Abstract
Living in a low socioeconomic status (SES) area is associated with an increased risk of cardiovascular events and all-cause mortality. Previous studies have suggested a socioeconomic gradient in daily physical activity (PA), but have mainly relied on self-reported data, and individual rather than residential area SES. This study aimed to investigate the relationships between residential area SES, PA pattern, compliance with PA-recommendations and fitness in a Swedish middle-aged population, using objective measurements. We included 948 individuals from the SCAPIS pilot study (Gothenburg, Sweden, 2012, stratified for SES, 49% women, median age: 58 years), in three low and three high SES districts. Accelerometer data were summarized into intensity-specific categories: sedentary (SED), low (LIPA), and medium-to-vigorous PA (MVPA). Fitness was estimated by submaximal ergometer testing. Participants of low SES areas had a more adverse cardiovascular disease risk factor profile (smoking: 20% vs. 6%; diabetes: 9% vs. 3%; hypertension: 38% vs. 25%; obesity: 31% vs. 13%), and less frequently reached 150 min of MVPA per week (67% vs. 77%, odds ratio [OR] = 0.61; 95% confidence interval [95% CI] = 0.46–0.82), from 10-minute bouts (19% vs. 31%, OR = 0.53, 95% CI = 0.39–0.72). Individuals in low SES areas showed lower PA levels (mean cpm: 320 vs. 348) and daily average MVPA (29.9 vs. 35.5 min), and 12% lower fitness (25.1 vs. 28.5 mL × min− 1 × kg− 1) than did those in high SES areas. Reduced PA and fitness levels may contribute to social inequalities in health, and should be a target for improved public health in low SES areas.
Keywords: Motor activity, Physical fitness, Social class
Highlights
-
•
We studied physical activity pattern and fitness between socioeconomic (SES) areas.
-
•
Low SES residents showed lower mean physical activity levels and 12% lower fitness.
-
•
Rates of adherence to physical activity guidelines were lower in low SES areas.
1. Introduction
Socioeconomic status (SES) refers to classification of an individual's position in society, usually assessed as education, income and/or occupation (Galobardes et al., 2006). Low SES is associated with a higher burden of cardiovascular disease (CVD) and all-cause mortality for the individual, as well as on a residential area level (Mackenbach et al., 2000, Meijer et al., 2012, Rosengren et al., 2009, Schaufelberger and Rosengren, 2007, Bergstrom et al., 2015a, Rawshani et al., 2015). Low SES is also associated with worse prognosis after manifestation of CVD (Bergstrom et al., 2015a). Although low SES is known to be associated with adverse CVD risk factors, such as smoking, hypertension, and hyperlipidemia, as well as health-associated behaviors (Manhem et al., 2000, Kanjilal et al., 2006), these factors only provide a partial explanation for discrepancies in SES with respect to CVD (Marmot et al., 1997, Laaksonen et al., 2008). Psychosocial factors have also been suggested as potential mediators (Marmot et al., 1997). The unexplained difference in morbidity and mortality in relation to SES needs to be further investigated.
The city of Gothenburg is socially segregated, with a clear geographical distinction between socioeconomic groups. There are also differences in prevalence and all-cause mortality of CVD between areas of high and low SES (Inequalities in Health and Living Conditions in Gothenburg: Interim Report, 2014). Area-level SES provides information of the habitants, as well as its history, class, accumulation of capital and other aspects shaping health. Therefore, relevant information regarding the social and health status of the investigated population may be lost when only investigating individual characteristics (Galobardes et al., 2007). Additionally, studying health effects at an area level is relevant for policy making having a potential effect on neighborhood health (Sugiyama et al., 2015).
Daily physical activity (PA) and cardiorespiratory fitness (CRF) have widely documented cardioprotective effects (Lee and et al., 2012, Blair et al., 1989). There is rising concern that sedentary behavior in itself may contribute to CVD independently of PA levels (Dunstan et al., 2012) or fitness. Direct measurement of absolute intensity of PA allows for detailed assessment of individual PA patterns. This can be defined as time spent in different activity levels, varying from sedentary behavior (SED) to light intensity PA (LIPA) and PA of moderate-to-vigorous intensity (MVPA).
Current national/international PA guidelines typically recommend at least 150 min/week of MVPA, spent in prolonged bouts of 10 min or longer, preferably on most days of the week (Haskell et al., 2007, The Swedish National Board of Health and Welfare, 2011). Previous studies that used objective measurements of PA have shown generally low rates of adherence to the current PA guidelines (Hagstromer et al., 2007). The daily movement pattern and fulfillment of national PA recommendations in Swedish men and women aged 50–65 years have previously been described (Ekblom-Bak et al., 2015). There are higher levels of MVPA and sedentary time in individuals with a higher education. However, the relationships between area-level SES, daily PA, fitness, and fulfillment of national PA recommendations have not been examined. Area-level SES is associated with objective and perceived environmental attributes known to correlate with physical activity, such as neighborhood density, esthetics, and fear of crime (Sugiyama et al., 2015). Therefore, area-level SES may influence physical activity independently of individual SES. This study aimed to investigate the relationships of area-level SES with PA patterns, CRF, and adherence to national physical activity guidelines in a middle-aged Gothenburg population.
