Abstract
Anxiety and obsessive compulsive disorders are among the earliest occurring psychopathology and may derive from atypical maturation of neural networks for error processing. Psychological models have alternately suggested that overdetection of errors, excessive caring about errors or failure of errors to elicit regulatory control could associate with the expression of anxiety. In this review article, the potential relevance of error processing for anxiety and obsessive compulsive disorders is described in the context of neurophysiological and functional magnetic resonance imaging (fMRI) research demonstrating altered brain response to errors in pediatric and adult patients. Finally, hypotheses about developmentally sensitive mechanisms of anxiety and obsessive compulsive disorders are drawn from the extant literature, and avenues for clinical translation are discussed.
Keywords: Anterior cingulate, anxiety, development, dorsolateral prefrontal cortex, error-processing, error-related negativity, obsessive-compulsive, pediatric, ventromedial prefrontal cortex
Introduction
Anxiety and obsessive-compulsive disorders are among the earliest occurring psychopathology, with onset during childhood or adolescence in half of all patients.1 High rates of comorbidity, overlapping phenomenology, and developmental fluidity between these disorders suggest common underlying mechanisms.2 The early emergence of symptoms may derive from atypical maturation of mechanisms underlying self regulation,3 including neural substrates for error processing. In adolescent and adult patients, increased midline prefrontal, electrophysiological response to errors has been consistently documented,4,5 and, recent work in children implicates abnormal neural mechanisms for error-processing from the earliest stages of illness. However, the functional significance of these electrophysiological signals remains unclear. In this review, we will consider several possibilities, integrating findings across electrophysiological and functional magnetic resonance imaging (MRI)-based studies in pediatric and adult patients. We will describe neural networks associated with error-processing, including substrate for affective valuation (how important an error is) and cognitive control (the ability to adjust behavior in response to errors or situations in which errors are likely). We conclude by hypothesizing that imbalances in these aspects of error processing may underlie obsessive compulsive and anxiety disorders, and may vary with age to represent developmentally sensitive targets for intervention.
The Relevance of Error Processing for Anxiety and Obsessive Compulsive Disorders: Theory and Electrophysiological Support
In 1987, Pitman6 suggested that the symptoms of OCD might originate with dysfunction in a comparator system that compares an internal goal with a perceived outcome, generating a mismatch, or error signal, when the perceived outcome does not match with intention, leading to performance adjustments. According to this “cybernetic theory,” in OCD, larger error signals (mismatches) are generated, leading to compulsive rituals to correct the mismatch, eg, repeated checking to ensure safety.6 The discovery of the error-related negativity (ERN), a negative amplitude, event-related potential (ERP) that occurs 50–100 msec after an erroneous response, permitted a test of this hypothesis. Indeed, in 2000, Gehring et al7 reported elevated ERN in patients with OCD in response to errors on a simple cognitive task that does not elicit OCD symptoms. The finding has since been replicated in multiple samples of adult8 and pediatric patients9–11 (see Table 1). Although the details of what causes the increased error signal were not specified (deficient comparator, overly low threshold for mismatch detection, unobtainable internal goals), the cognitive neuroscience approach of performance monitoring-detecting errors and adjusting behavior-held out the promise of a mechanistic understanding of OCD.
TABLE 1.
Error-related negativity (ERN) and pediatric obsessive compulsive and anxiety disorders: a summary of the published literature
| Study | Age (yrs) | Patient type | Design | Paradigm | Main results |
|---|---|---|---|---|---|
| Anxiety Disorders | |||||
| Ladouceur et al., 200619 | 8–14 | AD | Group comparison: AD (n = 12) v HC (n = 13) |
Flanker (arrow) | Increased ERN in AD compared to HC. |
| Carrasco et al., 201311,a | 8–16 | AD, OCD | Group comparison: AD (n = 13) v OCD (n = 26) v HC (n = 27) |
Flanker (arrow) | Increased ERN in both AD and OCD groups compared to HC. |
| Meyer et al., 201320,b | 5–7 | AD | Group comparison: AD (n = 48) v HC (n = 48) |
Go/NoGo | Increased ERN in AD compared to HC at young age (~6 years) |
| Santesso et al., 200670 | 10 +/− .25 | OCS, AS* | Correlational: ERN α OCS, AS |
Flanker (letter) | Greater ERN correlates with higher OCS. No significant relationship of ERN with AS. |
| OCD | |||||
| Hajcak et al., 20089 | 8–17 | OCD | Before CBT/After CBT: OCD (n = 18/10) v HC (n = 18/13) |
Simon | Increased ERN in OCD compared to HC before and after CBT, despite symptom reduction, suggests increased ERN is trait (not state) marker of OCD |
| Hanna et al., 201210,a | 10–19 | OCD +/− tics | Group comparison: OCD (n = 44) v OCD + tic (n = 9) v HC (n = 44) |
Increased ERN in non-tic related OCD compared to both tic-related OCD and HC, suggests OCD with and without tics are neurobiologically different subtypes. | |
| Carrasco et al., 201311,a | 10–17 | OCD, unaffected sibs | Group comparison: OCD (n = 40) v US (n = 19) v HC (n = 40) |
Increased ERN in both OCD and US groups compared to HC, suggesting ERN as biomarker for genetic risk of OCD. | |
| Community Samples | |||||
| Torpey et al., 201371,b | 5–7 | n/a | Correlational: ERN α behavioral fear at 3 yrs (n = 328) |
Go/NoGo | Greater ERN at ~6 years correlates with lower behavioral fear at ~3 years. |
| Meyer et al., 201218,c | 8–13 | n/a | Correlational: ERN α SCARED (n = 55) |
Flanker (arrow) | Greater ERN correlates with lower anxiety at 8–10 years, but higher anxiety at 11–13 years. |
| Bress et al., 201572,c | 11–13 | n/a | Correlational: ERN α SCARED & CDI (n = 25) |
Flanker (arrow) | Greater ERN correlates with higher anxiety; contrasted with inverse relationship of depressive symptoms with feedback related negativity, a neurophysiological marker of reward |
| McDermott et al., 200913 | 14–16 | n/a | Longitudinal: BI, ERN as predictors later anxiety (n = 82) |
Flanker (letter) | Greater ERN in at adolescence (14–16 yrs) moderates relationship of early inhibited temperament (2–3 yrs) with anxiety disorder in adolescence (14–16 yrs) |
| Lahat et al., 201412 | 7.7 +/− .25 | n/a | Longitudinal: BI, ERN as predictors later anxiety (n = 113) |
Flanker (fish) | Greater ERN at ~7 years moderates relationship of early inhibited temperament (2–3 yrs) with social phobia symptoms at 9 years. |
Anxiety disorder (AD) samples included generalized anxiety disorder, separation anxiety disorder, social phobia, and specific phobia. There were no obsessive-compulsive disorder (OCD) diagnoses in any AD sample, except for the study by Meyer et al,20 in which 2 of 48 AD patients had comorbid OCD (with other ADs). HC = healthy control; ERN = error-related negativity; CBT = cognitive behavior therapy; US = unaffected siblings; SCARED = Screen for Child Anxiety Related Disorders; CDI = Child Depression Inventory; BI = behavioral inhibition.
