Key Clinical Message
The present case emphasizes the importance of adhering to strict indications when prescribing fluoroquinolones. Although rare, drug‐induced tendinopathy is not confined to fluoroquinolones. The patient's and physician's awareness should be increased to reduce fluoroquinolones‐associated morbidity, particularly in patients with previously described risk factors.
Keywords: Bilateral, fluroquinolones‐induced, patellar tendon, spontaneous rupture, tendinopathy
Case presentation
A 47‐year‐old male amateur runner (five miles per day) without preexisting medical comorbidities presented to our emergency department with bilateral knee pain and inability to walk. He reported to have fallen suddenly while walking downstairs, developing acute knee pain. Subsequently, he was unable to stand up. Two weeks before presentation, the patient was treated for a community‐acquired pulmonary infection with ciprofloxacin (nonadjusted dose of 500 mg every 12 h).
The physical examination showed swollen knees, a high riding patella, a gap below the inferior poles (Fig. 1), and an inability to actively extend the knees. X‐ray showed a patella alta (Fig 2) and an Insall‐Salvati ratio >1.5, bilaterally. The diagnosis of bilateral patellar tendon rupture was made.
Figure 1.

Image showing a gap below the inferior pole of the patella.
Figure 2.

Bilateral knee x‐ray showing patella alta
Operative repair was performed the following day. A straight midline longitudinal incision was made, extending from the superior pole of the patella to the tibial tubercle. Thick medial and lateral subcutaneous flaps were observed. Intraoperative observation confirmed an intrasubstance rupture, and the tendons were torn just beneath the inferior pole of the patella (Fig. 3A). The torn end of the patellar tendon was then mobilized and minimally debrided of friable tissue. Nonabsorbable fiber wire sutures were then inserted with a Krackow stitch into each half of the tendon (Fig. 3B). Three parallel tunnels were placed through the patella. The inner limbs of each stitch were passed through the central tunnel; then, the outer limbs were passed through the outer tunnels (Fig. 3C). A drill hole was then created transversely through the tibial tubercle, and an additional Dall‐Miles cable was passed through this hole. This cable was then passed superiorly, within the quadriceps tendon, along the superior pole of the patella, in a figure of eight (Fig. 3D). Once the correct position was obtained, the repair sutures were tied, and the knee was carefully reexamined to assess the degree of knee flexion that could be obtained without causing excessive tension on the repair.
Figure 3.
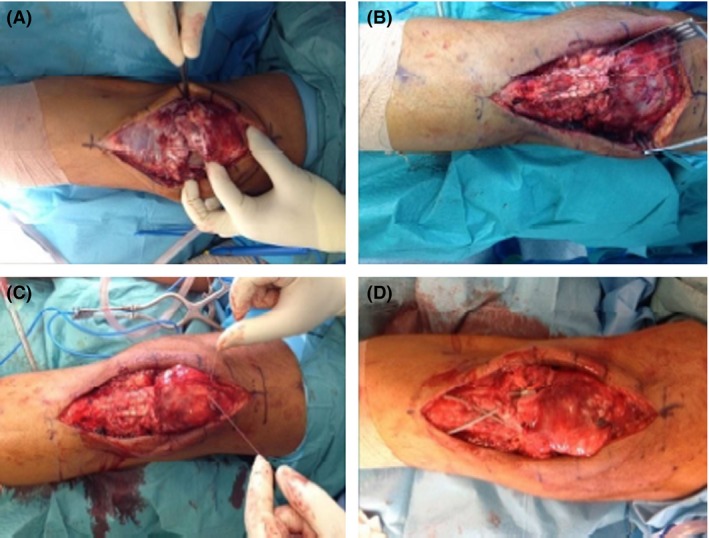
Intraoperative images of the surgical procedure: intraoperative observation confirmed an intrasubstance rupture and that the tendons were torn just beneath the inferior pole of the patella (A); nonabsorbable fiber wire sutures were then inserted with a Krackow stitch into each half of the tendon (B); the inner limbs of each stitch were passed through the central tunnel, then, the outer limbs were passed through the outer tunnels (C); a cable was then passed superiorly, within the quadriceps tendon, along the superior pole of the patella, in a figure of eight (D).
Results
After the repair, the patient began a postoperative rehabilitative program with these follow‐up care goals: 3–5 days – adequate pain control, decrease in swelling, wound check, no weight‐bearing, and immobilization with long leg casts in extension; 2 weeks – immobilization with a hinged knee brace, active flexion to 45°, full passive extension, and toe touch with crutches; 4 weeks – active flexion to 90°, maintenance of full passive extension, and progressive weight‐bearing as tolerated; 6–8 weeks – full active flexion; 3 months – straight leg raise with no extension lag, no immobilization, and full weight‐bearing; and 6 months – symmetric quadriceps size and strength. At 1 year follow‐up, the patient was able to walk without crutches, including nearly full return of knee motion (0° of extension to 155° of flexion), quadriceps strength, and preinjury activity levels. No quadriceps atrophy was noted.