2. Methods
2.1. Study population
The study population for this investigation originated from the Swedish CArdioPulmonary bioImage Study (SCAPIS) pilot trial, which was conducted at the Sahlgrenska University Hospital in Gothenburg, Sweden in 2012 (Bergstrom et al., 2015b). A total of 2243 middle-aged individuals (50–65 years) were selected from the Swedish population registries and stratified for socioeconomic area. Participation rates were significantly different (37.1% in low vs. 67.2% in high SES areas). A total of 1111 individuals agreed to participate. The extensive study procedures occurred during 2 or 3 days and included measurement of blood chemistry, anthropometry, electrocardiogram, blood pressure, and lung function testing, as well as imaging studies. To estimate daily PA and fitness, participants wore an accelerometer during 7 consecutive days and performed a submaximal bicycle test. All of the participants provided written informed consent. The study was approved by the Ethics Committee of the University of Umeå (Dnr 2010-228-31M).
2.2. Socioeconomic status
The known geographical disparities in the Gothenburg region, described above, enabled assessment of SES by residential area. Participants from the north-eastern residential areas were classified as having low SES, while residents of the western areas were classified as having high SES. Information regarding education level was also collected to control for individual-level SES. Education level was divided into four categories: (1) no basic education, (2) completed primary school, (3) completed secondary education, and (4) university degree or higher.
2.3. Physical activity
PA data were collected using the ActiGraph model GT3X/GT3X + accelerometer (Actigraph LCC, Pensacola, FL, USA). This small device measures acceleration, thereby providing continuous data of PA intensity and frequency, which is summarized into units called counts. The accelerometer is carried in an elastic belt over the right hip. Study participants were instructed to wear this device during waking hours for 7 consecutive days from the first study visit, the only exception being water-based activities. After completion, the accelerometer was returned to the laboratory by prepaid mail. The accelerometer was initialized and downloaded using ActiLife v.6.10.1 software. Raw data sampling frequency was set to 30 Hz, and extracted as 60-s epochs with a low frequency extension filter for the present analyses. Uniaxial data were analyzed.
Of the 1111 participants, 1067 (96%) agreed to wear the accelerometer and 948 (85.3%) showed valid data of at least 600 min of recording for at least 4 days (Trost et al., 2005). The majority (67%) showed valid data for the entire 7-day period, 19% had data for 6 days, 9% for 5 days, and 5% for 4 days. Accelerometer data are shown as average time per day spent in intensity-specific categories (SED, LIPA, and MVPA), using mean counts per minute (cpm) as a mean value of activity over the entire studied period, and as the degree of fulfillment of current PA recommendations. Wear time was defined as the non-wear time subtracted from 24 h. Non-wear time was defined as 0 cpm for more than 60 min, while allowing a maximum of 2 min between 0 and 100 (Troiano et al., 2008). With regard to intensity, cpm < 100 was defined as being in SED (Matthews et al., 2008), between 100 and 2019 cpm as LIPA, and > 2019 cpm as MVPA (Troiano et al., 2008). Mean cpm is a measure of total PA, which was calculated by dividing the total number of counts registered by total wear time.
To better understand to which extent Swedish national PA recommendations are actually met, analyses were performed with variation in strictness of interpretation as follows: (1) accumulating at least 150 min/week; (2) accumulating at least 150 min/week from prolonged bouts of 10 min or more; (3) accumulating at least 30 min/day on at least 5 days of the week; and (4) accumulating at least 30 min/day on at least 5 days of the week, all from bouts of 10 min or more.
2.4. Cardiorespiratory fitness
All of the participants were invited to undertake a submaximal ergometer test. CRF (VO2max, expressed as mL·min− 1·kg− 1) was estimated by the Åstrand method (Astrand, 1953, Astrand and Ryhming, 1954), which is based on a linear relationship between heart rate and oxygen consumption with workload. Measurement of heart rate at a sub-maximal work rate, usually 60–70%, allowed for estimation of maximal oxygen uptake. A total of 592 participants had valid tests. Participants with a diagnosed heart condition or taking beta-adrenergic blockers constituted a majority of excluded participants, other reasons for non-participation included pain (hips, back, knees), obesity and perceived inability to perform the test.
2.5. Other measurements
Anthropometrics, including weight, height, waist, and hip circumference, were measured at the first study visit. Body mass index (BMI) was calculated (body weight / height squared) and stratified into groups: (1) underweight (BMI < 20); (2) normal weight (BMI ≥ 20 and < 25); (3) overweight (BMI ≥ 25 and < 30); and (4) obese (BMI ≥ 30). The waist-hip-ratio (WHR) was calculated and classified as high or low according to current WHO guidelines, with > 0.90 for men and > 0.85 for women classified as high (Nishida et al., 2010). A comprehensive questionnaire was administered to collect data regarding self-reported health, and environmental and psychosocial factors. Self-reported active smoking, diabetes, and chronic obstructive pulmonary disease/asthma diagnosis were dichotomized. Measurements of brachial blood pressure and samples for blood chemistry were also collected.
