Abstract
Cardiometabolic diseases affect underserved groups disparately. Participation in health checks is also lower, widening health inequalities in society. Two-stage screening (non-invasive health risk assessment (HRA) and GP consultations for high-risk individuals) seems cost-effective, provided that drop-out rates are low in both steps. We aimed to explore the process of decision-making regarding HRA participation among underserved groups (45–70 y): native Dutch with a lower socioeconomic status (SES), Turkish, Moroccan, and Surinamese participants. We conducted a cross-sectional questionnaire study. The questionnaire comprised the following determinants: a self-formulated first reaction, a structured set of predefined determinants, and the most important barrier(s) and facilitator(s) for HRA completion. We used univariable and (stepwise) multivariate logistic regression analyses to assess which determinants were associated with HRA completion. Of the 892 participants in the questionnaire, 78% (n = 696) also completed the HRA. Moroccans and patients from GP practices with a predominantly non-Western population less often completed the HRA. A lower SES score, wanting to know one's risk, not remembering receiving the invitation (thus requiring a phone call), fear of the test result and/or adjusting lifestyle, perceived control of staying healthy, wanting to participate, and perceiving no barriers were associated with completing the HRA. We conclude that our ‘hard-to-reach’ population may not be unwilling to participate in the HRA. A more comprehensive approach, involving key figures within a community informing people about and providing help completing the HRA, would possibly be more suitable. Efforts should be particularly targeted at the less acculturated immigrants with an external locus of control.
Keywords: Cardiometabolic disease (cardiovascular disease, diabetes, and kidney disease); Participation in two-stage screening; Primary care; Underserved, high-risk populations
Highlights
-
•
Participation is lowest in GP practices with a predominant non-Western population.
-
•
Patients are positive about a health check, whether they participate or not.
-
•
Still, about one quarter of patients does not participate in the health check.
-
•
These patients do not want to know their risk and lack control over staying healthy.
-
•
Telephone follow-up is crucial as patients forget receiving the written invitation.
1. Introduction
Cardiometabolic diseases (cardiovascular disease, diabetes, and kidney disease) are leading causes of death in high-income countries (WHO, 2008). An increased risk of cardiometabolic disease is associated with a lower socioeconomic status (SES) and ethnicity (Mackenbach et al., 2008, Mackenbach et al., 1997). Among ethnic minorities in the Netherlands, cardiovascular disease is particularly prevalent among Surinamese and Turkish people (Bos et al., 2004, Leest van et al., 2002, Dijkshoorn et al., 2003). Turkish, Moroccan, and especially Hindustani Surinamese people have a higher risk of developing diabetes (Kunst et al., 2008). To early identify individuals with an increased risk of cardiometabolic disease, health checks are implemented worldwide (Dalton et al., 2011, Brunner-Ziegler et al., 2013, Amoroso et al., 2009). Several studies concluded that two-stage screening could be a cost-effective strategy (Khunti et al., 2012, Pandya et al., 2014). Two-stage screening usually refers to a non-invasive risk stratification tool, followed by a blood test during an assessment by a healthcare professional. The Dutch cardiometabolic health check imbedded in primary care follows this two-stage approach, comprising a short health risk assessment (HRA) to be completed at home, and two prevention consultations (PCs) with the GP for high-risk individuals according to the HRA (Dekker et al., 2011). This approach implies that patients can refrain from participation on two separate occasions (Assendelft et al., 2012). High drop-out rates may induce an even greater problem among underserved groups, as ethnicity and SES are inversely related to health check attendance (Dryden et al., 2012). These groups usually have greater difficulties in making an informed decision about participation (Smith et al., 2014). Presumably, higher participation rates in stage one (as a result of more informed decision-making) lead to higher participation rates in stage two. To increase informed decision-making about HRA completion, insight into its determinants plays a pivotal role. Few studies specifically investigated reasons for participation in cardiometabolic health checks of underserved groups. Studies reporting determinants in these populations exclusively focus on physical assessments at a doctor's office, not two-stage screening with risk stratification as a first step. Therefore, we conducted prior qualitative research on determinants of hypothetical HRA completion (Groenenberg et al., 2015a). These determinants were mainly of a cognitive nature and included (flawed) risk perceptions, health negligence, (health) illiteracy, and language barriers. With the current study we aim to explore the process of actual decision-making about HRA completion. Research questions were: (1) what are participants' self-formulated first reactions regarding the invitation?; (2) what predefined determinants play a role in completing the HRA?; (3) what are participants' most important barriers and facilitators?; and (4) which of the aforementioned determinants are associated with actual HRA completion?
2. Methods
2.1. Design and study population
This cross-sectional study is part of a larger study investigating reach and participation of underserved populations in the Dutch cardiometabolic health check.
Between May 2012 and December 2013, patients from six general practices were invited to participate. The six practices were located in The Hague and surroundings, and encompassed both large group as well as solo practices, and urban as well as rural environments. Patients had to be native Dutch with a lower SES or Turkish, Moroccan, or Surinamese. Ethnicity is not registered by GPs in the Netherlands, this was estimated by the researchers based on family name, and was subsequently checked by the GP. The GP also selected the native Dutch patients with a lower SES, which was afterwards corroborated with a neighborhood SES score (average income, proportion of individuals with a low income, with a low education, and without a paid job) (Social and Cultural Planning Office, 2014). These attributes are captured in one parameter: the socioeconomic status (SES) score and has been shown to be associated with deprivation in a community (Reijneveld, 1998). This score is assessed every four years by interviewing persons representing nearly each street in the Netherlands. The average SES score in the Netherlands is 0.17. Categorization of the SES scores was as follows: average to higher SES (score > 0); lower to average SES (score 0 till − 1.9); lower SES (score − 2 till − 3.9); lowest SES (score ≤ − 4).
Patients had to be 45–70 years old except for the Hindustani Surinamese. Their lower age limit was 35 years because of their genetically increased risk of diabetes. Exclusion criteria were: having (had) cardiometabolic disease, using drugs against cardiometabolic disease, or having had a complete cardiometabolic risk inventory less than a year ago (Appendix A). All patients who met the eligibility criteria (n = 1644) were invited.
