however, the highest rates of unmet need were not consistently seen among the same group. Parental health insurance was significantly associated with all measures except unmet prescription need. Parental employment appeared significant when considering unmet medical and dental needs, and household income was significantly associated with unmet prescription need. Rural children had higher rates of unmet medical and dental needs than others (Table 1).
Table 1. PERCENTAGE OF CHILDREN WITH UNMET HEALTH CARE NEEDS AND ACCESS PROBLEMS.
| Unmet medical need |
Unmet prescription need |
Big problem getting dental care |
Rarely or never got immediate care |
No doctor visits in past year |
|
|---|---|---|---|---|---|
| Demographic characteristics |
Weighted % |
Weighted % |
Weighted % |
Weighted % |
Weighted % |
| TOTAL | 16.1% | 22.0% | 26.0% | 21.7% | 13.8% |
| Age | |||||
| 1–4 years of age | 12.1% | 19.1% | 15.5% | 20.8% | 7.9% |
| 5–9 years of age | 15.8% | 20.5% | 26.9% | 21.6% | 13.4% |
| 10–14 years of age | 20.2% | 23.9% | 34.2% | 22.3% | 17.0% |
| 15–18 years of age |
17.5%
(p<.02) |
27.4% (p<.08) |
29.9%
(p<.01) |
22.8% (p<.96) |
20.7%
(p<.01) |
| Race/ethnicitya | |||||
| White, not Hispanic | 14.8% | 24.0% | 28.1% | 16.4% | 10.5% |
| Hispanic, any race | 17.2% | 19.3% | 25.2% | 44.3% | 26.8% |
| Non-White, non-Hispanic |
22.4%
(p<.05) |
14.6%
(p<.04) |
14.4%
(p<.01) |
21.3%
(p<.01) |
11.6%
(p<.01) |
| Parental employmentb | |||||
| Employed or self-employed |
18.4% | 24.2% | 28.7% | 23.3% | 14.6% |
| Not currently employed |
14.3%
(p<.04) |
20.5% (p<.11) |
23.7%
(p<.04) |
20.1% (p<.24) |
13.1% (p<.43) |
| Household income | |||||
| >133% FPL | 19.9% | 32.9% | 29.8% | 21.1% | 12.3% |
| 101%–133% FPL | 20.9% | 29.0% | 30.6% | 21.7% | 16.2% |
| 51%–100% FPL | 12.5% | 21.1% | 26.1% | 17.8% | 11.2% |
| 1%–50% FPL | 16.6% | 20.8% | 24.0% | 24.4% | 14.8% |
| Zero income | 17.1% (p<.08) |
16.0%
(p<.01) |
22.0% (p<.24) |
21.1% (p<.41) |
14.8% (p<.41) |
| Child’s insurance status | |||||
| Child insured | 13.5% | 20.1% | 22.0% | 18.5% | 10.9% |
| Child uninsured |
37.6%
(p<.01) |
38.7%
(p<.01) |
60.0%
(p<.01) |
51.8%
(p<.01) |
38.5%
(p<.01) |
| Parent insurance statusc | |||||
| Parent insured | 13.5% | 21.1% | 62.2% | 18.5% | 10.5% |
| Parent uninsured |
22.5%
(p<.01) |
23.9% (p<.25) |
37.8%
(p<.01) |
30.1%
(p<.01) |
20.5%
(p<.01) |
| Place of residenced | |||||
| Urban | 14.2% | 20.1% | 22.5% | 21.6% | 14.9% |
| Rural |
18.3%
(p<.04) |
24.3% (p<.06) |
30.3%
(p<.01) |
21.8% (p<.92) |
12.6% (p<.21) |
| Usual source of care | |||||
| Yes usual source of care |
14.3% | 21.1% | 23.3% | 18.8% | 10.7% |
| 29.3% | 29.5% | 46.5% | 46.1% | 45.6% | |
| No usual source of care | (p<.01) | (p<.04) | (p<.01) | (p<.01) | (p<.01) |
Race and ethnicity are combined into one variable.
Based on the employment status of the parent completing the survey.
Based on the insurance status of the parent completing the survey.
By ZIP code using Oregon Office of Rural Health designations.
FPL = federal poverty level
After controlling for all covariates, health insurance was the only predictor significantly associated with all five measures of health care access (Table 2). Compared with insured children (reference group = 1.00), uninsured children were more likely to report unmet medical need (adjusted odds ratio [OR] 2.97, 95% confidence interval [CI] 1.94, 4.56); unmet prescription need (OR 2.55, 95% CI 1.68, 3.87); unmet dental need (OR 5.39, 95% CI 3.67, 7.90); delayed urgent care (OR 3.88, 95% CI 2.30, 6.53); and no doctor visit in the past year (OR 2.40, 95% CI 1.51, 3.82). Moving beyond health insurance, disparities in reported access to care were most prominent based on age, race/ethnicity, rural/urban residence, and whether the child had a usual source of care. Compared with children aged 1–4 years, older children had higher rates of unmet dental need and delayed immediate care. Compared with White, non-Hispanic children, Hispanics across all racial categories had a higher likelihood of delayed urgent care (OR 3.36, 95% CI 2.13–5.31) and no doctor visits (OR 3.54, 95% CI 2.31–5.42). Non-White, non-Hispanic racial minorities reported more unmet medical need (OR 2.08, 95% CI 1.16–3.70). Compared with children living in urban areas, rural children had higher rates of unmet medical need (OR 1.39, 95% CI 1.01–1.92), and more significant problems accessing dental care (OR 1.37, 95% CI 1.04–1.80). Compared with children with a usual source of care, the most significant outcomes associated with having no usual source of care were higher odds of experiencing delays in care (OR 2.24, 95% CI 1.35–3.72), big problems accessing dental care (OR 2.11, 95% CI 1.33–3.33), and no doctor visits in the past year (OR 6.20, 95% CI 3.83–10.04).
