Abstract
Cell-based therapies including bone-marrow derived mononuclear cells (MNCs) are now widely being studied because of their pleotropic effects and promising results to improve recovery after stroke in animal models. Unlike other types of cell therapies, MNCs is a mixture of lymphoid, myeloid, erythroid, and stem cell populations. Which cell population(s) accounts for the beneficial effects of MNCs in stroke recovery is unclear. In this paper, we employed a mouse stroke model with middle cerebral artery occlusion (MCAo), and used positively and negatively sorted autologous MNCs by MACs to determine which fractions of the MNCs contribute to their beneficial effects. We evaluated the benefits of neurofunctional recovery produced by individual cell lineages within MNCs in a long-term observation study up to 28 days after stroke. Mortality and modulation of inflammation were also compared among different sub-populations. We further studied the impact of neurotoxicity posed by activated microglia in the presence of different cell lineages within MNCs. We concluded that myeloid cell lineage and stem cell/progenitors appear to be important components within MNCs that contribute to improved outcomes after stroke.
Introduction
After more than 1,000 neuroprotection agents failed in preclinical and clinical trials to treat ischemic stroke, cell-based therapies have gathered increasing attention because of their pleotropic effects and promising results in improving recovery after stroke in pre-clinical studies [1]. As one type of cell therapy, bone marrow derived mononuclear cells (MNCs) have been shown in multiple laboratories to improve neurological deficits after ischemic stroke in animal models [2–5]. Moreover, several small clinical studies have reported on the safeness of administering autologous MNCs in stroke patients [6–11].
Unlike many other types of cell therapy, adequate amounts of MNCs are easily isolated with simple, separate procedures within hours from a bone marrow aspiration and do not require further cell culture to match the cell quantity needed for appropriate dosing [4–7]. MNCs is a mixture of lymphoid, myeloid, erythroid, and stem cell populations [5]. However, the specific cell population contributing to beneficial effects of MNCs in stroke recovery is still unclear. It may be that certain cells are beneficial while others are detrimental. A mixture of different cell types may confer a greater advantage than more purified homogenous populations but it is unknown which populations of cells within the mononuclear fraction confer benefit or harm. Thus, by removing a specific cell sub-population from the mixture, the objective of this study was to determine which cell types are critical for the underlying benefit of MNCs to promote recovery after stroke. Isolating the differential impact of different cell populations within MNCs can further our understanding of their individual effects on stroke recovery and elucidate underlying mechanisms of MNCs for a better translational clinical trial.
Methods
Animal preparation and Middle Cerebral Artery occlusion (MCAo)
Two hundred and ten 8–10 week old male and 6 pregnant C57 BL/6 mice were used in this study. All animals were housed in pairs with free access to food and water. Subjects were maintained on a standard 12:12h light/dark cycle. All outcome assessments and data analysis were completed with the experimenter blinded to the treatment groups. All procedures were approved by the UT-Houston Health Science Center Animal Welfare Committee.
Focal ischemia with 60 minute duration in male C57 mice was induced by suture occlusion of the middle cerebral artery (MCAo). In brief, animals were anesthetized with 2% Isoflurane in a mixture of N2O/O2 (50%/50%). A 6-0 nylon monofilament with a heated blunt tip was introduced through the right external carotid artery and advanced to the beginning of the left middle cerebral artery (MCA). The rectal temperature was monitored and controlled at 36.5±0.5°C using a feed-forward temperature controller. Cerebral perfusion was monitored with a laser Doppler flowmeter (LDF) placed over the ischemic area and was used to confirm successful occlusion and reperfusion.
Bone marrow harvesting and bone marrow cell processing
Twenty two hours after stroke, the mice were anesthetized with isoflurane. An incision was made through the skin to the medial aspect of the left tibia. The periosteum was removed and the surgeon drilled a 0.5 ×0.5mm burr hole extending into the medullary cavity. A 261/2 gauge hypodermic needle was inserted into the medullary cavity and connected to a heparinized syringe. Bone marrow was aspirated while rotating and moving the needle back and forth. The medullary cavity was flushed with saline and the content aspirated. The burr hole was sealed with bone wax and the skin was closed. In the saline control group, only the needle was inserted into the medullary cavity but no content was aspirated.
The cells from the bone marrow aspirate were triturated, centrifuged, and washed in PBS + 0.5% bovine serum albumin (BSA). Cells were then suspended in Media 199 (Sigma, USA) and counted using a hemocytometer and coulter counter. The cell suspension was added on top of 5 mL Ficoll-Paque PLUS (GE, USA) in a 15mL conical vial and then centrifuged. The MNCs were collected, washed with PBS+0.5% BSA, and then counted. Cells were then suspended in sterile, iced PBS at the desired concentration before cell separation.
Cell separation of various populations within MNCs by magnetic assisted cell sorting (MACs)
We used magnetic assisted cell sorting technique (MACS, Miltenyi Biotec, USA) to separate the various cell populations from the whole MNCs. All procedures were performed as per manufacture’s protocol. Briefly, the whole MNCs at 3×107 cells/kg within 100ul vehicle were incubated on ice with nano-sized microbeads conjugated with primary antibody (direct magnetic labeling), or with biotinylated primary antibody first then nano-sized microbeads only (indirect magnetic labeling). The primary anti-mice antibodies were specifically used for CD90.2+CD45R+CD49b for lymphocytes separation (Miltenyi, USA), CD11b+Ly6-G for myeloid cells separation (Miltenyi, USA), CD71 for erythoid cell lineage separation (Biolegend, USA), CD117 and Sca-1 for stem cell and progenitor cell separation (Miltenyi, USA). After the incubation, the cells were applied to a MACS Column placed in a MACS Separator. The unlabeled cells passed through (negatively selected cells) while the magnetically labeled cells were retained within the column. After the column was removed from the separator, followed by flushing and washing with iced PBS, the magnetically-labeled cells eluted from the column were selected as the positive selected specific MNC subtraction. In the whole MNCs-treated group, MNCs were not incubated with primary antibodies and microbeads but were applied to a MACS Column placed in a MACs Separator as sham magnetic cell sorting procedure.