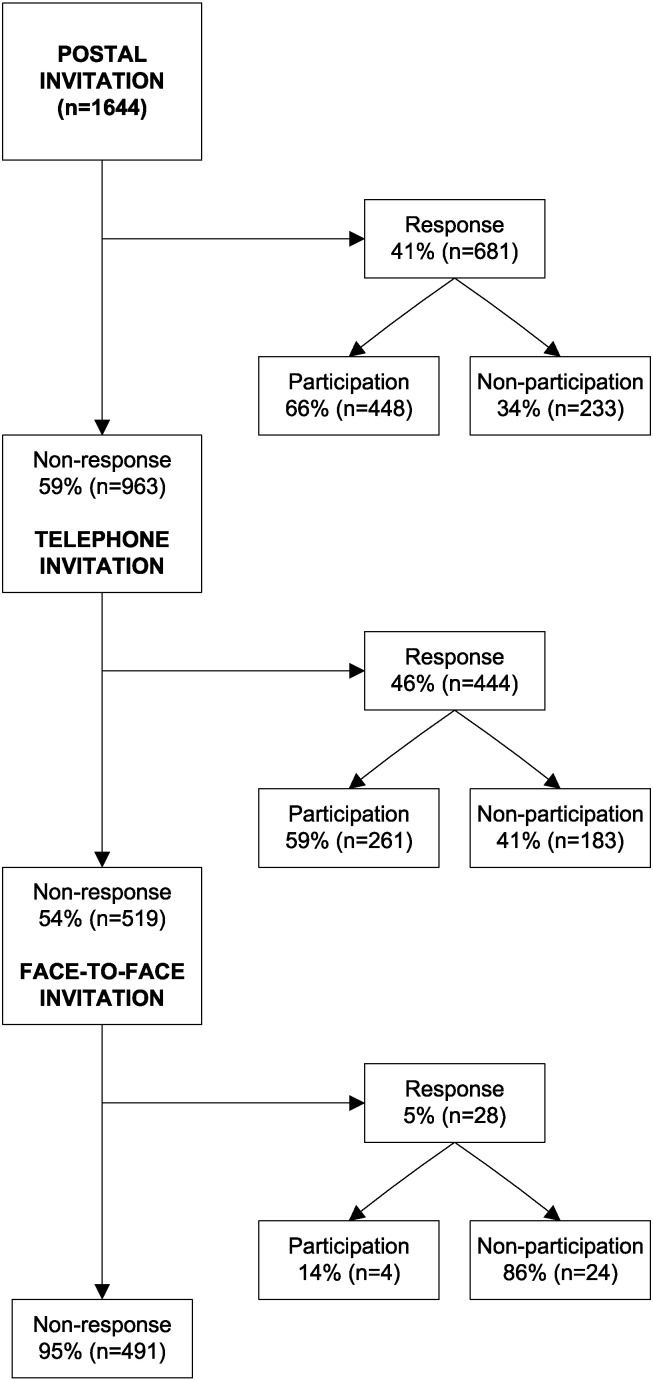
Three culturally targeted and personalized invitation steps were tested following an increasingly (cost-)intensive ‘funneled’ design: (1) all patients received a postal invitation; (2) non-reached were approached by telephone; (3) finally non-reached were approached face-to-face by their GP (Appendix A, Appendix B). The latter step was not included as participation rates were very low. Postal materials were provided in Dutch, and in Turkish/Arabic for Turkish/Moroccan patients, and included the questionnaire and the HRA simultaneously in one package. Patients were called by Turkish, Arabic, and Berber (oral-only language) speaking research assistants.
Ethical approval was given by the Committee Medical Ethics from the Leiden University Medical Center. The study followed an ‘opt-out procedure’ where patients could sign a response form when not interested in participation. The design and results of the larger study have been described in detail elsewhere (Groenenberg et al., 2015b).
The study population of this study consisted of those patients who completed the determinants questionnaire (n = 892), divided into two groups: HRA completers and non-completers. Postal responders filled out a self-administered written questionnaire and telephone responders answered the questionnaire by phone.
2.2. The questionnaire
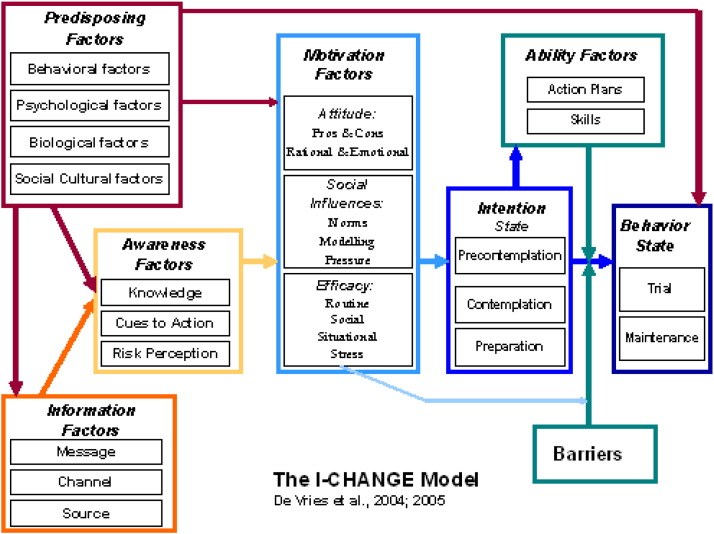
The postal- and telephone-administered questionnaires followed the same structure and were based on our previous work (Groenenberg et al., 2015a). This qualitative study was embedded in a theoretical framework based on the I-change model (Fig. 1), which aims to explain health behaviors and has been applied in studies among native and immigrant populations (Knops-Dullens et al., 2007, Vries de et al., 2005, Nierkens et al., 2006, Nierkens et al., 2005). The most important determinants in the qualitative study were turned into (simply formulated) questions. The questionnaire was pilot-tested among the target population. We incorporated three steps in the questionnaire: (1) a self-formulated first reaction regarding the invitation for the health check, (2) a structured set of predefined determinants that the participant could indicate to be of importance to his/her HRA completion, (3) most important barrier(s) and most important facilitator(s) regarding HRA completion (Appendix A, Appendix C).
Fig. 1.
The I-change model, from http://www.maastricht-university.eu/hein.devries/interests/i-change-model.
2.2.1. Step one: self-formulated first reaction
The questionnaire started with one (open answer) question prompting participants to express their thoughts about the invitation. Any reaction was possible: from positive to negative attitudes regarding the initiative, and from practical barriers to positive social influences. This and the open answer questions of step three were coded inductively and converted into a code tree. Coding was performed by the first author and randomly double coded by the second author. Both authors categorized the codes in the code tree conform the I-change model constructs (Appendix A, Appendix D). Codes and constructs were entered into SPSS. The first reactions were then computed into dichotomized variables representing the different reactions (0 = not mentioned, 1 = mentioned).
2.2.2. Step two: structured set of predefined determinants
The questionnaire continued with a structured set of predefined (multiple-choice) determinant questions. These determinants were categorized under the appropriate I-change construct (see Results, Table 3). Most questions consisted of three answer categories (mostly ‘no’, ‘a little’, ‘yes’), which were dichotomized for a better distribution.
Table 3.
Descriptive and univariable logistic regression analyses of step two: structured set of predefined determinants of HRA completion, for postal and telephone participants (n = 892).a
| HRA completers, %n agreement with factor, n = 696 | HRA non-completers, %n agreement with factor, n = 196 | OR (95% CI) of completing the HRA | Corresponding questiona | |
|---|---|---|---|---|
| Information factors; guidance | 74.6 | 70.1 | 1.25 (0.88–1.78) | ‘Do you trust you will get the guidance you need if you have an increased risk?’ |
| Awareness factors; prior experience | 25.2 | 28.4 | 0.85 (0.59–1.21) | ‘Have you ever done a health check for cardiovascular disease, diabetes, or kidney disease before?’ |
| Awareness factors; health complaints | 52.7 | 60.2 | 0.74 (0.53–1.02) | ‘Do you have one or more health complaints at the moment?’ |
| Awareness factors; perceived risk | 54.6 | 59.6 | 0.82 (0.59–1.13) | ‘Do you think the chance of getting these diseases is average to high? |
| Awareness factors; knowing risk | 91.2 | 85.6 | 1.73 (1.07–2.80)⁎ | ‘Do you want to know what your chance of these diseases is?’ |
| Motivation factors; fear test result | 23.4 | 28.5 | 0.77 (0.54–1.10) | ‘Are you afraid of the test result?’ |
| Motivation factors; fear adjusting lifestyle | 25.9 | 32.0 | 0.74 (0.53–1.05)⁎⁎ | ‘Are you afraid that you have to adjust your lifestyle habits?’ |
| Motivation factors; locus of control | 59.2 | 46.2 | 1.69 (1.23–2.33)⁎⁎⁎ | ‘Do you think you can control staying healthy?’ |
| Motivation factors; social influences | 67.7 | 59.9 | 1.40 (1.00–1.96)⁎ | ‘Do others find it important for you to participate?’ |
CI = confidence interval, NA = not applicable.
