Abstract
Background
Little data are available regarding individual patients’ risk of surgical site infection (SSI) following mastectomy with or without immediate reconstruction. Our objective was to develop a risk prediction model for mastectomy-related SSI.
Methods
We established a cohort of women < 65 years of age with mastectomy from 1/1/2004–12/31/2011 using commercial claims data. ICD-9-CM diagnosis codes were used to identify SSI within 180 days after surgery. SSI risk factors were determined with multivariable logistic regression using derivation data from 2004-2008 and validated with 2009–2011 data using discrimination and calibration measures.
Results
In the derivation cohort 595 SSIs were identified in 7,607 (7.8%) women, and 396 SSIs were coded in 4,366 (9.1%) women in the validation cohort. Independent risk factors for SSIs included rural residence, rheumatologic disease, depression, diabetes, hypertension, liver disease, obesity, preexisting pneumonia or urinary tract infection, tobacco use disorder, smoking-related diseases, bilateral mastectomy, and immediate reconstruction. Receipt of home health care was associated with lower risk. The model performed equally in the validation cohort per discrimination (C statistics 0.657 and 0.649) and calibration (Hosmer-Lemeshow P=0.091 and 0.462 for derivation and validation, respectively). Three risk strata were created based on predicted SSI risk, which demonstrated good correlation with the proportion of observed infections in the strata.
Conclusions
We developed and internally validated an SSI risk prediction model that can be used to counsel women concerning their individual risk of SSI post-mastectomy. Immediate reconstruction, diabetes, and smoking-related diseases were important risk factors for SSI in this nonelderly population of women undergoing mastectomy.
INTRODUCTION
The most common healthcare-associated infections among hospitalized patients are surgical site infections (SSIs).1 SSIs result in significant morbidity and mortality, prolong hospital stays, and increase healthcare costs.1;2 According to the National Healthcare Safety Network (NHSN), SSI incidence is expected to be low (1–2%) after clean procedures such as breast operations,3 but breast SSI rates reported in the literature are generally higher.
Several studies have examined independent risk factors for SSI after various breast operations including mastectomy and immediate or delayed breast reconstruction. Comorbid conditions, including obesity or increased body mass index (BMI),4-16 diabetes6;12;13;15;17 or hyperglycemia,18 smoking,6;12;13;15;19-21 heavy alcohol use,11;15 higher ASA score,6;11;14 and history of radiotherapy4;7;8;19;22;23 have been reported as risk factors for SSI after breast surgery. Longer duration of operation4;6;11 and implant8;19 or autologous reconstruction13;14;24 increase the risk of SSI. Despite a large body of literature, the inclusion of different types of breast operations, inconsistent definitions of SSI, variable duration of SSI surveillance, and the often limited number of risk factors analyzed make it difficult to conclusively determine the most important factors associated with infection risk. Additionally, the generalizability of findings is unknown because almost all studies have been from single institution/ hospitals or consortiums,4;8;10;15-22 or were based on the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database.6;7;9;11-14;24
The goal of our study was to develop a risk prediction model for SSI following mastectomy with and without immediate reconstruction in a large, geographically diverse population representing hundreds of institutions and providers. The results could be used to more effectively counsel women prior to surgery about their specific risk of SSI, discuss personalized strategies to reduce SSI risk, and facilitate informed decision making about the risks and benefits of different types and timing of breast procedures.
METHODS
Primary Data Source
We conducted a retrospective cohort study using all fully-adjudicated claims submitted for reimbursement from providers, facilities, and outpatient pharmacies linked to health plan enrollment information from 12 Anthem–affiliated plans, including over 8 million nonelderly women (see Appendix). We required complete medical and prescription drug coverage to identify relevant underlying conditions. Women with end-stage renal disease, prior organ transplant, or HIV infection were excluded due to the rare nature of the conditions and for privacy concerns.
Mastectomy Patient Population
We identified the first mastectomy among insured members aged 18–64 years from 1/1/2004–12/31/2011 using International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) and Current Procedural Terminology, 4th edition (CPT-4) procedure codes from inpatient and outpatient facilities and providers. The mastectomy patient population was further refined as reported previously.25 We implemented steps to increase the likelihood that the procedures were truly mastectomies, excluding claims containing CPT-4, HCPCS, or UB-04 revenue codes truncated to 4 digits and populated in the fields reserved for ICD-9-CM procedure codes, and claims in which a mastectomy procedure code was present only on one line on a single claim with no other claims on the same date. We also excluded mastectomy procedures that were more consistent with breast-conserving surgery (BCS) when both were coded during the same admission. For these analyses, we required insurance coverage 365 days before surgery and at least 30 days post-mastectomy to capture comorbidities and early postoperative factors associated with SSI.
SSI and Non-Infectious Wound Complications (NIWC)
SSIs and NIWCs first recorded 2–180 days after mastectomy procedures (beginning day 1 for hematoma) were identified using ICD-9-CM diagnosis codes from inpatient and outpatient facilities and provider claims, as reported previously.25 NIWCs included fat necrosis (567.82, 611.3), dehiscence (875.0, 875.1, 879.0, 879.1, 998.3, 998.32), hematoma (998.12), and necrosis (998.83). We censored the observation period to capture SSIs at the time of a subsequent breast or non-breast NHSN procedure.25 Since risk factors for SSIs and NIWCs may be similar, we excluded persons who did not have an SSI but did have an NIWC in risk factor analyses so that the comparison group was wound complication-free.
