Abstract
CAAT/enhancer-binding protein-beta (C/EBPβ) is a transcription factor that regulates interleukin-1β (IL-1β)-induced catabolic pathways, including the expression of matrix metalloproteinases (MMPs), in chondrocytes. We previously reported that suppressor of cytokine signaling 1 (SOCS1) inhibits IL-1β signaling in chondrocytes. However, the effect of SOCS1 on C/EBPβ has not been explored. To investigate the interaction between SOCS1 and C/EBPβ, we established human SW1353 cells with overexpression or knockdown of SOCS1 or C/EBPβ. Both SOCS1 and C/EBPβ were involved in transcription of MMP-3 and MMP-13. When stimulated with IL-1β, C/EBPβ levels were significantly increased by SOCS1 knockdown and decreased by SOCS1 overexpression. A similar change in IL-1β-induced C/EBPβ expression was observed in SOCS1-transfected human articular chondrocytes. However, C/EBPβ overexpression or knockdown did not change the levels of IL-1β-induced SOCS1. SOCS1 regulated the levels of C/EBPβ mRNA by ubiquitination of C/EBPβ as well as transcriptional regulation. Furthermore, it suppressed the phosphorylation of cAMP response element-binding protein (CREB), an active transcription factor of C/EBPβ. In addition, p38 mitogen-activated protein kinases, a target of SOCS1, was involved in CREB phosphorylation. The chromatin immunoprecipitation assay confirmed that SOCS1 overexpression led to reduced binding of C/EBPβ to the MMP-13 promoter. Taken together, our results demonstrate that SOCS1 downregulates the p38-CREB-C/EBPβ pathway resulting in increased expression of MMPs in chondrocytes.
Introduction
Osteoarthritis (OA) is characterized by a slowly progressive and irreversible loss of articular cartilage. Although it is the most common form of arthritis with an age-dependent incidence, its etiology and pathogenesis are poorly understood. The interaction of joint tissues including cartilage, subchondral bone and synovium could contribute to the pathogenesis of OA, but chondrocytes are considered central players in the pathogenesis of OA.1 It has been shown that phenotypical changes in chondrocytes have important implications in the development and/or progression of OA during aging. Some chondrocytes shift to the ‘hypertrophic-like' phenotype that is characterized by several molecular biomarkers such as matrix metalloproteinase (MMP)-13 and type X collagen (COL10A1).2 In addition, stress-induced senescence causes chondrocytes to produce pro-inflammatory cytokines including IL-1β and MMPs (senescent secretory phenotype).3 Proinflammatory cytokines such as IL-1β and TNF-α are also critical mediators of the further imbalance between anabolism and catabolism in OA cartilage. IL-1β is involved in cartilage destruction, whereas TNF-α seems to drive the inflammatory cascade in OA.4
CCAAT/enhancer-binding proteins (C/EBPs) are a family of transcription factors, containing a basic leucine zipper domain, that regulate various physiological and pathophysiological processes such as inflammation and differentiation.5 C/EBPβ is known to amplify IL-1β, TNFα or IFN-γ downstream signals.6 C/EBPβ expression is increased in OA cartilage,7 and stimulates the promoter activity of MMP-3 and MMP-13 in chondrocytes.8, 9 In addition, C/EBPβ represses type II collagen expression and enhances type X collagen synthesis.10, 11 Moreover, C/EBPβ was reported to have a role in the senescence or hypertrophy of chondrocytes.11, 12 In this context, C/EBPβ actively participates in the pathogenesis of OA.
Previously, we reported that suppressors of cytokine signaling 1 (SOCS1) is induced by IL-1β in chondrocytes and exerts chondroprotective effects via the suppression of IL-1β-induced secretion of matrix-degrading enzymes from chondrocytes, namely MMP-1, MMP-3, MMP-13, and disintegrin and metalloproteinase with thrombospondin type 1 motif-4 (ADAMTS4).13 Recently, Cui et al.14 reported that C/EBPβ was involved in increased SOCS1 expression induced by a growth hormone in the murine preadipocyte cell line. However, the effect of SOCS1 on C/EBPβ has not been studied in chondrocytes. Thus, we investigated the interaction between SOCS1 and C/EBPβ in the human chondrocyte-like cell line, SW1353, and primary human articular chondrocytes (HACs), using overexpression and knockdown systems to better understand the chondroprotective mechanisms of SOCS1.
Materials and methods
Plasmids and reagents
pBABE-C/EBPβ and the pShuttle2-SOCS1 viral vector were obtained from Addgene (Cambridge, MA, USA), and the pBABE-SOCS1 viral vector was generated as previously reported.13 SOCS1 shRNA and copGFP control lentivirus particles were purchased from Santa Cruz Biotechnology (Santa Cruz, CA, USA). Anti-C/EBPβ and anti-β-actin were also obtained from Santa Cruz Biotechnology. Anti-phospho-CREB (Ser133), anti-CREB and anti-ubiquitin antibodies were from Cell Signaling Technology (Beverly, MA, USA). Anti-SOCS1 was purchased from Chemicon International (Temecula, CA, USA). The p38 kinase inhibitor SB202190 was purchased from Alexis Biochemicals (Farmingdale, MI, USA) and MG132 was purchased from Sigma-Aldrich (St Louis, MO, USA). Recombinant human IL-1β and IFN-γ were purchased from PeproTech (Rocky Hill, NJ, USA). Specific TaqMan probe and primers for SOCS1 (assay ID Hs00705164_S1), MMP-1 (Hs00233958_m1), MMP-3 (Hs00968308_m1), MMP-13 (Hs00233992_m1) and large ribosomal protein (RPLPO, Hs99999902_m1) were purchased from Applied Biosystems (Foster City, CA, USA). Pronase and clostridial collagenase were from Sigma-Aldrich and Worthington (Freehold, NJ, USA), respectively. The SW1353 chondrosarcoma cell line (ATCC No. HTB-94) was obtained from American Type Culture Collection (Manassas, VA, USA). The Platinum-A retroviral packing cell line was procured from Cell BioLabs (San Diego, CA, USA).
