Abstract
Introduction
Globally, respiratory syncytial virus (RSV) is the most common cause of serious lower respiratory tract infections (LRTIs) in young children, and is a major cause of hospital admission in children <1 year of age. The study evaluated the severity of RSV-associated LRTI disease among premature (<36 weeks gestational age (GA)) and term children <1 year of age and assessed the influence of GA on outcomes of RSV LRTI hospitalization in Central and Eastern Europe (CEE).
Methods
Retrospective cohort survey of children <1 year of age hospitalized with an LRTI during the periods of October 2009 to April 2010 or October 2010 to April 2011 in 12 CEE countries.
Results
Across two RSV seasons, 3474 evaluable children were hospitalized because of LRTI; 757 (21.8%) were premature and 2679 (77.1%) were term. RSV tests were positive in 1423 (42.4%) cases, of which 266 (18.7%) were premature and 1034 (72.7%) were term children. Among the RSV-positive patients, premature children had a significantly longer hospital stay (17 vs 8 days; P < 0.001), were more frequently hospitalized in the intensive care unit (ICU) (41.4% vs 12.6%) and remained in the ICU significantly longer (13 vs 6 days; P < 0.001) compared with term children. Premature children had a 3.3-fold (95% CI, 2.66–4.09) increased risk for ICU hospitalization compared with term children (P < 0.001). ICU hospitalization, prolonged hospital stay, supplemental oxygen administration and death occurred significantly more frequently among children with lower vs higher GA.
Conclusion
RSV infection is associated with substantial morbidity in CEE among premature and term children. The attributable morbidity, however, is significantly greater among premature children compared with term children, including longer hospital stays and more frequent and longer stays in the ICU. These findings are consistent with previously published data outside of CEE, demonstrating prematurity as a significant and independent predictor for severe RSV disease.
Funding
AbbVie Inc.
Keywords: Gestational age category, ICU stay, Prematurity, Respiratory syncytial virus, RSV hospitalization
Introduction
Globally, respiratory syncytial virus (RSV) is a major cause of hospital admission in infants <1 year of age [1]. Mortality data demonstrate that RSV kills more infants in this age group than any other single pathogen with the exception of malaria [2]. Environmental factors and individual characteristics carrying increased risk of RSV-associated acute respiratory tract infections include low birth weight, being a member of a multiple birth, smoking during pregnancy, having siblings, day care attendance (or sibling attendance), living in a crowded household, low parental education, second-hand smoke exposure, history of atopy and lack of breastfeeding [3–10]. Notably, being male carries a risk ratio of 1.425:1 compared with being female [11]. Certain high-risk groups including premature infants, infants with bronchopulmonary dysplasia (more commonly referred to as chronic lung disease of prematurity) and those with congenital heart disease are particularly vulnerable to severe RSV disease [12, 13]. RSV is more likely to progress to the lower respiratory tract and cause more serious disease in these high-risk children compared with otherwise healthy term children. Furthermore, the course of illness tends to be more severe in these children versus otherwise healthy term children, and is associated with higher rates of hospitalization, intensive care unit admission, mechanical ventilation and death [14–18].
The RSV burden of disease is relatively well characterized in Western Europe; however, there are limited epidemiologic data available for Central and Eastern Europe (CEE) and the developing world. Mortality data are especially difficult to ascertain as the majority of children in developing countries die outside of the hospital setting [19]. Characterization of children with severe RSV disease is critically important to inform health care authorities to target interventions that maximize population health. The present study aimed to characterize RSV disease incidence and severity among premature and term children in CEE. We evaluated the severity of RSV-associated lower respiratory tract infection (LRTI) disease in children <1 year of age during the 2009–2010 and 2010–2011 RSV seasons and investigated the influence of gestational age (GA) on the treatment, complications and outcomes of RSV LRTI hospitalization.
Methods
Study Design
This retrospective, epidemiologic, cohort survey included children <1 year of age hospitalized with an LRTI during the periods October 2009 to April 2010 and October 2010 to April 2011. Children with duplicate records were excluded. Patients were hospitalized in the pediatric intensive care units and pediatrics wards of general, university, pediatric or other types of hospitals at 48 study sites across 12 CEE countries (Estonia, Lithuania, Hungary, Slovenia, Croatia, Serbia, Bosnia/Herzegovina, Bulgaria, Czech Republic, Slovakia, Romania, and Ukraine). Data collection was performed on day of hospital discharge or during first checkup visit after LRTI hospitalization. An enrollment form was used to collect demographic and clinical data from enrolled patients.
The study was conducted in compliance with any applicable national or institutional ethical and/or regulatory requirements. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964. Local law requirements for monitoring, notification/submission of an epidemiologic survey to the responsible ethics committee and/or regulatory body were followed, and ethical approval was obtained in the participating countries according to national legislation. The study sponsor vouches for the veracity of the multiple ethical approvals. The patient’s parent, guardian or legal representative provided oral/written authorization to the investigator to use and/or disclose personal and/or health data.
