Abstract
The RASopathies, which include Noonan syndrome (NS) and Cardiofaciocutaneous syndrome (CFC), are autosomal dominant disorders with genetic heterogeneity associated with germline mutations of genes in the Ras/mitogen-activated protein kinase (MAPK; RAS–MAP kinase) pathway. The conditions overlap and are characterised by facial dysmorphism, short stature and congenital heart disease. NS and CFC, in particular, are known to be associated with lymphatic problems, but this has not been well characterised to date. We describe 11 patients with Noonan or CFC syndrome with significant, persistent and progressive lymphatic dysplasia. The lymphatic disorders in Noonan and CFC syndrome are rare, but have a characteristic pattern with bilateral lower limb lymphoedema, genital swelling with chylous reflux and frequent systemic involvement, including intestinal lymphangiectasia and chylothoraces, which may be progressive. Lymphoscintigraphy demonstrates reflux and/or rerouting of lymphatic drainage associated with incompetent veins on the venous duplex scans.
Introduction
The RASopathies have an incidence of approximately 1/1000 live births, affecting males and females equally.1 They are autosomal dominant disorders with genetic heterogeneity and overlapping clinical features. Characteristic features include low-set, posteriorly rotated ears, hypertelorism, ptosis, short stature, congenital heart defects, webbed neck, and down-slanting palpebral fissures.2 Disorders of lymphatic development have been described in Noonan syndrome3 but the lymphatic abnormalities in this condition are poorly documented.4 Lymphoedema associated with Noonan syndrome usually presents at birth, although it is seen at all ages.4 The literature describes variable lymphatic abnormalities associated with Noonan syndrome. A cross-sectional cohort study of 35 Noonan syndrome patients found a 49% prevalence of lymphoedema, which was chronic and intermittent in nature and occurred at the extremities.5 Particular note was made of a 26-year-old man who had suffered from chronic scrotal oedema since the age of 6 years.5 However, very little information was provided in this review.
Variants affecting function of genes in the Ras–MAP kinase signal transduction pathway have been identified as those responsible for the RASopathies.1 To date, 15 genes have been identified: PTPN11, SOS1, RAF1, KRAS, HRAS, MAP2K1, MAP2K2, NRAS, CBL, SHOC2, BRAF, RIT1,6 A2ML1,7 SPRED1 and NF1. Over half of Noonan syndrome cases are caused by gene defects in PTPN11, which encodes SHP2, a tyrosine phosphatase.8
Cardiofaciocutaneous syndrome (CFC), an autosomal dominant disorder also due to causative genetic variants in the Ras–MAP kinase pathway, is considered to be on the more severe end of the spectrum. It was first described by Reynolds et al.9 Characteristic facies include down-slanting palpebral fissures, macrocephaly and high forehead.10 Congenital heart defects and short stature often feature. The degree of intellectual disability varies, but is generally on the moderate to severe end of the spectrum.10 There are marked similarities between CFC and NS patients, however, CFC patients may have palmoplantar and follicular hyperkeratosis and sparse hair and eyebrows.10 Four genes are known to be involved in CFC: BRAF, MAP2K1, MAP2K2 and KRAS. Gene defects in BRAF are responsible for 30–40% of cases of CFC.11
We report a characteristic lymphatic phenotype associated with the Noonan and CFC spectrum of the RASopathies in a series of 11 cases. This is characterised by lower limb lymphoedema with genital oedema and lymphorrhoea (leakage of lymph or chyle from lymph blisters). The leakage of milky lymph from these blisters is indicative of chylous reflux. Chylous reflux is used to describe a backflow of chyle from its normal route (ie, from the bowel to the cisterna chyli and thoracic duct and then into the blood stream).12
Patients and methods
The ethics for this study is covered by the ‘Analysis of genes and their functions in patients with primary lymphoedema' study, REC Reference: 05/Q0803/267. Eleven patients with Noonan/CFC spectrum disorders attending a specialist primary lymphoedema clinic were located via the genetics database by searching for ‘Noonan syndrome' and ‘lymphoedema'. The hospital records and genetic files were interrogated and information gathered on lymphatic abnormalities and molecular results was analysed. All of the patients were examined and investigated by at least one of the clinicians (PSM, SM, GWB, KG, SJ). Images and results of lymphoscintigraphy and venous duplex scan results were obtained where available.
