Abstract
Despite evidence that inactivity is a major factor causing ill health in people with intellectual disabilities (pwID) there are gaps in our knowledge of their physical activity (PA). To date, there is no published systematic review of their PA levels. Therefore, we performed a systematic review from January–October 2015, comprising studies from across the globe to establish PA levels, determine how they were measured, and what factors influenced PA in adults with intellectual disabilities (awID). Five databases were searched. Studies were included if written in English, peer-reviewed, had primary research data, and measured PA levels of awID. Quality was assessed using a 19-item checklist. Meta-summary of the findings was performed and a meta-analysis of factors influencing PA using multiple regression.
Fifteen studies were included consisting of 3159 awID, aged 16–81 years, 54% male and 46% female. Only 9% of participants achieved minimum PA guidelines. PA levels were measured using objective and subjective methods. ID severity, living in care, gender, and age were independently significantly correlated with the number of participants achieving PA guidelines with the strongest predictor being ID severity (Beta 0.631, p < 0.001). Findings should be in the context that most of the participants were in the mild/moderate range of ID severity and none of the studies objectively measured PA in people with profound ID. To inform measurement and intervention design for improved PA, we recommend that there is an urgent need for future PA studies in awID population to include all disability severity levels. PROSPERO registration number CRD42015016675.
Keywords: Intellectual disability, Physical activity, Physical activity level, Measurement of physical activity
Highlights
-
•
Only 9% of adults with ID achieved minimum PA guidelines.
-
•
Their PA levels are predicted by age, sex, ID severity, and living in care.
-
•
The strongest predictor of PA is high (severe/profound) ID severity.
-
•
None of the studies objectively measured PA in people with profound ID.
1. Introduction
Intellectual disabilities (ID1) also referred to as learning disability in the UK and intellectual developmental disorder in the U.S. is defined as ‘a significantly reduced ability to understand new or complex information and to learn and apply new skills. The intellectual disability begins before adulthood, resulting in a reduced ability to cope independently, with a lasting effect on development’ (World Health Organisation, 2015). In addition, the extent to which an individual is unable to face the demands established by society for the individual's age group can be further classified as: mild, moderate, severe, and profound (Katz and Lazcano-ponce, 2008, Salvador-Carulla et al., 2011, American Psychiatric Association aww, 2013). Estimates of prevalence of ID vary for several reasons, including methodological differences between studies (Harris, 2006, Doran et al., 2012, Maulik et al., 2011), the wealth of the country, and the age-group of the study population (Harris, 2006, Maulik et al., 2011, Maulik and Harbour, 2010). Maulik et al. (2011) reported a prevalence of 16.41 and 15.94/1000 population in low- and middle-income countries respectively, whereas in high-income countries, these figures are lower, at an estimated prevalence of 9.21/1000 population. Additionally, they reported higher prevalence among studies based on children/adolescents (18.30/1000), compared to those on adults (4.94/1000) (Maulik et al., 2011). Importantly, these figures are set to rise due to increase in life expectancy in this group of people (Harris, 2006, Holland, 2000, Emerson et al., 2014). This has implications as people with intellectual disabilities (pwID2) have poorer health than their non-disabled peers, with differences in health status that are avoidable (Emerson et al., 2014, Krahn et al., 2006, Heslop et al., 2014). These differences start early in life, with higher prevalence of diseases such as obesity, hypertension, and hyperlipidemia common among pwID as early as adolescence (Lin et al., 2010, Wallén et al., 2009). While there may be several reasons for these health differences (Krahn et al., 2006, Heslop et al., 2014, Emerson and Baines, 2011), low level of physical activity (PA3) is one of the key lifestyle factors causing ill health and an increased risk of chronic diseases in pwID (Bergstrom et al., 2013, Robertson et al., 2000). The medical and nonmedical lifetime costs associated with the diagnoses of ID are much higher than for non-ID individuals with many associated with an inactive lifestyle. These costs are substantially higher than those associated with the diagnosis of other disabilities (e.g., cerebral palsy, vision, and hearing impairments) and could potentially be reduced with lifestyle modifications (Doran et al., 2012, Honeycutt et al., 2004).
A physically inactive lifestyle increases the risk of non-communicable diseases. However, increasing PA has been shown to improve health outcomes (Richards et al., 2013, Lifestyles statistics team HaSCIC, 2014). In spite of clear guidance about the need for an active lifestyle, several studies in the literature reported absence of regular PA in adults with intellectual disabilities (awID4) (Robertson et al., 2000, Finlayson et al., 2009, McGuire et al., 2007, Haveman et al., 2011, Emerson, 2005, Frey, 2004, Draheim et al., 2002). Compared with the general population, there are gaps in our knowledge of their PA. For example, individual factors such as sex, race, and social status that have been shown in the general population to influence PA levels are yet to be established within ID populations. To implement effective non-communicable disease prevention programmes, policy makers need data for PA levels (Hallal et al., 2012). However, to date, there is no published systematic review of PA levels in awID. A review by Temple et al. (2006), on PA levels in awID, did not use systematic methodology. Out of the 14 papers included in their review, eight used questionnaires that were neither valid nor reliable and overall, their review data were informed by studies set within a limited context, with high levels of bias and samples that were not reflective of ID populations. This gap in the literature highlights the need for a systematic review to determine PA levels within ID populations, and factors relating to this behaviour in order to improve risk factor identification and better target PA promotion in this group. It is hoped that the findings of the review will promote our understanding of the factors influencing PA levels and in turn inform interventions to minimise inactivity. Therefore, the aims of this review will be to examine the published literature to establish PA levels, determine how PA levels were measured and examine the reported factors that influenced PA levels in awID.
2. Methods
The review was prepared and reported with reference to the ‘Preferred Reporting Items for Systematic Reviews and Meta-Analyses’ guidelines (Moher et al., 2009). A protocol for this review was registered with PROSPERO on 02/03/15, registration number CRD42015016675. Available at http://www.crd.york.ac.uk/PROSPERO.
2.1. Identification of literature
Searches of electronic literature databases were conducted in January 2015 from the earliest available date. The databases searched were Cochrane Library, PubMed, Web of Science, CINAHL, and MEDLINE (the latter two via EBSCO). In order to ensure that no relevant studies were missed, additional studies were identified by hand searching reference list of reviews and research papers relating to PA in pwID. The searches were re-run in July 2015 just before the final analyses, but no further study was retrieved.
2.1.1. Search strategy
In each database, terms for intellectual disability and associated synonyms were identified. These terms were then combined with search terms relating to PA and PA level/measurement. Searches were limited to papers published in English language, on humans and included adults (Appendix A).
2.2. Screening and eligibility
All articles identified by searches were exported to Endnote Web. Duplicates and irrelevant records were removed. Remaining records were screened by one review author (YD) to identify studies that potentially met the inclusion criteria outlined below (Section 2.2.1). The full text of these potentially eligible studies was retrieved and independently assessed for eligibility by the same reviewer. A second reviewer (JC) blinded to the first author's selection, randomly selected 8 (24%) potentially eligible studies and independently assessed their eligibility. Disagreement between reviewers was resolved through discussion with a third reviewer (HD). Using Cohen's k (Cohen, 1960), a substantial agreement was found between the first and second reviewers (k = 0.8, p < 0.05).
2.2.1. Inclusion criteria
-
1.
Studies that quantitatively measured levels of PA in awID (where ID is diagnosed using any recognised diagnostic criteria, or on a GP list of pwID or identified as having ID by the social services department or using the specialist ID service or had done so in the past)
-
2.
The following study designs were eligible for inclusion in the review: cross-sectional, cohort, and case control studies
-
3.
Published in English between 2004 and the present
-
4.
