Abstract
Objective
The purpose of this review was to identify how rural and urban food access differs across small food stores as well as the types of research strategies and methodologies that have been applied in each setting in the U.S.
Methods
Manuscripts were included in the review if they were published in English over the past ten years, with a clear delineation between urban and/or rural, conducted in the U.S., and reported data from small food store research.
Results
After elimination, 19 manuscripts representing rural (n = 5) and urban (n = 14) settings were included in the final review. The review was conducted in Nebraska between January 2015 and May 2015. Findings from the reviewed manuscripts revealed that rural communities might face different challenges with healthy food access in small food stores when compared to urban settings. In particular, small food stores in rural areas lacked healthy food options largely because storeowners perceived that their customers would not purchase healthier items and due to challenges with distribution. Conversely, studies reporting on small food stores in urban areas suggest challenges with transportation and safety concerns.
Conclusion
Research on small food stores is nascent and further research, especially intervention studies, is needed. Further, less evidence exists on healthy food access, in particular intervention testing on small food store research in rural areas.
Keywords: Hunger, Obesity, Community-based participatory research, Convenience foods
Highlights
-
•
We reviewed food environment literature and compared small store research in urban and rural settings.
-
•
We reviewed 19 manuscripts, the majority of which were in urban settings (n = 14).
-
•
The majority of the manuscripts reviewed were qualitative/descriptive (n = 14).
-
•
The few manuscripts that tested interventions (n = 5) were in urban settings.
1. Introduction
The food environment influences consumer food selection and health outcomes (Beaulac et al., 2009, Gustafson et al., 2013). Environmental and policy interventions that promote access to healthful choices may achieve the greatest benefits and broadest reach (Brennan et al., 2011, Frieden et al., 2010). Healthy food access is defined as having a wide variety of nutrient dense food options (e.g., fruits, vegetables, whole grains, low-fat dairy) available at a reasonable cost (Feenstra, 2002). Low access to healthful foods promotes reliance on pre-packaged foods (commonly nonperishable and energy-dense, nutrient-poor (EDNP) foods and beverages) (Moore et al., 2012).
Currently in the United States (U.S.), there are many geographic areas where access to healthful foods is low, commonly in limited resource communities with a greater proportion of racial/ethnic minority populations (Beaulac et al., 2009, Larson et al., 2009). Negative health outcomes and associations of access to EDNP foods have been well documented among urban areas (Kirkup et al., 2004, Lake and Townshend, 2006, Laska et al., 2010). More recently, research has demonstrated some of the unique challenges that rural areas face. These challenges include things such as a declining customer base, an increase in food store closures, aging ownership, and lack of available small business capital (Bailey, 2010, Bustillos et al., 2009, Kaufman et al., 1997, Liese et al., 2007, Yeager and Gatrell, 2014). Many rural residents travel long distances to reach the nearest food outlet (Bitto et al., 2003, Sharkey and Horel, 2008) and this issue is compounded by lack of public and/or individual transportation (Bitto et al., 2003, Sharkey and Horel, 2008).
Research on the food environment has also found that access to supermarkets may be associated with greater fruit and vegetable consumption (Franco et al., 2009, Larson et al., 2009, Rose and Richards, 2004), more affordable prices (Chung and Myers, 1999), and reduced BMI (Larson et al., 2009, Lopez, 2007). In addition, smaller grocery stores and corner stores (referred to as small food stores in the rest of the text) stocked with more healthful foods have been suggested as an alternative to improve healthful choices (Morton and Blanchard, 2007, Short et al., 2007). The distinction between urban and rural areas is particularly salient, since smaller and non-traditional food stores are more common in rural areas and tend to offer a smaller selection of more healthful foods than urban areas (Bustillos et al., 2009, Larson et al., 2009).
Several reviews exist that assess the relationship between access to less healthful foods and obesity-related outcomes (Beaulac et al., 2009, Caspi et al., 2012, Holsten, 2009, Papas et al., 2007). Specific to retail, previous reviews have largely summarized evidence-based research conducted in supermarkets and larger grocery stores (Escaron et al., 2013, Glanz et al., 2012, Glanz and Yaroch, 2004, Larson et al., 2009), as well as analyses of measurement tools (Gustafson et al., 2012, Kelly et al., 2011, Lytle, 2009, McKinnon et al., 2009, Sharkey, 2009). Other reviews have included small food stores, however, the geographic representation of the studies reviewed was largely urban-based (Gittelsohn et al., 2012) or tended to highlight specific challenges and characteristics of diverse populations (Gittelsohn and Sharma, 2009). The purpose of this review was to identify how rural and urban food access differs across small food stores and the types of research strategies and methodologies that have been applied in each setting.
2. Materials and Methods
An integrative review of this literature was conducted to understand the state of the science, critique research questions, find conceptual gaps, and determine the “best practices” for small food store interventions. One key utility of an integrative review is to bridge related areas of inquiry. Thus, an emphasis on comparing findings from urban and rural communities in the U.S. was carried out for this review. Counties outside of the U.S. were excluded from this review given varying policies and practice implications.
The review was conducted in Nebraska between January 2015 and May 2015. The criteria for inclusion of the studies were: (a) publication within the past ten years (May 2005–May 2015); (b) publication in the English language; (c) conducted in the U.S. with a clear delineation as to whether the research was urban and/or rural; and (d) and the study reported data or facilitated an intervention related to small food stores. Exclusion criteria for articles included: (a) measurement development study only; (b) unspecified geographic focus that limits ability to compare findings between urban and rural settings; and (c) assessment of multiple food outlets (e.g., restaurants, larger grocery stores). We did not define population density in a specific way, but rather, used the definitions and terms from the authors of the papers we reviewed to guide our decision as to whether there was a clear delineation of “urban” or “rural”.
Google Scholar, PubMed, and Web of Science were searched using the following key terms “corner store”, “convenience store”, “small store”, “bodega” AND “store-owner”, “manager”, “environment”, “food environment”, “availability”, “education”, “intervention” or “nutrition education.” The search process also included backward searches of cited articles. Titles, abstracts, and then full text were reviewed for inclusion after the initial search. The emphasis of this review was on small food stores, which included corner stores or convenience stores. In order to capture those papers that have a mixed focus (e.g., multiple store types), grocery stores were included in our initial searches, but papers were eliminated if they did not have some inclusion of corner stores or small stores (i.e., if small food stores were not the major focus of the paper, or at least equal in emphasis, they were eliminated).
A data extraction tool developed for the purpose of this study utilized the framework of Cooper (1998). Narrative synthesis methods were used to extract and summarize findings from multiple studies across urban and rural settings. The data extraction tool included the following categories: setting, constructs assessed, measurement tools used, methodology, location, rural versus urban, findings, implications for measurement, and intervention. Each full-text manuscript was independently reviewed by one of two coders (CAP, CBS) and then verified by a second author (CAP, CBS, SMH, or ALY). Inter-rater agreement was verified and multiple coders discussed any conflicts to reach consensus (Miller, 1999). Results for this small food store review are presented with urban-focused manuscripts first, rural-focused manuscripts, and followed by a comparison of rural and urban findings, each based on the type of study and methodology used.
