Abstract
Hydrogen sulfide (H2S) is a mediator with demonstrated protective effects for the cardiovascular system. On the other hand, prostaglandin (PG)E2 is involved in vascular wall remodeling by regulating matrix metalloproteinase (MMP) activities. We tested the hypothesis that endogenous H2S may modulate PGE2, MMP-1 activity and endogenous tissue inhibitors of MMPs (TIMP-1/-2). This regulatory pathway could be involved in thinning of abdominal aortic aneurysm (AAA) and thickening of saphenous vein (SV) varicosities. The expression of the enzyme responsible for H2S synthesis, cystathionine-γ-lyase (CSE) and its activity, were significantly higher in varicose vein as compared to SV. On the contrary, the endogenous H2S level and CSE expression were lower in AAA as compared to healthy aorta (HA). Endogenous H2S was responsible for inhibition of PGE2 synthesis mostly in varicose veins and HA. A similar effect was observed with exogenous H2S and consequently decreasing active MMP-1/TIMP ratios in SV and varicose veins. In contrast, in AAA, higher levels of PGE2 and active MMP-1/TIMP ratios were found versus HA. These findings suggest that differences in H2S content in AAA and varicose veins modulate endogenous PGE2 production and consequently the MMP/TIMP ratio. This mechanism may be crucial in vascular wall remodeling observed in different vascular pathologies (aneurysm, varicosities, atherosclerosis and pulmonary hypertension).
Introduction
Hydrogen sulfide (H2S) has recently been identified as gaseous mediator in the cardiovascular system. H2S is essentially generated from the endogenous amino acid L-cysteine by the cystathionine-γ-lyase (CSE) enzymatic activity in human and rodent blood vessels [1]. It has been suggested that H2S plays a protective role in the pathogenesis and development of cardiovascular disease such as systemic hypertension and atherosclerosis. This gaseous mediator is considered as an oxygen sensor [2] controlling vascular tone and/or vascular wall remodeling. In mice, treatment with sodium hydrosulfide (NaHS, a H2S donor), reduced systemic blood pressure [3]. This effect is supported by in vitro studies describing relaxation induced by exogenous NaHS in isolated human mammary artery [4] and in vascular preparations derived from different animal species [5]. Furthermore, NaHS decreased the area of atherosclerotic lesions in ApoE knock-out mice [6]. Endogenous H2S has been shown to control remodeling of the vascular wall as relative medial thickness of the pulmonary artery could be increased by CSE inhibitors in a model of rat pulmonary hypertension [7].
It has been shown that vascular wall remodeling involved in the pathology of abdominal aortic aneurysms (AAA) and varicose saphenous veins share common determinants, controlled in a reversed manner that results in thinning and thickening of their vascular wall, respectively. The pathogenesis of AAA is characterized by a breakdown of elastic and collagen fibers (the extracellular matrix) due to increased proteolytic activity of serine proteases and matrix metalloproteinases (MMP). The degradation of elastin and of collagens by MMP-1, -2 and -9 plays a major role in vascular wall thinning in AAA [8, 9]. On the contrary, it has been demonstrated that in varicose veins decreased MMP-1 and MMP-2 activities could result in accumulation of collagens and thickening of the vascular wall [10]. There are some studies which have demonstrated an inhibitory role of H2S on the expression of MMPs in rat lung [11] and mice brain tissue [12]. However, the significance of H2S on MMP expression and activities in varicose vein and AAA pathology, as well as in other human vascular diseases remains undefined.
H2S regulates cyclooxygenase (COX) expression and prostaglandin E2 (PGE2) synthesis. PGE2 is a prostanoid produced by nearly all vascular cell types and derives from the arachidonic acid metabolism through the COX and microsomal PGE synthase-1 (mPGES-1). PGE2 is degraded by 15-hydroxyprostaglandin dehydrogenase (15-PGDH). The expression of COX-2 and mPGES-1, and in turn the production of PGE2, are up-regulated under inflammatory conditions [13]. A number of studies suggest that H2S can inhibit COX-2-dependent PGE2 production in humans and rodents [14, 15].
It has been shown that EP4 receptors activated by PGE2 are involved in the pathogenesis of many vascular diseases, including atherosclerosis [16], AAA [17] and varicose veins [10]. This occurs via the activation of MMP or through regulation of endogenous tissue inhibitors of MMPs (TIMP); EP4 and mPGES-1 expression was found to be lower in varicose veins [10] and greater in AAA [17, 18] compared to healthy vessels. Regulation of MMP/TIMP ratio by PGE2 could be responsible for the observed thickening of the vascular wall in varicose veins, and thinning of the structure in AAA.
The entire biological pathway linking H2S, PGE2 and extracellular matrix expression has never been investigated globally in human vessels. We therefore tested the hypothesis that endogenous H2S may modulate PGE2, MMP/TIMP ratio and ultimately control the remodeling of the vascular wall in different vascular pathologies, in human varicose saphenous veins and AAA.
Materials and Methods
Human vascular preparations
Human aorta (healthy and abdominal aneurysm)
All experiments with human subjects were performed in accordance with the Helsinki Declaration of 1975, as revised in 1983. Seventeen healthy aortas (HA; 10 males and 7 females, aged 56 ± 6 years) were sampled either from cardiac transplantation surgery or organ donors with the authorization of the French Biomedicine Agency (PFS 09–007). Seventeen AAA samples (14 males and 3 females, aged 67 ± 2 years) were obtained from patients undergoing surgery, enrolled in the RESAA protocol [19] (REflet Sanguin de l’evolutivité des Anévrismes de l’Aorte abdominale, Comité Consultatif de Protection des Personnes dans la Recherche Biomédicale, CCPRB Paris-Cochin, approval no 2095). All the aorta samples were without thrombus (luminal layer, at the interface with circulating blood), and adventitia was removed. All patients gave informed written consent and the protocol was approved by a French ethics committee (CPB Paris-Cochin, approval no. 2095, France).
Human saphenous veins (healthy and varicose)
Twenty one healthy saphenous veins (SV) from patients undergoing coronary artery bypass surgery (11 males and 10 females, aged 67 ± 5 years) and 23 varicose saphenous veins from patients undergoing vein stripping (11 males and 12 females, aged 61 ± 6 years) were obtained at Bichat Hospital (Paris, France). The varicose veins were obtained from patients at the clinical stage C2 of the disease (CEAP classification of chronic venous disease [20]) without inflammation [21]. Pre-operative evaluation of the vein condition showed retrograde flow but no presence of edema or ulcer. Furthermore, these vessels presented histological features of varicose veins as previously described [20]. All tissues were obtained after patients’ written informed consent. Research programs involving the use of human tissues are supported by the National Institute for Health and Medical Research (INSERM) ethics committee and approved by the French ethics law (L.1211-3–L.1211-9).
After the surgical procedure, the vessels were rapidly transported to the laboratory in ice-cold saline. All tissues were processed within two hours of excision. They were cleaned of adipose tissue and blood, no trace of thrombosis was detectable. Healthy SV used in these experiments were of approximately 3 mm in internal diameter. The varicose veins segments were divided into small diameter varicosity group (SDv) and a large diameter varicosity group (LDv) of approximately 4 mm and 8 mm in internal diameter, respectively. Some fresh vascular samples were incubated for 24h for ELISA measurements (PG, TxB2, MMP-1 and TIMPs) or frozen for subsequent analyses (western blot analysis and H2S measurement).