Peer reviewed
-
5.
Included subjects that are aged 16 + (at least 95% of the participants are aged 16 +)
-
6.
Have primary research data.
2.2.2. Exclusion criteria
-
1.
Intervention studies (both field and clinical trials) and single case studies
-
2.
Papers that were not published in English language
-
3.
Published before 2004
-
4.
Not peer reviewed
-
5.
Studies on children and young people up to 16 years
-
6.
Studies that did not have primary research data
-
7.
Grey literature, e.g. dissertations, conference abstracts, research reports, chapter(s) from a book, personal correspondence or commentaries, and policy documents.
2.2.3. Context
There have been several delineations of PA proposed and used in the literature with Strath and colleagues (Strath et al., 2013) suggesting that they are derivatives of the definition by Caspersen et al. (1985). Therefore, for this review, the working definition for PA was described as: ‘Any bodily movements produced by skeletal muscles that result in energy expenditure.’ (Caspersen et al., 1985).
The date limit for the searches was set between 2004 and the present, because the majority of older researches measuring PA levels in pwID used questionnaires and interview that were likely not to be validated. Consequently, for the quality assessment of the studies in this review, one of the criteria addressed the subject of instrument validity and reliability (question 13, Table 1).
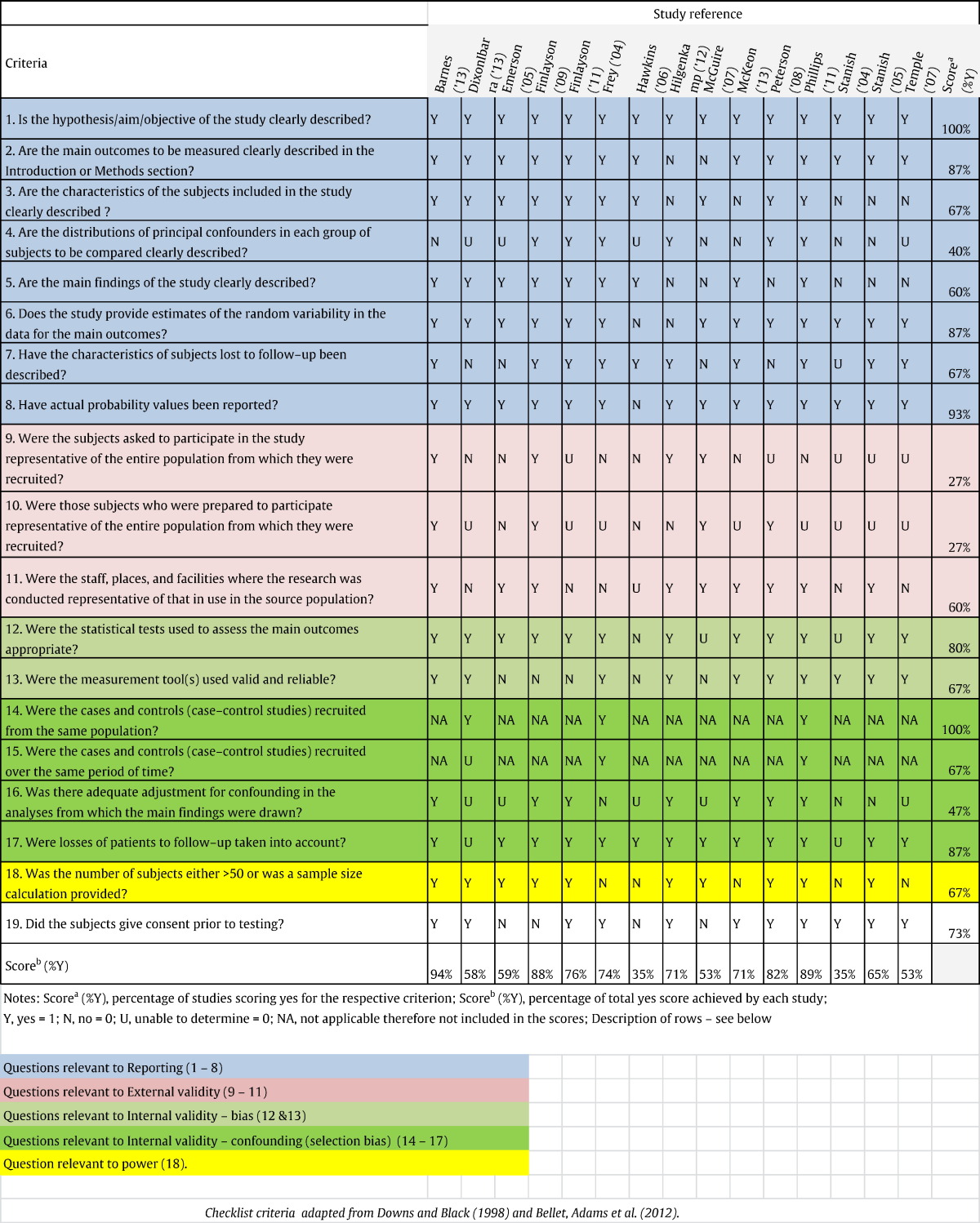
Table 1.
Critical appraisal of included studies.
2.3. Quality assessment
Each included study was critically appraised for its methodological quality using a 19-item checklist (Table 1). Items 1–17 were adapted from a 27-item checklist developed by Downs and Black (Downs and Black, 1998). Nine items from the original checklist were excluded as they were only relevant to studies investigating the effectiveness of an intervention and one item, the one relating to power calculation was adapted in line with the checklist developed by Bellet et al. (2012).
2.4. Data extraction
Data extraction was developed based on existing systematic review articles in related fields. The form was pilot-tested on three randomly selected included studies and refined accordingly. Data extraction was completed by one reviewer (YD); extracted information included: bibliographic details (author and year); the country within which the study took place; sample size and participants' demographic data (Table 2) including characteristics of the groups as well classification of ID severity (i.e. mild, moderate, severe, and profound); study design; measurement tools; inclusion and exclusion criteria; outcome measures; main results and issues raised in the discussion. Missing data were requested from study authors by e-mail.
Table 2.
Summary of included studies (bibliographic details and participants' demographic data).