Risk Factors for SSI
Potential risk factors for SSI included demographics, comorbidities (primarily using the Elixhauser classification),26 medications, and cancer-related and operative factors with clinical or biologic plausability for association with infection risk. We matched patients’ zip code to the 2000 U.S. census median household income27 to determine income quartile and to the 2006 urban-rural classification scheme28 to determine urban-rural status. Comorbidities and postoperative risk factors were identified using ICD-9-CM diagnosis codes, ICD-9-CM/CPT-4 procedure codes, and outpatient prescription drug claims (Appendix Table 1).26;29-33 Postoperative factors in the month after surgery were not counted if first coded after an SSI. For postoperative home health care, we did not count home health visits for persons with an SSI or NIWC during the mastectomy admission as these women were likely receiving follow up wound care (Appendix Table 1). Cancer-related risk factors included cancer stage, history of breast cancer, previous radiotherapy, neoadjuvant chemotherapy, previous breast conserving surgery, and previous lymph node surgery (Appendix Table 1). Neoadjuvant chemotherapy was identified by chemotherapy claims within 60 days before mastectomy. We identified cancer stage using ICD-9-CM diagnosis codes on pathology claims, when available, as described previously.25;34 Potential operative risk factors included unilateral versus bilateral mastectomy,25 immediate breast implant and/or flap reconstruction,25 sentinel node, and simple versus modified radical mastectomy (Appendix Table 1).
Statistical Analysis
The mastectomy population was divided into derivation and validation cohorts based on procedures performed from 2004–2008 and 2009–2011, respectively, to determine whether the model was robust to changes over time. SSI risk factors with p < 0.2 in univariable analysis were included in the multivariable logistic regression model with backward selection based on a cutoff of p < 0.075. Postoperative variables that could not be assessed prior to surgery were not included in the risk prediction model. We assessed multicollinearity by examining the tolerance values in each model to ensure independence of explanatory variables.
The final logistic regression model from the derivation cohort was evaluated first by determining the performance of the derivation model parameter estimates in the validation cohort. Second, the variables retained in the derivation cohort model were re-fit with the validation cohort, allowing the parameter estimates to vary from the derivation model. We used the C statistic to assess discrimination, the Hosmer-Lemeshow test35;36 to evaluate calibration, and the Brier score to measure overall performance of the models. Based on the predicted probability of SSI in the validated model using the parameter estimates from the derivation cohort, we grouped women into low-, moderate-, and high-risk groups. We obtained similar results in a Cox proportional hazards model; hence only logistic regression results are presented.
All data management and analyses were performed using SAS v9.3 (SAS Institute Inc., Cary, NC). This study was approved by the Washington University Human Research Protection Office.
RESULTS
A total of 11,973 women undergoing mastectomy met inclusion criteria for the study from 2004 to 2011. The 180-day incidence of SSI in the population was 8.3% (595/7,607 in the derivation cohort and 396/4,366 in the validation cohort), and the incidence of NIWC-alone (without SSI) was 6.9%. The cumulative incidence of SSI after mastectomy plus implant reconstruction was 4.9% within 30 days, 8.6% within 90 days, and 10.2% within 180 days. The cumulative incidence of SSI after mastectomy without implant reconstruction (i.e., mastectomy only or autologous flap) was 3.5% within 30 days, 5.6% within 90 days, and 6.5% within 180 days. For all subsequent analyses, 831 patients with an NIWC but no SSI were excluded in order to have a wound complication-free comparison group. The final populations for SSI risk factor analyses included 7,115 patients in the derivation cohort with 595 SSI, and 4,027 patients in the validation cohort with 396 SSI (Appendix Figure 1). A number of factors were associated with SSI in univariable analysis (Table 1). Independent risk factors for SSI in the derivation model included rural patient residence, rheumatologic disease, depression, diabetes, hypertension, liver disease, obesity, preoperative pneumonia or UTI, tobacco use disorder, and smoking-related diseases (e.g., chronic obstructive pulmonary disease). Significant operative risk factors included bilateral mastectomy and immediate breast implant and flap reconstruction. Receipt of home health care after surgery was associated with significantly lower risk of SSI (Table 2). In post-hoc testing of the derivation model, the parameter estimates for tobacco use disorder and smoking-related diseases were significantly different (p=0.030). The odds ratios and 95% confidence intervals for the various risk factors differed when the variables in the model were fit to the validation cohort (Table 2).