Isolation of primary human articular chondrocytes
Femoral and tibial cartilage was harvested from five patients with primary knee OA who underwent total knee replacement arthroplasty. HACs were isolated by sequential enzymatic digestion using 0.2% pronase and 0.3% clostridial collagenase. Isolated HACs were plated in 100-mm-diameter dishes and cultured to 70% confluence in Dulbecco's Modified Eagle's Medium containing 10% fetal bovine serum (FBS), 100 IU ml−1 penicillin and 100 μg ml−1 streptomycin at 37 °C in a humidified atmosphere containing 5% CO2. This study has been approved by the Institutional Review Board of Seoul National University Bundang Hospital (IRB No. B-0607/035-018), and written informed consent was obtained from the study participants.
Overexpression and knockdown of human SOCS1 and C/EBPβ
To produce the retrovirus, the pBABE-C/EBPβ viral vector was transfected into a platinum-A retroviral packing cell line, and supernatants were collected 72 h after transfection. To infect SW1353 cells, the viral supernatant was mixed with fresh medium with 8 μg ml−1 polybrene at a 1:1 ratio, and the mixture was applied to SW1353 cells. C/EBPβ-overexpressing cell lines were selected with puromycin (2 μg ml−1). Human SOCS1-overexpressing or knockdown cell lines were prepared as previously reported.13 SOCS1 overexpression or knockdown was quantitated by western blot analysis or real time RT-PCR, respectively (Supplementary Figure 1). To establish SOCS1-overexpressing HACs, pShuttle2-SOCS1 or empty vector was electrotransfected using a Gene Pulser Xcell System (Bio-Rad, Hercules, CA, USA) under 50 V and 2 ms pulse (4-mm cuvette). Synthetic siRNA duplex oligonucleotides against C/EBPβ were electrotransfected under 200 V and 20 ms pulse (4-mm cuvette); the target sequences were 5′-GGCCCUGAGUAAUCGCUUAtt-3′(sense) and 5′-UAAGCGAUUACUCAG-GGCCcg-3′ (antisense).9
Reverse transcriptase-polymerase chain reaction for MMP-1, -3, -13 and C/EBPβ
Quantitative real-time RT-PCR was performed using an ABI-7500 real-time PCR machine (Applied Biosystems) and the TaqMan probes for MMP-1, -3 and -13. Quantitative C/EBPβ mRNA expression was determined using the SYBR green Master Mix (Applied Biosystems). Specific primers for C/EBPβ and GAPDH were designed as follows: human C/EBPβ 5′-CGAGCGGCAGCAGCG-3′ (sense) and 5′-CTCGCGCCGGATCTTGTA-3′ (antisense, GeneBank accession number NM_005194); human GAPDH 5′-TCCCTGAGCTGAACGGGAAG-3′ (sense) and 5′-GGAGGAGTGGGTGTCGCTGT-3′ (antisense, GeneBank accession number NM_002046).15 The number-fold difference in the expression of target mRNA was calculated with a comparative Ct method (2−ΔΔCt), and normalized to RPLPO or GAPDH.
Western blotting and immunoprecipitation
To prepare the total cell lysates, SW1353 cells were washed twice with ice-cold phosphate-buffered saline (PBS), harvested and lysed in immunoprecipitation (IP) buffer for 1 h on ice as previously described.13 The whole-cell extracts (500 μg) and anti-C/EBPβ antibody (2 μg) were incubated on a rotator overnight at 4 °C and then protein G-agarose beads were further incubated for 3 h at 4 °C. The mixtures were centrifuged at 2095 g for 3 min. After washing the precipitates three times in pre-cold IP buffer, the beads were resuspended in 2 × SDS sample buffer. The immunoprecipitates or whole-cell lysates were resolved on 10% denaturing polyacrylamide gels. After transfer to polyvinylidene difluoride membranes, the membranes were probed with appropriate primary antibodies and IgG horseradish peroxidase-conjugated secondary antibodies. The signals were visualized using an enhanced chemiluminescence system (Amersham Biosciences, Little Chalfont, UK).
Chromatin immunoprecipitation
SW1353 cells were stimulated with IL-1β (10 ng ml−1) in FBS-free media for 24 h. The cells were fixed in 0.8% formaldehyde, and glycine (125 mM) was added to stop the cross-linking reaction. Cells were lysed with chromatin immunoprecipitation (ChIP) lysis buffer (50 mM Tris-Cl pH 8.0, 1 mM EDTA, 0.5% Triton X-100, 0.1% sodium deoxycholate, 0.1% SDS, 140 mM NaCl, 1 mM PMSF and protease inhibitor cocktail) for 30 min on ice and sonicated using a Sonifier (Branson Sonifier, Branson Ultrasonic Corporation, Danbury, CT, USA; 40% amplification, 20 s, three times). After the supernatant was collected, chromatin fragments were cleared with preimmune serum and protein G beads. IP was carried out for 16 h with anti-C/EBPβ antibody. Normal rabbit IgG was used as the control sample. After IP, protein G beads were added and incubated for 2 h. Protein G beads were sequentially washed with low-salt buffer, high-salt buffer, LiCl buffer and ammonium sulfate buffer (20 mM Tris-Cl pH 8.0, 1 mM EDTA, 0.5% TritonX-100, 150 mM NaCl or 500 mM NaCl or 250 mM LiCl or 150 mM (NH4)2SO4) three times and then extracted with elution buffer (1% SDS, 0.1 M NaHCO3). Eluates were heated at 65 °C for 5 h to reverse the formaldehyde cross-linking reaction. DNA fragments were purified by phenol extraction and ethanol precipitation. Purified DNA fragments were amplified with specific primers. Primers used for the ChIP assay were previously published by Hayashida et al.8; 5′-GGACTATTTTCCTGATGGTTGGAC-3′ and 5′-GGAACGGAACAACTGTAATGGC-3′ to amplify between −1081 bp and −650 bp on MMP13 promoter including C/EBPβ consensus-binding motifs; 5′-GCGCTGATTATGTTCTTAAATGG-3′ and 5′-TGGAAATGAAATGAAGGCTAAAA-3′ to amplify between −2112 bp and −1913 bp for the negative control.
