Abstract
Objective
There are limited data on the effects of adaptive social communication interventions with a speech-generating device in autism. This study is the first to compare growth in communications outcomes among three adaptive interventions in school-aged children with autism spectrum disorder (ASD) who are minimally verbal.
Methods
Sixty-one children, aged 5–8 years participated in a sequential, multiple-assignment randomized trial (SMART). All children received a developmental communication intervention: joint attention, symbolic play, engagement and regulation (JASP) with enhanced milieu teaching (EMT). The SMART included three two-stage, 24-week adaptive interventions with different provisions of a speech-generating device (SGD) in the context of JASP+EMT. The first adaptive intervention, with no SGD, initially assigned JASP+EMT alone; then intensified JASP+EMT for slow responders. In the second adaptive intervention, slow responders to JASP+EMT were assigned JASP+EMT+SGD. The third adaptive intervention initially assigned JASP+EMT+SGD; then intensified JASP+EMT+SGD for slow responders. Analyses examined between-group differences in change in outcomes from baseline to week 36. Verbal outcomes included spontaneous communicative utterances and novel words. Non-linguistic communication outcomes included initiating joint attention and behavior regulation, and play.
Results
The adaptive intervention beginning with JASP+EMT+SGD was estimated as superior. There were significant (P<0.05) between-group differences in change in spontaneous communicative utterances and initiating joint attention.
Conclusions
School-aged children with ASD who are minimally verbal make significant gains in communication outcomes with an adaptive intervention beginning with JASP+EMT+SGD. Future research should explore mediators and moderators of the adaptive intervention effects and second-stage intervention options that further capitalize on early gains in treatment.
Keywords: adaptive treatment strategies, alternative and augmentative communication, autism spectrum disorder, JASPER, EMT, minimally verbal
INTRODUCTION
Significant progress has been made in identifying core features of autism spectrum disorder (ASD) and developing effective interventions for pre-school age children with this disorder (National Research Council, 2001). However, until recently, these efforts have generally overlooked the estimated 25–30% of school-aged children with ASD who do not make significant progress in spoken communication despite access to (sometimes, years of) traditional interventions (Anderson et al., 2007; Kasari, Tager-Flusberg, & Cooper, 2010). These older, minimally verbal children with ASD are often excluded from research studies aiming to develop or evaluate interventions (Tager-Flusberg & Kasari, 2013). Given the often-cited finding that failure to develop spoken language by the time children reach school age increases the likelihood of a poor long-term prognosis for social and adaptive functioning (Howlin, Goode, Hutton, & Rutter, 2004; Lord, 2000; Rutter, 1978), this state of the intervention science is of great concern to parents, teachers, researchers and other stakeholders.
One class of supportive interventions that is commonly used with this population, for which there is a growing but limited evidence base, is known as alternative and augmentative communication (AAC) interventions. AACs most commonly involve either a picture symbol system, for example, a Picture Exchange Communication System (PECS; Frost & Bondy, 2002), or a speech generating device (SGD), such as a dedicated device or an off-the-shelf tablet with communication software. In a review of 23 studies involving the use of an SGD with children with ASD (van der Meer & Rispoli, 2010), the great majority of the studies were single-case research designs (Gast & Ledford, 2009)—there were 51 children in total across all 23 studies—and none of the studies involved randomized comparisons. Most of them focused on teaching requesting or responding to questions. Few of these studies addressed language used for broader, socially communicative purposes. The majority of these studies focused on teaching a child to use an SGD directly, rather than adding in the SGD to an already tested early intervention model for improving social communication and language outcomes in children with ASD. Thus, a consideration in this study was whether using an SGD in the context of an efficacious behavioral intervention targeting social communication might prove more effective with these older, minimally verbal children. Studying the effectiveness of SGD is particularly important given concern by some parents and providers that use of an SGD might hinder (not improve) spoken language development (Cress & Marvin, 2003).