Molecular results were available for all 11 patients in the following genes: PTPN11 (NM_002834.3, NG__007459.1), KRAS (NM_004985.3, NG_007524.1), BRAF (NM_004333.4, NG_007873.3), RIT1 (NM_006912.5, NG_033885.1). All variants have been submitted to gene specific databases. Patients 1–6 to http://databases.lovd.nl/shared/genes/PTPN11 (Individual IDs:43985-43990), patients 7–8 to http://databases.lovd.nl/shared/genes/KRAS (Individual IDs: 43991-43992), patient 9 to http://databases.lovd.nl/shared/genes/BRAF (Individual ID: 43993) and patient 10–11 to http://databases.lovd.nl/shared/genes/RIT1 (Individual IDs: 43984-43983).
Results
Eleven patients with Noonan/CFC syndrome and persistent lymphatic abnormalities were identified. The details are summarised in Table 1.
Table 1. Summary of clinical information for the 11 NS/CFC patients.
| Case | Sex | Current age (years) | Gene | Exon | Variant | Protein change | Sites affected | Age of onset (years) | Systemic involvement | Complications | Lymphoscintigram results | Venous duplex scan results |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 37 | PTPN11 | 3 | c.181G>A | p.(Asp61Asn) | BLL and genitalia | 27 | Chylous reflux, intestinal lymphangiectasia | Genital lymphorrhoea | Lymph reflux/rerouting. R: popliteal LN present. Contrast in vulva and multiple channels in both legs | Unavailable |
| 2 | M | 19 | PTPN11 | 3 | c.182A>G | p.(Asp61Gly) | BLL and genitalia | 14 | Hydrops fetalis at birth | Genital lymphorrhoea, recurrent cellulitis | Bilateral lymph reflux/rerouting | L: long saphenous vein and R: superficial femoral and popliteal vein incompetence |
| 3 | M | 56 (died) | PTPN11 | 3 | c.188A>G | p.(Tyr63Cys) | BLL and suprapubic swelling | 55 | Bilateral CT, intestinal lymphangiectasia? | Unavailable | Unavailable | |
| 4 | M | 26 | PTPN11 | 7 | c.802G>A | p(.Gly268Ser) | BLL and genitalia | 4 | Bilateral CT | Cellulitis, lymphorrhoea (legs) | L: Lymph reflux/rerouting, popliteal LN present R: functional aplasia | Unavailable |
| 5 | M | 11 (died) | PTPN11 | 13 | c.1504T>G | p.(Ser502Ala) | BLL and genitalia | 6 | Bilateral CT, chylous reflux, pulmonary lymphangiectasia | Genital lymphorrhoea, cellulitis | Unavailable | Normal |
| 6 | M | 63 | PTPN11 | 13 | c.1510A>G | p.(Met504Val) | BLL and genitalia | 53 | Chylous reflux | Genital lymphorrhoea, cellulitis | lymph reflux/rerouting R>L | Sapheno-popliteal junction incompetence with reflux |
| 7 | M | 25 | KRAS | 2 | c.178G>C | p.(Gly60Arg) | BLL and genitalia | 8 | Hydrops fetalis, bilateral CT, chylous reflux, pericardial effusions, intestinal lymphangiectasia | Genital lymphorrhoea, cellulitis | Unavailable | Normal |
| 8 | M | 37 | KRAS | 1 | c.34G>A | p.(Gly12Ser) | BLL and genitalia | 4 | Chylous reflux | Genital lymphorrhoea, plantar warts | Unavailable | Bilateral superficial and deep venous reflux |
| 9 | M | 27 | BRAF | 6 | c.770A>G | p.(Gln257Arg) | BLL and genitalia | 26 | Bilateral pleural effusions, intestinal lymphangiectasia | None noted | Lymph reflux/rerouting, bilateral popliteal LN, contrast in scrotum, multiple widened channels | Left deep venous incompetence with reflux |
| 10 | M | 17 | RIT1 | 5 | c.246T>G | p.(Phe82Leu) | BLL and genitalia | 6 | Bilateral CT, chylous reflux, intestinal lymphangiectasia | Genital lymphorrhoea, cellulitis | L: Lymph reflux/rerouting R: Functional aplasia | Bilateral deep and superficial venous reflux |
| 11 | M | 21 | RIT1 | 5 | c.246T>G | p.(Phe82Leu) | BLL | 17 | Bilateral CT | None noted | Lymph reflux/rerouting, Bilateral popliteal LN present | Unavailable |
Abbreviations: ASD, Atrial septal defect; AVSD, atrioventricular septal defect; BLL, bilateral lower limb; CT, chylothoraces; L, left; LD, learning difficulties; LN, lymph nodes; PS, pulmonary stenosis; R, right; SN, sensorineural.