Statistical analysis
All experiments were performed at least three times and data are expressed as mean±s.e.m. The quantitative real-time PCR was performed in triplicate using three independent biological samples for SW1353 cells and were performed in duplicate using five independent samples for HACs. The Mann–Whitney test was used to compare continuous variables. Semiquantitative densitometry analysis was performed using ImageJ software (National Institutes of Health, USA). Statistical analyses were performed using the PASW statistics version 18 software (SPSS Inc., Chicago, IL, USA) and P<0.05 was considered statistically significant.
Results
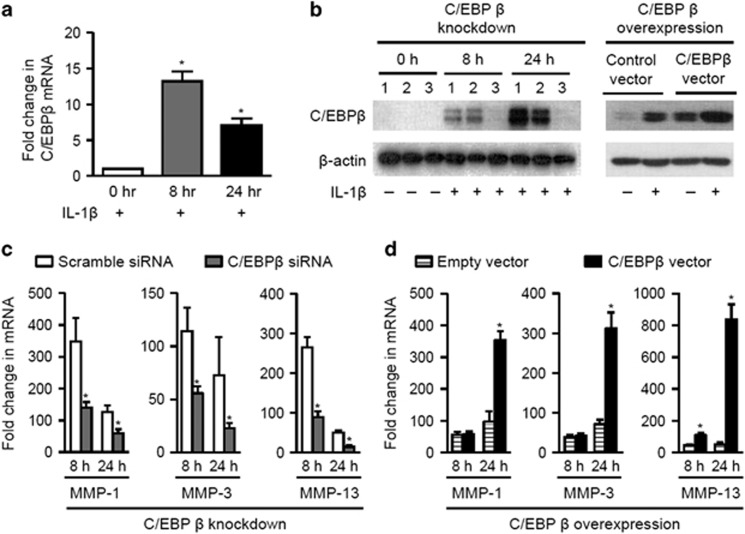
IL-1β induces C/EBPβ expression and C/EBPβ upregulates mRNA levels of MMPs in SW1353 cells
As shown in Figures 1a and b, SW1353 cells significantly increased the expression of C/EBPβ at the transcript and protein level 8 h after IL-1β (10 ng ml−1) stimulation. To investigate the effect of C/EBPβ on IL-1β-induced MMP production, we established C/EBPβ-overexpressing or knockdown SW1353 cell lines (Figure 1b). When C/EBPβ-knockdown SW1353 cells were stimulated with IL-1β, the mRNA levels of MMP-1, MMP-3 and MMP-13 were significantly decreased, compared with scramble siRNA-transfected cells (Figure 1c, all P<0.05). In contrast, the MMP mRNA levels were significantly increased after stimulation with IL-1β for 24 h in C/EBPβ-overexpressing SW1353 cell lines (Figure 1d, P<0.05).
Figure 1.
The effects of C/EBPβ on the production of MMPs. (a) C/EBPβ mRNA expression was significantly increased 8 h after IL-1β (10 ng ml−1) stimulation in SW1353 cells. (b) IL-1β increased C/EBPβ protein levels over time (lane 1 of the left panel, SW1353 cells; lane 2 of the left panel, SW1353 cells transfected with control siRNA). However, C/EBPβ protein expression was successfully suppressed by C/EBPβ siRNA (lane 3 of the left panel). Overexpression of C/EBPβ was confirmed by western blot in pBABE-C/EBPβ-transfected SW1353 cells (right panel). (c) C/EBPβ gene knockdown leaded to a significant reduction in MMP-1, MMP-3 and MMP-13 mRNA levels after IL-1β stimulation in SW1353 cells. (d) In contrast, IL-1β-induced increase in MMP mRNA levels was further enhanced in C/EBPβ-overexpressing SW1353 cells. Data are expressed as the mean±s.e.m. (all n=3). *P<0.05.
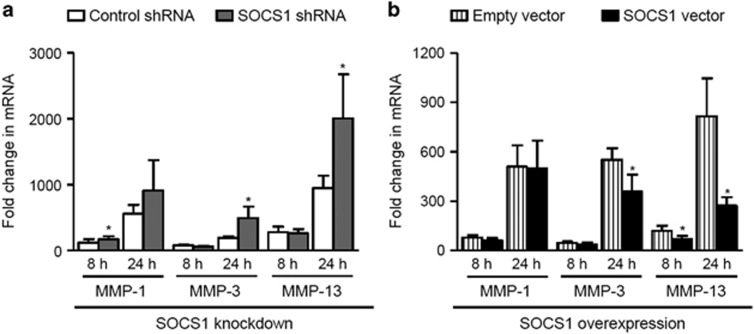
Effects of SOCS1 on IL-1β-induced expression of MMPs transcripts
Our previous study showed that SOCS1 suppressed the secretion of MMPs and ADAMTS-4 in SW1353 cells and primary HACs.13 We therefore examined IL-1β-induced expression of MMP mRNA over time in SOCS1-overexpressing or knockdown SW1353 cells. Although MMP-3 and MMP-13 transcripts remained unchanged at 8 h, SOCS1-knockdown SW1353 cells demonstrated significantly increased MMP-3 and MMP-13 mRNA levels at 24 h (Figure 2a, P<0.05). Moreover, IL-1β-induced expression of MMP-3 and MMP-13 mRNA was suppressed after 24 h in SOCS1-overexpressing cell lines (Figure 2b, P<0.05).
Figure 2.
Changes in MMP transcripts induced by SOCS1 overexpression and knockdown. (a) Compared with scramble shRNA-transfected cells (white bars), SW 1353 cells with SOCS1 knockdown (gray bars) showed a significant increase in MMP-3 and MMP-13 mRNA at 24 h. (b) Conversely, SOCS1-overexpressing SW1353 cells (black bars) produced significantly lower levels of MMP-3 and MMP-13 mRNA at 24 h after IL-1β stimuli. The levels of MMP-1 transcript were not affected by up- or downregulation of SOCS1 at 24 h. Data are expressed as the mean±s.e.m. (all n=3). *P<0.05.