A key challenge in developing any type of intervention for children with ASD who are minimally verbal is that this group is highly heterogeneous (Anderson et al., 2007; Tager-Flusberg & Kasari, 2013; Wodka, Mathy, & Kalb, 2013), both in their presentation at baseline and in their progress over time in response to any single intervention. Coupled with the closing developmental window for acquiring spoken communication, this argues for an adaptive approach to intervention whereby treatment is adapted to the evolving status of the child. Children exhibiting an early slower response to a behavioral communication intervention that targets spoken language may be subsequently offered an augmentation with SGD, whereas children exhibiting a faster response to their initial intervention may remain on their current treatment (and not receive an SGD). A related rationale for an adaptive, sequential approach to treatment is the consideration of cost, either in terms of monetary cost or in terms of treatment burden. The example given above illustrates this idea in that professionals may hesitate to recommend an SGD for all children up-front due to concerns over the monetary cost of an SGD (which could range from hundreds to thousands of dollars), especially if some children may respond equally well in the long-term without an SGD. Adaptive interventions (Almirall, Nahum-Shani, Sherwood, & Murphy, 2014; Nahum-Shani et al., 2012) provide one way to guide this kind of sequential clinical decision-making, which more closely resembles the kind of treatment decision-making that occurs in actual practice. More formally, an adaptive intervention is a sequence of treatment decision rules that specify whether, how or when, and based on which measures, to alter the dosage or type of treatment (Murphy & Almirall, 2009). Adaptive interventions hold the promise of improving outcomes for greater numbers of children with ASD by guiding clinicians/therapists in how to take advantage of heterogeneity in response to treatment.
A recent sequential multiple-assignment randomized trial (SMART) of sixty-one (n=61) minimally verbal children with ASD between the ages of 5 and 8 tested the effect of adding in an SGD to a naturalistic, developmental behavioral intervention (Kasari et al., 2014). Joint attention, symbolic play, engagement and regulation (JASP; Kasari, Freeman, & Paparella, 2006; Kasari, Paparella, Freeman, & Jahromi, 2008) has improved social communication outcomes (e.g., initiating joint attention, play diversity) and spoken language in preverbal children with ASD in a number of randomized trials (Kasari et al, 2006, 2008, 2014). In this study JASP was blended with a spoken language intervention (enhanced milieu training, or EMT) that has been applied to children with a variety of language impairments (Hancock & Kaiser, 2006). The JASP+EMT intervention was implemented with children with or without the addition of a SGD. Specifically, children in this study were assigned to one of three adaptive interventions, which differed primarily with respect to the provision of a speech-generating device in the context of JASP+EMT (see Table 1). All three adaptive interventions were provided in two stages (12 weeks each), over the course of 24 weeks. In all three adaptive interventions, parents (or guardians) of all children received a JASP+EMT parent training intervention in stage 2 (Shire et al., 2014).
Table 1.
Comparison of the three adaptive interventions embedded in the SMART design.
| Adaptive Intervention |
Stage 1 Treatment |
Responder Status |
Stage 2 Treatment |
Cells in Figure 1 |
Number of Participants |
|---|---|---|---|---|---|
| (No SGD, No SGD) | JASP + EMT | Responder | Continued JASP + EMT |
A + B | 24 |
| Slow Responder |
Intensified JASP + EMT |
||||
| (No SGD, SGD) | JASP + EMT | Responder | Continued JASP + EMT |
A + C | 24 |
| Slow Responder |
JASP + EMT + SGD | ||||
| (SGD, SGD) | JASP + EMT + SGD | Responder | JASP + EMT + SGD | D + E | 31 |
| Slow Responder |
Intensified JASP + EMT + SGD |
Notes.
See manuscript text for definition of Responder versus Slow Responder. Abbreviations: JASP—Joint attention, social engagement, and play; EMT—Enhanced milieu training; SGD—Speech generating device.
Results of the primary study analyses indicated that participants who began an adaptive intervention with JASP+EMT+SGD (versus those who began adaptive interventions with JASP+EMT) had significant improvements in total number of spontaneous communicative utterances (the primary spoken language outcome), as well as in total novel words and comments (secondary outcomes). However, the initial report did not analyze how the three adaptive interventions impacted longitudinal outcomes from baseline through follow-up (week 36), first, because this was not the primary aim of the SMART study and, second, because the statistical methodology for this kind of analysis did not yet exist. The original study also did not examine the key, non-linguistic outcomes that are typically examined in studies using JASP, namely initiating joint attention and play diversity.
