Abstract
This MRI study explores the individual variation of the rotational axes of the distal femur, and investigate the relationship of this variation with overall coronal alignment in the osteoarthritic knee,The mean surgical epicondylar axis (SEA) was 1.7°, anatomical epicondylar axis (AEA) 5.6° and AP trochlea axis (APA) 94.3° external rotation, compared to the posterior condylar line. Investigating this relationship between different coronal alignment groups, there were statistically significant differences between excessive varus and excessive valgus knees for SEA (0.9:3.0 p < 0.001) and AEA (4.7:7.0 p < 0.001). There was no statistical difference for APA (93.9:95.3 p = 0.238).
Keywords: Total knee replacement, Rotational alignment, Osteoarthritis, MRI
1. Introduction
Successful total knee arthroplasty requires the femoral component to be accurately positioned in the axial plane. This is commonly referred to as the rotational alignment.
Several studies have demonstrated that femoral component rotation affects flexion stability, patellofemoral and tibiofemoral kinematics, and alignment in flexion. Both, excessive internal rotation and excessive external rotation, result in poor outcomes.1, 2, 3, 4, 5
The frequently used methods of obtaining correct positioning of the femoral component utilize the surface-derived landmarks of the distal femur, including a line either perpendicular to the AP trochlea axis (Whitesides line),6 3° externally rotated relative to the posterior condylar line,7 or parallel to the transepicondylar axis.8, 9 Traditional instrumentation for a total knee replacement (TKR), using matched resection technique, sets the femoral rotation routinely 3° externally rotated to the posterior condylar line.
Numerous studies have investigated the relationship between these commonly used rotational axes of the knee.8, 10, 11, 12 Victor's paper from 200911 presented a comprehensive review of published papers describing rotational alignment of the distal femur. In summarizing, they reported the following mean angular relationships between the axes of the knee: the posterior condylar line is on average 3° internally rotated to the surgical epicondylar axis; 5° internally rotated to the anatomical transepicondylar axis; and 4° relative to the perpendicular to the trochlear anteroposterior axis.
More recently, studies have identified a wide variability in this relationship and one that may be linked to overall coronal alignment.13, 14, 15 This study aims to use magnetic resonance imaging (MRI) to define the individual variation of the commonly used rotational axes of the distal femur and investigate the relationship of this variation with overall coronal alignment in the osteoarthritic knee.
2. Methods
We reviewed one hundred and twenty-six preoperative knee MRI scans taken between 2010 and 2014. All patients had osteoarthritis and were awaiting total knee replacement. The MRI scans were taken in conjunction with a Patient-Specific Instrumentation (PSI) protocol (Visionaire, Smith & Nephew, Memphis).
The MRI scans were taken using a Siemens Espree 1.5T scanner. Patients were placed supine with their knee in extension and stabilized in a knee holder. The knee was imaged perpendicular to the joint line from the superior aspect of the patella to the fibula head. Patients all had an axial scan with 2 mm slices. Images were imported into a dicom viewer (Osirix version 6.5) for analysis.
A method was developed on the OsiriX program, using the axial images to determine the posterior condylar line (PCL), the surgical epicondylar axis (SEA), the anatomical epicondylar axis (AEA), and the AP trochlea axis (APA). This required scrolling through the axial images to find which axial slice best defined each of the landmark points. These points were then transposed onto a single axial slice, to allow each axis to be defined, and the relative angular relationship between them to be measured (Fig. 1). Each of SEA, AEA, and APA were measured and recorded relative to the posterior condylar line. Two surgeons reviewed all 126 scans. To assess both intra- and interobserver reliability, one of the surgeons repeated the measurements after a three-week interval.
Fig. 1.

Measuring axes on MRI image.
The patient's standing long leg radiographs were used to determine their overall mechanical alignment as part of the preoperative PSI plan. Using the methods described by Paley,16 the femoral mechanical axis and the tibia mechanical axis were identified and then the Hip Knee Angle (HKA) was defined. The patients were then subdivided into three categories, excessive varus – defined as >6° varus, neutral – between 6° varus and 6° valgus, and excessive valgus – >6° valgus.
We determined the overall mean of the angular variation of each of SEA, AEA, and APA relative to the PCL. We then compared the means in each of the varus, neutral, and valgus-aligned knees.