Flow cytometry and characterization of the MNCs Population
We performed flow cytometry to characterize the MNCs after MACS procedures. Briefly, mice were subjected to MCAo for 60 minutes and 22 hours later, bone marrow MNCs were collected as described above. Then, 5 vials with 1×106 MNCs each underwent MACS positive selection as described previously. Among them, the whole MNCs groups underwent a sham MACS procedure. Lastly, the exact number of the remaining cells after MACS was counted with the help of CountBright absolute counting beads (Life Technology) by Gallios Flow Cytometer (Beckman Coulter, USA) according to the manufacture protocol. Cell viability was assessed by exclusion of 7-amino actinomycin (7-AAD) (Biolegend, USA) according to manufacture suggestions. Briefly, 1 million MNCs were suspended in 0.5 mL vehicle and 5 µl of 7-AAD was added. After incubation for 5–10 minutes in the dark, flow cytometry was performed with laser excitation at 546um. 7-AAD positive cells were regarded as dead cells. Data was analyzed with Kaluza software (Beckman Coulter, USA). The percentage of each sorted cell subpopulation number out of the whole MNCs was recorded as the characterization of MNCs (N=6 per group).
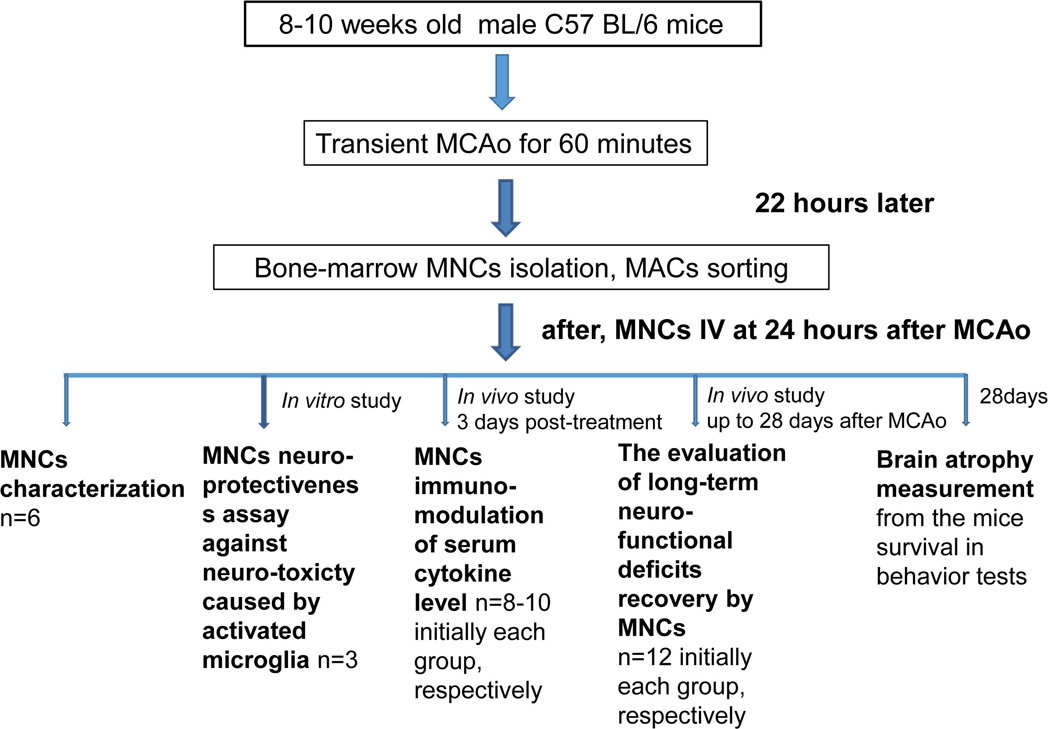
Experiments and experimental groups in vivo and ex vivo: (Fig-Flow Chart)
Flow Chart.
MNCs characterization: Mice were subjected to MCAo and 22 hours later, bone marrow MNCs were collected from each animal. After MACS sorting, the resulting population of cells were characterized by flow cytometry to determine actual cell composition (see table 1). N=6.
- The evaluation of long-term neurofunctional deficits: Mice were subjected to MCAo and 22 hours later, MNCs were collected and sorted by MACS. We used both negatively and positively sorted cells in two separate experiments.
- With negative selection: Mice were randomly treated with: 1) saline; 2) whole MNCs; 3) MNCs with Lymphoid cell depletion; 4) MNCs with Myeloid cell depletion; 5) MNCs with Erythroid lineage cell depletion; 6) MNCs with stem cell and progenitor cell depletion. N=12 per group.
- With positive selection: Mice were randomly treated with: 1) saline; 2) whole MNCs; 3) Lymphoid cell fraction within MNCs; 4) Myeloid cell fraction within MNCs; 5) Erythroid lineage cell fraction within MNCs; 6) Stem cell and progenitor cell fraction within MNCs. N=12 per group.
- Inflammatory modulation effects in serum cytokines level by individual cell lineages within MNCs:
- Groups: Sham stroke with saline treatment, and stroke with mice assigned into: 1) saline; 2) whole MNCs; 3) MNCs with lymphoid cells depletion; 4) MNCs with myeloid cell depletion; 5) MNCs with erythroid lineage cell depletion; 6) MNCs with stem cell and progenitor cell depletion groups. N=8–10 per group.
Table 1. Percentage and exact cell numbers of each sub-population within MNCs.