This manuscript presents a secondary analysis of the above SMART study, with the following two novel contributions. First, this manuscript uses new methods (Lu et al., 2015) to examine the longitudinal impact of the three adaptive interventions that are embedded within the SMART study. By comparing the three adaptive interventions on longitudinal outcomes, this study sheds additional light on how SGDs impact the rate of change in outcomes in the context of JASP+EMT, both overall and during each stage of treatment. This can contribute to the development of more refined scientific models that explicate how SGDs facilitate improvement in minimally verbal children with ASD when used at varying stages in the course of naturalistic intervention such as JASP+EMT. Moreover, these insights could help to more effectively target interventions for minimally verbal children with ASD. For example, adaptive interventions that demonstrate a slowing in the extent of improvement during the second stage could be improved in subsequent research. Because many children in this population have already demonstrated limited progress after intensive intervention, it is especially important to understand the trajectory of effects produced by different adaptive interventions so that they and future adaptive interventions can best be used to maximize long-term outcomes.
Second, this manuscript focuses on the comparison of the three adaptive interventions in terms of growth in both verbal and key non-linguistic outcomes. For the verbal outcomes, we examined treatment effects on the total number of (i) spontaneous communicative utterances and (ii) different word roots measured in a naturalistic language sample. The total number of spontaneous communicative utterances is the primary, direct measure of spoken communication in this study. It includes the total number of unprompted comments and spontaneous requests made by the child, as well as “other” uncategorized utterances. The total number of different word roots is the total number of unique words used (variants of the same word are counted as only once; e.g., plurals, past tense of the a word are the same as the root). Three additional outcomes were examined: (iii) initiating joint attention, (iv) initiating behavior regulation and (v) unique play actions. We chose to focus on these three additional outcomes because increased initiating joint attention and play are two key mechanisms by which JASP is expected to lead to improved spoken communication (Kasari et al., 2008; Mundy & Newell, 2007; Mundy, Sigman, Ungerer, & Sherman, 1986), and, while initiating behavior regulation is not targeted as often as part of JASP, it is expected to improve in concert with initiating joint attention. Hence, our comparison of the three adaptive interventions sheds light on the role of SGDs in amplifying the intended effects of JASP+EMT.
We hypothesized that the three adaptive interventions would differ on change in total number of spontaneous communicative utterances and novel words, initiating joint attention and initiating behavior regulation, but not on play. Both joint attention and behavior regulation are components of social communication (as well as communicative utterances and novel words), and are targeted directly with all three adaptive interventions. Because the addition of SGD provides additional support for performing these communicative acts, we hypothesized that JASP+EMT+SGD would result in greater increases. While play provides the appropriate context for JASP+EMT, it is targeted similarly across all three adaptive interventions; hence we hypothesized no effect on play. While the primary focus of this study was on between-group differences in change, all outcomes were expected to improve over time, on average.
METHODS
Study Design
Complete study design details, including a CONSORT diagram, detailed demographic information concerning the study sample at baseline, more detailed information concerning the treatments provided, power/sample size considerations, and the results of the primary aims of this trial are provided elsewhere (Kasari et al., 2014).
Briefly, the inclusion criteria were: (a) ASD diagnosis, (b) between 5 and 8 years of age, (c) minimally verbal, with fewer than 20 spontaneous novel words in a 20-minute natural language sample, (4) at least two years of previous intervention, and (5) at least 24 months developmentally. The exclusion criteria included: (a) SGD proficiency, (b) Fragile X, (c) Down syndrome, (d) tuberous sclerosis, (e) cerebral palsy or other major motor disability, (f) blindness, (g) deafness, or (h) uncontrolled seizures. One-hundred thirty-four (134) children were screened, and sixty-one (61) children met criteria to participate in the study (for details see CONSORT diagram in Kasari et al. (2014)).