2.1. Statistical analysis
The data were analyzed using ANOVA for testing between the groups utilizing least significant difference (LSD) post hoc testing. Homogeneity of variance was confirmed using Levene's statistic. Interobserver and intraobserver reliability were assessed using the intraclass correlation coefficient (ICC), two-way random effects model for consistency. ICC levels were classified as poor 0–0.2; fair 0.3–0.4; moderate 0.5–0.6; strong 0.7–0.8 and excellent >0.8.
3. Results
One hundred and twenty-six knee MRI scans were reviewed. There were 87 varus (>0°) and 39 valgus (<0°) knees. The excessive alignment groups numbered 50 (excessive varus > 6°), 60 (neutral −6° > 6°), and 16 (excessive valgus < −6°).
Excellent levels of interobserver and intraobserver reliability were measured as for the SEA and AEA (Table 1, Table 2), but measuring the APA was less consistent (Table 1, Table 2).
Table 1.
Interobserver reliability.
| Measure | ICC (95% CI) | Rated |
|---|---|---|
| SEA | 0.83 (0.76–0.88) | Excellent |
| AEA | 0.85 (0.79–0.89) | Excellent |
| APA | 0.63 (0.47–0.74) | Moderate |
Table 2.
Intraobserver reliability.
| Measure | ICC (95% CI) | Rated |
|---|---|---|
| SEA | 0.96 (0.94–0.97) | Excellent |
| AEA | 0.98 (0.98–0.99) | Excellent |
| APA | 0.29 (−0.02 to 0.50) | Poor |
Reviewing initially the entire study group, relative to the posterior condylar line, the mean SEA was 1.7° (95% CI 1.3–2.0), AEA 5.6° (95% CI 5.2–5.9), and APA 94.3° (95% CI 93.8–94.8) externally rotated (Table 3).
Table 3.
Average (95% CI) angular relationships compared to posterior condylar line and alteration with coronal alignment.
| Measure | Mean overall | Excessive valgus | Neutral | Excessive varus | p-Value |
|---|---|---|---|---|---|
| SEA | 1.7 (1.3–2.0) | 3.0 (2.0–4.1) | 2.0 (1.4–2.5) | 0.9 (0.4–1.4) | p < 0.001 |
| AEA | 5.6 (5.2–5.9) | 7.0 (5.8–8.1) | 5.9 (5.3–6.5) | 4.7 (4.2–5.2) | p < 0.001 |
| APA | 94.3 (93.8–94.8) | 95.3 (93.3–97.2) | 94.4 (93.7–95.1) | 93.9 (93.1–94.7) | p = 0.238 |
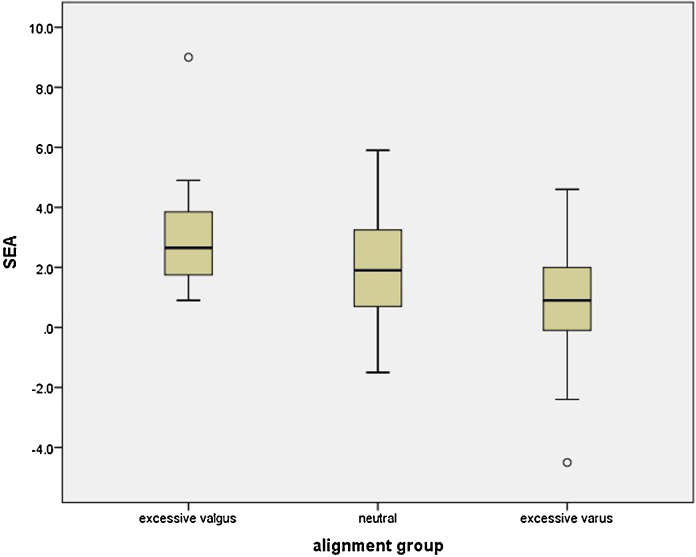
Dividing into excessive alignment groups, there were statistically significant differences in the SEA between both the excessive varus and excessive valgus (means of 0.9° vs 3.0°, p < 0.001 groups, Fig. 2) and AEA between the excessive varus and excessive valgus (means of 4.7° vs 7.0°, p < 0.001) groups (Fig. 3). There was no statistical difference in the AP trochlea axis between the groups (Table 3).
