New social and environmental forces, including economic downturns, climate change, and human migrations from the Middle East and North Africa, are merging into a “perfect storm” to promote the widespread emergence of neglected tropical diseases (NTDs) in Southern Europe.
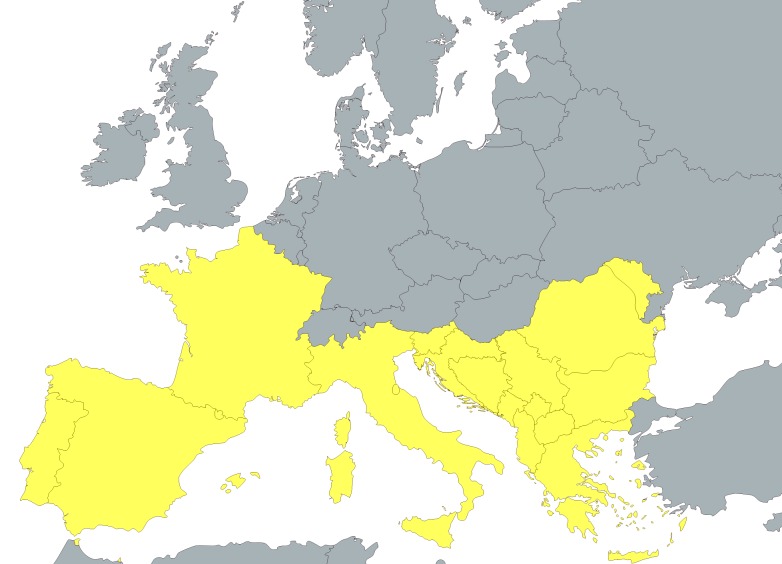
There is no single definition of the area or countries comprising Southern Europe, but most focus on the countries aligning the Mediterranean Sea, including Spain and Portugal (comprising the Iberian Peninsula), Italy (especially the portion on the Italian Peninsula), Southern France and Corsica, and Greece (Fig 1). The Balkan countries in southeastern Europe, including Croatia, are also sometimes included in this definition.
Fig 1. Southern Europe.
Map of Southern Europe. Figure created with mapchart.net
Throughout recorded history, vector-borne tropical infections have flourished in the warm Mediterranean climate of Southern Europe. For centuries, malaria (known as Roman estivo-autumnal fever) was endemic to the Pontine Marshes and low-lying area known as the Campagna surrounding Rome [1]. Some scholars have even attributed the decline of the Roman Empire partly to malaria [2,3], while others have conversely linked the dramatic upturns in the economies of Southern European countries to malaria elimination in the years following World War II [4]. Similarly, leishmaniasis caused by Leishmania infantum has also been an important vector-borne NTD in Southern Europe, as well as an important opportunistic infection in the region’s HIV/AIDS epidemic [5,6].
Over the last decade, however, a number of vector-borne diseases have emerged or re-emerged in Southern Europe. The major diseases are highlighted in Box 1, and include five diseases listed among WHO’s 17 NTDs, including Dengue, Chagas disease, leishmaniasis, opisthorchiasis, and schistosomiasis, as well as five others listed within the scope of PLOS Neglected Tropical Diseases—other arbovirus infections and vivax malaria—in addition to the borrelioses (relapsing fever is also in the scope of PLOS Neglected Tropical Diseases).
Box 1. Emerging Vector-Borne Diseases and Neglected Tropical Diseases in Southern Europe
| Viral Infections | Chikungunya |
| Dengue (DENV-1) | |
| West Nile virus infection | |
| Crimean-Congo hemorrhagic fever | |
| Toscano virus infection | |
| Bacterial Infections | Lyme Disease and other borrelioses |
| Protozoan Infections | Chagas disease |
| Leishmaniasis | |
| Vivax malaria | |
| Helminth Infections | Opisthorchiasis |
| Schistosomiasis |
Of particular concern is the recent emergence or re-emergence of arbovirus infections [7]. In terms of indigenous transmission, Chikungunya first emerged in Italy in 2007, with a second outbreak of in France in 2010 [7–10]. According to WHO, chikungunya also emerged in Spain in 2015 [11]. In 2012–2013, dengue fever re-emerged (after a period of decades) on Madeira off of the Atlantic coast of Portugal [12–14]. More than 1,000 cases were confirmed in the outbreak, caused by dengue virus type 1 (DENV-1), which may have been introduced from tropical regions of South America [12–14]. In Europe, both DENV-1 and Chikungunya are transmitted by Aedes albopictus (the Asian tiger mosquito) [15]. Ae. albopictus was first detected in Spain in 2004 [16].