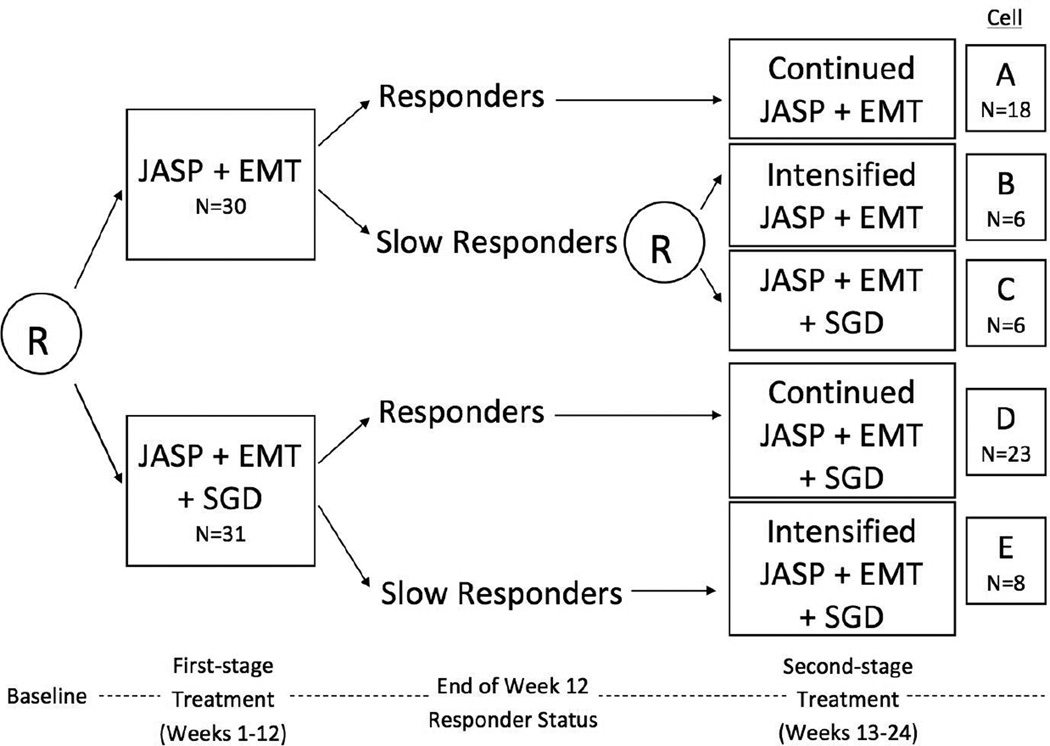
The study design was a longitudinal (research outcomes collected at baseline and weeks 12, 24 and 36), multi-site (UCLA, Vanderbilt University, and Kennedy Krieger Institute) sequential multiple-assignment randomized trial (SMART; Lavori & Dawson, 2000; Murphy, 2005). The SMART included two stages of treatment for all children (each stage was 12 weeks in duration) plus a follow-up stage. The study duration was 9 months (36 weeks). Figure 1 depicts the study design. At baseline, the sixty-one children that met inclusion/exclusion criteria were randomized with equal probability to JASP+EMT versus JASP+EMT+SGD for 12 weeks (stage 1). At the end of 12 weeks, children were assessed for responder versus slow-responder status to stage 1 treatment (defined immediately below). At the beginning of the stage 2 (beginning of week 13), all responders continued with the same treatment for another 12 weeks. For slow-responders to JASP+EMT+SGD, treatment was intensified. Slow-responders to JASP+EMT were re-randomized with equal probability to intensified JASP+EMT versus augmented JASP+EMT+SGD. The Institutional Review Board at each site approved the study protocol.
Figure 1.
Schematic of the sequential multiple assignment randomized trial (SMART) design, with sample sizes at each stage.
Notes. See manuscript text for definition of Responder versus Slow Responder. Abbreviations: JASP—Joint attention, social engagement, and play; EMT—Enhanced milieu training; SGD—Speech generating device.
Data Sources and Measures
Demographics Questionnaire
At baseline, parents of participating children completed a demographic questionnaire, which included age, ethnicity (Caucasian versus other), and gender.
Leiter International Performance Scale-Revised (Leiter-R)
At baseline, nonverbal intelligence was measured by the Leiter-R, a nonverbal cognitive assessment. Tasks, which do not require verbal responses, include matching, pattern completion, and sequential order. The assessment provides two scores: a non-verbal intelligence quotient (IQ) and an age-equivalent score.
Autism Diagnostic Observation Schedule (ADOS)
At baseline, diagnosis of ASD was based on a 30–45 minute behavioral observation using the first module of the ADOS (Lord et al., 2000). The first module of the ADOS was used because this module focuses specifically on children who are not exhibiting phrase speech. The total baseline ADOS score is the sum of sub-scales of social communication, reciprocal social interaction, and restricted and repetitive behavior.
Naturalistic Language Sample
Various measures of spoken communication were extracted from a series of natural language samples (NLS), administered at baseline and at the end of weeks 12, 24, and 36. The NLS is a 20-minute standardized, naturalistic interaction between the child and an adult. A standardized set of toys was used with all children; toys included a set of blocks and cars, food with dolls, Play-Doh®, and a book. The aim of the NLS is to evaluate the child’s spontaneous expressive language ability. NLS videos were then transcribed by independent evaluators/coders who were blind to randomly assigned treatment using standard Systematic Analysis of Language Transcripts (SALT) conventions (Miller & Chapman, 1985). The following variables were coded from the NLS: total number of spontaneous communicative utterances (TSCU), proportion of spontaneous communicative utterances (PSCU), number of different word roots (NDWR), mean length utterances in words (MLU), words per minute (WPM), total number of comments (TCOM), unique word combinations (UWC), and total number of spontaneous requests (SPRQ).