Occasional slight adjustments in formulation so all questions are answered with yes/no.
p < .05.
p < .01.
p < .001.
2.2.3. Step three: most important barriers and facilitators
The final two (open answer) questions aimed to unravel what participants perceived to be the most important barrier(s) and facilitator(s) for HRA completion. The telephone questions were rephrased to match the willingness to complete the HRA: e.g. when the participant indicated to be willing to complete the HRA, the barrier(s) question was rephrased as ‘what could be a disadvantage for you of completing the HRA?’. Coding of these questions was performed as described under step one.
2.3. Measures
Primary outcome measure was HRA completion (no/yes). Patient characteristics were: gender, ethnicity, age, and SES score. We also looked at the predominant patient population of a GP practice: native Dutch with a lower SES, mixed, or non-Western immigrants.
2.4. Data analyses
Descriptive analyses were used to describe the patient population. Differences regarding sociodemographic characteristics between the patients in the postal versus the telephone step were assessed by means of t-tests and ANOVA.
(Univariable) Logistic regression analyses were performed to explore the associations with HRA completion. First, we assessed the influence of the first reactions variable as a categorical variable (reference group: not having provided a reaction); second, the influence of the structured set of predefined determinants; third, the most important barriers and facilitators. The facilitators and barriers were included jointly in the regression model as patients could report more than one barrier or facilitator. Significant associations with HRA-completion (p < 0.05) from these initial analyses were included in a final stepwise multivariate logistic regression model. By adding the various constructs in a stepwise manner, we investigated which associations remained significant when adjusting for each other. The first step included the relevant sociodemographic variables (model 1). Each consecutive step added the significant determinants from respectively self-formulated first reactions (model 2), predefined determinants (model 3), and most important barrier(s) and facilitator(s) (model 4).
Because the number of telephone participants who did not complete the HRA was very low, stratified analyses for the telephone step could not be performed. Only strategy-dependent or very notable differences between postal and telephone participants are highlighted in the text.
3. Results
3.1. Demographics
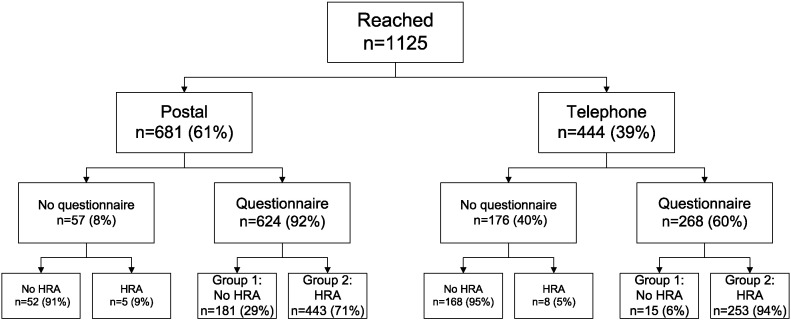
Of the 1644 eligible patients, 1125 responded to the invitation (response rate: 68%) by either completing the HRA or answering that they did not want to participate. Of those who responded to the invitation, 892 participated in the questionnaire (participation rate: 79%). Among the postal responders (n = 681), this percentage was 92% (n = 624); among the telephone responders (n = 444), it was 60% (n = 268) (Fig. 2). Not surprisingly, the questionnaire participants differed from the non-participants regarding all demographic factors except for age (data not shown). The non-participants were more often male (p < 0.001), Moroccan or Surinamese (p < 0.001), from a GP practice with a predominantly non-Western patient population, and with a lower SES score (p = 0.039).
Fig. 2.
Flowchart of individuals reached by mail or telephone and their participation in the questionnaire and in the health risk assessment (HRA).
Telephone participants were more often from a GP practice with a predominantly non-Western patient population and had a lower SES score than postal participants (Table 1). Gender, ethnicity, and age were similarly distributed between postal and telephone participants.
Table 1.
Sociodemographic characteristics of all questionnaire participants, and stratified by those reached by postal and telephone invitation.
| Total (n = 892) |
Postal (n = 624) |
Telephone (n = 268) |
p value | ||||
|---|---|---|---|---|---|---|---|
| n (%) | Mean (SD) | n (%) | Mean (SD) | n (%) | Mean (SD) | ||
| Gender | |||||||
| Male | 441 (49) | 314 (50) | 127 (47) | .207 | |||
| Female | 451 (51) | 310 (50) | 141 (53) | ||||
| Ethnicity | |||||||
| Dutch | 264 (30) | 193 (31) | 71 (27) | .179 | |||
| Turkish | 207 (23) | 148 (24) | 59 (22) | ||||
| Moroccan | 169 (19) | 120 (19) | 49 (18) | ||||
| Surinamese | 252 (28) | 163 (26) | 89 (33) | ||||
| Age (years) | 50 (6.7) | 51 (6.6) | 49 (6.5) | .247 | |||
| 30–44 | 111 (12) | 60 (10) | 51 (19) | ||||
| 45–49 | 344 (39) | 235 (38) | 109 (41) | ||||
| 50–54 | 226 (25) | 162 (26) | 64 (24) | ||||
| 55–59 | 115 (13) | 90 (14) | 25 (9) | ||||
| 60–64 | 63 (7) | 51 (8) | 12 (5) | ||||
| 65 + | 33 (4) | 26 (4) | 7 (3) | ||||
| Predominant GP practice population | |||||||
| Dutch | 226 (25) | 165 (26) | 61 (23) | .024 | |||
| Mix | 127 (14) | 99 (16) | 28 (10) | ||||
| Non-Western | 539 (60) | 360 (58) | 179 (67) | ||||
| SES score | − 2.0 (2.5) | − 1.9 (2.4) | − 2.2 (2.6) | .043 | |||
| Average to higher (> 0) | 283 (32) | 204 (33) | 79 (29) | ||||
| Lower to average (0 till − 1.9) | 202 (23) | 144 (23) | 58 (22) | ||||
| Lower (− 2 till − 3.9) | 130 (15) | 94 (15) | 36 (13) | ||||
| Lowest (≤− 4) | 277 (31) | 182 (29) | 95 (35) | ||||
Of the questionnaire participants, 78% completed the HRA. Among the postal questionnaire participants, the completion rate was 71%, among the telephone questionnaire participants, it was 94%. A minority of the patients (7%) who did not fill out the questionnaire did complete the HRA.
3.2. The decision making process
3.2.1. Step one: self-formulated first reaction to the invitation
Table 2 presents the association of the self-formulated first reactions with HRA completion. In this table, we describe the frequencies of the different first reactions. The first reaction variables were entered into a univariable regression analysis (reference group: not having provided a reaction) to explore which reactions were most important for HRA completion.
Table 2.
