It is now known that nearly half of the toll that illness takes in developed countries is linked to four unhealthy behaviors: smoking, excess alcohol intake, poor diet, and physical inactivity. These common risk behaviors cause preventable, delayed illness that then manifests as chronic disease, requiring extended medical care with associated financial costs. Chronic disease already accounts for 75% of U.S. health-care costs, foreshadowing an unsustainable financial burden for the aging population [1]. We are facing an urgent need to re-engineer health systems to improve public health through behavior change, and technology-supported behavioral change interventions will be a part of 21st-century health care. As new technical capabilities to observe behavior continuously in context make it possible to tailor interventions in real time, the way we understand and try to influence behavior will change fundamentally.
Health Behavioral Change intervention Theory
The goals of health behavioral interventions are to spark and sustain health-enhancing activities, such as exercising and using sunscreen, and stop health-compromising behaviors, such as tobacco use and excessive alcohol intake. Similarly, preventive interventions are designed to discourage unhealthy habits before they start. Applying theory is useful because it is well established that interventions based on theory are more effective at modifying behavior than those not based on theory [2]. Most behavioral interventions derive from social science theories that posit how different individual, community, and environmental factors influence behavior and the mechanisms whereby altering these factors will bring about behavior change. Each theory specifies a set of abstract concepts (constructs), related measurable variables, and a set of propositions that systematically explain how these concepts are interrelated. Thus, health behavioral theories predict how applying an intervention (input) will drive change in underlying behavioral mechanisms or determinants (mediating constructs) that will in turn drive health behavioral change (output).
For example, the health belief theory proposes that a person’s odds of discontinuing an unhealthy behavior are jointly determined by his expectations about perceived susceptibility to illness, perceived severity of illness, and perceived value (benefits and barriers) of giving up the behavior. Since the 1950s, this theory has guided most behavior change counseling performed in general medical practice. Social cognitive theory, the health behavioral theory most extensively applied in behavioral research today, posits that a person’s odds of initiating a behavior are determined predominantly by his confidence about being able to perform the behavior (self-efficacy) and beliefs about the probability and value of the behavior’s consequences (outcome expectancies).
These theories have done a good job at guiding behavioral change approaches that made use of conventional assessment and interventional technologies. Their cause-and-effect models are largely static, assuming a single set of mediating causal pathways, rather than dynamic feedback loops or evolution of changing determinants over time. Most theories make some mention of environmental determinants (e.g., the health beliefs theory includes cues to action; the social cognitive theory posits reciprocal determinism, whereby people both choose and are acted upon by their environments). However, the vast majority of causal constructs in these theories are intrapsychic, conscious, somewhat vaguely specified processes whose quantitative relationship to health behavioral change is only imprecisely specified.
Because intervention has been predictable, fixed, and protocol driven rather than response dependent, assessment of mediators has only needed to be done infrequently (e.g., baseline and follow-up). For example, a smoking cessation treatment that is based on the social cognitive theory will be implemented based on the fixed sequence of sessions specified by the treatment manual, rather than changing dose or technique in response to fluctuations in a client’s self-efficacy to quit. Indeed, the main reason why mediators have been assessed in the past has been to determine, after the fact, whether any change in the targeted health behavior could be accounted for statistically by change in the mediator.
Fast-forward now to the current era of mobile technologies that allows continuous recording of both objective and subjective data. These tools, and the engineers and computer scientists who developed them, introduced behavioral scientists to new interventional capabilities and a different approach to causal modeling. From our professional vantage points in psychology, design, and engineering, we discuss how the interjection of continuous monitoring technologies is likely to disrupt health behavioral change theory and treatment—for the better, we think.