2.6. Statistical analysis
Data were tested for normality using the Shapiro–Wilk test. Because most variables were skewed, descriptive data are shown untransformed as median and interquartile range (Q1–Q3). We used multiple regression models to estimate the associations of our main outcomes and SES areas, independently of sex, age, and educational level, and their interactions. For intensity-specific PA, MVPA, and PA recommendation outcomes we used linear, Poisson, and logistic regression, respectively. In the linear regression model, the outcome (intensity-specific PA) was logarithmically transformed. Model coefficients and their 95% confidence intervals (95% CIs) are presented. Variables that were included in the models were checked for collinearity. The level of significance was set at p ≤ 0.05. All statistical computations were made using SAS 9.4 TS Level 1M0.
3. Results
A total of 947 subjects were included in the analyses (women, 51%). The median age was 58 years (54–62 years). A total of 69% of participants were overweight or obese (63% in the high SES group vs. 74% in the low SES group). Notably, the largest difference in proportion of BMI was observed in the obese group (BMI > 30), with 31% in the low SES group versus 13% in the high SES group. A total of 77% of participants were classified as having a high WHR, while 13% reported regular smoking and 6% reported having diabetes in the total study group. The majority of the population reported complete upper secondary school as their highest education (44%), with marked differences between SES strata (Table 1).
Table 1.
Characteristics of the study population regarding SES. Data are shown as the median (Q1–Q3) (Gothenburg, Sweden, 2012).
| SES |
All n = 1111 |
||
|---|---|---|---|
| High n = 559 |
Low n = 552 |
||
| Age | 57.0 (54.0–62.0) | 58.0 (54.0–62.0) | 58.0 (54.0–62.0) |
| BMI | 25.9 (23.8–28.3) | 28.0 (24.9–31.1) | 26.6 (24.3–29.5) |
| Female, % (n) | 50 (283) | 50 (273) | 50 (556) |
| Waist cm | 94.0 (84.0–101) | 98.0 (88.0–105.0) | 96.0 (86.0–103.0) |
| SBP mm Hg | 120 (112–132) | 123 (115–135) | 122 (113–133) |
| DBP mm Hg | 73.0 (67.0–79.0) | 75.0 (69.5–80.8) | 74.0 (68.5–80.0) |
| WHR | 0.91 (0.86–0.96) | 0.94 (0.88–0.99) | 0.93 (0.87–0.98) |
| WHR low, % (n) | 29 (160) | 16 (91) | 23 (251) |
| WHR high, % (n) | 71 (397) | 84 (461) | 77 (858) |
| S-Cholesterol (mmol/L) | 5.80 (5.10–6.50) | 5.60 (4.90–6.40) | 5.70 (5.00–6.50) |
| S-LDL (mmol/L) | 3.80 (3.10–4.50) | 3.70 (3.10–4.40) | 3.80 (3.10–4.40) |
| BMI < 20, % (n) | 3 (18) | 2 (9) | 2 (27) |
| BMI 20–25, % (n) | 34 (188) | 24 (134) | 29 (322) |
| BMI 25–30, % (n) | 50 (278) | 43 (239) | 47 (517) |
| BMI > 30, % (n) | 13 (75) | 31 (170) | 22 (245) |
| Smoking, % (n) | 6 (35) | 20 (106) | 13 (141) |
| Diabetes diagnosis, % (n) | 3 (15) | 9 (47) | 6 (62) |
| Asthma/COPD diagnosis,% (n) | 7 (19) | 9 (29) | 8 (48) |
| Hypertension diagnosis, % (n) | 25 (140) | 38 (208) | 32 (348) |
| Education group 1 (no basic education), % (n) | 0 (2) | 5 (28) | 3 (30) |
| Education group 2 (completed primary school), % (n) | 9 (51) | 25 (134) | 17 (185) |
| Education group 3 (completed upper secondary school), % (n) | 39 (218) | 48 (262) | 44 (480) |
| Education group 4 (university degree or higher), % (n) | 52 (288) | 22 (120) | 37 (408) |
3.1. Moderate-to-vigorous intensity physical activity recommendations
The degree of fulfillment of current PA recommendations differed between SES groups (Table 2). A total of 72% of the study population achieved 150 min/week of MVPA. However, only 7% of the total population adhered to the strictest form of the guidelines (30 min/day on at least 5 days of the week, from bouts of 10 min or more). Notably, adherence was generally lower in the low SES areas. After adjustment for age, sex, and wear time, the odds ratio (OR) for comparing low SES areas to high SES areas for achieving 150 min of MVPA per week without any further requirements was 0.61 (95% CI = 0.46–0.82), although further controlling for education level abolished this relationship (OR = 0.84, CI = 0.61–1.16). The OR was slightly lower when we added the requirement of MVPA to be performed in bouts of at least 10 min (OR = 0.53, CI = 0.39–0.72). When further controlling for educational level, the OR was 0.66 (CI = 0.48–0.91). When we compared high and low SES areas and included the further requirement of 30 min of MVPA daily at least 5 days of the week, no difference between SES areas was observed (OR = 0.92, CI = 0.70–1.20), even after adjusting for age, sex, and wear time (OR = 1.04, CI = 0.77–1.34), when additionally controlling for education. Similarly, for the most restrictive demand that required 30 min/day on at least 5 days of the week in prolonged bouts of 10 min or more, no significant difference was observed between SES areas (OR = 0.62, CI = 0.37–1.04). When additionally controlling for education (OR = 0.64, CI = 0.37–1.11, Table 3).