Descriptive and multivariate logistic regression analyses regarding step one: self-formulated first reaction in response to the HRA invitation, for postal and telephone participants (n = 892), coded according to I-change model constructs.
| I-change construct | HRA completers, %n with this reaction n = 696 | HRA non-completers, %n with this reaction n = 196 | OR (95% CI) of completing the HRA | Main exemplification |
|---|---|---|---|---|
| Not answered | 10.3 | 23.5 | 1.00 | |
| Information factors; positive | 13.2 | 8.2 | 1.89 (1.08–3.32)⁎ | ‘Initiative GP/researcher/other’ |
| Information factors; negative | 4.6 | 1.0 | 6.44 (1.49–27.90)⁎ | ‘Cannot remember/have not received invitation’ |
| Awareness factors; positive | 12.9 | 10.2 | 1.39 (0.83–2.35) | ‘Obtain insight into risks’, ‘importance prevention’, ‘health/healthy aging’ |
| Awareness factors; negative | 3.0 | 3.6 | 1.06 (0.44–2.58) | ‘More useful for others’ |
| Motivation factors; positive/rational attitude | 57.8 | 55.1 | 1.53 (1.06–2.20)⁎ | ‘Good’, ‘positive’, ‘important’ |
| Motivation factors; negative/emotional attitude | 2.9 | 4.6 | 0.88 (0.38–2.06) | ‘Unnecessary’ |
| Motivation factors; positive social influences | 1.1 | 0 | NA | ‘Action linkage: help from others’ |
| Intention state; precontemplation | 1.7 | 3.6 | 0.69 (0.26–1.88) | ‘Not wanting to participate’ |
| Intention state; contemplation | 14.4 | 8.2 | 2.30 (1.29–4.08)⁎⁎ | ‘Wanting to participate’ |
| Barriers | 4.2 | 0.5 | 13.88 (1.85–104.21)⁎ | ‘No time’ |
| Ability factors | 3.7 | 3.1 | 2.10 (0.82–5.40)⁎⁎⁎ | ‘Having no barriers’ |
| Other | 4.3 | 2.6 | 2.33 (0.87–6.26) | Not specified |
CI = confidence interval, NA = not applicable.
p < .05.
p < .01.
p < .001.
In total, 13% of the participants did not provide a first reaction, most often when they did not complete the HRA. When a first reaction was provided, usually it was a positive or rational attitude (‘good’ or ‘useful’). A positive attitude towards the invitation was associated with HRA completion, as well as expressing the intention to complete the HRA.
Paradoxically, those who mentioned negative information factors (not remembering having received an invitation) and barriers to participating (having no time) were more likely to complete the HRA. This was mainly due to the telephone participants who did not remember the postal invitation or said to have had no time to participate, but were apparently able or willing to answer it when approached by phone (separate analyses on postal participants only, ORs not significant anymore: negative information factors p = 0.627, barriers p = 0.477, data not shown).
3.2.2. Step two: structured set of predefined determinants
Table 3 presents the influence of the predefined determinants on HRA completion, analyzed by means of univariable logistic regression. Missing values varied from n = 4 (locus of control question) to n = 34 (social influences question), but were usually limited. The HRA completers were more likely than the non-completers of wanting to know their risk, of thinking that staying healthy can be controlled, and of having others finding it important for them to participate. Postal participants having one or more health complaints less often completed the HRA (separate analyses on postal participants only: OR 0.68, 95% CI 0.48–0.97, data not shown), while for the group as a whole (postal and telephone participants) we found no association.
3.2.3. Step three: most important barrier(s) and facilitator(s)
Table 4 presents the most important barrier(s) and facilitator(s) and their relation with HRA completion. A regression analysis was conducted including both the barriers and facilitators to assess which of them were significantly related to HRA-completion. Almost half of the participants did not answer the most important barrier(s) question and were less likely to complete the HRA. Those who did answer most often reported having no barriers (37%) or having a negative or emotional attitude (29%). Positive awareness factors (‘obtaining insight into risks’) were most often mentioned as important facilitator(s) (77%).
Table 4.
Descriptive and multivariate logistic regression analyses regarding step three: most important barrier(s) and facilitator(s) of HRA completion, for postal and telephone participants (n = 892).
| HRA completers, %n with this barrier/facilitator n = 696 | HRA non-completers, %n with this barrier/facilitator n = 196 | OR (95% CI) of completing the HRA | Main exemplification | |
|---|---|---|---|---|
| Not answered | 38.2 | 62.2 | 1.00 | |
| Information factors; negative | 3.3 | 4.1 | 1.10 (0.48–2.55) | ‘Privacy’ |
| Awareness factors; negative | 12.5 | 11.2 | 1.62 (0.97–2.86) | ‘No health complaints’ |
| Motivation factors; negative/emotional attitude | 18.4 | 8.2 | 3.39 (1.94–5.38)⁎⁎⁎ | ‘Fear for the test result’, ‘Afraid to have to adjust lifestyle habits’ |
| Motivation factors; negative social influences | 0.4 | 0 | NA | ‘Action linkage: no help from others’ |
| Intention state; precontemplation | 0.6 | 0.5 | 0.95 (0.10–9.38) | ‘Not wanting to participate’ |
| Barriers | 4.0 | 5.1 | 1.06 (0.50–2.26) | ‘No time’ |
| Ability factors | 23.6 | 10.2 | 3.57 (2.15–5.95) ⁎⁎⁎ | ‘Having no barriers’ |
| Other | 2.2 | 2.0 | 1.56 (0.51–4.79) | |
| Not answered | 11.6 | 24.5 | 1.00 | |
| Information factors; positive | 4.5 | 5.1 | 1.18 (0.53–2.60) | ‘Knowledge development GP/researcher/other’, ‘Trust in guidance’ |
| Awareness factors; positive | 68.0 | 57.1 | 1.67 (1.16–2.39)⁎⁎ | ‘Obtain insight into risks’, ‘healthy aging’ |
| Awareness factors; negative | 4.0 | 4.6 | 1.22 (0.55–2.72) | ‘Already health complaints/already ill/receiving treatment’ |
| Motivation factors; positive/rational attitude | 18.1 | 12.8 | 1.63 (1.01–2.62)⁎ | ‘Important’ |
| Motivation factors; negative/emotional attitude | 1.4 | 0.5 | 3.64 (0.46–28.97) | ‘Worries about health’ |
| Motivation factors; positive social influences | 1.9 | 0.5 | 3.82 (0.49–29.68) | ‘Important for offspring |
| Motivation factors; negative social influences | 0.1 | 1.0 | 0.20 (0.02–2.39) | ‘Social pressure’ |
| Intention state; contemplation | 7.9 | 9.2 | 0.80 (0.45–1.42) | ‘Wanting to participate’ |
| Ability factors | 2.9 | 4.6 | 0.85 (0.37–1.95) | ‘Having no facilitators’ |
| Other | 2.3 | 3.1 | 0.90 (0.34–2.40) |
CI = confidence interval, NA = not applicable.
p < .05.
p < .01.
p < .001.
Participants who indicated fear (mainly for the test result) to be their most important barrier or who perceived no barriers (hence, ability factor) more often completed the HRA. Participants who expressed obtaining insight into risks and finding it important as their most important facilitator more often completed the HRA.
3.2.4. Stepwise model of determinants for HRA completion
Significant associations with HRA-completion (p < 0.05) from the initial analyses were included in a final stepwise multivariate logistic regression model. Step one of the stepwise model showed that the probability of HRA completion was highest among participants with a lower SES (score − 2 till − 3.9), and lowest among Moroccan participants and patients from non-Western GP practices (Table 5). Each consecutive model added the significant determinants from respectively self-formulated first reactions (model 2), predefined determinants (model 3), and most important barrier(s) and facilitator(s) (model 4). In model 2, the self-formulated first reactions significant in the initial analyses remained significantly associated with HRA completion when adjusted for characteristics of model 1, except for the positive/rational attitude. In model 3, the significant association between HRA completion and wanting to know one's risk and perceived control over staying healthy remained significant. Positive social influences were no longer significantly associated with HRA completion. In the final model the negative information factors and the contemplation state remained the only significant first reactions associated with HRA completion. The significant associations from model 3 were supplemented with fear regarding the test result and reporting no barriers, which both remained positively associated with HRA completion. The Nagelkerke R square indicates that 24% of the variance was explained by the final model.