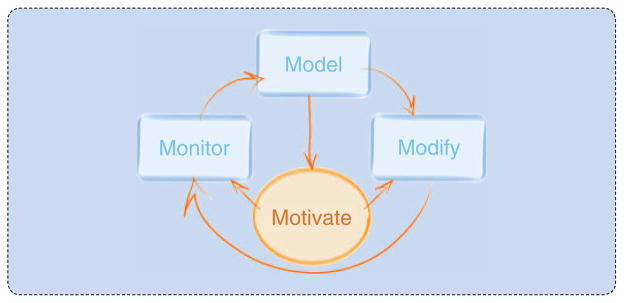
Changing a deeply ingrained health risk behavior requires addressing what we conceptualize as the “4 Ms”: monitoring, modeling, motivating, and modifying (Figure 1). Monitoring (measuring) is needed to track if and how behavior changes in response to an intervention and whether the theorized mediators change in parallel. The highly granular information afforded by new wearable, wireless, and digital technologies (sensors, beacons, and smartphones) can help build a model of how the behavior truly works in real time—what prompts it; when, where, and with whom it occurs; and what the person is feeling and thinking before and after the behavior.
FIGURE 1.
Changing a long-standing health risk behavior requires addressing the “4 Ms”: monitoring, modeling, motivating, and modifying.
To collect the rich data needed to launch into modeling and then intervention, we must first address motivation. Motivation is the engine that drives the entire behavior change undertaking because it is the energizing force that catalyzes and sustains an organism’s goal-directed behavior. Motivation plays a critically important double role in behavioral change intervention. First, motivation influences a person’s willingness to engage with self-monitoring his own behavior or being monitored by someone else. Privacy concerns, burden, personal temperament, and the extrinsically rewarding or persuasive features of a technology all enter the equation here. Unless this initial motivational engagement challenge can be overcome, the behavior change game is over because it will not be possible for ubiquitous technologies to monitor behavior to determine whether a change has occurred. Second, motivation enters our conceptual model at a later point. There, motivation reflects the person’s volition to cooperate with the intervention and modify the targeted behavior as intended, rather than pushing back to resist change.
Monitoring
Until now, our understanding of human behaviors has been based on snapshots in time, such as a questionnaire completed once (or even several times), direct observation for short periods of time, or an interview. The models we built from such data did not reflect how behaviors were elicited by circumstances or time, or how they changed throughout the day. For the most part, they were based on self-reported measures that are subject to several forms of bias, including the fact that people forget answers to some questions, such as: how many hours of television have you watched this week? They may not know the answers to other questions, such as: how many minutes did you spend in moderate-to-vigorous physical activity yesterday? Sometimes people are hesitant to answer questions (for example, about drug usage), and sometimes they answer dishonestly to portray themselves in a positive light.
New technologies, such as the smartphone and wearable, implantable, and environmental sensors have revolutionized our ability to monitor peoples’ behavior and the ability of people to monitor their own behavior in real time. These technologies allow us to reduce participant bias by objectively measuring such behaviors as physical activity, smoking, place, time spent in various activities, and so forth. Data can be collected through combinations of ubiquitous mobile, body, and environmentally embedded devices that people wear, use, and otherwise encounter throughout their day and night. People leave a broad swath of digital footprints: through Internet use, credit card purchases, entrance and exit scanners, and the like. These traces let us measure things that we never thought to measure (and thus never included in our earlier models of behavior).
This deluge of data tells us more about peoples’ behavior than we ever imagined we could know a decade ago. Although we still rely on self-reported measures for some things (for instance, there is no objective measure of “toothache”), we now can elicit self-reported measures at designated times, in prespecified locations, or in reaction to key events using a combination of sensors and cell phone technologies. The ability to collect such a rich array of objective and subjective measures in real time and context provides unprecedented opportunity to develop more sophisticated causal models of what, how, who, when, where, and, ultimately, why behaviors occur and shift.