Early Social Communication Scales (ESCS)
Measures of early social communication behaviors were obtained at baseline and at the end of weeks 12, 24, and 36 using the ESCS (Mundy et al., 2013). The ESCS is a structured observation-based assessment, requiring 15–25 minutes to administer. Two measures were derived from the ESCS: total initiating joint attention (IJA) and total initiating behavioral regulation (IBR). IJA measures the frequency with which a child uses language, gesture and/or eye contact to share an object or event (e.g., child points at a toy to share his excitement for the toy with a social partner). IBR measures the frequency with which a child uses these social communication behaviors to request or have his needs met (e.g., giving or reaching for an object for help).
Structured Play Assessment (SPA)
Measures of play were obtained at baseline and at the end of weeks 12, 24, and 36 using the SPA (Ungerer & Sigman, 1981). The SPA is also a semi-structured observation-based assessment, requiring 15–20 minutes to administer. The total number of unique play actions (UPA) measure was derived from the SPA. This measure refers to the total number of spontaneous novel play acts initiated by the child. For play acts that are initiated by the child more than once, only one count contributes to this total measure.
Study Outcomes
Five longitudinal outcome measures (two verbal and three non-linguistic) were considered. The two verbal outcomes—total number of spontaneous communicative utterances (TSCU) and number of different word roots (NDWR)—were taken from the NLS. The three non-linguistic outcomes were initiating joint attention (IJA) and initiating behavioral regulation (IBR) taken from the Early Social Communication Scales (ESCS), and unique play actions (UPA) taken from the Structured Play Assessment (SPA). All outcomes were continuous. For all outcomes, a larger value was regarded as better.
Interventions
Interventions included: (i) stage 1 treatment options, (ii) the identification of responders and slow responders to stage 1 treatment, and (iii) stage 2 treatment options. The treatment options in stage 1 included JASP+EMT or JASP+EMT+SGD, defined as follows:
JASP+EMT
Children initially assigned to JASP+EMT received two-hour long sessions per week of JASPER blended with EMT for 12 weeks. Joint attention, symbolic play, engagement and regulation (JASP) focused on social-communication skills (Kasari et al., 2008) by creating contextually relevant learning opportunities with parents and therapists, responding to child interest and actions, modeling and expanding play, engagement and language. Enhanced milieu teaching (EMT) focused on spoken language acquisition skills (Kaiser & Roberts, 2013) using responsive interaction strategies, modeling target language, expansions, and behavioral prompts to support learning and use of functional spoken language in everyday interactions. All of the skills that were the focus of JASPER and EMT are known to be predictive of later spoken communication in children with autism (Mundy, Sigman, & Kasari, 1990).
JASP+EMT+SGD
Children initially assigned to JASP+EMT+SGD also received two-hour long sessions per week of JASP+EMT for 12 weeks, with the addition of a speech-generating device (SGD). The device used was an iPad with an AAC app or a dedicated communication device (e.g., DynaVox V or DynaVox Maestro) programmed with picture symbols representing activity-relevant vocabulary. The device was always available during JASP+EMT sessions for these children; devices were not provided for use at home. In order for the child to learn how to use the device, during JASP+EMT sessions, the therapist was required to model language using the device a minimum of 50% of the time. Children were not required to use the device. However, even if the child did not use the device to initiate communication, the therapist was required to expand on the child’s spoken or gestural communication using the device at least 80% of the time.
Response versus Slow-response to Stage 1 Treatment
Seven measures of spoken communication, measured in two different contexts, were used to determine response versus slow response to stage 1 treatment. The seven measures—TSCU, PSCU, NDWR, MLU, WPM, TCOM, and UWC—were extracted from the Natural Language Sample (NLS, see above) and from session intervention transcripts, which were also coded for these seven measures using the same procedures used for the NLS. A child was considered a responder if he or she exhibited greater than or equal to 25% improvement from baseline to week 12 on at least 7 of the 14 measures; otherwise, the child was considered a slow responder.