West Nile virus (WNV) infection, transmitted by Culex mosquitoes, has also emerged in Southern Europe [17,18]. According to the European Centre for Disease Control and Prevention (ECDC), WNV re-emerged in Romania in 1996, but today the nation of Greece has the highest case rate, with Athens also being affected [7]. WNV cases are also occurring in southeastern Europe—Bulgaria, Hungary, and Romania—as well as in Italy [7], and there are concerns that these Southern European foci could spread to other parts of Europe [19].
Certain vector-borne viruses are endemic to Southern Europe. For instance, Toscano virus, transmitted by sand flies, is a significant cause of disease and aseptic meningitis in Italy [6]. Among the tick-borne arboviruses, Crimean-Congo hemorrhagic fever (CCHF) is endemic to the Balkans, with Turkey exhibiting the highest numbers of cases [7], but the infection has also emerged in Greece [20]. In contrast to CCHF, the flavivirus responsible for tick-borne encephalitis is mostly found in northeastern Europe [7], while the highest endemicity of Lyme borreliosis, a bacterial vector-borne disease, may be in Central Europe [21].
Vector-borne parasitic infections are also now important NTDs emerging in Southern Europe. Chagas disease is increasingly reported in Spain and elsewhere in Southern Europe due to importation from Bolivia where the prevalence rate is the highest, as well as Argentina, Brazil, and Mexico where the largest numbers of people are currently living with Chagas disease [22,23]. However, in terms of autochthonous transmission, leishmaniasis, caused mostly by Leishmania infantum and transmitted by Phlebotomus sandflies, has emerged as the most important protozoan NTD, especially as an opportunistic infection in AIDS patients [24,25]. L. infantum is a zoonotic infection that relies on canine reservoir hosts, and results in both human cutaneous and visceral leishmaniasis. Leishmania tropica, the major cause of old world anthroponotic cutaneous leishmaniasis in the Middle East and North Africa, has also occurred sporadically in Greece and elsewhere in Southern Europe [24].
Greece underwent a national malaria elimination effort in the years following World War II and up to 1960s [26]. As noted above, such efforts are believed to have promoted important economic returns on investment [4]. However, in 2009, autochthonous cases of vivax malaria were reported regularly from Greece, and have continued annually ever since [7,27]. Thus, these cases in Greece represent the first consistent European indigenous transmission of malaria in many years [27]. A new geospatial analysis has now identified transmission hotspots in Greece where it is expected that indigenous malaria transmission will continue [26]. Autochthonous malaria transmission has also been reported from Italy and Spain [7,28,29].
In terms of helminth infections, there is evidence for the Southern European emergence of snail-transmitted fluke infections, including opisthrochiasis in Italy [30], and schistosomiasis in Corsica, off the coast of southern France [31].
With the exceptions of CCHF and Lyme borreliosis, Southern Europe has become “ground zero” for the vector-borne NTDs now significantly affecting the public health and, potentially, the future economy of the Eurozone. Many of these diseases, such as chikungunya, dengue fever, WNV, malaria, and the snail-transmitted helminth infections, have emerged or re-emerged only in the past few years. Indeed, there is now a startling similarity between the vector-borne diseases patterns of North Africa and Southern Europe so that all the nations surrounding the Mediterranean Sea have become almost unified with respect to their endemic NTDs.
The factors responsible for promoting the vector-borne NTDs in Southern Europe are under investigation, but there are some key lead possibilities to consider.