For instance, if global positioning system (GPS) sensors in your phone or fitness device let us know that you are entering a fast food restaurant, we can make this time-and-location-stamped data quickly available for analysis on a smartphone, the cloud, or a back-end secure server. That enables us to apply the method of ecological momentary assessment, whereby your smartphone “pings” you to ask if you are hungry or stressed, or what you plan on buying. Through this combination of technologies and methods, we can begin to form a rich and detailed picture of how your feelings, thoughts, and behaviors affect each other that is accurately placed in time, and in social- and built-environmental context. As discussed later in this article, we can apply analytical and simulation techniques to these data to develop dynamic models of health behavior determinants that help us adapt to intervention strategies in real time.
Two other types of life record—health and entertainment—afford additional opportunities to monitor very diverse data on human behavior. Many health systems have already implemented electronic health records (EHRs) that can be tapped to guide intervention both at the point of care and beyond it. For example, by depicting information about food stores in a patient’s neighborhood, some EHRs equip providers to deliver context-sensitive counseling about how to make healthier eating choices. Other EHRs offer patients a special portal to transmit data continually about their glucose level, weight, physical activity, and diet. Giving health professionals access to these digital data and letting patients know that caring staff are looped in creates a technology-supported behavior change system that can be highly effective. Knowing that a coach is monitoring and supporting their behavior change efforts keeps patients accountable and reinforced for staying on track to meet their goals. Mining the data generated by such a system makes it possible to derive algorithms that detect periods of risk so that an intervention can be triggered before an unhealthy behavior pattern can take hold. For example, if the weight of a formerly obese patient starts to creep back up during weight-loss maintenance, we can prompt the patient to make small adjustments in sleep, diet, and exercise behaviors to preempt the return of obesity.
It may seem odd to suggest that data from entertainment usage be combined with that from medical records to model information about health behaviors. Yet it makes perfect sense. Digital data about the type of entertainment we choose and how we consume it is abundantly available and greatly underutilized. Through back-end technologies, we know much about the games people play, when, and with whom. Our selections of streaming video and music convey information about our frame of mind and our emotional and cognitive well-being. Whether we choose to watch a comedy, a horror flick, religious programming, or a documentary says something about our mood at the time of making the choice. Moreover, our pattern of media consumption and the behaviors we pair with being entertained can feed back to influence affective tone. For example, binge watching several films in a row while sitting on the couch consuming pizza, beer, and chocolates suggests the onset of a downward spiral that involves a cascade of health-compromising behaviors. Being able to capture and model such sequences of health-compromising behaviors opens the possibility of being able to disrupt the pattern to interject healthier habits.
Modeling
Our new access to data about sequences of cues and behavioral response patterns that recur throughout the day permits the development of dynamic relational computational models. Such data-driven models depict how behaviors link dynamically to events in the person’s physiology, psychological state, and surrounding social and physical contexts. Extracting patterns from the obtained data allows behaviors, emotions, and urges to be inferred and classified, offering a high-level interpretation of the data. Recording behaviors together with time and location stamps adds contextual data that enriches the model sufficiently to allow intelligent prediction of the precise moment and place in the social–emotional–physical space when intervention can optimally be delivered.
At this point, we can apply control systems engineering principles [3] to design and implement a behavior change system that is optimized to deploy finely tailored, properly dosed, just-in-time bouts of intervention at the precise moment and context when they will be maximally effective at influencing your behavior. Consider, for example, the scenario of a recovering cocaine user whose voice samplings indicate that he had an argument with his employer earlier in the day and whose respiratory and heart rate patterns suggest lingering signs of stress. The GPS on his phone now shows him to be driving toward a part of town where he has previously purchased drugs. Our model predicts that the precipitating conditions are present to trigger an urge to use cocaine, and, moreover, that a facilitating environment of drug access is about to be present. Armed with such a model, a human coach, an avatar, or the technology itself can apply an assortment of prompts, nudges, or back-pats to preempt risk behaviors and reinforce healthier responses. We can monitor the behavioral outcomes of this experiment to determine if positive change occurred and build what we learn into the next version of our predictive model. Then, we can continue to test and modify our model linking risk behaviors to their triggering cues and contexts until we can predict and preempt risk behaviors with great precision.