OCS = obsessive compulsive symptoms in a community (ie, nonclinical) ranged from none to subclinical based on parent report on the obsessive-compulsive subscale of the Child Behavior Checklist (CBCL) (Achenbach, 1991). Non-OCD anxiety symptoms (AS) were also examined in the same sample using the CBCL.
Partial subject overlap across studies.
However, it soon became apparent that hyperactive ERN is not specific to OCD. ERN hyperactivity also occurs in non-OCD anxiety and in relationship to anxious temperament in nonclinical populations, including in pediatric samples.4,5,8,12,13. Interestingly, ERN magnitudes are reduced in persons with psychotic disorders14 and attention deficit hyperactivity disorder,15 leading some investigators to hypothesize that a hyperactive response to errors is a sign of internalizing disorders.4
What, then, is the function of hyperactive error responses in obsessive compulsive and anxiety disorders, in general, and in pediatric patients in particular? Several possible theories relating increased ERN to anxiety have been suggested. Anxiety involves the anticipation of future threat or the worry of an imminent bad outcome. Clinically, it manifests across a spectrum of disorders in children, eg, excessive fear of bad consequences due to temporary separation from parents (separation anxiety), being observed by peers (social anxiety), minor mistakes carrying out “every day” concerns (generalized anxiety), or accidental harm to self or loved ones (OCD). Thus, increased ERN may reflect a source of worry, indexing increased affective valuation of errors4,16 and driving obsessions or worries about errors leading to bad outcomes. Alternatively, it is possible that an increased ERN reflects a compensatory response for deficiencies in control systems, and that these deficits give rise to anxiety,17 as detailed in the next section. Another recent theory posits that increased ERN may reflect a secondary effect of anxiety on the brain, rather than a source of anxiety itself; specifically, Moser et al5 suggested that increased ERN may signify a mechanism by which anxious individuals re-activate task goals, in the face of distracting levels of anxiety, to maintain normal performance. In this scenario, an increased ERN occurs to prevent decrements in performance due to anxiety, but the ERN does not directly contribute to anxiety expression.
These theoretical explanations are important steps in understanding the mechanistic significance of increased ERN in OCD and anxiety disorders, but a definitive explanation has yet to emerge. However, in combination with neuroimaging studies, the performance monitoring approach has begun to shed light on neurocircuits that may underlie anxiety. As we will postulate below, imbalanced engagement of brain circuits involved in affective valuation of performance and those engaged in control of performance may combine to drive symptom expression.
Neurodevelopment of ERN in Anxious Youth
Emerging research shows interactions between developmental stage and the relationship of ERN to anxiety in children that, hypothetically, could derive from differential development of affective valuation relative to cognitive control during error-processing. For instance, greater ERN amplitude has been associated with higher levels of subclinical anxiety in early adolescence (11–13 years),18 which is consistent with findings in older youth,10,11,19 whereas the opposite pattern was observed in younger children (greater ERN with lower levels of subclinical anxiety at 8–10 years).18 Even further complexity is suggested by the finding that young children with clinically significant anxiety exhibit increased ERN relative to age-matched healthy controls.20
At this stage, these findings are not completely reconciled, but suggest complex interactions between error processing, developmental stage, and severity of anxiety. In prepubertal children with low subclinical anxiety,18 greater ERN amplitude may reflect effective signaling for higher level cognitive control, which, in turn, could mitigate subclinical anxiety symptoms by enabling behavioral adjustment (e.g., switching from repetitive worries or compulsions to more appropriate, less anxious behaviors).21 In contrast, in prepubertal children with clinically significant anxiety20 and in postpubertal individuals with subclinical to clinical levels of severity,4,5,8,18 increased ERN could reflect increased affective valuation of errors, unresponsive control system driving error signal up, and/or an imbalance between these processes. Emerging research supports the contribution of both affective and cognitive subcomponents of error-processing to the ERN22—sub-components that may mature at different time points and may differentially contribute to ERN–anxiety associations during specific periods of development.