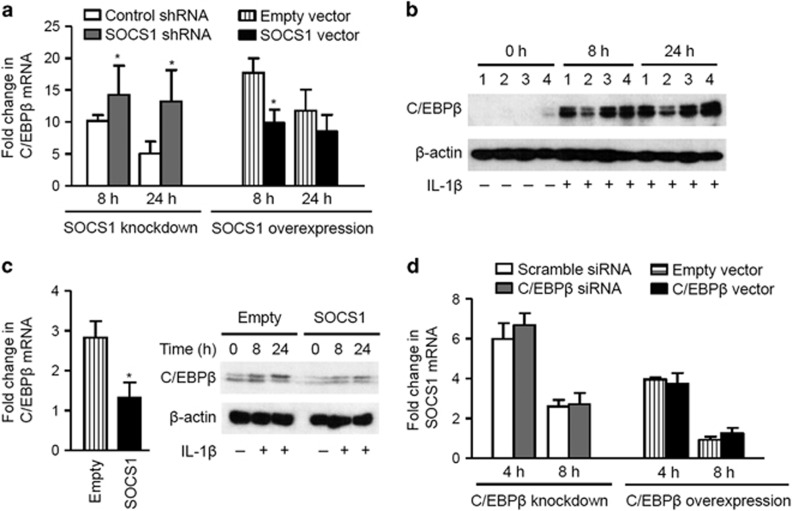
IL-1β-induced C/EBPβ was downregulated by SOCS1 in chondrocytes
SOCS1 and C/EBPβ have an inverse impact on MMP expression. Therefore, we next evaluated C/EBPβ expression in SOCS1-knockdown or -overexpression systems. After IL-1β stimulation for 8 h, C/EBPβ mRNA expression was significantly increased in SOCS1-knockdown SW1353 cells and significantly decreased in SOCS1-overexpressing SW1353 cells (Figure 3a, P<0.05). Moreover, the levels of C/EBPβ protein induced by IL-1β were altered upon overexpression or knockdown of SOCS1 (Figure 3b). In primary HACs, which were transiently electrotransfected with the pShuttle2-SOCS1 vector, the levels of C/EBPβ mRNA and protein were downregulated after IL-1β stimulation (Figure 3c, P<0.05). However, when SOCS1 expression was analyzed, C/EBPβ overexpression or knockdown did not affect the expression of SOCS1 induced by IL-1β (Figure 3d). These data suggest that SOCS1 can suppress the catabolic response of C/EBPβ in chondrocytes.
Figure 3.
The effect of SOCS1 on IL-1β-induced C/EBPβ expression. (a) IL-1β-induced C/EBPβ mRNA expression was significantly increased in SW1353 cells with knockdown of the SOCS1 gene (gray bars), and decreased in the SOCS1-overexpressing SW1353 cells after 8 h (black bars; n=3). (b) A representative immunoblot showing that IL-1β-induced expression of the C/EBPβ protein was lower in SOCS1-overexpressing SW1353 cells than in other cells (lane 1, empty vector; lane 2, SOCS1 vector; lane 3, scramble shRNA; lane 4, SOCS1 shRNA). (c) SOCS1 decreased the levels of IL-1β-induced C/EBPβ transcript and protein expression in human articular chondrocytes (HACs) electrotransfected with the SOCS1 vector (n=5). (d) C/EBPβ knockdown or overexpression did not affect the levels of SOCS1 mRNA upon IL-1β stimulation (n=3). Data are expressed as the mean±s.e.m. *P<0.05.
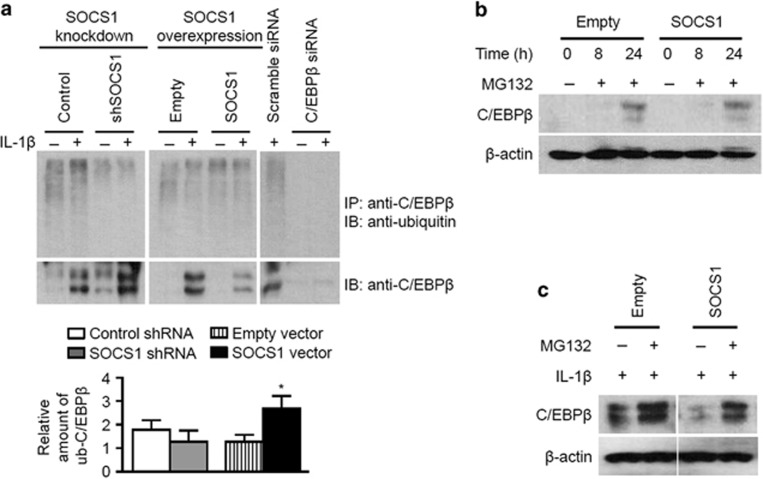
Post-translational ubiquitination of C/EBPβ by SOCS1
SOCS proteins are also known to promote ubiquitination and proteasomal degradation of target substrates.16 In addition, C/EBPβ is ubiquitinated and degraded by the 26S proteasome.17 Therefore, we examined whether SOCS1 affects C/EBPβ ubiquitination in chondrocytes. Immunoprecipitation coupled with immunoblot analysis showed that the SOCS1 was involved in the ubiquitination of C/EBPβ (Figure 4a). The amount of ubiquitinated C/EBPβ (relative to that of total C/EBPβ) was decreased or increased by SOCS1 knockdown or overexpression, respectively. After the treatment of a proteasome inhibitor MG132, endogenous C/EBPβ proteins could be detected when cells were not stimulated by IL-1β, irrespective of SOCS1 overexpression status (Figure 4b). However, IL-1β-induced C/EBPβ levels were lower in SOCS1-overexpressing cells than in empty vector-transfected cells, regardless of MG132 treatment (Figure 4c). These results suggested that SOCS1 could affect C/EBPβ expression by a transcriptional regulation mechanism as well as post-translational ubiquitination.
Figure 4.