The information derived from continuous observation and modeling also can be used at the macrolevel by health institutions and policy makers. Technologies that supply data storms from large numbers of individuals make it feasible to create snapshots of the behavior of entire populations. Recent advances in systems science [4] and social simulation now allow us to connect these temporally dense snapshots, coming from the observed data, into predictive models that simulate populations as dynamical networks whose shapes change as new behavior patterns emerge and shift. At a pragmatic level, the ability to perform data-based simulations of complex systems enables decision makers to try out and adjust potential policies and interventions in simulated reality before implementing programmatic change in the real world. That capability helps decision makers envision both the intended positive consequences and any unintended adverse ones they should anticipate from applying a contemplated health promotion strategy to a population.
Thus far, we have discussed modeling as if the process could be reduced to a series of programming operations that occurs quasi-magically under the hood of a computer. It is easy to forget that the programming operations that translate data into models are crafted by human beings who select and interpret data through the lens of their prior experiences and beliefs. Increasingly, public opinion holds that health promotion is everybody’s business. That is, the responsibility for inculcating and sustaining healthy lifestyles extends beyond the individual or the doctor–patient dyad to include families, communities, social institutions, and the government. Hence, there are more stakeholders whose insights and purviews on data about behavioral determinants add value and need to be taken into account.
The need to determine which data should be presented to which user, when, and how has made data visualization and visual analytics a ripe area for design and development. The dialectical relationship between viewers and data presents many nuances in how audiences differing in demographic attributes and expertise perceive and interpret information. To engage these diverse and important audiences in filtering, curating, interpreting, and using data displays is a challenge that 21st- century model building still needs to address.
Two groups of stakeholders that collaborate to develop technology supported behavioral change interventions are behavioral scientists and computer science engineers. The approach to modeling in these two disciplines reflects divergent methodological traditions. Behavioral scientists on the team are usually puzzled by the absence of theorized mediating mechanisms in engineering models of behavior change. Conversely, like the computer scientist depicted in Figure 2, team members from engineering express frustration about how to specify computational relationships among the numerous fuzzily defined concepts in behavioral science theory.
FIGURE 2.
A computer scientist tries to grasp a behavioral scientist’s approach to modeling. Behavioral science theories are models that are specified in advance to guide the design of an intervention. Even though the theory usually lacks quantitative details, behavioral interventions based on theory are more effective at changing behavior than those not based on theory.
Like the health beliefs, social cognitive and other theories used by behavioral scientists, the computational models that engineers derive (from analysis of continuous observations) depict an understanding of the web of influences that surround a health behavior. The difference is that computational modeling is driven descriptively from the bottom up by the obtained data, consistent with methodological tradition in engineering science, rather than top down by a set of constructs and propositions that predicts a priori how the data should look, consistent with methodological tradition in behavioral science. Studies of team science suggest that this type of challenging dialogue across different scientific disciplines can produce transformative change and scientific breakthroughs so long as diverse collaborators persist in trying to develop a shared mental model of their work.
A fruitful and needed outcome of such interdisciplinary cross-talk should be to bring 20th-century behavioral theories up to the task of guiding intervention delivery in the age of mobile technologies and mobile-enabled interventions. Existing behavioral change theories have in many respects become ossified, failing to be revised or refuted by the emergence of data that contradict them. We can now construct new, more dynamic descriptive models of how behavior works using technology-enabled denser, richer, continuous storms of data than have previously been available. For these developed, ground-up descriptive models to achieve generalized utility beyond a specific local context; however, we have to restore the appropriate iterative relationship among data, modeling, and theory. As the engineer in Figure 2 is attempting to do, a scientist ought to be able to express behavioral science theory quantitatively in computational models that can be tested through simulation and real-world application. The results of such testing need to iterate back to inform revision of not only the computational model but also ultimately the theory so that behavioral science theories remain viable and useful.