Table 5.
Stepwise multivariate logistic regression analyses presenting associations with HRA completion for postal and telephone participants, OR (95% CI).
| Variable | Model 1 OR (95% CI) |
Model 2 OR (95% CI) |
Model 3 OR (95% CI) |
Model 4 OR (95% CI) |
|---|---|---|---|---|
| Ethnicity | ||||
| Dutcha | 1.00 | 1.00 | 1.00 | 1.00 |
| Turkish | 0.58 (0.30–1.10) | 0.51 (0.26–1.01) | 0.47 (0.23–0.95)⁎ | 0.61 (0.29–1.27) |
| Moroccan | 0.44 (0.25–0.78)⁎⁎ | 0.40 (0.22–0.73)⁎⁎ | 0.35 (0.19–0.66)⁎⁎ | 0.38 (0.20–0.74)⁎⁎ |
| Surinamese | 0.89 (0.46–1.73) | 0.80 (0.40–1.58) | 0.68 (0.34–1.38) | 0.82 (0.39–1.72) |
| GP practice | ||||
| Dutcha | 1.00 | 1.00 | 1.00 | 1.00 |
| Mix | 0.70 (0.37–1.33) | 0.70 (0.36–1.35) | 0.69 (0.35–1.34) | 0.67 (0.33–1.34) |
| Non-Western | 0.45 (0.23–0.88)⁎ | 0.44 (0.22–0.88)⁎ | 0.43 (0.21–0.87)⁎ | 0.33 (0.16–0.69)⁎⁎ |
| SES score | ||||
| Average to higher (> 0)a | 1.00 | 1.00 | 1.00 | 1.00 |
| Lower to average (0 till − 2) | 1.54 (0.92–2.57) | 1.41 (0.83–2.39) | 1.52 (0.88–2.60) | 1.69 (0.96–2.96) |
| Lower (− 2 till − 3.9) | 1.82 (1.01–3.29)⁎ | 1.87 (1.02–3.43)⁎ | 1.87 (1.01–3.46)⁎ | 2.13 (1.12–4.07)⁎ |
| Lowest (≤− 4) | 1.14 (0.69–1.88) | 1.11 (0.66–1.88) | 1.12 (0.66–1.91) | 1.20 (0.69–2.09) |
| Self-formulated first reactionb | ||||
| Not answered | 1.00 | 1.00 | 1.00 | |
| Information factors; positive | 2.24 (1.23–4.06)⁎⁎ | 2.13 (1.17–3.88)⁎ | 1.76 (0.94–3.31) | |
| Information factors; negative | 6.75 (1.53–29.79)⁎ | 6.98 (1.56–31.20)⁎ | 6.57 (1.29–33.43)⁎ | |
| Motivation factors; positive/rational attitude | 1.45 (0.98–2.15) | 1.38 (0.92–2.05) | 1.22 (0.80–1.88) | |
| Intention state; contemplation | 2.34 (1.27–4.30)⁎⁎ | 2.24 (1.22–4.12)⁎ | 2.19 (1.16–4.13)⁎ | |
| Barriers | 9.19 (1.20–70.22)⁎ | 7.95 (1.04–61.04)⁎ | 4.56 (0.57–36.70) | |
| Predefined determinants | ||||
| Awareness factors; knowing risk | 2.36 (1.28–4.34)⁎⁎ | 1.99 (1.02–3.88)⁎ | ||
| Motivation factors; locus of control | 1.61 (1.13–2.30)⁎⁎ | 1.63 (1.12–2.36)⁎ | ||
| Motivation factors; social influences | 1.25 (0.86–1.82) | 1.20 (0.81–1.77) | ||
| Most important barrier(s)b | ||||
| Not answered | 1.00 | |||
| Motivation factors; negative/emotional attitude | 3.25 (1.69–6.25)⁎⁎⁎ | |||
| Ability factors | 3.85 (2.14–6.95)⁎⁎⁎ | |||
| Most important facilitator(s)b | ||||
| Not answered | 1.00 | |||
| Awareness factors; positive | 1.12 (0.72–1.74) | |||
| Motivation factors; positive/rational attitude | 1.38 (0.81–2.35) | |||
| Nagelkerke R square | 0.07 | 0.15 | 0.17 | 0.24 |
OR = odds ratio, CI = confidence interval
Reference category.
All answer categories are included, only those significant in first step are presented.
p < .05.
p < .01.
p < .001.
4. Discussion
4.1. Conclusion
More than three quarters of the questionnaire participants also completed the HRA, mostly patients in the lower SES group. Those who did not were more often of Moroccan origin or from a non-Western GP practice. The self-formulated first reactions were generally positive and many participants expressed the wish to participate. Barriers formulated as first reaction were mostly not remembering receiving the postal invitation or not having (had) time, thus requiring a phone call. Although positive at first, when HRA non-completers further considered participation they more often did not want to know their risk and were less certain of their ability to control staying healthy. Most of the completers reported having no barriers at all. Some of them ventilated fear for the test result, but this did not prevent them from completing the HRA.
4.2. Strengths and weaknesses
To our knowledge, this is the first study exploring the decision making process of underserved populations regarding their completion in the first stage (HRA) of a cardiometabolic health check. The main strength of the study is the exertion to study both HRA completers and non-completers in the context of actual decision-making, reducing potential hypothetical bias. Given the lower levels of (health) literacy levels among these underserved groups, questionnaire missings were limited. This study was embedded in an encompassing theoretical framework. We chose this model as health check attendance can be seen as a health behavior and in that sense be studied with this comprehensive model. In addition to our positive experiences in explaining determinants of hypothetical HRA completion (Groenenberg et al., 2015a) we conclude that the I-change model is also valuable in explaining determinants of actual HRA completion.
Some limitations should be noted. First, given the lower (health) literacy levels of our populations, it is debatable whether the participants were able to formulate their answers in a way that really reflected their opinions. Those with the lowest literacy levels may have more often skipped questions that were difficult for them to fill out (i.e. the open answer questions). The open answer questions were also more often skipped by the HRA non-completers. Related to this is the fact that we tried to make the postal and telephone questionnaire as similar as possible. It cannot be denied, however, that during the telephone questionnaire our populations may have more easily elaborated on their answers when compared to the self-administered questionnaire. Also, our rephrasing of the barriers/facilitators question may have resulted in slight differences in information obtained, but not rephrasing would have led to unnatural conversations as the research assistant would not react to the willingness already expressed by the participant. Second, all GP practices were located in The Hague and surroundings. It is, therefore, debatable whether the findings from these practices are generalizable to other practices in the Netherlands, let alone other countries. Nevertheless, we do not expect major differences with other practices with similar lower SES/ethnic groups. We expect the major differences to occur between ethnic groups, and between socioeconomic strata. Increasing the chance of generalizability was the fact that we included both large group as well as solo practices, and urban as well as rural environments. Third, potential residual confounding may have been present due to possible errors in the estimation of ethnicity based on last name and because the SES score was a neighborhood score and not an individual score. Fourth, in the larger study we have not reached 30% of the patients, of whom we have no information on determinants of their HRA non-completion whatsoever. Aiming to reduce health inequalities, obtaining insight into the determinants of particularly these non-participants is important. Fifth, we used a cross-sectional study design. This means that we cannot conclude that the correlates we found caused the HRA completion. We can conclude that some differences exist between HRA completers and non-completers. Finally, it is possible that our simultaneously sending a questionnaire for research purposes led to distrust among some individuals, as we have shown before to be a potential problem for these vulnerable groups (Groenenberg et al., 2015a). With this simultaneous sending and our structured design of the questionnaire we might also have enabled participants to reflect on participation and to make an informed decision about HRA completion. However, we have no control group, nor a measure for informed decision making, allowing us to draw a conclusion about whether we have succeeded.