3. Results
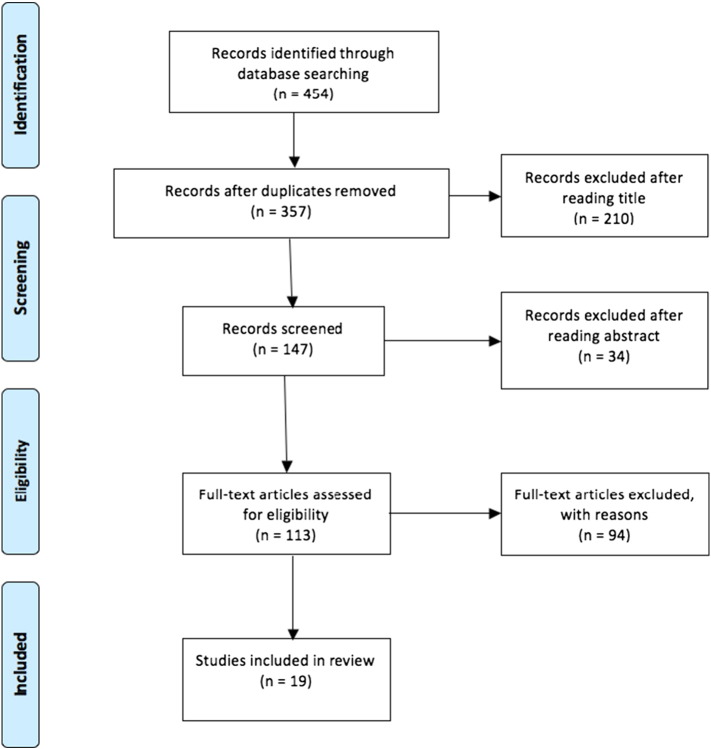
The initial database search retrieved 454 articles and 357 unique manuscripts. After reviewing titles, 210 manuscripts were eliminated, another 34 manuscripts were eliminated based on abstract, and the final 92 manuscripts were eliminated after reading the full article, resulting in a final inclusion of 19 manuscripts (see Fig. 1). The main reasons for exclusion that the study did not report evidence focusing on small food stores (n = 124) or provided evidence from research where the geographic focus was not clear (i.e., urban and/or rural) were difficult to delineate (n = 68) (other reasons, n = 146).
Fig. 1.
Evidence acquisition.
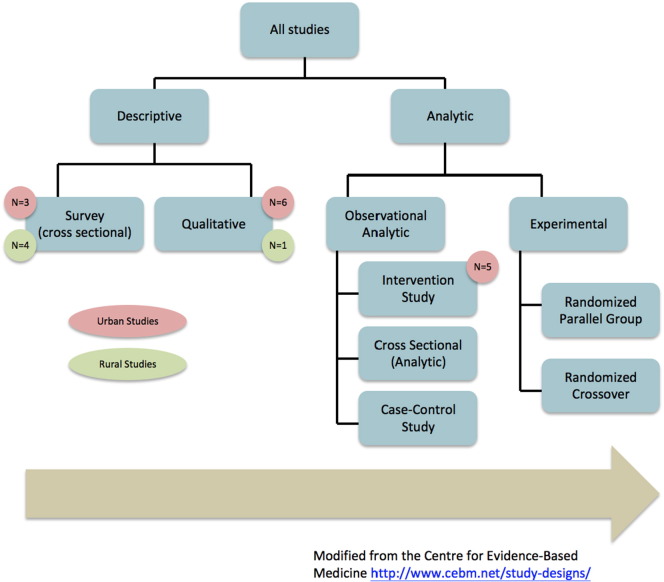
Of the 19 papers identified as eligible for review, five (26%) focused on rural settings, while 14 (74%) focused on urban settings. Fig. 2 describes the types of studies included in this review: eight (42%) utilized qualitative methodologies, six (32%) utilized descriptive or cross-sectional methodologies, and another five (26%) reported outcomes from an intervention study. All studies using intervention methodologies (n = 5; 26%) were focused in urban areas. Table 1 describes the key constructs, methodologies, and findings from each of the 19 papers reviewed and the table is summarized below.
Fig. 2.
Flow of evidence and study type.
Table 1.
Summary of literature reviewed.
| Reference (1st author, date) | City/town, state | Measurement method |
Constructs assessed and methodology used | Findings summary | ||
|---|---|---|---|---|---|---|
| Qualitative | Descriptive Cross Sectional | Intervention | ||||
| Urban studies | ||||||
| Lent et al. (2014) | Philadelphia, PA | X | Adult food purchases and dietary quality (intercept interviews). | Beverage purchases occurred during 66% of intercepts and accounted for 39% of all items. Regular soda was the most popular beverage purchase. Compared with children and adolescents, adults spent the most money and purchased the most energy. | ||
| Borradaile et al. (2009) | Philadelphia, PA | X | Child purchases at corner stores close to schools (intercept surveys about food purchases). | Most frequently purchased items were energy-dense, low-nutritive foods and beverages, such as chips, candy, and sugar-sweetened beverages. More calories came from foods than from beverages. | ||
| Cannuscio et al. (2010) | Philadelphia, PA | X | Production to consumption and health concerns of residents (photo-elicitation interviews). | 75% raised concerns regarding adverse health effects of food environment (“foodways”, production to consumption); 25% were concerned about dearth of supermarkets; other concerns included inaccessibility to public transit; discussions included: families and schoolchildren ritualizing trips to corner stores, feeling powerless to intervene, public alcohol consumption and safety concerns as barriers to grocery shopping, racial tensions between neighborhood residents and immigrant storeowners. | ||
| O′Malley et al. (2013) | New Orleans, LA | X | Food store type use and shopping patterns (customer intercept interviews), energy intake (24-h recalls), barriers to stocking (storeowner interviews), changes in delivery and products sold (wholesaler interviews). | Typical corner stores purchases were prepared foods and/or beverages, which accounted for 1/3 daily energy intake. Most individuals cited that they would purchase fresh fruit and vegetables from corner stores if available. Store operators identified cost, infrastructure and lack of customer demand as barriers. | ||
| Song et al. (2011) | Baltimore, MD | X | Motivating factors for program participation, barriers to program implementation, perceived effectiveness of intervention materials, and perceptions about the program (in-depth interviews with storeowners and follow-up survey). | Strong and moderate support storeowners were more likely to have an open store layout, good relationship with customers, and better healthy food stocking status at baseline compared to weak support storeowners. Perceived barriers included limited store space, less effective interventionists, and interruption of store business. | ||
| Sherman et al. (2015) | Philadelphia, PA | X | Elementary school age children have early experiences as corner store shoppers, how children select stores, reasons for shopping at corner stores, parental guidance about corner store shopping, and what children's ideal corner store would look like (focus groups with youth). | Children report going to corner stores with family members at an early age (1st grade). By 2nd/3rd grades, youth reported shopping unaccompanied. Products sold in stores were the key reason they choose a specific store. A few children cited their parents offering guidance on their corner store purchases. Children's dream corner store would include a combination of healthful and less healthful foods. | ||
| D'Angelo et al. (2011) | Baltimore, MD | X | Shopping patterns and consumer perceptions (Consumer Impact Questionnaire) access factors and travel time | Supermarkets and corner stores were the most common food outlets used. The choice of food source was related to frequency of obtaining less healthful foods. Corner store shoppers obtained more EDNP foods than people shopping at other outlets. Corner store shoppers purchased more sugary beverages and snacks (e.g., potato chips and pretzels) than supermarket shoppers. Corner store shoppers were more likely to walk as a form of transport. | ||
| Cavanaugh et al. (2013) | Philadelphia, PA | X | Food environment (availability of healthy foods, NEMS-S), store characteristics (SNAP, number of aisles, square footage, stores' conversion potential rating. | Healthy options across all of the categories were less available and more expensive. The number of aisles was positively associated with availability score. | ||
| Lucan et al. (2010) | Philadelphia, PA | X | Types of snack foods stocked by corner stores and their nutritional values (categorizing snack foods and assessing nutritional content). | Stores stocked 452 kinds of snacks, with only 15% of items common across three neighborhoods. Distribution in snack type did not vary. There were no fruit or vegetable snacks, only 4% of snacks were whole grain. | ||
| Paek et al. (2014) | Grand Rapids, MI | X | Food environment (availability of healthy foods, NEMS-S), perceived changes in store, branding awareness, purchasing patterns, dietary patterns (in-store customer survey). | Three intervention stores improved in healthful food availability as a result of the intervention. A significantly higher level of intervention awareness and monthly bean and nut consumption was reported post-intervention by the customers. | ||