Motivating
As the force that drives goal-directed behavior, motivation is integral to the entire endeavor of understanding, changing, and maintaining health behavior. Three main challenges need to be addressed: motivating people to self-monitor their behavior (or be monitored by someone else), motivating them actually to change their behavior, and motivating them to maintain positive behavior change. Because different people are motivated differently, personalization is the key to maintaining diverse participants in the cycle of continuous observation and real-time adaptation.
The self-monitoring required by behavioral change techniques traditionally has been highly burdensome. Until passive sensing technologies became available, self-monitoring necessitated keeping detailed paper records of target behaviors (eating, activity, or substance use) throughout the day and also noting the antecedents and consequences of each bout of behavior. Getting feedback about behavior change required analyzing and manually plotting the data, or waiting for an appointment with a specialist who did so. It was the rare individual who enjoyed doing this kind of self-monitoring. Recent developments in technology have, however, made it easier to motivate people to engage actively in self-monitoring. Indeed, those who affiliate with the quantified self movement find it inherently reinforcing to use self-tracking tools. Many say that self-tracking helps them attain self-knowledge through numbers. Self-measuring clearly can become intrinsically motivating by leveraging people’s inherent desires for competence and competition.
Although engaging design features embedded within a technology help facilitate uptake, it is not solely the physical attributes of the technology that heighten peoples’ desire to engage but rather the way these features interact with users’ psychological predispositions. For example, a successful system might combine several new technological capabilities and incorporate a menu of assets such as a playful interface and microeconomies, or a compelling story that leverages people’s intrinsic desires to be entertained, to participate in narrative, and to generate or be told a story. Intuitive interaction, appealing user interfaces, variety in incentives, scripted storytelling or user-generated narrative, characters that empathize with users, characters that users can empathize with, fantasy worlds that can be explored, or real worlds that can be augmented—these are all ingredients that can influence the success of a designed experience [5].
The self-determination theory of motivation posits that human beings have three innate developmental needs: competence, autonomy, and relatedness. The need for competence is reinforced by feelings of mastery that result from experiences that increase our knowledge and skills. The need for autonomy is grounded in the desire to act of our own free will without the direct intervention of others. We all have a desire to be causal agents of our own lives, acting with a feeling that we are in full volitional control [6]. Indeed, for some individuals, the perception of being controlled by others is sufficient to provoke reactance [7], an aversive feeling of being externally controlled that motivates the person to push back and resist intervention. Interventions that neglect this principle are likely to face serious problems with continuing usage (compliance). For example, having your mobile telephone always tell you as you walk into an ice cream shop that you should not indulge might be a nice gimmick initially but may ultimately lead to irritation and a smashed smartphone rather than behavior modification. Less commanding messages that suggest options and ask what you prefer are likely to be better received and more effective.
Importantly, the needs to experience competence and autonomy do not suggest needs to be independent of others. Quite the contrary, a third fundamental need is to feel meaningfully connected with others. Current technologies allow people to share data about their health behaviors almost in real time with others in an extended social network. Social media, including blogs, tweets, and virtual social networks, let us share information about our actions with a large population of friends, family, health-care providers, and even strangers. Broadcasting our behavioral data serves many different motivational functions. For example, social sharing allows us to elicit encouragement and emotional support from peers, who may also help by holding us accountable for meeting our goals. The ability to perform social comparisons against others is informative and can spur competitive motivation to surpass the performance of networked others, potentially energizing the entire group.
Modifying
Since the goal of health behavioral intervention is to effectively modify health-compromising actions, we conclude by discussing how technology-supported interventions produce positive behavior change. In the language of behavioral science theory, which mechanisms mediate improvement? Despite all the novel, exciting features offered by new technologies, we do not believe that widgets, in and of themselves, magically modify behavior. Technologies merely offer affordances [8] that allow people to perform an action in relation to a device. A pedometer affords walking and receiving feedback about step counts. A pedometer purchased and kept in a drawer will not increase walking because the device is not magical. However, a worn pedometer may increase walking because wearing the device allows walking to trigger feedback, which reinforces more walking. As the example illustrates, the sensors and devices incorporated into effective technology-supported treatments largely serve as channels to deploy the validated behavior change principles set forth in health behavioral theories. Technologies work to modify behavior when they afford the user a relationship with a system that activates effective behavior change mechanisms.