Fig. 2.
Comparison of SEA with differing alignment groups.
Fig. 3.
Comparison of AEA with differing alignment groups.
4. Discussion
An understanding of distal femoral geometry is a crucial element in establishing correct rotation for the femoral component in total knee arthroplasty. Whilst the determination of what is the “desired axis” remains a subject of ongoing debate, and any complete rotational discussion should recognize the dependent connection between the femur and the tibia, the consideration of the relationship between the surface-derived landmarks that contribute to positioning of the femoral component will always be fundamental.
Numerous studies have investigated the relationship between the commonly used rotational axes of the knee.8, 10, 11, 12 In a CT-based kinematic cadaver study from 2009,12 Victor et al. used the dependent relationship between the transverse axis of the femur and tibia to explore the true, three-dimensional, rotational axis of the knee and found that of all the surface-derived landmarks, the SEA had the closest relationship to this “femoral transverse” 3D axis.
The concept of axial geometry differing with varying coronal alignment was introduced by Matsuda in 200413 and further explored by Aglietti et al. in 200814 when they observed a linear relationship between the posterior condylar angle (PCA), the angle between the posterior condylar line and the transepicondylar axis, and coronal deformity. From varus to valgus, with every 10° change in coronal deformity, the PCA increased by 1°.
The advent of advanced imaging studies and subsequent introduction of patient-specific instrumentation has improved our ability to study these axes and appreciate variability in patient anatomy. Tan et al. in 200617 attempted to measure the relationship between rotational axes on a single 5-mm cut MRI image, but found it not to be accurate enough because no single image satisfactorily positioned the landmarks.
Luyckx et al. in 201215 reviewed 231 preoperative CT scans in patients with osteoarthritis and concluded that on average the PCL was only 1.6° internal rotation (IR) relative to the SEA. They identified a statistically significant difference in the relationship in different coronal plane alignments – 1.0° in the varus knee, 2.1° in the neutral knee, and 2.6° in the valgus knee. They reported that “for every 1° in coronal alignment increment from varus to valgus, there is a 0.1° increment in posterior condylar angle (PCL vs SEA).”
The results of our MRI-based study correlate well with the Luyckx CT study15 in recognizing that there is a relationship between rotational and coronal alignment. We found a significant difference in the surgical and anatomical epicondylar axes compared to the posterior condylar line in the excessively varus (mean 0.9°) and excessively valgus (mean 3.0°) arthritic knees. Our data also exposed the trend of increasing external rotation progressing from varus to valgus.
These studies in combination suggest that aiming for a standard 3° ER relative to the posterior condylar line may produce significant alignment errors in many knees. In our series, if the surgeon aimed for 3° ER and accepted between 1° and 5° ER, the outcome would have been correct only 59% of the time. Surgeons are traditionally more wary of this relationship in the valgus knee; however, we suggest that this angular relationship being 0.9° in the excessively varus knee might be an unexpected finding for many surgeons.
Our study had excellent intra- and interobserver reliability for assessment of both the surgical and anatomical epicondylar axis compared to the posterior condylar line, but moderate and poor reliability for the AP trochlea axis. In practice, determining this axis is particularly difficult in the hypoplastic trochlea and highlights the difficulty on relying solely on this marker during knee arthroplasty. Park et al.18 also studied rotational landmarks on MRI and reported good interobserver and intraobserver reliability in determining the posterior condylar angle. Other studies have reported wide variability in the AP trochlea axis with many outliers and lower interobserver reliability.5, 19
The use of the MRI scan to determine anatomical landmarks and measure axes provides the advantage of utilizing the chondral surface and theoretically a more life-like model. Matsuda et al.13 used MRI and the articular boundaries of the femoral condyles for the posterior condylar line and concluded that there was “no hypoplasia of the medial femoral condyle in the varus knees, but the lateral condyle in the valgus knees was significantly distorted”. Howell20 in 2010, however, in their MRI study concluded that there was clinically no asymmetry between the medial and lateral femoral condyles in the arthritic varus and valgus knee.