| Gittelsohn et al. (2010) | Baltimore, MD | X | Process indicators (number of visitors, fliers, food samples and giveaways per visit). | Program achieved a moderate to high level of fidelity in terms of promoted food availability. Creative solutions for smaller scale print and display materials were developed to adapt to small space available. | ||
| Song et al. (2009) | Baltimore, MD | X | Storeowner perspective and psychosocial variables (Store Impact Questionnaire); changes in stock and foods promoted (food sales records, storeowner interviews). | During and post intervention, stocking of healthy foods and weekly reported sales of some promoted foods increased significantly in intervention stores. Intervention storeowners also showed higher self-efficacy for stocking some healthy foods. | ||
| Jetter and Cassady (2009) | Sacramento, CA | X | Sales, consumer use of products, observations (stocking). | Sales of fresh produce increased as a result of the intervention. By providing assistance to storeowners to cover the fixed costs of developing a fresh produce section, sufficient stock could be sold to cover variable costs of operating produce cases, such as stock, spoilage, and electricity. However, sales were not sufficient to cover management costs. | ||
| Freedman and Connors (2011) | San Jose, CA | X | Sales data from targeted items. | Sales of tagged items, as a percentage of total sales in the targeted items increased as a result of the intervention. | ||
| Rural studies | ||||||
| McGee et al. (2011) | Counties in Arkansas, Louisiana, and Mississippi | X | Factors affecting consumption of healthful foods; agreement between perceptions, behaviors, and ability to purchase healthful food; availability of healthful items. | Limited availability and perceived costs of healthful food in the target area influenced purchasing behaviors. Attitudes and perceptions should be incorporated into interventions in conjunction with increasing availability of healthful foods in rural areas. | ||
| Findholt et al. (2014) | Several counties in Oregon | X | Healthy snack availability (author developed checklist) and food outlet type (NAICS code). | Stores near high-income urban schools had higher availability, compared to stores near low-income schools. Stores near rural schools generally had the lowest availability. | ||
| Sharkey et al. (2013) | Texas Border Colonias | X | 1) Spatial access to food stores (ground-truthed methods computed using the distance from each participant's residence to each food store); 2) survey data (demographics, access to transportation, food purchasing habits, child independent food purchases, food assistance participation, food security); 3) household food inventories (presence and amount of food items in the home). | Children that independently purchased food from convenience stores tended to have greater availability of foods that were higher in energy and fat in their homes. Families that lived further from convenience stores had reduced availability of total energy. | ||
| Gustafson et al. (2014) | Webster and Woodford counties, KY | X | Food shopping patterns, behaviors, and dietary intake among adolescents and their parents. | Adolescents and parents typically shopped together (~ 60%). Parents and adolescents agreed that they ate fast food together, but had less agreement for purchasing food from convenience stores. Adolescents who purchased food from school vending, gas stations, and convenience stores often consumed more energy-dense, nutrient-poor foods. | ||
| Jilcott Pitts et al., 2013a, Jilcott Pitts et al., 2013b | Pitt County, NC | X | Healthy food availability (NEMS-S Revised). | Corner stores in rural areas had higher availability scores but similar price and quality scores than corner stores in urban areas. The availability and overall NEMS-S-Rev scores were slightly lower for corner stores in rural areas when corner stores in crossroads communities were excluded from the analysis. | ||
| Creel et al. (2008) | Six rural counties in the central Brazos Valley region of Texas | X | Food outlet type and entrée analysis. | Healthy options for all meals were significantly higher among fast food restaurants versus grocery and/or convenience stores. Supermarkets, however, did have a more varied selection than convenience stores. | ||
3.1. Summary of Findings — Urban
3.1.1. Qualitative
Several studies (n = 7) employed qualitative methodologies of various types including key informant interviews (O’Malley et al., 2013, Song et al., 2011), intercept interviews (Borradaile et al., 2009, Lent et al., 2014), focus groups (Sherman et al., 2015), and PhotoVoice (Cannuscio et al., 2010) to study small food stores in urban areas. The one study that utilized PhotoVoice, an analysis method that combines photography with qualitative evaluation to stimulate grassroots social action (Catalani and Minkler, 2010), conducted elicitation interviews to encourage participants to explore food access in their urban neighborhoods (Cannuscio et al., 2010). Concerns raised about urban food access to small food stores through the PhotoVoice process included: adverse health effects of food environment, dearth of supermarkets, inaccessibility to public transit (creating a dependence on corner stores), families and schoolchildren ritualizing trips to corner stores, feeling powerless to intervene, public alcohol consumption and safety concerns as barrier to grocery shopping, and racial tensions between neighborhood residents and immigrant storeowners (Cannuscio et al., 2010).
Two papers reported intercept interviews at baseline from a corner store initiative in Philadelphia (Borradaile et al., 2009, Lent et al., 2014). Among the adults and children interviewed (over 9000) regarding corner store purchases the most common items purchased included sugar-sweetened beverages, chips, prepared foods, candy, and pastries (Lent et al., 2014). Consequently, purchases made with one trip to the corner store yielded approximately one-third of total daily caloric intake (Lent et al., 2014). The second paper corroborated these findings with interviews among children in grades 4 through 6 at corner stores before and after school, revealing that the most frequently purchased items were energy dense nutrient poor (EDNP) foods (Borradaile et al., 2009).