Western blot analysis
Expressions of CSE and mPGES-1 proteins were detected by Western blot. After incubations, the tissue samples were ground in liquid nitrogen and homogenized in RIPA buffer as previously described [21]. Following 15 min of centrifugation at 4500 g, the supernatants were collected and stored at -20°C. Proteins were quantified using a bicinchoninic acid assay kit (ThermoScientific, Rockford, IL, USA). Fifty micrograms of tissue proteins and Western ready controls (CSE ready control from Santa Cruz biotechnology, CA, USA; mPGES-1 ready control from Cayman, Ann Arbour, MI, USA) were submitted to SDS-PAGE and transferred on PVDF membranes. After blocking with PBS 0.5% Tween-20/5% dry milk for 1h, the membranes were probes with a primary antibody, rinsed 3 times for 5 min in PBS /0.5% Tween-20 and incubated with an anti-mouse/rabbit antibody coupled to HRP for 1h (Jackson Immuno Research, West Grove, PA, USA; 1/20,000 dilution). Western blots were revealed by ECL prime (Amersham Biosciences, Glattbrugg, Switzerland). The protein expressions were normalised to beta-actin. The following antibodies were used: CSE (Santa Cruz, 1/5000), mPGES-1 (Oxford Biomedical Research, Oxford, MI, USA; 1/1000), beta-actin (Sigma-Aldrich, Saint-Quentin Fallavier, France; 1/5000).
Polarographic measurement of hydrogen sulfide production
Endogenous H2S production was measured using a polarographic sensor (ISO-H2S-2, WPI) together with an Apollo 1000 free radical analyser (WPI) [22]. The sensor was regularly calibrated with freshly prepared NaHS stock solution using the same buffer and conditions as the experiment. Entire tissue specimens were preincubated for 1 hour at room temperature in 4 ml RPMI solution. Specimens were subsequently placed in the polarographic sensor for a 30 minutes equilibration period in the presence or absence of the CSE inhibitor β cyano-L-alanine at 1 mmol/L (BCA, Cayman, CA, USA). After the equilibration period, L-cysteine was added at incremental concentrations (10 μmol/L, 100 μmol/L, 1 mmol/L, Sigma) every 6–8 min when a plateau was obtained. For basal level of H2S measurement, the polarographic sensor was placed alone for equilibration. After 30 minutes, tissues were placed with the sensor for 30 minutes.
Measurement of prostanoid (PGE2, TxB2, 15d-PGJ2), MMP and TIMP concentrations
Fresh tissue specimens were incubated in RPMI solution (Gibco Invitrogen, Paisley, UK; 166 mg wet weight tissue / mL solution for aorta samples, 70 mg wet weight tissue / mL solution for saphenous vein samples) with 5% CO2 for 24h in the absence or presence of NaHS (10 μmol/L, 100 μmol/L, 1 mmol/L, 10 mmol/L; Cayman), of the CSE inhibitor β-cyano-L-alanine (BCA, 10 μmol/L, 100 μmol/L, 1 mmol/L), of PGE2 (10 μmol/L, Cayman) or of EP4 receptor antagonist GW627368X (1 μmol/L, Cayman). Incubations with different pharmacological treatments were performed only in venous preparations due to the limited access to aorta samples. RPMI solution always contained antibiotics (penicillin, 1000 IU/mL; streptomycin, 100 μg/mL) and the antimycotic amphotericin (0.25 μg/mL). Supernatants were harvested and frozen until used. The concentrations of PGE2, TxB2 (stable metabolite of TxA2), 15d-PGJ2 (stable metabolite of PGD2) (Cayman, EIA kits) and MMP/TIMP (DuoSet, R&D systems, Minneapolis, MN, USA, ELISA kits) were measured using an enzyme immunoassay kit according to the manufacturer’s instructions. Results were expressed in pg or ng of tissue wet weight. The concentrations of active MMP-1 were calculated from the measurement of human pro-MMP-1 and total (free and complexed) human MMP-1 using 2 different kits. TIMP-1 and TIMP-2 concentrations were measured using 2 different kits, which recognize the total human TIMP-1 and -2 (free and complexed with MMPs), respectively. Total MMP-2 and MMP-9 (free and complexed) content were quantified by using 2 different kits.
Data analysis
For protein expression analysis by Western blotting, the optical density (OD) of each band was quantitated from the films using a Scion Image® imaging system. The protein expression detected was normalised to β-actin. For EIA/ELISA measurements, normalisation was performed by correcting for tissue wet weight.
Statistical analysis was performed using the program SigmaStat® (Systat Software, IL, USA). All data are presented as means ± sem derived from (n) patients. Statistical analysis was performed using a two-way ANOVA followed by Bonferroni post-hoc test or a paired t-test between SDv and LDv. P-value<0.05 indicates a statistically significant difference between the compared values. However, in few protocols, when a small number of samples have been used, the results should be taken cautiously.
Results
Content of CSE in the saphenous vein and abdominal aorta (healthy and pathological)
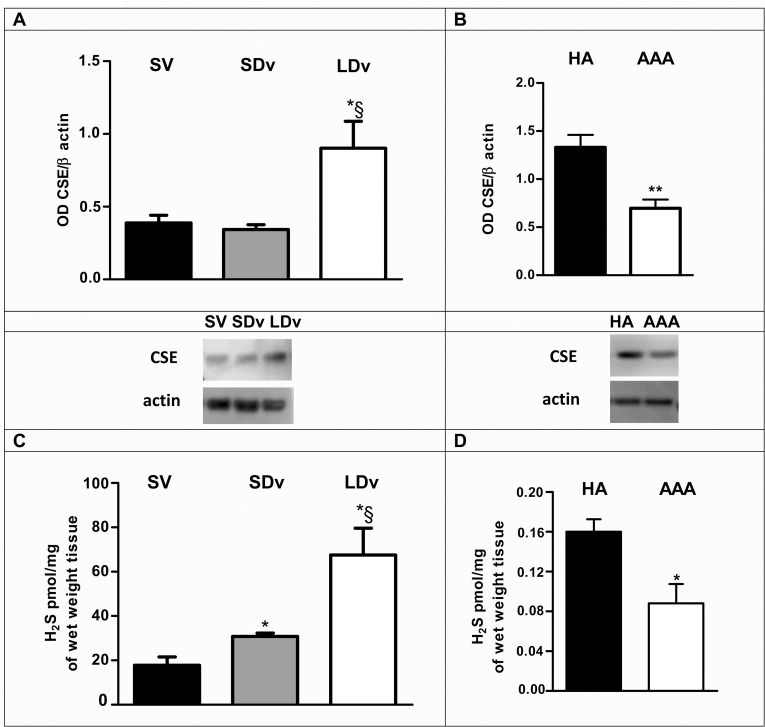
CSE protein corresponding to a 44 kDa band, was found in all vascular homogenates, in SV, in varicose veins (SDv and LDv, Fig 1A), in healthy and pathological aortas (Fig 1B). A significant increase of CSE expression was observed in the LDv samples as compared to SDv and healthy SV. On the contrary, a significant decrease was found in AAA when compared with HA.
Fig 1. CSE expression and H2S production in saphenous veins and abdominal aortas (healthy and pathological).
Western blot quantification and representative images of cystathionine-γ-lyase (CSE) normalized to β-actin are shown: (A) in healthy saphenous veins (SV, n = 4), in small (SDv) and large diameter (LDv) varicosities (paired n = 4); (B) in healthy aortas (HA, n = 5) and abdominal aortic aneurysms (AAA, n = 5). Basal production of hydrogen sulfide (H2S) (C) by healthy SV (n = 4), varicose veins (SDv and LDv, paired n = 4) and (D) by HA (n = 5) and AAA (n = 5) are shown. *P<0.05 versus healthy vessels and §P<0.05 between SDv and LDv.
H2S production is increased in varicose veins and decreased in AAA
A progressive and significant increase in basal H2S production was observed in varicose veins as compared to healthy SV (n = 4; Fig 1C). On the contrary, basal H2S production by the media derived from AAA preparations was found significantly lower in comparison to HA (n = 5; Fig 1D).