Table 2. ADJUSTED ODDS OF CHILD HAVING UNMET HEALTH CARE NEEDS AND ACCESS PROBLEMS.
| Unmet medical need |
Unmet prescription need |
Big problem getting dental care |
Rarely or never got immediate care |
No doctor visits in past year |
|
|---|---|---|---|---|---|
| N=72,077 (n=2313) |
N=71,453 (n=2291) |
N=71,192 (n=2286) |
N=49,574 (n=1572) |
N=72,819 (n=2336) |
|
| Demographic characteristics |
Adjusted OR (95% CI) |
Adjusted OR (95% CI) |
Adjusted OR (95% CI) |
Adjusted OR (95% CI) |
Adjusted OR (95% CI) |
| Age | |||||
| 1–4 years of age | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 5–9 years of age | 1.25 (0.80, 1.95) | 0.98 (0.68, 1.43) | 1.98 (1.35, 2.92) | 0.88 (0.54, 1.44) | 1.78 (1.06, 2.98) |
| 10–14 years of age | 1.71 (1.08, 2.68) | 1.31 (0.89, 1.93) | 2.57 (1.74, 3.82) | 1.13 (0.67, 1.89) | 2.93 (1.71, 5.03) |
| 15–18 years of age | 1.37 (0.85, 2.20) | 1.42 (0.93, 2.15) | 2.08 (1.32, 3.26) | 1.00 (0.60, 1.65) | 4.39 (2.50, 7.69) |
| Race/ethnicitya | |||||
| White, not Hispanic | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Hispanic, any race | 0.96 (0.61, 1.52) | 0.73 (0.48, 1.10) | 0.77 (0.52, 1.14) | 3.36 (2.13, 5.31) | 3.54 (2.31, 5.42) |
| Non-White, non-Hispanic |
2.08 (1.16, 3.70) | 0.68 (0.37, 1.22) | 0.31 (0.17, 0.55) | 1.45 (0.72, 2.92) | 0.93 (0.45, 1.91) |
| Parental employmentb | |||||
| Employed/self-employed | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Not employed | 0.79 (0.56, 1.11) | 0.90 (0.67, 1.21) | 0.95 (0.72, 1.26) | 0.73 (0.49, 1.07) | 1.01 (0.69, 1.47) |
|
Household monthly
income |
|||||
| >133% FPL | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 101%–133% FPL | 1.43 (0.77, 2.66) | 1.04 (0.63, 1.71) | 1.40 (0.84, 2.33) | 1.50 (0.73, 3.12) | 1.54 (0.68, 3.48) |
| 51%–100% FPL | 0.75 (0.42, 1.36) | 0.64 (0.40, 1.02) | 0.99 (0.62, 1.58) | 1.12 (0.60, 2.10) | 0.93 (0.45, 1.94) |
| 1%–50% FPL | 1.11 (0.63, 1.96) | 0.64 (0.40, 1.01) | 0.92 (0.57, 1.48) | 1.52 (0.83, 2.75) | 1.11 (0.54, 2.30) |
| Zero income | 1.39 (0.69, 2.79) | 0.47 (0.26, 0.84) | 0.82 (0.44, 1.52) | 1.49 (0.67, 3.32) | 1.25 (0.54, 2.93) |
| Child’s insurance status | |||||
| Child insured | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Child uninsured | 2.97 (1.94, 4.56) | 2.55 (1.68, 3.87) | 5.39 (3.67, 7.90) | 3.88 (2.30, 6.53) | 2.40 (1.51, 3.82) |
| Parent insurance statusc | |||||
| Parent insured | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Parent uninsured | 1.48 (1.04, 2.12) | 0.89 (0.64, 1.22) | 0.82 (0.60, 1.10) | 1.08 (0.70, 1.68) | 1.18 (0.80, 1.76) |
| Place of residenced | |||||
| Urban | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Rural | 1.39 (1.01, 1.92) | 1.18 (0.90, 1.55) | 1.37 (1.04, 1.80) | 1.00 (0.70, 1.45) | 0.73 (0.51, 1.04) |
| Usual source of care | |||||
| Yes usual source of care | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| No usual source of care | 1.44 (0.90, 2.31) | 1.03 (0.66, 1.61) | 2.11 (1.33, 3.33) | 2.24 (1.35, 3.72) | 6.20 (3.83, 10.04) |
Race and ethnicity are combined into one variable.
Based on the employment status of the parent completing the survey.
Based on the insurance status of the parent completing the survey.
By ZIP code using Oregon Office of Rural Health designations.