| Bibliographic details |
Sample size |
Age range: mean (SD) |
Level of disability |
Sex |
Race |
Residence |
Employment |
Risk factors for cardiovascular diseases |
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author & year | Country where study took place | Mild | Moderate | Severe | Profound | Male | Female | Caucasian | African | Asian | Others | Alone | Supervised apartment/residential home | With family | Full/part time | Not working | BMI < 20 (kg/m2) underweight | BMI 20–25 (kg/m2) normal | BMI 25–30 (kg/m2) overweight | BMI > 30 (kg/m2) obese | Hypertension | Cholesterol level | ||
| Barnes et al. (2013) | USA | 131 | 18–65: 37.5 (11.8) | NR | NR | 0 | 0 | 70a | 61a | 52a | 76a | 0 | 3a | 2 | 63 | 66 | NR | NR | 0c | 26a | 105a | NR | NR | NR |
| Dixon-Ibarra et al. (2013) | USA | 76 | 20–77: 42.8a (7.80a) | NR | NR | 0 | 0 | 48 | 36 | 72 | 2 | 1 | 1 | 17 | 50 | 9 | 55 | 21 | 2 | 23 | 26 | 20 | NR | NR |
| Emerson (2005) | UK | 1542 | 16–75 +: 49.3 (15.5) | 504 | 443 | 441 | NR | 824 | 693 | 1485 | 10 | 9 | 10 | 0 | 1542 | 0 | NR | NR | 183 | 404 | 365 | 352 | NR | NR |
| Finlayson et al. (2009) | UK | 433 | 16–75a: 44.1 (14.0) | 158 | 99 | 91 | 85 | 232 | 201 | NR | NR | NR | NR | 35 | 225 | 173 | 102 | 331 | 27 | 103 | 140 | 108 | NR | NR |
| Finlayson et al. (2011) | UK | 62 | 18–66: 37.1 (12.8) | 62c | 0 | 0 | 0 | 27 | 35 | 61 | 0 | 1 | 0 | 2 | 27 | 33 | 51 | 11 | 0 | 16 | 46 | 0 | NR | NR |
| Frey (2004) | USA | 22 | 26–44a: 34.9 (9.0) | 22 | 0 | 0 | 0 | 11 | 11 | NR | NR | NR | NR | 3 | 7a | 12 | 21 | 1 | NR | NR | NR | NR | 2 | 1 |
| Hawkins and Look (2006) | UK | 19 | 22–25: 38 (NR) | 6 | 6 | 7 | 0 | 16 | 3 | NR | NR | NR | NR | 0 | 19 | 0 | NR | NR | 3 | 6 | 6 | 4 | NR | NR |
| Hilgenkamp et al. (2012) | Netherlands | 257 | 50–81: 59.7 (6.9)d | 88 | 143 | 10 | 0 | 133 | 124 | NR | NR | NR | NR | 17 | 237d | 3 | NR | NR | NR | NR | NR | NR | NR | NR |
| McGuire et al. (2007) | Ireland | 157 | 16–65: 37 (11.73) | 22 | 99 | 20 | 14 | 81 | 74 | NR | NR | NR | NR | 0c | 88 | 64 | NR | NR | 3 | 39a | 49 | 39 | NR | NR |
| McKeon et al. (2013) | Irelandd | 17 | 19–59c: 42 (NR) | 6 | 2 | 9a | 0a | 17 | 0 | NR | NR | NR | NR | 5 | 2d | 10d | NR | NR | NR | NR | NR | NR | NR | NR |
| Peterson et al. (2008) | USA | 131 | 18–60: 37.2 (11.6) | 73 | 41 | 0 | 0 | 63 | 68 | NR | NR | NR | NR | 0 | 131 | 0 | 124 | 7 | NR | NR | NR | NR | NR | NR |
| Phillips and Holland (2011)b | UK (check age) | 152 | 12–64: 33.6 (14.7) | 54 | 56 | 42 | 0 | 74 | 78 | NR | NR | NR | NR | 0 | 91 | 61 | 14 | 138 | 3 | 45 | 50 | 54 | NR | NR |
| Stanish (2004) | Canada | 20 | 19–65: 36.8a (NR) | 20 | 0 | 0 | 0 | 8 | 12 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Stanish and Draheim (2005) | Canada | 103 | 19–65: 37.3 (10.7) | NR | NR | 0 | 0 | 65 | 38 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Temple (2007) | Canada | 37 | 18–52: NR | NR | NR | NR | NR | 18 | 19 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
Notes: sample size = intellectual disability sample size in the studies; SD = standard deviation; NR = not recorded.
Calculated based on data provided.
< 5% of data is from participants < 16 years old.
Inferred but not stated.
Data/information obtained from author.
2.5. Data analysis
A descriptive summary of the included studies was completed (Table 2, Table 3). A metasummary was performed structured around PA levels of awID and its measurements. A meta-analysis was performed with a pooled summary of the variables and using simple linear regression models. The models were run separately for each of the independent variables (mean age, proportion of male, proportion living in care, and proportion with high ID severity) to determine the association between the percentage of participants achieving physical activity guidelines (PAG5) and each of the independent variables. We thereafter used a multiple regression model to examine the combined associations between all the independent variables and the percentage of participants achieving PAG as shown in Table 4.
Table 3.
Synopsis of included studies on the measurements of physical activity levels and key findings.
| Author & year | Sample size | Study design | Inclusion criteria | Measurement tool | PAG | % meeting PAG | Mean steps/d (SD) | Main results and issues raised in the discussion |
|---|---|---|---|---|---|---|---|---|
| Barnes et al. (2013) | 131 | Cross-sectional | Aged 18–65 years, have mild to moderate ID, were ambulatory, were not underweight, and did not have any serious medical conditions, were able to comprehend and communicate verbally, and able to give informed consent. | Physical Activity Checklist Interview (PACI) + accelerometer | 150 min of MVPA | 23.70% | NR | Older individuals had a significant lower MVPA compared with younger adults; males had a significant higher MVPA than females; the most common activity reported was walking (53.7%) followed by inside chores (42.5%). |
| Dixon-Ibarra et al. (2013) | 76 | Case control | All participants were verbal, ambulatory, and could recite what they had to do for the study and did not have severe ID | Pedometer and accelerometer | > 10,000 steps/day 150 min of moderate PA/75 min of vigorous PA in bouts > 10 min | 7.2% b 11.76%b | 5452.26b (3024.85b) | A small proportion of older adults with ID (6%) met national physical activity guideline and sedentary behaviour was also an observable factor in this study. |
| Finlayson et al. (2011) | 62 | Cross-sectional | Participants were aged 16 and over with mild to moderate intellectual disabilities with capacity to consent. | Semi structured interviews & accelerometer | > 10,000 steps/day 30 mins of MVPA for at least 5 days/week |
27% 15% |
8509 (4384) | Sixty-six percent of participants wore the activity monitor at least 5 days. Mean steps/day was significantly different between men and women (p = 0.001): 11,101 and 6481, respectively. |
| Frey (2004) | 48 | Case control | Participants were free from physical or sensory conditions that could impede or interfere with movement; ambulated freely; co-existing morbidity did not limit PA participation or other activities of daily living. | Accelerometer | 30 min of continuous bouts of moderate to very hard activity | 0%a | NR | PA levels of adults with mental retardation are similar to those of sedentary peers without. Neither group engages in recommended levels of PA |
| McKeon et al. (2013) | 17 | Cross-sectional | NR | International Physical Activity Questionnaire (IPAQ) + accelerometer | Moderate to high activity 5 days/weeka | 46%b | 5308 (5502) | The average time spent in sedentary behaviour from the accelerometer and IPAQ (short version) was 10.17 (SD, 2.06) and 9.36 h (SD, 3.21) per day, respectively |
| Phillips and Holland (2011)c | 152 | Cross-sectional | Participants were known to intellectual disability services, were aged 12 years and above, and could walk unaided. |
IPAQ — Short Version + accelerometer | 30 min of MVPA for at least 5 days/week in bouts of 10 min | 0% | 6334c | Males were more active than females. There was a trend for physical activity to decline and sedentary behaviour to increase with age, and for those with more severe levels of intellectual disability to be more sedentary and less physically active. |
| Hilgenkamp et al. (2012) | 257 | Cross-sectional | They were eligible if they found pedometer acceptable and have a comfortable walking speed of 3.2 km/h or more in at least one of three recordings. | Pedometer and a diary | > 10,000 steps/day | 16.7% | 6600.99b (3519.95b) | The measured sample was the more functionally able part of the total sample; therefore, this result is likely to be a considerable overestimation of the actual physical activity levels in this population. |