Clinical details
Patient 1 (female) has facial features consistent with Noonan syndrome, including strabismus, low-set posteriorly rotated ears and hypertelorism. She was diagnosed with pulmonary stenosis, coeliac disease, learning difficulties and menorrhagia associated with factor XI deficiency. There was no swelling at birth, but bilateral lower limb and genital swelling presented at the age of 27 years. Systemically, there was intestinal lymphangiectasia. Vulval lymphangiectasia (lymph blisters) leaked chyle, with fluctuating severity and were treated with laser therapy. Following the introduction of a low-fat MCT diet, she lost 2 kg in five months (predominantly fluid as skin caliber was stable) and there was no further discharge from her vulval lymphangiectasia. Daily incontinence pads were no longer required. The associated itching and soreness also resolved. A previously reported genetic variant (rs397507510) was identified in exon 3 of PTPN11 (c.181G>A; p.Asp61Asn). Parental DNA was not available. No venous duplex results were available. Lymphoscintigraphy was carried out (Figure 3).
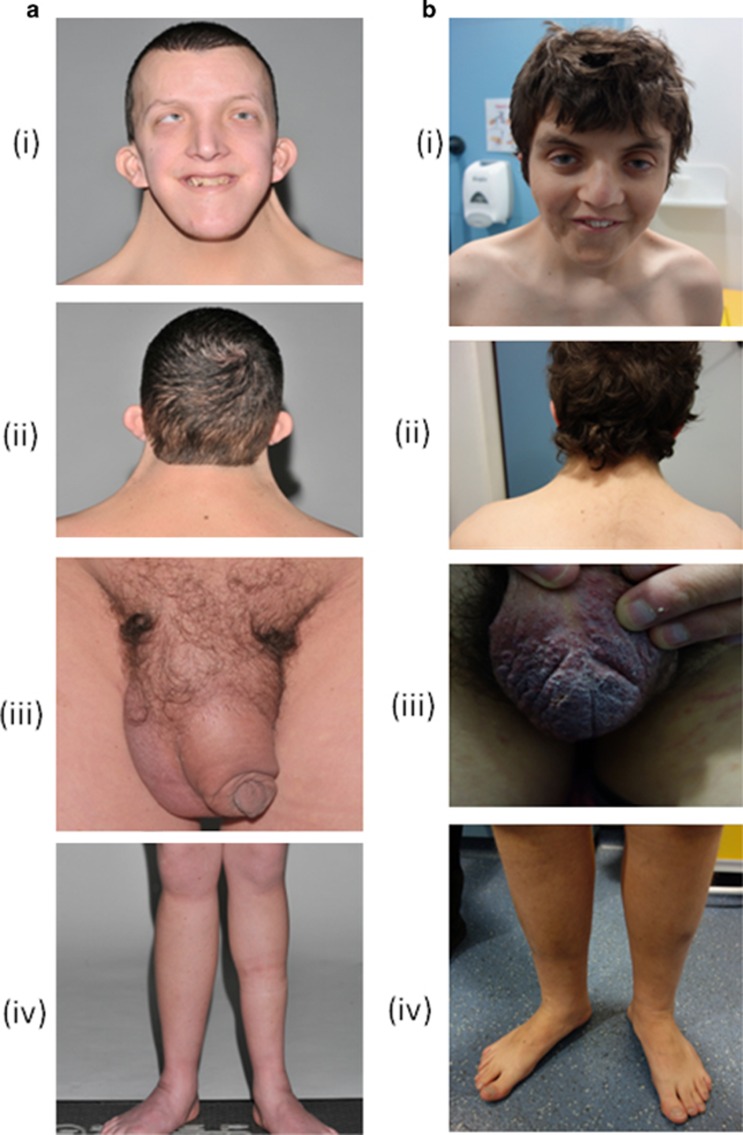
Patient 2 (male) presented antenatally with hydrops fetalis that resolved after birth. He was diagnosed with a hypertrophic cardiomyopathy, which also resolved, atrial septal defect and pulmonary stenosis. A diagnosis of Noonan syndrome was made in infancy based on his facial features (Figure 1), webbed neck and significant feeding difficulties, he required feeding via a gastrostomy until 13 years of age. Other problems include short stature, moderate learning difficulties, congenital hypothyroidism, bilateral cryptorchidism and thrombocytopenia (autoimmune). At the age of 14 years he developed bilateral swelling of the lower limbs and later (17 years) developed lymphangiectasia of the scrotum with intermittent leaking of blood stained fluid. A previously reported heterozygous variant (rs121918461) was identified in exon 3 of PTPN11 (c.182A>G), confirming his diagnosis. Parental DNA was available and it was confirmed the variant was de novo in the patient. Lymphoscintigraphy and venous duplex scans were performed.