Table 1.
Univariable Risk Factors for Surgical Site Infection (SSI) After Mastectomy, Derivation Cohort of 7,115 Women, 2004–2008
| Variablea | Category | SSI N (%) |
No Complication N (%) |
Odds Ratio (95% CI) |
P |
|---|---|---|---|---|---|
| Total | 595 | 6,520 | |||
| Patient factors | |||||
| Demographics | |||||
| Age | 18–35 years | 20 (3.4) | 292 (4.5) | 0.72 (0.44, 1.20) | 0.208 |
| 36–40 years | 52 (8.7) | 511 (7.8) | 1.08 (0.75, 1.54) | 0.689 | |
| 41–45 years | 89 (15.0) | 941 (14.4) | 1.00 | ||
| 46–50 years | 117 (19.7) | 1,382 (21.2) | 0.90 (0.67, 1.19) | 0.451 | |
| 51–55 years | 123 (20.7) | 1,240 (19.0) | 1.05 (0.79, 1.40) | 0.744 | |
| 56–60 years | 119 (20.0) | 1,261 (19.3) | 1.00 (0.75, 1.33) | 0.988 | |
| 61–64 years | 75 (12.6) | 893 (13.7) | 0.89 (0.64, 1.22) | 0.468 | |
| Patient residence | Urban | 478 (80.3) | 5,315 (81.5) | 1.00 | |
| Rural | 99 (16.6) | 919 (14.1) | 1.20 (0.95, 1.50) | 0.120 | |
| Missing | 18 (3.0) | 286 (4.4) | 0.70 (0.43, 1.14) | 0.150 | |
| Income quartile | 0–25th percentile | 143 (24.0) | 1,602 (24.6) | 0.97 (0.76, 1.24) | 0.796 |
| 26–50th percentile | 152 (25.5) | 1,572 (24.1) | 1.05 (0.82, 1.33) | 0.698 | |
| 51–75th percentile | 144 (24.2) | 1,563 (24.0) | 1.00 (0.78, 1.28) | 0.996 | |
| 76–100th percentile | 138 (23.2) | 1,497 (23.0) | 1.00 | ||
| Missing | 18 (3.0) | 286 (4.4) | 0.68 (0.41, 1.13) | 0.140 | |
| Comorbidities/ Medications | |||||
| Anticoagulant drugs | 13 (2.2) | 139 (2.1) | 1.03 (0.58, 1.82) | 0.931 | |
| Blood loss anemia | 7 (1.2) | 55 (0.8) | 1.40 (0.64, 3.09) | 0.404 | |
| Coagulopathy | 6 (1.0) | 46 (0.7) | 1.44 (0.61, 3.37) | 0.407 | |
| Congestive heart failure | 7 (1.2) | 35 (0.5) | 2.14 (0.95, 4.84) | 0.066 | |
| Congestive heart failure drugs | 22 (3.7) | 129 (2.0) | 1.90 (1.20, 3.01) | 0.006 | |
| Deficiency anemia | 39 (6.6) | 462 (7.1) | 0.92 (0.66, 1.29) | 0.628 | |
| Depression | 45 (7.6) | 312 (4.8) | 1.63 (1.18, 2.25) | 0.003 | |
| Diabetes | 76 (12.8) | 379 (5.8) | 2.37 (1.83, 3.08) | <0.001 | |
| DMARD or biologic drugs | 64 (10.8) | 631 (9.7) | 1.12 (0.86, 1.48) | 0.397 | |
| Hypertension | 242 (40.7) | 1,936 (29.7) | 1.62 (1.37, 1.93) | <0.001 | |
| Liver disease | 7 (1.2) | 19 (0.3) | 4.08 (1.71, 9.74) | 0.002 | |
| Malnutrition/weight loss | 8 (1.3) | 58 (0.9) | 1.52 (0.72, 3.20) | 0.271 | |
| Non-breast malignancy | 40 (6.7) | 522 (8.0) | 0.83 (0.59, 1.16) | 0.267 | |
| Obesity | 48 (8.1) | 295 (4.5) | 1.85 (1.35, 2.54) | <0.001 | |
| Oral steroids | 73 (12.3) | 767 (11.8) | 1.05 (0.81, 1.36) | 0.715 | |
| Peripheral vascular disease | 5 (0.8) | 31 (0.5) | 1.77 (0.69, 4.58) | 0.236 | |
| Pneumonia or UTI | 19 (3.2) | 114 (1.7) | 1.85 (1.13, 3.04) | 0.014 | |
| Psychoses | 31 (5.2) | 208 (3.2) | 1.67 (1.13, 2.46) | 0.010 | |
| Rheumatologic disease | 17 (2.9) | 96 (1.5) | 1.97 (1.17, 3.32) | 0.011 | |
| Skin disease | 17 (2.9) | 109 (1.7) | 1.73 (1.03, 2.90) | 0.038 | |
| Tobacco use disorder | 74 (12.4) | 646 (9.9) | 1.29 (1.00, 1.67) | 0.051 | |
| Smoking-related diseases | 34 (5.7) | 173 (2.7) | 2.22 (1.52, 3.24) | <0.001 | |
| Cancer-related | |||||
| Stage of breast cancer | Benign or prophylactic |
18 (3.0) | 185 (2.8) | 1.00 | |
| Carcinoma in situ | 74 (12.4) | 805 (12.4) | 0.94 (0.55, 1.62) | 0.836 | |
| Local | 361 (60.7) | 4,178 (64.1) | 0.89 (0.54, 1.46) | 0.639 | |
| Regional | 126 (21.2) | 1,199 (18.4) | 1.08 (0.64, 1.81) | 0.771 | |
| Metastatic | 16 (2.7) | 153 (2.4) | 1.07 (0.53, 2.18) | 0.841 | |
| Previous breast cancer | 99 (16.6) | 997 (15.3) | 1.11 (0.88, 1.39) | 0.384 | |
| Previous radiotherapy | 35 (5.9) | 363 (5.6) | 1.06 (0.74, 1.52) | 0.749 | |
| Neoadjuvant chemotherapy | 71 (11.9) | 813 (12.5) | 0.95 (0.73, 1.23) | 0.704 | |
| Previous breast-conserving surgery |
182 (30.6) | 2,108 (32.3) | 0.92 (0.77, 1.11) | 0.384 | |
| Previous lymph node surgery | 82 (13.8) | 949 (14.6) | 0.94 (0.74, 1.20) | 0.608 | |
| Inflammatory breast disease | 13 (2.2) | 91 (1.4) | 1.58 (0.88, 2.84) | 0.128 | |
| Operative factors | |||||
| Inpatient admission | 516 (86.7) | 5,305 (81.4) | 1.50 (1.17, 1.91) | 0.001 | |
| Bilateral mastectomy | 263 (44.2) | 2,253 (34.6) | 1.50 (1.27, 1.78) | <0.001 | |
| Modified radical mastectomy | 267 (44.9) | 2,900 (44.5) | 1.02 (0.86, 1.20) | 0.853 | |
| Concurrent sentinel node dissection |
116 (19.5) | 1,427 (21.9) | 0.86 (0.70, 1.07) | 0.176 | |
| Concurrent breast implant | 318 (53.4) | 2,757 (42.3) | 1.57 (1.32, 1.85) | <0.001 | |
| Concurrent flap reconstruction | 118 (19.8) | 879 (13.5) | 1.59 (1.28, 1.97) | <0.001 | |
| Postoperative factors | |||||
| Anemia | 45 (7.6) | 424 (6.5) | 1.18 (0.85, 1.62) | 0.319 | |
| Pneumonia or UTI | 14 (2.4) | 77 (1.2) | 2.02 (1.13, 3.59) | 0.017 | |
| Home health care | 110 (18.5) | 1,542 (23.7) | 0.73 (0.59, 0.91) | 0.004 |
CI confidence interval, DMARD disease-modifying antirheumatic drugs, UTI urinary tract infection.
Additional variables dropped due to small numbers within a cell (≤ 5) of the contingency table included previous sepsis or S. aureus infection, chronic renal failure, alcohol abuse, and drug abuse.
Table 2.