The treatment options in stage 2 included JASP+EMT+SGD, Continued JASP+EMT, Continued JASP+EMT+SGD, Intensified JASP+EMT, or Intensified JASP+EMT+SGD. JASP+EMT+SGD in stage 2 was administered just as it was in stage 1. All responders to stage 1 treatment continued on their assigned stage 1 treatment (e.g., Continued JASP+EMT or Continued JASP+EMT+SGD) for another 12 weeks. The two intensified treatment options (i.e., Intensified JASP+EMT or Intensified JASP+EMT+SGD) are similar to their stage 1 counterparts, except that they occurred for a total of three sessions (or hours) per week rather than two sessions (or hours) per week.
In addition, in stage 2, all parents were trained in JASP+EMT with the aim of teaching them to deliver JASP+EMT-like intervention in the home (Shire et al., 2014). For children in a treatment condition receiving SGD during stage 2, parents were trained in the use of the device with the JASP +EMT intervention.
Adaptive Interventions
An adaptive intervention is a sequence of clinical care decision rules that leads to individualized sequences of treatment (Lavori & Dawson, 2000, 2004; Lavori, Dawson, & Rush, 2000). This SMART had three, two-stage adaptive interventions embedded within it, by design (Almirall, Compton, Rynn, Walkup, & Murphy, 2012; Almirall et al., 2014; Nahum-Shani et al., 2012). Table 1 describes the three adaptive interventions and how each arises from the study design (i.e., relation to cells A-E in Figure 1). Each adaptive intervention involves a stage 1 treatment option, the classification of children as responders or slow-responders to stage 1 treatment, and a decision rule linking response/slow-response status to a stage 2 treatment option. An important, but perhaps subtle, point is that adaptive interventions guide the provision of sequences of treatment for both responders and slow-responders (this is made explicit in Table 1). In the statistical literature, adaptive interventions are known as dynamic treatment regimens (Chakraborty, 2011; Chakraborty & Moodie, 2013; Lavori & Dawson, 2014; Moodie, Richardson, & Stephens, 2007; Orellana, Rotnitzky, & Robins, 2010; Zhang, Tsiatis, Laber, & Davidian, 2013).
All three adaptive interventions in the SMART involved JASP+EMT, but differed, primarily, in their provision of a SGD in the context of JASP+EMT; indeed, the three adaptive interventions can be ordered in terms of “dosage of SGD”. In the first adaptive intervention, children were initially assigned JASP+EMT alone in stage 1; slow responders were assigned intensified JASP+EMT in stage 2; and responders remain on JASP+EMT in stage 2. This adaptive intervention did not involve SGD; we denote it by the pair (No SGD, No SGD) referring to each stage of treatment. In the second adaptive intervention, children were initially assigned JASP+EMT in stage 1; slow responders to JASP+EMT were assigned JASP+EMT+SGD in stage 2; responders remained on JASP+EMT in stage 2. This adaptive intervention assigned SGD only in stage 2 and only for children who were slow-responders; we denote it by (No SGD, SGD). In the third adaptive intervention, labeled (SGD, SGD), children were initially assigned JASP+EMT+SGD in stage 1; slow responders were assigned intensified JASP+EMT+SGD in stage 2; responders remained on JASP+EMT+SGD in stage 2. This adaptive intervention involved SGD in both stages of treatment, for all children; we denote it by (SGD, SGD).
As a result, the three adaptive interventions differed, secondarily, in terms of the number of clinical sessions per week. The adaptive interventions (No SGD, No SGD) and (SGD, SGD) both provide an increase in the number of sessions per week for slower responders (from 2 to 3), whereas all children in the (No SGD, SGD) adaptive intervention always receive 2 sessions per week.
Statistical Analysis
Study Sample and Descriptive Statistics
In accordance with intention-to-treat principles, all sixty-one children who were randomized at stage 1 were used in all statistical analyses. Pre-treatment descriptive statistics (mean and standard deviation), overall and by assigned stage 1 treatments, were conducted for age, race, gender, site, ADOS score, and for baseline measures of TSCU, NDWR, TCOM, SPRQ, IJA, IBR and UPA.