Table 2.
Fulfillment of different interpretations of MVPA guidelines between study groups (Gothenburg, Sweden, 2012).
| SES |
All | ||
|---|---|---|---|
| High | Low | ||
| 150 min/week, % (n) | 77 (379)a, c | 67 (307)a, c | 72 (686) |
| 150 min/week, bouts of ≥ 10 min, % (n) | 31 (151)a | 19 (87)a | 25 (238) |
| 30 min/day ≥ 5 days/week, % (n) | 36 (179)b | 34 (156)b | 35 (335) |
| 30 min/day ≥ 5 days/week, in bouts ≥ 10 min, % (n) | 9 (42) | 5 (25) | 7 (67) |
| 30 min/day ≥ 5 days/week, in bouts ≥ 10 min, % (n) | 9 (42) | 5 (25) | 7 (67) |
Significant SES difference (p < 0.05).
Significant sex difference (p < 0.05).
Significant age difference (p < 0.05).
Table 3.
Multiple logistic regression for achieving different interpretations of physical activity guidelines (Gothenburg, Sweden, 2012).
| 150 min of MVPA per week | 150 min of MVPA per week, bouts of ≥ 10 min | 30 min of MVPA/day ≥ 5 days/week | 30 min of MVPA/day ≥ 5 days/week, in bouts ≥ 10 min | |
|---|---|---|---|---|
| SES, high vs. low, OR (95% CI) | 0.61 (0.46–0.82) | 0.53 (0.39–0.72) | 0.918 (0.70–1.20) | 0.62 (0.37–1.04) |
| Sex, women vs. men, OR (95% CI) | 1.32 (0.99–1.77) | 1.19 (0.89–1.60) | 1.56 (1.19–2.04) | 0.74 (0.44–1.22) |
| Age, per 1 year increase, OR (95% CI) | 1.06 (1.03–1.10) | 1.02 (0.99–1.05) | 1.02 (0.99–1.05) | 0.97 (0.92–1.03) |
| Wear time, per 1 minute increase, OR (95% CI) | 1.00 (0.99–1.00) | 1.00 (0.99–1.00) | 0.99 (0.99–1.00) | 1.00 (0.99–1.00) |
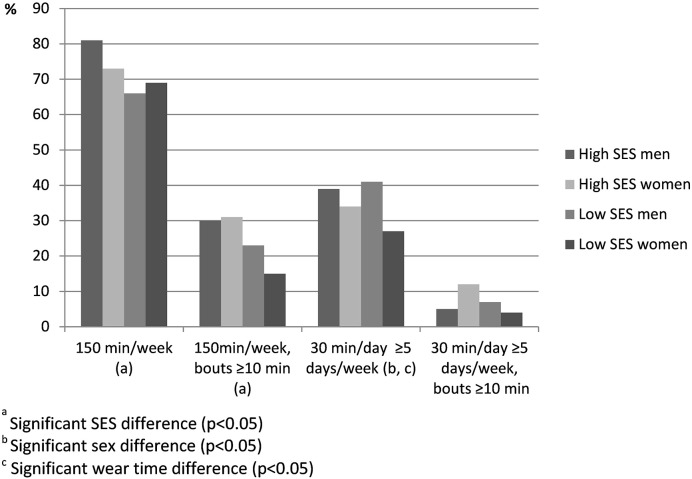
Fulfillment of PA recommendations also varied with sex, but no interaction effect was found across SES × sex (Fig. 1) for any of the levels of strictness.
Fig. 1.
Fulfillment of different interpretations of MVPA guidelines between study groups by sex (Gothenburg, Sweden, 2012).
3.2. Physical activity patterns.
The median wear time was 14.3 h per day, with a small, but significant, difference in observation time between the study groups (861 vs. 847 min for high and low SES, respectively, Table 4). A total of 60% of the wear time was spent in SED (mean, 515 min/day) and 36% was spent in LIPA (mean, 303 min/day), with no difference between the groups. The high SES group spent more time in MVPA compared with the low SES group (35 vs. 30 min/day), which was significant in the regression model when corrected for age, sex, and wear time. However, this relationship did not persist after additionally controlling for education level. There was a significant difference in levels of overall PA estimated by mean cpm (348 vs. 320), after controlling for age, sex, and wear time. Educational level had no effect on this relationship.
Table 4.