Discussion
Bilateral rupture of the patellar tendons is an extremely rare lesion in healthy individuals and is usually associated with systemic diseases, such as lupus erythematosus, rheumatoid arthritis, chronic renal failure and other conditions that weaken tendinous tissues 1, 2, 3, 4, 5, 6. In addition, long‐term microtrauma and corticosteroid use may also be present 2, 7. Fluoroquinolones are increasingly being recognized as a cause of tendinitis and tendon rupture 8, but the specific pathophysiological mechanisms involved in drug‐induced tendinopathies remain unknown. Several risk factors have been identified, including advanced age (>60 years), corticosteroid use, renal failure, female sex and non‐obesity 9. The most common sites of involvement are the lower limb tendons, more frequently the Achilles tendon 8, 10. Fluoroquinolones are widely used antibiotics that are indicated in the treatment of wide range of urinary, gastrointestinal, pulmonary, and even bone infections. They have excellent gastrointestinal absorption, superior tissue penetration, and broad‐spectrum activity 10. Although well tolerated and relatively safe, numerous side effects have been reported, including a spectrum of tendinopathies, gastrointestinal disorders, cutaneous eruptions, neurological signs, myalgia, elevated serum transaminases, and arthralgia 11. The presumptive diagnosis of fluoroquinolone‐induced tendinopathy rests on a converging set of arguments as well as on the absence of any other obvious cause, such as trauma‐induced injuries. While our patient was 47 years old, he had no known systemic disorder or risk factor for tendon rupture other than recent fluoroquinolone use.
The first reported case of fluoroquinolone‐associated tendinopathy was described in 1983 in renal‐transplant patient, treated with norfloxacin, who developed Achilles tendinopathy 12. Since then, fluoroquinolone‐induced tendinopathy has been the subject of many articles and case reports in the medical literature 13. Spontaneous patellar tendon rupture is an extremely rare pathology, and it is even rarer for it to present as bilateral, without any systemic pathological conditions, and in the absence of long‐term corticosteroid use. To the best of our knowledge, after literature review, we could only find one case of an atraumatic bilateral patellar tendon ruptures following a treatment course of fluoroquinolone medication 14.
Still, tendinopathy is a rare side effect, with an estimated incidence of 0.14–0.4% among patients treated with fluoroquinolone therapy 11. It usually occurs within the first 2 weeks, but cases have been described up to 6 months after therapy termination 11. The Achilles tendon is the most common site of involvement (90%) 15. The mean age for affected patients is 64 years, with a male‐to‐female ratio of 2:1, and there is 27% bilateral involvement. Ciprofloxacin is the most common fluoroquinolone associated with tendon disorders 11.
The mechanism by which fluoroquinolones cause tendinitis and tendon rupture remains relatively unknown, but it is known that they decrease fibroblastic metabolism and increase matrix degradative activity, causing disorganization of the paratenon and degenerative changes in tendon cells 15. The following fluoroquinolone‐induced effects have been proposed: reduced expression of extracellular matrix proteins 16, 17, noncytotoxic inhibition of tendon cell proliferation and migration 18, and enhanced matrix metalloproteinase expression 16, 17. At the molecular level, aging could also play a role, affecting the metabolic activity of senescent tenocytes as well as rendering them more prone to the deleterious effects of fluoroquinolones 16.
Patients with tendinopathy should be investigated about antibiotic use in the preceding 90 days. The diagnosis is usually clinical, which is sometimes corroborated by musculoskeletal ultrasound or magnetic resonance imaging. In cases of tendinopathy, treatment should include discontinuation of fluoroquinolone therapy, rest, use of anti‐inflammatory drugs, and an alternative nonquinolone antibiotic should be considered 11.
Tendon rupture should be treated operatively as soon as possible 19. The goal of surgical treatment is to achieve a strong repair enough to allow for early movement and weight‐bearing, granting a more rapid gradual rehabilitation. When early surgical repair is undertaken and the normal patellar tendon length is restored, the long‐term results are excellent 20.
Conclusion
The present case emphasizes the importance of adhering to strict indications when prescribing fluoroquinolones. Although rare, drug‐induced tendinopathy is not confined to fluoroquinolones. The patient's and physician's awareness should be increased to reduce fluoroquinolones‐associated morbidity, particularly in patients with the previously described risk factors.
Conflict of Interest
None declared.