Poverty. Throughout the world’s low- and middle-income countries, poverty is a major social determinant promoting the ongoing transmission of NTDs. Previous findings have determined that comparable levels of extreme poverty can also be found among the G20 countries and are also contributing to widespread NTDs [32,33]. It is interesting to note how the emergence or re-emergence of Southern Europe’s major NTDs roughly coincides with the European debt crisis that began in 2009 when countries such as Greece, Portugal, and Spain experienced difficulties in repaying their government debts without outside assistance. Ultimately, Greece defaulted on its debt to the International Monetary Fund in 2015, thereby precipitating a financial crisis linked to high unemployment. There is an important need to better understand the link between poverty and NTDs. So far, it has been found that NTDs flourish in impoverished settings, but also that NTDs exhibit a unique ability to reinforce poverty through their debilitating effects on workers, women, and growing and developing children.
Mass human migrations. Still another key social factor may be the humanitarian crisis linked to hundreds of thousands of people fleeing conflicts in Libya, Syria, and Iraq due to the occupation of ISIS [34]. In so doing, they could be introducing or re-introducing NTDs endemic to the Middle East and North Africa, including the vector-borne NTDs highlighted above. For example, cutaneous leishmaniasis in Syria, where it is often known as “Aleppo Evil,” has reached hyperendemic proportions due to breakdowns in health systems and lack of access to essential medicine, with at least tens of thousands of new cases annually [35]. Quite possibly both cutaneous leishmaniasis and sand fly vectors are being routinely re-introduced into Southern Europe.
Climate change. Finally, it has been noted that outside of the Arctic region, Europe’s single largest temperature increases associated with serious heat waves are now occurring in Southern Europe [36]. The factors promoting climate change include increased greenhouse gas emissions as a result of agriculture; burning of coal, oil, and gas (fossil fuels); landfills; and industrial pollutants [36]. Increased temperatures are helping to facilitate the survival and longevity of insects and snails with the capacity to transmit NTDs. Climate change may also promote the spread of some of Southern Europe’s vector-borne NTDs to Northern Europe, including WNV and leishmaniasis [19,37].
The needs for tackling Southern Europe’s emerging NTDs are pervasive and will need to include increased active surveillance activities, studies to elucidate the modes of indigenous transmission, and prevention measures. The ECDC has helped to establish an innovative European Environment and Epidemiology (E3) Network that will include geospatial mapping for next generation emerging vector-borne disease threats [26]. In parallel, many of the tools needed to control or eliminate these newly emerging NTDs have not yet been developed and we will require an aggressive program of focused research and development (R&D) on this front. Previously (together with a colleague), I have proposed the establishment of such a R&D center in Greece for this purpose [38]. Our rationale in proposing to locate the institute in Greece is because this country is geographically located at the confluence of the three major forces highlighted above—European poverty, the refugee crisis, and climate change—and because of their existing strengths in biotechnology. There is also an urgency to maintain biotechnology infrastructure in Greece (and prevent further brain drain) in light of its recent economic downturns and hardships. In addition, however, we must now consider dedicated funds from the European Union or perhaps another European body in order to launch initiatives to combat emerging NTDs and other vector-borne diseases in Southern Europe.
Funding Statement
The author received no specific funding for this work.
References
- 1.Harrison G (1978) Mosquitoes, Malaria, and Man: A History of the Hostilities Since 1880; EP Dutton; /New York, p. 171. [Google Scholar]
- 2.Sallares R (2002) Malaria and Rome: A History of Malaria in Ancient Italy; Oxford University Press, p. 358. [Google Scholar]
- 3.Wilford JN. DNA Shows Malaria Helped Topple Rome. The New York Times. 20 Feb 2001. Available: http://www.nytimes.com/2001/02/20/science/dna-shows-malaria-helped-topple-rome.html. Accessed 8 Sep 2015.
- 4.Gallup JL, Sachs JD (2001) The economic burden of malaria. Am J Trop Med Hyg 64 (1–2 Suppl): 85–96. [DOI] [PubMed] [Google Scholar]
- 5.Dujardin JC, Campino L, Canavate C, Dedet JP, Gradoni L, Soteriadou K, et al. (2008) Spread of vector-borne diseases and neglected of leishmaniasis, Europe. Emerg Infect Dis 14: 1013–8. 10.3201/eid1407.071589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hotez PJ, Gurwith M (2011) Europe’s neglected infections of poverty. Int J Infect Dis 15: e611–9. 10.1016/j.ijid.2011.05.006 [DOI] [PubMed] [Google Scholar]
- 7.European Centre for Disease Control and Prevention (2014) Annual epidemiological report Emerging and vector-borne diseases 2014, Stockholm 2014.