Figure 1.
Patient 9 (Ai-iv) and patient 2 (Bi-iv) demonstrating low-set posteriorly rotated ears, neck webbing, low posterior hairline, genital oedema and bilateral lower limb lymphoedema.
Patient 3 (male) had a low posterior hairline, neck webbing and short stature. Intelligence was normal. A congenital heart defect (atrioventricular septal defect) was repaired in childhood but he developed atrial arrhythmias and an atrioventricular valve repair with a maze procedure and epicardial pacing was carried out at age 46 years. At age 49 years, further cardiac surgery was complicated post operatively by a right-sided chylothorax, necessitating thoracic duct ligation and a right pleurodesis. Subsequent pleural effusions were managed with intravenous diuretics. He had recurrent episodes of diarrhoea, not associated with fatty food consumption, raising the suspicion of a protein losing enteropathy. After a 5-week bout of profuse watery diarrhoea, bilateral below-knee pitting oedema developed, along with suprapubic/ lower abdominal lymphoedema at the age of 55 years. He was referred for compression garments. There was no genital, upper limb, facial or truncal lymphoedema. Haemosiderin deposition was noted in his lower limbs, but there were no other clinical signs suggestive of venous incompetence. He was peripherally cyanosed in all four limbs, but pulses were present. Weight loss and poor appetite prompted review with dieticians, but a high-protein diet and nutritional supplements did not alleviate this, and low energy persisted. He received fortnightly albumin infusions to correct low albumin levels. Blood tests revealed elevated B-type natriuretic peptide (BNP) indicating heart failure and abnormal renal and liver function. He became increasingly short of breath on exertion with a nonproductive cough, and basal crepitations were noted. He died at age 56 years of congestive cardiac failure. Nonmelanoma skin cancer of the left preauricular region was identified at age 55 years. A previously reported heterozygous PTPN11 variant (rs121918459) was found (c.188A>G; p.Tyr63Cys). There was no family history of lymphoedema, although his mother has pulmonary stenosis and his brother has a septal defect. They have not been tested for the familial PTPN11 mutation. No venous duplex results or lymph scans were available so it was not possible to confirm the diagnosis of primary lymphoedema. It is possible, therefore, that the leg oedema and pleural effusions were due to his congestive cardiac failure.
Patient 4 (male) has facial features consistent with Noonan syndrome with low-set posteriorly rotated ears, down-slanting palpebral fissures, neck webbing, low posterior hairline, mild pectus excavatum, sensorineural deafness, and short stature with mild to moderate learning difficulties. He presented with feeding difficulties at birth. There was bilateral lower limb swelling (Figure 2) with weeping lymph blisters (lymphorrhoea), and genital swelling from the age of 4 years, which progressively worsened. There was one episode of cellulitis in the more severely affected right leg at age 17 years. Bilateral chylothoraces developed recently. Left orchidopexy was carried out at age 11 years. The diagnosis was confirmed by the identification of a previously reported variant (rs397507527) in PTPN11 exon 7 (c.802G>A; p.Gly268Ser). Parental DNA was not available. Lymphoscintigraphy was performed (Figure 3).
Figure 2.
Patient 4 bilateral lower limb lymphoedema before (i) and after (ii) treatment with compression garments.