Clinical Case Reports 2016; 4(7): 678–681
References
- 1. Quesada, J. Q. , Villadeamigo J. M., and Rico J. I. A.. 2003. Spontaneuous bilateral pattelar tendon rupture in an otherwise healthy patient: a case report. Acta Orthop. Belg. 69:89–91. [PubMed] [Google Scholar]
- 2. Moretti, B. , Notarnicola A., Moretti L., Garofalo R., and Patella V.. 2008. Spontaneous bilateral patellar tendon rupture: a case report and review of the literature. Chir. Organi Mov. 91:51–55. [DOI] [PubMed] [Google Scholar]
- 3. Van Glabbeek, F. , De Groof E., and Boghemans J.. 1992. Bilateral patellar tendon rupture: case report and literature review. J. Trauma 33:790–792. [PubMed] [Google Scholar]
- 4. Morgan, J. , and McCarty D. J.. 1974. Tendon ruptures in patients with systemic lupus erythematosus treated with corticosteroids. Arthritis Rheum. 17:1033–1036. [DOI] [PubMed] [Google Scholar]
- 5. Peiro, A. , Ferrandis R., Gracia I., and Alcazar E.. 1975. Simultaneous and spontaneous bilateral rupture of the patellar tendon in rheumatoid arthritis. A case report. Acta Orthop. Scand. 46:700–703. [DOI] [PubMed] [Google Scholar]
- 6. Sullivan, R. L. 1986. Traumatic bilateral patellar tendon rupture with chronic renal disease. Wis. Med. J. 85:12–13. [PubMed] [Google Scholar]
- 7. Clark, S. C. , Jones M. W., Choudhury R. R., and Smith E.. 1995. Bilateral patellar tendon rupture secondary to repetead steroid injections. J. Accid. Emerg. 12:300–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Khanzada, Z. , Rethnam U., Widdowson D., and Mirza A.. 2011. Bilateral spontaneous non‐traumatic rupture of the Achilles tendon: a case report. J. Med. Case Rep. 5:263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wise, B. L. , Peloquin C., Choi H., Lane N. E., and Zhang Y.. 2012. Impact of age, sex, obesity and steroid use on quinolone‐associated tendon disorders. Am. J. Med. 125:1228.e23–1228.e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kawtharani, F. , Mashoura K. Z., and Afeiche N.. 2016. Bilateral Achilles tendon ruptures associated with ciprofloxacin use in the setting of minimal change disease: case report and review of the literature. J. Foot Ankle Surg. 55:276–278. [DOI] [PubMed] [Google Scholar]
- 11. Tsai, W. C. , and Yang Y. M.. 2011. Fluoroquinolone‐associated tendinopathy. Chang Gung Med. J. 34:461–467. [PubMed] [Google Scholar]
- 12. Bailey, R. R. , Kirk J. A., and Peddie B. A.. 1983. Norfloxacin‐induced rheumatic disease. N Z Med. J. 96:590. [PubMed] [Google Scholar]
- 13. Lewis, T. , and Cook J.. 2014. Fluoroquinolones and tendinopathy: a guide for athletes and sports clinicians and a systematic review of the literature. J. Athl. Train. 49:422–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Stinner, C. D. J. , Orr J.D., Hsu J.R. 2010. Fluoroquinolone‐associated bilateral patellar tendon rupture: a case report. Mil. Med. 175:457. [DOI] [PubMed] [Google Scholar]
- 15. Kato, M. , Takada S., Kashida Y., Nomura M.. 1995. Histological examination on Achilles tendon lesions induced by quinolone antibacterial agents in juvenile rats. Toxicol. Pathol. 23:385–392. [DOI] [PubMed] [Google Scholar]
- 16. Chang, H. , Pang J., Chen C., Ko P., Lin M., Tsai W., Yang Yun‐Ming. 2012. The effect of aging on migration, proliferation and collagen expression of tenocytes in response to ciprofloxacin. J. Orthop. Res. 30:764–768. [DOI] [PubMed] [Google Scholar]
- 17. Bernard‐Beaubois, K. , Hecquet C., Hayem G., Rat P., Adolphe M.. 1998. In vitro study of cytotoxicity of quinolones on rabbit tenocytes. Cell Biol. Toxicol. 14:283–292. [DOI] [PubMed] [Google Scholar]
- 18. Tsai, W. C. , Hsu C. C., Chen H. C., Hsu Ya‐Hui, Lin Mao‐Sui, Wu Chin‐Wen, Pang Jong‐Hwei S.. 2009. Ciprofloxacin‐mediated inhibition of tenocyte migration and down‐regulation of focal adhesion kinase phosphorylation. Eur. J. Pharmacol. 607:23–26. [DOI] [PubMed] [Google Scholar]
- 19. Siwek, C. , and Rao J.. 1981. Ruptures of the extensor mechanism of the knee joint. J. Bone Joint Surg. 63:932–937. [PubMed] [Google Scholar]
- 20. Dejong, C. H. C. , Van de Luytgaarden W. G. A. C., and Vroeman J. P. A. M.. 1991. Bilateral simultaneous rupture of the patellar tendon. Case report and review of the literature. Arch. Orthop. Trauma Surg. 110:222–226. [DOI] [PubMed] [Google Scholar]