Consider the ENGAGED weight loss app [9], shown in Figure 3, an enhanced Android version of an effective mHealth program for weight loss [10]. The app is part of a technology-supported system that the first author and her colleagues developed to deliver the Diabetes Prevention Program (DPP), a gold standard intensive lifestyle intervention to treat obesity. The DPP applies a number of effective behavior change techniques drawn from social cognitive theory. The first, self-monitoring (of food intake and exercise), is a staple of behavior change techniques. Doing this kind of monitoring, usually in and of itself, improves problematic behaviors, probably by heightening awareness of them.
FIGURE 3.
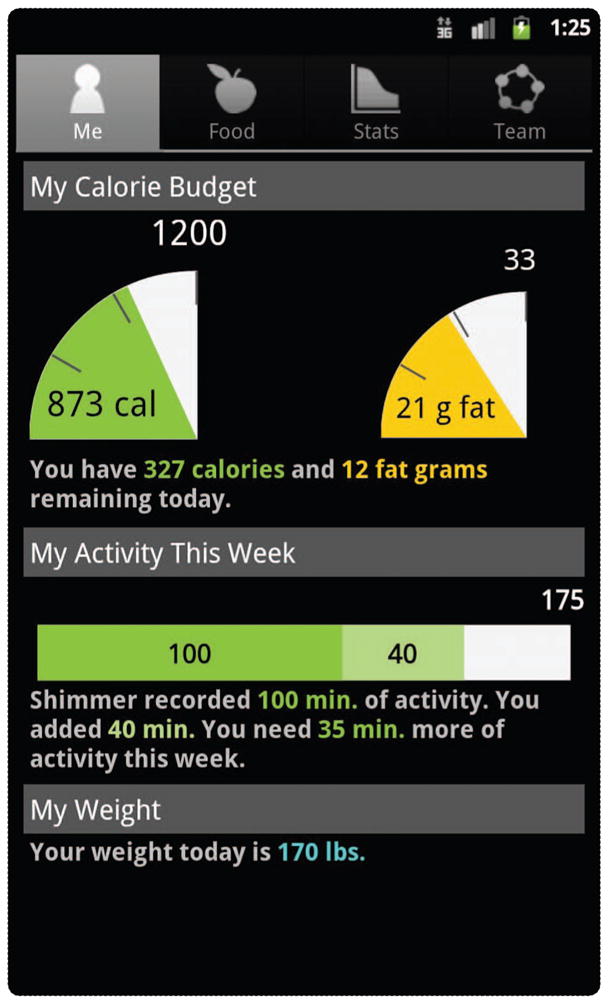
The smartphone display for the ENGAGED weight loss app [9]. Fans coded in traffic light colors show how much you have already eaten today relative to your daily allowances for calories and fat. The green fan signifies that you can still eat 327 more calories today. However, if you enter the steak that you are thinking about ordering, the fan will turn bright red. You can top up the green physical activity thermometer by accumulating more minutes of moderate intensity exercise until you reach your weekly goal. Wearing the study accelerometer lets your minutes of activity accumulate automatically, but if you forget to wear it, you can get credit (in lighter green) by entering your exercise manually.
The second technique, goal setting, specifies the target behaviors needed to achieve the valued health outcome: for DPP, the targets are daily calorie and fat intake allowances and physical activity goals. Participating in the DPP traditionally requires people to use paper and pencil to write down everything they eat. Only later when they look up and tally the calories and fat grams in those foods can they get delayed feedback on whether they met their goals. In contrast, using an app like ENGAGED to enter food intake creates a simple control system [2] that immediately detects and visualizes discrepancy between current behavior and goal as color-coded positive (green) or negative (red) feedback (Figure 3). Additionally, the app gives the user more accurate and motivating exercise feedback than paper and pencil by having them fill up a goal thermometer on the smartphone by accumulating physical activity counts that are Bluetoothed in real time from an accelerometer.