OR = odds ratio
CI = confidence interval
FPL = federal poverty level
Qualitative analysis
The 722 respondents who provided additional written comments wrote passionate narratives about numerous difficulties obtaining health care for themselves and their children. Consistent with findings from the quantitative analysis about how insurance coverage was a key predictor associated with the lowest rates of unmet health care need, narrative respondents were most concerned about a total lack of parental insurance coverage (36%) and significant insurance coverage gaps for their children (23%). Other comments related to two additional sub-themes about access barriers (23%) and cost barriers for children (20%). In a closer examination of the three themes that parents related directly to children’s unmet health care needs—coverage gaps, lack of access, and unaffordable costs—the rates of reporting about each theme appeared to differ based on the current and continuous health insurance status of the focal child. Fewer reporting differences were noted based on whether or not the child had a usual source of care (Table 3).
Table 3. PERCENTAGE OF PARENTS REPORTING THREE MAJOR THEMES INFLUENCING CHILD’S UNMET HEALTH CARE NEEDS, BY CHILD’S CURRENT INSURANCE STATUS AND USUAL SOURCE OF CARE.
| TOTAL |
Child’s current insurance status |
Child’s 12-month insurance coverage |
Child’s usual source of care? |
|||||
|---|---|---|---|---|---|---|---|---|
| Themes | All respondents N=722 |
Public insurance N=401 |
Uninsured N=135 |
Private insurance (or combo) N=176 |
Continuous 12-month coverage N=431 |
Coverage gap in past 12 months N=275 |
No usual source of care N=92 |
Yes usual source of care N=591 |
| Insurance coverage discontinuities (gaps) |
23% | 18% | 42% | 17% | 18% | 29% | 20% | 23% |
| Difficulty accessing health care services |
23% | 26% | 13% | 20% | 23% | 20% | 27% | 21% |
| Unaffordable costs of medical care |
20% | 15% | 15% | 32% | 19% | 20% | 15% | 20% |
Note: Child’s insurance status and usual source of care missing for a small number of respondents (totals do not equal 722).
Not surprisingly, gaps in children’s insurance coverage was the most commonly cited concern among parents with uninsured children. Among all families, parents with children currently uninsured were more likely to share concerns about coverage gaps for their children than those with current children’s coverage. Most often, parental comments expressed frustration with inflexibilities in the public system, such as income requirements and age limits. For example,
My raise at work did not outweigh my loss of [Medicaid] benefits. Maybe I should work less so I can qualify again. [Child: 6 yrs, male, non-Hispanic American Indian, public health insurance, rural, household income between 101–133% FPL, parent currently uninsured.]
I was 5 dollars over poverty and lost Oregon Health Plan [OHP]. [Child: 4 yrs, female, Hispanic White, public health insurance, urban, household income between 51–100% FPL, parent currently has public insurance.]
With no health insurance and no immediate means of obtaining insurance, I feel very vulnerable. It’s scary to think about getting sick with no way to get medical care. [Child: 17 yrs, female, Hispanic White, public health insurance, rural, household income between 1–50% FPL, parent currently uninsured.]
I lost my OHP because of the premiums. I was barely able to get by and had to pay an extra $20 to OHP. [Child: 4 yrs, female, non-Hispanic White, public health insurance, urban, household income between 1–50% FPL, parent currently has public insurance.]
Access barriers topped the list of concerns for parents with publicly-insured children (26% reported access vs. 15% unaffordable costs and 18% insurance gaps). Similarly, a greater proportion of families with current public insurance coverage for their children reported access barriers (26%) than of families with uninsured children (13%) or privately-insured children (20%). These access comments were most often about a shortage of providers or non-covered services. Examples to illustrate these points include:
It is great that we have the OHP but it is very hard to find a doctor or dentist that will accept you. We have to drive for 1.5 hours just to see a dentist for a check-up or cleaning. [Child: 5 yrs, male, non-Hispanic White, public health insurance, rural, household income between 51–100% FPL, parent currently has public insurance.]
He was never able to get in to see a doctor because no one was taking any new patients. Therefore it wasn’t even worth having him on OHP … [Child: 7 yrs, male, non-Hispanic White, private health insurance, urban, household income between 133–185% FPL, parent currently has private insurance.]
[We need] more plans, better dental, and more doctors to choose from. Recently, one of us got sick and not one doctor could see us in the office. We need more doctors available. [Child: 15 yrs, female, non-Hispanic White, public health insurance, rural, household income between 51–100% FPL, parent currently has public insurance.]
One parent reported not applying for public insurance coverage because of the access difficulties:
I’ve heard that it’s hard to find doctors who are accepting new OHP patients. We are generally healthy, so we are risking it. [Child: 10 yrs, female, non-Hispanic White, uninsured, urban, household income between 101–133% FPL, parent currently uninsured.]
Cost barriers were a concern to a greater proportion of parents of privately-insured children (32%) than of those with publicly-insured (15%) or uninsured children (15%). With cost concerns at the top of their list (32%) compared with insurance gaps and a lack of access (17% and 20%, respectively), many of these families described making difficult choices about their children’s health due to cost:
The doctor orders prescriptions, then we can’t get them because they cost so much. [Child: 9 yrs, female, non-Hispanic White, public health insurance, urban, household income between 51–100% FPL, parent currently has public insurance.]
We make sure our children get the medical care and medications they need, but sometimes this leaves us without money for other things. [Child: 15 yrs, female, non-Hispanic White, private health insurance, rural, household income between 101–133% FPL, parent currently has private insurance.]