Post-translational ubiquitination of C/EBPβ by SOCS1. (a) SOCS1-knockdown or -overexpressing SW1353 cells were incubated with IL-1β (10 ng ml−1) for 24 h, lysed and subjected to immunoprecipitation (IP) using antibodies to C/EBPβ. The precipitates were analyzed by immunoblot with antibodies to ubiquitin. The lysates before IP were subjected to immunoblot analysis with antibodies to C/EBPβ. In C/EBPβ-siRNA-transfected SW1353 cells, the disappearance of ubiquitinated C/EBPβ was confirmed. A representative figure and densitometric analysis demonstrated that C/EBPβ ubiquitination was increased by SOCS1 overexpression and tended to be decreased by SOCS1 knockdown. (b) Treatment with MG132, a proteasome inhibitor, led to increased endogenous C/EBPβ protein expression after 24 h in SW1353 cells, regardless of SOCS1 expression status. (c) IL-1β stimulation of SOCS1-overexpressing SW1353 cells led to reduced C/EBPβ protein levels, compared with empty vector-transfected cells, even with the treatment of MG132. The data presented are representative of three independent experiments. *P<0.05 compared with empty vector-transfected SW1353 cells.
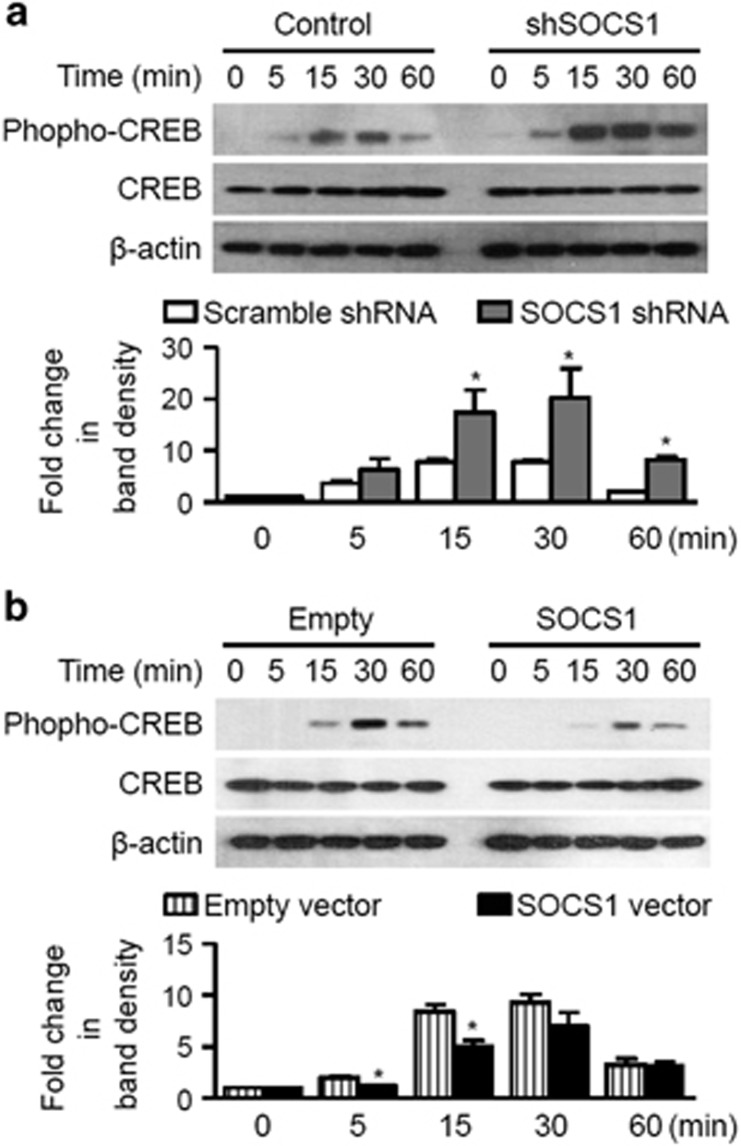
Mechanisms of transcriptional regulation of C/EBPβ by SOCS1
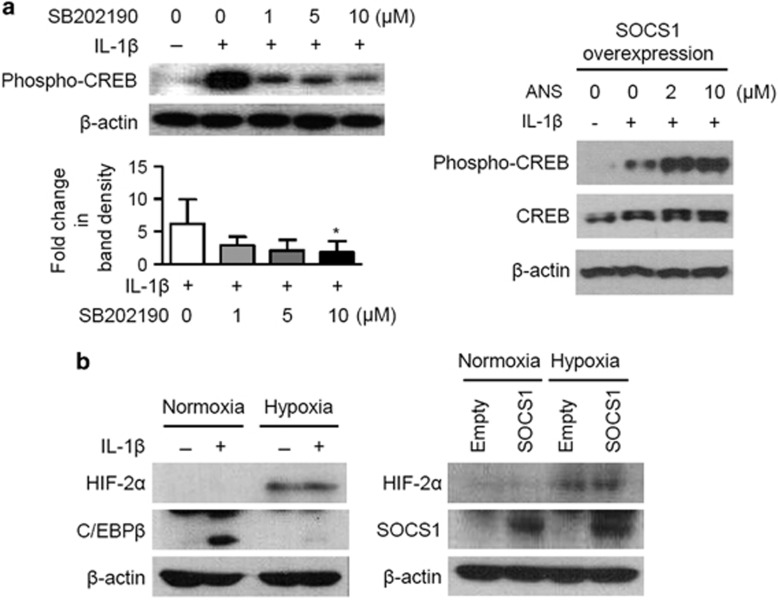
Accordingly, we next investigated whether SOCS1 could modulate the levels of phospho-CREB, a potent transcription factor that promotes C/EBPβ expression.18 In SOCS1-knockdown cells stimulated with IL-1β, phospho-CREB levels were significantly elevated within 15–60 min, compared with those transfected with scramble shRNA (Figure 5a). However, SOCS1 overexpression repressed the levels of phospho-CREB (Figure 5b). IL-1β-induced CREB phosphorylation at Ser133 is known to be mediated by the mitogen-activated protein kinases pathway.19, 20 Since we previously published that SOCS1 blocks IL-1β-induced activation of p38 mitogen-activated protein kinases, the effect of the p38 inhibitor SB202190 on CREB phosphorylation was examined in SW1353 cells. When SB202190 was added 1 h before IL-1β stimulation (10 ng ml−1), the amount of phospho-CREB protein decreased in a dose-dependent manner (Figure 6a). In addition, in SOCS1-overexpressing cells, the decrement in phospho-CREB level was recovered by a p38 kinase activator, anisomycin. (Figure 6a). Hypoxia-inducible factor-2α (HIF-2α) was recently discovered to be a novel inducer of C/EBPβ in chondrocytes;21 therefore, we also examined the effect of SOCS1 on HIF-2α. IL-1β did not induce HIF-2α expression and SOCS1 did not change the levels of HIF-2α in SW1353 cells under both normoxic and hypoxic conditions (Figure 6b).