In addition to building self-efficacy about the ability to meet diet and activity goals, the ENGAGED system applies two further principles of the social cognitive theory. By being embedded in a smartphone that is ever present for most users, the app creates a facilitating physical environment to support weight self-management. The ENGAGED system also establishes a facilitating social environment by transmitting behavioral data to others who provide support and accountability for self-monitoring and healthy change. Complete data are sent to an interventionist who monitors recording compliance and behavior and then provides personalized coaching by telephone. Additionally, as shown in Figure 4, data on one another’s recording adherence are sent to a group of eight participants who have been incentivized as a team in a weight loss competition against other teams. The purpose of the incentive is to align team members’ financial interests so that they are motivated to care about and support one another’s weight loss efforts. Color-coded icons on the smartphone convert from red to yellow to green as participants enter more meals and wear the accelerometer for longer portions of the day. Armed with these data about their team-mates’ compliance with self-monitoring, team members use a private message board to communicate and support each other.
FIGURE 4.
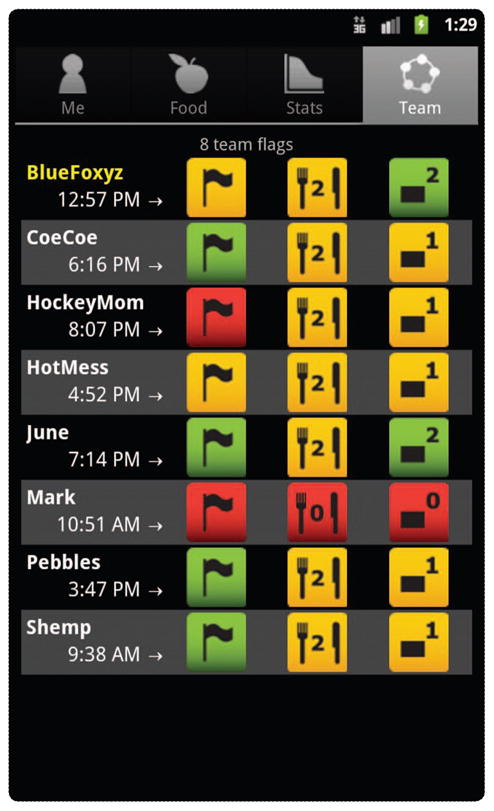
Color-coded information about team members in the ENGAGED weight loss competition. The left-most flag tab shows each person’s self-reported status. Mark seems to need help. He posted his status as red (danger). His middle (knife and fork) tab is also red, indicating that he has not yet entered any meals today, and his right-most (accelerometer) tab is red, showing that he has not put on his accelerometer. Everyone else on the team has already recorded two meals, but no one has turned the knife and fork tab green by entering three meals. Two people (June and BlueFoxyz) have turned the physical activity tab green by wearing the accelerometer for two-thirds of the day. Everyone else besides Mark has accumulated one-third of a day of accelerometer wear.
Many unknowns remain about how technology can best facilitate healthy lifestyle change. One important gap in knowledge concerns how easy to make self-monitoring. Will behavioral tracking be as effective in reducing problematic responses when it can be done passively by sensors, or is the burdensome conscious reflection implicit in written recording necessary for benefit to occur? Can technological systems function as effectively to shape healthy new behaviors as to disrupt problematic ones? Finally, and very importantly, how will 21st-century interventions incorporate and use continuous observational data about behavior?