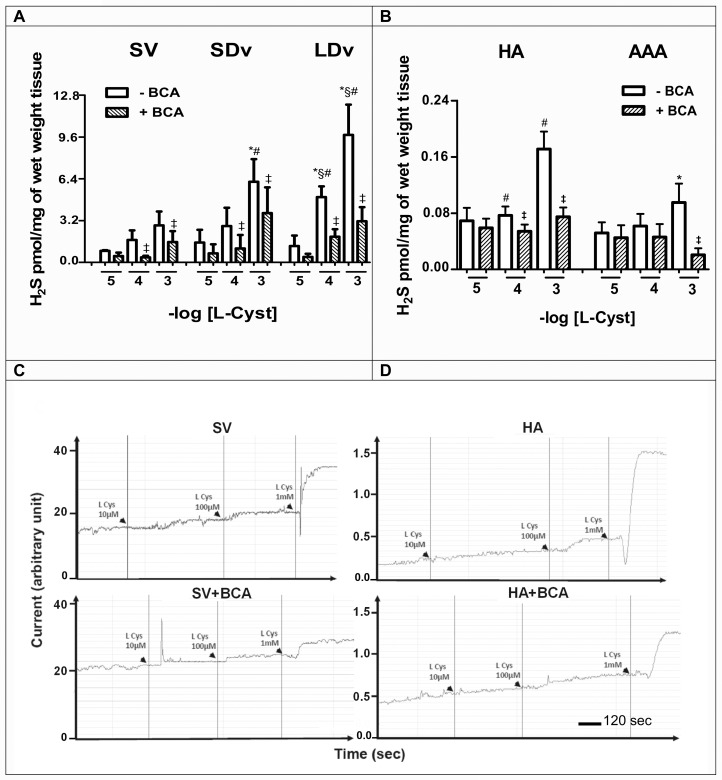
Production of H2S following L-cysteine addition in healthy and pathological preparations
In all vessels studied, a concentration-dependent production of H2S was measured after stimulation with increasing concentrations of L-cysteine (10−5–10−3 mol/L); these productions were significantly inhibited in the presence of the CSE inhibitor, BCA (1 mmol/L; Fig 2). L-cysteine addition resulted in a significant increase of H2S production in LDv as compared to SDv (n = 4) and healthy SV (n = 4; Fig 2A and 2C). On the contrary, H2S production was significantly lower in AAA preparations versus HA after addition of L-cysteine (1 mmol/L; n = 5–6; Fig 2B and 2D).
Fig 2. H2S production after L-cysteine addition in saphenous veins and abdominal aortas (healthy and pathological).
L-cysteine (10−5–10−3 mol/L) was added in the presence or absence of β-cyano-L-alanine (BCA, 1 mmol/L) in (A) healthy saphenous veins (SV, n = 4), small and large diameter varicosities (paired SDv and LDv, n = 4), (B) healthy aortas (HA, n = 5) and abdominal aortic aneurysms (AAA, n = 5). *P<0.05 versus healthy vessels or §P<0.05 versus SDv treated with the same concentration of L-Cyst; #P<0.05 versus L-cysteine 10 μmol/L or ‡P<0.05 versus absence of BCA in respective vessels. (C, D) Representative traces of production of H2S after L-cysteine addition in the presence or absence of BCA in healthy SV and HA using a polarographic sensor.
Variable expression of mPGES-1 in SV and in aorta
mPGES-1 protein corresponding to a 16 kDa band, was found in homogenates of healthy SV (n = 4). A significant decrease of mPGES-1 expression was observed in the healthy SV after 24h incubation with NaHS (10−5 and 10−4 mol/L; Fig 3A). mPGES-1 protein was also found in homogenates of healthy aorta (HA, n = 5) and abdominal aortic aneurysm (AAA, n = 5). A significant increase of mPGES-1 expression was observed in the AAA when compared to HA (Fig 3B).
Fig 3. mPGES-1 expression and PGE2 production are regulated by H2S.
Western blot quantifications of microsomal prostaglandin E synthase-1 expression (mPGES-1; normalized to β actin) and representative images are presented. In (A) healthy SV untreated (Ct, black bar) or treated (white bars) with NaHS (10−5 and 10−4 mol/L, 24h, n = 4), in (B) healthy aortas (HA, n = 5) and abdominal aneurysmal aortas (AAA, n = 5). PGE2 content (C) in healthy saphenous veins (SV, n = 14), in small and large diameter varicosities (paired SDv and LDv, n = 14), in (D) healthy aorta (HA, n = 3) and abdominal aortic aneurysm (AAA, n = 3) preparations. PGE2 concentrations were measured by EIA after 24h incubation with or without the treatments indicated: NaHS (10−5–10−2 mol/L, n = 4–5) or CSE inhibitor β-cyano-L-alanine (BCA, 10−5–10−3 mol/L, n = 4–5). *P<0.05, ****P<0.0001 versus respective untreated healthy vessels without treatment; §P<0.05 between SDv and LDv; #P<0.05 versus respective control.
PGE2 production is decreased in varicose veins and increased in AAA
A progressive and significant decrease in PGE2 concentrations in varicose veins (SDv and LDv; n = 14) and a significant increase in AAA preparations (n = 3) were observed in comparison to healthy vessels after 24h incubation (Fig 3C and 3D).
PGE2 production is regulated by H2S
After 24h incubation, NaHS (10−5–10−2 mol/L) significantly decreased PGE2 levels in healthy SV (n = 4) and varicose veins (n = 5). In contrast, incubation of varicose veins with BCA (10−5–10−3 mol/L) reversed significantly the effects of endogenous H2S on PGE2 (Fig 3C).
TxB2 and 15d-PGJ2 productions are not regulated by H2S
A significant increase in TxA2 and PGD2 stable metabolites (TxB2 and 15d-PGJ2, respectively) productions in LDv (n = 5–11) was found compared to healthy SV and SDv. After incubation with NaHS (10−5–10−2 mol/L; n = 4) or BCA (10−5–10−3 mol/L; n = 4) for 24h, no effect on TxB2 or 15d-PGJ2 release was detected in both healthy SV and varicose veins (Fig 4A and 4B).
Fig 4. TxB2 and 15d-PGJ2 productions are not regulated by H2S.
TxB2 (A) and 15d-PGJ2 (B) contents in healthy saphenous veins (SV, n = 4–10) and small and large diameter varicosities (paired SDv and LDv, n = 5–11) were measured by EIA after 24h incubation. Values are normalized by tissue wet weight. Treatments with NaHS (10−5–10−2 mol/L) and CSE inhibitor β-cyano-L-alanine (BCA, 10−5–10−3 mol/L) are presented. Ct indicates the respective untreated preparations. *P<0.05 versus healthy SV without treatment. §P<0.05 between SDv and LDv.
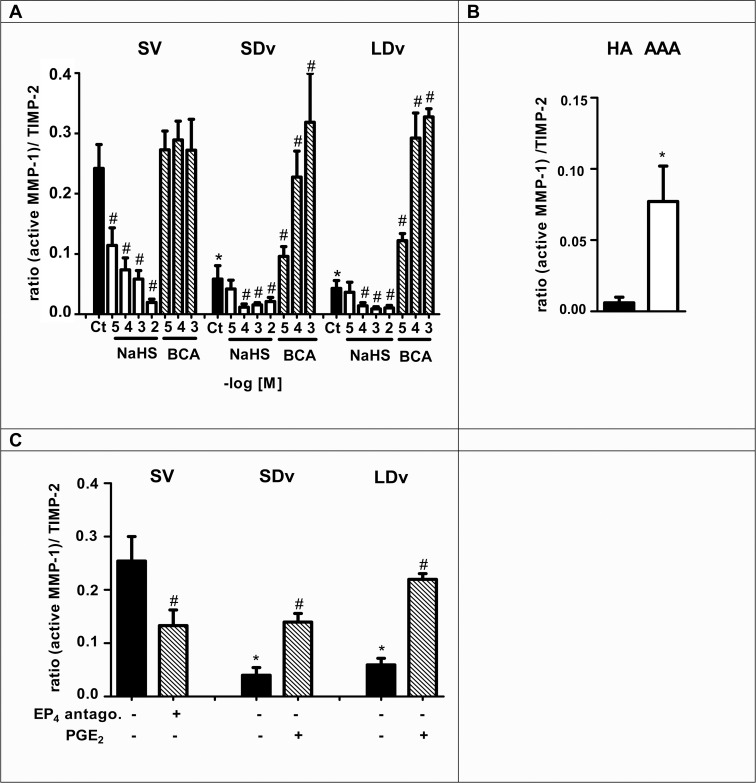
Active MMP-1/TIMPs ratios are decreased in varicose veins and increased in AAA
Measurement of active MMP-1, TIMP-1 and TIMP-2 presented Tables 1 and 2 were performed in the same samples used for PGE2 measurements after 24h incubation. Increased active MMP-1 levels and decreased TIMP-2 levels were found in AAA preparations compared to HA (Table 2), while exactly the reverse was observed when healthy and varicose veins were compared (Table 1). The ratio of (active MMP-1)/TIMP-1 and (active MMP-1)/TIMP-2 were significantly decreased in varicose veins (n = 6, Fig 5A and 5C and Fig 6A and 6C) and increased in AAA preparations (n = 6–7, Figs 5B and 6B) as compared with their respective healthy vessels (n = 4–5).