Study Endpoints, Outcome Measurements and Definitions
The primary endpoint was to evaluate the severity of RSV-associated LRTI disease in premature and term children. Primary outcomes included duration of hospitalization and the incidence, duration and risk of intensive care unit (ICU) hospitalization. Secondary endpoints included the assessment of the influence of GA on the treatment, complications and outcomes of RSV LRTI hospitalization. Secondary outcomes included the use of supplemental oxygen administration, use of bronchodilators, duration of hospitalization, the incidence and duration of ICU hospitalization and death.
LRTI was defined as a diagnosis of pneumonia and/or bronchiolitis according to individual hospital/physician procedures. Radiographic evidence of LRTI was not collected. RSV-positive children were defined as all children who had an LRTI hospitalization with RSV-positivity confirmed by the RSV rapid diagnostic test. Because RSV testing was not standardized across the study sites, inter-site quality analysis was not performed within the study group. RSV-positive children with a known GA ≤36 weeks were defined as premature. RSV-positive children with a known GA ≥37 weeks and no other risk factors (congenital heart disease, bronchopulmonary dysplasia, Down syndrome or neuromuscular disease) were defined as term children. Gestational age was categorized into subgroups, based on World Health Organization criteria [20], for further analysis of the impact of preterm birth on outcomes: extremely preterm (<28 weeks), very preterm (28 to <32 weeks) and moderate preterm (32–36 completed weeks of gestation). Congenital heart disease, bronchopulmonary dysplasia, Down syndrome and neuromuscular disease were not uniformly defined or standardized in the protocol. Diagnoses of these conditions were based on the individual physician’s experience and local practice guidelines.
Statistical Analysis
Standard descriptive statistics were used to describe the data: counts and percentages for categorical data, mean and standard deviation for continuous data, and absolute frequency for incidence of cases. The denominator used to determine the incidence of ICU hospitalization and death was the total population of children <1 year of age hospitalized with an LRTI at participating sites during the study periods. Calculation of incidence did not include compensation for the use of seasonal data versus year-round data.
The type of admission diagnosis was compared between groups via two-sided Chi-square tests on a 5% level of significance. Duration of hospitalization and duration of supplemental oxygen administration was compared between groups by means of two-sided t tests on a 5% level of significance. The influence of admission diagnosis on the observed effects was investigated by means of two-sided t tests on a 5% level of significance [equivalent to a one-way analysis of variance (ANOVA) with group in the model] with admission diagnosis as an additional factor. Duration of hospitalization and duration of supplemental oxygen administration were compared between groups (RSV-positive and RSV-negative, RSV-positive premature and RSV-negative premature, RSV-positive premature and RSV-positive term). To adjust for the influence of admission diagnosis, this model was extended to a two-factor ANOVA with group and admission diagnosis in the model. In large study populations such as these, the two-sided t test (one-way ANOVA) and two-factor ANOVA are robust against deviations from the normality of assumption and homogeneity of variances assumption.
For the endpoint of ICU hospitalization, the relative risk and associated two-sided asymptotic 95% CIs were derived to compare the risk of ICU hospitalization between the groups. A Chi-square test was performed to compare the occurrence of ICU hospitalizations between groups at a 5% level of significance. A Cochran–Mantel–Haenszel test was used post hoc to adjust for admission diagnosis differences between groups. A Chi-square test, Cochran–Mantel–Haenszel test and relative risk with associated two-sided asymptotic 95% CIs were also performed for the occurrence of supplemental oxygen administration and death.
The influence of GA at birth on admission diagnosis, ICU hospitalization, use of bronchodilators and oxygen administration was compared between groups using two-sided Chi-square tests at a 5% level of significance. The influence of GA at birth on the duration of hospitalization, duration of ICU hospitalization and duration of oxygen administration was assessed using analysis of variance at the 5% level of significance. All statistical analyses were carried out by means of the SAS® package (version 9.2) (GKM Gesellschaft für Therapieforschung mbH, Munich, Germany).