Qualitative evidence has also informed feasibility of interventions in small food stores. O'Malley et al. (2013) conducted household interviews, corner store customer intercept interviews, and interviews with corner store operators to inform work with neighborhood corner stores to increase the availability of fresh fruits and vegetables in low-income urban environments (O'Malley et al., 2013). Those who shopped at corner stores typically purchased prepared foods and/or beverages, making up nearly one third of their daily energy intake. The authors found that most individuals would be likely to purchase fresh fruits and vegetables from corner stores if these foods were offered (O'Malley et al., 2013). Store operators identified cost, infrastructure, and lack of customer demand as major barriers to stocking more fresh produce (O'Malley et al., 2013). Similarly, in-depth interviews with Korean storeowners probed them to describe motivators and barriers to providing healthier food options in their stores (Song et al., 2011). Greater support from food storeowners for providing healthy food options was more likely when their stores had an open layout, they had a good relationship with customers, and storeowners had greater access to source more healthful food (Song et al., 2011). In addition, the storeowners reported that they were motivated to participate in the intervention because the author with the same cultural and ethnic background led the store recruitment (Song et al., 2011). Perceived barriers mainly included limited store space, perceived effectiveness of the intervention, and interruption of store business (Song et al., 2011). These findings can inform intervention strategies in small food stores that are most feasible and effective, tailored to the particular community, with consideration of both the consumer and the storeowners to promote further uptake.
The last qualitative urban-based study in this review included focus groups that were conducted with children, from kindergarten through 8th grade, to determine how and why these participants shopped at corner stores (Sherman et al., 2015). It was found that children started visiting corner stores with family members at an early age (1st grade), and that by 2nd or 3rd grade, they were shopping unaccompanied by an older sibling or adult (Sherman et al., 2015). Food purchased at the corner stores were used to supplement school meals and home food as well as provide a social outlet (Sherman et al., 2015). Youth described their “ideal” corner store as offering a combination of “healthy” and “less-healthy” foods (Sherman et al., 2015).
3.1.2. Descriptive and Cross-sectional Data
Data were used in a variety of ways to help characterize the urban food environment specific to corner stores. One study characterized shoppers who frequented corner stores utilizing the Consumer Impact Questionnaire and other items for understanding shopping patterns (D'Angelo et al., 2011). It was found that low-income inner city residents who visited corner stores shopped more frequently (i.e., daily), traveled shorter distances, tended to use walking as a mode of transportation, and reported purchasing significantly more EDNP foods when compared to supermarket shoppers (D'Angelo et al., 2011). Reasons given for shopping at corner stores included convenience, quality, cleanliness, good service, and being within walking distance (D'Angelo et al., 2011).
In one study, evaluation of food store characteristics showed that corner stores were perceived as “less healthy” and more expensive, when compared to full service grocery stores by consumers (Cavanaugh et al., 2013). In addition, a larger number of aisles were positively associated with improved availability of more healthful foods (Cavanaugh et al., 2013). Using focus groups and direct observation, another study identified stores that students were visiting and categorized snack foods that students were purchasing (Lucan et al., 2010). The lack of more healthful snack options and overabundance of pre-packaged snack foods at these corner stores was demonstrated, as there were no whole fruits or vegetables offered as snacks, and only 4% of all snacks were whole grain (Lucan et al., 2010). The lack of nutritional variety that exists in corner stores may be, in part, due to the fact that five of the 65 manufacturers that supplied the stores in the assessment neighborhoods accounted for nearly three quarter of all corner store snack food inventories (Lucan et al., 2010).
3.1.3. Outcomes From Intervention Studies
Much of the intervention research conducted in small food stores has utilized varying strategies aimed to increase the amount of more healthful foods stocked and sold to customers across the country (Dannefer et al., 2012, Sharkey et al., 2012, Song et al., 2009, Zenk et al., 2011). One study conducted surveys with customers and food environment assessments among intervention corner stores in an urban Michigan setting and found increased healthy food availability, awareness of the program by customers, and more healthful food consumption post-intervention (Paek et al., 2014). Similarly, Song et al. (2009) described that stores receiving interventions had higher likelihood for stocking more healthful foods, successfully promoted these foods, and showed higher self-efficacy for stocking these foods when compared to non-intervention stores (Song et al., 2009). Consumer demand for more healthful foods is necessary; however, there is also a need to concurrently build capacity at the store level. For example, it was demonstrated that the sales of fresh produce could cover the fixed costs of adding fresh produce (e.g., spoilage, produce cases), but not the added management costs (Jetter and Cassady, 2009). In addition, point-of-purchase (POP) information can help consumers make informed, healthful choices. One study provided POP information on food items at an on-campus convenience store and found that there was an increase in sales of the items that were promoted (Freedman and Connors, 2011).
From these studies, it appears that detailed process evaluation is essential for examining how well intervention approaches in food stores were implemented, and to determine best practices for further expanded studies. One study used a combination of interviews and observations to monitor program interventions and ultimately assess fidelity (Gittelsohn et al., 2010). The process evaluations helped identify high fidelity specific to branded materials (e.g., posters) in one study (Gittelsohn et al., 2010).
3.2. Summary of Findings — Rural
3.2.1. Qualitative
There were two rural-based qualitative studies included in this review. In one study, rural residents in the southern U.S. were asked about factors affecting consumption of more healthful foods, food purchasing behaviors, and the perceived availability of healthful items (McGee et al., 2011). One significant barrier to healthful eating was the distance to the market, in particular, for low- income, elderly, and rural residents (McGee et al., 2011). Many participants reported some nutritional knowledge, but also some misconceptions about foods that they considered healthful (McGee et al., 2011). The authors concluded that changes in healthful food access and ultimately consumption of healthful foods in rural areas will happen only through understanding and addressing the experiences, knowledge, and needs of the residents (McGee et al., 2011).
3.2.2. Descriptive and Cross-sectional Data
Findings from descriptive and cross-sectional studies on food access in rural areas have tended to characterize a food environment that greatly lacks availability of more healthful items that are also low in cost. In order to inform a future intervention to improve children's snacking habits, Findholt et al. (2014) conducted observations at stores surrounding schools in rural and urban Oregon (Findholt et al., 2014). Generally, they found that the availability of healthy snack foods and beverages was low in all stores, with stores near rural schools having the lowest availability (Findholt et al., 2014). As children mature, they typically have increased freedom and access to foods at corner stores. One study showed that households in which the child independently purchased food from a convenience store at least once a week consumed foods and beverages with higher amounts of EDNP foods (Sharkey et al., 2013).
The overall lack of availability and quality of more healthful food options in rural areas was identified through food store audits in rural Eastern North Carolina (Jilcott Pitts et al., 2013a). However, the authors acknowledged the challenge in collecting this type of data, as the storeowners may fear that the audit results will have negative repercussions. In rural Texas, there was a lack of healthy food options found at convenience stores, with fast food restaurants and supermarkets having more varied and healthful selections (Creel et al., 2008).
Adolescents from rural Ohio and Kentucky completed surveys about their food purchasing habits and dietary behaviors (Gustafson et al., 2014). It was found that close to 60% of adolescents reported grocery shopping with their parent and eating fast food together as a family (Gustafson et al., 2014). In addition, when adolescents were with their peers or parents at corner stores, the social influence resulted in purchase and consumption of higher sugar and calorically dense items (Gustafson et al., 2014). Finally, adolescents who purchased food from school vending, gas stations, and convenience stores combined often consumed more added sugars and sugar-sweetened beverages overall (Gustafson et al., 2014). Table 1 describes the key constructs, methodologies, and findings from each of the 19 papers reviewed and described above.