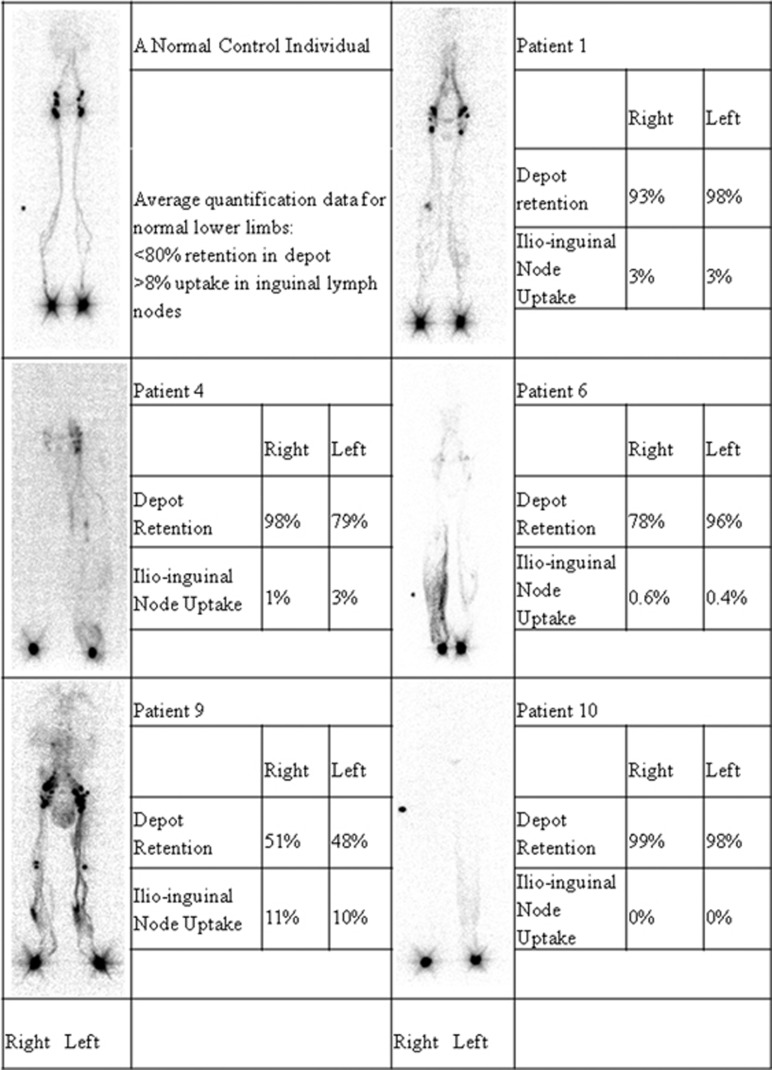
Figure 3.
Lymphoscintigraphy images with quantification at 2 h post injection of 99technetium for a normal control individual and patients 1, 4, 6, 9 and 10.
Patient 5 (male) has low-set posteriorly rotated ears, low posterior hairline, webbed neck, ptosis and short stature. He had a mild pulmonary valve stenosis and an atrial septal defect. He was born at term after hydrothoraces were aspirated in utero. Pleural effusions developed at age 6 years and onset of bilateral lower limb swelling at age 8 years. Scrotal lymph blisters and lymphorrhoea were present. A lung biopsy revealed pulmonary lymphangiectasia. His IQ is normal, although poor concentration has been noted. There was one episode of cellulitis. A previously reported PTPN11 variant (rs121918458) was identified in exon 13 (c.1504T>G; p.Ser502Ala). Parental DNA was available and it was confirmed the variant was de novo in the patient. A venous duplex scan was carried out at the age of 8 years, giving a normal result but no lymphoscintigraphy has been performed. He died unexpectedly at 11 years of age from overwhelming Streptococcus pyogenes septicaemia.
Patient 6 (male) has clinical features of low-set ears, low posterior hairline, neck webbing and medial epicanthic folds. Very little medical history was available. There was no family history of note. Cellulitis in his right leg at 52 years of age was followed ~1 year later by leg swelling. The swelling was complicated by recurrent cellulitis. In recent years, penile and scrotal swelling developed, along with a lymphocele that leaked blood and milky and colourless fluid on an intermittent basis, and which was improved by endovenous laser ablation. On examination, bilateral lower limb swelling was noted, with the right leg being worse than the left. A previously reported heterozygous PTPN11 variant (rs397507547) was identified (c.1519A>G; p.Met504Val). Parental DNA was not available. Venous duplex scans and lymphoscintigraphy were performed (Figure 3).
Patient 7 (male) presented with dysmorphic facies typical of CFC with low-set posteriorly rotated ears, and hypertelorism. Other features present were hypertrophic cardiomyopathy and pulmonary stenosis, wide carrying angle, strabismus, moderate learning difficulties and hearing loss. Atypically, he also had proptosis and craniosynostosis with hydrocephalus. He was noted to be oedematous in the neonatal period due to nonimmune hydrops fetalis, but this resolved. Lymphoedema involving both lower limbs and genitalia developed at the age of 8 years. Bilateral chylothoraces developed at age 11 years following a chest infection, and was treated with prednisolone, vancomycin and drainage. There was a subsequent chylothorax episode at age 20 years. Other complications included recurrent cellulitis in the swollen legs, diarrhoea due to the intestinal lymphangiectasia and genital lymphorrhoea due to chylous reflux. A previously reported variant (rs104894359) in exon 2 of KRAS (c.178G>C; p.Gly60Arg) was identified. Parental DNA was unavailable. Venous duplex scanning was carried out.