4.3. Comparison with other studies
We aimed to explore the process of decision making regarding HRA completion among underserved populations. Most first reactions provided were positive, possibly because patients felt obliged to react positively or to provide some excuse for not having completed the HRA. Which raises the question on the value of these reactions for explaining HRA participation. In the final model, most of the associations of these positive first reactions with participation disappeared. The only negative first reaction (not remembering/receiving the invitation) remained significantly associated with HRA participation. This implies that this determinant may not have been used as an excuse, and follow-up by telephone may actually be crucial.
Despite the generally positive self-formulated first reactions, still about a quarter did not complete the HRA. A qualitative investigation among non-responders to the NHS health check concluded that participants viewed the health check positively, but lacked personal relevance (Ellis et al., 2015). They concluded that, perhaps, people considered themselves in good health or had regular contact with primary care for their health complaints. To promote personal relevance and more informed decision making, it has been proposed to provide more personalized risk communication and using telephone/verbal methods (Ellis et al., 2015, Burgess et al., 2014). In the current study, patients with health complaints less often participated in the postal HRA, but not so in the telephone HRA. This indicates that personalized risk communication by telephone may increase personal relevance. It has been found that up to 40% of non-participants in cardiovascular screening would reconsider their participation decision when given additional information (Sogaard et al., 2013).
The argument of not wanting to know one's risk is in line with findings of other studies (McAndrew et al., 2008, Farrimond et al., 2010). The current study adds that participation in a health check is influenced by a perceived lack of control over staying healthy. This external locus of control may also imply that the HRA non-completers were the less acculturated minorities, as they more often feel that the doctor, God, or a higher power could help prevent cardiometabolic disease, rather than they themselves (Edelman et al., 2009). Indeed, HRA completion was lowest in non-Western GP practices, situated in neighborhoods with stronger non-Western communities, with generally lower acculturation rates. Additionally, Turkish and Moroccan immigrants had the lowest HRA completion rates and have been found to be less acculturated than Surinamese immigrants, and less often participate in Dutch society (Nap et al., 2014). Efforts should, therefore, be particularly targeted at the less acculturated immigrants, emphasizing the modifiability of cardiometabolic disease through lifestyle changes and boosting the confidence in their own abilities.
Interestingly, the most important barrier expressed by the completers was fear of the test result. However, as the results of the predefined set of determinants showed, many were not actually scared of the test result. This barrier may, thus, have been a potential barrier imagined to be applicable to others in the same situation. On the other hand, these participants may have participated despite of their anxiety so that in case of a high-risk test result, they would at least know that they would experience the benefits of early diagnosis (Kaltsa et al., 2013, Hennelly et al., 2014). Indeed, a large majority of these HRA completers expressed their most important facilitator to be obtaining insight into risks.
4.4. Implications and future research
To explore the influence of perceived personal relevance on informed decision making, future studies should focus on personalized/verbalized cardiometabolic risk communication, emphasizing the modifiability of cardiometabolic risk factors and boosting the confidence of these underserved groups. Most of our underserved participants, often depicted as ‘hard-to-reach’, had a positive attitude towards the cardiometabolic health check. This, combined with the strongest correlates being not remembering having received an invitation and having had no time (thus requiring a phone call), gives rise to the idea that these groups may not be hard-to-reach in the sense that they are unwilling to complete the HRA. The results of this pragmatic intervention provide interesting leads for follow-up by means of a controlled study. Special efforts should then be made at those ‘hardest-to-reach’. A more comprehensive approach, including the involvement of key figures within a community informing people about and providing help with the HRA (reducing the amount of time needed) would possibly be more suitable for these groups. Efforts should be particularly aimed at the less acculturated immigrants.
Conflicts of interest
The authors declare that there are no conflicts of interest.
Authors' contributions
MC, SD, WG, and AS filed the proposal for this study. The design, execution, and analysis were mainly done by IG and MC, in close collaboration with the research team. The paper was written by IG and critically revised by all authors. All authors had full access to all of the data in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis. IG is guarantor.
Funding
This study was funded by the Dutch Heart Foundation, the Dutch Diabetes Foundation, and the Dutch Kidney Foundation in a collaboration called LekkerLangLeven [Living nice and long] (2008.20.005). The views presented in this manuscript are those of the authors and do not necessarily reflect those of the study funders.
Ethical approval
This study was approved by the Medical Ethical Committee of Leiden University Medical Center (P11.151).
Transparency document
Transparency document
Acknowledgments
The authors thank all GP practices for their cooperation in conducting the study at their locations, and the patients in particular for their participation.
Footnotes
The Transparency document associated with this article can be found, in online version.
Contributor Information
I. Groenenberg, Email: i.groenenberg@lumc.nl.
M.R. Crone, Email: m.r.crone@lumc.nl.
S. van Dijk, Email: s.van_dijk@lumc.nl.
J. Ben Meftah, Email: j.ben_meftah@lumc.nl.
B.J.C. Middelkoop, Email: b.j.c.middelkoop@lumc.nl.
W.J.J. Assendelft, Email: w.assendelft@elg.umcn.nl.
A.M. Stiggelbout, Email: a.m.stiggelbout@lumc.nl.
Appendix A. Exclusion criteria
-
•Having (had) one or more of the following diseases (in ICPC codes):
-
oK74 ANGINA PECTORIS
-
oK75 ACUTE MYOCARDIAL INFARCTION
-
oK76 OTHER CHRONIC ISCHEMIC HEART DISEASES
-
oK77 CONGESTIVE HEART FAILURE
-
oK78 ATRIAL FIBRILLATION/-FLUTTER
-
oK79 PAROXYSMAL TACHYCARDIA
-
oK82 COR PULMONARY
-
oK83 VALVE DISEASE NOT RHEUMATIC/NOS
-
oK84 OTHER HEART DISEASES
-
oK86 HYPERTENSION WITHOUT ORGAN DAMAGE.
-
oK87 HYPERTENSION WITH ORGAN DAMAGE.
-
oK89 TRANSIENT CEREBRAL ISCHEMIA/TIA
-
oK90 CEREBROVASCULAR ACCIDENT (CVA) [EX.TIA]
-
oK91 ATHEROSCLEROSIS [EX.CORON.,CEREBR.]
-
oK92 OTHER DISEASES PERIFERAL ARTERIES
-
oT90 DIABETES
-
oT93 LIPID DISORDER
-
oU88 GLOMERULONEPHRITIS/NEFROSIS
-
oU99 OTHER DISEASES URINARY TRACT
-
o
-
•Use of one of the following drugs (in ATC-classifications):
-
oA10 ANTIDIABETICS
-
oB01/C01/C02/C03/C07/C08/C09 ANTIHYPERTENSIVES
-
oC10 ANTILIPAEMICS
-
o
-
•Complete risk profile with a maximum of one year old with a known measurement for all of the following factors:
-
oSmoking status
-
oComments on characteristics of diet
-
oPhysical activity
-
oAlcohol use
-
oBMI
-
oWaist circumference
-
oSystolic blood pressure
-
oFasting glucose
-
oLDL
-
o
Appendix B
Fig. B.1.
Results of response and participation in three culturally targeted and personalized invitation steps following an increasingly (cost-)intensive ‘funneled’ design.