I have to pay a lot out of pocket [for employer-sponsored insurance] and can’t afford it, so my son goes without. [Child: 15 yrs, male, non-Hispanic White, uninsured, rural, household income between 1–50% FPL, parent currently has private insurance.]
I was actually relieved when my husband lost his job because it made my son eligible for coverage again. There is no feeling in the world worse than trying to figure out if you should really take an injured child to the doctor or not because of lack of money. [Child: 3 yrs, male, non-Hispanic Black and American Indian, public health insurance, rural, household income between 1–50% FPL, parent currently uninsured.]
I believe we don’t qualify for OHP because we had a COBRA option, but we couldn’t afford it because it was $763—more than my rent. [Child: 9 yrs, male, non-Hispanic White, private health insurance, urban, household income between 133–185% FPL, parent currently has private insurance.]
Summary of findings
In the quantitative analysis, having health insurance was most consistently associated with the lowest rates of unmet need. Even with insurance, some parents reported difficulty obtaining necessary health care services for their children. One in five insured children rarely or never got immediate care as soon as it was needed. Qualitatively, parents were greatly concerned about their children’s unmet needs and most often identified children’s insurance coverage gaps, lack of access to health care services, and frustrations about the costs of medical care as the major contributing factors. Concerns about the difficulties accessing necessary health care services and unaffordable costs were more common among families with health insurance coverage (publicly-insured and privately-insured, respectively), while uninsured families were more focused on obtaining and maintaining insurance coverage.
Discussion
In the low-income population studied, parents of insured children were less likely than parents of uninsured children to report unmet children’s health care needs. Similarly, narrative responses from a subset of these parents revealed that health insurance coverage for both parents and children matters greatly to this population. When describing their experiences navigating the health care system, parents made distinctions between insurance coverage and access to services, and there seemed to be a hierarchy of concerns. Insurance coverage was the primary concern; access and costs were secondary. Reporting of these three themes was disproportionate, depending on the child’s insurance status, further demonstrating the primary importance of insurance.
We created a modified Venn diagram (the Snowman Model) to depict this hierarchy of needs, synthesizing our quantitative and qualitative findings (Figure 1). The largest, anchoring snowball is stable and continuous insurance coverage. Once a health insurance foundation is secured and covers the entire family, then families can direct attention towards accessing services and worrying about costs. Gaining easy access to services is the next concern to arise, and has two major arms: provider acceptance of insurance and insurance coverage of services. For families with public insurance as the foundation, there was more concern about access barriers. In this population, if the insurance plan does not have provisions for certain services or if providers do not accept the coverage, there are limited options for obtaining the care. In this case, cost was probably not reported as a problem because most of the children were going without the services. After the barriers of obtaining insurance and access are overcome, the next concern is cost, represented by the top of the snowman. For those with private insurance, access may have been somewhat better but at higher, and often unaffordable, costs. While there is a hierarchy, all three elements—insurance, access, and cost—are related. Over all three themes is the sense of emotional and financial security that comes when the snowman is balanced. If stable insurance begins to melt away, access and cost become unstable (metaphorically, the snowman leans over). Eventually, the snowman collapses (melts) requiring a fresh start in rebuilding again. Once insurance is solidly in place, it still takes continued effort to achieve optimal access at an affordable cost.
Figure 1.
The Snowman Model—a hierarchy of needs for obtaining health care.
Previous studies have demonstrated that significant access and utilization barriers exist for poor, uninsured children.8,9 As confirmed by our study, insurance status is not a static phenomenon and parental concerns extend to the instability of coverage. Parents constantly fear the loss of insurance, which can be devastating to a child’s care. Even short insurance gaps are increasingly recognized as frequent and significant barriers to care.58 Gaps act in a “dose-response” manner to inhibit access to care and increase unmet medical need—the longer the gap, the worse the problems with access.59–61
Having stable, continuous insurance is associated with better access to health care and less unmet need,11 but insurance alone is not a guarantee of access to health care. As recently reported, even privately-insured children do not get optimal quality health care up to 50% of the time.4 Beyond insurance, many other factors affect whether children have unmet health care need. As other risk factors mount, including language barriers, lack of parental education, and poverty, children experience greater barriers to accessing care.2
Findings from this study contribute to current discussions about how insurance coverage, while important, may not provide unfettered access to quality health care for low-income children. This study confirms that parents are aware of these factors, and goes beyond past research in using a mixed-methods approach to develop a conceptual framework of the hierarchy of health care needs for low-income children (the Snowman Model in Figure 1). This hierarchical model of health care needs illustrates the need to restructure the current health care system in the United States beyond measures that expand insurance coverage.
Study considerations
Interpretation of the data here requires consideration of some important issues. First, families already connected to at least one system of public benefits (food stamps) may encounter fewer health insurance coverage problems than the low-income population generally. In addition, every state has a unique health insurance environment, so parental perspectives may differ depending on how the state administers public insurance programs. Because the data from this study can only be generalized to Oregon’s food stamp population, these results may understate the prevalence of insurance instabilities among all low-income families. This study, however, does capture the relationship between lack of insurance and higher rates of unmet need.