Patient 8 (male) had typical facial features of CFC including low-set posteriorly rotated ears and down-slanting palpebral fissures. Also noted were short stature, strabismus, moderate learning difficulties, delayed puberty, keratosis pilaris, small disc colobomata, and a thickened pulmonary valve. He suffered from childhood myeloid leukaemia (the specific type is not documented) at 4 months of age. Bilateral lower limb and genital swelling developed at the age of 4 years, with genital lymphorrhoea due to chylous reflux. Scrotal reduction surgery reduced chyle leakage from the scrotum, but occasional penile leakage persists. A previously reported variant (rs121913530) was identified in KRAS in exon 1 (c.34G>A; p.Gly12Ser). Parental DNA was not available. Lymphoscintigraphy images were unavailable. Venous duplex scans were performed.
Patient 9 (male) has typical facies, with moderate ptosis, down-slanting palpebral fissures, low posterior hairline, neck webbing, low nasal bridge, bilateral epicanthic folds, multiple lentigines and low-set posteriorly rotated ears (Figure 1). He has short stature, despite treatment with growth hormone. Pectus carinatum and excavatum were also noted. There was mild polyhydramnios during pregnancy. He was born at 35 weeks, with a normal vaginal delivery. A murmur was noted at 2 weeks, leading to a diagnosis of hypertrophic cardiomyopathy, which resolved. He had severe feeding difficulties during the first year of life, necessitating feeding via a gastrostomy until the age of 4.5 years. He had delayed developmental milestones and mild to moderate learning difficulties. He developed pubertal onset epilepsy. There is no family history of similar problems. Onset of lymphoedema was at age 26 years, starting with genital swelling, and progressing to include bilateral lower limb lymphoedema within 2 months, extending as far as the thighs. No chylous discharge or lymphangiectasia has been noted. Recently, he developed bilateral pleural effusions and evidence of a protein losing enteropathy with low albumin, low immunoglobulins and raised faecal alpha trypsin levels. A low fat, high-protein diet is being introduced. A heterozygous variant was identified in BRAF exon 6 (c.770A>G; p.Gln257Arg). Parental DNA was available and it was confirmed the variant was de novo in the patient. Venous duplex scanning and lymphoscintigraphy were carried out (Figure 3).
Patient 10 (male) displayed clinical features that included low-set posteriorly rotated ears, low posterior hairline, short stature (treated with growth hormone), wide-spaced nipples, short neck and pulmonary stenosis. He has adrenal insufficiency and low factor VII. Increased nuchal translucency was noted in utero. There was also in utero hydronephrosis. A bilateral orchidopexy for undescended testes was carried out at 15 months. The onset of swelling was at 6 years of age with bilateral lower limb and genital involvement. Systemic involvement included intestinal lymphangiectasia with chylous reflux, and hence, he was started on a low fat, high calorie, high-protein diet. Chylothoraces occurred at 18 years of age, requiring VATS (video-assisted thoracoscopic surgery) pleural biopsy and bilateral talc pleurodesis. The lower limb lymphoedema was complicated by recurrent cellulitis and genital lymphorrhoea, which consisted of penile and scrotal oedema with chylous reflux and lymphangiectasia. Prominent lymph blisters on the scrotum leaked chyle on an almost daily basis. Skin graft surgery alleviated this and the lymphorrhoea is now minimal, however, he continues to experience lymphoedema of the mons pubis. A previously reported RIT1 germline variant (rs730881014) was identified in exon 5 (c.246T>G; p.Phe82Leu). Lymphoscintigraphy (Figure 3) and venous duplex scans were performed.
Patient 11 (male) presented with low-set posteriorly rotated ears, short-webbed neck, ptosis and mild pulmonary stenosis. At birth, lymphoedema was noted, along with a chylothorax that was drained twice in the special care baby unit. There was no leg oedema or ascites at that time. At the age of 17 years, he developed bilateral lower limb lymphoedema, but there has been no genital involvement. He underwent testosterone treatment at age 17 years. He had undescended testes and bilateral inguinal herniotomy and orchidopexy at around age 3 years. Recently, he has developed bilateral pleural effusions. No problems with hearing or eyesight have been noted, and normal developmental milestones were reached. A previously reported RIT1 variant (rs730881014) was identified in exon 5 (c.246T>G; p.Phe82Leu). Parental DNA was available and it was confirmed the variant was de novo in the patient. Lymphoscintigraphy was carried out.
All 11 patients had bilateral lymphoedema of the lower limbs. Onset of lymphoedema ranged from 4 to 55 years, with a mean of 20 years and a median of 14 years. Nine had swelling of the genitalia, all 11 had systemic involvement (four, possibly five, were confirmed to have intestinal lymphangiectasia, six had chylous reflux and six had chylothoraces). There was also one biopsy confirming pulmonary lymphangiectasia. Three (Patients 7, 9 and 10) had a progressive form of lymphatic dysplasia with the development of chylothoraces, (two requiring bilateral pleurodeses) and worsening protein losing enteropathy. Interestingly, 10 of the 11 patients were male.