| Peterson et al. (2008) | 131 | Cross-sectional | Ambulatory individuals aged 18–60 years with mild–moderate ID receiving ≥ 10 h/week of group supported living services; lived outside the family home; able complete interview meaningfully. | Pedometer | > 10,000 steps/day | 14.10% | 6621 (3366) | Physical activity (steps/day) achieved by the majority of this population is insufficient for health benefits, particularly among individuals with moderate intellectual disability. Evenings and weekends are especially inactive time periods. |
| Stanish (2004) | 20 | Cross-sectional | NR | Pedometers | > 10,000 steps/day | 45% | 9631.8b | Week days steps per day in this group are comparable to the general population. Males and females with mental retardation are a homogenous group in regard to walking activity. |
| Stanish and Draheim (2005) | 103 | Cross-sectional | NR | National Health and Nutrition Examination Survey (NHANES) III + Pedometers | > 10,000 steps/day Five or more bouts of MVPA/week totalling 30 min per bout | 21.4% 17.5% | 7832b | Only 17.5% of the participants reported engaging in five bouts of MVPA per week totalling 30 min per bout. |
| Temple (2007) | 37 | Cross-sectional | NR | Pedometers | > 10,000 steps/day | Not stated | 8100 (3735.4) | The best predictive variables of steps/day were barriers to PA and preference for sedentary behaviour |
| Emerson (2005) | 1542 | Cross-sectional | They were eligible if they lived in supported accommodation | Physical Activity Scale | 12 bouts of MVPA in 4 weeks (retrospectively) | 4% | NR | Men and women with ID were less active than men and women without ID in all age groups (p < 0.001) |
| Finlayson et al. (2009) | 433 | Prospective longitudinal study | All adults with ID within a defined geographical area were included | Semi structured interviews | 30 min of MVPA for at least 5 days/week | 5% | NR | Walking is the commonest regular physical activity, but not at a sufficient intensity level or duration; older age, immobility, epilepsy, no daytime opportunities, living in congregate care and faecal incontinence were independently predictive of low levels of activity. |
| Hawkins and Look (2006) | 19 | Cross-sectional | They were eligible if they were able to walk unaided | Diary | 30 min of MVPA for at least 5 days/week | 11%b | NR | The levels of physical activity were higher in the sample population than previous figures for adults with learning disabilities, but lower than figures for the general population. |
| McGuire et al. (2007) | 157 | Cross-sectional | Included in the study were careers of adults with an ID – in residential group homes and in the family setting | Lifestyle and Health Behaviour Questionnaire | 20 min of mild exercise 4 or more times/weekd | 25.90% | NR | There were no gender differences in health and lifestyle profiles. |
Notes: sample size = intellectual disability sample size in the studies; Measurement tool = Physical activity measuring tools; % meeting PAG = percentage of participants that met specified physical activity guideline; PAG = physical activity guideline used as an outcome measure; NR = not recorded; ID = intellectual disabilities; PA = physical activities; moderate to vigorous physical activity (MVPA); mean steps/d, mean steps per day or per week day.
Inferred but not stated.
Calculated based on data provided.
< 5% of data is from participants < 16 years old.
It is unclear if this is equivalent to 150 min of moderate physical activities.
Table 4.
Summary of multiple linear regression analysis for the variables predicting the percentage of adults with intellectual disabilities that met physical activity guidelines (n = 2999).
| Model summary⁎⁎ |
ANOVAb |
Coefficientsb |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| R | R square | Adjusted R square | Std. error of the estimate | df (regression, residual) |
Mean square (regression, residual) |
F | B | Beta | t | |
| .746a | 0.557 | 0.556 | 0.05352 | 4 | 2.695 | 941.168⁎ | (Constant) | 0.063 | 5.213⁎ | |
| 2994 | 0.003 | Proportion living in supervised/residential care | − 0.169 | − 0.477 | − 30.039⁎ | |||||
| Mean age of participants | 0.001 | 0.101 | 6.354⁎ | |||||||
| Proportion of male | 0.368 | 0.232 | 18.092⁎ | |||||||
| Proportion with severe and profound disability | − 0.385 | − 0.631 | − 49.934⁎ | |||||||
Predictors: (constant), mean age of participants, proportion of male, proportion with severe and profound ID severity, proportion living in supervised/residential care.
Dependent variable: % meeting physical activity guidelines.
Significant at p value < 0.001.
Using the enter method.
Results were expressed as regression coefficients representing the variation in the numbers achieving PAG (see Section 2.6.) explained by the regression model. All analyses were conducted using SPSS for Windows (version 22.0), and cases were weighted by sample size.
2.6. PA guidelines
The current minimum weekly aerobic ‘global PAG for Health’ is that adults should do at least 150 min of moderate-intensity aerobic PA or 75 min of vigorous-intensity aerobic PA throughout the week or an equivalent combination of moderate - and vigorous-intensity activity. These activities should be in bouts of at least 10 min (World Health Organisation, 2011). These guidelines are similar to the ones used in many westernised nations (Chief Medical Officer C, 2011, The Office of Disease Prevention and Health Promotion, 2008, Australian Government Department of Health, 2014) and similar to the ones used in the included studies. The minimum PAG used in majority of the studies was 150 min of moderate to vigorous physical activity/week (150 min MVPA6). Some studies also used the number of steps/week as their PA criteria.
3. Results
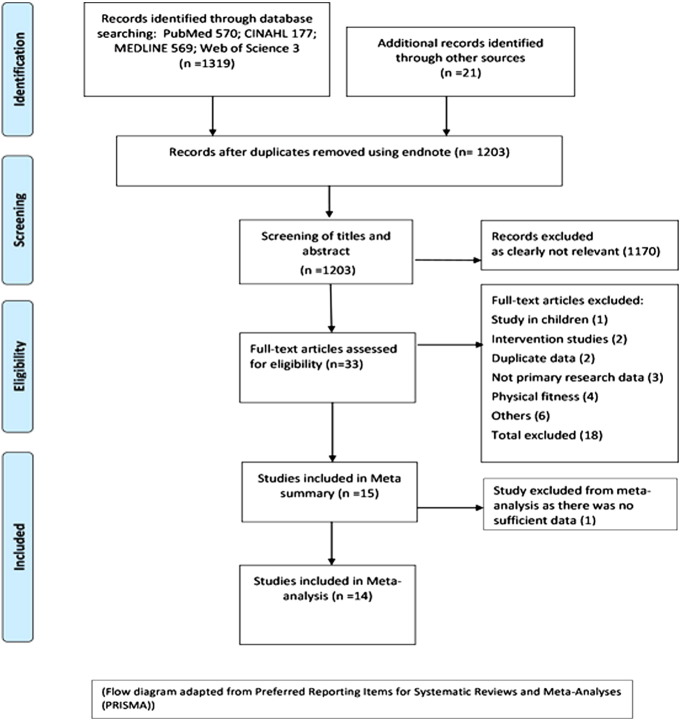
Total records found were 1319, and review flow is given in Fig. 1. Fifteen studies were included in this review. The studies comprised 3159 awID, aged 16 to 81 years (mean age 45.99 years, SD 6.79), 54% male and 46% female. Eighty three percent had their ID severity reported as 39% mild, 34% moderate, 23% severe, and 4% profound. Of the 28% asked about employment, 42% were employed. Table 1 summarises the result of the quality assessment, while Table 2 provides a summary of the bibliographic details as well as participants' demographic data. The methodological quality of the included studies varied greatly, with none of the studies achieving 100% yes score in the 19-item checklist (Table 1). Five studies scored > 75% (Finlayson et al., 2009, Barnes et al., 2013, Finlayson et al., 2011, Peterson et al., 2008, Phillips and Holland, 2011), eight studies scored > 50%, but < 75% (McGuire et al., 2007, Emerson, 2005, Frey, 2004, Dixon-Ibarra et al., 2013, Hilgenkamp et al., 2012, McKeon et al., 2013, Stanish, 2004, Stanish and Draheim, 2005, Temple, 2007), and two studies scored < 50% (Stanish, 2004, Hawkins and Look, 2006). Only 3 (Finlayson et al., 2009, McGuire et al., 2007, Barnes et al., 2013) out of the 15 studies met all the criteria for external validity assessment items. There was evidence of high selection bias as demonstrated by the relatively low score with respect to the questions addressing adjustment for confounding variables (Table 1, questions 4 and 16). Most studies did not describe the distributions of principal confounders in each group of subjects compared, nor did they investigate possible confounders or adjust for them in their analysis. A summary of PA measurements and results of individual studies is presented in Table 3.