A Neural Network for Affective Valuation and Cognitive Control in Response to Errors: Evidence from fMRI
Functional neuroimaging research has provided important data about possible neural substrates of the ERN in particular, and error processing in general, that can inform theory linking this psychological function to anxiety and OCD. For instance, functional MRI (fMRI) has been combined with electrophysiological methods in healthy individuals to localize the ERN to dorsal anterior cingulate cortex (dACC),23,24 as well as rostral ACC,22,23,25 mid-cingulate,25 lateral prefrontal cortex,22,26 and inferior parietal cortex.26 Historically, most of the fMRI research on error processing has focused on the posterior medial frontal cortex (pMFC), encompassing dACC and pre-SMA,27 which operates as part of a system of dissociable neural networks that regulate cognitive and affective response to errors28 (Figure 1). In healthy individuals, the pMFC co-activates with anterior insula across a wide variety of tasks,28 comprising a network that is centrally involved in performance monitoring to integrate external task demands with internal motivational state.29–32 During performance monitoring, the pMFC also co-activates with other regions, such as dorsolateral prefrontal cortex (dlPFC), to mediate adjustments in behavioral response to external task demands.33 While the pMFC is anatomically linked to motor and pre-motor areas that carry out response selection, the anterior insula plays a more prominent role in detecting salience (both externally and internally cued) through bidirectional projections to pMFC and emotion processing regions, such as the ventro-medial prefrontal cortex (vmPFC).34 The vmPFC, a brain region that evaluates the significance of stimuli and events,35–37 normally deactivates with errors and exhibits a reciprocal, anti-correlated relationship with the pMFC and anterior insula.
FIGURE 1.
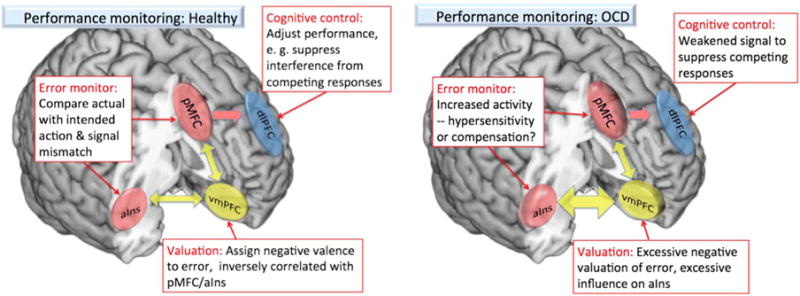
Schematic illustration of performance monitoring and proposed disruptions in OCD. (A) In healthy subjects, components of the performance monitoring network include the pMFC working in concert with the anterior insula (aIns) to monitor behavior and detect mismatches (errors), and then send a signal to the dlPFC, which increases control to suppress unwanted interference and improve performance. The vmPFC, which typically deactivates during tasks that require an external focus of attention, also modulates activity in the pMFC and aIns, possibly to provide a signal that determines the value of a task and a subsequent error. (B) In OCD, evidence suggests that several of these components are disrupted (although results in children and adults differ slightly). Activity is increased in the monitoring nodes (pMFC and anterior insula, aIns), and the connection between the vmPFC and aIns is increased, which may signal the greater negative valuation that OCD patients place on errors. Other disrupted nodes may include the pMFC-dlPFC connection, and a weakened ability to overcome interfering activity from valuation centers that drive compulsive behaviors.
The networks that support performance monitoring functions mature dramatically in adolescents,38–41 which provides a context for considering how pathological development of these networks could contribute to pediatric anxiety disorders. Closely related to performance monitoring are executive functions that resolve conflict between competing response options, thus adjusting performance to overcome interference. According to conflict theory, errors are merely a manifestation of unsuccessfully processing response options that interfere with one another.42,43 In typically developing youth, age-related changes in the location of midline prefrontal activation, from more rostral (vmPFC) to more dorsal areas (pMFC), have been observed for conflict-processing,44 as well as emotion regulation.45 These findings suggest that mobilization of networks involved in task control (eg, pMFC), over those involved in affective valuation (eg, vmPFC), could contribute to the maturation of capacity for performance monitoring. Studies of connectivity between network nodes for task control (pMFC, dlPFC, anterior insula) and affective valuation (vmPFC), at rest and during task, support this notion. With age, resting state connectivity between pMFC and anterior insula increases, while connectivity with vmPFC decreases.46 Age-related increases in functional coupling between vmPFC and dlPFC support improved performance in children during tasks that require cognitive control over affective valuation,47 implicating interactions between nodes for cognitive and affective aspects of performance monitoring in its maturation.
Increased pMFC-Based Error-Signaling in OCD and Anxiety Disorders: An Adaptive Response for the Recruitment of Cognitive Control?