Results
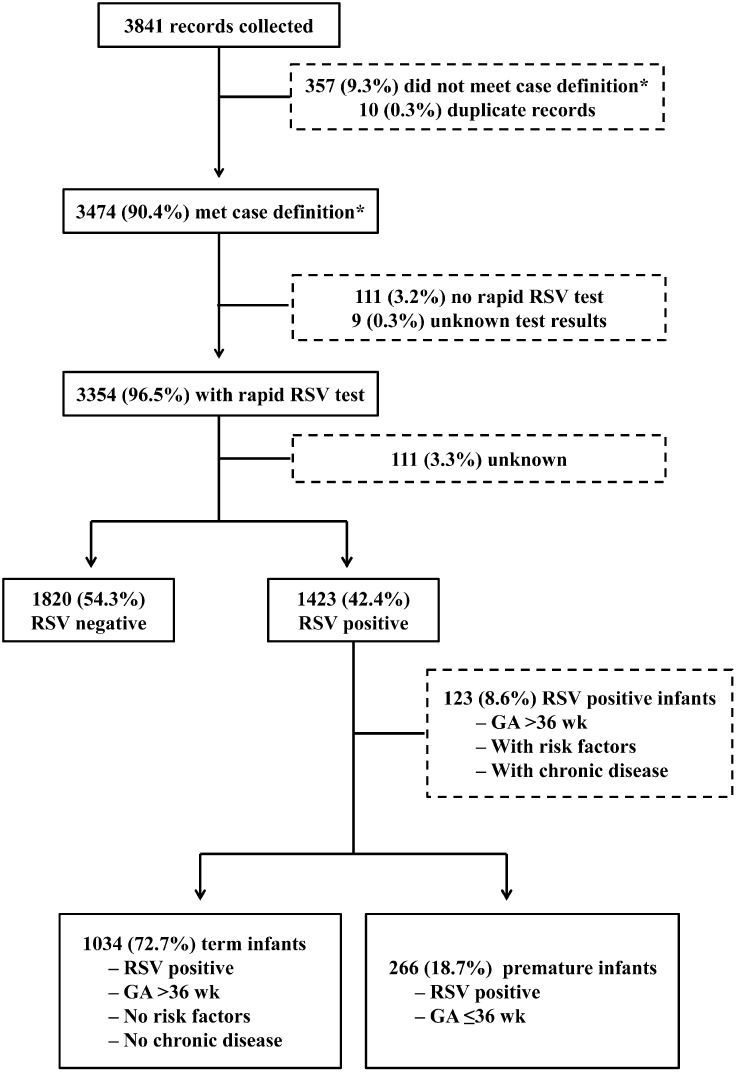
During the study period of October 2009–April 2010 and October 2010–April 2011, overall, 3841 records were collected from 48 sites across 12 CEE countries. Among them, 3474 children (90.4%) fulfilled the case definition of a documented hospitalized LRTI and were enrolled in the study (Fig. 1). Of the 3474 evaluable children, 757 children (21.8%) were premature (≤36 weeks GA) and 2679 (77.1%) were term. The majority of the population was male (58.3%) and younger than 6 months (69.1%) at the time of admission. RSV prophylaxis had been administered in 2% (n = 68) of the entire cohort. Demographic and clinical characteristics of the study cohort are summarized in Table 1.
Fig. 1.
Disposition of study population. *Children who met the case definition had to be <1 year of age and hospitalized with a diagnosis of bronchiolitis and/or pneumonia within the observational periods October 2009 through April 2010 or October 2010 through April 2011. GA gestational age, RSV respiratory syncytial virus
Table 1.
Demographics and clinical characteristics of the study population
| Characteristic | Study population (n = 3474) |
|---|---|
| Sex, n (%) | |
| Male | 2024 (58.3) |
| Female | 1409 (40.6) |
| Unknown | 41 (1.2) |
| Age at admissiona, month, mean (SD) | 5 (3) |
| Age category at admission, month, n (%) | |
| 0–<6 | 2400 (69.1) |
| 6–12 | 1074 (30.9) |
| Gestational ageb, week, mean (SD) | 36 (2) |
| Gestational age categories, week, n (%) | |
| <29 | 121 (3.5) |
| 29–32 | 233 (6.7) |
| 33–36 | 403 (11.6) |
| >36 | 2679 (77.1) |
| Unknown | 38 (1.1) |
| BW, g, mean (SD) | 2998 (841) |
| BW categories, g, n (%) | |
| Extremely low BW (BW < 1000 g) | 101 (2.9) |
| Very low BW (1000 g ≤ BW < 1500 g) | 176 (5.1) |
| Low BW (1500 g ≤ BW < 2500 g) | 482 (13.9) |
| Normal BW (2500 g ≤ BW ≤ 4200 g) | 2592 (74.6) |
| High BW (BW > 4200 g) | 114 (3.3) |
| Unknown | 9 (0.3) |
| Diagnosis at admission, n (%) | |
| Bronchiolitis only | 1983 (57.1) |
| Pneumonia only | 1183 (34.1) |
| Bronchiolitis and pneumonia | 308 (8.9) |
| RSV diagnosisc, n (%) | |
| RSV-positive | 1423 (42.4) |
| RSV-negative | 1820 (54.3) |
| Unknown | 111 (3.3) |
| Risk factors for severe RSV infection, n (%) | |
| Premature (GA ≤36 week) | 757 (21.8) |
| Congenital heart disease | 166 (4.8) |
| Bronchopulmonary dysplasia | 145 (4.2) |
| Neuromuscular disease | 108 (3.1) |
| Duration of hospitalization, day, mean (95% CI) | 10.8 (10.4–11.2) |
| Hospital duration categories, day, n (%) | |
| 1–3 | 224 (6.4) |
| 4–7 | 1360 (39.1) |
| 8–14 | 1408 (40.5) |
| ≥15 | 470 (13.5) |
| Unknown | 12 (0.3) |
| ICU hospitalization, n (%) | 671 (19.3) |
| Length of ICU stay, dayd, mean (95% CI) | 11.0 (9.9–12.1) |
| Supplemental oxygen use, n (%) | 1563 (45.0) |
| Duration of supplemental oxygen use, daye, mean (95% CI) | 6.4 (5.9–6.9) |
| Bronchodilator use, n (%) | 2698 (77.7) |
| Duration of bronchodilator use, dayf, mean (95% CI) | 7.4 (7.1–7.6) |
| Patient outcome at discharge, n (%) | |
| Complete recovery | 1623 (46.7) |
| Improvement | 1782 (51.3) |
| Death | 30 (0.9) |
| Transfer to another hospital | 21 (0.6) |
| Unknown | 18 (0.5) |
BW birth weight, GA gestational age, ICU intensive care unit, RSV respiratory syncytial virus
aAge was recorded on the case report form. The mean calculation category 0–6 months was analyzed as 3 months; the age category 6–12 months was analyzed as 9 months
bGestational age was recorded on the case report form
cPercentages were calculated on 3354 cases with RSV rapid tests
dOnly for patients who were hospitalized