Multivariable Logistic Regression Model of Significant Risk Factors for Surgical Site Infection After Mastectomy, in the Derivation Cohort of 7,115 Women, 2004–2008 and Validation Cohort of 4,027 Women, 2009-2011a
| Variable | Category | Derivation Cohort | Validation Cohort |
|---|---|---|---|
| Odds Ratio (95% CI) | Odds Ratio (95% CI)b | ||
| Bilateral mastectomy | 1.39 (1.16, 1.67) | 1.27 (1.02, 1.59) | |
| Breast implant reconstruction |
1.83 (1.52, 2.21) | 2.26 (1.76, 2.91) | |
| Autologous flap reconstruction |
2.01 (1.60, 2.51) | 2.29 (1.71, 3.07) | |
| Diabetes | 2.16 (1.63, 2.87) | 1.54 (1.07, 2.20) | |
| Obesity | 1.57 (1.12, 2.19) | 1.46 (1.06, 2.02) | |
| Tobacco use disorderc | 1.29 (0.99, 1.68) | 1.26 (0.96, 1.65) | |
| Smoking-related diseases | 2.23 (1.50, 3.31) | 1.60 (0.97, 2.64) | |
| Depression | 1.52 (1.09, 2.12) | 1.18 (0.83, 1.68) | |
| Hypertension | 1.48 (1.23, 1.79) | 1.79 (1.42, 2.26) | |
| Liver disease | 3.65 (1.48, 8.97) | 1.80 (0.57, 5.68) | |
| Previous pneumonia or urinary tract infection |
1.60 (0.97, 2.66) | 0.67 (0.29, 1.55) | |
| Rheumatologic disease | 1.81 (1.05, 3.09) | 0.88 (0.41, 1.89) | |
| Home health care | 0.78 (0.63, 0.98) | 1.10 (0.86, 1.42) | |
| Patient residence | Urban | 1.00 | 1.00 |
| Rural | 1.35 (1.06, 1.70) | 1.07 (0.79, 1.46) | |
| Missing | 0.76 (0.47, 1.24) | 0.96 (0.54, 1.71) |
All variables in the model were dichotomous (yes/no), unless otherwise noted.
Model used the variables from the final derivation cohort model, re-fit to the validation cohort.
ICD-9-CM diagnosis codes for tobacco use disorder or history of tobacco use or prescription claims for smoking deterrents. The parameter estimates for tobacco use disorder and smoking-related diseases were significantly different in post hoc testing (p=0.030).
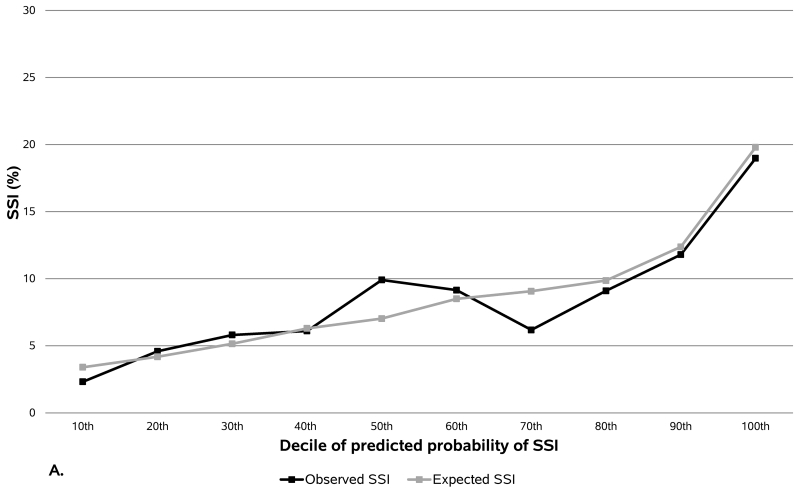
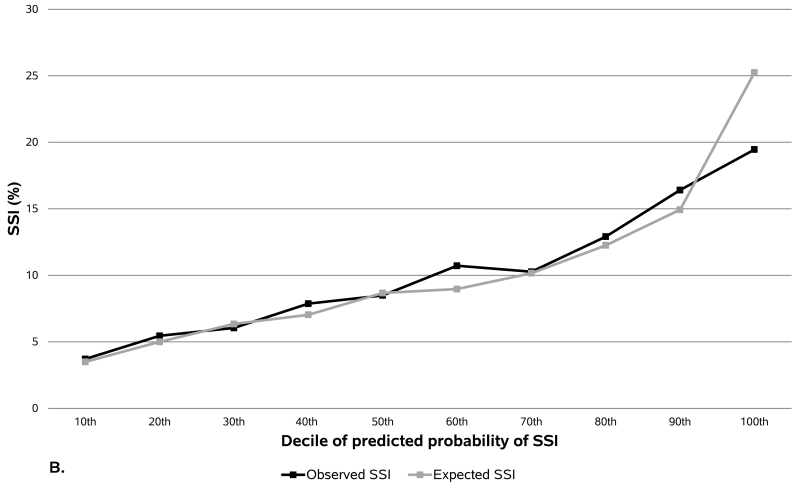
The ability of the model to discriminate between SSI and no wound complication was very similar in the derivation and validation cohorts (Table 3). The Brier score was near zero, indicating that overall the predicted values were close to the actual values in both the derivation and validation cohorts. The predicted probability of SSI in the model was well calibrated to the true outcome based on the Hosmer-Lemeshow test and observed versus predicted SSI (Figure 1). Observed SSI rates ranged from 2.3% to 19.0% for the lowest and highest deciles in the derivation cohort (Figure 1A), and from 3.7% to 19.5% in the validation cohort (Figure 1B).
Table 3.