4. Discussion
To date, food access related research has been conducted largely among urban communities (Whelan et al., 2002, Wrigley et al., 2002), but more recently, attention has been given to the rural counterpart, where health disparities in food access also exist (Yeager and Gatrell, 2014, Yousefian et al., 2011). Our integrated review focused on small food stores in rural and urban settings and highlights the lack of studies conducted in rural settings, with over 70% of the 19 manuscripts reviewed conducted in urban settings. Specifically, rural populations experience greater burden of nutrition-related diseases (such as cardiovascular disease, type two diabetes), economic restrictions, and greater spatial inequality for access to healthful food when compared to urban populations (Jensen et al., 2003, Liese et al., 2007, Yeager and Gatrell, 2014). A recent study identified several potential areas of opportunity to help prioritize a research agenda for studying policies that address rural food access, and described the need for improved food retail systems that allow for a diversity of food retail options, including sufficient access to affordable small markets (Johnson et al., 2014).
Key findings highlighted in the current review of small food stores suggest that the challenges in urban communities stem from the lack of healthy food access among a plethora of unhealthy options, sometimes referred to as a “food swamp,” as well as safety concerns (Cannuscio et al., 2010). Many residents reported frequenting corner stores in urban areas to purchase EDNP foods (Borradaile et al., 2009, Lent et al., 2014). In comparison, the barriers to healthy food access in rural communities are typically associated with transportation issues and an overall lack of access to food outlets (McGee et al., 2011). Additionally, studies found a lack of healthy food options in rural stores (Gustafson et al., 2014, Jilcott Pitts et al., 2013a), largely because store-owners perceived that their customers would not purchase healthier items (Jilcott Pitts et al., 2013b). In one paper, both urban and rural stores were assessed, and it was found that the rural stores had the lowest healthy food availability (Findholt et al., 2014). Further work should be conducted focusing on food access issues in rural communities, and identifying distinctions and parallels are compared to urban settings in order to inform best practices in strategies.
Interestingly, of the six studies reporting on rural communities, none described findings from an intervention study. A few frameworks designate a hierarchy of evidence, and randomized controlled trials (RCTs) are often considered the most robust type of approach, while other forms of observational or single case studies frequently fall near the bottom of the hierarchy of evidence (Brownson et al., 2009, Daly et al., 2007, Ho et al., 2008, Popay and Roen, 2003). However, given the complexities of public health issues like food access in small food stores, consideration of study design alone is not adequate to grade the quality of evidence (Rychetnik et al., 2002). All of the studies conducted in rural settings were non-analytic, or descriptive, suggesting that food access research in urban settings has progressed further to include other analytic methods (Centre for Evidence-Based Medicine, 2014). Fig. 2 describes the breakdown of study types by first differentiating between descriptive and analytic study types. A non-analytic or descriptive study does not try to quantify the relationship but attempts to give us a snapshot of what is happening in a population (e.g., the prevalence, incidence, or experience of a group), which is an important base to build support for evidence-based approaches being implemented across rural communities. Previous reviews have highlighted the need for more interventions and longitudinal studies addressing purchasing habits, diet, and obesity outcomes related to neighborhood food store access (Gustafson et al., 2012); this gap is also relevant to the current review.
Recent studies conducted in Canada have also identified and measured food access in similar ways, using distance to the nearest food outlet as a proxy for food access (Apparicio et al., 2007, Larsen and Gilliland, 2008, Smoyer-Tomic et al., 2006). Although these papers have similarities to the ones reviewed in the current study, there are important policy and environmental differences between Canada and the U.S. with respect to small store interventions. For instance, in Canada, there is a different emphasis on food access than in the U.S. and the right to food in Canada is implicit within broader human rights, as reflected in the International Covenant on Economic, Social and Cultural Rights (acceded 1976). In addition, the emphasis on food sovereignty, in particular among first nations in Canada is a unique geopolitical conversation that is not in the forefront of dialogue in the U.S. (Desmarais and Wittman, 2014). A final notable difference between these two countries is that Healthy Food Financing Initiatives (HFFI) are prevalent throughout the U.S., and support healthy food businesses, often with federal funding; whereas, Canada does not have a parallel initiative (Holzman, 2010). Future studies may want to compare data on small stores from Canada and U.S. within the context of these differing and complex layers of policy, environment, and culture.
Given the complexities underscored in food access research, multi-pronged approaches are suggested (Cummins and Macintyre, 2006, Lucan and Mitra, 2011, Story et al., 2008). These approaches should reach beyond the addition of food outlets to include strategies that engage communities, such as interactive forms of nutrition education (e.g., cooking classes) (Blakely et al., 2011, Gittelsohn and Lee, 2013). One recommended practice is for communities to work together, creating solutions jointly (Campbell, 2004). This grassroots approach can help create “food citizens” that are fully engaged in the democratic process of changing the food system (Campbell, 2004). In order to maximize the impact of multi-pronged strategies to promote healthful eating in small food stores, consideration of affordability, traveling distance, and social norms should be explored further (Walker et al., 2010). For the largest impact, consumers, storeowners, and producers need to be represented in the research more, compared to existing literature that focuses on characterizing the food environment. Unique challenges exist among rural populations in accessing more healthful foods, which include longer distances to food outlets, higher prices, and limited quality of fresh fruits and vegetables (Dean and Sharkey, 2011). Competition with larger chains has forced many small food stores to close their doors, yet small food stores tend to be more accessible to the rural consumer than full service grocery stores, and should be considered within future community-based nutrition interventions (Connell et al., 2007).
This integrative review is not without limitations, as the findings described are mainly descriptive, in order to provide a broad examination of food access research among urban and rural communities. One issue was the lack of consistent outcome data and measurement protocols across studies, preventing a meta-analysis or other statistical comparisons of differences between urban and rural food environments. This is partially due to the emergent nature of this research, and heavy reliance on non-analytic, descriptive, and cross-sectional methodologies in the identified literature. Cross-sectional studies may not provide explicit information about cause-and-effect relationships since it is a single snapshot in time. Fig. 2 depicts that as the healthy food access evidence-base is built, more experimental studies should be conducted with a variety of methodological approaches. However, the nascence of this area of research calls for more exploratory, cross-sectional, and descriptive types of studies that we saw in this review. In addition, the validity and reliability of the methods utilized to assess the food environment have not been established, as these methods are still evolving. Further work in developing and testing methods for assessing rural and urban food environments is needed. The lack of focus on rural areas was still apparent, even with this acknowledgment of study design.
Strengths of this integrative review include being the first to characterize and attempt to disentangle factors related to small-store food access, comparing urban and rural settings. There were several important distinctions highlighted between urban and rural small-store settings to consider as the field continues to grow and to advance strategies to improve food access for various populations. In particular, there are implications for policy and environmental approaches for urban and rural settings. The unique barriers and characteristics of rural and urban communities will influence the effectiveness of strategies. Public health professionals and policymakers should be elucidated on the unique factors related to small food stores in both urban and rural areas as research progresses and the evidence base is developed. Successful interventions in these communities can ultimately shape policy and practice.
The authors declare that there is no conflict of interest.