eOnly for patients who used oxygen
fOnly for patients who used bronchodilators
A rapid RSV test was performed in 3354 (96.5%) cases and RSV tests were positive in 1423 (42.4%). Of the RSV-positive cases, 266 (18.7%) were premature children and 1034 (72.7%) were term children with no risk factors or chronic diseases. RSV prophylaxis had been administered in 11 RSV-positive cases, among them 9 children with GA <33 weeks and 2 term children. A comparison of the baseline admission demographics, clinical characteristics and outcomes of RSV LRTI hospitalization between premature and term children is illustrated in Table 2.
Table 2.
Baseline admission demographics, clinical characteristics and outcomes of RSV LRTI hospitalization between premature and term children
| Characteristic | Premature (n = 266) | Term (n = 1034) | P value |
|---|---|---|---|
| Sex, n (%) | ND | ||
| Male | 147 (55.3) | 591 (57.2) | |
| Female | 114 (42.9) | 426 (41.2) | |
| Unknown | 5 (1.9) | 17 (1.6) | |
| Age at admission, n (%) | ND | ||
| 0–<6 months | 203 (76.3) | 770 (74.5) | |
| 6–12 months | 63 (23.7) | 264 (25.5) | |
| Presence of chronic diseases at admission, n (%) | ND | ||
| Any chronic disease | 91 (34.2) | 0 | |
| Congenital heart disease | 27 (10.2) | 0 | |
| Bronchopulmonary dysplasia | 41 (15.4) | 0 | |
| Neuromuscular disease | 18 (6.8) | 0 | |
| Other chronic diseases | 42 (15.8) | 0 | |
| RSV prophylaxis, n (%) | 9 (3.4) | 2 (0.2) | ND |
| Diagnosis at admission, n (%) | <0.001* | ||
| Bronchiolitis only | 129 (48.5) | 736 (71.2) | |
| Pneumonia only | 100 (37.6) | 207 (20.0) | |
| Both diagnoses | 37 (13.9) | 91 (8.8) | |
| Duration of hospitalization, day, mean (SD) | 17 (20) | 8 (5) | <0.001† |
| ICU hospitalization, n (%) | 110 (41.4) | 130 (12.6) | ND |
| Length of ICU stay, day, mean (SD) | 13 (15) | 6 (5) | <0.001† |
| Supplemental oxygen use, n (%) | 194 (72.9) | 479 (46.3) | ND |
| Duration of supplemental oxygen use, day, mean (SD) | 9 (12) | 4 (3) | <0.001† |
| Outcome at discharge, n (%) | ND | ||
| Complete recovery | 122 (45.9) | 418 (40.4) | |
| Improved | 132 (49.6) | 601 (58.1) | |
| Death | 7 (2.6) | 3 (0.3) | |
| Transfer to other hospital | 3 (1.1) | 6 (0.6) | |
| Unknown | 2 (0.8) | 6 (0.6) |
ICU intensive care unit, LRTI lower respiratory tract infection, ND not determined, RSV respiratory syncytial virus
* Statistical significance was determined using two-sided Chi-square tests on a 5% level of significance
†Statistical significance was determined using analysis of variance on a 5% level of significance
Significant differences in the diagnosis at admission were observed between premature and term children. Premature children were more frequently hospitalized due to pneumonia (37.6% vs 20.0%) and term children were more frequently hospitalized due to bronchiolitis (48.5% vs 71.2%; P < 0.001). Hospital stays were significantly longer for premature children compared with term children (17 vs 8 days; P < 0.001; P value adjusted for admission diagnosis: <0.001). Premature children had a 3.3-fold (95% CI: 2.66, 4.09) increased risk for ICU hospitalization compared with term children (P < 0.001); after adjustment for admission diagnosis (including only those admitted with a diagnosis of either pneumonia or bronchiolitis), risk was increased 2.8-fold (95% CI: 2.23, 3.47; P < 0.001). ICU hospitalizations were more frequent for premature children (41.4% vs 12.6%; P value not determined), and ICU stays were longer (13 vs 6 days; P < 0.001) compared with term children (P value adjusted for admission diagnosis: <0.001).