Comparison of Model Fit, Calibration, and Discrimination of Multivariable Logistic Regression Model of Risk Factors for Surgical Site Infection (SSI) After Mastectomy, Derivation (2004–2008) Versus Validation Cohort (2009–2011)
| Derivation Cohorta | Validation Cohort – Fit Using Parameter Estimates From Derivation Modelb |
Validation Cohort – Refitting Model With Variables From Derivation Modelc |
|
|---|---|---|---|
| Hosmer-Lemeshow P | 0.091 | 0.462 | 0.635 |
| C-statistic | 0.657 | 0.649 | 0.669 |
| Brier score | 0.074 | 0.087 | 0.086 |
The derivation model was also fit with a more restricted set of variables (obesity, diabetes, smoking-related diseases, bilateral mastectomy, implant reconstruction, and flap reconstruction) to determine the impact of the additional conditions on model performance. The derivation model fit with the more restricted set of variables had a significantly lower C-statistic (0.637) compared to the full model above (P = 0.007),37 Hosmer-Lemeshow P = 0.775, and Brier score = 0.075.
The validation model was fit using the beta coefficients of all variables in the final derivation cohort model.
Model used the variables from the final derivation cohort model, re-fit in the validation cohort (i.e., parameter estimates allowed to vary compared to the derivation model).
Figure 1.
Observed versus expected surgical site infection (SSI) per the risk prediction model in the (a) derivation and (b) validation cohorts. The y-axis represents the number of observed or expected SSIs divided by the number of women in the decile, as a percentage. The validation cohort was fit using the beta coefficients from the final derivation cohort model.
Based on the predicted probability of SSI, women were classified into one of three risk strata: low (0–7.5%), moderate (7.5–15%), and high (>15%) probability of SSI risk. The majority of women with an observed SSI in both the derivation and validation cohorts were classified as moderate or high predicted risk by the risk prediction model (Table 4).
Table 4.
Distribution of Surgical Site Infections (SSIs) Within Each Predicted Risk Strata
| Derivation Cohort | Validation Cohorta | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Predicted Risk of SSI | N SSI | % With Observed SSI Within Risk Group |
% of Total Observed SSI Within Cohort |
N SSI | % With Observed SSI Within Risk Group |
% of Total Observed SSI Within Cohort |
| Low Risk (0–7.5%) | 206 | 5.3 | 34.6 | 95 | 5.8 | 24.0 |
| Moderate Risk (7.5–15%) | 278 | 10.4 | 46.7 | 193 | 10.6 | 48.7 |
| High Risk (>15%) | 111 | 18.9 | 18.7 | 108 | 18.9 | 27.3 |
Model used the beta coefficients from the final derivation cohort model in the validation cohort.
DISCUSSION
We developed and internally validated a risk prediction model for SSI after mastectomy with or without immediate reconstruction. Several risk factors we identified in our large, geographically diverse, privately insured population are novel, while others are consistent with previously reported risk factors for breast SSI.
Diabetes and obesity were associated with increased risk of SSI, confirming previous reports.4-17;21 Our finding of a dose-response for smoking and smoking-related diseases is consistent with a previous observation of progressively increased risk of SSI after breast surgery associated with light and heavy smoking.15 Rheumatologic and liver disease, hypertension, depression, and preoperative pneumonia or urinary tract infection were also independent risk factors for SSI. Hypertension may be functioning as a proxy for obesity, since 62% of the women coded for obesity were also coded for hypertension, and obesity was undercoded in our dataset compared to the U.S. adult female population (4.8% versus 36%).38 Alternatively, hypertension may be a proxy for cardiovascular or peripheral vascular disease which restrict blood flow and tissue oxygenation, increasing SSI risk. The association of preexisting infections at other sites with SSI was reported decades ago but has rarely been described since,39;40 although identification and treatment of preadmission infections is considered standard practice to decrease the risk of SSI.41
Bilateral mastectomy and immediate breast implant and flap reconstruction were operative risk factors for SSI. In previous studies, immediate implant reconstruction was associated with increased risk of SSI compared to mastectomy19;23 and flap reconstruction,8 however immediate pedicled and free transverse rectus abdominis flap reconstructions were associated with increased risk of SSI compared to implant reconstruction in another study.14 We previously reported higher risk of SSI after mastectomy with immediate reconstruction compared with mastectomy-only and after bilateral versus unilateral mastectomy using these same data,25 and others have reported increased wound complications42 or SSI23 associated with bilateral versus unilateral mastectomy. Home health care was associated with decreased risk of SSI in the derivation model, controlling for other risk factors for infection. This suggests that home health care may be an important preventive strategy, particularly for high-risk women.
To our knowledge, only Kim and colleagues have reported the results of SSI risk prediction models for mastectomy with immediate breast reconstruction. They first used 2005-2011 NSQIP data to develop an SSI risk prediction model containing 12 variables, including reconstruction type, age, BMI, higher ASA score, bleeding disorder, previous cardiac revascularization, diabetes, active smoking, dyspnea, and hypertension, with a c-statistic of 0.678.14 Kim subsequently used plastic surgeon self-reported data from the Tracking Operations and Outcomes for Plastic Surgeons database to develop a SSI risk prediction model for immediate breast reconstruction.43 This model contained 9 variables available preoperatively (age, BMI, former or current smoker, diabetes, higher ASA score, and type of reconstruction) and had a c-statistic of 0.637. Neither model has been validated with additional internal or external datasets.
Our model using private insurer claims data included patient residence, obesity, five comorbid conditions, current or history of tobacco use disorder, recent infection at a distant site, bilateral versus unilateral surgery, type of reconstruction, and home health care. All of these variables are available prior to operation, including home health, which can be included in the risk prediction model as intent to prescribe home health after surgery discharge. The model had c-statistics of 0.657 and 0.649 in the derivation and validation datasets using the derivation cohort parameter estimates, respectively, and Brier scores were < 0.10 in both datasets. We performed temporal validation of the model with subsequent years of data using the parameter estimates from the derivation model, considered an intermediate method of validation, since it is external with respect to time but internal with respect to the information present in the data.44;45
The calibration of our model was not optimal with a C-statistic of about 0.65, with values closer to 0.8 indicating good calibration (0.5 indicating random concordance and 1.0 perfect concordance). In the derivation cohort, the model predicted cases better in the highest deciles (Figure 1A), and in the validation cohort the model performed well until the highest decile in which it over-predicted SSI cases (Figure 1B). Before implementing this model, modifications including BMI to measure obesity and more accurate information concerning current and past tobacco use could potentially improve its predictive ability. We have found that the ICD-9-CM codes for obesity are a better indicator of morbid obesity than obesity per se, and miss a large proportion of women with BMI between 30 and 34 (unpublished data). In addition, inclusion of BMI would allow for capture of a dose-response with increasing BMI. Use of clinical data would allow for better discrimination between active versus past smoking, and more accurate information on comorbidities which could improve the model. External validation adapting the model to clinical data with more detailed information concerning BMI, smoking history, and relevant comorbid conditions should be performed to ensure the model is robust to data collected from medical records and different populations.