Lymphoscintigraphy results
Lymphoscintigraphy is the gold-standard investigation for lymphoedema. A representative image of the lymph drainage pathways is created using a gamma camera following an interdigital injection of a radiolabelled tracer (99technitium). Images are taken at 15 min and 2 h. Lymph transport was determined by calculating the % of tracer, relative to amount injected, accumulating in regional lymph nodes by 2 h (>8% normal; <3% lymphoedema; 3–8% indeterminant).
Unfortunately, lymphoscintigraphy is not routinely performed in patients with Noonan syndrome and some reports/images have been lost. Results were available for seven (patients 1, 2, 4, 6, 9, 10 and 11). Figure 3 shows the qualitative images and quantification at 2 h for Patients 1, 4, 6, 9 and 10. Dermal rerouting was a common feature and interpreted as reflux, particularly when the scrotum was seen in profile, as reflux would be the only explanation for such a finding. The consistent clinical complication of chylous lymphorrhoea in the genital area is highly suggestive of reflux.
For Patient 1, lymphoscintigraphy at 2 h shows presence of contrast in the vulva and multiple lymphatic channels in each leg suggest lymph reflux. In addition, there is a popliteal lymph node on the right, which also indicates deep rerouting/reflux (Figure 3).
Lymphoscintigraphy for Patient 2 at 2 h demonstrates bilateral lymph reflux/ rerouting.
Lymphoscintigraphy for Patient 4 at 2 h shows numerous lymphatic drainage tracts with visualisation of the popliteal nodes and an outline of the left leg, indicative of reflux or rerouting. The right leg shows no main tract definition (Figure 3).
Patient 6's lymphoscintigraphy showed impaired lymphatic drainage in both lower limbs, with evidence of dermal rerouting/reflux in the right calf and some pooling of activity in the left calf (Figure 3).
Lymphoscintigraphy for Patient 9 shows presence of contrast in the scrotum and multiple widened channels, suggestive of lymph reflux. Bilateral popliteal nodes indicate deep rerouting or reflux. Quantification is normal despite abnormal images suggestive of reflux (Figure 3).
For Patient 10, lymphoscintigraphy at 2 h shows an outline of the left lower leg suggestive of rerouting of the lymphatics. Lymph drainage in the right lower limb was not visualised suggesting poor lymph absorption and drainage (Figure 3).
Patient 11 was reported to have bilateral rerouting or reflux of lymph in the lower limbs. There was bilateral popliteal lymph node uptake.
Venous duplex scan results
Noninvasive doppler waveform analysis was performed on seven patients (Patients 2, 5, 6, 7, 8, 9 and 10), and in five of these there was a pattern consistent with bilateral venous incompetence with reflux. In Patient 2, venous duplex scanning confirmed incompetence in the left long saphenous, right superficial femoral and popliteal veins. In two patients (5 and 7) the results were normal.
Discussion
Lymphatic disorders are a well recognised complication of the RASopathies. Antenatal presentation of an increased nuchal translucency, hydrothoraces or hydrops fetalis are common in these disorders and represent abnormalities in lymphatic development. Some of the characteristics of this condition, webbed neck, low-set ears, low hairline and ptosis may be related to in utero oedema.13 Although swelling of the feet at birth is frequently described in NS/CFC, persistent lymphatic disorders are rare. This observational study is limited by the small numbers of patients, however, it identifies a specific lymphatic phenotype associated with the NS/CFC spectrum of the RASopathies characterised by childhood or adult onset of bilateral lower limb lymphoedema (11/11 (100%)), genital oedema (9/11 (82%)) and chylous reflux with lymphorrhoea particularly in the genital area (8/11 (73%)). There is frequent systemic involvement including intestinal lymphangiectasia and/or chylothoraces. Swelling of the face or upper limbs was not observed in this small cohort. The age of onset varied, ranging from 4 to 55 years of age in our patients. The lymphatic disorder may be progressive with onset of chylothoraces, sometimes requiring pleurodesis, and protein losing enteropathy. These complications should be actively investigated and if present, a low fat, high protein, high-calorie diet may be beneficial. Management of these patients is still confined to physical measures such as compression garments and bandaging. A low fat diet or cryotherapy may be effective in reducing the genital lymphorrhoea and debulking may help with the genital oedema.