Table 1. Active MMP-1 and TIMP release from SV, SDv and LDv.
| Active MMP-1 | TIMP-1 | TIMP-2 | |
|---|---|---|---|
| Tissue | ng/mg of wet weight tissue | ng/mg of wet weight tissue | ng/mg of wet weight tissue |
| Healthy SV (n = 15) | 0.057 ± 0.006 | 0.623 ± 0.089 | 0.231 ± 0.003 |
| SDv (n = 16) | 0.017 ± 0.003* | 1.130 ± 0.035* | 0.351 ± 0.028* |
| LDv (n = 16) | 0.016 ± 0.002* | 1.665 ± 0.078*† | 0.308 ± 0.017* |
MMP: matrix metalloproteinase, TIMP: tissue inhibitor of matrix metalloproteinases, SV: saphenous vein, SDv: small diameter varicosity, LDv: large diameter varicosity.
*P<0.05 versus healthy vessels and
† P<0.05 between SDv and LDv
Table 2. Active MMP-1 and TIMP release from HA and AAA.
| Active MMP-1 | TIMP-1 | TIMP-2 | |
|---|---|---|---|
| Tissue | pg/mg of wet weight tissue | ng/mg of wet weight tissue | ng/mg of wet weight tissue |
| HA (n = 5) | 1.24± 0.67 | 0.41 ± 0.07 | 0.16 ± 0.02 |
| AAA (n = 7) | 6.62±1.71* | 0.44± 0.08 | 0.10 ± 0.06* |
MMP: matrix metalloproteinase, TIMP: tissue inhibitor of matrix metalloproteinases, HA: healthy aorta, AAA: abdominal aortic aneurysm.
*P<0.05 versus healthy vessels
Fig 5. H2S is responsible for decreased active MMP-1/TIMP-1 ratio.
This ratio was calculated after measurement of active MMP-1 and TIMP-1 contents in healthy saphenous veins (SV, n = 5), small and large diameter varicosities (paired SDv and LDv, n = 6), healthy aortas (HA, n = 5) and abdominal aortic aneurysms (AAA, n = 6–7) by EIA after 24h incubation. MMP-1 and TIMP-1 contents have been normalized by tissue wet weight and ratios are expressed into arbitrary unit. (A-B) Treatments with NaHS (10−5–10−2 mol/L, n = 4–5) or CSE inhibitor β-cyano-L-alanine (BCA, 10−5–10−3 mol/L, n = 4) are presented. Ct indicates the respective control preparations without treatment. (C) PGE2 is responsible for active MMP-1/TIMP-1 ratio regulation (n = 4–5). Healthy SV were treated with an EP4 antagonist (GW627368X, 1 μmol/L, 24h), SDv and LDv were treated with PGE2 (10 μmol/L, 24h). *P<0.05 versus respective healthy vessel; §P<0.05 between SDv and LDv; #P<0.05 versus respective vessel without treatment.
Fig 6. H2S is responsible for decreased active MMP-1/TIMP-2 ratio.
This ratio was calculated after measurement of active MMP-1 and TIMP-2 contents in healthy saphenous veins (SV, n = 4), small and large diameter varicosities (paired SDv and LDv, n = 5), healthy aortas (HA, n = 5) and aneurysmal aortas (AAA, n = 7) by EIA after 24h incubation. MMP-1 and TIMP-2 contents have been normalized by tissue wet weight and ratios are expressed into arbitrary unit. (A-B) Treatments with NaHS (10−5–10−2 mol/L, n = 3–4) or CSE inhibitor β-cyano-L-alanine (BCA, 10−5–10−3 mol/L, n = 4) are presented. Ct indicates the respective control preparations without treatment. (C) PGE2 is responsible for active MMP-1/TIMP-2 ratio regulation (n = 4–5). Healthy SV were treated with an EP4 antagonist (GW627368X, 1 μmol/L, 24h), SDv and LDv were treated with PGE2 (10 μmol/L, 24h). *P<0.05 versus respective healthy vessel; #P<0.05 versus respective vessel without treatment.
H2S is responsible for decreased (active MMP-1)/TIMP ratio
Exogenous H2S led to a significant decrease in active MMP-1/TIMP-1 and MMP-1/TIMP-2 ratios in all segments (n = 4–5). Inhibition of endogenous H2S production with BCA induced a significant increase of both ratios in varicose veins versus untreated varicose veins (Figs 5A and 6A).
PGE2 is responsible for increased active MMP-1/TIMP ratio
Exogenous PGE2 (10 μmol/L) led to a significant increase of active MMP-1/TIMP-1 ratio (Fig 5C) and active MMP-1/TIMP-2 ratio in varicose veins (n = 5, Fig 6C). The EP4 antagonist (GW627368X, 1 μmol/L) decreased significantly both ratios in healthy SV by inhibiting endogenous PGE2 effect (Figs 5C and 6C).
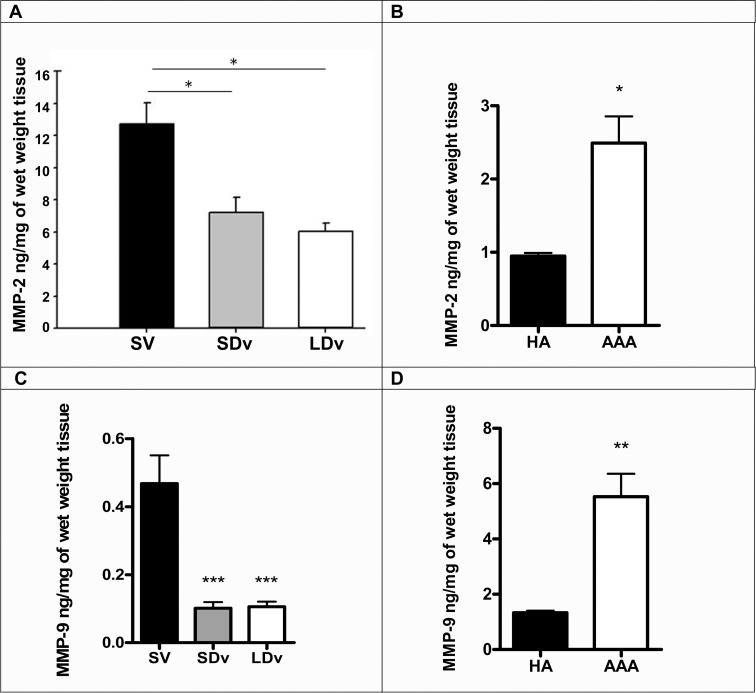
MMP-2 and -9 are decreased in varicose veins and increased in AAA
Measurement of total MMP-2 and MMP-9 were performed after 24h incubation. Increased total MMP-2 and -9 levels levels were found in AAA preparations compared to HA (Fig 7B and 7D), while exactly the reverse was observed when healthy and varicose veins were compared (Fig 7A and 7C).
Fig 7. MMP-2 and -9 are decreased in varicose veins and increased in AAA.