We grouped women into risk strata based on the predicted probability of SSI from the final regression model. The moderate plus high risk groups accounted for 65% of all observed SSI in the derivation cohort and 76% in the validation cohort. Since SSI is a relatively uncommon event, the percentages of women with an infection in the moderate and high risk groups were still relatively low at 10% and 19%, respectively. Communicating the predicted probability of SSI or the more general predicted risk stratum to women may be valuable during preoperative visits. This information can be used to discuss the most appropriate timing of breast reconstruction (immediate versus delayed) given the woman’s preferences and personal SSI risk. It can also be used to discuss personal risk reduction strategies (e.g., smoking cessation, losing weight before semi-elective reconstructive procedures, careful attention to glucose control and prevention of hyperglycemia46) and guide use of preventive measures by physicians (e.g., home health post-discharge, delaying surgery to ensure resolution of preexisting infection, psychiatric referral for treatment of depression). Focusing additional preventive measures in the moderate and high-risk populations (SSI risk > 7.5%) would target 45% of the population, which would be more cost-effective for interventions such as post-discharge home health.
The cumulative incidence of SSI within 180 days we found in this study was high compared to that reported by the National Surgical Improvement Project (NSQIP),11;47 although the surveillance period to identify SSI is much shorter in NSQIP (30 days) and also shorter in the National Healthcare Safety Network surveillance system (30 days, 90 days with an implant). To avoid misclassification, we used ICD-9-CM diagnosis codes in our algorithm specific for SSI. The use of only specific ICD-9-CM diagnosis codes may have resulted in under-detection of infections.48;49 We also likely missed minor infections that did not require surgical treatment or intravenous antibiotics during the 90-day global surgical reimbursement period.50 Thus, our reported incidence of SSI, even though higher than reported by NSQIP, is likely an underestimate of the true infection rate within 180 days after mastectomy.
A limitation of our study is that the data were designed for administrative rather than research purposes. As with infection, comorbidities were likely subject to undercoding and misclassification, depending on whether coding influenced reimbursement or was relevant to the encounter. We focused on women 18–64 years who are more likely to undergo breast reconstruction, and thus our findings may not be generalizable to older women or younger women lacking private health insurance.
We identified and validated risk factors for SSI after mastectomy that could be used by physicians to initiate discussion with patients of their individual risk/treatment options and care strategies to decrease infection risk. The model could also be used to facilitate discussion of the patient’s role in management of comorbidities to minimize complications and avoid delay of oncologic treatment, and to better balance the advantages of delayed reconstruction in high risk women against the perceived benefit of immediate reconstruction.
Supplementary Material
SYNOPSIS.
Using commercial claims data, we developed validated a risk prediction model for surgical site infection (SSI) after mastectomy. The patient and operative risk factors for SSI we identified are important to assess patients’ individual risk of infection.
ACKNOWLEDGMENTS
We thank Cherie Hill for database and computer management support.
FUNDING
Funding for this project was provided by the National Institutes of Health (NIH) (5R01CA149614 to MAO). Additional support was provided by the Centers for Disease Control and Prevention (CDC) Epicenters Program (U54CK000162 to VJF).
MAO reports consultant work with Pfizer, Merck, and Sanofi Pasteur and grant funding through Pfizer, Sanofi Pasteur, and Cubist Pharmaceuticals for work outside the submitted manuscript.
Footnotes
All other authors report no conflicts of interest relevant to this article.
REFERENCES
- (1).Anderson DJ, Pyatt DG, Weber DJ, Rutala WA. Statewide costs of health care-associated infections: estimates for acute care hospitals in North Carolina. Am J Infect Control. 2013;41:764–768. doi: 10.1016/j.ajic.2012.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (2).Shepard J, Ward W, Milstone A, et al. Financial impact of surgical site infections on hospitals: the hospital management perspective. JAMA Surg. 2013;148:907–914. doi: 10.1001/jamasurg.2013.2246. [DOI] [PubMed] [Google Scholar]
- (3). [November 14, 2013];National Healthcare Safety Network (NHSN) Procedure-Associated (PA) module: surgical site infection (SSI) event. Centers for Disease Control and Prevention. 2013 http://www.cdc.gov/nhsn/PDFs/pscManual/9pscSSIcurrent.pdf.