In adult OCD, imaging studies of error-processing have shown increased pMFC activation,48 as well as greater activation of more rostral aspects of the ACC.49,50 Hyperactivation of the pMFC to cognitive conflict has also been reported by some,48,50,51 but not all studies of adult OCD.49,52 In patients with pediatric OCD (8–19 years), increased pMFC activation occurs during high-conflict trials (collapsed across correct and incorrect)53 and when errors are examined in separation.54
The role of pMFC hyperactivation in OCD during performance monitoring remains unclear, but recent clinical translation work provides some clues. In an fMRI study of patients with pediatric OCD before and after cognitive behavioral therapy (CBT), Huyser et al54 found that conflict-related pMFC and dlPFC activity increases associated with symptom improvement. The relationship of increasing pMFC and dlPFC activity with decreasing OCD severity suggests that greater activation of these regions may reflect a compensatory mechanism, enhanced by CBT, to enable young patients to control symptoms. That is, patients typically endorse insight that their anxiety-provoking obsessions are excessive, raising the possibility that feared outcomes are appropriately detected as “thinking errors,” but cognitive control is insufficiently engaged, allowing symptoms to persist. In other words, greater pMFC activity may reflect conflict between intentions and affect-the normal “security concerns” that become exaggerated in OCD57-and not errors, per se, but situations where errors are perceived as possible. Signaling by pMFC may enable engagement of dlPFC to implement cognitive control32,33 over inappropriate intrusion of affect during task execution in OCD. In theory, this mechanism would support response to CBT, which teaches patients to ignore anxiety induced by obsessions as a “false alarm” and resist compulsive urges until the anxiety fades away.58
Functional neuroimaging research in patients with non-OCD anxiety disorders has traditionally employed emotion-inducing, rather than error-eliciting, cognitive conflict tasks, but recent work supports the possibility that anxiety could manifest as the result of impoverished recruitment of prefrontal cortical control. Some studies of non-OCD anxiety have examined cognitive control over emotion, and these studies show excessive pMFC activation to emotional conflict,59 but reduced dlPFC recruitment during tasks requiring the regulation of emotional response.60 During non-emotional cognitive conflict, higher levels of trait anxiety in healthy adults associate with exaggerated electrophysiological response in an area of midline prefrontal cortex that may localize to pMFC,61,62 but reduced dlPFC recruitment.17 In our own work, we have found reduced dlPFC activation to errors in pediatric OCD and non-OCD anxiety,63 consistent with earlier work in pediatric OCD patients.64 Failure to appropriately recruit dlPFC during performance monitoring may reflect insufficient capacity to engage cognitive control, contributing to deficient capacity for adjusting repetitive anxious thoughts and behavior. Taken together, these findings raise the possibility that increased pMFC and reduced dlPFC recruitment by conflict and errors may generalize across OCD and non-OCD anxiety disorders. Since greater pMFC signaling in response to error- and conflict-detection recruits more dlPFC-based cognitive control,33 increased activation in both regions may support increased regulatory control over anxiety.
Excessive Affective Response and Insufficient Cognitive Control During Performance Monitoring in OCD and the Anxiety Disorders: An Integrated Model
At this stage of research, many questions remain about the cause of ERN hyperactivity in OCD and anxiety disorders, particularly in pediatric patients. The developmental trajectory of neurocircuits complicates the picture for performance monitoring. Given these considerations, we suggest it may be useful to consider that an imbalance between neural networks for affective evaluation and task execution occurs during error-processing in patients.
Given emerging evidence that a widely distributed network contributes to the ERN,22,26,65 multiple sub-component processes mediated by distinct network nodes may contribute to the ERN. Indeed, Edwards et al22 recently used joint independent component analysis of simultaneously collected ERN and fMRI to reveal two temporo-spatially distinct components contribute to the ERN: (1) an earlier component (48 msec) associated with fMRI activity in caudal ACC and lateral prefrontal cortex (lPFC) and (2) a later component (86 msec) associated with activity in the rostral ACC. The authors interpreted their results as evidence that the ERN reflects early engagement of cognitive processes in caudal ACC and lPFC (eg, mismatch detection, signaling for adaptive control) and later engagement of affective processes in rostral ACC (eg, affective valuation of error significance).
These separable substrates for cognitive and affective response to errors may show differential rates of development, such that links between neurocircuits for performance monitoring and anxiety could differ at different stages of development. Specifically, deficits of neural substrate for adaptive control (e.g., caudal ACC, lPFC) may couple with excessive reactivity in substrate for affective response (e.g., rostal ACC, vmPFC) to drive anxiety across development, while the specific nature of these abnormalities (too little adaptive control, too much affective response, or the combination) may vary with patient age.
Accordingly, several imaging studies of error processing in OCD show increased activity not in the dorsal or caudal ACC, but in the rostral-ventral extent of the medial prefrontal cortex, including the vmPFC49,50,52 (however, see Ursu et al48 and Woolley et al64). In resting state studies, patients with OCD have shown hyperactivity66 and aberrant connectivity of the orbitofrontal region, including vmPFC.67 In adult patients, we have found excessive activity in the anterior insula related to the negative valuation of an error, and this activity was associated with increased connectivity between the vmPFC and anterior insula.52 More ventral midline response to errors in the perigenual ACC and vmPFC could be a source of inappropriate intrusion of negative affect (ie, hypersensitive emotional response to errors) that requires enhancing cognitive control mechanisms (increasing pMFC, dlPFC) or restoring separation between circuits for affect and cognition during error processing (eg, reciprocal anterior insula-vmPFC interactions) to improve OCD. Interestingly, in pediatric OCD, error-related activation in the rostral ACC increases from childhood through adolescence,54 suggesting that atypical engagement of this vmPFC sub-region may represent a developmentally sensitive mechanism of illness that emerges with age. Atypical interactions between anterior insula and vmPFC have not been demonstrated in pediatric patients, and additional research will be needed to determine whether failure to develop reciprocal interactions between these regions uniquely characterizes OCD in adults.
A consideration of a cognitive-affective imbalance in OCD and anxiety disorders has several implications for future research. For example, it is not clear if the negative affect associated with an error represents a more general signature of anxiety, or more specific affects, such as worry, apprehension,5 or frustration.68 Additional research is needed to determine whether vmPFC hyperactivity may be the source of a pathological negative appraisal of error commission in OCD and non-OCD anxiety disorders. In addition, developmental neuroimaging work is needed to determine whether there are sensitive periods for performance monitoring abnormalities during which certain interventions are most likely to be successful.3 For instance, in healthy youth, pMFC-based networks for performance monitoring continue to develop through adolescence and into young adulthood,46,69 suggesting plasticity that may make performance enhancing strategies (eg, cognitive control training) particularly beneficial for adolescent patients. By contrast, in anxiety, atypical vmPFC-insula interactions during performance monitoring may emerge later in development, necessitating other strategies to reduce anxiety in older patients.