Premature children had a 1.6-fold (95% CI: 1.43, 1.74) increased risk of receiving supplemental oxygen compared with term children (P < 0.001); after adjustment for admission diagnosis, risk was 1.6-fold greater (95% CI: 1.44, 1.78; P < 0.001). Compared with term children, oxygen was administered in premature children markedly more frequently (72.9% vs 46.3%; P value not determined) and for a significantly longer mean duration (9 vs 4 days; P < 0.001; P value adjusted for admission diagnosis: <0.001).
Evaluation of RSV LRTI Hospitalization by Gestational Age
GA was reported for 1412 (99.2%) children hospitalized for RSV LRTI hospitalized children. A comparison of the baseline admission demographics, clinical characteristics and outcomes of RSV LRTI hospitalization between the GA strata is illustrated in Table 3. No substantial differences in age at admission were observed among the considered strata. The proportion of children with an admission diagnosis of bronchiolitis (with or without pneumonia) significantly increased through the GA strata, ranging from 34.3% in the ≤28-week stratum to 78.9% in the ≥37-week stratum (P < 0.001). The mean duration of hospitalization decreased significantly through the GA strata, ranging from 29 days in the ≤28-week stratum to 9 days in the ≥37-week stratum (P < 0.001).
Table 3.
Baseline admission demographics, clinical characteristics and outcomes of RSV LRTI hospitalization between gestational age at birth
| RSV-positive cases | Gestational age | P value | |||
|---|---|---|---|---|---|
| ≤28 weeks (n = 35) | 29–32 weeks (n = 86) | 33–36 weeks (n = 145) | ≥37 weeks (n = 1146) | ||
| Sex, n (%) | ND | ||||
| Male | 15 (42.9) | 60 (69.8) | 72 (49.7) | 663 (57.9) | |
| Female | 20 (57.1) | 26 (30.2) | 68 (46.9) | 465 (40.6) | |
| Unknown | 0 | 0 | 5 (3.4) | 18 (1.6) | |
| Age at admission, n (%) | ND | ||||
| 0–<6 months | 27 (77.1) | 70 (81.4) | 106 (73.1) | 857 (74.8) | |
| 6–12 months | 8 (22.9) | 16 (18.6) | 39 (26.9) | 289 (25.2) | |
| Diagnosis at admission, n (%) | <0.001* | ||||
| Bronchiolitis only | 12 (34.3) | 37 (43.0) | 80 (55.2) | 788 (68.8) | |
| Pneumonia only | 23 (65.7) | 41 (47.7) | 36 (24.8) | 241 (21.0) | |
| Both diagnoses | 0 | 8 (9.3) | 29 (20.0) | 117 (10.2) | |
| Chronic diseases at admission, n (%) | ND | ||||
| Any chronic disease | 16 (45.7) | 44 (51.2) | 31 (21.4) | 107 (9.3) | |
| Congenital heart disease | 4 (11.4) | 9 (10.5) | 14 (9.7) | 34 (3.0) | |
| Bronchopulmonary dysplasia | 12 (34.3) | 25 (29.1) | 4 (2.8) | 0 | |
| Neuromuscular disease | 2 (5.7) | 11 (12.8) | 5 (3.4) | 18 (1.6) | |
| Other chronic diseases | 7 (20.0) | 17 (19.8) | 18 (12.4) | 76 (6.6) | |
| RSV prophylaxis, n (%) | 6 (17.1) | 3 (3.5) | 0 | 2 (0.2) | ND |
| Duration of hospitalization, day, mean (SD) | 29 (34) | 24 (21) | 11 (10) | 9 (7) | <0.001† |
| 1–3, n (%) | 1 (2.9) | 1 (1.2) | 8 (5.5) | 93 (8.1) | |
| 4–7, n (%) | 8 (22.9) | 11 (12.8) | 44 (30.3) | 494 (43.1) | |
| 8–14, n (%) | 11 (31.4) | 26 (30.2) | 68 (46.9) | 466 (40.7) | |
| ≥15, n (%) | 15 (42.9) | 48 (55.8) | 23 (15.9) | 91 (7.9) | |
| ICU hospitalization, n (%) | 19 (54.3) | 42 (48.8) | 49 (33.8) | 162 (14.1) | <0.001* |
| Length of stay in ICU, day, mean (SD) | 19 (21) | 17 (18) | 7 (6) | 7 (6) | <0.001† |
| Supplemental oxygen use, n (%) | 28 (80.0) | 67 (77.9) | 99 (68.3) | 546 (47.6) | <0.001* |
| Duration of supplemental oxygen use, day, mean (SD) | 19 (23) | 12 (10) | 5 (3) | 5 (5) | <0.001† |
| Use of bronchodilators, n (%) | 21 (60.0) | 60 (69.8) | 118 (81.4) | 952 (83.1) | |
| Outcome at discharge | ND | ||||
| Complete recovery | 11 (31.4) | 35 (40.7) | 76 (52.4) | 464 (40.5) | |
| Improved | 19 (54.3) | 46 (53.5) | 67 (46.2) | 663 (57.9) | |
| Death | 3 (8.6) | 3 (3.5) | 1 (0.7) | 5 (0.4) | |
| Transfer to other hospital | 1 (2.9) | 2 (2.3) | 0 | 7 (0.6) | |
| Unknown | 1 (2.9) | 0 | 1 (0.7) | 7 (0.6) | |
Gestational age was reported for 1412 of the 1423 children with RSV infections
ICU intensive care unit, LRTI lower respiratory tract infection, ND not determined, RSV respiratory syncytial virus