- (4).Vilar-Compte D, Rosales S, Hernandez-Mello N, Maafs E, Volkow P. Surveillance, control, and prevention of surgical site infections in breast cancer surgery: a 5-year experience. Am J Infect Control. 2009;37:674–679. doi: 10.1016/j.ajic.2009.02.010. [DOI] [PubMed] [Google Scholar]
- (5).Arver B, Isaksson K, Atterhem H, et al. Bilateral prophylactic mastectomy in Swedish women at high risk of breast cancer: a national survey. Ann Surg. 2011;253:1147–1154. doi: 10.1097/SLA.0b013e318214b55a. [DOI] [PubMed] [Google Scholar]
- (6).Davis GB, Peric M, Chan LS, Wong AK, Sener SF. Identifying risk factors for surgical site infections in mastectomy patients using the National Surgical Quality Improvement Program database. Am J Surg. 2013;205:194–199. doi: 10.1016/j.amjsurg.2012.05.007. [DOI] [PubMed] [Google Scholar]
- (7).Ogunleye AA, de BC, Curtis MS, Colakoglu S, Tobias AM, Lee BT. An analysis of delayed breast reconstruction outcomes as recorded in the American College of Surgeons National Surgical Quality Improvement Program. J Plast Reconstr Aesthet Surg. 2012;65:289–294. doi: 10.1016/j.bjps.2011.09.031. [DOI] [PubMed] [Google Scholar]
- (8).Clayton JL, Bazakas A, Lee CN, Hultman CS, Halvorson EG. Once is not enough: withholding postoperative prophylactic antibiotics in prosthetic breast reconstruction is associated with an increased risk of infection. Plast Reconstr Surg. 2012;130:495–502. doi: 10.1097/PRS.0b013e31825dbefe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (9).El-Tamer MB, Ward BM, Schifftner T, Neumayer L, Khuri S, Henderson W. Morbidity and mortality following breast cancer surgery in women: national benchmarks for standards of care. Ann Surg. 2007;245:665–671. doi: 10.1097/01.sla.0000245833.48399.9a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (10).Chun YS, Verma K, Rosen H, et al. Implant-based breast reconstruction using acellular dermal matrix and the risk of postoperative complications. Plast Reconstr Surg. 2010;125:429–436. doi: 10.1097/PRS.0b013e3181c82d90. [DOI] [PubMed] [Google Scholar]
- (11).Nguyen TJ, Costa MA, Vidar EN, et al. Effect of immediate reconstruction on postmastectomy surgical site infection. Ann Surg. 2012;256:326–333. doi: 10.1097/SLA.0b013e3182602bb7. [DOI] [PubMed] [Google Scholar]
- (12).de Blacam C, Ogunleye AA, Momoh AO, et al. High body mass index and smoking predict morbidity in breast cancer surgery: a multivariate analysis of 26,988 patients from the national surgical quality improvement program database. Ann Surg. 2012;255:551–555. doi: 10.1097/SLA.0b013e318246c294. [DOI] [PubMed] [Google Scholar]
- (13).Gart MS, Smetona JT, Hanwright PJ, et al. Autologous options for postmastectomy breast reconstruction: a comparison of outcomes based on the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2013;216:229–238. doi: 10.1016/j.jamcollsurg.2012.11.003. [DOI] [PubMed] [Google Scholar]
- (14).Kim JY, Khavanin N, Jordan SW, et al. Individualized risk of surgical-site infection: an application of the breast reconstruction risk assessment score. Plast Reconstr Surg. 2014;134:351e–362e. doi: 10.1097/PRS.0000000000000439. [DOI] [PubMed] [Google Scholar]
- (15).Sorensen LT, Horby J, Friis E, Pilsgaard B, Jorgensen T. Smoking as a risk factor for wound healing and infection in breast cancer surgery. Eur J Surg Oncol. 2002;28:815–820. doi: 10.1053/ejso.2002.1308. [DOI] [PubMed] [Google Scholar]
- (16).Khansa I, Hendrick RG, Jr., Shore A, Meyerson J, Yang M, Boehmler JH. Breast reconstruction with tissue expanders: implementation of a standardized best-practices protocol to reduce infection rates. Plast Reconstr Surg. 2014;134:11–18. doi: 10.1097/PRS.0000000000000261. [DOI] [PubMed] [Google Scholar]
- (17).Kato H, Nakagami G, Iwahira Y, et al. Risk factors and risk scoring tool for infection during tissue expansion in tissue expander and implant breast reconstruction. Breast J. 2013;19:618–626. doi: 10.1111/tbj.12175. [DOI] [PubMed] [Google Scholar]
- (18).Vilar-Compte D, Alvarez dI, I, Martin-Onraet A, Perez-Amador M, Sanchez-Hernandez C, Volkow P. Hyperglycemia as a risk factor for surgical site infections in patients undergoing mastectomy. Am J Infect Control. 2008;36:192–198. doi: 10.1016/j.ajic.2007.06.003. [DOI] [PubMed] [Google Scholar]
- (19).Olsen MA, Lefta M, Dietz JR, et al. Risk factors for surgical site infection after major breast operation. J Am Coll Surg. 2008;207:326–335. doi: 10.1016/j.jamcollsurg.2008.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (20).Selber JC, Kurichi JE, Vega SJ, Sonnad SS, Serletti JM. Risk factors and complications in free TRAM flap breast reconstruction. Ann Plast Surg. 2006;56:492–497. doi: 10.1097/01.sap.0000210180.72721.4a. [DOI] [PubMed] [Google Scholar]
- (21).Ducic I, Spear SL, Cuoco F, Hannan C. Safety and risk factors for breast reconstruction with pedicled transverse rectus abdominis musculocutaneous flaps: a 10-year analysis. Ann Plast Surg. 2005;55:559–564. doi: 10.1097/01.sap.0000184463.90172.04. [DOI] [PubMed] [Google Scholar]
- (22).Francis SH, Ruberg RL, Stevenson KB, et al. Independent risk factors for infection in tissue expander breast reconstruction. Plast Reconstr Surg. 2009;124:1790–1796. doi: 10.1097/PRS.0b013e3181bf80aa. [DOI] [PubMed] [Google Scholar]
- (23).Jagsi R, Jiang J, Momoh AO, et al. Complications after mastectomy and immediate breast reconstruction for breast cancer: a claims-based analysis. Ann Surg. 2015 doi: 10.1097/SLA.0000000000001177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (24).Mioton LM, Smetona JT, Hanwright PJ, et al. Comparing thirty-day outcomes in prosthetic and autologous breast reconstruction: a multivariate analysis of 13,082 patients? J Plast Reconstr Aesthet Surg. 2013;66:917–925. doi: 10.1016/j.bjps.2013.03.009. [DOI] [PubMed] [Google Scholar]
- (25).Olsen MA, Nickel KB, Fox IK, et al. Incidence of surgical site infection following mastectomy with and without immediate reconstruction using private insurer claims data. Infect Control Hosp Epidemiol. 2015;36:907–914. doi: 10.1017/ice.2015.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (26).Elixhauser A, Steiner C, Harris R, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- (27).American fact finder [March 10, 2015];U S Census Bureau. 2000 http://factfinder2.census.gov.