Appendix C
| Question | Answer options |
|---|---|
| 1. What is your first reaction about this invitation? | Open |
| 2. Have you ever done a health check for cardiovascular disease, diabetes, or kidney disease before? | No (or for something else) — Yes, more than 1 year ago — Yes, less than 1 year ago |
| 3. Are you afraid of the result? | No — A little — Yes |
| 4. Are you afraid that you have to adjust your lifestyle habits? | No — A little — Yes |
| 5. Do you trust you will get the guidance you need if you have an increased risk? | No — A little — Yes |
| 6. Do you have health complaints at the moment? | None — One — A couple |
| 7. How high do you think your chance is of getting these diseases? | Small — Average — High |
| 8. Do you want to know what your chance of these diseases is? | No — Dubiety — Yes |
| 9. Do you think you can control staying healthy? | No — Partly — Yes |
| 10. Do others find it important for you to participate? | No — Little — Yes |
| 11. What is the most important reason for you not to participate in the HRA? Of course, this may be another reason than what has been mentioned above. Also fill out this question if you do participate in the HRA! | Open |
| 12. What is the most important reason for you to do participate in the HRA? Of course, this may be another reason than what has been mentioned above. Also fill out this question if you do not participate in the HRA! | Open |
Appendix D
Code tree assigned to I-change constructs
Predisposing factors
None.
Information factors; positive
-
•Healthcare professional
-
oInitiative GP/researcher/other
-
oAttention from GP/researcher/other
-
oKnowledge development GP/researcher/other
-
oTrust in guidance
-
oRelationship with GP
-
o
-
•Information factors
-
oHad understood it
-
oTaking the target population into account
-
o(Remembered) Having received it
-
o
Information factors; negative
-
•Healthcare professional
-
oNo treatment options
-
oPrivacy issues
-
o
-
•Obligation
-
oFeeling of obligation
-
oNo Feeling of obligation
-
o
-
•Information factors
-
oHad not understood it
-
oLanguage barrier
-
o(Health) Illiteracy
-
oNot (remembering) having received it
-
oDoubts about content aspects
-
oJudgment about materials
-
o
Awareness factors; positive
-
•
Importance prevention
-
•Health status
-
oObtain insight into risks
-
oObtain certainty about health
-
o(Being) Health(y)
-
oHealthy aging
-
oBelieves to be low-risk and wants to know risk
-
oBelieves to be high-risk and wants to know risk
-
oDecrease risks
-
oRisk perception with regard to family history
-
oRisk perception with regard to lifestyle
-
oNever too old
-
oPrevious experience with a health check
-
oNo previous experience with a health check
-
o
Awareness factors; negative
-
•Health status
-
oToo old
-
oAlready health complaints/already ill/receiving treatment
-
oNo health complaints
-
oConvinced of own health
-
o
-
•Social environment
-
oMore useful for others
-
o
Motivation factors; positive/rational attitude
-
•Positive
-
oNice
-
oGood
-
oUseful
-
oOkay
-
oSurprising
-
oInteresting
-
oHappy
-
oRelieved
-
oCan do no harm
-
oCurious
-
oSensible
-
oImportant
-
oNecessary
-
oSatisfied
-
oEnthusiastic
-
oGrateful
-
oPositive
-
o
-
•
Normal/neutral
-
•Health status
-
oNot afraid to have to adjust lifestyle habits
-
o
-
•Locus of control
-
oBelieves to control staying healthy
-
o
-
•Fear
-
oNo fear
-
oNo fear for the test result
-
o
Motivation factors; negative/emotional attitude
-
•Negative
-
oNot good
-
oNot important
-
oUnreliable
-
oNot interested
-
oDon't feel like it
-
oNot necessary
-
oStrange
-
oDoubt
-
oNegative
-
o
-
•Health status
-
oAfraid to have to adjust lifestyle habits
-
oWorries about health
-
oIgnoring/denial
-
o
-
•Healthcare professional
-
oGuinea pig
-
o
-
•Locus of control
-
oBelieves not to control staying healthy
-
oReligious beliefs
-
o
-
•Fear
-
oFear for the test result
-
oFear for the consequences of the test result
-
oFear for doctors/hospitals
-
oPanic/agitation
-
oFear
-
o
-
•
Own responsibility
Motivation factors; positive social influences
-
•Social environment
-
oAction linkage: help from others
-
oImportant for offspring
-
oOthers find it important
-
o
Motivation factors; negative social influences
-
•Social environment
-
oSocial pressure
-
oGossip
-
o
Intention state; precontemplation
-
•(Non-)Participation
-
oNot wanting to participate
-
oDoubts about participation
-
o
Intention state; contemplation
-
•(Non-)Participation
-
oWanting to participate
-
oNeed
-
o
Ability factors
-
•Time
-
oTakes little time
-
o
-
•
Not applicable/none
Barriers
-
•Time
-
oNo time
-
oOther priorities
-
oJob
-
oForgot it
-
oHolidays/in home country/sick
-
o
-
•
Money issues
Other
-
•Health status
-
oPregnant
-
o
-
•
Psychological problems
-
•
Other
References
- Amoroso C., Harris M.F., Ampt A. The 45 year old health check - feasibility and impact on practices and patient behaviour. AustFamPhysician. 2009;38(5):358–362. [PubMed] [Google Scholar]
- Assendelft WJ, Nielen MM, Hettinga DM, Meer van der, V, Vliet van, M, Drenthen, AJ, et al. Bridging the gap between public health and primary care in prevention of cardiometabolic diseases; background of and experiences with the Prevention Consultation in The Netherlands. Fam Pract [Internet]. 2012; 29:[i126-i31 pp.]. Available from: (http://www.ncbi.nlm.nih.gov/pubmed/22399541). [DOI] [PMC free article] [PubMed]
- Bos V., Kunst A.E., Keij-Deerenberg I.M., Garssen J., Mackenbach J.P. Ethnic inequalities in age- and cause-specific mortality in The Netherlands. Int. J. Epidemiol. 2004;33(5):1112–1119. doi: 10.1093/ije/dyh189. [DOI] [PubMed] [Google Scholar]
- Brunner-Ziegler S., Rieder A., Stein K.V., Koppensteiner R., Hoffmann K., Dorner T.E. Predictors of participation in preventive health examinations in Austria. BMC Public Health. 2013;13:1138. doi: 10.1186/1471-2458-13-1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgess C., Wright A.J., Forster A.S. Influences on individuals' decisions to take up the offer of a health check: a qualitative study. Health Expect. 2014 doi: 10.1111/hex.12212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalton A.R., Bottle A., Okoro C., Majeed A., Millett C. Uptake of the NHS Health Checks programme in a deprived, culturally diverse setting: cross-sectional study. J Public Health (Oxf) 2011;33(3):422–429. doi: 10.1093/pubmed/fdr034. [DOI] [PubMed] [Google Scholar]
- Dekker J.M., Alssema M., Janssen P.G.H. NHG-Standaard Het PreventieConsult module Cardiometabool [NHG Guideline Prevention consultation Cardiometabolic module] Huisarts Wet. 2011;54(3):138–155. [Google Scholar]
- Dijkshoorn H., Uitenbroek D.G., Middelkoop B.J. Prevalentie van diabetes mellitus en hart- en vaatziekten onder Turkse, Marokkaanse en autochtone Nederlanders [Prevalence of diabetes mellitus and cardiovascular disease among immigrants from Turkey and Morocco and the indigenous Dutch population] Ned. Tijdschr. Geneeskd. 2003;147(28):1362–1366. [PubMed] [Google Scholar]