Cells were sorted from 1×106 whole MNCs by MACs, n=6
| MNCs characterization with MACS | |||
|---|---|---|---|
| Cell Lineage | Marker | Mean±SD (% within MNCs) |
Mean±SD (Exact cell number) ×105 |
| Lymphoid cell | CD90.2, CD45R and CD49b | 29.88±14.59 | 2.43±2.57 |
| Myeloid cell | CD11b and Ly6-G | 35.62±18.71 | 2.78±1.26 |
| Erythroid cell | CD71 | 3.15±2.20 | 0.26±0.18 |
| Stem cell and progenitor cell | CD117 and Sca-1 | 11.86±4.23 | 0.95±0.31 |
The dosage and delivery route of MNC treatment
Whole MNCs were initially suspended at 3×107 cells/kg within 100µl PBS in all the MNC treatment groups before MACS. After MACS, each cell population collected from the initial dosage was suspended into 100µl saline again and injected back into the same animal via tail vein. The cells were infused at a rate of 0.2 mL/min over 5 minutes with the help of an auto-injection pump. The dosage was determined from our previous dosage study in the rat model [12]. We chose the higher dosage in case there was insufficient cell numbers after the MACS procedure.
Behavioral tests
Animals underwent long-term behavioral testing, which was performed by an examiner blinded to treatment allocation. Animals were pretested before MCAo and before cell administration after MCAo, and then tested on days 7, 14, 21, and 28 after stroke. The cylinder and ladder test was used to evaluate dysfunction in our model:
-
Asymmetry in the use of forelimbs for postural support (cylinder test):
Mice were placed into a plexiglass cylinder and observed for asymmetry forelimb-use during vertical movements along the wall of the cylinder. The final score = (nonimpaired forelimb paw placement − impaired forelimb paw placement) / (nonimpaired forelimb paw placement + impaired forelimb paw placement + both forelimb paw placement). A total of 20 movements were recorded up to a maximum of 10-minutes.
-
Ladder Rung test:
Mice were videotaped walking across a horizontal ladder. The ladder rung apparatus was composed of an elevated horizontal ladder (80cm long and 12cm in elevation). The ladder had evenly spaced rungs, 1mm in diameter, and evenly spaced with 15cm tall Plexiglass sides. For each trial, the mouse was placed on one end of the ladder and videotaped walking across. The percent error (total faults/total steps) on the impaired side was scored.
Brain atrophy measurement
Twenty-eight days after stroke, mice were anesthetized and intra-cardially perfused with ice-cold PBS, followed by ice-cold 4% paraformaldehyde (PFA) in PBS and decapitated. Brains were harvested, post-fixed in 4% PFA in PBS for 24 hours, immersed in 20% sucrose for 2 days, and divided into 6 coronal sections (1.2 mm for each). Coronal 20-µm frozen sections from each section were stained with cresyl violet. As we reported previously, brain loss of the ipsilateral chronic infarct was measured using the indirect method and expressed as a percentage of the contralateral hemisphere by a researcher blinded to treatment groups: brain loss (percentage) = (the volume of contra-lateral hemisphere − ipsilateral hemisphere) / the volume of contralateral hemisphere × 100%.
Serum Cytokine Measurements
We measured serum cytokines with a Multiplex assay kit with Luminex (Millipore, USA). Three days post stroke, animals from each experimental group were sacrificed, the peripheral blood was collected, and the serum was prepared for the assay. All measurements were performed as per the manufacture’s protocol with MAGPIX (Millipore, USA).
Cell culture and neurotoxicity assay
Neuronal co-culture model with microglia: Neurons and microglia were isolated from post-natal day 1 mice pups as previously reported, respectively [13]. Neurons were seeded in 24-wells plate at 1×105 with B27 based neuron culture medium and cultured for 9 days. Microglia were seeded on German glass and then activated by oxygen glucose deprivation for 4 hours. German glass containing microglia was added by placing it on the top of neurons [14] with a 1:10 ratio to neuronal cultures with DMEM+10% FBS. Neurons without microglia served as a control group. Twenty-four hours later, the German glass with microglia was removed. The cells in the well were fixed by 10% Formalin first. After washing, the primary antibody anti-mouse NeuN (Millipore, USA) at 1:100 was added in and incubated overnight at 4°C, followed by a secondary antibody of Alex Fluor 488 (Invitrogen, USA). NeuN positive neurons were counted under fluorescence microscopy. Neuronal survival rate was calculated as neuron number in the presence of microglia/number of neurons without microglia × 100%.
MNCs effects in co-culture model: Whole MNCs and specific cell-subtype depleted MNCs groups (as described previously) were added to microglia-neuron co-cultures, described above. For the group that contained whole MNCs, the ratio of MNCs to microglia was 1:1. The cell-subtype depleted MNC groups contained the same number of remaining cells, MNCs after MACS from the same number of whole MNCs. The neurons were counted and the cell survival rate was measured.
Statistical Analysis
All data are presented as means ± SD. A repeated-measures ANOVA and Bonferroni post-test were used for comparison among groups at different days after stroke in the behavioral tests. For the lesion size and the cytokine measurement, a one-way ANOVA was performed with a post hoc Tukey–Kramer test. Behavior testing, lesion size, and serum cytokines were analyzed across all groups in each separate experiment. Statistical significance was set at p<0.05 level.
Results
MNCs is a mixture of various cell subpopulation in a mouse MCAo model
We used 7-ADD to assess the viability of whole MNCs and cell lineages within MNCs after MACS selection. The viability was approximately 93% in all groups. After a sham MACS run (no antibody), there was 8.11± 1.68 × 105 cells left from the initial 1× 106 whole MNCs, suggesting an approximately 20% cell loss due to the sorting procedure. The characterization of major cell lineages within MNCs is provided in Table 1.
Mortality after MCAo and MNCs treatment
Mortality was as high as 50% in our MCAo model with the majority of the mortality occurring within the first 3 days after stroke. Mortality rates were not significantly different for any of the experimental groups in the first days after MCAo and treatment (data not shown). Between 3 and 28 days after stroke, there was no mortality among the remaining groups except for mice treated with MNCs that were depleted of myeloid cells; these mice had a100% mortality rate within 9 days after MCAo.