Physical activity patterns and cardiorespiratory fitness in relation to SES area. Data are shown as the median (Q1–Q3) (Gothenburg, Sweden, 2012).
| Accelerometry | SES |
All (n = 947) | |
|---|---|---|---|
| High (n = 492) | Low (n = 455) | ||
| Average wear time/day (min) | 861 (820–903)a | 847 (787–904)a | 855 (803–903) |
| Mean counts per minute (n) | 348a, c | 320a, c | 336 |
| Average MVPA/day (min) | 35.5 (22.9–49.3)a, b, c | 29.9 (18.7–45.2)a, b, c | 32.8 (19.9–48.3) |
| Average SED per day (min) | 519 (468–573)b, c, d | 507 (437–580)b, c, d | 515 (457–575) |
| Average LIPA per day (min) | 305 (256–350)b, d | 302 (249–357)b, d | 303 (253–352) |
| Cardiorespiratory fitness | (n = 338) | (n = 254) | (n = 592) |
| (mL × min− 1 × kg− 1) | 28.5 (24.1–32.7)a, c | 25.1 (21.9–29.3)a, c | 26.8 (23.0–31.3) |
Significant SES difference (p < 0.05).
Significant sex difference (p < 0.05).
Significant age difference (p < 0.05).
Significant wear time difference (p < 0.05).
3.3. Cardiorespiratory fitness
A total of 592 subjects provided valid ergometer tests (338 from the high SES group and 254 from the low SES group, Table 4). The high SES group showed 12% higher mean values of VO2max than did the low SES group (28.5 vs. 25.1 mL × min− 1 × kg− 1). These results were significant in the binominal regression model, controlling for sex, age, and active smoking (p < 0.001). When additionally controlling for education level, the effect of area-level SES persisted. Analysis showed no significance for the lowest education group (group 1), while groups 2 and 3 showed significantly lower levels of CRF compared with the highest group (4).
4. Discussion
The main findings of the present study were that living in a low SES area was associated with less daily PA and lower CRF in regression models, which were corrected for age, sex, and other potential confounders. This effect also proved largely independent of individual-level SES, which was estimated through education. This finding indicated that the correlation between area-level SES and PA may have other mediators.
The cardiovascular risk factor profile was generally poorer in subjects living in low SES areas (Table 1). Previous investigations of the current population sample showed that accelerometer-assessed PA level and CRF were correlated with metabolic syndrome, as well as its sub-components (Ekblom et al., 2015). Additionally, an inverse relationship between education and MVPA, with a linear relationship with aspects of sedentary behavior, further supports the existence of a socioeconomic gradient in PA at the individual level (Ekblom-Bak et al., 2015). These results combined with the previously known associations between SES and known cardiovascular risk factors, prevalence, and mortality in CVD (Mackenbach et al., 2000, Meijer et al., 2012, Rosengren et al., 2009, Schaufelberger and Rosengren, 2007, Bergstrom et al., 2015a, Rawshani et al., 2015, Manhem et al., 2000, Kanjilal et al., 2006), further support the idea of physical inactivity as a potential mediator.
With regard to accelerometer measurements, the study population showed generally low levels of PA and high levels of sedentary behavior, as previously described (Ekblom-Bak et al., 2015). Importantly, there were no significant differences in daily average SED or LIPA between study groups. There was a significant difference in MVPA between groups, with less MVPA in low SES areas. The same pattern was observed in mean accelerometer activity. Interestingly, while the observed difference in MVPA between study groups was attributable to a difference in education, the relationship between average accelerometer activity level and SES area was persistent, independent of educational differences. This finding indicates that the effect of area-level SES on daily PA patterns may be mediated only partly by individual SES, as assessed by education level. A possible explanation for this effect is differences in neighborhood walkability, which is a measure of the PA-promoting ability of the local environment, known to be correlated with PA regardless of area level SES (Sugiyama et al., 2015). It has also been found that low-SES area residents have less positive perceptions of their physical environment (Leslie et al., 2010). As the studied areas might differ in environmental attributes (e.g. residential density, traffic, and neighborhood esthetics) disfavoring the low-SES areas, these could be considered potential targets for future PA-promoting interventions. In summary, these findings support studies that used self-reported measurements suggesting a socioeconomic gradient in PA (Kavanagh et al., 2005, McNeill et al., 2006, Rodjer et al., 2012).
Analysis of national recommendations showed low rates of adherence in the total study population, with only 7% reaching fulfillment of the strictest category of interpretation, with no observed difference found between the study groups. For the least strict interpretations of reaching 150 min of MVPA per week, or adding accumulation of these through prolonged bouts of 10 or more minutes, a significantly higher rate of fulfillment was observed in the high SES group than in the low SES group. The effect of education on these outcomes was inconsistent, with only the least strict interpretation of the recommendations affected. Previous studies on adherence to PA recommendations showed a socioeconomic gradient on the individual level, although the majority of these used self-reported data (Marques et al., 2014, Parks et al., 2003, Carlson et al., 2010, Jones et al., 1998, Macera et al., 2005). Not all studies have shown an association between low SES and lower adherence to guidelines. In a study of 1470 Swedish adults using the short version of the IPAQ-questionnaire, subjects with a college/university degree were less likely to be classified as highly active (minimum of 1500 metabolic equivalent [MET]-minutes per week), (Bergman et al., 2008) although this relationship was significant only in men. Few studies have investigated socioeconomic aspects of PA recommendations while simultaneously using objective methods. Ekblom-Bak et al. (2015) showed a significantly lower rate of adherence for achieving 150 min of MVPA per week from prolonged bouts of 10 min or more for subjects with a lower educational level. Similar results were obtained by Scheers et al. (2013). However, this finding did not persist when adding accumulation of 30 min on most days of the week. Because the current recommendations are based on studies that used self-reported data, caution is advised for transferring these to objective measurements of PA.