Figure 5.
The effect of SOCS1 on CREB phosphorylation. (a) IL-1β stimulation led to significantly increased amounts of phospho-CREB protein at 15–60 min post stimulation in SOCS1-knockdown SW1353 cells (gray bars) compared with control shRNA-transfected cells (white bars). (b) In contrast, phospho-CREB levels were significantly lower at 5–15 min in SOCS1-overexpressing SW1353 cells (black bars). The densitometry data were normalized to β-actin and expressed as the means±s.e.m. (n=3). *P<0.05.
Figure 6.
The involvement of a p38 MAPK on CREB phosphorylation and the interaction between HIF-2α and SOCS1. (a) Pretreatment with SB202190 suppressed IL-1β (10 ng ml−1) induced expression of phospho-CREB in a dose-dependent manner. In addition, in SOCS1-overexpressing SW1353 cells, IL-1β-induced CREB phosphorylation was further increased by adding anisomycin (ANS) as a p38 kinase inhibitor. (b) Under normoxic conditions, IL-1β induced C/EBPβ expression, but not HIF-2α expression. Hypoxia-induced HIF-2α expression was unchanged by SOCS1. The densitometry data were normalized to β-actin and expressed as the means±s.e.m. (n=3).
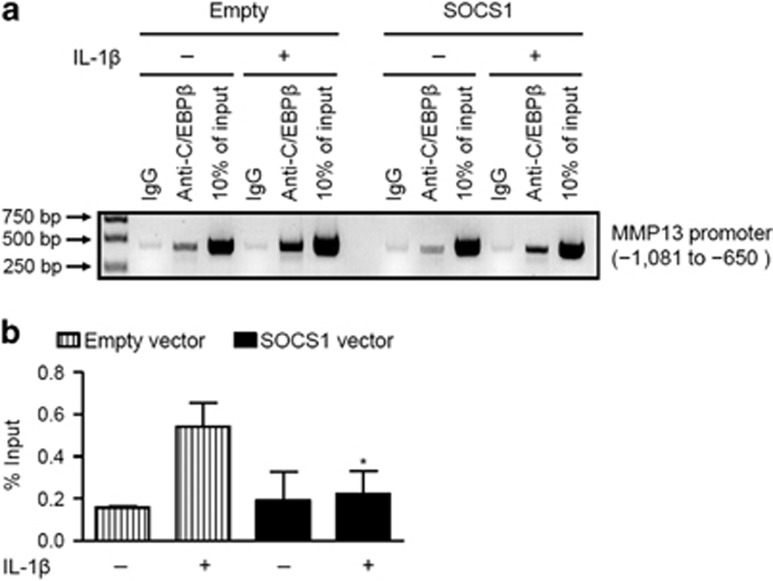
Effects of SOCS1 overexpression on binding of C/EBPβ to the MMP-13 promoter region
We performed ChIP assays to confirm that SOCS1 inhibits C/EBPβ-mediated MMP-13 transcription. IL-1β treatment for 24 h enhanced the binding of C/EBPβ to the MMP-13 promoter (Figure 7a, left panel), whereas SOCS1 overexpression reduced this binding effect (Figure 7a, right panel). The semi-quantitative analysis of ChIP data showed that binding was significantly reduced in SOCS1-overexpressing SW1353 cells (Figure 7b, P<0.05). These results demonstrate that SOCS1 can downregulate C/EBPβ transcription and consequently decrease its binding to the MMP-13 promoter and subsequent MMP-13 mRNA expression.
Figure 7.
Chromatin immunoprecipitation (ChIP) assay of C/EBPβ binding to the MMP-13 promoter. (a) Binding of C/EBPβ to the MMP-13 promoter was reduced in SOCS1-overexpressing SW1353 cells under IL-1β stimulation (10 ng ml−1, right panel), compared with empty vector-transfected cells. (b) Semiquantitative densitometric analysis of ChIP data showed that SOCS1 significantly decreased C/EBPβ binding to the MMP-13 promoter under IL-1β stimulation. The relative intensity of C/EBPβ binding to the MMP-13 promoter was normalized to PCR-amplified input DNA (10%) in each case. The error bars represent the s.e.m. from three independent measurements. *P<0.05.
Discussion
The present study showed that SOCS1 inhibits the p38-pCREB-C/EBPβ signaling pathway leading to suppression of IL-1β-induced MMP production in chondrocytes. This provides the first evidence of SOCS1-mediated translational regulation of C/EBPβ, an important chondrodestructive mediator.
Cartilage degradation with secondary synovitis is considered as a main pathological characteristic in OA joints.22 In the catabolic response and inflammatory process of chondrocytes, IL-1β is the central mediator of cartilage loss and functions via suppression of extracellular matrix synthesis and induction of cartilage-degrading enzymes such as MMPs.23 IL-1β is highly expressed in the synovial fluid, synovial membrane, cartilage and the subchondral bone layer in OA patients.22, 23, 24 The NF-κB, AP-1 and MAP kinase pathways have been implicated as major players in IL-1β-mediated induction of MMPs.25, 26 Recently, there has been increasing evidence to suggest that the C/EBPβ protein could be involved in inflammatory and catabolic responses in chondrocytes. Hayashida et al.8 reported that C/EBPβ stimulates the expression of MMP-13 by its direct binding to the MMP-13 promoter region in chondrocytes. Tsushima et al.9 revealed that C/EBPβ expression was induced by IL-1β treatment, and enhanced MMP-3, MMP-13 and ADAMTS-5 expression in arthritic synovium and cartilage.