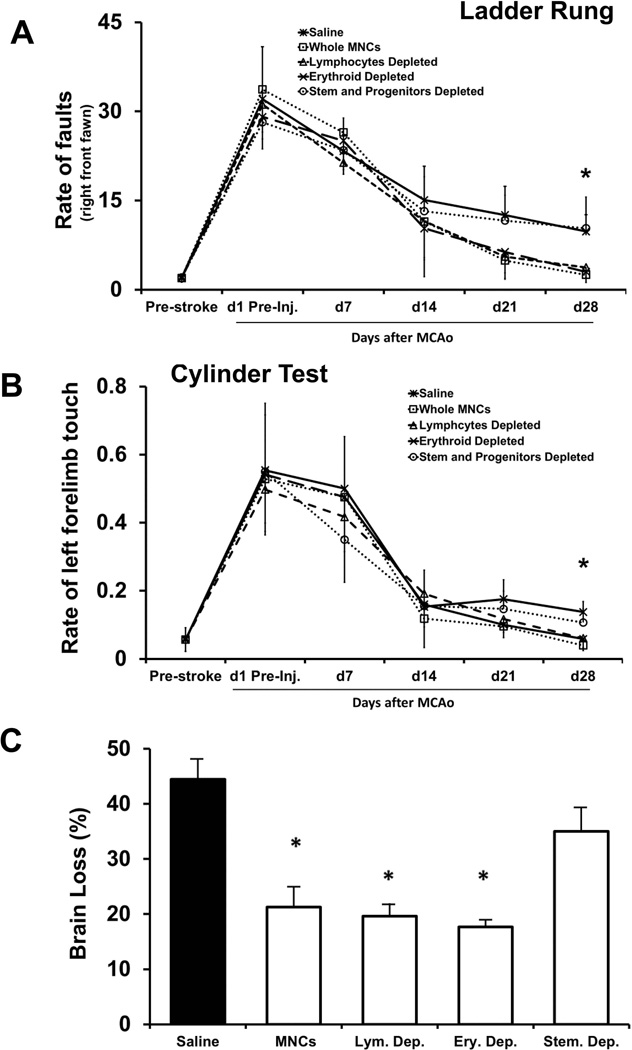
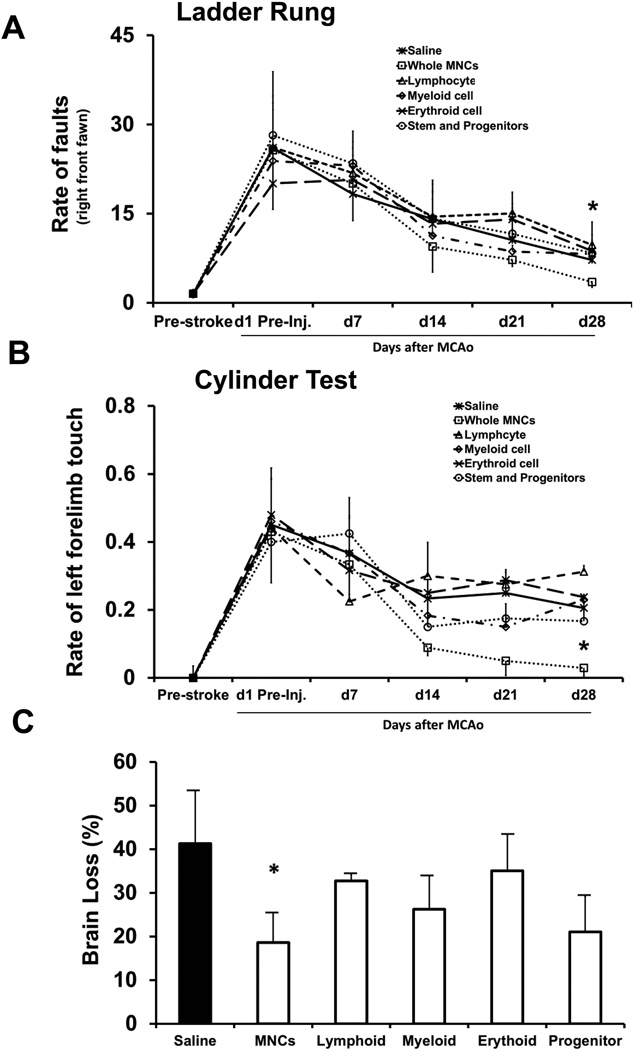
Individual cell lineages with MNCs showed different effects on stroke recovery
We first depleted MNCs of specific cell populations and then injected the remaining cell mixtures at 24 hrs after stroke to test for their therapeutic effect. Compared to the saline group, animals treated with whole MNCs showed significant improvement on both the cylinder and ladder rung tests at 28 days after stroke (p<0.05) (Fig 1). When the lymphoid or erythroid cell lineages were removed, the remaining cells also significantly improved neurological outcome at 28 days after stroke, compared to the saline group, respectively (p<0.05). When the stem and progenitor cell populations were removed, the remaining cells did not significantly change neurological outcome on ladder rung and cylinder (Fig 1A&B) tests compared to saline controls. Unexpectedly, in the animal group treated with MNCs depleted of myeloid cells, all animals died in the first 9 days after stroke. After sacrifice at day 28 after stroke, we found that in animals treated with whole MNCs or MNCs depleted of lymphocytes or erythroid cells, there was a significant reduction in brain atrophy compared to the saline group. When the stem cell and progenitor cell populations were removed, the remaining MNC fraction did not have an effect on atrophy compared with saline treatment (Fig 1C).
Fig 1. Functional improvement in mice treated with whole MNCs and MNCs depleted of specific sub-populations of cells via IV at 24 hrs after stroke.