* Statistical significance was determined using two-sided Chi-square tests on a 5% level of significance
†Statistical significance was determined using analysis of variance on a 5% level of significance
The proportion of cases requiring ICU hospitalization decreased significantly through the GA strata, ranging from 54.3% in the ≤28-week stratum to 14.1% in the ≥37-week stratum (P < 0.001). The length of stay in the ICU was comparable in the 33- to 36-week stratum and the ≥37-week stratum (7 days for both groups); however, the duration was significantly longer in children with GA <33 weeks (P < 0.001; 17 days in the 29- to 32-week stratum and 19 days in the ≤28-week stratum). Overall, the observed differences in length of stay in the ICU were statistically significant (P < 0.001) across the GA strata.
The proportion of children requiring supplemental oxygen significantly decreased through the GA strata, ranging from 80.0% in the ≤28-week stratum to 47.6% in the ≥37-week stratum (P < 0.001). Duration of supplemental oxygen use also significantly decreased as GA increased, ranging from 19 days in the ≤28-week stratum to 5 days in the ≥37-week stratum (P < 0.001). The proportion of children treated with bronchodilators increased through the strata, ranging from 60.0% in the ≤28-week stratum to 83.1% in the ≥37-week stratum. Regarding outcome at discharge, the proportion of children who recovered completely ranged from 31.4% in the ≤28-week stratum to 52.4% in the 33- to 36-week stratum. There were 12 deaths, with the proportion of deaths decreasing with increasing GA. Among them, six premature children (three deaths in each of the ≤28- and 29- to 32-week strata, one death in the 33- to 36-week stratum) and five term children died.
Discussion
The main objective of this multinational study was to characterize the severity of RSV-associated LRTI disease among premature and term CEE children younger than 1 year across two RSV seasons. Our analysis of 1423 RSV-positive children demonstrates substantial morbidity in the first year of life among children hospitalized for RSV LRTI in CEE. Consistent with other geographic regions, premature children with chronological age <1 year are at greater risk for a more severe course of RSV disease compared with their term-delivered counterparts. These results provide further evidence that, like exposure to second-hand smoke, being male, and living with siblings, prematurity is a near-universal risk factor for severe RSV-associated infection [3–9, 11].
Premature children were more frequently hospitalized due to pneumonia (with and without bronchiolitis) than term children (51.5% vs 28.8%; P < 0.001). The observed differences in admission diagnosis might reflect different hospitalization strategies for premature and term children. We cannot determine from this analysis whether premature and term children presenting with similar symptoms were equally likely to be hospitalized.
Premature children exhibited longer stays in the hospital, more frequent and longer stays in the ICU and more frequent and longer administration of supplemental oxygen than term children; even after adjusting for the admission diagnosis, the differences remain significant (P < 0.001). In fact, the risk of an ICU stay was 2.8 times higher in premature than term children after adjusting for admission diagnosis. Furthermore, decreasing GA at birth was found to increase risk for ICU hospitalization, prolonged duration of hospitalization, supplemental oxygen administration and death. Even among late premature children (33–36 weeks gestation), the course of RSV-positive LRTI disease was more severe than that of full-term children. Compared with term children, a greater proportion of late premature children (33–36 weeks gestation) with RSV LRTI were hospitalized in the ICU (33.8% vs 14.1%), spent ≥15 days in the hospital (1.4% vs 1.0%) and required supplemental oxygen administration (68.3% vs 47.6%). These findings are consistent with previous studies in Western Europe and the United States that reported a high rate of healthcare utilization for RSV-positive LRTI among premature children 33–35 weeks gestation [15, 21].