Fig. 1.
Flow of studies in the systematic review.
3.1. PA level measurement
Methods used to measure PA levels are summarised in Table 3. Objective measuring instruments used were accelerometers and pedometers, while the subjective measuring instruments were diaries (Hilgenkamp et al., 2012, Hawkins and Look, 2006), and the following semi-structured interviews and questionnaire surveys: International Physical Activity Questionnaire (IPAQ7) (Phillips and Holland, 2011, McKeon et al., 2013); Physical Activity Checklist Interview (PACI) (Barnes et al., 2013); physical activity scale (Emerson, 2005); National Health and Nutrition Examination Survey (NHANES) III (Stanish and Draheim, 2005).
Six studies (Barnes et al., 2013, Finlayson et al., 2011, Phillips and Holland, 2011, Hilgenkamp et al., 2012, McKeon et al., 2013, Stanish and Draheim, 2005) used both direct observations as well as either a survey/interview/dairy. Eleven studies used objective methods, five of which used accelerometers (Frey, 2004, Barnes et al., 2013, Finlayson et al., 2011, Phillips and Holland, 2011, McKeon et al., 2013), five used pedometers (Peterson et al., 2008, Hilgenkamp et al., 2012, Stanish, 2004, Stanish and Draheim, 2005, Temple, 2007), and one study used both accelerometers and pedometers (Dixon-Ibarra et al., 2013). Nine studies reported the number of steps/day (Table 3) with a mean of 6794.7 (range 5308 to 9632, SD 908.6) steps/day.
Overall, only two of the included studies (Finlayson et al., 2009, McGuire et al., 2007) measured PA in participants with profound ID, and they used semi-structured interview and a questionnaire survey, neither of which was shown to be valid or reliable (see Table 1, question 13).
Most of the studies did not record the number of invitees, consequently, it was difficult to predict recruitment rate. However, one study consisting of people with mild to moderate ID found that 39% of people invited agreed to take part (Peterson et al., 2008) and two of the studies that used survey/interview found the response rate in people with mild-moderate ID to be above 60% (Finlayson et al., 2009, McGuire et al., 2007).
3.2. PA level of awID
The studies used different PAG as outcome measures to determine the number of participants classified as ‘active’ (Table 3). PAG were country specific and some of these were based on frequency and intensity of PA, while others were based on number of steps/week. The intensity/frequency based PA criterion were essentially a derivative of the ‘global PAG for health’ (World Health Organisation, 2011), whereas the health related criterion for number of steps was those achieving ≥ 10,000 steps/day (Tudor-Locke et al., 2008). In the majority of the studies, only one PAG was used to determine percentage of active people, however, three studies (Finlayson et al., 2011, Dixon-Ibarra et al., 2013, Stanish and Draheim, 2005) used two different guidelines on the same population. They used intensity/frequency based PA criterion as well as number of steps. There was a difference between the number of participants that achieved equivalent 150 min MVPA and those achieving ≥ 10,000 steps/day. Two of the studies found that higher number of participants achieved ≥ 10,000 steps compared with those that achieved 150 min MVPA (Finlayson et al., 2011, Stanish and Draheim, 2005).
Between 0 and 46% achieved 150 min MVPA, while 7–45% took ≥ 10,000 steps/day with an average of 6851 steps/day (range 5308 to 9632). Overall, the number of participants that achieved the equivalent of 150 min MVPA or ≥ 10,000 steps/day was 9% (weighted average) with a range of 0–46%. For larger studies (those that included 50 participants or more) this range drops to 0–27%.
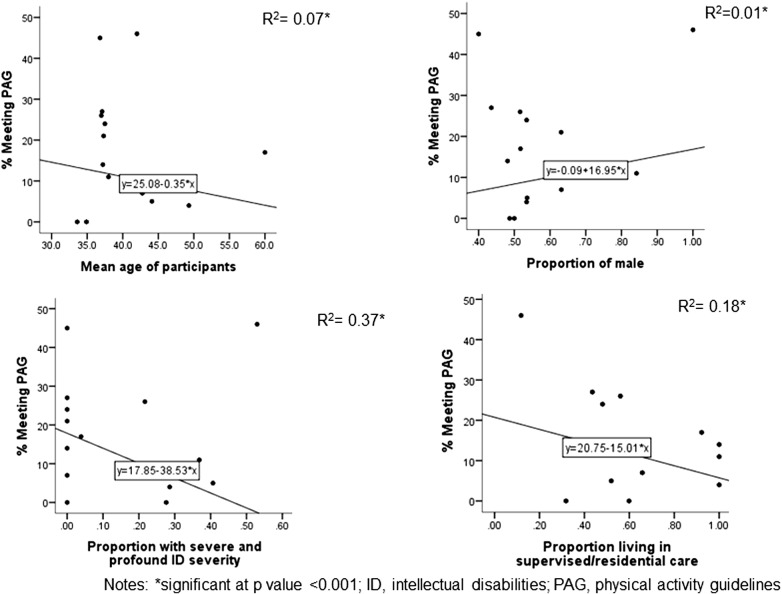
3.3. Factors influencing PA levels in awID
A multiple linear regression analysis revealed a significant linear relationship between the percentage of participants meeting PAG and the independent/predictor variables of age, sex, residence, and ID severity. The regression model was highly significant [F (4, 2994) = 941.17, p < 0.001] with an Adjusted R2 of 0.56 (Table 4). On average the percentage of participants predicted to achieve PAG was estimated to be = 0.063–0.169 (living in care) + 0.001 (age) + 0.368 (sex) − 0.385 (ID severity); where living in care was coded as the proportion of participants living in supervised or residential care, age was measured in years (mean age from each study), sex was coded as the proportion of male, and high ID severity was coded as the proportion of participants with severe and profound ID.
These results showed that generally 56% of the total variability in the percentage of people meeting PAG was explained by the predictor variables; age, sex, proportion of people with severe and profound ID, and the proportion of people living in supervised or residential care. The analysis shows that among all predictive variables, the strongest predictor is the proportion of participants with severe and profound ID with a Beta of 0.631 (t(4) = 49.934, p < 0.001). Therefore, a 1% increase in the proportion of participants with severe and profound ID had a relative contribution of approximately 0.63% of the dependent variable when all the other factors were controlled for. On the other hand, age had the weakest contribution to the regression equation with a Beta 0.101 (t(4) = 6.354, p < 0.001). These results were consistent with the linear regression performed on individual relationships between predictor variables and percentage of awID who met PAG.
The linear regression showed a significant linear relationship between the percentage of participants meeting PAG and each of the predictor variables; age, sex, residence, and ID severity. Each of the regression equation was significant as shown in Fig. 2. All the relationships were also significant, p < 0.001 (Fig. 2).
Fig. 2.
Summary of linear regression analysis for the variables predicting the percentage of participants that met PAG (n = 2999).