Measurement of total MMP-2 (A-B) and MMP-9 (C-D) contents in healthy saphenous veins (SV, n = 5), small and large diameter varicosities (paired SDv and LDv, n = 6), healthy aortas (HA, n = 7) and abdominal aortic aneurysms (AAA, n = 7) by EIA after 24h incubation. MMP-2 and MMP-9 contents have been normalized by tissue wet weight *P<0.05 and **P<0.01 versus respective healthy vessel.
Discussion
Our results demonstrate that in healthy and pathological human vessels H2S and PGE2 modulate MMPs involved in vascular wall remodeling. In varicose veins, the increased CSE expression and consequently the increased H2S production are responsible for the reduced PGE2 content and the reduced MMP/TIMP ratios. In contrast, in medias of AAA, we show a similar cascade of biological events but with a reverse regulation. In consequence, these H2S/PGE2 regulations are associated with changes in MMP/TIMP ratio and consequently in vascular wall thickening in varicose veins or thinning in AAA.
Varicose veins
In the present report, H2S production was increased in all varicose veins. This is supported by the measurements of CSE content and H2S productions in basal conditions or after addition of the CSE substrate (L-Cystein; Figs 1A, 1C and 2A). In addition, the selective CSE inhibitor BCA reduced at least by 50% these responses (Fig 2A) suggesting that H2S could also be produced by other enzymes such as cystathionine beta-synthase (CBS) or mercaptopyruvate sulfurtransferase (3-MST) [23].
In the present study, as in our previous report [10], a progressive and significant decrease of PGE2 production was observed in varicose veins versus healthy saphenous veins. These new measurements are due to lower mPGES-1 expression in the pathological veins [10]. This decreased expression of mPGES-1 in varicose veins is associated with increased expression of CSE and H2S production (Fig 1A and 1C).
Now we show that when venous preparations are incubated with NaHS, mPGES-1 expression and PGE2 production are significantly decreased (Fig 3A and 3C). In varicose veins, incubation with BCA restored PGE2 content to a level similar to that observed in healthy saphenous veins (Fig 3C). Together these results suggest that endogenous or exogenous H2S controls PGE2 release in human saphenous vein while other prostanoids release, such as PGD2 or TxA2, was not affected (Fig 4A and 4B) suggesting that H2S could only effect mPGES-1 expression. The increased levels of PGD2 and TxA2 (measured by their stable metabolites Fig 4) in varicose veins could be due to increased expression of COX-1 [10]. Previously, it has been shown that a H2S donor caused a decrease in COX-2 expression and consequently PGE2 levels in human keratinocytes and chondrocytes in inflammatory conditions [24, 25]. More recently, Burguera et al. (2014) have demonstrated that H2S donors cause a decrease in PGE2 levels by downregulating both COX-2 and mPGES-1 mRNA in interleukin-1beta (IL1β)-stimulated human chondrocytes [14]. Our results are consistent with these previously published results and extend them to the human vascular field.
Even if the pathogenesis of varicose veins is poorly understood, the vascular wall remodeling has been analysed by various studies [26, 27]. Those studies have shown a dysregulation in MMP activities in varicose veins compared to healthy SV. These activities are dependent on MMP activation and concentration of their endogenous inhibitors (TIMP). Increased collagen content has been shown in varicose vein pathology [10], for this reason active collagenase MMP-1 was measured in the present study and we have calculated the active MMP-1/TIMP-1 and MMP-1/TIMP-2 ratios (Figs 5A and 6A). Decreased ratios have been found to correlate with increased collagen content of the venous wall as quantified in our previous report [10]. This result is also supported by the reduced quantities of MMP-2 and -9 measured in varicose veins (Fig 7A and 7C). Furthermore, our pharmacological studies (Figs 5 and 6) show that there is a similar decrease of MMP-1/TIMP ratio after incubation of the healthy saphenous veins with either H2S donor or an EP4 antagonist. Conversely, the reduced MMP-1/TIMP ratio measured in varicose veins could be restored (completely or over 50% of the level in healthy saphenous veins), following treatment with a H2S synthesis inhibitor or PGE2.
Several reports are in accordance with our results obtained in human varicose veins (Table 3). Talaei et al. (2012) showed an inhibitory effect of endogenous H2S synthesis on MMP activities (MMP-2, MMP-9) in hamster lung during hibernation [28]. In this study, decreased MMP activity was associated with increased collagen deposition. The H2S donors Diallyl(di)sulfide also reduces MMP-2 and MMP-9 activities in human LNCaP prostate cancer cells [29] and in an animal model of lung fibrosis [11]. Similar mechanism could explain the significant decreases of MMP-2 and -9 observed in varicose veins (Fig 7A and 7C). Reversely, in mice cardiac tissues obtained following myocardial infarction, the observed decrease in CSE expression was associated with an increase in MMPs [30]. Other studies have also demonstrated that exogenous H2S sources (NaHS) led to reduction of MMP-13 and/or MMP-8 levels in human chondrocytes under inflammatory conditions [14] and in a model of rat heart disease [31].
Table 3. Reverse regulatory pathway (H2S / PGE2 / MMP) in different pathologies.
| CSE | H2S | mPGES-1 | PGE2 | 15-PGDH | EP4 | MMP | Collagen Elastin | Consequence on vascular wall | |
|---|---|---|---|---|---|---|---|---|---|
| Varicose Vein | + * | + * | - [10] | - [10] | + [10] | - [10] | - (MMP-1, -2 [10]; MMP-9 *) | + Collagen [10] | Thickness [32] |
| Pulmonary hypertension | + [33] | + [33] | - [34] | + [35] | + Collagen [7] | Thickness [35] | |||
| AAA | - * | - * | + [18] | + [18, 36, 37] | + [17, 18] | + (MMP-2 [17]; MMP-1, -9 * | - Elastin [17] | Thinness [38] | |
| Atherosclerosis | - [1] | - [6] | + [16, 39] | + [39] | + [39] | + MMP-1 [40] | - Collagen [40] | Thinness [41, 42] of fibrous cap or media |
*Results presented in this manuscript. AAA: abdominal aortic aneurysm, CSE: Cystathionine-γ-lyase, mPGES-1: microsomal PGE synthase-1, 15-PGDH: 15-hydroxyprostaglandin dehydrogenase, MMP: matrix metalloproteinases. (+) indicates increase and (-) decrease of expression or density of the molecules.
A similar regulation of collagen accumulation has been observed by Li et al (2007, 2009) who demonstrated that increased CSE and endogenous H2S levels in lung tissues of pulmonary hypertensive rat were correlated with increased collagen I and III levels [7, 33]. Thus, the down-regulation of MMP activities by endogenous H2S production should increase vascular wall thickness. However, the consequences of MMP regulation are not always negatively correlated to collagen production, some authors showed positive correlations [11, 30] however, these findings are difficult to interpret.
Taken together, these results demonstrate a clear regulatory pathway: high levels of endogenous H2S induce a decrease of mPGES-1 expression and PGE2 concentration which reduces MMP/TIMP ratio via EP4 receptor activation. This could result in the accumulation of collagen and thickening of vascular wall as it is described either in pulmonary hypertension or in varicose veins (Table 3). Our results support a vasculoprotective role for H2S as suggested by a clinical study (thermal hydrotherapy) with sulphurous water in patients with varicose veins [43]. In this treatment, H2S has an analgesic effect [44] possibly by reducing PGE2 content. However, additionally H2S may strengthen the varicose wall by increasing collagen content and so restrain the blood stasis.
Abdominal aortic aneurysm
To our knowledge, there is currently no evidence regarding H2S production and its role in AAA. Studies concerning the effects of H2S in human aorta smooth muscle cells (HASMC) suggest that overexpression of CSE stimulates apoptosis due to an increased endogenous production of H2S [45]. Furthermore, H2S induces hyperpolarization of HASMC and is responsible for relaxation of rat aorta [46].