Mice were assigned to 6 treatment groups: 1) saline; 2) whole MNCs; 3) MNCs with Lymphoid cell depletion; 4) MNCs with Myeloid cell depletion; 5) MNCs with Erythroid lineage cell depletion; 6) MNCs with stem cell and progenitor cell depletion. Line diagrams illustrating evaluation on the Cylinder (A) and Ladder run (B) tests up to 28 days after stroke. Data are mean ± SD; N= 12 per group initially but only 6 survived to the end of observation and all mice with myeloid cell depleted MNCs died within 9 days after stroke. *P < 0.05, compared with saline controls. The bar graph (C) exhibiting significantly reduced cerebral atrophy among the same experimental groups at 28 days after stroke. Data are mean ± SD. N= 6 per group. *P < 0.05 compared with saline controls.
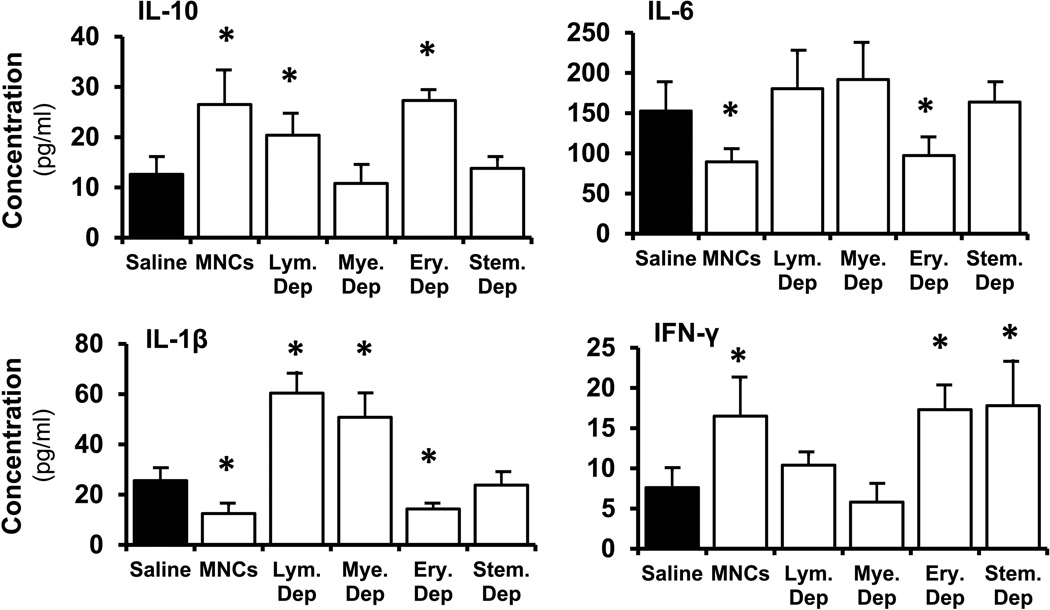
Different cell subpopulations showed different effects on modulating the acute inflammatory response
Given that certain subpopulations within MNCs are important for their therapeutic effects on stroke recovery form the experiments above, and inflammatory pathways are possible targets of MNCs[15], we examined the reactions of different MNC subpopulations obtained by positive selection on the inflammatory response after stroke. We chose day 3 after stroke as the primary endpoint to allow for inclusion of the group depleted of the myeloid fraction. At day 3 post-stroke, the peripheral blood was collected and serum cytokine levels were measured. Whole MNCs and MNCs depleted of erythroid cells significantly decreased serum IL-1β and IL-6 levels and significantly increased serum IL-10 levels (p<0.05). MNCs depleted of other cell lineages showed different results: MNCs depleted of lymphoid cells increased IL-1β and increased IL-10, while MNCs depleted of myeloid cells increased IL-1β but did not increase IL-10. Whole MNCs and MNCs depleted of erythroid or stem cell and progenitors also significantly increased IFN-γ levels but neither MNCs depleted of lymphoid nor MNCs depleted of myeloid cells caused changes to IFN-γ levels, compared to saline treatment group.(Fig 2).
Fig 2. Serum cytokine measurements from animals treated with MNCs and MNCs depleted of specific sub-populations of cells administered at 24 h after stroke.
Cytokines were measured at 3 days after stroke from each group. Data are mean ± SD. N= 8–10 per group initially and N= 6 per group for the end assay. *P < 0.05 compared with saline controls.
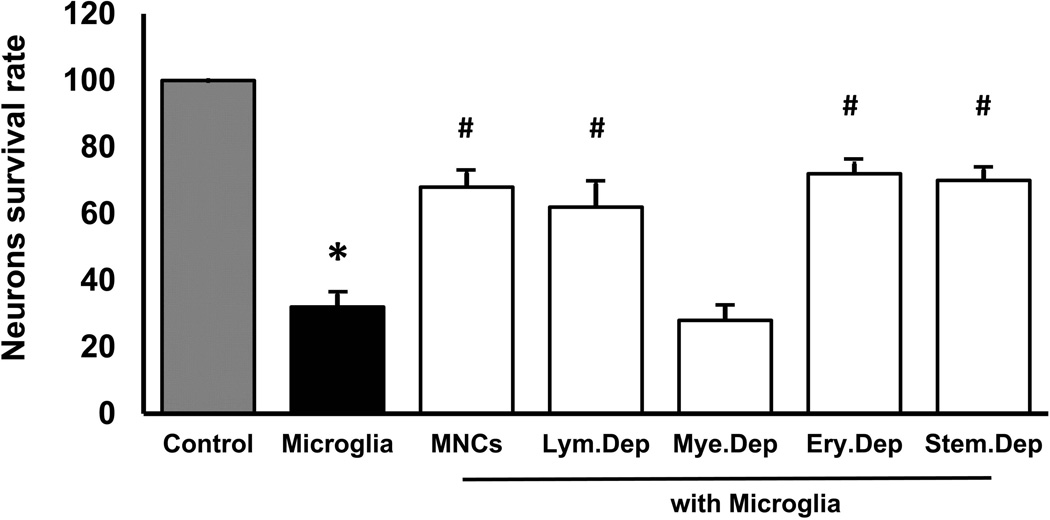
Different cell subpopulation showed different neuroprotective results against neurotoxicity caused by activated microglia
Based on the experiments above, the depletion of different cell lineages leads to different effects on the inflammatory response after stroke. However, we still could not understand why the myeloid depleted MNCs resulted in exacerbation of outcome. We previously reported that MNCs could protect neurons by alleviating microglia’s neurotoxicity [16]. Thus, we conducted another experiment to determine whether MNCs without certain cell populations would lose their neuroprotective effect. We confirmed that activated microglia are neurotoxic in a microglia-neuron co-culture model, and the whole MNCs significantly improved neurons survival rates. With MNCs depleted of myeloid cells, these neuroprotective effects were completely abolished while depletion of other cells lineage had no difference compared with the effects of whole MNCs. (Fig 3)
Fig 3. Neuroprotective effects by MNCs.