- (28).Ingram DD, Franco SJ. NCHS urban-rural classification scheme for counties. 154. Vol. 2. National Center for Health Statistics; 2012. [PubMed] [Google Scholar]
- (29).Klabunde CN, Potosky AL, Legler JM, Warren JL. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53:1258–1267. doi: 10.1016/s0895-4356(00)00256-0. [DOI] [PubMed] [Google Scholar]
- (30).Kahende JW, Woollery TA, Lee CW. Assessing medical expenditures on 4 smoking-related diseases, 1996-2001. Am J Health Behav. 2007;31:602–611. doi: 10.5555/ajhb.2007.31.6.602. [DOI] [PubMed] [Google Scholar]
- (31).Du X, Freeman JL, Goodwin JS. Information on radiation treatment in patients with breast cancer: the advantages of the linked medicare and SEER data. Surveillance, Epidemiology and End Results. J Clin Epidemiol. 1999;52:463–470. doi: 10.1016/s0895-4356(99)00011-6. [DOI] [PubMed] [Google Scholar]
- (32).National Cancer Institute . Procedure codes for SEER-Medicare analyses. National Cancer Institute; [February 9, 2015]. 2013. http://appliedresearch.cancer.gov/seermedicare/considerations/procedure_codes.html. [Google Scholar]
- (33).Du X, Goodwin JS. Increase of chemotherapy use in older women with breast carcinoma from 1991 to 1996. Cancer. 2001;92:730–737. doi: 10.1002/1097-0142(20010815)92:4<730::aid-cncr1376>3.0.co;2-p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (34).Olsen MA, Nickel KB, Margenthaler JA, et al. Increased risk of surgical site infection among breast-conserving surgery re-excisions. Ann Surg Oncol. 2015;22:2003–2009. doi: 10.1245/s10434-014-4200-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (35).Cook N, SAS Macros [February 10, 2015];Brigham & Women’s Hospital Division of Preventive Medicine. 2015 http://ncook.bwh.harvard.edu/sas-macros.html.
- (36).Raval MV, Cohen ME, Ingraham AM, et al. Improving American College of Surgeons National Surgical Quality Improvement Program risk adjustment: incorporation of a novel procedure risk score. J Am Coll Surg. 2010;211:715–723. doi: 10.1016/j.jamcollsurg.2010.07.021. [DOI] [PubMed] [Google Scholar]
- (37).Rosner B, Glynn RJ. Power and sample size estimation for the Wilcoxon rank sum test with application to comparisons of C statistics from alternative prediction models. Biometrics. 2009;65:188–197. doi: 10.1111/j.1541-0420.2008.01062.x. [DOI] [PubMed] [Google Scholar]
- (38).Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (39).Edwards LD. The epidemiology of 2056 remote site infections and 1966 surgical wound infections occurring in 1865 patients: a four year study of 40,923 operations at Rush-Presbyterian-St. Luke’s Hospital, Chicago. Ann Surg. 1976;184:758–766. doi: 10.1097/00000658-197612000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (40).Haley RW, Hooton TM, Culver DH, et al. Nosocomial infections in U.S. hospitals, 1975-1976: estimated frequency by selected characteristics of patients. Am J Med. 1981;70:947–959. doi: 10.1016/0002-9343(81)90561-1. [DOI] [PubMed] [Google Scholar]
- (41).Anderson DJ, Podgorny K, Berrios-Torres SI, et al. Strategies to prevent surgical site infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35(Suppl 2):S66–S88. doi: 10.1017/s0899823x00193869. [DOI] [PubMed] [Google Scholar]
- (42).Osman F, Saleh F, Jackson TD, Corrigan MA, Cil T. Increased Postoperative Complications in Bilateral Mastectomy Patients Compared to Unilateral Mastectomy: An Analysis of the NSQIP Database. Ann Surg Oncol. 2013;20:3212–3217. doi: 10.1245/s10434-013-3116-1. [DOI] [PubMed] [Google Scholar]
- (43).Kim JY, Mlodinow AS, Khavanin N, et al. Individualized Risk of Surgical Complications: An Application of the Breast Reconstruction Risk Assessment Score. Plast Reconstr Surg Glob Open. 2015;3:e405. doi: 10.1097/GOX.0000000000000351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (44).Altman DG, Vergouwe Y, Royston P, Moons KG. Prognosis and prognostic research: validating a prognostic model. BMJ. 2009;338:b605. doi: 10.1136/bmj.b605. doi: 10.1136/bmj.b605.:b605. [DOI] [PubMed] [Google Scholar]
- (45).Moons KG, Altman DG, Reitsma JB, et al. Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis (TRIPOD): explanation and elaboration. Ann Intern Med. 2015;162:W1–73. doi: 10.7326/M14-0698. [DOI] [PubMed] [Google Scholar]
- (46).Kao LS, Phatak UR. Glycemic control and prevention of surgical site infection. Surg Infect (Larchmt ) 2013;14:437–444. doi: 10.1089/sur.2013.008. [DOI] [PubMed] [Google Scholar]
- (47).Costa MA, Rommer E, Peric M, et al. Incidence of surgical-site infection is not affected by method of immediate breast reconstruction. Plast Reconstr Surg. 2013;132:20e–29e. doi: 10.1097/PRS.0b013e318290f87e. [DOI] [PubMed] [Google Scholar]
- (48).Yokoe DS, Noskin GA, Cunningham SM, et al. Enhanced identification of postoperative infections among inpatients. Emerg Inf Dis. 2004;10:1924–1930. doi: 10.3201/eid1011.040572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (49).Olsen MA, Fraser VJ. Use of diagnosis codes and/or wound culture results for surveillance of surgical site infection after mastectomy and breast reconstruction. Infect Control Hosp Epidemiol. 2010;31:544–547. doi: 10.1086/652155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (50).Centers for Medicare & Medicaid Services [November 14, 2013];Global Surgery Fact Sheet. Centers for Medicare & Medicaid Services. 2013 http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/GloballSurgery-ICN907166.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.