CRF levels were significantly lower in the low SES group than in the high SES group and, interestingly, were not modified by differences in mean activity level, minutes of MVPA, or education level. A few studies investigated the effect of socioeconomic factors on fitness. Lakka et al. showed an inverse relationship between CRF and individual-level SES (education, income, occupation) in a population of middle aged Finnish men, using a maximal ergometer bicycle test (Lakka et al., 1996). In a sample of healthy young adults, Shishenbor et al. showed a strong relationship between low neighborhood SES and impaired VO2max, as measured through a symptom-limited graded treadmill exercise test (Shishehbor et al., 2008). Therefore, the present study is consistent with, and adds to the knowledge of previous studies, regarding the negative association of fitness and the level of SES.
In our study, the difference in fitness, with a 3.4 mL × min− 1 × kg− 1 lower mean CRF in low SES areas, corresponding to 1 MET, is clinically relevant. In a meta-analysis of 33 observational cohort studies, Kodama et al. showed that an increase in maximum aerobic capacity of 1 MET was associated with a 13% and 15% decreased risk of all-cause mortality and CVD events, respectively (Kodama et al., 2009). Another previous study (Blair et al., 1989) also indicated health-related threshold values for fitness of 32 and 35 mL × min− 1 × kg− 1 for women and men, respectively. Below these values, mortality rates increased markedly over an 8-year follow-up (Blair et al., 1989). The observed absolute values in the present study, with medians of 25 and 28 mL × min− 1 × kg− 1, indicate that a large proportion of participants have a CRF at or below these thresholds. This fact suggests that even modest differences between SES strata may be important for health-related outcomes. As individual fitness levels are explained by genetic variation and the amount of aerobic PA undertaken (Lavie et al., 2015), these findings emphasize the importance of PA for middle-aged people in general, but especially for low SES populations.
4.1. Study limitations and strengths
Strengths of this study include the selection of a sample designed to provide a maximal difference with respect to social advantages, with an even distribution of participants between contrasting SES groups. Furthermore, the use of objectively measured PA through accelerometer assessment provided more detailed and reliable information compared with self-reported measurements. Because the study was conducted throughout the year, this limited the potential confounding of seasonal variability in PA. However, this suggested effect has, as yet, not been observed in Sweden (Hagstromer et al., 2014). The cross-sectional design of the study did not permit a causal explanation of observed relationships. Uneven participation rates between SES areas were a potential source of selection bias, which possibly diminished the observed disparities because non-respondents may potentially also be less active. There are other methodological issues, such as the limited validity in assessing posture (sitting and standing still). The current definition of non-wear time might have led to excluded observations. However, concordance with previous studies allow for correct comparisons. Moreover, because the device is worn over the hip, upper body movements will not have been accurately estimated. Further, because CRF was estimated indirectly through a sub-maximal test, rather than direct measurement of aerobic capacity, this may have introduced a risk of measurement error. However, this method has been repeatedly validated and tested for reliability.
5. Conclusions
This study showed an association between residential area SES and PA pattern and fitness, which were at least partly independent of individual SES. Living in a low SES area was associated with significantly fewer minutes of MVPA and lower mean PA levels. Residents of low SES areas were also significantly less likely to reach 150 min of MVPA per week, from bouts of 10 min or more. In addition, low SES was associated with a significantly reduced level of fitness in the studied population. While low SES is undeniably associated with health-related outcomes, these results indicate that disparities between SES areas are potentially mediated through PA and fitness levels. These results further add to the body of evidence that physical inactivity and low fitness levels are potential contributors to social inequalities in health, and may be primary targets for improving public health in populations of low SES.
Conflict of interest statement
The authors declare that there are no conflicts of interest.
Transparency document
Transparency document.
Acknowledgments
The study was financed by grants from the Swedish state, under the agreement between the Swedish government and the county councils concerning economic support of research and education of doctors (ALF-agreement, ALFGBG-427301), the Swedish Heart and Lung Foundation (2015-0438 2012-0325), the Swedish Research Council (2013-4236, 2013-5187), and the Swedish Council for Working Life and Social Research (Epilife).
Footnotes
The Transparency document associated with this article can be found, in online version.