Bar graph exhibiting the number of surviving neurons (NeuN-positive cells) upon exposure to activated microglia in presence or absence of MNCs or MNCs without specific cell sub-population. Data are mean ± SD. N= 3. *P < 0.05 compared with naïve neuron culture. # P < 0.05 compared with microglia treated only.
Single cell lineages within MNCs at one dose did not improve recovery after stroke
Since we found that various cell subpopulations of MNCs exert different effects on recovery after stroke, we administered single cell lineage populations obtained through positive selection. Unexpectedly, in each cell lineage treatment group obtained from the same dosage of the whole MNCs, we did not observe any significant neurological improvement on either of the two behavior tests up to 28 days after stroke, compared to the saline group. (Fig 4A&B). The similar absence of effect was found in the evaluation of brain atrophy. The whole MNCs significantly reduced brain tissue loss compared to the saline controls (p<0.05). However, in the other groups treated with the specific cell population, we did not find any difference in brain tissue loss compared to the saline control (Fig 4C).
Fig 4. Functional improvement in mice treated with whole MNCs or a single cell lineage component within MNCs via IV delivery at 24 hrs after stroke.
Mice were randomly assigned to 6 treatment groups after MCAo and autologous MNCs positive selection:1) saline; 2) whole MNCs; 3) Lymphoid cell within MNCs; 4) Myeloid cell within MNCs; 5) Erythroid lineage cell within MNCs; 6) Stem cell and progenitor cell within MNCs. Line diagrams illustrating the evaluation on the Ladder run (A) and Cylinder (B) tests up to 28 days after stroke. The bar graph (C) exhibiting the cerebral atrophy among the same experimental groups at 28 days after stroke. Data are mean ± SD. N= 12 per group initially and N= 6–8 at the end of experiment per group. *P < 0.05 compared with saline controls.
Discussion
Among various types of cell-based therapies for stroke, the application of autologous bone marrow derived mononuclear cells has been one of the most extensively studied for a range of CNS disorders[5, 17–20]. Herein, we sought to determine if there are specific subpopulations of cells within the mononuclear fraction that preferentially account for the seemingly beneficial effects of MNCs in rodent stroke. To address this question, we developed a mouse stroke model to mimic some of the clinical conditions of ischemic stroke. The mice underwent a bone marrow aspiration after stroke then treated in an autologous manner with different components of the bone marrow MNC fraction. We began our studies by depleting cell populations representing different fractions of MNCs to determine the effects of their removal on functional and histological outcomes after stroke.
There have been few published studies using mice models examining the effects of MNCs in stroke [21–22]. Nearly all of the rodent literature on MNCs in stroke has been conducted in rats. One study has shown that labelled MNCs administered intravenously migrate to the site of infarction in a mouse stroke model [22]. We now add that autologous MNCs improve long term functional and histological outcomes in mice after stroke. Mouse models expand opportunities to conduct mechanistic studies to better elucidate the biochemical pathways of MNCs in stroke recovery. However, using this model, we encountered an approximate 50% mortality rate. Death occurred in the majority of cases in the first 3 days after stroke. The mortality could be explained by the severity of the ischemic insult in combination with the multiple surgical procedures under isoflurane anesthesia in the first two days. It is reported that repeated or long-term use of isoflurane may increase neurotoxicity [23–24]. Conversely, we did not observe similar mortality in our rat models and neither have other groups using sheep that underwent similar surgical procedures for MCAo and MNCs collection and infusion [5, 25–26]. Larger animal models might be more tolerant of repeated anesthesia for these types of studies. The underlying causes for mortality should be further explored.
We found that in our mouse model, around 30% of MNCs are lymphoid cells and that they were not essential to the therapeutic effects of MNCs as their removal did not change histological or functional outcomes compared with whole MNC treatment. We found similar results for the erythroid population. Thus, based on our findings, neither lymphoid or erythroid cells appear to be critical cell populations underlying the benefit of MNCs. Depletion of the myeloid fraction, however, led to surprising results. Treatment with MNCs without the myeloid fraction led to 100% mortality within first 9 days. One explanation may be that the removal of myeloid cells creates an environment in which the other cell populations exert a detrimental effect. In a study of human umbilical cord blood (HUCB) mononuclear cells, Wombla et al reported that HUCB monocytes are essential for reducing infarct volume and promoting functional recovery in a rat stroke model[27]. Therefore, it is possible that the monocytes within the myeloid fraction are important cell types that we will need to investigate in more details in future studies. Lastly, animals given MNCs that were depleted of the stem and progenitor cell population provided no functional benefit. Conclusively, our findings suggest that stem cells within MNCs are another important component that underlies the potential benefits of MNCs in a mouse stroke model.
To better understand why certain subpopulations of cells within the MNCs exert differential effects on stroke recovery, we examined the inflammatory response after stroke. We have reported that MNCs decrease serum and brain homogenate pro-inflammatory cytokines and increase anti-inflammatory cytokines in rats[25]. In the present study, we observed similar changes in that MNCs reduced IL-1β while increasing IL-10. However, when certain cell lineages were removed from MNCs, the synergetic effect of decreasing pro-inflammatory cytokines and increasing anti-inflammatory cytokines changed. The one population that had consistent effects on changes in cytokines is the myeloid fraction. Depletion of the myeloid cells prevents the increase in IL-10 and the decrease in IL-1β as well as IL-6. Furthermore, sustained tissue protection was observed at 28 days in animals treated with MNCs but not MNCs depleted with stem cells. These findings support the hypothesis that both myeloid cells and stem cell populations may be important cell types that reduce inflammation and subsequent infarct maturation.