References
- Apparicio P., Cloutier M.S., Shearmur R. The case of Montreal's missing food deserts: evaluation of accessibility to food supermarkets. Int. J. Health Geogr. 2007;6(1):4. doi: 10.1186/1476-072X-6-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey J. Center for Rural Affairs; Lyons, NE: 2010. Rural Grocery Stores: Importance and Challenges. (Retrieved from http://files.cfra.org/pdf/rural-grocery-stores.pdf) [Google Scholar]
- Beaulac J., Kristjansson E., Cummins S. A systematic review of food deserts, 1966–2007. Prev. Chronic Dis. 2009;6 [PMC free article] [PubMed] [Google Scholar]
- Bitto E.A., Morton L.W., Oakland M.J., Sand M. Grocery store access patterns in rural food deserts. J. Study Food Soc. 2003;6:35–48. [Google Scholar]
- Blakely T., Mhurchu C.N., Jiang Y. Do effects of price discounts and nutrition education on food purchases vary by ethnicity, income and education? Results from a randomised, controlled trial. J. Epidemiol. Community Health. 2011;65:902–908. doi: 10.1136/jech.2010.118588. [DOI] [PubMed] [Google Scholar]
- Borradaile K.E., Sherman S., Vander Veur S.S. Snacking in children: the role of urban corner stores. Pediatrics. 2009;124:1293–1298. doi: 10.1542/peds.2009-0964. [DOI] [PubMed] [Google Scholar]
- Brennan L., Castro S., Brownson R.C., Claus J., Orleans C.T. Accelerating evidence reviews and broadening evidence standards to identify effective, promising, and emerging policy and environmental strategies for prevention of childhood obesity. Annu. Rev. Public Health. 2011;32:199–223. doi: 10.1146/annurev-publhealth-031210-101206. [DOI] [PubMed] [Google Scholar]
- Brownson R.C., Fielding J.E., Maylahn C.A. Evidence-based public health: a fundamental concept for public health practice. Annu. Rev. Public Health. 2009;30:175–201. doi: 10.1146/annurev.publhealth.031308.100134. [DOI] [PubMed] [Google Scholar]
- Bustillos B., Sharkey J.R., Anding J., McIntosh A. Availability of more healthful food alternatives in traditional, convenience, and nontraditional types of food stores in two rural Texas Counties. J. Am. Diet. Assoc. 2009;109:883–889. doi: 10.1016/j.jada.2009.02.011. [DOI] [PubMed] [Google Scholar]
- Campbell M.C. Building a common table the role for planning in community food systems. J. Plan. Educ. Res. 2004;23:341–355. [Google Scholar]
- Cannuscio C.C., Weiss E.E., Asch D.A. The contribution of urban foodways to health disparities. J. Urban Health. 2010;87:381–393. doi: 10.1007/s11524-010-9441-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi C.E., Sorensen G., Subramanian S.V., Kawachi I. The local food environment and diet: a systematic review. Health Place. 2012;18:1172–1187. doi: 10.1016/j.healthplace.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catalani C., Minkler M. Photovoice: a review of the literature in health and public health. Health Educ. Behav. 2010;37:424–451. doi: 10.1177/1090198109342084. [DOI] [PubMed] [Google Scholar]
- Cavanaugh E., Mallya G., Brensinger C., Tierney A., Glanz K. Nutrition environments in corner stores in Philadelphia. Prev. Med. 2013;56:149–151. doi: 10.1016/j.ypmed.2012.12.007. [DOI] [PubMed] [Google Scholar]
- Centre for Evidence-Based Medicine 2014. http://www.cebm.net/study-designs/ Retrieved May 22, 2015, from.
- Chung C., Myers S.L. Do the poor pay more for food? An analysis of grocery store availability and food price disparities. J. Consum. Aff. 1999;33:276–296. [Google Scholar]
- Connell C.L., Yadrick M.K., Simpson P., Gossett J., McGee B.B., Bogle M.L. Food supply adequacy in the lower Mississippi Delta. J. Nutr. Educ. Behav. 2007;39:77–83. doi: 10.1016/j.jneb.2006.10.007. [DOI] [PubMed] [Google Scholar]
- Cooper H.M. vol. 2. Sage; 1998. Synthesizing Research: A Guide for Literature Reviews. [Google Scholar]
- Creel J.S., Sharkey J.R., McIntosh A., Anding J., Huber J.C. Availability of healthier options in traditional and nontraditional rural fast-food outlets. BMC Public Health. 2008;8:395. doi: 10.1186/1471-2458-8-395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummins S., Macintyre S. Food environments and obesity—neighbourhood or nation? Int. J. Epidemiol. 2006;35:100–104. doi: 10.1093/ije/dyi276. [DOI] [PubMed] [Google Scholar]
- D'Angelo H., Suratkar S., Song H.-J., Stauffer E., Gittelsohn J. Access to food source and food source use are associated with healthy and unhealthy food-purchasing behaviours among low-income African-American adults in Baltimore City. Public Health Nutr. 2011;14:1632–1639. doi: 10.1017/S1368980011000498. [DOI] [PubMed] [Google Scholar]
- Daly J., Willis K., Small R. A hierarchy of evidence for assessing qualitative health research. J. Clin. Epidemiol. 2007;60:43–49. doi: 10.1016/j.jclinepi.2006.03.014. [DOI] [PubMed] [Google Scholar]
- Dannefer R., Williams D.A., Baronberg S., Silver L. Healthy Bodegas: increasing and promoting healthy foods at corner stores in New York City. Am. J. Public Health. 2012;102:e27–e31. doi: 10.2105/AJPH.2011.300615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dean W.R., Sharkey J.R. Rural and urban differences in the associations between characteristics of the community food environment and fruit and vegetable intake. J. Nutr. Educ. Behav. 2011;43:426–433. doi: 10.1016/j.jneb.2010.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desmarais A.A., Wittman H. Farmers, foodies and first nations: getting to food sovereignty in Canada. J. Peasant Stud. 2014;41(6):1153–1173. [Google Scholar]
- Escaron A.L., Meinen A.M., Nitzke S.A., Martinez-Donate A.P. Peer reviewed: supermarket and grocery store-based interventions to promote healthful food choices and eating practices: a systematic review. Prev. Chronic Dis. 2013;10 doi: 10.5888/pcd10.120156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feenstra G. Creating space for sustainable food systems: lessons from the field. Agric. Hum. Values. 2002;19(2):99–106. [Google Scholar]
- Findholt N.E., Izumi B.T., Nguyen T., Pickus H., Chen Z. Availability of healthy snack foods and beverages in stores near high-income urban, low-income urban, and rural elementary and middle schools in Oregon. Child Obes. 2014;10:342–348. doi: 10.1089/chi.2014.0020. [DOI] [PubMed] [Google Scholar]
- Franco M., Diez-Roux A.V., Nettleton J.A. Availability of healthy foods and dietary patterns: the multi-ethnic study of Atherosclerosis. Am. J. Clin. Nutr. 2009;89:897–904. doi: 10.3945/ajcn.2008.26434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman M.R., Connors R. Point-of-purchase nutrition information influences food-purchasing behaviors of college students: a pilot study. J. Am. Diet. Assoc. 2011;111:S42–S46. doi: 10.1016/j.jada.2011.03.008. [DOI] [PubMed] [Google Scholar]