Conclusion
ERN and fMRI research consistently demonstrate hyper-activation to errors in midline prefrontal cortex in pediatric and adult patients with OCD and non-OCD anxiety disorders. These abnormalities have been variably localized, and we have suggested that more posterior activations may reflect a compensatory process by which increased signaling for cognitive control can reduce anxiety, while more ventral activations may represent the source of a pathological negative appraisal of error commission, triggering anxiety symptoms. We have also considered the maturation of neural substrate for cognitive control and affective/evaluative aspects of error-processing, suggesting that specific abnormalities of these functions may vary with illness severity and stage of development. For instance, impoverished recruitment of prefrontal control may set the stage for the emergence of anxiety, and may need to be specifically targeted in young patients to reduce symptoms. By contrast, adult patients may have missed the developmental window in which mechanisms for cognitive control are most amenable to modulation. Instead, in older patients, enhancing reciprocal connections between pMFC- and dlPFC-based networks for control and vmPFC-based affective valuation may need to be a focus of treatment. It is also important to understand whether or not the signals from ERP and fMRI studies represent compensations for or causes of anxiety, in order to design cognitive training or neuromodulatory therapies that would seek to increase (in the case of compensatory activity) or decrease (for targets causing anxiety) signaling. In conclusion, error-processing networks present potential targets for novel treatments, such as cognitive training or transcranial magnetic stimulation, to reduce and even prevent illness. However, developmentally sensitive alterations of error processing will need to be considered, since these networks may need to be targeted differently at different stages of development.
TABLE 2.
fMRI studies of error-processing in pediatric obsessive compulsive and anxiety disorders: a summary of the published literature
| Study | Age (yrs) | Patient type | Design | Paradigm | Main results |
|---|---|---|---|---|---|
| Wooley et al., 200864 | 12–16 (boys only) | OCD | Group comparison: OCD (n = 10) v HC (n = 9) |
Stop Task | Decreased activation in mesial frontal gyrus, reaching laterally into left dorsolateral prefrontal cortex and ventrally into anterior cingulate gyrus in OCD compared to HC for Stop Failure minus Go trials. |
| Fitzgerald et al., 201040 | 8–19 | OCD | Group comparison: OCD (n = 15) v HC (n = 12) |
MSIT | Increased activation in ventral medial prefrontal cortex in OCD compared to HC for error minus correct trials (across incongruent and congruent trials). |
| Huyser et al., 201154 | 8–19 | OCD | Before/after CBT: OCD (n = 25/24) v HC (n = 25/22) |
Flanker (arrow) | Increased activation in anterior cingulate cortex and right insula at older ages in OCD compared to HC before and after treatment for error minus correct trials (across incongruent and congruent trials). |
| Fitzgerald et al., 201363 | 8–19 | AD, OCD | Group comparison: OCD (n = 17), AD (n = 13) v HC (n = 20) |
MSIT | Decreased left dorsolateral prefrontal cortex in AD and OCD compared to HC for error minus correct trials (incongruent trials only). |
OCD = obsessive-compulsive disorder; AD = anxiety disorders including generalized anxiety disorder, separation anxiety disorder, social phobia and specific phobia; CBT = cognitive behavioral therapy; HC = healthy controls; MSIT = Multisource Interference Task.
Footnotes
Disclosures
Kate Fitzgerald has the following disclosures: NIMH, independent investigator, research support. Stephan Taylor has the following disclosures: St. Jude Medical, independent investigator, research support; Neuronetics, independent investigator, research support; NIMH, independent investigator, research support.
References
- 1.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, Ormel J, Petukhova M, et al. Development of lifetime comorbidity in the World Health Organization world mental health surveys. Arch Gen Psychiatry. 2011;68(1):90–100. doi: 10.1001/archgenpsychiatry.2010.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Casey BJ, Pattwell SS, Glatt CE, Lee FS. Treating the developing brain: implications from human imaging and mouse genetics. Annu Rev Med. 2013;64:427–439. doi: 10.1146/annurev-med-052611-130408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Olvet DM, Hajcak G. The error-related negativity (ERN) and psychopathology: toward an endophenotype. Clin Psychol Rev. 2008;28(8):1343–1354. doi: 10.1016/j.cpr.2008.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moser JS, Moran TP, Schroder HS, Donnellan MB, Yeung N. On the relationship between anxiety and error monitoring: a meta-analysis and conceptual framework. Front Hum Neurosci. 2013;7:466. doi: 10.3389/fnhum.2013.00466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pitman RK. A cybernetic model of obsessive-compulsive psychopathology. Compr Psychiatry. 1987;28(4):334–343. doi: 10.1016/0010-440x(87)90070-8. [DOI] [PubMed] [Google Scholar]
- 7.Gehring WJ, Himle J, Nisenson LG. Action-monitoring dysfunction in obsessive-compulsive disorder. Psychol Sci. 2000;11(1):1–6. doi: 10.1111/1467-9280.00206. [DOI] [PubMed] [Google Scholar]
- 8.Endrass T, Ullsperger M. Specificity of performance monitoring changes in obsessive-compulsive disorder. Neurosci Biobehav Rev. 2014;46(Pt 1):124–138. doi: 10.1016/j.neubiorev.2014.03.024. [DOI] [PubMed] [Google Scholar]