4. Discussion and conclusions
4.1. Discussion
We observed that only 9% of the participants in the studies achieved an equivalent of the global PAG of 150 min MVPA. This number that achieved PAG ranged from 0–46%, with two of the studies reporting 0% (Frey, 2004, Phillips and Holland, 2011). ID severity, living in care, gender, and age were independently significantly correlated to the number of participants achieving minimum PAG; the strongest predictor being ID severity. Overall, awID were not as active as the general population. Given our findings that only 9% of the participants met PAG, this means that 91% of the participants were not sufficiently active. In 2010, WHO defined insufficient PA as not performing at least 150 min of moderate-intensity PA per week (or equivalent), and they estimated that globally, 23% of adults aged 18 + years were insufficiently active (men 20% and women 27%), and older adults were less active than younger adults. Clearly, the percentage of inactive participants in our review is higher than the global healthy population, despite the fact that the participants in our review are relatively young adults with an approximate mean (weighted) age of 46 years. Interestingly, for those participants with number of steps/week recorded, they took an average of 6851 steps/day. Although this number of steps/week is within the range of the general adult population, it falls within older adult range, the lower end of the range. A meta-analysis by Bohannon (Bohannon, 2007) estimated daily adults steps to be within a range of 3766 to 18,425 steps/day, these were greater in subjects younger than 65 years of age (216–10,377) compared with subjects 65 years of age or older (897–8233).
A review by Temple et al. (2006) found that 18–45% of awID met the health promotion recommendation of 30-mins of moderate intensity PA a day or accrued ≥ 10,000 steps/day. That range is narrower compared to the 0–46% found in this review. This might be because, as well as methodological differences, most countries had revised their PAG with current guidelines considering continuous bouts of PA as well as overall duration and frequencies of PA/week. Allowing for continuous bouts of PA is likely to reduce the number of participants who are judged to be active.
It is difficult generalising PA levels of the participants in this review to the whole ID population for several reasons. It is likely that they were more active than the general ID population as the data in this review was informed by a sample that was selective and did not appear to represent the ID population as a whole. Only 99 out of the 3159 participants were reported as having profound ID with most of them classified as having mild to moderate ID severity. The inclusion criteria also meant that only the very active part of the mild to moderate ID was included. For example, most of the studies excluded people who required walking aids and although there is no available statistics on the number of pwID requiring walking aids, motor impairment is very common among this group of people (Harris, 2006, Pratt and Greydanus, 2007). This selectivity in sampling was also evident in the fact that nearly half of the participants were reported to be in employment and four of the six studies that reported employment history had more people in work than out of work (Table 2), which is in stark contrast to 6.4% of the ID population reported to be in paid employment (Health and Social Care Information Centre, 2011).
However, there is a chance that the number of participants meeting PAG was underestimated as all of the studies that used number of steps criteria used ≥ 10,000 steps/day. Tudor-Locke et al. (2011)) found that 150 min MVPA translated to approximately 7000 steps/day. Consequently, participants who took less than 10,000 but > 7000 steps/day who may have been deemed inactive would have achieved 150 min of MVPA, and so increasing the number meeting PAG. In spite of this, it is more likely that the data from this review is an upward estimate of PA levels within the ID population because of the relatively low number of participants with severe to profound ID severity, and the stringent inclusion criteria.
4.1.1. Predictors of PA levels
The results from the meta-analysis show that higher ID severity, living in supervised/residential care, and older age were independently negatively correlated to the number of participants achieving PAG, while proportion of male was positively correlated. These correlations were not always evidenced by the individual studies, and in some instances the studies reported conflicting results. For example, Finlayson et al. (2009) and Hilgenkamp et al. (2012) found that male participants were more active than females, whereas Stanish (2004) reported the opposite. The latter study was small, consisting of only 20 participants who were all in the mild range of ID severity and were younger compared to the other two studies, both of which were of better quality as evidenced by their higher quality scores.
When all the predictive factors were considered, the strongest indicator of PA level is the level of ID severity. The higher the proportion of people with severe and profound ID, the lower the number of participants achieving PAG. This finding is important as approximately a quarter (27%) of the sample in this review had severe to profound ID. People with severe or profound ID are characterised among other things by limited motor functioning (Harris, 2006, Pratt and Greydanus, 2007). This is likely to make PA more difficult than in people with mild to moderate range of ID severity.
Although age on its own had a negative correlation with PA level, when combined with the other predictor variables in a multiple linear regression, the correlation becomes a positive one, albeit with a very small coefficient of 0.001. This is probably because mean age was used with a relatively narrow range of 33.6 to 59.7 years and without the Hilgenkamp, et al. study (Hilgenkamp et al., 2012), which was primarily in older adults (age range 50–81), this range narrows even further to 33.6 to 49.3 years. Another possible reason could have been a multicollinearity effect, however, the multicollinearity test was non-significant for the predictor variables.
4.1.2. Implications for future research
The objective PA measures used in this study have been shown to be practicable within ID population, but only on participants who are mild to severely disabled, and they are yet to be used on individuals with profound ID severity. Future studies could examine the feasibility/practicability of using motion sensors such as accelerometers or pedometers in individuals with profound ID. Additionally, future PA research in this population should consider issues of validity and reliability when using subjective PA measures as they may be more applicable in large scale population studies. Matthews et al. (2011) argue that less resource intensive methods are required for large-scale surveillance. In the general population, the IPAQ (Craig et al., 2003) is commonly used for surveillance studies worldwide and some studies (Phillips and Holland, 2011, McKeon et al., 2013, Matthews et al., 2011) have used it as a PA measure within the ID population, but its validation studies are inconsistent. Matthews et al. (2011) found that as PA increased above 10 min/day, the agreement between accelerometer and IPAQ decreases, while McKeon et al. (2013) reported equivalent results from PA levels obtained from accelerometer and IPAQ. These inconsistencies indicate the need for more research in this area.
Unlike the objective measures that have been demonstrated to be valid among awID with mild to moderate ID severity (McKeon et al., 2013, Stanish, 2004), none of the subjective methods used in this review have been validated in pwID with the exception of IPAQ. Therefore, further research is required to validate these instruments across individuals with different ID severity levels, especially in those with profound ID.
Finally, apart from the data quality, the scope of PA data would need to be improved and widened so that comparison with the general population is possible in terms of different age groups, ID severity (mild, moderate, severe, profound), ethnicity, presence or absence of co-morbidities, and presence of CVD risk factors.
4.2. Limitations
4.2.1. Risk of bias
Due to time and resource constrictions, only peer reviewed articles published in the English language were included in this review. Although the search strategy did not return any articles published in other languages or unpublished thesis, it is possible that the search filters applied may have excluded such articles. Likewise, no attempt was made to locate unpublished studies, therefore we cannot rule out publication bias.
4.2.2. Quality of identified research
Intervention studies in awID were excluded. While this reduced the PA data included, the exclusion was applied so as to limit potential selection bias from intervention studies due to more stringent inclusion criteria.
4.2.3. Reporting bias
Further limitations of this review arise from the included studies' methodological differences, namely sampling method, inclusion criteria, differences in PA measuring instruments, and outcome measures (inconsistencies in the PAG used by different researchers and how they were used). All these factors hampered synthesis of results, made comparisons between studies difficult and also made it difficult to make full use of the extracted data. Meta-analysis was only possible using a simple linear regression as there were insufficient data values for meta-regression and one study was excluded from the meta-analysis due to insufficient data. Also, subgroup analysis was impossible as there were insufficient data for different age groups, ID severity, and the presence of CVD risk factors such as overweight, cholesterol, and hypertension. This limited any further comparison with the general population.
4.3. Conclusion
This review has established that awID are incredibly inactive, and that even in those who are active, their PA is only comparable to lesser active people in the general population. It also shows that objective measures of PA have been used successfully within the ID population, but mostly in those with mild to moderate ID severity, and while subjective measures have been used across all ID severity levels, they were likely to not be validated. Lastly, the results indicated that ID severity, living in care, gender, and age were independently significantly correlated with the number of participants achieving minimum PAG, the strongest predictor being ID severity (Beta 0.631, p < 0.001). These findings highlight a crucial need to increase PA in this population. To inform measurement and intervention design for improved PA, we recommend that there is an urgent need for future PA studies in awID population to include all ID severity levels including those with severe and profound ID severity. Such research should include information to enable subgroup analysis in particular across different ages, sex, ID severity, and CVD risk factors in order to inform risk factor identification for low PA and develop more targeted PA promotion within ID populations.