Microglia are associated with brain inflammatory responses as well as tissue repair after stroke [28–29]. In the present study, we found OGD-activated microglia significantly reduced neuronal survival in a neuron-microglia co-cultured model. When whole MNCs were added, the deleterious effect of microglia on neuron survival was reduced. However, the beneficial effect on MNCs was lost following depletion of myeloid cells. This suggests an important role for the myeloid population in the neuroprotective effects of MNCs against activated microglia-mediated neurotoxicity. These results could partially account for the high mortality after stroke in animals treated with myeloid depleted MNCs.
Our study suggests that myeloid cells and stem/progenitor cells may provide most of the biological input toward the therapeutic effects of MNCs in post-stroke recovery. However, one of the limitations of this interpretation is that we tested only one dose of cells for each of the cellular sub-population. It is possible that a higher dose of lymphoid or erythroid cells is needed to demonstrate biological effect. Another limitation of this study is that when using positively selected cells, we used MACs to sort the individual cell lineage within MNCs thus generating antibody-conjugated cells for treatment of animals. With this, we could not exclude the possibility that cells with conjugated antibody or microbeads would lose their bioactivities or be recognized as opsonized and eliminated by blood or tissue phagocytes.
We believe that the interactions among various cell subpopulations within MNCs are important for their optimal effect in improving post-stroke recovery. Ultimately, future studies will need to focus around identifying which myeloid cell types are critical to the beneficial effects of MNCs. We also seek to identify which stem and progenitor cells are important. More precise and single cell lineage studies are needed to better understand the mechanisms of MNCs.
Acknowledgments
Funding: This study was funded by NIH R-01 NS071127
Footnotes
Compliance with Ethical Standards:
Ethical approval: All animal experiments and surgical procedures were approved by the University of Texas Health Science Center Animal Welfare Committee and followed NIH guidelines and regulations.
Ethical approval: This article does not contain any studies with human participants performed by any of the authors.
Conflict of Interest: No competing financial interests exist. All authors declare that they have no conflict of interest.
References
- 1.Hossmann KA. The two pathophysiologies of focal brain ischemia: implications for translational stroke research. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2012;32(7):1310–1316. doi: 10.1038/jcbfm.2011.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Iihoshi S, Honmou O, Houkin K, Hashi K, Kocsis JD. A therapeutic window for intravenous administration of autologous bone marrow after cerebral ischemia in adult rats. Brain research. 2004;1007(1–2):1–9. doi: 10.1016/j.brainres.2003.09.084. [DOI] [PubMed] [Google Scholar]
- 3.Kamiya N, Ueda M, Igarashi H, Nishiyama Y, Suda S, Inaba T, et al. Intra-arterial transplantation of bone marrow mononuclear cells immediately after reperfusion decreases brain injury after focal ischemia in rats. Life Sci. 2008;83(11–12):433–437. doi: 10.1016/j.lfs.2008.07.018. [DOI] [PubMed] [Google Scholar]
- 4.Giraldi-Guimardes A, Rezende-Lima M, Bruno FP, Mendez-Otero R. Treatment with bone marrow mononuclear cells induces functional recovery and decreases neurodegeneration after sensorimotor cortical ischemia in rats. Brain research. 2009;1266:108–120. doi: 10.1016/j.brainres.2009.01.062. [DOI] [PubMed] [Google Scholar]
- 5.Brenneman M, Sharma S, Harting M, Strong R, Cox CS, Jr, Aronowski J, et al. Autologous bone marrow mononuclear cells enhance recovery after acute ischemic stroke in young and middle-aged rats. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2010;30(1):140–149. doi: 10.1038/jcbfm.2009.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mendonca ML, Freitas GR, Silva SA, Manfrim A, Falcao CH, Gonzales C, et al. Safety of intra-arterial autologous bone marrow mononuclear cell transplantation for acute ischemic stroke. Arq Bras Cardiol. 2006;86(1):52–55. doi: 10.1590/s0066-782x2006000100008. [DOI] [PubMed] [Google Scholar]
- 7.Battistella V, de Freitas GR, da Fonseca LM, Mercante D, Gutfilen B, Goldenberg RC, et al. Safety of autologous bone marrow mononuclear cell transplantation in patients with nonacute ischemic stroke. Regen Med. 2011;6(1):45–52. doi: 10.2217/rme.10.97. [DOI] [PubMed] [Google Scholar]
- 8.Rosado-de-Castro PH, Schmidt FdaR, Battistella V, Lopes de Souza SA, Gutfilen B, Goldenberg RC, et al. Biodistribution of bone marrow mononuclear cells after intra-arterial or intravenous transplantation in subacute stroke patients. Regen Med. 2013;8(2):145–155. doi: 10.2217/rme.13.2. [DOI] [PubMed] [Google Scholar]
- 9.Prasad K, Mohanty S, Bhatia R, Srivastava MV, Garg A, Srivastava A, et al. Autologous intravenous bone marrow mononuclear cell therapy for patients with subacute ischaemic stroke: a pilot study. Indian J Med Res. 2012;136(2):221–228. [PMC free article] [PubMed] [Google Scholar]
- 10.Prasad K, Sharma A, Garg A, Mohanty S, Bhatnagar S, Johri S, et al. Intravenous autologous bone marrow mononuclear stem cell therapy for ischemic stroke: a multicentric, randomized trial. Stroke; a journal of cerebral circulation. 2014;45(12):3618–3624. doi: 10.1161/STROKEAHA.114.007028. [DOI] [PubMed] [Google Scholar]