- 9.Hajcak G, Franklin ME, Foa EB, Simons RF. Increased error-related brain activity in pediatric obsessive-compulsive disorder before and after treatment. Am J Psychiatry. 2008;165(1):116–123. doi: 10.1176/appi.ajp.2007.07010143. [DOI] [PubMed] [Google Scholar]
- 10.Hanna GL, Carrasco M, Harbin SM, et al. Error-related negativity and tic history in pediatric obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry. 2012;51(9):902–910. doi: 10.1016/j.jaac.2012.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carrasco M, Hong C, Nienhuis JK, et al. Increased error-related brain activity in youth with obsessive-compulsive disorder and other anxiety disorders. Neurosci Lett. 2013;541:214–218. doi: 10.1016/j.neulet.2013.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lahat A, Lamm C, Chronis-Tuscano A, Pine DS, Henderson HA, Fox NA. Early behavioral inhibition and increased error monitoring predict later social phobia symptoms in childhood. J Am Acad Child Adolesc Psychiatry. 2014;53(4):447–455. doi: 10.1016/j.jaac.2013.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McDermott JM, Perez-Edgar K, Henderson HA, Chronis-Tuscano A, Pine DS, Fox NA. A history of childhood behavioral inhibition and enhanced response monitoring in adolescence are linked to clinical anxiety. Biol Psychiatry. 2009;65(5):445–448. doi: 10.1016/j.biopsych.2008.10.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Foti D, Kotov R, Bromet E, Hajcak G. Beyond the broken error-related negativity: functional and diagnostic correlates of error processing in psychosis. Biol Psychiatry. 2012;71(10):864–872. doi: 10.1016/j.biopsych.2012.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Geburek AJ, Rist F, Gediga G, Stroux D, Pedersen A. Electrophysiological indices of error monitoring in juvenile and adult attention deficit hyperactivity disorder (ADHD)–a meta-analytic appraisal. Int J Psychophysiol. 2013;87(3):349–362. doi: 10.1016/j.ijpsycho.2012.08.006. [DOI] [PubMed] [Google Scholar]
- 16.Proudfit GH, Inzlicht M, Mennin DS. Anxiety and error monitoring: the importance of motivation and emotion. Front Hum Neurosci. 2013;7:636. doi: 10.3389/fnhum.2013.00636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bishop SJ. Neurocognitive mechanisms of anxiety: an integrative account. Trends Cogn Sci. 2007;11(7):307–316. doi: 10.1016/j.tics.2007.05.008. [DOI] [PubMed] [Google Scholar]
- 18.Meyer A, Weinberg A, Klein DN, Hajcak G. The development of the error-related negativity (ERN) and its relationship with anxiety: evidence from 8 to 13 year-olds. Dev Cogn Neurosci. 2012;2(1):152–161. doi: 10.1016/j.dcn.2011.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ladouceur CD, Dahl RE, Birmaher B, Axelson DA, Ryan ND. Increased error-related negativity (ERN) in childhood anxiety disorders: ERP and source localization. J Child Psychol Psychiatry. 2006;47(10):1073–1082. doi: 10.1111/j.1469-7610.2006.01654.x. [DOI] [PubMed] [Google Scholar]
- 20.Meyer A, Hajcak G, Torpey DC, et al. Increased error-related brain activity in six-year-old children with clinical anxiety. J Abnorm Child Psychol. 2013;41(8):1257–1266. doi: 10.1007/s10802-013-9762-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Muris P, van der Pennen E, Sigmond R, Mayer B. Symptoms of anxiety, depression, and aggression in non-clinical children: relationships with self-report and performance-based measures of attention and effortful control. Child Psychiatry Hum Dev. 2008;39(4):455–467. doi: 10.1007/s10578-008-0101-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Edwards BG, Calhoun VD, Kiehl KA. Joint ICA of ERP and fMRI during error-monitoring. Neuroimage. 2012;59(2):1896–1903. doi: 10.1016/j.neuroimage.2011.08.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mathalon DH, Whitfield SL, Ford JM. Anatomy of an error: ERP and fMRI. Biol Psychology. 2003;64(1):119–141. doi: 10.1016/s0301-0511(03)00105-4. [DOI] [PubMed] [Google Scholar]
- 24.Debener S, Ullsperger M, Siegel M, Fiehler K, von Cramon DY, Engel AK. Trial-by-trial coupling of concurrent electroencephalogram and functional magnetic resonance imaging identifies the dynamics of performance monitoring. J Neurosci. 2005;25(50):11730–11737. doi: 10.1523/JNEUROSCI.3286-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Agam Y, Hämäläinen MS, Lee AK, et al. Multimodal neuroimaging dissociates hemodynamic and electrophysiological correlates of error processing. Proc Natl Acad Sci U S A. 2011;108(42):17556–17561. doi: 10.1073/pnas.1103475108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Doñamayor N, Heilbronner U, Münte TF. Coupling electrophysiological and hemodynamic responses to errors. Hum Brain Mapp. 2012;33(7):1621–1633. doi: 10.1002/hbm.21305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ridderinkhof KR, Ullsperger M, Crone EA, Nieuwenhuis S. The role of the medial frontal cortex in cognitive control. Science. 2004;306(5695):443–447. doi: 10.1126/science.1100301. [DOI] [PubMed] [Google Scholar]
- 28.Sridharan D, Levitin DJ, Menon V. A critical role for the right fronto-insular cortex in switching between central-executive and default-mode networks. Proc Natl Acad Sci U S A. 2008;105(34):12569–12574. doi: 10.1073/pnas.0800005105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Allman JM, Hakeem A, Erwin JM, Nimchinsky E, Hof P. The anterior cingulate cortex: the evolution of an interface between emotion and cognition. Ann N Y Acad Sci. 2001;935:107–117. [PubMed] [Google Scholar]