Intraoperative determination of landmarks is inherently difficult and prone to error.21, 22 It is unreasonable to suggest that this can be accurately established to fractions of degrees, but understanding what measurement is ideal is imperative. As described by Victor in 2009,12 individual variability in the angular relation between the desired axis and the surgical axis is one of the common sources of error in establishing femoral alignment in total knee arthroplasty. This variability has been highlighted in our study as well as many others.14, 15, 18, 23, 24, 25
5. Conclusion
Coronal alignment and axial rotational alignment are related in the osteoarthritic knee. There is a statistically significant difference in the relationship between both the surgical epicondylar axis and the anatomical epicondylar axis, and the posterior condylar line with changing coronal alignment. The average surgical epicondylar axis is 1.7° externally rotated relative to the posterior condylar line, 0.9° in the excessively varus knee and 3.0° in the excessively valgus knee. The average anatomical epicondylar axis is 5.6° externally rotated relative to the posterior condylar line, 4.7° in the excessively varus knee and 7.0° in the excessively valgus knee. Not considering these relationships may produce alignment errors in total knee replacement.
Conflict of interest
The authors have none to declare.
References
- 1.Merican A.M., Ghosh K.M., Iranpour F., Deehan D.J., Amis A.A. The effect of femoral component rotation on the kinematics of the tibiofemoral and patellofemoral joints after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2011;19(9):1479–1487. doi: 10.1007/s00167-011-1499-8. [DOI] [PubMed] [Google Scholar]
- 2.Berger R.A., Crossett L.S., Jacobs J.J., Rubash H.E. Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res. 1998;356:144–153. doi: 10.1097/00003086-199811000-00021. [DOI] [PubMed] [Google Scholar]
- 3.Fehring T.K. Rotational malalignment of the femoral component in total knee arthroplasty. Clin Orthop Relat Res. 2000;380:72–79. doi: 10.1097/00003086-200011000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Bell S.W., Young P., Drury C. Component rotational alignment in unexplained painful primary total knee arthroplasty. Knee. 2014;21(1):272–277. doi: 10.1016/j.knee.2012.09.011. [DOI] [PubMed] [Google Scholar]
- 5.Uehara K., Kadoya Y., Kobayashi A., Ohashi H., Yamano Y. Bone anatomy and rotational alignment in total knee arthroplasty. Clin Orthop Relat Res. 2002;402:196–201. doi: 10.1097/00003086-200209000-00018. [DOI] [PubMed] [Google Scholar]
- 6.Whiteside L.A., Arima J. The anteroposterior axis for femoral rotational alignment in valgus total knee arthroplasty. Clin Orthop Relat Res. 1995;321:168–172. [PubMed] [Google Scholar]
- 7.Siston R.A., Patel J.J., Goodman S.B., Delp S.L., Giori N.J. The variability of femoral rotational alignment in total knee arthroplasty. J Bone Joint Surg Am. 2005;87(10):2276–2280. doi: 10.2106/JBJS.D.02945. [DOI] [PubMed] [Google Scholar]
- 8.Berger R.A., Rubash H.E., Seel M.J., Thompson W.H., Crossett L.S. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res. 1993;286:40–47. [PubMed] [Google Scholar]
- 9.Katz M.A., Beck T.D., Silber J.S., Seldes R.M., Lotke P.A. Determining femoral rotational alignment in total knee arthroplasty: reliability of techniques. J Arthroplasty. 2001;16(3):301–305. doi: 10.1054/arth.2001.21456. [DOI] [PubMed] [Google Scholar]
- 10.Yoshino N., Takai S., Ohtsuki Y., Hirasawa Y. Computed tomography measurement of the surgical and clinical transepicondylar axis of the distal femur in osteoarthritic knees. J Arthroplasty. 2001;16(4):493–497. doi: 10.1054/arth.2001.23621. [DOI] [PubMed] [Google Scholar]