Venous duplex scanning revealed superficial venous reflux. Lymphoscintigraphy shows abnormalities consistent with reflux. Chylous reflux with genital lymph leakage (or lymphorrhoea) is a major problem for these patients. The presence of chylous reflux and lymphorrhoea in the genitalia, together with the venous incompetence and reflux seen on lymphoscintigraphy are highly suggestive of reflux being the underlying abnormality in this cohort of patients. It is not clear whether the primary problem is an abnormality of the valves in the lymphatics and veins, or whether the reflux in the legs and genital region is a result of the chylous reflux from the intestines. It is possible that there is an underlying weakness or abnormality in the cisterna chyli or thoracic duct, however, visualisation of the internal lymphatics is very limited, so the mechanism of this presentation is still not understood. It is also unclear why this presents in childhood or adulthood; the triggers are not known.
It is of interest that 10 of these 11 patients were male and it is possible that males with NS/CFC syndrome have a higher incidence of persistent lymphatic abnormalities. However, with such a small cohort, it is difficult to show statistical significance.
PTPN11 variants affecting the function of the gene were identified in 6 of the 11 patients, (~55%).8 Other germline variants were represented in this cohort including two patients with KRAS, one with a BRAF and two with RIT1. A previously reported case of a RASopathy with bilateral lower limb lymphoedema was associated with a germline CBL mutation.14 This suggests there is no genotype–phenotype correlation with this presentation of lymphatic disorder.
In summary, within the patient group studied, a consistent pattern of lymphatic abnormality was seen: lower limb lymphoedema with variable age of onset, and genital involvement with chylous reflux.
Acknowledgments
We thank all the patients who took part in this study and the Noonan Syndrome Association who sponsored this study.
The authors declare no conflict of interest.
References
- Rauen KA: The RASopathies. Annu Rev Genomics Hum Genet 2013; 14: 355–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts AE, Allanson JE, Tartaglia M, Gelb BD: Noonan syndrome. Lancet 2013; 381: 333–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tartaglia M, Zampino G, Gelb BD: Noonan syndrome: clinical aspects and molecular pathogenesis. MolSyndromol 2010; 1: 2–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witt DR, Hoyme HE, Zonana J et al: Lymphedema in Noonan syndrome: clues to pathogenesis and prenatal diagnosis and review of the literature. Am J Med Genet 1987; 27: 841–856. [DOI] [PubMed] [Google Scholar]
- Smpokou P, Tworog-Dube E, Kucherlapati RS, Roberts AE: Medical complications, clinical findings and educational outcomes in adults with Noonan syndrome. Am J Med Genet Part A 2012; 158A: 3106–3111. [DOI] [PubMed] [Google Scholar]
- Aoki Y, Niihori T, Banjo T et al: Gain-of-function mutations in RIT1 cause Noonan syndrome, a RAS/MAPK pathway syndrome. Am J Hum Genet 2013; 93: 173–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vissers LE, Bonetti M, Paardekooper Overman J et al: Heterozygous germline mutations in A2ML1 are associated with a disorder clinically related to Noonan syndrome. Eur J Hum Genet 2014; 23: 317–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tartaglia M, Mehler EL, Goldberg R et al: Mutations in PTPN11, encoding the protein tyrosine phosphatise SHP-2, cause Noonan syndrome. Nat Genet 2001; 29: 465–468. [DOI] [PubMed] [Google Scholar]
- Reynolds JF, Neri G, Hermann JP et al: New multiple congenital anomalies/ mental retardation syndrome with cardio-facio-cutanous involvement. Am J Med Genet 1986; 23: 413–427. [DOI] [PubMed] [Google Scholar]
- Nava C, Hanna N, Michot C et al: Cardio-facio-cutaneous and Noonan syndromes due to mutations in the RAS/MAPK signalling pathway: genotype-phenotype relationships and overlap with Costello syndrome. J Med Genet 2007; 44: 763–771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee BH, Kim JM, Jin HY et al: Spectrum of mutations in Noonan syndrome and their correlation with phenotypes. J Paediatr 2011; 159: 1029–1035. [DOI] [PubMed] [Google Scholar]
- Kinmonth JB, Taylor GW: Chylous reflux. Br Med J 1964; 1: 529–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opitz JM: On congenital lymphedema. Am J Med Genet 1986; 24: 127–129. [DOI] [PubMed] [Google Scholar]
- Hanson HL, Wilson MJ, Short JP et al: Germline CBL mutation associated with a noonan-like syndrome with primary lymphedema and teratoma associated with acquired uniparental isodisomy of chromosome 11q23. Am J Med Genet A 2014; 164A: 1003–1009. [DOI] [PubMed] [Google Scholar]