References
- Astrand P.O. Nomogram for calculation of maximal oxygen uptake capacity. Medd Flyg Navalmed Namnd Statens Namnd For Flyg Navalmed Forsk Forsoksvererksamhet. 1953;4:16–17. [PubMed] [Google Scholar]
- Astrand P.O., Ryhming I. A nomogram for calculation of aerobic capacity (physical fitness) from pulse rate during sub-maximal work. J. Appl. Physiol. 1954;7(2):218–221. doi: 10.1152/jappl.1954.7.2.218. [DOI] [PubMed] [Google Scholar]
- Bergman P. Adherence to physical activity recommendations and the influence of socio-demographic correlates — a population-based cross-sectional study. BMC Public Health. 2008;8:367. doi: 10.1186/1471-2458-8-367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergstrom G. Low socioeconomic status of a patient's residential area is associated with worse prognosis after acute myocardial infarction in Sweden. Int. J. Cardiol. 2015;182:141–147. doi: 10.1016/j.ijcard.2014.12.060. [DOI] [PubMed] [Google Scholar]
- Bergstrom G. The Swedish CArdioPulmonary BioImage Study: objectives and design. J. Intern. Med. 2015;278(6):645–659. doi: 10.1111/joim.12384. Epub 2015 Jun 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair S.N. Physical fitness and all-cause mortality. A prospective study of healthy men and women. JAMA. 1989;262(17):2395–2401. doi: 10.1001/jama.262.17.2395. [DOI] [PubMed] [Google Scholar]
- Carlson S.A. Trend and prevalence estimates based on the 2008 Physical Activity Guidelines for Americans. Am. J. Prev. Med. 2010;39(4):305–313. doi: 10.1016/j.amepre.2010.06.006. [DOI] [PubMed] [Google Scholar]
- Dunstan D.W. Too much sitting — a health hazard. Diabetes Res. Clin. Pract. 2012;97(3):368–376. doi: 10.1016/j.diabres.2012.05.020. [DOI] [PubMed] [Google Scholar]
- Ekblom O. Cardiorespiratory fitness, sedentary behaviour and physical activity are independently associated with the metabolic syndrome, results from the SCAPIS Pilot Study. PLoS One. 2015;10(6):e0131586. doi: 10.1371/journal.pone.0131586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekblom-Bak E. The daily movement pattern and fulfilment of physical activity recommendations in Swedish middle-aged adults: the SCAPIS Pilot Study. PLoS One. 2015;10(5) doi: 10.1371/journal.pone.0126336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galobardes B. Indicators of socioeconomic position (part 1) J. Epidemiol. Community Health. 2006;60(1):7–12. doi: 10.1136/jech.2004.023531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galobardes B., Lynch J., Smith G.D. Measuring socioeconomic position in health research. Br. Med. Bull. 2007;81–82(1):21–37. doi: 10.1093/bmb/ldm001. [DOI] [PubMed] [Google Scholar]
- Hagstromer M., Oja P., Sjostrom M. Physical activity and inactivity in an adult population assessed by accelerometry. Med. Sci. Sports Exerc. 2007;39(9):1502–1508. doi: 10.1249/mss.0b013e3180a76de5. [DOI] [PubMed] [Google Scholar]
- Hagstromer M., Rizzo N.S., Sjostrom M. Associations of season and region on objectively assessed physical activity and sedentary behaviour. J. Sports Sci. 2014;32(7):629–634. doi: 10.1080/02640414.2013.844349. [DOI] [PubMed] [Google Scholar]
- Haskell W.L. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med. Sci. Sports Exerc. 2007;39(8):1423–1434. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 2014. Inequalities in Health and Living Conditions in Gothenburg: Interim Report 2014. (Swedish) [Google Scholar]
- Jones D.A. Moderate leisure-time physical activity: who is meeting the public health recommendations? A national cross-sectional study. Arch. Fam. Med. 1998;7(3):285–289. doi: 10.1001/archfami.7.3.285. [DOI] [PubMed] [Google Scholar]
- Kanjilal S. Socioeconomic status and trends in disparities in 4 major risk factors for cardiovascular disease among US adults, 1971–2002. Arch. Intern. Med. 2006;166(21):2348–2355. doi: 10.1001/archinte.166.21.2348. [DOI] [PubMed] [Google Scholar]
- Kavanagh A.M. Urban area disadvantage and physical activity: a multilevel study in Melbourne, Australia. J. Epidemiol. Community Health. 2005;59(11):934–940. doi: 10.1136/jech.2005.035931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kodama S. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA. 2009;301(19):2024–2035. doi: 10.1001/jama.2009.681. [DOI] [PubMed] [Google Scholar]
- Laaksonen M. Health behaviours as explanations for educational level differences in cardiovascular and all-cause mortality: a follow-up of 60 000 men and women over 23 years. Eur. J. Pub. Health. 2008;18(1):38–43. doi: 10.1093/eurpub/ckm051. [DOI] [PubMed] [Google Scholar]
- Lakka T.A., Kauhanen J., Salonen J.T. Conditioning leisure time physical activity and cardiorespiratory fitness in sociodemographic groups of middle-ages men in eastern Finland. Int. J. Epidemiol. 1996;25(1):86–93. doi: 10.1093/ije/25.1.86. [DOI] [PubMed] [Google Scholar]