Longitudinal Adaptive Intervention Effect Analyses
The aim of the statistical analyses was to compare growth in verbal and social communication outcomes between the three adaptive interventions given above. Longitudinal regression models, adapted for the analysis of data arising from a longitudinal SMART (Lu et al., 2015), were used to examine between-group differences (i.e., differences between adaptive interventions) in change in outcomes from baseline through weeks 12, 24, 36. Separate models were fit for each longitudinal outcome, specified as follows: For each of the three adaptive interventions, a piecewise-linear model with a knot at week 12 was used to model the temporal trend over the course of the study; i.e., linear trend from baseline to week 12, and a linear trend form week 12 to week 36. A piece-wise linear growth model was chosen to allow for changes/deflections in the average trend following week 12, when all children transitioned to second stage treatment. (In addition, note that the more common approach of using a linear trend from baseline to week 36 for all three adaptive interventions would not allow for a proper comparison of the two adaptive interventions beginning with JASP since they are identical, by design, from baseline to week 12; a piece-wise linear model allows for greater flexibility in comparing the three adaptive interventions.) Hence, in these models, each adaptive intervention has its own slope in stage 2. In stage 1, there were only two slopes since two of the three adaptive interventions share the same trend between baseline and week 12; i.e., the two adaptive interventions beginning with JASP+EMT (no SGD) are identical up to week 12. Each model included the following baseline covariates: age (in years), gender (female as referent), indicator for white versus non-white, site (indicators for UCLA and Vanderbilt, with KKI as referent), and total ADOS score at baseline. An exchangeable (i.e., compound symmetric) working correlation structure was used to model the within-person correlation in the repeated outcome measures. All assumptions, such as the choice of baseline covariates, piece-wise linear model for time, and correlation structure were specified a priori; i.e., prior to analyzing the data.
Weighted and replicated generalized estimating equations were used to estimate each longitudinal model (e.g., to estimate and compare the slopes at each stage for each adaptive intervention). By design, slower responders to JASP+EMT had a 1/4 chance of following their assigned treatment sequence (slower responders to JASP+EMT were randomized twice with probability 1/2), whereas responders to JASP+EMT and children who began with JASP+EMT+SGD had a 1/2 chance of following their assigned treatment sequence (these children were randomized once with probability 1/2). Weighting is used to account for this known under-representation of slow responders to JASP+EMT. Specifically, slower responders to JASP+EMT were assigned a weight of 4 of following their assigned sequence of treatments; all other children were assigned a weight of 2. In addition, since responders to JASP+EMT are consistent with two of the three adaptive interventions being compared, the data for responders to JASP+EMT was replicated (i.e., used twice) in order to facilitate a more efficient comparison of the three adaptive interventions. For more details on weighting and replication, see Nahum-Shani et al. (2012); for details on the extension of weighting and replication to the analysis of longitudinal outcomes, see Lu et al. (2015). Bootstrapped standard errors, which account for the multiple (longitudinal) observations per child, replication, and sampling variation in the unknown distribution of the weights, were used. Data were analyzed using the geepack package in R (Yan, Hojsgaard, & Halekoh, 2015).
Contrasts of Clinical Interest and Effect Sizes
For all five outcomes, slope estimates at each stage were calculated for each of the three adaptive interventions. Larger slopes indicate more improved outcomes. Between-group differences in slope at each stage were also provided. To facilitate the comparison of each adaptive intervention using a single-number summary (as opposed to two slopes), the average area under the longitudinal curve from baseline to week 36 divided by 36 (AUC, for short) was calculated for each adaptive intervention, as well as estimates of the between-group differences in AUC. The AUC has the interpretation as the average of the outcome over the course of the study. In non-linear trend models (e.g., the piece-wise linear models we employ, or in models with quadratic trends), the AUC is a useful single-number summary of the mean outcome trajectory across both stages of treatment. 95% confidence intervals (CI) were calculated for all point estimates.
For each outcome, we report the results of the multivariate hypothesis test that there is no between-group difference in slope at any point in the course of the study. This is a test of the null hypothesis that the three adaptive interventions have equal slope at both stages. (This null hypothesis implies that there is no between-group difference in AUC.) A P-value of less than 0.05 (two-sided) was considered statistically significant for this hypothesis test.
To enhance clinical interpretation of the results, effect sizes (Cohen, 1988) were calculated for the differences in slope at stage 1, differences in slope at stage 2, and the differences in AUC. Effect sizes are defined as point estimates divided by an estimate of the standard deviation of the slopes or AUC, respectively. Effect sizes of 0.2, 0.5, and 0.8 are generally regarded as small, moderate, and large, respectively. Plots of the average trend under each adaptive intervention are provided.