Second, for budgetary reasons, the survey was only administered in English, Spanish, and Russian; telephone follow-up was not possible. Although the survey was written at a fifth-grade reading level with no writing requirement, it is also likely that low literacy rates among this population contributed to a lack of response from many potential participants. While our response rate is comparable to other similar studies of Medicaid-eligible populations, even some that employed telephone follow-up and personal interviews, response bias remains an important consideration. The comprehensive food stamp administrative database allowed us to account for slight demographic differences between respondents and non-respondents in the weighting process. The raking ratio estimation adjustments for non-response were also conducted to further address this anticipated bias.
Finally, there is always the potential for recall bias with self-reported data. To minimize recall bias, validated questions were used from national surveys that ask respondents to recall events and occurrences only in the past 12 months, and several questions pertained to similar topics. Narrative responses to the open-ended question may have been biased by the content of the survey, which included specific queries about health insurance coverage for both children and parents, access to health care, and costs of health care. These questions did, however, provide several opportunities to report barriers and concerns about access to health care. It is significant that, after completing the survey, many parents still felt compelled to write further narratives about their situations. Finally, it is possible that we received narrative responses from only those families who encountered the most difficulties with the system, so the results may not be generalizeable to all families. The sub-sample, however, does have demographic characteristics similar to the original population.
Conclusions and Policy Implications
As a foundation for children to have adequate access to health care, families must be able to obtain and maintain stable insurance coverage. Parents of low-income children are greatly concerned about maintaining health insurance coverage for both their children and themselves, yet current fiscal constraints have led many states to terminate public health insurance coverage for parents and to increase restrictions on continuous children’s coverage. Importantly, SCHIP has dramatically improved access to care and decreased unmet need for children.62 Unfortunately, re-authorization and/or expansion of SCHIP at the federal level faced substantial opposition from the executive branch in 2007.19,63 SCHIP continues to be vulnerable, with current funding only temporarily extended via short-term continuing resolutions. Concurrently, in the United States, the number of uninsured children is dramatically increasing—one in five U.S. children in poverty is uninsured.64 If SCHIP is not reauthorized, let alone expanded, many more children will face the pivotal barrier of uninsurance.
Low-income parents who overcome the uninsurance barrier to obtain insurance coverage for their children will still face concerns about gaining adequate access to the health care system. Public cost containment efforts continually target reductions in public health insurance payments to providers, forcing providers in turn to limit the number of publicly-insured patients they serve. This cascade affects access. Even if insurance coverage is attainable for some low-income families, many of them have difficulty accessing necessary health care services and cannot afford medical care costs. Broader and more comprehensive reforms, beyond those that incrementally expand coverage, are needed to ensure quality, cost-effective, integrated care for U.S. children and adults.65,66
Acknowledgments
Support: The study was funded by a grant from the Health Resources and Services Administration (HRSA) obtained by the Office for Oregon Health Policy and Research. Jen DeVoe’s time on this project was supported by grant numbers 5-F32-HS014645 and 1-K08-HS16181 from the Agency for Health care Research and Quality (AHRQ). Alia Baez’s time on this project was supported by a medical student research grant from the Oregon Academy of Family Physicians.
Appendix—Outcome Variables Pertaining to Unmet Health Care Needs for Children
| Outcome variable | Corresponding Survey Question(s) |
|---|---|
| Unmet Medical Need | • In the last 12 months, was there any time when YOUR CHILD needed medical care, but did NOT get it? [yes/no] |
|
Unmet Prescription Need |
• In the last 12 months, was there ever a time YOUR CHILD needed prescription medicines but you could NOT afford to fill the prescription? (DO NOT count free samples as a filled prescription.) [yes/no] |
|
Unmet Dental Need (Big Problem Getting Dental Care) |
• In the last 12 months, how much of a problem, if any, was it to get dental care for your child? [dichotomized: big problem, not a problem/small problem] |
|
Delayed Urgent Care (Rarely or never Got Immediate Care) |
• In the last 12 months, when YOUR CHILD needed care right away for an illness, injury, or condition, how often did your child get care as soon as you wanted it? INCLUDED OPTION TO OPT OUT IF CHILD DID NOT NEED CARE |
| • [dichotomized: rarely/never; always/usually] | |
| No Doctor Visits | • In the last 12 months, how many times did you take YOUR CHILD to a doctor’s office or clinic for care? (DO NOT include emergency room or hospital visits. Your best estimate is fine.) [continuous variable, dichotomized as no doctor visits/yes doctor visits in past year] |
Footnotes
Prior Presentations: Qualitative themes presented at Society of Teachers of Family Medicine, Annual Meeting, April 28, 2007, Chicago; Conceptual Model presented at North American Primary Care Research Group Annual Meeting, October 15–18, 2007, Vancouver, British Columbia.