- Lavie C.J. Exercise and the cardiovascular system: clinical science and cardiovascular outcomes. Circ. Res. 2015;117(2):207–219. doi: 10.1161/CIRCRESAHA.117.305205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee I.M. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380(9838):219–229. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leslie E., Cerin E., Kremer P. Perceived neighborhood environment and park use as mediators of the effect of area socio-economic status on walking behaviors. J. Phys. Act. Health. 2010;7(6):802–810. doi: 10.1123/jpah.7.6.802. [DOI] [PubMed] [Google Scholar]
- Macera C.A. Prevalence of physical activity in the United States: Behavioral Risk Factor Surveillance System, 2001. Prev. Chronic Dis. 2005;2(2):A17. [PMC free article] [PubMed] [Google Scholar]
- Mackenbach J.P. Socioeconomic inequalities in cardiovascular disease mortality; an international study. Eur. Heart J. 2000;21(14):1141–1151. doi: 10.1053/euhj.1999.1990. [DOI] [PubMed] [Google Scholar]
- Manhem K. Social gradients in cardiovascular risk factors and symptoms of Swedish men and women: the Goteborg MONICA Study 1995. J. Cardiovasc. Risk. 2000;7(5):359–368. doi: 10.1177/204748730000700509. [DOI] [PubMed] [Google Scholar]
- Marmot M.G. Contribution of job control and other risk factors to social variations in coronary heart disease incidence. Lancet. 1997;350(9073):235–239. doi: 10.1016/s0140-6736(97)04244-x. [DOI] [PubMed] [Google Scholar]
- Marques A. The correlates of meeting physical activity recommendations: a population-based cross-sectional study. Eur. J. Sport Sci. 2014;14(Suppl. 1):S462–S470. doi: 10.1080/17461391.2012.713008. [DOI] [PubMed] [Google Scholar]
- Matthews C.E. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am. J. Epidemiol. 2008;167(7):875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeill L.H., Kreuter M.W., Subramanian S.V. Social environment and physical activity: a review of concepts and evidence. Soc. Sci. Med. 2006;63(4):1011–1022. doi: 10.1016/j.socscimed.2006.03.012. [DOI] [PubMed] [Google Scholar]
- Meijer M. Do neighborhoods affect individual mortality? A systematic review and meta-analysis of multilevel studies. Soc. Sci. Med. 2012;74(8):1204–1212. doi: 10.1016/j.socscimed.2011.11.034. [DOI] [PubMed] [Google Scholar]
- Nishida C., Ko G.T., Kumanyika S. Body fat distribution and noncommunicable diseases in populations: overview of the 2008 WHO Expert Consultation on Waist Circumference and Waist-Hip Ratio. Eur. J. Clin. Nutr. 2010;64(1):2–5. doi: 10.1038/ejcn.2009.139. [DOI] [PubMed] [Google Scholar]
- Parks S.E., Housemann R.A., Brownson R.C. Differential correlates of physical activity in urban and rural adults of various socioeconomic backgrounds in the United States. J. Epidemiol. Community Health. 2003;57(1):29–35. doi: 10.1136/jech.57.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rawshani A. Impact of socioeconomic status on cardiovascular disease and mortality in 24,947 individuals with type 1 diabetes. Diabetes Care. 2015;38(8):1518–1527. doi: 10.2337/dc15-0145. [DOI] [PubMed] [Google Scholar]
- Rodjer L. Self-reported leisure time physical activity: a useful assessment tool in everyday health care. BMC Public Health. 2012;12:693. doi: 10.1186/1471-2458-12-693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosengren A. Education and risk for acute myocardial infarction in 52 high, middle and low-income countries: INTERHEART case–control study. Heart. 2009;95(24):2014–2022. doi: 10.1136/hrt.2009.182436. [DOI] [PubMed] [Google Scholar]
- Schaufelberger M., Rosengren A. Heart failure in different occupational classes in Sweden. Eur. Heart J. 2007;28(2):212–218. doi: 10.1093/eurheartj/ehl435. [DOI] [PubMed] [Google Scholar]
- Scheers T., Philippaerts R., Lefevre J. Compliance with different physical activity recommendations and its association with socio-demographic characteristics using an objective measure. BMC Public Health. 2013;13:136. doi: 10.1186/1471-2458-13-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shishehbor M.H. Association of neighborhood socioeconomic status with physical fitness in healthy young adults: the Coronary Artery Risk Development in Young Adults (CARDIA) study. Am. Heart J. 2008;155(4):699–705. doi: 10.1016/j.ahj.2007.07.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugiyama T. Do relationships between environmental attributes and recreational walking vary according to area-level socioeconomic status? J. Urban Health. 2015;92(2):253–264. doi: 10.1007/s11524-014-9932-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Swedish National Board of Health and Welfare . 2011. National Guidelines for Methods of Preventing Disease. [Google Scholar]
- Troiano R.P. Physical activity in the United States measured by accelerometer. Med. Sci. Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- Trost S.G., McIver K.L., Pate R.R. Conducting accelerometer-based activity assessments in field-based research. Med. Sci. Sports Exerc. 2005;37(11 Suppl.):S531–S543. doi: 10.1249/01.mss.0000185657.86065.98. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transparency document.