- 8.Angelini R, Finarelli AC, Angelini P, Po C, Petropulacos K, Macini P, et al. An outbreak of chikungunya fever in the province of Ravenna, Italy. Euro Surveill. 2007. September; 12, E 0709906. [DOI] [PubMed] [Google Scholar]
- 9.Grandadam M, Caro V, Plumet S, Thiberge JM, Souarès Y, Failloux AB, et al. Chikungunya virus, southeastern France. Emerg Infect Dis. 2011. May;17:910–3. 10.3201/eid1705.101873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tomasello D, Schlagenhauf P (2013) Chikungunya and dengue autochthonous cases in Europe, 2007–2012. Travel Med Infect Dis 11: 274–84. 10.1016/j.tmaid.2013.07.006 [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization (2015) Outbreak news: Chikungunya, Spain. Weekly Epidemiol Rec 90: 409–20. [PubMed] [Google Scholar]
- 12.Alves MJ, Fernandes PL, Amaro F, Osório H, Luz T, Parreira P, et al. Clinical presentation and laboratory findings for the first autochthonous cases of dengue fever in Madeira island, Portugal, October 2012. Euro Surveill. 2013; 18:pii = 20398. [PubMed] [Google Scholar]
- 13.Sousa CA, Clairouin M, Seixas G, Viveiros B, Novo MT, Silva AC, et al. Ongoing outbreak of dengue type 1 in the Autonomous Region of Madeira, Portugal: preliminary report. Euro Surveill. 2012; 17(49):pii = 20333. [DOI] [PubMed] [Google Scholar]
- 14.Schaffner F, Mathis A (2014) Dengue and dengue vectors in the WHO European region: past, present, and scenarios for the future. Lancet Infect Dis 14: 1271–80. 10.1016/S1473-3099(14)70834-5 [DOI] [PubMed] [Google Scholar]
- 15.Kraemer MU, Sinka ME, Duda KA, Mylne AQ, Shearer FM et al. (2015) The global distribution of the arbovirus vectors Aedes aegypti and Ae albopictus. Elife. 2015 4:e08347 10.7554/eLife.08347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lucientes-Curdi J, Molina-Moreno R, Amela-Heras C, Simon-Soria F, et al. (2014) Dispersion of Aedes albopictus in the Spanish Mediterranean area. Eur J Public Health 24: 637–40. 10.1093/eurpub/cku002 [DOI] [PubMed] [Google Scholar]
- 17.Di Sabatino D, Bruno R, Sauro F, Danzetta ML, Cito F, Iannetti S, Narcisi V, De Massis F, Calistri P (2014) Epidemiology of West Nile disease in Europe and in the Mediterranean basin from 2009 to 2013. Biomed Res Int 2014: 907852 10.1155/2014/907852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pupella S, Pisani G, Cristiano K, Catalano L, Grazzini G (2014) Update on West Nile virus in Italy. Blood Transfus 12: 626–7. 10.2450/2014.0110-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fros JJ, Geertsema C, Vogels CB, Roosjen PP, Failloux A-B, Vlak JM, et al. (2015) West Nile Virus: High Transmission Rate in North-Western European Mosquitoes Indicates Its Epidemic Potential and Warrants Increased Surveillance. PLoS Negl Trop Dis 9: e0003956 10.1371/journal.pntd.0003956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Papa A, Sidira P, Larichev V, Gavrilova L, Kuzmina K, Mousavi-Jazi M, Mirazimi A, Stroher U, Nichol S (2014) Crimean-Congo hemorrhagic fever virus Greece. Emerg Infect Dis 20: 288–90. 10.3201/eid2002.130690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rizzoli A, Hauffe HC, Carpi G, Vourc’h GI, Neteler M, Rosa R (2011) Lyme borreliosis in Europe. Eurosurveillance 16: pii: 19906. [PubMed] [Google Scholar]
- 22.Perez-Molina JA, Perez AM, Norman FF, Monge-Maillo B, Lopez-Velez R (2015) Old and new challenges in Chagas disease. Lancet Infect Dis 15: 1347–56. 10.1016/S1473-3099(15)00243-1 [DOI] [PubMed] [Google Scholar]