- Frieden T.R., Dietz W., Collins J. Reducing childhood obesity through policy change: acting now to prevent obesity. Health Aff. 2010;29:357–363. doi: 10.1377/hlthaff.2010.0039. [DOI] [PubMed] [Google Scholar]
- Gittelsohn J., Lee K. Integrating educational, environmental, and behavioral economic strategies may improve the effectiveness of obesity interventions. Appl. Econ. Perspect. Policy. 2013;35:52–68. [Google Scholar]
- Gittelsohn J., Sharma S. Physical, consumer, and social aspects of measuring the food environment among diverse low-income populations. Am. J. Prev. Med. 2009;36:S161–S165. doi: 10.1016/j.amepre.2009.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gittelsohn J., Suratkar S., Song H.-J. Process evaluation of Baltimore healthy stores: a pilot health intervention program with supermarkets and corner stores in Baltimore City. Health Promot. Pract. 2010;11:723–732. doi: 10.1177/1524839908329118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gittelsohn J., Rowan M., Gadhoke P. Interventions in small food stores to change the food environment, improve diet, and reduce risk of chronic disease. Prev. Chronic Dis. 2012;9 [PMC free article] [PubMed] [Google Scholar]
- Glanz K., Yaroch A.L. Strategies for increasing fruit and vegetable intake in grocery stores and communities: policy, pricing, and environmental change. Prev. Med. 2004;39:75–80. doi: 10.1016/j.ypmed.2004.01.004. [DOI] [PubMed] [Google Scholar]
- Glanz K., Bader M.D.M., Iyer S. Retail grocery store marketing strategies and obesity: an integrative review. Am. J. Prev. Med. 2012;42:503–512. doi: 10.1016/j.amepre.2012.01.013. [DOI] [PubMed] [Google Scholar]
- Gustafson A., Hankins S., Jilcott S. Measures of the consumer food store environment: a systematic review of the evidence 2000–2011. J. Community Health. 2012;37:897–911. doi: 10.1007/s10900-011-9524-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson A., Christian J.W., Lewis S., Moore K., Jilcott S. Food venue choice, consumer food environment, but not food venue availability within daily travel patterns are associated with dietary intake among adults, Lexington Kentucky 2011. Nutr. J. 2013;12:17. doi: 10.1186/1475-2891-12-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson A., Wu Q., Spees C. How adolescents and parents food shopping patterns and social interaction when shopping is associated with dietary outcomes in rural communities. J. Obes. Weight Loss Ther. 2014;4:214. [Google Scholar]
- Ho P.M., Peterson P.N., Masoudi F.A. Evaluating the evidence is there a rigid hierarchy? Circulation. 2008;118:1675–1684. doi: 10.1161/CIRCULATIONAHA.107.721357. [DOI] [PubMed] [Google Scholar]
- Holsten J.E. Obesity and the community food environment: a systematic review. Public Health Nutr. 2009;12:397–405. doi: 10.1017/S1368980008002267. [DOI] [PubMed] [Google Scholar]
- Holzman D.C. Diet and nutrition: White House proposes healthy food financing initiative. Environ. Health Perspect. 2010;118(4):A156. doi: 10.1289/ehp.118-a156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen L., McLaughlin D.K., Slack T. Challenges for Rural America in the Twenty-first Century. 2003. Rural poverty: the persisting challenge; pp. 118–131. [Google Scholar]
- Jetter K.M., Cassady D.L. Increasing fresh fruit and vegetable availability in a low-income neighborhood convenience store: a pilot study. Health Promot. Pract. 2009;11:694–702. doi: 10.1177/1524839908330808. [DOI] [PubMed] [Google Scholar]
- Jilcott Pitts S.B., Bringolf K.R., Lawton K.K. Peer reviewed: formative evaluation for a healthy corner store initiative in Pitt County, North Carolina: assessing the rural food environment, part 1. Prev. Chronic Dis. 2013;10 doi: 10.5888/pcd10.120318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jilcott Pitts S.B., Bringolf K.R., Lloyd C.L., McGuirt J.T., Lawton K.K., Morgan J. Peer reviewed: formative evaluation for a healthy corner store initiative in Pitt County, North Carolina: engaging stakeholders for a healthy corner store initiative, part 2. Prev. Chronic Dis. 2013;10 doi: 10.5888/pcd10.120319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson D.B., Quinn E., Sitaker M. Developing an agenda for research about policies to improve access to healthy foods in rural communities: a concept mapping study. BMC Public Health. 2014;14:592. doi: 10.1186/1471-2458-14-592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman P.R., MacDonald J.M., Lutz S.M., Smallwood D.M. Agricultural Economics Reports No. 34065. United States Department of Agriculture, Economic Research Service; 1997. Do the poor pay more for food? Item selection and price differences affect low-income household food costs. (Retrieved from http://econpapers.repec.org/paper/agsuerser/34065.htm) [Google Scholar]
- Kelly B., Flood V.M., Yeatman H. Measuring local food environments: an overview of available methods and measures. Health Place. 2011;17:1284–1293. doi: 10.1016/j.healthplace.2011.08.014. [DOI] [PubMed] [Google Scholar]
- Kirkup M., Kervenoael R.D., Hallsworth A., Clarke I., Jackson P., del Aguila R.P. Inequalities in retail choice: exploring consumer experiences in suburban neighbourhoods. Int. J. Retail Distrib. Manag. 2004;32:511–522. [Google Scholar]
- Lake A., Townshend T. Obesogenic environments: exploring the built and food environments. J. R. Soc. Promot. Heal. 2006;126:262–267. doi: 10.1177/1466424006070487. [DOI] [PubMed] [Google Scholar]
- Larsen K., Gilliland J. Mapping the evolution of ‘food deserts’ in a Canadian city: supermarket accessibility in London, Ontario, 1961–2005. Int. J. Health Geogr. 2008;7(1):16. doi: 10.1186/1476-072X-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson N.I., Story M.T., Nelson M.C. Neighborhood environments: disparities in access to healthy foods in the U.S. Am. J. Prev. Med. 2009;36:74–81. doi: 10.1016/j.amepre.2008.09.025. [DOI] [PubMed] [Google Scholar]
- Laska M.N., Borradaile K.E., Tester J., Foster G.D., Gittelsohn J. Healthy food availability in small urban food stores: a comparison of four US cities. Public Health Nutr. 2010;13:1031–1035. doi: 10.1017/S1368980009992771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lent M.R., Vander Veur S., Mallya G. Corner store purchases made by adults, adolescents and children: items, nutritional characteristics and amount spent. Public Health Nutr. 2014;18:1706–1712. doi: 10.1017/S1368980014001670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liese A.D., Weis K.E., Pluto D., Smith E., Lawson A. Food store types, availability, and cost of foods in a rural environment. J. Am. Diet. Assoc. 2007;107:1916–1923. doi: 10.1016/j.jada.2007.08.012. [DOI] [PubMed] [Google Scholar]
- Lopez R.P. Neighborhood risk factors for obesity. Obesity. 2007;15(8):2111–2119. doi: 10.1038/oby.2007.251. [DOI] [PubMed] [Google Scholar]