Our results show for the first time a lower endogenous H2S production in AAA compared to HA preparations correlated with a decrease of CSE content (Figs 1B and 1D, 2B and 2D). This reduction was partly due to a reduced CSE activity, since it increased after addition of the substrate of CSE (L-cysteine) and was inhibited by a CSE inhibitor (Fig 2D). This reduction in H2S production was associated with increased mPGES-1 content and PGE2 synthesis in AAA as compared to HA preparations (Fig 3B and 3D). In accordance with our results, PGE2 involvement in the pathogenesis of AAA was observed by other groups [36, 37]. Camacho et al. (2013) showed that mPGES-1/PGE2/EP4 axis was up-regulated in human AAA [18]. All these data also are consistent with studies showing that inhibition of mPGES-1 or EP4 expression reduced AAA formation in animal models [47, 48]. Taken together, we suggest a new additional level of regulation of the PGE2 pathway by H2S in AAA when compared to HA preparations.
We measured active MMP-1 since our study focused on collagen degradation which is required for AAA evolution, even if elastolytic enzymes are important in initiating AAA. The present report shows increased active MMP-1/TIMP-1 and active MMP-1/TIMP-2 ratios in AAA compared to HA. Similarly total MMP-2 and MMP-9 were also increased in AAA. It has been demonstrated that EP4 activation by PGE2 is responsible for activation of MMP-2 in human AAA [17]. This activation is in correlation with our data and the increase of total MMP-2 content in AAA (Fig 7B). Yokoyama and coworkers show that this regulation is responsible for decreased elastin levels observed in AAA. This result is in accordance with increased levels of elastin observed in aorta of EP4 knock-out mice and with the negative correlation between EP4 expression versus elastic fiber formation in human AAA preparations [17].
For these reasons, the thinning of human AAA wall may be linked to a reduction in H2S production that up-regulates the mPGES-1/PGE2/EP4/MMP axis, a reversal of the regulatory processes that result in wall thickening in varicose veins and pulmonary hypertension as previously described.
Our results suggest a clear, common regulatory pathway for the vascular wall remodeling in human AAA and varicose vein pathogenesis. This control is also described in the literature for other vascular pathologies such as atherosclerosis or pulmonary hypertension (see Table 3). This pathway starts from endogenous H2S production and regulates in fine the collagen content/degradation via intermediary modulation of PGE2 and MMP metabolisms. As supported by the literature, the mechanistic behind the effect induced by H2S is more probably associated with molecules such as IL-1b and NF-kB. A microarray hybridation study showed that the NF-kB pathway is reversely regulated in human artery and saphenous vein, after OxLDL stimulation [49]. H2S protects human H9c2 cardiac cells against high glucose-induced inflammation or against chemical hypoxia-induced injuries, by inhibiting the NF-κB/IL-1β pathway [25, 50]. This down-regulation has been correlated with a decrease of mPGES-1 expression and/or PGE2 synthesis in atherosclerotic plaques derived from diabetic patients treated with simvastatin and also in H9c2 cardiac cells [25, 51]. Furthermore, since H2S production is intertwined to oxygen partial pressure [2], H2S synthesis will depend on the vascular bed and/or the physiopathological state of the vascular wall. In consequence, high or low level of local H2S synthesis will result either in thickening (varicose vein) or thinning (aneurysmal aorta) of the vascular wall, respectively.
Acknowledgments
We would like to thanks Tariya Zaoui (CHU X. Bichat; Paris, France) for her help in obtaining the vascular preparations and Dr Mary Osborne-Pellegrin and Ben Ward, MSc (Infection, Immunity and Cardiovascular Science, University of Sheffield, UK) for his help in editing the manuscript. This work was supported by INSERM (Institut National de la Santé et de la Recherche Médicale). Gulsev Ozen is a recipient of a postgraduate fellowship (BIDEB-2214) from the Scientific and Technological Research Council of Turkey (TUBITAK). Ingrid Gomez was supported by a PhD grant from Paris 13 University.
Data Availability
All relevant data are within the paper.
Funding Statement
This work was supported by INSERM (Institut National de la Santé et de la Recherche Médicale). Gulsev Ozen is a recipient of a postgraduate fellowship (BIDEB-2214) from the Scientific and Technological Research Council of Turkey (TUBITAK). Ingrid Gomez was supported by a PhD grant from Paris 13 University. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Mani S, Li H, Untereiner A, Wu L, Yang G, Austin RC, et al. Decreased endogenous production of hydrogen sulfide accelerates atherosclerosis. Circulation. 2013;127(25):2523–34. Epub 2013/05/25. 10.1161/CIRCULATIONAHA.113.002208 CIRCULATIONAHA.113.002208 [pii]. . [DOI] [PubMed] [Google Scholar]
- 2.Olson KR. Hydrogen sulfide as an oxygen sensor. Antioxid Redox Signal. 2015;22(5):377–97. Epub 2014/05/08. 10.1089/ars.2014.5930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al-Magableh MR, Kemp-Harper BK, Hart JL. Hydrogen sulfide treatment reduces blood pressure and oxidative stress in angiotensin II-induced hypertensive mice. Hypertens Res. 2015;38(1):13–20. Epub 2014/08/08. 10.1038/hr.2014.125 hr2014125 [pii]. . [DOI] [PubMed] [Google Scholar]
- 4.Webb GD, Lim LH, Oh VM, Yeo SB, Cheong YP, Ali MY, et al. Contractile and vasorelaxant effects of hydrogen sulfide and its biosynthesis in the human internal mammary artery. J Pharmacol Exp Ther. 2008;324(2):876–82. Epub 2007/11/22. jpet.107.133538 [pii] 10.1124/jpet.107.133538 . [DOI] [PubMed] [Google Scholar]
- 5.Beltowski J, Jamroz-Wisniewska A. Hydrogen sulfide and endothelium-dependent vasorelaxation. Molecules. 2014;19(12):21183–99. Epub 2014/12/19. 10.3390/molecules191221183 molecules191221183 [pii]. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang Y, Zhao X, Jin H, Wei H, Li W, Bu D, et al. Role of hydrogen sulfide in the development of atherosclerotic lesions in apolipoprotein E knockout mice. Arterioscler Thromb Vasc Biol. 2009;29(2):173–9. Epub 2008/11/08. 10.1161/ATVBAHA.108.179333 ATVBAHA.108.179333 [pii]. . [DOI] [PubMed] [Google Scholar]
- 7.Li X, Jin H, Bin G, Wang L, Tang C, Du J. Endogenous hydrogen sulfide regulates pulmonary artery collagen remodeling in rats with high pulmonary blood flow. Exp Biol Med (Maywood). 2009;234(5):504–12. Epub 2009/02/24. 10.3181/0807-RM-230 0807-RM-230 [pii]. . [DOI] [PubMed] [Google Scholar]