Notes
- 1.Chung P, Schuster M. Access and quality in child health services: voltage drops. Health Aff (Millwood) 2004 Sep-Oct;23(5):77–87. doi: 10.1377/hlthaff.23.5.77. [DOI] [PubMed] [Google Scholar]
- 2.Stevens GD, Seid M, Mistry R, et al. Disparities in primary care for vulnerable children: the influence of multiple risk factors. Health Serv Res. 2006 Apr;41(2):507–31. doi: 10.1111/j.1475-6773.2005.00498.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stevens GD, Seid M, Halfon N. Enrolling vulnerable, uninsured but eligible children in public health insurance: association with health status and primary care access. Pediatrics. 2006 Apr;117(4):e751–9. doi: 10.1542/peds.2005-1558. [DOI] [PubMed] [Google Scholar]
- 4.Mangione-Smith R, DeCristofaro AH, Setodji CM, et al. The quality of ambulatory care delivered to children in the United States. N Engl J Med. 2007 Oct 11;357(15):1515–23. doi: 10.1056/NEJMsa064637. [DOI] [PubMed] [Google Scholar]
- 5.Starfield B. U.S. child health: what’s amiss, and what should be done about it? Health Aff (Millwood) 2004 Sep-Oct;23(5):165–70. doi: 10.1377/hlthaff.23.5.165. [DOI] [PubMed] [Google Scholar]
- 6.Starfield B, Shi L. The medical home, access to care, and insurance: a review of evidence. Pediatrics. 2004 May;113(5 Suppl):1493–8. [PubMed] [Google Scholar]
- 7.Newacheck PW, Stoddard JJ, Hughes DC, et al. Health insurance and access to primary care for children. N Engl J Med. 1998 Feb 19;338(8):513–9. doi: 10.1056/NEJM199802193380806. [DOI] [PubMed] [Google Scholar]
- 8.Newacheck PW, Hughes DC, Hung YY, et al. The unmet health needs of America’s children. Pediatrics. 2000 Apr;105(4 Pt 2):989–97. [PubMed] [Google Scholar]
- 9.Newacheck P, Hughes D, Stoddard J. Children’s access to primary care: differences by race, income, and insurance status. Pediatrics. 1996 Jan;97(1):26–32. [PubMed] [Google Scholar]
- 10.Kaiser Commission on Medicaid and the Uninsured . Children’s health—why insurance matters. Kaiser Family Foundation; Washington, DC: 2002. Available at: http://www.kff.org/uninsured/4055-index.cfm. [Google Scholar]
- 11.Kaiser Commission on Medicaid and the Uninsured . Enrolling uninsured low-income children in Medicaid and SCHIP. Kaiser Family Foundation; Washington, DC: 2007. Available at: http://www.kff.org/medicaid/upload/2177-05.pdf. [Google Scholar]
- 12.U.S. Census Bureau . 2005 U.S. Census Bureau Fact Finder. U.S. Census Bureau; Washington, DC: 2005. [Google Scholar]
- 13.Kaiser Commission on Medicaid and the Uninsured . Health coverage for low-income children. Kaiser Family Foundation; Washington, DC: 2007. Available at: http://www.kff.org/uninsured/upload/2144-05.pdf. [Google Scholar]
- 14.Sommers B. Why millions of children eligible for Medicaid and SCHIP are uninsured: poor retention versus poor take-up. Health Aff (Millwood) 2007 Sep-Oct;26(5):w560–7. doi: 10.1377/hlthaff.26.5.w560. Epub 2007 Jul 26. [DOI] [PubMed] [Google Scholar]
- 15.Sommers BD. From Medicaid to uninsured: drop-out among children in public insurance programs. Health Serv Res. 2005 Feb;40(1):59–78. doi: 10.1111/j.1475-6773.2005.00342.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hudson JL, Selden TM. Children’s eligibility and coverage: recent trends and a look ahead. Health Aff (Millwood) 2007 Sep-Oct;26(5):w618–29. doi: 10.1377/hlthaff.26.5.w618. Epub 2007 Aug 16. [DOI] [PubMed] [Google Scholar]
- 17.Fairbrother GL, Emerson HP, Partridge L. How stable is medicaid coverage for children? Health Aff (Millwood) 2007 Mar-Apr;26(2):520–8. doi: 10.1377/hlthaff.26.2.520. [DOI] [PubMed] [Google Scholar]
- 18.Office for Oregon Health Policy and Research . Issue brief: covering kids in Oregon. Office for Oregon Health Policy and Research; Salem, OR: 2005. Available at http://ohpr.oregon.gov/OHPPR/RSCH/docs/CKidsbrief_Final.pdf. [Google Scholar]
- 19.Perrin JM. SCHIP, children, and politics. Ambul Pediatr. 2007 Nov-Dec;7(6):405–6. doi: 10.1016/j.ambp.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 20.Center on Budget and Policy Priorities . The President’s comments on Congress’ SCHIP plan. Center on Budget and Policy Priorities; Washington, DC: 2007. Available at http://www.cbpp.org/9-20-07health.htm. [Google Scholar]
- 21.Kaiser Commission on Medicaid and the Uninsured . Children’s health insurance program reauthorization act of 2007. Kaiser Family Foundation; Washington, DC: 2007. Available at http://www.kff.org/medicaid/upload/7714.pdf. [Google Scholar]
- 22.Kenney G, Yee J. SCHIP at a crossroads: experiences to date and challenges ahead. Health Aff (Millwood) 2007 Mar-Apr;26(2):356–69. doi: 10.1377/hlthaff.26.2.356. [DOI] [PubMed] [Google Scholar]