- 11.Savitz SI, Misra V, Kasam M, Juneja H, Cox CS, Jr, Alderman S, et al. Intravenous autologous bone marrow mononuclear cells for ischemic stroke. Annals of neurology. 2011;70(1):59–69. doi: 10.1002/ana.22458. [DOI] [PubMed] [Google Scholar]
- 12.Yang B, Strong R, Sharma S, Brenneman M, Mallikarjunarao K, Xi X, et al. Therapeutic time window and dose response of autologous bone marrow mononuclear cells for ischemic stroke. Journal of neuroscience research. 2011;89(6):833–839. doi: 10.1002/jnr.22614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Floden AM, Combs CK. Beta-amyloid stimulates murine postnatal and adult microglia cultures in a unique manner. J Neurosci. 2006;26(17):4644–4648. doi: 10.1523/JNEUROSCI.4822-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhao X, Sun G, Zhang J, Strong R, Song W, Gonzales N, et al. Hematoma resolution as a target for intracerebral hemorrhage treatment: role for peroxisome proliferator-activated receptor gamma in microglia/macrophages. Ann Neurol. 2007;61(4):352–362. doi: 10.1002/ana.21097. [DOI] [PubMed] [Google Scholar]
- 15.Yang B, Xi X, Aronowski J, Savitz SI. Ischemic stroke may activate bone marrow mononuclear cells to enhance recovery after stroke. Stem cells and development. 2012;21(18):3332–3340. doi: 10.1089/scd.2012.0037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sharma S, Yang B, Strong R, Xi X, Brenneman M, Grotta JC, et al. Bone marrow mononuclear cells protect neurons and modulate microglia in cell culture models of ischemic stroke. J Neurosci Res. 2010;88(13):2869–2876. doi: 10.1002/jnr.22452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bedi SS, Walker PA, Shah SK, Jimenez F, Thomas CP, Smith P, et al. Autologous bone marrow mononuclear cells therapy attenuates activated microglial/macrophage response and improves spatial learning after traumatic brain injury. The journal of trauma and acute care surgery. 2013;75(3):410–416. doi: 10.1097/TA.0b013e31829617c6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leal MM, Costa-Ferro ZS, Souza BS, Azevedo CM, Carvalho TM, Kaneto CM, et al. Early transplantation of bone marrow mononuclear cells promotes neuroprotection and modulation of inflammation after status epilepticus in mice by paracrine mechanisms. Neurochem Res. 2014;39(2):259–268. doi: 10.1007/s11064-013-1217-7. [DOI] [PubMed] [Google Scholar]
- 19.Guo X, Bu X, Li Z, Yan Z, Jiang J, Zhou Z. Comparison of autologous bone marrow mononuclear cells transplantation and mobilization by granulocyte colony-stimulating factor in experimental spinal injury. Int J Neurosci. 2012;122(12):723–733. doi: 10.3109/00207454.2012.716109. [DOI] [PubMed] [Google Scholar]
- 20.Kanamaru T, Kamimura N, Yokota T, Nishimaki K, Iuchi K, Lee H, et al. Intravenous transplantation of bone marrow-derived mononuclear cells prevents memory impairment in transgenic mouse models of Alzheimer's disease. Brain research. 2015 doi: 10.1016/j.brainres.2015.02.011. [DOI] [PubMed] [Google Scholar]
- 21.Nakano-Doi A, Nakagomi T, Fujikawa M, Nakagomi N, Kubo S, Lu S, et al. Bone marrow mononuclear cells promote proliferation of endogenous neural stem cells through vascular niches after cerebral infarction. Stem cells (Dayton, Ohio) 2010;28(7):1292–1302. doi: 10.1002/stem.454. [DOI] [PubMed] [Google Scholar]
- 22.Prabhakar S, Muthaian R, Chabbra R, Anand A. Analysis of homing potential of marrow-derived mononuclear cells in an experimentally-induced brain stroke mouse model. Brain Inj. 2010;24(12):1485–1490. doi: 10.3109/02699052.2010.520298. [DOI] [PubMed] [Google Scholar]
- 23.Zhou Z, Ma D. Anaesthetics-induced neurotoxicity in developing brain: an update on preclinical evidence. Brain Sci. 2014;4(1):136–149. doi: 10.3390/brainsci4010136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lin EP, Soriano SG, Loepke AW. Anesthetic neurotoxicity. Anesthesiol Clin. 2014;32(1):133–155. doi: 10.1016/j.anclin.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 25.Yang B, Migliati E, Parsha K, Schaar K, Xi X, Aronowski J, et al. Intra-arterial delivery is not superior to intravenous delivery of autologous bone marrow mononuclear cells in acute ischemic stroke. Stroke; a journal of cerebral circulation. 2013;44(12):3463–3472. doi: 10.1161/STROKEAHA.111.000821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Boltze J, Nitzsche B, Geiger KD, Schoon HA. Histopathological Investigation of Different MCAO Modalities and Impact of Autologous Bone Marrow Mononuclear Cell Administration in an Ovine Stroke Model. Translational stroke research. 2011;2(3):279–293. doi: 10.1007/s12975-011-0101-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Womble TA, Green S, Shahaduzzaman M, Grieco J, Sanberg PR, Pennypacker KR, et al. Monocytes are essential for the neuroprotective effect of human cord blood cells following middle cerebral artery occlusion in rat. Mol Cell Neurosci. 2014;59:76–84. doi: 10.1016/j.mcn.2014.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Patel AR, Ritzel R, McCullough LD, Liu F. Microglia and ischemic stroke: a double-edged sword. Int J Physiol Pathophysiol Pharmacol. 2013;5(2):73–90. [PMC free article] [PubMed] [Google Scholar]
- 29.Kim JY, Kawabori M, Yenari MA. Innate inflammatory responses in stroke: mechanisms and potential therapeutic targets. Curr Med Chem. 2014;21(18):2076–2097. doi: 10.2174/0929867321666131228205146. [DOI] [PMC free article] [PubMed] [Google Scholar]