- 8.Annabi B, Shedid D, Ghosn P, Kenigsberg RL, Desrosiers RR, Bojanowski MW, et al. Differential regulation of matrix metalloproteinase activities in abdominal aortic aneurysms. J Vasc Surg. 2002;35(3):539–46. Epub 2002/03/06. S0741521402122609 [pii]. . [DOI] [PubMed] [Google Scholar]
- 9.Benjamin MM, Khalil RA. Matrix metalloproteinase inhibitors as investigative tools in the pathogenesis and management of vascular disease. EXS. 2012;103:209–79. Epub 2012/05/31. 10.1007/978-3-0348-0364-9_7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gomez I, Benyahia C, Louedec L, Leseche G, Jacob MP, Longrois D, et al. Decreased PGE(2) content reduces MMP-1 activity and consequently increases collagen density in human varicose vein. PLoS One. 2014;9(2):e88021 Epub 2014/02/08. 10.1371/journal.pone.0088021 PONE-D-13-37666 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kalayarasan S, Sriram N, Soumyakrishnan S, Sudhandiran G. Diallylsulfide attenuates excessive collagen production and apoptosis in a rat model of bleomycin induced pulmonary fibrosis through the involvement of protease activated receptor-2. Toxicol Appl Pharmacol. 2013;271(2):184–95. Epub 2013/05/10. 10.1016/j.taap.2013.04.021 S0041-008X(13)00176-2 [pii]. . [DOI] [PubMed] [Google Scholar]
- 12.Tyagi N, Givvimani S, Qipshidze N, Kundu S, Kapoor S, Vacek JC, et al. Hydrogen sulfide mitigates matrix metalloproteinase-9 activity and neurovascular permeability in hyperhomocysteinemic mice. Neurochem Int. 2010;56(2):301–7. Epub 2009/11/17. 10.1016/j.neuint.2009.11.002 S0197-0186(09)00305-2 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Samuelsson B, Morgenstern R, Jakobsson PJ. Membrane prostaglandin E synthase-1: a novel therapeutic target. Pharmacol Rev. 2007;59(3):207–24. Epub 2007/09/20. 59/3/207 [pii] 10.1124/pr.59.3.1 . [DOI] [PubMed] [Google Scholar]
- 14.Burguera EF, Vela-Anero A, Magalhaes J, Meijide-Failde R, Blanco FJ. Effect of hydrogen sulfide sources on inflammation and catabolic markers on interleukin 1beta-stimulated human articular chondrocytes. Osteoarthritis Cartilage. 2014;22(7):1026–35. Epub 2014/05/17. 10.1016/j.joca.2014.04.031 S1063-4584(14)01069-3 [pii]. . [DOI] [PubMed] [Google Scholar]
- 15.Du C, Jin M, Hong Y, Li Q, Wang XH, Xu JM, et al. Downregulation of cystathionine beta-synthase/hydrogen sulfide contributes to rotenone-induced microglia polarization toward M1 type. Biochem Biophys Res Commun. 2014;451(2):239–45. Epub 2014/08/03. 10.1016/j.bbrc.2014.07.107 S0006-291X(14)01356-4 [pii]. . [DOI] [PubMed] [Google Scholar]
- 16.Cipollone F, Prontera C, Pini B, Marini M, Fazia M, De Cesare D, et al. Overexpression of functionally coupled cyclooxygenase-2 and prostaglandin E synthase in symptomatic atherosclerotic plaques as a basis of prostaglandin E(2)-dependent plaque instability. Circulation. 2001;104(8):921–7. Epub 2001/08/22. . [DOI] [PubMed] [Google Scholar]
- 17.Yokoyama U, Ishiwata R, Jin MH, Kato Y, Suzuki O, Jin H, et al. Inhibition of EP4 signaling attenuates aortic aneurysm formation. PLoS One. 2012;7(5):e36724 Epub 2012/05/10. 10.1371/journal.pone.0036724 PONE-D-12-08789 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Camacho M, Dilme J, Sola-Villa D, Rodriguez C, Bellmunt S, Siguero L, et al. Microvascular COX-2/mPGES-1/EP-4 axis in human abdominal aortic aneurysm. J Lipid Res. 2013;54(12):3506–15. Epub 2013/10/18. 10.1194/jlr.M042481 jlr.M042481 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dejouvencel T, Feron D, Rossignol P, Sapoval M, Kauffmann C, Piot JM, et al. Hemorphin 7 reflects hemoglobin proteolysis in abdominal aortic aneurysm. Arterioscler Thromb Vasc Biol. 2010;30(2):269–75. Epub 2009/11/17. 10.1161/ATVBAHA.109.198309 ATVBAHA.109.198309 [pii]. . [DOI] [PubMed] [Google Scholar]
- 20.Bergan JJ, Schmid-Schonbein GW, Smith PD, Nicolaides AN, Boisseau MR, Eklof B. Chronic venous disease. N Engl J Med. 2006;355(5):488–98. Epub 2006/08/04. 355/5/488 [pii] 10.1056/NEJMra055289 . [DOI] [PubMed] [Google Scholar]
- 21.Gomez I, Benyahia C, Le Dall J, Payre C, Louedec L, Leseche G, et al. Absence of inflammatory conditions in human varicose saphenous veins. Inflamm Res. 2013;62(3):299–308. Epub 2012/12/15. 10.1007/s00011-012-0578-8 . [DOI] [PubMed] [Google Scholar]
- 22.Doeller JE, Isbell TS, Benavides G, Koenitzer J, Patel H, Patel RP, et al. Polarographic measurement of hydrogen sulfide production and consumption by mammalian tissues. Anal Biochem. 2005;341(1):40–51. Epub 2005/05/04. S0003-2697(05)00222-8 [pii] 10.1016/j.ab.2005.03.024 . [DOI] [PubMed] [Google Scholar]
- 23.Liu YH, Lu M, Hu LF, Wong PT, Webb GD, Bian JS. Hydrogen sulfide in the mammalian cardiovascular system. Antioxid Redox Signal. 2012;17(1):141–85. Epub 2012/02/07. 10.1089/ars.2011.4005 . [DOI] [PubMed] [Google Scholar]
- 24.Li L, Fox B, Keeble J, Salto-Tellez M, Winyard PG, Wood ME, et al. The complex effects of the slow-releasing hydrogen sulfide donor GYY4137 in a model of acute joint inflammation and in human cartilage cells. J Cell Mol Med. 2013;17(3):365–76. Epub 2013/01/30. 10.1111/jcmm.12016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang C, Yang Z, Zhang M, Dong Q, Wang X, Lan A, et al. Hydrogen sulfide protects against chemical hypoxia-induced cytotoxicity and inflammation in HaCaT cells through inhibition of ROS/NF-kappaB/COX-2 pathway. PLoS One. 2011;6(7):e21971 Epub 2011/07/23. 10.1371/journal.pone.0021971 PONE-D-11-04140 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Badier-Commander C, Verbeuren T, Lebard C, Michel JB, Jacob MP. Increased TIMP/MMP ratio in varicose veins: a possible explanation for extracellular matrix accumulation. J Pathol. 2000;192(1):105–12. Epub 2000/08/22. 10.1002/1096-9896(2000)9999:9999<::AID-PATH670>3.0.CO;2–1 [pii]. . [DOI] [PubMed] [Google Scholar]
- 27.Kucukguven A, Khalil RA. Matrix metalloproteinases as potential targets in the venous dilation associated with varicose veins. Curr Drug Targets. 2013;14(3):287–324. Epub 2013/01/16. CDT-EPUB-20130107-2 [pii]. [PMC free article] [PubMed] [Google Scholar]
- 28.Talaei F, Bouma HR, Hylkema MN, Strijkstra AM, Boerema AS, Schmidt M, et al. The role of endogenous H2S formation in reversible remodeling of lung tissue during hibernation in the Syrian hamster. J Exp Biol. 2012;215(Pt 16):2912–9. Epub 2012/07/28. 10.1242/jeb.067363 215/16/2912 [pii]. . [DOI] [PubMed] [Google Scholar]
- 29.Shin DY, Kim GY, Kim JI, Yoon MK, Kwon TK, Lee SJ, et al. Anti-invasive activity of diallyl disulfide through tightening of tight junctions and inhibition of matrix metalloproteinase activities in LNCaP prostate cancer cells. Toxicol In Vitro. 2010;24(6):1569–76. Epub 2010/07/06. 10.1016/j.tiv.2010.06.014 S0887-2333(10)00156-6 [pii]. . [DOI] [PubMed] [Google Scholar]