SOCS proteins are a family of negative feedback inhibitors of cytokine networks. They are induced by gp130 cytokines through the JAK/STAT signaling pathway or JAK/STAT-independent stimuli such as LPS, CpG and insulin.16 The mechanisms of SOCS proteins include suppression of JAK activity by binding to either the signaling receptor or to the JAK activation loop, substrate competition or ubiquitination-mediated degradation of target substrates.27 Furthermore, SOCS proteins can modulate other signaling pathways such as PI3K-AKT, p38 and NF-κB.28, 29, 30 We previously reported that SOCS1 expression is increased in the damaged cartilage of OA patients, and can be induced by IL-1β in chondrocytes.13 In addition, we showed that SOCS1 exerts chondroprotective effects by decreasing IL-1β-induced secretion of MMPs and ADAMTS4 from chondrocytes by blocking p38, JNK, transforming growth factor-β-activated kinase 1 (TAK1) and NF-κB.
On the basis of these findings, we hypothesized that C/EBPβ could be regulated by SOCS1 in chondrocytes. SOCS1 overexpression caused a significant reduction in C/EBPβ expression, whereas SOCS1 knockdown had the opposite effect in C/EBPβ expression in SW1353 and HACs. In contrast, SOCS1 expression did not change according to the C/EBPβ levels. These findings suggest that C/EBPβ could be a target of SOCS1. We investigated the mechanism of the SOCS1-mediated C/EBPβ inhibition. Because SOCS1 promotes proteasomal degradation of target proteins via interaction with SOCS-box and the Elongin B/C complex,27 we first assessed C/EBPβ ubiquitination in SOCS1 overexpressing or knockdown cells by IP assay. As shown in Figure 4, SOCS1 overexpression augmented the post-translational ubiquitination of C/EBPβ. However, since IL-1β-induced C/EBPβ levels were lower in SOCS1-overexpressing cells than in empty vector-transfected cell (Figure 4c) regardless of MG132 treatment, a transcriptional regulation was thought to be involved in SOCS1-mediated C/EBPβ downregulation. The transcription of C/EBPβ is regulated by a variety of transcriptional factors including C/EBPβ itself and CREB.6 CREB has been reported to be involved in the synthesis of MMP-13 in chondrocytes,31 therefore, we examined the levels of phospho-CREB in IL-1β stimulated SW1353 cells with overexpressed or knockdown SOCS1. We observed that CREB phosphorylation was increased with knockdown of SOCS1 and decreased in SOCS1-overexpressing SW1353 cells (Figure 5). IL-1β-induced CREB activation by phosphorylation on Ser133 is mainly dependent on p38 kinases,19, 20 and our previous study showed an inhibitory action of SOCS1 on p38 in chondrocytes.13 In the present study, the inhibition of p38 kinase decreased IL-1β-induced CREB phosphorylation and the activation of p38 kinase decreased SOCS1-mediated suppression of CREB phosphorylation (Figure 6). Moreover, we confirmed SOCS1-mediated transcriptional regulation of MMP-13 via the p38-CREB-C/EBPβ pathway using ChIP assay.
Conclusively, these results demonstrate for the first time that SOCS1 modulates the p38-CREB-C/EBPβ signaling pathway. Despite a high prevalence and substantial socioeconomic burden of OA, few pharmacological agents with an effect to halt or delay disease progression have been introduced in the treatment for OA.1 Considering these findings, SOCS1 may serve as a potential therapeutic target for the treatment of OA.
Acknowledgments
This work was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF), which is funded by the Ministry of Education, Science and Technology (grant number 2011-0007463), and the Seoul National University Bundang Hospital Research Fund (grant number 14-2014-025).
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies the paper on Experimental & Molecular Medicine website (http://www.nature.com/emm)
Supplementary Material
References
- Glyn-Jones S, Palmer AJ, Agricola R, Price AJ, Vincent TL, Weinans H et al. Osteoarthritis. Lancet 2015; 386: 376–387. [DOI] [PubMed] [Google Scholar]
- Goldring MB, Otero M, Plumb DA, Dragomir C, Favero M, El Hachem K et al. Roles of inflammatory and anabolic cytokines in cartilage metabolism: signals and multiple effectors converge upon MMP-13 regulation in osteoarthritis. Eur Cell Mater 2011; 21: 202–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeser RF. Aging and osteoarthritis: the role of chondrocyte senescence and aging changes in the cartilage matrix. Osteoarthritis Cartilage 2009; 17: 971–979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapoor M, Martel-Pelletier J, Lajeunesse D, Pelletier JP, Fahmi H. Role of proinflammatory cytokines in the pathophysiology of osteoarthritis. Nat Rev Rheumatol 2011; 7: 33–42. [DOI] [PubMed] [Google Scholar]
- Ramji DP, Foka P. CCAAT/enhancer-binding proteins: structure, function and regulation. Biochem J 2002; 365: 561–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huber R, Pietsch D, Panterodt T, Brand K. Regulation of C/EBPbeta and resulting functions in cells of the monocytic lineage. Cell Signal 2012; 24: 1287–1296. [DOI] [PubMed] [Google Scholar]
- Nishioka K, Ohshima S, Umeshita-Sasai M, Yamaguchi N, Mima T, Nomura S et al. Enhanced expression and DNA binding activity of two CCAAT/enhancer-binding protein isoforms, C/EBPbeta and C/EBPdelta, in rheumatoid synovium. Arthritis Rheum 2000; 43: 1591–1596. [DOI] [PubMed] [Google Scholar]
- Hayashida M, Okazaki K, Fukushi J, Sakamoto A, Iwamoto Y. CCAAT/enhancer binding protein beta mediates expression of matrix metalloproteinase 13 in human articular chondrocytes in inflammatory arthritis. Arthritis Rheum 2009; 60: 708–716. [DOI] [PubMed] [Google Scholar]