- 23.Kronebusch K, Elbel B. Simplifying children’s Medicaid and SCHIP. Health Aff (Millwood) 2004 May-Jun;23(3):233–46. doi: 10.1377/hlthaff.23.3.233. [DOI] [PubMed] [Google Scholar]
- 24.Reschovsky JD, Hadley J. Employer health insurance premium subsidies unlikely to enhance coverage significantly. Center for Studying Health System Change; Washington, DC: 2001. Available at http://www.hschange.com/CONTENT/392/?topic=topic01. [PubMed] [Google Scholar]
- 25.Thompson F. Children and the take-up challenge: renewal processes in Medicaid and CHIP. Federalism Research Group; Albany, NY: 2003. Available at http://www.rockinst.org/WorkArea/showcontent.aspx?id=6924. [Google Scholar]
- 26.Hadley J, Holahan J. How much medical care do the uninsured use, and who pays for it? Health Aff (Millwood) 2003 Jan-Jun;:W3-66-81. doi: 10.1377/hlthaff.w3.66. Suppl Web Exclusives. [DOI] [PubMed] [Google Scholar]
- 27.Hadley J, Holahan J. Who pays and how much? The cost of caring for the uninsured. The Urban Institute; Washington, DC: 2003. [Google Scholar]
- 28.Holahan J, Zedlewski S. Expanding Medicaid to cover uninsured Americans. Health Aff (Millwood) 1991;10(1):45–61. doi: 10.1377/hlthaff.10.1.45. Spring. [DOI] [PubMed] [Google Scholar]
- 29.Sloan F, Conover C. Effects of state reforms on health insurance coverage of adults. Inquiry. 1998;35(3):280–93. Fall. [PubMed] [Google Scholar]
- 30.Mitchell JB, Haber SG, Khatutsky G, et al. Impact of the Oregon Health Plan on access and satisfaction of adults with low income. Health Serv Res. 2002 Feb;37(1):11–31. [PubMed] [Google Scholar]
- 31.Haber SG, Khatutsky G, Mitchell JB. Covering uninsured adults through Medicaid: lessons from the Oregon health plan. Health Care Financ Rev. 2000;22(2):119–35. Winter. [PubMed] [Google Scholar]
- 32.Moreno L, Hoag SD. Covering the uninsured through TennCare: does it make a difference? Health Aff (Millwood) 2001 Jan-Feb;20(1):231–9. doi: 10.1377/hlthaff.20.1.231. [DOI] [PubMed] [Google Scholar]
- 33.Tollen L, Crane RM. A temporary fix? Implications of the move away from comprehensive health benefits. EBRI Issue Brief. 2002 Apr;(244):1–27. [PubMed] [Google Scholar]
- 34.Lee JS, Tollen L. How low can you go? The impact of reduced benefits and increased cost sharing. Health Aff (Millwood) 2002 Jul-Dec;:W229–41. doi: 10.1377/hlthaff.w2.229. Suppl Web Exclusives. [DOI] [PubMed] [Google Scholar]
- 35.Schoen C, Lyons D, Rowland D, et al. Insurance matters for low-income adults: results from a five-state survey. Health Aff (Millwood) 1997 Sep-Oct;16(5):163–71. doi: 10.1377/hlthaff.16.5.163. [DOI] [PubMed] [Google Scholar]
- 36.Ku L, Coughlin TA. Sliding-scale premium health insurance programs: four states’ experiences. Inquiry. 1999–2000;36(4):471–80. Winter. [PubMed] [Google Scholar]
- 37.Newhouse J, Insurance Experiment Group . Free for all? Lessons from the RAND health insurance experiment. Harvard University Press; Cambridge, MA: 1996. Reprint ed. [Google Scholar]
- 38.Wong MD, Andersen R, Sherbourne CD, et al. Effects of cost sharing on care seeking and health status: results from the Medical Outcomes Study. Am J Public Health. 2001 Nov;91(11):1889–94. doi: 10.2105/ajph.91.11.1889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Long S. Hardship among the uninsured: choosing among food, housing and health insurance. The Urban Institute; Washington, DC: 2003. [Google Scholar]
- 40.Fairbrother G, Dutton MJ, Bachrach D, et al. Costs of enrolling children in Medicaid and SCHIP. Health Aff (Millwood) 2004 Jan-Feb;23(1):237–43. doi: 10.1377/hlthaff.23.1.237. [DOI] [PubMed] [Google Scholar]
- 41.Kenney G, Haley J, Dubay L. How familiar are low-income parents with Medicaid and SCHIP? Number B-34 in series, New Federalism: National Survey of America’s Families. The Urban Institute; Washington, DC: 2001. [Google Scholar]
- 42.Selden T, Hudson J. Access to care and utilization among children: estimating the effects of public and private coverage. Med Care. 2006 May;44(5 Suppl):I19–26. doi: 10.1097/01.mlr.0000208137.46917.3b. [DOI] [PubMed] [Google Scholar]
- 43.Sommers A, Dubay L, Blumberg L, et al. Dynamics in Medicaid and SCHIP eligibility among children in SCHIP’s early years: implications for reauthorization. Health Aff (Millwood) 2007 Sep-Oct;26(5):w598–607. doi: 10.1377/hlthaff.26.5.w598. Epub 2007 Aug 7. [DOI] [PubMed] [Google Scholar]
- 44.Bodenheimer T. The Oregon health plan—lessons for the nation. First of two parts. N Engl J Med. 1997 Aug 28;337(9):651–5. doi: 10.1056/NEJM199708283370923. [DOI] [PubMed] [Google Scholar]