- 30.Critchley HD. Neural mechanisms of autonomic, affective, and cognitive integration. J Comp Neurol. 2005;493(1):154–166. doi: 10.1002/cne.20749. [DOI] [PubMed] [Google Scholar]
- 31.Dolan RJ. Emotion, cognition, and behavior. Science. 2002;298(5596):1191–1194. doi: 10.1126/science.1076358. [DOI] [PubMed] [Google Scholar]
- 32.Cavanaugh JF, Shackman AJ. Frontal midline theta reflects anxiety and cognitive control: meta-analytic evidence. J Physiol Paris. doi: 10.1016/j.jphysparis.2014.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kerns JG, Cohen JD, MacDonald AW, 3rd, Cho RY, Stenger VA, Carter CS. Anterior cingulate conflict monitoring and adjustments in control. Science. 2004;303(5660):1023–1026. doi: 10.1126/science.1089910. [DOI] [PubMed] [Google Scholar]
- 34.Barbas H. Connections underlying the synthesis of cognition, memory, and emotion in primate prefrontal cortices. Brain Res Bull. 2000;52(5):319–330. doi: 10.1016/s0361-9230(99)00245-2. [DOI] [PubMed] [Google Scholar]
- 35.Roy M, Shohamy D, Wager TD. Ventromedial prefrontal-subcortical systems and the generation of affective meaning. Trends Cogn Sci. 2012;16(3):147–156. doi: 10.1016/j.tics.2012.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Myers-Schulz B, Koenigs M. Functional anatomy of ventromedial prefrontal cortex: implications for mood and anxiety disorders. Mol Psychiatry. 2012;17(2):132–141. doi: 10.1038/mp.2011.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Taylor SF, Martis B, Fitzgerald KD, et al. Medial frontal cortex activity and loss-related responses to errors. J Neurosci. 2006;26(15):4063–4070. doi: 10.1523/JNEUROSCI.4709-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rubia K, Smith AB, Taylor E, Brammer M. Linear age-correlated functional development of right inferior fronto-striato-cerebellar networks during response inhibition and anterior cingulate during error-related processes. Hum Brain Mapp. 2007;28(11):1163–1177. doi: 10.1002/hbm.20347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Velanova K, Wheeler ME, Luna B. Maturational changes in anterior cingulate and frontoparietal recruitment support the development of error processing and inhibitory control. Cereb Cortex. 2008;18(11):2505–2522. doi: 10.1093/cercor/bhn012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fitzgerald KD, Perkins SC, Angstadt M, et al. The development of performance-monitoring function in the posterior medial frontal cortex. Neuroimage. 2010;49(4):3463–3473. doi: 10.1016/j.neuroimage.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Davies PL, Segalowitz SJ, Gavin WJ. Development of response-monitoring ERPs in 7- to 25-year-olds. Dev Neuropsychol. 2004;25(3):355–376. doi: 10.1207/s15326942dn2503_6. [DOI] [PubMed] [Google Scholar]
- 42.Yeung N, Cohen JD, Botvinick MM. The neural basis of error detection: conflict monitoring and the error-related negativity. Psychol Rev. 2004;111(4):931–959. doi: 10.1037/0033-295x.111.4.939. [DOI] [PubMed] [Google Scholar]
- 43.Carter CS, Braver TS, Barch DM, Botvinick MM, Noll D, Cohen JD. Anterior cingulate cortex, error detection, and the online monitoring of performance. Science. 1998;280(5364):747–749. doi: 10.1126/science.280.5364.747. [DOI] [PubMed] [Google Scholar]
- 44.Perkins SC, Welsh RC, Stern ER, Taylor SF, Fitzgerald KD. Topographic analysis of the development of individual activation patterns during performance monitoring in medial frontal cortex. Dev Cogn Neurosci. 2013;6:137–148. doi: 10.1016/j.dcn.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Perlman SB, Pelphrey KA. Regulatory brain development: balancing emotion and cognition. Soc Neurosci. 2010;5(5–6):533–542. doi: 10.1080/17470911003683219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fair DA, Dosenbach NU, Church JA, et al. Development of distinct control networks through segregation and integration. Proc Natl Acad Sci U S A. 2007;104(33):13507–13512. doi: 10.1073/pnas.0705843104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Steinbeis N, Haushofer J, Fehr E, Singer T. Development of behavioral control and associated vmPFC-DLPFC connectivity explains children’s increased resistance to temptation in intertemporal choice. Cereb Cortex. doi: 10.1093/cercor/bhu167. [DOI] [PubMed] [Google Scholar]
- 48.Ursu S, Stenger VA, Shear MK, Jones MR, Carter CS. Overactive action monitoring in obsessive-compulsive disorder: evidence from functional magnetic resonance imaging. Psychol Sci. 2003;14(4):347–353. doi: 10.1111/1467-9280.24411. [DOI] [PubMed] [Google Scholar]
- 49.Fitzgerald KD, Welsh RC, Gehring WJ, et al. Error-related hyperactivity of the anterior cingulate cortex in obsessive compulsive disorder. Biol Psychiatry. 2005;57(3):287–294. doi: 10.1016/j.biopsych.2004.10.038. [DOI] [PubMed] [Google Scholar]
- 50.Maltby N, Tolin DF, Worhunsky P, O’Keefe TM, Kiehl KA. Dysfunctional action monitoring hyperactivates frontal-striatal circuits in obsessive-compulsive disorder: an event-related fMRI study. Neuroimage. 2005;24(2):495–503. doi: 10.1016/j.neuroimage.2004.08.041. [DOI] [PubMed] [Google Scholar]
- 51.Yucel M, Harrison BJ, Wood SJ, et al. Functional and biochemical alterations of the medial frontal cortex in obsessive-compulsive disorder. Arch Gen Psychiatry. 2007;64(8):946–955. doi: 10.1001/archpsyc.64.8.946. [DOI] [PubMed] [Google Scholar]