- Dryden R., Williams B., McCowan C., Themessl-Huber M. What do we know about who does and does not attend general health check? Findings from a narrative scoping review. BMC Public Health [Internet] 2012;12 doi: 10.1186/1471-2458-12-723. http://www.biomedcentral.com/1471-2458/12/723 (Available from:) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edelman D., Christian A., Mosca L. Association of acculturation status with beliefs, barriers, and perceptions related to cardiovascular disease prevention among racial and ethnic minorities. J. Transcult. Nurs. 2009;20(3):278–285. doi: 10.1177/1043659609334852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis N., Gidlow C., Cowap L., Randall J., Iqbal Z., Kumar J. A qualitative investigation of non-response in NHS health checks. Archives of public health = Archives belges de sante publique. 2015;73(1):14. doi: 10.1186/s13690-015-0064-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrimond H., Saukko P.M., Qureshi N., Evans P.H. Making sense of being at 'high risk' of coronary heart disease within primary prevention. Psychol. Health. 2010;25(3):289–304. doi: 10.1080/08870440802499382. [DOI] [PubMed] [Google Scholar]
- Groenenberg I., Crone M.R., van Dijk S. Response and participation of underserved populations after a three-step invitation strategy for a cardiometabolic health check. BMC Public Health. 2015;15:854. doi: 10.1186/s12889-015-2139-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groenenberg I., Crone M.R., van Dijk S. ‘Check it out!’ Decision-making of vulnerable groups about participation in a two-stage cardiometabolic health check: a qualitative study. Patient Educ. Couns. 2015;98(2):234–244. doi: 10.1016/j.pec.2014.10.010. [DOI] [PubMed] [Google Scholar]
- Hennelly M.O., Sly J.R., Villagra C., Jandorf L. Narrative message targets within the decision-making process to undergo screening colonoscopy among Latinos: a qualitative study. J. Cancer Educ. 2014 doi: 10.1007/s13187-014-0765-0. [DOI] [PubMed] [Google Scholar]
- Kaltsa A., Holloway A., Cox K. Factors that influence mammography screening behaviour: a qualitative study of Greek women's experiences. Eur. J. Oncol. Nurs. 2013;17(3):292–301. doi: 10.1016/j.ejon.2012.08.001. [DOI] [PubMed] [Google Scholar]
- Khunti K., Gillies C.L., Taub N.A. A comparison of cost per case detected of screening strategies for Type 2 diabetes and impaired glucose regulation: modelling study. Diabetes Res. Clin. Pract. 2012;97(3):505–513. doi: 10.1016/j.diabres.2012.03.009. [DOI] [PubMed] [Google Scholar]
- Knops-Dullens T., Vries de N., Vries de H. Reasons for non-attendance in cervical cancer screening programmes: an application of the Integrated Model for Behavioural Change. Eur. J. Cancer Prev. 2007;16(5):436–445. doi: 10.1097/01.cej.0000236250.71113.7c. [DOI] [PubMed] [Google Scholar]
- Kunst A.E., Mackenbach J.P., Lamkaddem M., Rademakers J., Devillé W. 2008. Overzicht en evaluatie van resultaten van wetenschappelijk onderzoek naar etnische verschillen in gezondheid, gezondheidsrisico's en zorggebruik in Nederland [Overview and evaluation of results from scientific research on ethnic differences in health, health risks, and health care use in the Netherlands]. Utrecht, the Netherlands. [Google Scholar]
- Leest van L.A.T.M., Dis van S.J., Verschuren W.M.M. Report Number: 26185006. 2002. Hart- en vaatziekten bij allochtonen in Nederland, een cijfermatige verkenning naar leefstijl- en risicofactoren, ziekte en sterfte [Cardiovascular diseases in non-Western immigrants in the Netherlands. An exploratory study into lifestyle, risk factors, morbidity, and mortality]. Bilthoven, the Netherlands. [Google Scholar]
- Mackenbach J.P., Kunst A.E., Cavelaars A.E., Groenhof F., Geurts J.J. Socioeconomic inequalities in morbidity and mortality in western Europe. The EU Working Group on Socioeconomic Inequalities in Health. Lancet. 1997;349(9066):1655–1659. doi: 10.1016/s0140-6736(96)07226-1. [DOI] [PubMed] [Google Scholar]
- Mackenbach J.P., Stirbu I., Roskam A.J. Socioeconomic inequalities in health in 22 European countries. N. Engl. J. Med. 2008;358(23):2468–2481. doi: 10.1056/NEJMsa0707519. [DOI] [PubMed] [Google Scholar]
- McAndrew L.M., Musumeci-Szabo T.J., Mora P.A. Using the common sense model to design interventions for the prevention and management of chronic illness threats: from description to process. Br. J. Health Psychol. 2008;13(Pt 2):195–204. doi: 10.1348/135910708X295604. [DOI] [PubMed] [Google Scholar]
- Nap A., van Loon A., Peen J., van schaik D.J., Beekman A.T., Dekker J.J. The influence of acculturation on mental health and specialized mental healthcare for non-western migrants. The International Journal of Social Psychiatry. 2014 doi: 10.1177/0020764014561307. [DOI] [PubMed] [Google Scholar]
- Nierkens V., Stronks K., Oel van C.J., Vries de H. Beliefs of Turkish and Moroccan immigrants in The Netherlands about smoking cessation: implications for prevention. Health Educ. Res. 2005;20(6):622–634. doi: 10.1093/her/cyh026. [DOI] [PubMed] [Google Scholar]
- Nierkens V., Stronks K., Vries de H. Attitudes, social influences and self-efficacy expectations across different motivational stages among immigrant smokers: replication of the O pattern. Prev. Med. 2006;43(4):306–311. doi: 10.1016/j.ypmed.2006.05.005. [DOI] [PubMed] [Google Scholar]
- Pandya A., Weinstein M.C., Salomon J.A., Cutler D., Gaziano T.A. Who needs laboratories and who needs statins?: comparative and cost-effectiveness analyses of non-laboratory-based, laboratory-based, and staged primary cardiovascular disease screening guidelines. Circ Cardiovasc Qual Outcomes. 2014;7(1):25–32. doi: 10.1161/CIRCOUTCOMES.113.000397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reijneveld S.A. The impact of individual and area characteristics on urban socioeconomic differences in health and smoking. Int. J. Epidemiol. 1998;27(1):33–40. doi: 10.1093/ije/27.1.33. [DOI] [PubMed] [Google Scholar]
- Smith S.K., Simpson J.M., Trevena L.J., McCaffery K.J. Factors associated with informed decisions and participation in bowel cancer screening among adults with lower education and literacy. Med. Decis. Mak. 2014;34(6):756–772. doi: 10.1177/0272989X13518976. [DOI] [PubMed] [Google Scholar]
- Status scores. Sociaal en Cultureel Planbureau [Social and Cultural Planning Office] 2014.
- Sogaard R., Lindholt J., Gyrd-Hansen D. Individual decision making in relation to participation in cardiovascular screening: a study of revealed and stated preferences. Scand J Public Health. 2013;41(1):43–50. doi: 10.1177/1403494812468519. [DOI] [PubMed] [Google Scholar]
- Vries de H., Mesters I., Steeg van de H., Honing C. The general public's information needs and perceptions regarding hereditary cancer: an application of the Integrated Change Model. Patient Educ. Couns. 2005;56(2):154–165. doi: 10.1016/j.pec.2004.01.002. [DOI] [PubMed] [Google Scholar]
- WHO. Fact Sheet Number 310: The Top Ten Causes of Death 2008 [updated 2008]. (Available from:) http://www.who.int/mediacentre/factsheets/fs310_2008.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transparency document