The strength of this study is that it investigates a large multinational cohort of children from a geographical area that has not been previously well characterized. However, this study has several key limitations. We acknowledge that the study data from the 2009 to 2010 and 2010 to 2011 RSV seasons may not appear current. However, to our knowledge, no substantial developments in the medical practice of prevention or care of these children for RSV LRTI, including the use of prophylaxis with palivizumab, have since occurred in CEE that would change study results if conducted today. As such, the clinical relevance and severity of RSV-associated LRTI disease likely has remained the same. RSV reinfection is a common occurrence [22] and we were not able to account for possible reinfections in this study. In addition, the number of collected cases in our study was affected by factors associated with the recruitment process, such as time resources of the investigators, availability of diagnostic tests, strategies for identifying cases and obtaining consent for study participation. Given that data were collected on the day of hospital discharge or during the first checkup visit after LRTI hospitalization, bias may have been introduced. The RSV rapid diagnostic tests that utilize antigen capture technology have a sensitivity and specificity of approximately 90%. Data regarding timing of the RSV rapid test during the course of the disease were not captured. As a result, the true proportion of RSV infections may have been underestimated. Use of univariate analyses, instead of multivariate analyses, may have increased the likelihood of an analysis reaching statistical significance by chance. Furthermore, the lack of adjustment for potential confounders or other potential risk factors limits the value of the univariate assessment of potential risk factors. However, the primary endpoint was to evaluate the severity of RSV-associated LRTI disease in premature and term children. Primary outcomes included duration of hospitalization, and the incidence, duration and risk of ICU hospitalization. Because investigation of the potential risk factors was an additional, exploratory data analysis in the statistical analysis plan and the findings would not have impacted the primary endpoint of this study, we did not pursue a multivariate analysis of these factors. Because diagnosis of LRTI was based on individual physician/hospital practice, local or regional differences may also have introduced bias. National and regional differences in treatment practice and healthcare systems, especially the criteria for hospitalization, may have affected our overall risk factor findings and may also affect assessments of congenital heart disease, bronchopulmonary dysplasia, Down syndrome and neuromuscular disease, ICU admittance and use of supplemental oxygen and bronchodilators.
Conclusion
Overall, the results of this study demonstrate the importance of RSV as a significant contributor to pediatric morbidity in the first year of life and confirm results from studies outside of CEE that show that prematurely born children hospitalized for RSV-related infections have a more severe course of disease than full-term children, as demonstrated by longer stays in the hospital and more frequent and longer stays in the ICU than term children without risk factors.
Acknowledgments
We thank all of the investigators who participated in this study. Funding for this study was provided by AbbVie. AbbVie contributed to its design and participated in the collection, analysis and interpretation of the data, and in the writing, review and approval of the final version. All authors contributed to the development of the content; all authors reviewed and approved the manuscript; the authors maintained control over the final content. Input for the study design was provided by Bruno Baršić, MD, PhD, Professor, University of Zagreb School of Medicine. Medical writing services were provided by Joann Hettasch, PhD, of Arbor Communications, Inc., Ann Arbor, MI, USA, and funded by AbbVie. Additional formatting services provided by Complete Publication Solutions, LLC (North Wales, PA, USA), were also funded by AbbVie.
Disclosures
Olivier Van de Steen, Farzaneh Miri, Marta Gunjaca, Vanesa Klepac, Baerbel Gross, Gerard Notario and Colleen M. Wegzyn are AbbVie employees or were AbbVie employees at the time of study conduct and analysis and may hold stocks or options.
Compliance with Ethics Guidelines
The study was conducted in compliance with any applicable national or institutional ethical and/or regulatory requirements. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964. The study sponsor, AbbVie (formerly known as Abbott), vouches for the veracity of the multiple ethical approvals. The patient’s parent, guardian or legal representative provided oral authorization to the investigator to use and/or disclose personal and/or health data.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
Footnotes
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/64C4F0605464E11B.