- 52.Stern ER, Welsh RC, Fitzgerald KD, et al. Hyperactive error responses and altered connectivity in ventromedial and frontoinsular cortices in obsessive-compulsive disorder. Biol Psychiatry. 2011;69(6):583–591. doi: 10.1016/j.biopsych.2010.09.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fitzgerald KD, Stern ER, Angstadt M, et al. Altered function and connectivity of the medial frontal cortex in pediatric obsessive-compulsive disorder. Biol Psychiatry. 2010;68(11):1039–1047. doi: 10.1016/j.biopsych.2010.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Huyser C, Veltman DJ, Wolters LH, de Haan E, Boer F. Developmental aspects of error and high-conflict-related brain activity in pediatric obsessive-compulsive disorder: a fMRI study with a Flanker task before and after CBT. J Child Psychol Psychiatry. 2011;52(12):1251–1260. doi: 10.1111/j.1469-7610.2011.02439.x. [DOI] [PubMed] [Google Scholar]
- 55.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th. Washington, DC: American Psychiatric Association; 2000. text rev. [Google Scholar]
- 56.Gilbert P. The evolved basis and adaptive functions of cognitive distortions. Br J Med Psychol. 1998;71(Pt 4):447–463. doi: 10.1111/j.2044-8341.1998.tb01002.x. [DOI] [PubMed] [Google Scholar]
- 57.Szechtman H, Woody E. Obsessive-compulsive disorder as a disturbance of security motivation. Psychol Rev. 2004;111(1):111–127. doi: 10.1037/0033-295X.111.1.111. [DOI] [PubMed] [Google Scholar]
- 58.Schwartz JM. A role for volition and attention in the generation of new brain circuitry: toward a neurobiology of mental force. Journal of Conciousness Studies. 1999;6(8–9):115–142. [Google Scholar]
- 59.van den Heuvel OA, Veltman DJ, Groenewegen HJ, et al. Disorder-specific neuroanatomical correlates of attentional bias in obsessive-compulsive disorder, panic disorder, and hypochondriasis. Arch Gen Psychiatry. 2005;62(8):922–933. doi: 10.1001/archpsyc.62.8.922. [DOI] [PubMed] [Google Scholar]
- 60.Goldin PR, Manber T, Hakimi S, Canli T, Gross JJ. Neural bases of social anxiety disorder: emotional reactivity and cognitive regulation during social and physical threat. Arch Gen Psychiatry. 2009;66(2):170–180. doi: 10.1001/archgenpsychiatry.2008.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Moser JS, Moran TP, Jendrusina AA. Parsing relationships between dimensions of anxiety and action monitoring brain potentials in female undergraduates. Psychophysiology. 2012;49(1):3–10. doi: 10.1111/j.1469-8986.2011.01279.x. [DOI] [PubMed] [Google Scholar]
- 62.Righi S, Mecacci L, Viggiano MP. Anxiety, cognitive self-evaluation and performance: ERP correlates. J Anxiety Disord. 2009;23(8):1132–1138. doi: 10.1016/j.janxdis.2009.07.018. [DOI] [PubMed] [Google Scholar]
- 63.Fitzgerald KD, Liu Y, Stern ER, et al. Reduced error-related activation of dorsolateral prefrontal cortex across pediatric anxiety disorders. J Am Acad Child Adolesc Psychiatry. 2013;52(11):1183–1191. doi: 10.1016/j.jaac.2013.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Woolley J, Heyman I, Brammer M, Frampton I, McGuire PK, Rubia K. Brain activation in paediatric obsessive compulsive disorder during tasks of inhibitory control. Br J Psychiatry. 2008;192(1):25–31. doi: 10.1192/bjp.bp.107.036558. [DOI] [PubMed] [Google Scholar]
- 65.Gehring WJ, Liu Y, Orr JM, Carp J. The error-related negativity (ERN/Ne) In: Luck SK, Kappenman E, editors. Oxford Handbook of Event-Related Potential Components. New York: Oxford University Press; 2012. pp. 231–291. [Google Scholar]
- 66.Whiteside SP, Port JD, Abramowitz JS. A meta-analysis of functional neuroimaging in obsessive-compulsive disorder. Psychiatry Res. 2004;132(1):69–79. doi: 10.1016/j.pscychresns.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 67.Beucke JC, Sepulcre J, Talukdar T, et al. Abnormally high degree connectivity of the orbitofrontal cortex in obsessive-compulsive disorder. JAMA Psychiatry. 2013;70(6):619–629. doi: 10.1001/jamapsychiatry.2013.173. [DOI] [PubMed] [Google Scholar]
- 68.Spunt RP, Lieberman MD, Cohen JR, Eisenberger NI. The phenomenology of error processing: the dorsal ACC response to stop-signal errors tracks reports of negative affect. J Cogn Neurosci. 2012;24(8):1753–1765. doi: 10.1162/jocn_a_00242. [DOI] [PubMed] [Google Scholar]
- 69.Ferdinand NK, Kray J. Developmental changes in performance monitoring: how electrophysiological data can enhance our understanding of error and feedback processing in childhood and adolescence. Behav Brain Res. 2014;263:122–132. doi: 10.1016/j.bbr.2014.01.029. [DOI] [PubMed] [Google Scholar]
- 70.Santesso DL, Segalowitz SJ, Schmidt LA. Error-related electrocortical responses are enhanced in children with obsessive-compulsive behaviors. Dev Neuropsychol. 2006;29(3):431–445. doi: 10.1207/s15326942dn2903_3. [DOI] [PubMed] [Google Scholar]
- 71.Torpey DC, Hajcak G, Kim J, Kujawa AJ, Dyson MW, Olino TM, Klein DN. Error-related brain activity in young children: associations with parental anxiety and child temperamental negative emotionality. J Child Psychol Psychiatry. 2013;54(8):854–862. doi: 10.1111/jcpp.12041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bress JN, Meyer A, Hajcak G. Differentiating anxiety and depression in children and adolescents: Evidence from event-related brain potentials. J Clin Child Adolesc Psychol. 2015;44(2):238–249. doi: 10.1080/15374416.2013.814544. [DOI] [PubMed] [Google Scholar]
- 73.Achenbach TM. The Achenbach System of Empirically Based Assessemnt (ASEBA): Development, Findings, Theory, and Applications. Burlington, VT: University of Vermont Research Center for Children, Youth & Families; 2009. [Google Scholar]