- Tsushima H, Okazaki K, Hayashida M, Ushijima T, Iwamoto Y. CCAAT/enhancer binding protein beta regulates expression of matrix metalloproteinase-3 in arthritis. Ann Rheum Dis 2012; 71: 99–107. [DOI] [PubMed] [Google Scholar]
- Tsuchimochi K, Otero M, Dragomir CL, Plumb DA, Zerbini LF, Libermann TA et al. GADD45beta enhances Col10a1 transcription via the MTK1/MKK3/6/p38 axis and activation of C/EBPbeta-TAD4 in terminally differentiating chondrocytes. J Biol Chem 2010; 285: 8395–8407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ushijima T, Okazaki K, Tsushima H, Iwamoto Y. CCAAT/enhancer-binding protein beta regulates the repression of type II collagen expression during the differentiation from proliferative to hypertrophic chondrocytes. J Biol Chem 2014; 289: 2852–2863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huggins CJ, Malik R, Lee S, Salotti J, Thomas S, Martin N et al. C/EBPgamma suppresses senescence and inflammatory gene expression by heterodimerizing with C/EBPbeta. Mol Cell Biol 2013; 33: 3242–3258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi YS, Park JK, Kang EH, Lee YK, Kim TK, Chung JH et al. Cytokine signaling-1 suppressor is inducible by IL-1beta and inhibits the catabolic effects of IL-1beta in chondrocytes: its implication in the paradoxical joint-protective role of IL-1beta. Arthritis Res Ther 2013; 15: R191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui TX, Lin G, LaPensee CR, Calinescu AA, Rathore M, Streeter C et al. C/EBPbeta mediates growth hormone-regulated expression of multiple target genes. Mol Endocrinol 2011; 25: 681–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zainuddin A, Chua KH, Abdul Rahim N, Makpol S. Effect of experimental treatment on GAPDH mRNA expression as a housekeeping gene in human diploid fibroblasts. BMC Mol Biol 2010; 11: 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trengove MC, Ward AC. SOCS proteins in development and disease. Am J Clin Exp Immunol 2013; 2: 1–29. [PMC free article] [PubMed] [Google Scholar]
- Hattori T, Ohoka N, Inoue Y, Hayashi H, Onozaki K. C/EBP family transcription factors are degraded by the proteasome but stabilized by forming dimer. Oncogene 2003; 22: 1273–1280. [DOI] [PubMed] [Google Scholar]
- Niehof M, Manns MP, Trautwein C. CREB controls LAP/C/EBP beta transcription. Mol Cell Biol 1997; 17: 3600–3613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost RA, Nystrom GJ, Lang CH. Stimulation of insulin-like growth factor binding protein-1 synthesis by interleukin-1beta: requirement of the mitogen-activated protein kinase pathway. Endocrinology 2000; 141: 3156–3164. [DOI] [PubMed] [Google Scholar]
- Funding AT, Johansen C, Kragballe K, Iversen L. Mitogen- and stress-activated protein kinase 2 and cyclic AMP response element binding protein are activated in lesional psoriatic epidermis. J Invest Dermatol 2007; 127: 2012–2019. [DOI] [PubMed] [Google Scholar]
- Hirata M, Kugimiya F, Fukai A, Saito T, Yano F, Ikeda T et al. C/EBPbeta and RUNX2 cooperate to degrade cartilage with MMP-13 as the target and HIF-2alpha as the inducer in chondrocytes. Hum Mol Genet 2012; 21: 1111–1123. [DOI] [PubMed] [Google Scholar]
- Goldring MB, Otero M. Inflammation in osteoarthritis. Curr Opin Rheumatol 2011; 23: 471–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daheshia M, Yao JQ. The interleukin 1beta pathway in the pathogenesis of osteoarthritis. J Rheumatol 2008; 35: 2306–2312. [DOI] [PubMed] [Google Scholar]
- Wojdasiewicz P, Poniatowski LA, Szukiewicz D. The role of inflammatory and anti-inflammatory cytokines in the pathogenesis of osteoarthritis. Mediators Inflamm 2014; 2014: 561459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mengshol JA, Vincenti MP, Coon CI, Barchowsky A, Brinckerhoff CE. Interleukin-1 induction of collagenase 3 (matrix metalloproteinase 13) gene expression in chondrocytes requires p38, c-Jun N-terminal kinase, and nuclear factor kappaB: differential regulation of collagenase 1 and collagenase 3. Arthritis Rheum 2000; 43: 801–811. [DOI] [PubMed] [Google Scholar]
- Vincenti MP, Brinckerhoff CE. Transcriptional regulation of collagenase (MMP-1, MMP-13) genes in arthritis: integration of complex signaling pathways for the recruitment of gene-specific transcription factors. Arthritis Res 2002; 4: 157–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang Y, Xu WD, Peng H, Pan HF, Ye DQ. SOCS signaling in autoimmune diseases: molecular mechanisms and therapeutic implications. Eur J Immunol 2014; 44: 1265–1275. [DOI] [PubMed] [Google Scholar]
- Souma Y, Nishida T, Serada S, Iwahori K, Takahashi T, Fujimoto M et al. Antiproliferative effect of SOCS-1 through the suppression of STAT3 and p38 MAPK activation in gastric cancer cells. Int J Cancer 2012; 131: 1287–1296. [DOI] [PubMed] [Google Scholar]
- Madonna S, Scarponi C, Pallotta S, Cavani A, Albanesi C. Anti-apoptotic effects of suppressor of cytokine signaling 3 and 1 in psoriasis. Cell Death Dis 2012; 3: e334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strebovsky J, Walker P, Lang R, Dalpke AH. Suppressor of cytokine signaling 1 (SOCS1) limits NFkappaB signaling by decreasing p65 stability within the cell nucleus. FASEB J 2011; 25: 863–874. [DOI] [PubMed] [Google Scholar]
- Bui C, Barter MJ, Scott JL, Xu Y, Galler M, Reynard LN et al. cAMP response element-binding (CREB) recruitment following a specific CpG demethylation leads to the elevated expression of the matrix metalloproteinase 13 in human articular chondrocytes and osteoarthritis. FASEB J 2012; 26: 3000–3011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.