- 30.Qipshidze N, Metreveli N, Mishra PK, Lominadze D, Tyagi SC. Hydrogen sulfide mitigates cardiac remodeling during myocardial infarction via improvement of angiogenesis. Int J Biol Sci. 2012;8(4):430–41. Epub 2012/03/16. 10.7150/ijbs.3632 ijbsv08p0430 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang CY, Li XH, Zhang T, Fu J, Cui XD. Hydrogen sulfide suppresses the expression of MMP-8, MMP-13, and TIMP-1 in left ventricles of rats with cardiac volume overload. Acta Pharmacol Sin. 2013;34(10):1301–9. Epub 2013/08/27. 10.1038/aps.2013.84 aps201384 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Badier-Commander C, Couvelard A, Henin D, Verbeuren T, Michel JB, Jacob MP. Smooth muscle cell modulation and cytokine overproduction in varicose veins. An in situ study. J Pathol. 2001;193(3):398–407. Epub 2001/03/10. 10.1002/path.819 [pii] 10.1002/path.819 . [DOI] [PubMed] [Google Scholar]
- 33.Li XH, Bu DF, Jin HF, Ding YG, Du JB, Li J, et al. [The dynamic changes in endogenous hydrogen sulfide pathway at the early stage of pulmonary hypertension induced by high pulmonary flow in rats]. Zhongguo Ying Yong Sheng Li Xue Za Zhi. 2007;23(1):75–9. Epub 2007/02/01. . [PubMed] [Google Scholar]
- 34.Badesch DB, Orton EC, Zapp LM, Westcott JY, Hester J, Voelkel NF, et al. Decreased arterial wall prostaglandin production in neonatal calves with severe chronic pulmonary hypertension. Am J Respir Cell Mol Biol. 1989;1(6):489–98. Epub 1989/12/01. 10.1165/ajrcmb/1.6.489 . [DOI] [PubMed] [Google Scholar]
- 35.Wei L, Yu X, Shi H, Zhang B, Lian M, Li J, et al. 15-PGDH/15-KETE plays a role in hypoxia-induced pulmonary vascular remodeling through ERK1/2-dependent PAR-2 pathway. Cell Signal. 2014;26(7):1476–88. Epub 2014/03/25. 10.1016/j.cellsig.2014.03.008 S0898-6568(14)00101-6 [pii]. . [DOI] [PubMed] [Google Scholar]
- 36.Holmes DR, Wester W, Thompson RW, Reilly JM. Prostaglandin E2 synthesis and cyclooxygenase expression in abdominal aortic aneurysms. J Vasc Surg. 1997;25(5):810–5. Epub 1997/05/01. A79847 [pii]. . [DOI] [PubMed] [Google Scholar]
- 37.Reilly JM, Miralles M, Wester WN, Sicard GA. Differential expression of prostaglandin E2 and interleukin-6 in occlusive and aneurysmal aortic disease. Surgery. 1999;126(4):624–7; discussion 7–8. Epub 1999/10/16. S0039606099003074 [pii]. . [PubMed] [Google Scholar]
- 38.Lopez-Candales A, Holmes DR, Liao S, Scott MJ, Wickline SA, Thompson RW. Decreased vascular smooth muscle cell density in medial degeneration of human abdominal aortic aneurysms. Am J Pathol. 1997;150(3):993–1007. Epub 1997/03/01. [PMC free article] [PubMed] [Google Scholar]
- 39.Gomez-Hernandez A, Martin-Ventura JL, Sanchez-Galan E, Vidal C, Ortego M, Blanco-Colio LM, et al. Overexpression of COX-2, Prostaglandin E synthase-1 and prostaglandin E receptors in blood mononuclear cells and plaque of patients with carotid atherosclerosis: regulation by nuclear factor-kappaB. Atherosclerosis. 2006;187(1):139–49. Epub 2005/10/11. S0021-9150(05)00577-0 [pii] 10.1016/j.atherosclerosis.2005.08.035 . [DOI] [PubMed] [Google Scholar]
- 40.Sukhova GK, Schonbeck U, Rabkin E, Schoen FJ, Poole AR, Billinghurst RC, et al. Evidence for increased collagenolysis by interstitial collagenases-1 and -3 in vulnerable human atheromatous plaques. Circulation. 1999;99(19):2503–9. Epub 1999/05/20. . [DOI] [PubMed] [Google Scholar]
- 41.Heo SH, Cho CH, Kim HO, Jo YH, Yoon KS, Lee JH, et al. Plaque rupture is a determinant of vascular events in carotid artery atherosclerotic disease: involvement of matrix metalloproteinases 2 and 9. J Clin Neurol. 2011;7(2):69–76. Epub 2011/07/23. 10.3988/jcn.2011.7.2.69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.van der Wal AC, Becker AE, Das PK. Medial thinning and atherosclerosis—evidence for involvement of a local inflammatory effect. Atherosclerosis. 1993;103(1):55–64. Epub 1993/10/01. 0021-9150(93)90039-W [pii]. . [DOI] [PubMed] [Google Scholar]
- 43.Mancini S Jr., Piccinetti A, Nappi G, Mancini S, Caniato A, Coccheri S. Clinical, functional and quality of life changes after balneokinesis with sulphurous water in patients with varicose veins. Vasa. 2003;32(1):26–30. Epub 2003/04/08. 10.1024/0301-1526.32.1.26 . [DOI] [PubMed] [Google Scholar]
- 44.Distrutti E, Cipriani S, Renga B, Mencarelli A, Migliorati M, Cianetti S, et al. Hydrogen sulphide induces micro opioid receptor-dependent analgesia in a rodent model of visceral pain. Mol Pain. 2010;6:36 Epub 2010/06/15. 10.1186/1744-8069-6-36 1744-8069-6-36 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yang G, Wu L, Wang R. Pro-apoptotic effect of endogenous H2S on human aorta smooth muscle cells. FASEB J. 2006;20(3):553–5. Epub 2006/03/02. 05-4712fje [pii] 10.1096/fj.05-4712fje . [DOI] [PubMed] [Google Scholar]
- 46.Martelli A, Testai L, Breschi MC, Lawson K, McKay NG, Miceli F, et al. Vasorelaxation by hydrogen sulphide involves activation of Kv7 potassium channels. Pharmacol Res. 2013;70(1):27–34. Epub 2013/01/05. 10.1016/j.phrs.2012.12.005 S1043-6618(12)00241-1 [pii]. . [DOI] [PubMed] [Google Scholar]
- 47.Cao RY, St Amand T, Li X, Yoon SH, Wang CP, Song H, et al. Prostaglandin receptor EP4 in abdominal aortic aneurysms. Am J Pathol. 2012;181(1):313–21. Epub 2012/05/19. 10.1016/j.ajpath.2012.03.016 S0002-9440(12)00305-7 [pii]. . [DOI] [PubMed] [Google Scholar]
- 48.Wang M, Lee E, Song W, Ricciotti E, Rader DJ, Lawson JA, et al. Microsomal prostaglandin E synthase-1 deletion suppresses oxidative stress and angiotensin II-induced abdominal aortic aneurysm formation. Circulation. 2008;117(10):1302–9. Epub 2008/02/21. 10.1161/CIRCULATIONAHA.107.731398 CIRCULATIONAHA.107.731398 [pii]. . [DOI] [PubMed] [Google Scholar]
- 49.Deng DX, Spin JM, Tsalenko A, Vailaya A, Ben-Dor A, Yakhini Z, et al. Molecular signatures determining coronary artery and saphenous vein smooth muscle cell phenotypes: distinct responses to stimuli. Arterioscler Thromb Vasc Biol. 2006;26(5):1058–65. Epub 2006/02/04. 01.ATV.0000208185.16371.97 [pii] 10.1161/01.ATV.0000208185.16371.97 . [DOI] [PubMed] [Google Scholar]
- 50.Xu W, Chen J, Lin J, Liu D, Mo L, Pan W, et al. Exogenous H2S protects H9c2 cardiac cells against high glucose-induced injury and inflammation by inhibiting the activation of the NF-kappaB and IL-1beta pathways. Int J Mol Med. 2015;35(1):177–86. Epub 2014/11/21. 10.3892/ijmm.2014.2007 . [DOI] [PubMed] [Google Scholar]
- 51.Cuccurullo C, Iezzi A, Fazia ML, De Cesare D, Di Francesco A, Muraro R, et al. Suppression of RAGE as a basis of simvastatin-dependent plaque stabilization in type 2 diabetes. Arterioscler Thromb Vasc Biol. 2006;26(12):2716–23. Epub 2006/10/14. 01.ATV.0000249630.02085.12 [pii] 10.1161/01.ATV.0000249630.02085.12 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.