- 11.Victor J. Rotational alignment of the distal femur: a literature review. Orthop Traumatol Surg Res. 2009;95(5):365–372. doi: 10.1016/j.otsr.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 12.Victor J., Van Doninck D., Labey L., Van Glabbeek F., Parizel P., Bellemans J. A common reference frame for describing rotation of the distal femur: a CT-based kinematic study using cadavers. J Bone Joint Surg Br. 2009;91(5):683–690. doi: 10.1302/0301-620X.91B5.21827. [DOI] [PubMed] [Google Scholar]
- 13.Matsuda S., Miura H., Nagamine R. Anatomical analysis of the femoral condyle in normal and osteoarthritic knees. J Orthop Res. 2004;22(1):104–109. doi: 10.1016/S0736-0266(03)00134-7. [DOI] [PubMed] [Google Scholar]
- 14.Aglietti P., Sensi L., Cuomo P., Ciardullo A. Rotational position of femoral and tibial components in TKA using the femoral transepicondylar axis. Clin Orthop Relat Res. 2008;466(11):2751–2755. doi: 10.1007/s11999-008-0452-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Luyckx T., Zambianchi F., Catani F., Bellemans J., Victor J. Coronal alignment is a predictor of the rotational geometry of the distal femur in the osteo-arthritic knee. Knee Surg Sports Traumatol Arthrosc. 2013;21(10):2331–2337. doi: 10.1007/s00167-012-2306-x. [DOI] [PubMed] [Google Scholar]
- 16.Paley D. Springer; Berlin/New York: 2002. Principles of Deformity Correction. [Google Scholar]
- 17.Tan C.M., Liau J.J., Chen W.T., Cheng C.K. The accuracy of posterior condylar angles measured by one MR image. Clin Orthop Relat Res. 2007;456:159–163. doi: 10.1097/01.blo.0000246566.80961.1b. [DOI] [PubMed] [Google Scholar]
- 18.Park A., Nam D., Friedman M.V., Duncan S.T., Hillen T.J., Barrack R.L. Inter-observer precision and physiologic variability of MRI landmarks used to determine rotational alignment in conventional and patient-specific TKA. J Arthroplasty. 2015;30(2):290–295. doi: 10.1016/j.arth.2014.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patel A.R., Talati R.K., Yaffe M.A., McCoy B.W., Stulberg S.D. Femoral component rotation in total knee arthroplasty: an MRI-based evaluation of our options. J Arthroplasty. 2014;29(8):1666–1670. doi: 10.1016/j.arth.2014.02.033. [DOI] [PubMed] [Google Scholar]
- 20.Howell S.M., Howell S.J., Hull M.L. Assessment of the radii of the medial and lateral femoral condyles in varus and valgus knees with osteoarthritis. J Bone Joint Surg Am. 2010;92(1):98–104. doi: 10.2106/JBJS.H.01566. [DOI] [PubMed] [Google Scholar]
- 21.Robinson M., Eckhoff D.G., Reinig K.D., Bagur M.M., Bach J.M. Variability of landmark identification in total knee arthroplasty. Clin Orthop Relat Res. 2006;442:57–62. doi: 10.1097/01.blo.0000197081.72341.4b. [DOI] [PubMed] [Google Scholar]
- 22.Kinzel V., Ledger M., Shakespeare D. Can the epicondylar axis be defined accurately in total knee arthroplasty? Knee. 2005;12(4):293–296. doi: 10.1016/j.knee.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 23.Luyckx T., Peeters T., Vandenneucker H., Victor J., Bellemans J. Is adapted measured resection superior to gap-balancing in determining femoral component rotation in total knee replacement? J Bone Joint Surg Br. 2012;94(9):1271–1276. doi: 10.1302/0301-620X.94B9.28670. [DOI] [PubMed] [Google Scholar]
- 24.Thienpont E., Schwab P.E., Paternostre F., Koch P. Rotational alignment of the distal femur: anthropometric measurements with CT-based patient-specific instruments planning show high variability of the posterior condylar angle. Knee Surg Sports Traumatol Arthrosc. 2014;22(12):2995–3002. doi: 10.1007/s00167-014-3086-2. [DOI] [PubMed] [Google Scholar]
- 25.Gu Y., Roth J.D., Howell S.M., Hull M.L. How frequently do four methods for mechanically aligning a total knee arthroplasty cause collateral ligament imbalance and change alignment from normal in white patients? AAOS exhibit selection. J Bone Joint Surg Am. 2014;96(12):e101. doi: 10.2106/JBJS.M.00306. [DOI] [PubMed] [Google Scholar]