References
- 1.Nair H, Nokes DJ, Gessner BD, et al. Global burden of acute lower respiratory infections due to respiratory syncytial virus in young children: a systematic review and meta-analysis. Lancet. 2010;375:1545–1555. doi: 10.1016/S0140-6736(10)60206-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shi T, Balsells E, Wastnedge E, et al. Risk factors for respiratory syncytial virus associated with acute lower respiratory infection in children under five years: systematic review and meta-analysis. J Glob Health. 2015;5:020416. doi: 10.7189/jogh.05.010408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gijtenbeek RG, Kerstjens JM, Reijneveld SA, et al. RSV infection among children born moderately preterm in a community-based cohort. Eur J Pediatr. 2015;174:435–442. doi: 10.1007/s00431-014-2415-2. [DOI] [PubMed] [Google Scholar]
- 5.Ambrose CS, Anderson EJ, Simoes EA, et al. Respiratory syncytial virus disease in preterm infants in the US born at 32–35 weeks gestation not receiving immunoprophylaxis. Pediatr Infect Dis J. 2014;33:576–582. doi: 10.1097/INF.0000000000000219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blanken MO, Koffijberg H, Nibbelke EE, et al. Prospective validation of a prognostic model for respiratory syncytial virus bronchiolitis in late preterm infants: a multicenter birth cohort study. PLoS ONE. 2013;8:e59161. doi: 10.1371/journal.pone.0059161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Figueras-Aloy J, Carbonell-Estrany X, Quero-Jimenez J, et al. FLIP-2 Study: risk factors linked to respiratory syncytial virus infection requiring hospitalization in premature infants born in Spain at a gestational age of 32 to 35 weeks. Pediatr Infect Dis J. 2008;27:788–793. doi: 10.1097/INF.0b013e3181710990. [DOI] [PubMed] [Google Scholar]
- 8.Law BJ, Langley JM, Allen U, et al. The Pediatric Investigators Collaborative Network on Infections in Canada study of predictors of hospitalization for respiratory syncytial virus infection for infants born at 33 through 35 completed weeks of gestation. Pediatr Infect Dis J. 2004;23:806–814. doi: 10.1097/01.inf.0000137568.71589.bd. [DOI] [PubMed] [Google Scholar]
- 9.Liese JG, Grill E, Fischer B, et al. Incidence and risk factors of respiratory syncytial virus-related hospitalizations in premature infants in Germany. Eur J Pediatr. 2003;162:230–236. doi: 10.1007/s00431-002-1105-7. [DOI] [PubMed] [Google Scholar]
- 10.American Academy of Pediatrics Committee on Infectious Diseases, American Academy of Pediatrics Bronchiolitis Guidelines Committee Updated guidance for palivizumab prophylaxis among infants and young children at increased risk of hospitalization for respiratory syncytial virus infection. Pediatrics. 2014;134:415–420. doi: 10.1542/peds.2014-1665. [DOI] [PubMed] [Google Scholar]
- 11.Simoes EA. Environmental and demographic risk factors for respiratory syncytial virus lower respiratory tract disease. J Pediatr. 2003;143:S118–S126. doi: 10.1067/S0022-3476(03)00511-0. [DOI] [PubMed] [Google Scholar]
- 12.Sommer C, Resch B, Simoes EA. Risk factors for severe respiratory syncytial virus lower respiratory tract infection. Open Microbiol J. 2011;5:144–154. doi: 10.2174/1874285801105010144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Simoes EA. Respiratory syncytial virus infection. Lancet. 1999;354:847–852. doi: 10.1016/S0140-6736(98)10263-5. [DOI] [PubMed] [Google Scholar]
- 14.Meert K, Heidemann S, Abella B, Sarnaik A. Does prematurity alter the course of respiratory syncytial virus infection? Crit Care Med. 1990;18:1357–1359. doi: 10.1097/00003246-199012000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Horn SD, Smout RJ. Effect of prematurity on respiratory syncytial virus hospital resource use and outcomes. J Pediatr. 2003;143:S133–S141. doi: 10.1067/S0022-3476(03)00509-2. [DOI] [PubMed] [Google Scholar]
- 16.Geskey JM, Cyran SE. Managing the morbidity associated with respiratory viral infections in children with congenital heart disease. Int J Pediatr. 2012;2012:646780. doi: 10.1155/2012/646780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Resch B, Gusenleitner W, Muller W. The impact of respiratory syncytial virus infection: a prospective study in hospitalized infants younger than 2 years. Infection. 2002;30:193–197. doi: 10.1007/s15010-002-2122-1. [DOI] [PubMed] [Google Scholar]
- 18.Holman RC, Shay DK, Curns AT, Lingappa JR, Anderson LJ. Risk factors for bronchiolitis-associated deaths among infants in the United States. Pediatr Infect Dis J. 2003;22:483–490. doi: 10.1097/01.inf.0000069765.43405.3b. [DOI] [PubMed] [Google Scholar]
- 19.UNICEF. Goal: Reduce child mortality. http://www.unicef.org/mdg/childmortality.html. Accessed 19 Jan 2016.
- 20.World Health Organization. Preterm birth. http://www.who.int/mediacentre/factsheets/fs363/en/. Accessed 4 Mar 2016.
- 21.Carbonell-Estrany X, Figueras-Aloy J, Law BJ, Infeccion Respiratoria Infantil por Virus Respiratorio Sincitial Study Group, Pediatric Investigators Collaborative Network on Infections in Canada Study Group Identifying risk factors for severe respiratory syncytial virus among infants born after 33 through 35 completed weeks of gestation: different methodologies yield consistent findings. Pediatr Infect Dis J. 2004;23:S193–S201. doi: 10.1097/01.inf.0000144664.31888.53. [DOI] [PubMed] [Google Scholar]
- 22.Bosis S, Esposito S, Niesters HG, et al. Role of respiratory pathogens in infants hospitalized for a first episode of wheezing and their impact on recurrences. Clin Microbiol Infect. 2008;14:677–684. doi: 10.1111/j.1469-0691.2008.02016.x. [DOI] [PMC free article] [PubMed] [Google Scholar]