- 45.Oberlander J. Health reform interrupted: the unraveling of the Oregon Health Plan. Health Aff (Millwood) 2007 Jan-Feb;26(1):w96–105. doi: 10.1377/hlthaff.26.1.w96. Epub 2006 Dec 19. [DOI] [PubMed] [Google Scholar]
- 46.Carlson M, DeVoe J, Wright B. Short-term impacts of coverage loss in a Medicaid population: early results from a prospective cohort study of the Oregon Health Plan. Ann Fam Med. 2006 Sep-Oct;4(5):391–8. doi: 10.1370/afm.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Solotaroff R, DeVoe J, Wright B, et al. Medicaid programme changes and the chronically ill: early results from a prospective cohort study of the Oregon Health Plan. Chronic Illn. 2005 Sep;1(3):191–205. doi: 10.1177/17423953050010030301. [DOI] [PubMed] [Google Scholar]
- 48.Wright B, Carlson M, Edlund C, et al. The impact of increased cost sharing on Medicaid enrollees. Health Aff (Millwood) 2005 Jul-Aug;24(4):1106–16. doi: 10.1377/hlthaff.24.4.1106. [DOI] [PubMed] [Google Scholar]
- 49.Westat . Annual Report of the National CAHPS Benchmarking Database 2000. U.S. Agency for Healthcare Research and Quality/U.S. Department of Health and Human Services; Rockville, MD: 2001. [Google Scholar]
- 50.Elliot D. Weighting for non-response: a survey researcher’s guide. Office of Population Censuses and Surveys, Social Survey Division; London, England: 1991. [Google Scholar]
- 51.Kalton G, Kasprzyk D. The treatment of missing survey data. Survey Methodology. 1986;12(1):1–16. [Google Scholar]
- 52.Agency for Healthcare Research and Quality . CAHPS 2.0 Survey and Reporting Kit. Agency for Healthcare Research and Quality; Silver Springs, MD: 2002. [Google Scholar]
- 53.Center for Studying Health System Change . Community tracking study, household survey instrument 2000–2001, round three, technical publication #54. Center for Studying Health System Change; Washington, DC: 2004. [Google Scholar]
- 54.Agency for Healthcare Research and Quality . Medical expenditure panel survey. Agency for Healthcare Research and Quality; Rockville, MD: 2006. Available at http://www.meps.ahrq.gov/mepsweb/ [Google Scholar]
- 55.National Center for Health Statistics . National health interview survey. National Center for Health Statistics/Centers For Disease Control and Prevention; Hyattsville, MD: 2007. Available at http://www.cdc.gov/nchs/nhis.htm. [Google Scholar]
- 56.Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974;9(3):208–20. Fall. [PMC free article] [PubMed] [Google Scholar]
- 57.Borkan J. Immersion/crystallization. In: Crabtree BF, Miller W, editors. Doing qualitative research. 2nd edition Sage Publications; Thousand Oaks, CA: 1999. pp. 179–94. [Google Scholar]
- 58.Olson LM, Tang SF, Newacheck PW. Children in the United States with discontinuous health insurance coverage. N Engl J Med. 2005 Jul 28;353(4):382–91. doi: 10.1056/NEJMsa043878. [DOI] [PubMed] [Google Scholar]
- 59.Federico SG, Steiner JF, Beaty B, et al. Disruptions in insurance coverage: patterns and relationship to health care access, unmet need, and utilization before enrollment in the State Children’s Health Insurance Program. Pediatrics. 2007 Oct;120(4):e1009–16. doi: 10.1542/peds.2006-3094. [DOI] [PubMed] [Google Scholar]
- 60.Aiken K, Freed G, Davis M. When insurance status is not static: insurance transitions of low-income children and implications for health and health care. Ambul Pediatr. 2004;4(3):237–43. doi: 10.1367/A03-103R.1. [DOI] [PubMed] [Google Scholar]
- 61.DeVoe JE, Graham A, Krois L, et al. “Mind the Gap” in children’s health insurance coverage: does the length of a child’s coverage gap matter? Ambul Pediatr. 2008 Mar-Apr;8(2):129–34. doi: 10.1016/j.ambp.2007.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kempe A, Beaty B, Crane L, et al. Changes in access, utilization, and quality of care after enrollment into a state child health insurance plan. Pediatrics. 2005 Feb;115(2):364–71. doi: 10.1542/peds.2004-0475. [DOI] [PubMed] [Google Scholar]
- 63.Gorin SH, Moniz C. Why does President Bush oppose the expansion of SCHIP? Health Soc Work. 2007 Nov;32(4):243–6. doi: 10.1093/hsw/32.4.243. [DOI] [PubMed] [Google Scholar]
- 64.DeNavas-Walt C, Proctor B, Smith J. Income, poverty, and health insurance coverage in the United States: 2006 (Current Population Reports) U.S. Census Bureau; Washington, DC: Aug, 2007. pp. P60–233. [Google Scholar]
- 65.Mongan JJ, Lee TH. Do we really want broad access to health care? N Engl J Med. 2005 Mar 24;352(12):1260–3. doi: 10.1056/NEJMsb043863. [DOI] [PubMed] [Google Scholar]
- 66.Emanuel EJ, Fuchs VR. Health care vouchers—a proposal for universal coverage. N Engl J Med. 2005 Mar 24;352(12):1255–60. doi: 10.1056/NEJMsb041704. [DOI] [PubMed] [Google Scholar]