Conflict of interest
None.
Transparency Document
Transparency Document.
Acknowledgments
This systematic review was conducted as part of Dairo's PhD, part-funded by Oxford Brookes University; Collett is funded by Health Education Thames Valley, and Dawes is funded by the Elizabeth Casson Trust.
Footnotes
Intellectual disabilities (ID).
People with intellectual disabilities (pwID).
Physical activity (PA).
Adults with intellectual disabilities (awID)
Physical activity guidelines (PAG).
150 min of moderate to vigorous physical activity/week (150 min MVPA).
International Physical Activity Questionnaire (IPAQ).
The Transparency Document associated with this article can be found, in online version.
Supplementary data to this article can be found online at http://dx.doi.org/10.1016/j.pmedr.2016.06.008.
Contributor Information
Yetunde Marion Dairo, Email: yetunde.dairo-2014@brookes.ac.uk.
Johnny Collett, Email: jcollett@brookes.ac.uk.
Helen Dawes, Email: hdawes@brookes.ac.uk.
G. Reza Oskrochi, Email: roskrochi@brookes.ac.uk.
Appendix A. Supplementary data
Search history.
Updated search history.
References
- American Psychiatric Association aww . fifth ed. American Psychiatric Publishing; Washington, D.C.: 2013. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. [Google Scholar]
- Australian Government Department of Health . 2014. Australia's Physical Activity and Sedentary Behaviour Guidelines. (Available from: http://www.health.gov.au/internet/main/publishing.nsf/content/health-pubhlth-strateg-phys-act-guidelines#apaadult) [Google Scholar]
- Barnes T.L., Howie E.K., McDermott S., Mann J.R. Physical activity in a large sample of adults with intellectual disabilities. J. Phys. Act. Health. 2013;10(7):1048–1056. doi: 10.1123/jpah.10.7.1048. [DOI] [PubMed] [Google Scholar]
- Bellet R.N., Adams L., Morris N.R. The 6- minute walk test in outpatient cardiac rehabilitation: validity, reliability and responsiveness—a systematic review. Physiotherapy. 2012;98(4):277–287. doi: 10.1016/j.physio.2011.11.003. [DOI] [PubMed] [Google Scholar]
- Bergstrom H., Hagstromer M., Hogberg J., Elinder L.S. A multi-component universal intervention to improve diet and physical activity among adults with intellectual disabilities in community residences: a cluster randomised controlled trial. Res. Dev. Disabil. 2013;34(11):3847–3857. doi: 10.1016/j.ridd.2013.07.019. [DOI] [PubMed] [Google Scholar]
- Bohannon R.W. Number of pedometer- assessed steps taken per day by adults: a descriptive meta-analysis. Phys. Ther. 2007;87(12):1642. doi: 10.2522/ptj.20060037. [DOI] [PubMed] [Google Scholar]
- Caspersen C.J., Powell K.E., Christenson G.M. Physical activity, exercise,and physical fitness:definitions and distinctionsfor health-related research. Public Health Rep. 1985;100(2 127):126–131. [PMC free article] [PubMed] [Google Scholar]
- Chief Medical Officer C . Department of Health; 2011. Start Active, Stay Active: A Report on Physical Activity for Health From the Four Home Countries. [Google Scholar]
- Cohen J. A coefficient of agreement for nominal scales. Educ. Psychol. Meas. 1960;20:37–46. [Google Scholar]
- Craig C.L., Marshall A.L., Sjostrom M. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003;35(8):1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- Dixon-Ibarra A., Lee M., Dugala A. Physical activity and sedentary behavior in older adults with intellectual disabilities: a comparative study. Adapt. Phys. Act. Q. 2013;30(1):1–19. doi: 10.1123/apaq.30.1.1. [DOI] [PubMed] [Google Scholar]
- Doran C.M., Einfeld S.L., Madden R.H. How much does intellectual disability really cost? First estimates for Australia. J. Intellect. Develop. Disabil. 2012;37(1):42–49. doi: 10.3109/13668250.2011.648609. [DOI] [PubMed] [Google Scholar]
- Downs S.H., Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J. Epidemiol. Community Health. 1998;52(6):377. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Draheim C.C., Williams D.P., McCubbin J.A. Prevalence of physical inactivity and recommended physical activity in community-based adults with mental retardation. Ment. Retard. 2002;40(6):436–444. doi: 10.1352/0047-6765(2002)040<0436:POPIAR>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Emerson E. Underweight, obesity and exercise among adults with intellectual disabilities in supported accommodation in Northern England. J. Intellect. Disabil. Res. 2005;49(Part 2):134–143. doi: 10.1111/j.1365-2788.2004.00617.x. [DOI] [PubMed] [Google Scholar]
- Emerson E., Baines S. Health inequalities and people with learning disabilities in the UK. Tizard Learn. Disabil. Rev. 2011;16(1):42. [Google Scholar]
- Emerson E., Glover G., Hatton C., Wolstenholme J. Trends in age-standardised mortality rates and life expectancy of people with learning disabilities in Sheffield over a 33-year period. Tizard Learn. Disabil. Rev. 2014;19(2):90–95. [Google Scholar]
- Finlayson J., Jackson A., Cooper S.-A. Understanding predictors of low physical activity in adults with intellectual disabilities. J. Appl. Res. Intellect. Disabil. 2009;22(3):236–247. [Google Scholar]
- Finlayson J., Turner A., Granat M.H. Measuring the actual levels and patterns of physical activity/inactivity of adults with intellectual disabilities. J. Appl. Res. Intellect. Disabil. 2011;6:508–517. [Google Scholar]
- Frey G.C. Comparison of physical activity levels between adults with and without mental retardation. J. Phys. Act. Health. 2004;1(3):235–245. [Google Scholar]
- Hallal P.C., Andersen L.B., Bull F.C., Guthold R., Haskell W., Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380(9838):247–257. doi: 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]
- Harris J.C. Oxford University Press; New York: 2006. Understanding its Development, Causes, Classification, Evaluation, and Treatment. [Google Scholar]
- Haveman M., Perry J., Salvador-Carulla L. Ageing and health status in adults with intellectual disabilities: results of the European POMONA II study. J. Intellect. Develop. Disabil. 2011;36(1):49–60. doi: 10.3109/13668250.2010.549464. [DOI] [PubMed] [Google Scholar]
- Hawkins A., Look R. Levels of engagement and barriers to physical activity in a population of adults with learning disabilities. Br. J. Learn. Disabil. 2006;34(4):220–226. [Google Scholar]
- Health and Social Care Information Centre . 2011. Social Care and Mental Health Indicators From the National Indicator Set. (Available from: https://data.gov.uk/dataset/social-care-and-mental-health-indicators-from-the-national-indicator-set) [Google Scholar]
- Heslop P., Blair P.S., Fleming P., Hoghton M., Marriott A., Russ L. The confidential inquiry into premature deaths of people with intellectual disabilities in the UK: a population-based study. Lancet. 2014;383(9920):889–895. doi: 10.1016/S0140-6736(13)62026-7. [DOI] [PubMed] [Google Scholar]
- Hilgenkamp T.I.M., Reis D., van Wijck R., Evenhuis H.M. Physical activity levels in older adults with intellectual disabilities are extremely low. Res. Dev. Disabil. 2012;33(2):477–483. doi: 10.1016/j.ridd.2011.10.011. [DOI] [PubMed] [Google Scholar]
- Holland A. Ageing and learning disability. Br. J. Psychiatry. 2000;176:26–31. doi: 10.1192/bjp.176.1.26. [DOI] [PubMed] [Google Scholar]
- Honeycutt A., Dunlap L., Chen H., al Homsi G., Grosse S. 2004. Economic Costs Associated With Mental Retardation, Cerebral Palsy, Hearing Loss, and Vision Impairment—United States, 2003; p. 57. [PubMed] [Google Scholar]
- Katz G., Lazcano-ponce E. Intellectual disability: definition, etiological factors, classification, diagnosis, treatment and prognosis. Salud Publica Mex. 2008;50 doi: 10.1590/s0036-36342008000800005. [DOI] [PubMed] [Google Scholar]
- Krahn G.L., Hammond L., Turner A. A cascade of disparities: health and health care access for people with intellectual disabilities. Ment. Retard. Dev. Disabil. Res. Rev. 2006;1:70–82. doi: 10.1002/mrdd.20098. [DOI] [PubMed] [Google Scholar]
- Lifestyles statistics team HaSCIC . 2014. Statistics on Obesity, Physical Activity and Diet: England. (Report No.: Contract No., http://www.hscic.gov.uk/catalogue/PUB13648/Obes-phys-acti-diet-eng-2014-rep.pdf) [Google Scholar]
- Lin P.-Y., Lin L.-P., Lin J.-D. Hypertension, hyperglycemia, and hyperlipemia among adolescents with intellectual disabilities. Res. Dev. Disabil. 2010;31(2):545–550. doi: 10.1016/j.ridd.2009.12.002. [DOI] [PubMed] [Google Scholar]
- Matthews L., Hankey C., Penpraze V. Agreement of accelerometer and a physical activity questionnaire in adults with intellectual disabilities. Prev. Med. 2011;52(5):361–364. doi: 10.1016/j.ypmed.2011.02.001. [DOI] [PubMed] [Google Scholar]
- Maulik PK, Harbour CK. Epidemiology of intellectual disability. In J. H. Stone & M. Blouin (Eds.) In: International Encyclopedia of Rehabilitation. Buffalo, Exchange. CfIRRIa, editors. 2010.