Technologies such as the ENGAGED app currently collapse minute-by-minute data into cumulative aggregate scores, discarding tremendous amounts of real-time information. Now that behavioral change technologies are capable of processing responses to learn in real time and change their treatment algorithms accordingly, interventions can be personalized and adaptive so that doses and even modalities and messages are tailored on the fly. How shall we use these capabilities to optimize behavioral treatment? Will an ability to perform single-case experiments in real time replace the need to perform randomized controlled trials? Will we now abandon the underlying premise of evidence-based treatment guidelines that effective interventions produce generalized benefit for many individuals? Will our new default assumption be that a unique personalized treatment algorithm needs to be learned for each person and relearned as time, circumstance, and context change? How will the needs for technology redesign and reprogramming keep up with the pace of intervention refinement for individuals over time? And how practical is any of this for a cash-strapped health-care delivery system?
Fewer than 20 years ago, personal digital assistants were cutting-edge intervention technology. Yet, despite massive changes in the operating systems, sensors, and design of contemporary mobile technologies, the theory-derived change principles implemented for behavioral intervention remain largely the same today. Interest in doing real-time intervention refinement based on continuously observed behavioral response data is inspired as much by new interdisciplinary collaboration among behavioral scientists, engineers, and computer scientists as it is by new technological capabilities. As these new collaborations, technologies, and computational modeling capabilities create new intervention capabilities over the next several decades, we look forward to seeing our behavioral change theories catch up.
Contributor Information
Bonnie Spring, Email: bspring@northwestern.edu, Northwestern University Feinberg School of Medicine, Chicago, Illinois.
Marientina Gotsis, University of Southern California, Los Angeles.
Ana Paiva, GAIPS, INESC-ID and Instituto Superior Técnico, Lisboa, Portugal.
Donna Spruijt-Metz, University of Southern California, Los Angeles.
References
- 1.World Health Organization. 2008–2013 Action Plan for the Global Strategy for the Prevention and Control of Noncommunicable Diseases. Vol. 36. Geneva: WHO; 2008. [Google Scholar]
- 2.Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annu Rev Pub Health. 2010;31:399–418. doi: 10.1146/annurev.publhealth.012809.103604. [DOI] [PubMed] [Google Scholar]
- 3.Rivera DE. Optimized behavioral interventions: What does system identification and control engineering have to offer?. Proc. 16th Int. Federation of Automatic Control (IFAC) Workshop on System Identification (SYSID 2012); pp. 882–893. [Google Scholar]
- 4.Hammond RA. Complex systems modeling for obesity research. Prev Chronic Dis. 2009 Jul;6:A97. [PMC free article] [PubMed] [Google Scholar]
- 5.Vassileva J. Motivating participation in social computing applications: A user modeling perspective. User Model User-Adapt Interact. 2012 Mar;22:177–201. [Google Scholar]
- 6.Deci EL, Ryan RM. Overview of self-determination theory. In: Ryan RM, editor. The Oxford Handbook of Human Motivation. London, U.K: Oxford Univ. Press; 2012. pp. 85–107. [Google Scholar]
- 7.Brehm SS, Brehm JW. Psychological Reactance: A Theory of Freedom and Control. New York: Academic Press; 1981. [Google Scholar]
- 8.Norman DA. The Design of Everyday Things. New York: Basic Books; 2002. [Google Scholar]
- 9.Pellegrini CA, Duncan JM, Moller AC, Buscemi J, Sularz A, DeMott A, Pictor A, Pagoto S, Siddique J, Spring B. A smartphone-supported weight loss program: Design of the ENGAGED randomized controlled trial. BMC Pub Health. 2012;12:1041. doi: 10.1186/1471-2458-12-1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spring B, Duncan JM, Janke EA, Kozak AT, McFadden HG, DeMott A, Pictor A, Epstein LH, Siddique J, Pellegrini CA. Integrating technology into standard weight loss treatment: A randomized controlled trial. JAMA Intern Med. 2013 Jan;173(2):105. doi: 10.1001/jamainternmed.2013.1221. [DOI] [PMC free article] [PubMed] [Google Scholar]