- 23.Salvador F, Treviño B, Sulleiro E, Pou D, Sánchez-Montalvá A, Cabezos J, Soriano A, Serre N, Gómez I Prat J, Pahissa A, Molina I (2014) Trypanosoma cruzi infection in a non-endemic country: epidemiological and clinical profile. Clin Microbiol Infect. 20:706–12. 10.1111/1469-0691.12443 [DOI] [PubMed] [Google Scholar]
- 24.Ready PD (2010) Leishmaniasis emergence in Europe. Eurosurveillance 15: 19505 [PubMed] [Google Scholar]
- 25.Antoniou M, Gramiccia M, Molina AR, Dvorak V, Volf P (2013) The role of indigenous phlebotomine sandflies in mammals in the spreading of leishmaniasis agents in the Mediterranean region. Euro Surveill 18: 20540 [DOI] [PubMed] [Google Scholar]
- 26.Semenza JC, Sudre B, Oni T, Suk JE, Giesecke J (2013) Linking Environmental Drivers to Infectious Diseases: The European Environment and Epidemiology Network. PLoS Negl Trop Dis 7: e2323 10.1371/journal.pntd.0002323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Danis K, Baka A, Lenglet A, Van Bortel W, Terzaki I, Tseroni M,et al. (2011) Autochthonous Plasmodium vivax malaria in Greece, 2011. Euro Surveill. 16: 19993 [PubMed] [Google Scholar]
- 28.Santa-Olalla Peralta P, Vazquez-Torres MC, Latorre-Fandos E, Mairal-Claver P, Cortina-Solano P, Puy-Azón A, et al. (2010) First autochthonous malaria case due to Plasmodium vivax since eradication, Spain, October 2010. Euro Surveill. 15:19684 [DOI] [PubMed] [Google Scholar]
- 29.Romi R, Boccolini D, Menegon M, Rezza G (2012) Probable autochthonous introduced malaria cases in Italy in 2009–2011 and the risk of local vector-borne transmission. Euro Surveill. 17: 20325 [PubMed] [Google Scholar]
- 30.Pozio E, Armignacco O, Ferri F, Gomez Morales MA (2013) Opisthorchis felineus, an emerging infection in Italy and its implication for the European Union. Acta Trop 126: 54–62. 10.1016/j.actatropica.2013.01.005 [DOI] [PubMed] [Google Scholar]
- 31.de Laval F, Savini H, Biance-Valero E, Simon F (2014) Human schistosomiasis: an emerging threat for Europe. Lancet. 384:1094–5. [DOI] [PubMed] [Google Scholar]
- 32.Hotez PJ (2013) NTDs V.2.0: “Blue Marble Health”—Neglected Tropical Disease Control and Elimination in a Shifting Health Policy Landscape. PLoS Negl Trop Dis 7: e2570 10.1371/journal.pntd.0002570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hotez PJ (2015) Blue Marble Health Redux: Neglected Tropical Diseases and Human Development in the Group of 20 (G20) Nations and Nigeria. PLoS Negl Trop Dis 9: e0003672 10.1371/journal.pntd.0003672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.UNHCR. The UN Refugee Agency. 2015 UNHCR Regional Operations Profile–Europe. http://www.unhcr.org/pages/4a02d9346.html. Accessed 8 Sep 2015.
- 35.Du R, Hotez PJ, Al-Salem WS, Acosta-Serrano A. Old World Cutaneous Leishmaniasis and Refugee Crises in the Middle East and North Africa. PLoS Negl Trop Dis 10: e0004545 10.1371/journal.pntd.0004545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.European Environment Agency. Climate Change. http://www.eea.europa.eu/themes/climate/intro. Accessed 8 Sep 2015.
- 37.Naucke TJ, Menn B, Massberg D, Lorentz S (2008) Sandflies and leishmaniasis in Germany. Parasitol Res. 2008 December;103 Suppl 1:S65–8. 10.1007/s00436-008-1052-y [DOI] [PubMed] [Google Scholar]
- 38.Hotez PJ, Papageorgiou TD (2013) A New European Neglected Diseases Center for Greece? PLoS Negl Trop Dis 7: e1757 10.1371/journal.pntd.0001757 [DOI] [PMC free article] [PubMed] [Google Scholar]