- Maulik P.K., Mascarenhas M.N., Mathers C.D., Dua T., Saxena S. Prevalence of intellectual disability: a meta-analysis of population-based studies. Res. Dev. Disabil. 2011;32(2):419–436. doi: 10.1016/j.ridd.2010.12.018. [DOI] [PubMed] [Google Scholar]
- McGuire B.E., Daly P., Smyth F. Lifestyle and health behaviours of adults with an intellectual disability. J. Intellect. Disabil. Res. 2007;51(7):497–510. doi: 10.1111/j.1365-2788.2006.00915.x. [DOI] [PubMed] [Google Scholar]
- McKeon M., Slevin E., Taggart L. A pilot survey of physical activity in men with an intellectual disability. J. Intellect. Disabil. 2013;17(2):157–167. doi: 10.1177/1744629513484666. [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann. Intern. Med. 2009;151(4):264. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- Peterson J.J., Janz K.F., Lowe J.B. Physical activity among adults with intellectual disabilities living in community settings. Prev. Med. 2008;47(1):101–106. doi: 10.1016/j.ypmed.2008.01.007. [DOI] [PubMed] [Google Scholar]
- Phillips A.C., Holland A.J. Assessment of objectively measured physical activity levels in individuals with intellectual disabilities with and without Down's syndrome. PLoS One. 2011;6(12) doi: 10.1371/journal.pone.0028618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pratt H.D., Greydanus D.E. Intellectual disability (mental retardation) in children and adolescents. Prim. Care. 2007;34(2):375–386. doi: 10.1016/j.pop.2007.04.010. [DOI] [PubMed] [Google Scholar]
- Richards J., Hillsdon M., Thorogood M., Foster C. Face-to-face interventions for promoting physical activity. Cochrane Database Syst. Rev. 2013;9 doi: 10.1002/14651858.CD010395.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson J., Emerson E., Gregory N. Lifestyle related risk factors for poor health in residential settings for people with intellectual disabilities. Res. Dev. Disabil. 2000;21(6):469–486. doi: 10.1016/s0891-4222(00)00053-6. [DOI] [PubMed] [Google Scholar]
- Salvador-Carulla L., Reed G.M., Vaez-Azizi L.M. Intellectual developmental disorders: towards a new name, definition and framework for “mental retardation/intellectual disability” in ICD-11. World Psychiatry. 2011;10(3):175. doi: 10.1002/j.2051-5545.2011.tb00045.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanish H.I. Accuracy of pedometers and walking activity in adults with mental retardation. Adapt. Phys. Act. Q. 2004;21(2):167–179. [Google Scholar]
- Stanish H.I., Draheim C.C. Assessment of walking activity using a pedometer and survey in adults with mental retardation. Adapt. Phys. Act. Q. 2005;22(2):136–145. [Google Scholar]
- Strath S.J., Kaminsky L.A., Ainsworth B.E. Guide to the assessment of physical activity: clinical and research applications: a scientific statement from the American Heart Association. (AHA scientific statement) (report) Circulation. 2013;128(20):2259–2279. doi: 10.1161/01.cir.0000435708.67487.da. [DOI] [PubMed] [Google Scholar]
- Temple V.A. Barriers, enjoyment, and preference for physical activity among adults with intellectual disability. Int. J. Rehabil. Res. 2007;30(4):281–287. doi: 10.1097/MRR.0b013e3282f144fb. [DOI] [PubMed] [Google Scholar]
- Temple V.A., Frey G.C., Stanish H.I. Physical activity of adults with mental retardation: review and research needs. Am. J. Health Promot. 2006;21(1):2–12. doi: 10.1177/089011710602100103. [DOI] [PubMed] [Google Scholar]
- The Office of Disease Prevention and Health Promotion . 2008. Physical Activity Guidelines for Americans Summary. (Available from: http://health.gov/paguidelines/guidelines/summary.aspx) [Google Scholar]
- Tudor-Locke C., Hatano Y., Pangrazi R.P., Kang M. Revisiting “how many steps are enough?”. Med. Sci. Sports Exerc. 2008;40(7 Suppl.):S537–S543. doi: 10.1249/MSS.0b013e31817c7133. [DOI] [PubMed] [Google Scholar]
- Tudor-Locke C., Leonardi C., Johnson W.D., Katzmarzyk P.T., Church T.S. Accelerometer steps/day translation of moderate-to-vigorous activity. Prev. Med. 2011;53(1):31–33. doi: 10.1016/j.ypmed.2011.01.014. [DOI] [PubMed] [Google Scholar]
- Wallén E.F., Müllersdorf M., Christensson K., Malm G., Ekblom O., Marcus C. High prevalence of cardio-metabolic risk factors among adolescents with intellectual disability. Acta Paediatr. (Oslo, Norway: 1992) 2009;98(5):853–859. doi: 10.1111/j.1651-2227.2008.01197.x. [DOI] [PubMed] [Google Scholar]
- World Health Organisation . 2011. Global Recommendations on Physical Activity for Health Online. (Available from: http://www.who.int/dietphysicalactivity/publications/recommendations18_64yearsold/en/Available from: http://www.who.int/dietphysicalactivity/factsheet_olderadults/en/) [Google Scholar]
- World Health Organisation . 2015. W. Health Topics Online. (Available from: http://www.euro.who.int/en/health-topics/noncommunicable-diseases/mental-health/news/news/2010/15/childrens-right-to-family-life/definition-intellectual-disability.) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transparency Document.
Search history.
Updated search history.