- Lucan S.C., Mitra N. Perceptions of the food environment are associated with fast-food (not fruit-and-vegetable) consumption: findings from multi-level models. Int. J. Public Health. 2011;57:599–608. doi: 10.1007/s00038-011-0276-2. [DOI] [PubMed] [Google Scholar]
- Lucan S.C., Karpyn A., Sherman S. Storing empty calories and chronic disease risk: snack-food products, nutritive content, and manufacturers in Philadelphia corner stores. J. Urban Health. 2010;87:394–409. doi: 10.1007/s11524-010-9453-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lytle L.A. Measuring the food environment: state of the science. Am. J. Prev. Med. 2009;36:S134–S144. doi: 10.1016/j.amepre.2009.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGee B.B., Johnson G.S., Yadrick M.K. Food shopping perceptions, behaviors, and ability to purchase healthful food items in the lower Mississippi delta. J. Nutr. Educ. Behav. 2011;43:339–348. doi: 10.1016/j.jneb.2010.10.007. [DOI] [PubMed] [Google Scholar]
- McKinnon R.A., Reedy J., Morrissette M.A., Lytle L.A., Yaroch A.L. Measures of the food environment: a compilation of the literature, 1990–2007. Am. J. Prev. Med. 2009;36:S124–S133. doi: 10.1016/j.amepre.2009.01.012. [DOI] [PubMed] [Google Scholar]
- Miller W.L. vol. 3. Sage; 1999. Doing Qualitative Research. [Google Scholar]
- Moore L.V., Roux A.V.D., Franco M. Measuring availability of healthy foods: agreement between directly measured and self-reported data. Am. J. Epidemiol. 2012 doi: 10.1093/aje/kwr445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morton L., Blanchard T. Starved for access: life in rural America's food deserts. Rural Realities. 2007;1:1–10. [Google Scholar]
- O'Malley K., Gustat J., Rice J., Johnson C.C. Feasibility of increasing access to healthy foods in neighborhood corner stores. J. Community Health. 2013:1–9. doi: 10.1007/s10900-013-9673-1. [DOI] [PubMed] [Google Scholar]
- Paek H.-J., Oh H.J., Jung Y. Assessment of a healthy corner store program (FIT store) in low-income, urban, and ethnically diverse neighborhoods in Michigan. Fam. Community Health. 2014;37:86–99. doi: 10.1097/FCH.0000000000000014. [DOI] [PubMed] [Google Scholar]
- Papas M.A., Alberg A.J., Ewing R., Helzlsouer K.J., Gary T.L., Klassen A.C. The built environment and obesity. Epidemiol. Rev. 2007;29:129–143. doi: 10.1093/epirev/mxm009. [DOI] [PubMed] [Google Scholar]
- Popay J., Roen K. Joanna Briggs Institute; 2003. Synthesis of Evidence From Research Using Diverse Study Designs: A Review of Selected Methodological Work. [Google Scholar]
- Rose D., Richards R. Food store access and household fruit and vegetable use among participants in the US Food Stamp Program. Public Health Nutr. 2004;7:1081–1088. doi: 10.1079/PHN2004648. [DOI] [PubMed] [Google Scholar]
- Rychetnik L., Frommer M., Hawe P., Shiell A. Criteria for evaluating evidence on public health interventions. J. Epidemiol. Community Health. 2002;56:119–127. doi: 10.1136/jech.56.2.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharkey J.R. Measuring potential access to food stores and food-service places in rural areas in the U.S. Am. J. Prev. Med. 2009;36:S151–S155. doi: 10.1016/j.amepre.2009.01.004. [DOI] [PubMed] [Google Scholar]
- Sharkey J.R., Horel S. Neighborhood socioeconomic deprivation and minority composition are associated with better potential spatial access to the ground-truthed food environment in a large rural area. J. Nutr. 2008;138:620–627. doi: 10.1093/jn/138.3.620. [DOI] [PubMed] [Google Scholar]
- Sharkey J.R., Dean W.R., Nalty C. Convenience stores and the marketing of foods and beverages through product assortment. Am. J. Prev. Med. 2012;43:S109–S115. doi: 10.1016/j.amepre.2012.05.012. [DOI] [PubMed] [Google Scholar]
- Sharkey J.R., Dean W.R., Nalty C.C., Xu J. Convenience stores are the key food environment influence on nutrients available from household food supplies in Texas Border Colonias. BMC Public Health. 2013;13:45. doi: 10.1186/1471-2458-13-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman S., Grode G., McCoy T. Corner stores: the perspective of urban youth. J. Acad. Nutr. Diet. 2015;115:242–248. doi: 10.1016/j.jand.2014.10.017. [DOI] [PubMed] [Google Scholar]
- Short A., Guthman J., Raskin S. Food deserts, oases, or mirages? Small markets and community food security in the San Francisco Bay Area. J. Plan. Educ. Res. 2007;26:352–364. [Google Scholar]
- Smoyer-Tomic K.E., Spence J.C., Amrhein C. Food deserts in the prairies? Supermarket accessibility and neighborhood need in Edmonton, Canada. Prof. Geogr. 2006;58(3):307–326. [Google Scholar]
- Song H.-J., Gittelsohn J., Kim M., Suratkar S., Sharma S., Anliker J. A corner store intervention in a low-income urban community is associated with increased availability and sales of some healthy foods. Public Health Nutr. 2009;12:2060–2067. doi: 10.1017/S1368980009005242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song H.-J., Gittelsohn J., Kim M., Suratkar S., Sharma S., Anliker J. Korean American storeowners' perceived barriers and motivators for implementing a corner store-based program. Health Promot. Pract. 2011;12:472–482. doi: 10.1177/1524839910364369. [DOI] [PubMed] [Google Scholar]
- Story M., Kaphingst K.M., Robinson-O'Brien R., Glanz K. Creating healthy food and eating environments: policy and environmental approaches. Annu. Rev. Public Health. 2008;29:253–272. doi: 10.1146/annurev.publhealth.29.020907.090926. [DOI] [PubMed] [Google Scholar]
- Walker R.E., Keane C.R., Burke J.G. Disparities and access to healthy food in the United States: a review of food deserts literature. Health Place. 2010;16:876–884. doi: 10.1016/j.healthplace.2010.04.013. [DOI] [PubMed] [Google Scholar]
- Whelan A., Wrigley N., Warm D., Cannings E. Life in a “Food Desert.”. Urban Stud. 2002;39:2083–2100. [Google Scholar]
- Wrigley N., Warm D., Margetts B., Whelan A. Assessing the impact of improved retail access on diet in a “Food Desert”: a preliminary report. Urban Stud. 2002;39:2061–2082. [Google Scholar]
- Yeager C.D., Gatrell J.D. Rural food accessibility: an analysis of travel impedance and the risk of potential grocery closures. Appl. Geogr. 2014;53:1–10. [Google Scholar]
- Yousefian A., Leighton A., Fox K., Hartley D. Understanding the rural food environment—perspectives of low-income parents. Rural Remote Health. 2011;11:1631. [PubMed] [Google Scholar]
- Zenk S.N., Odoms-Young A.M., Dallas C. “You have to hunt for the fruits, the vegetables”: environmental barriers and adaptive strategies to acquire food in a low-income African American neighborhood. Health Educ. Behav. 2011;38:282–292. doi: 10.1177/1090198110372877. [DOI] [PMC free article] [PubMed] [Google Scholar]