Missing Data
Multiple imputation was used to replace missing values in the outcomes, and other measures. A sequential regression multivariate imputation algorithm, adapted for SMART studies (Shortreed, Laber, Stroup, Pineau, & Murphy, 2014), was implemented using the mice package in R (Buuren & Groothuis-Oudshoorn, 2011). For additional details, including the percentage of missing data, the imputation model used, and a sensitivity analysis of robustness to the missing-at-random assumption, see Kasari et al. (2014). Twenty imputed data sets were generated. All point estimates, standard errors, and hypothesis tests reported below were calculated using standard rules (Schafer, 1999) for combining the results of identical analyses performed on each of the 20 imputed data sets.
RESULTS
Descriptive statistics prior to treatment are provided in Table 2. Children were between the ages of 4.42 and 9.00 (mean=6.31, SD=1.16); the majority of them were non-white (52%) males (83%). At baseline, children had an average of 20.07 on the ADOS (SD=4.4), an average non-verbal IQ of 68.2 (SD=19.0) and mental age of 4 years on the Leiter-R, 29.44 spontaneous communicative utterances (SD=25.37), 17.2 different word roots (SD=16.44), 6.02 total comments (SD=8.17), 7.62 requests (SD=7.62), 6.43 instances of initiating joint attention (SD=7.98), 14.32 instances of initiating behavioral regulation (SD=10.23) and 14.39 unique play actions (SD=9.61). Children assigned to JASP+EMT versus JASP+EMT+SGD did not differ in clinically or statistically significant ways on any of these pre-treatment measures.
Table 2.
Pre-treatment descriptive statistics, overall and by stage 1 randomization.
| Overall n=61 |
JASP+EMT n=30 |
JASP+EMT+SGD n=31 |
||||
|---|---|---|---|---|---|---|
| % | n | % | n | % | n | |
| Gender | ||||||
| Male | 83% | 51 | 87% | 26 | 79% | 25 |
| Female | 17% | 10 | 13% | 4 | 21% | 6 |
| Race | ||||||
| White | 48% | 29 | 47% | 14 | 48% | 15 |
| Non-white | 52% | 32 | 53% | 16 | 52% | 16 |
| Site | ||||||
| UCLA | 39% | 24 | 40% | 12 | 39% | 12 |
| Vanderbilt | 33% | 20 | 33% | 10 | 32% | 10 |
| Kennedy Krieger | 28% | 17 | 27% | 8 | 29% | 9 |
| Mean (SD) | Mean (SD) | Mean (SD) | ||||
| Age | ||||||
| Years | 6.31 (1.16) | 6.18 (1.08) | 6.44 (1.23) | |||
| Cognitive Assessment (Leiter-R) |
||||||
| Non-verbal IQ | 68.2 (19.0) | 68.7 (21.3) | 67.6 (16.8) | |||
| Age-equivalent | 4.00 (1.12) | 3.93 (1.12) | 4.07 (1.14) | |||
| Autism Diagnostic Observation Schedule |
||||||
| ADOS | 20.07 (4.40) | 19.55 (4.27) | 20.60 (4.55) | |||
| Natural Language Sample |
||||||
| TSCU | 29.44 (25.37) | 28.37 (29.96) | 30.48 (20.35) | |||
| NDWR | 17.20 (16.44) | 16.78 (19.52) | 17.61 (12.91) | |||
| TCOM | 6.02 (8.17) | 7.01 (11.0) | 5.07 (3.8) | |||
| SPRQ | 7.62 (9.63) | 7.19 (10.26) | 8.03 (9.09) | |||
| Early Social Communication Scale |
||||||
| IJA | 6.43 (7.98) | 6.52 (8.80) | 6.29 (7.04) | |||
| IBR | 14.32 (10.23) | 15.65 (11.87) | 13.03 (8.28) | |||
| Structured Play Assessment |
||||||
| UPA | 14.39 (9.61) | 13.73 (9.40) | 15.03 (9.82) | |||
Notes. Abbreviations: JASP—Joint attention, social engagement, and play; EMT—Enhanced milieu training; SGD—Speech generating device; TSCU—Total socially communicative utterances; NDWR—Number of direct word roots; TCOM—Total number of comments; SPRQ—Spontaneous requests; IJA—Initiating joint attention; IBR—Initiating behavioral regulation; UPA—Unique play acts.
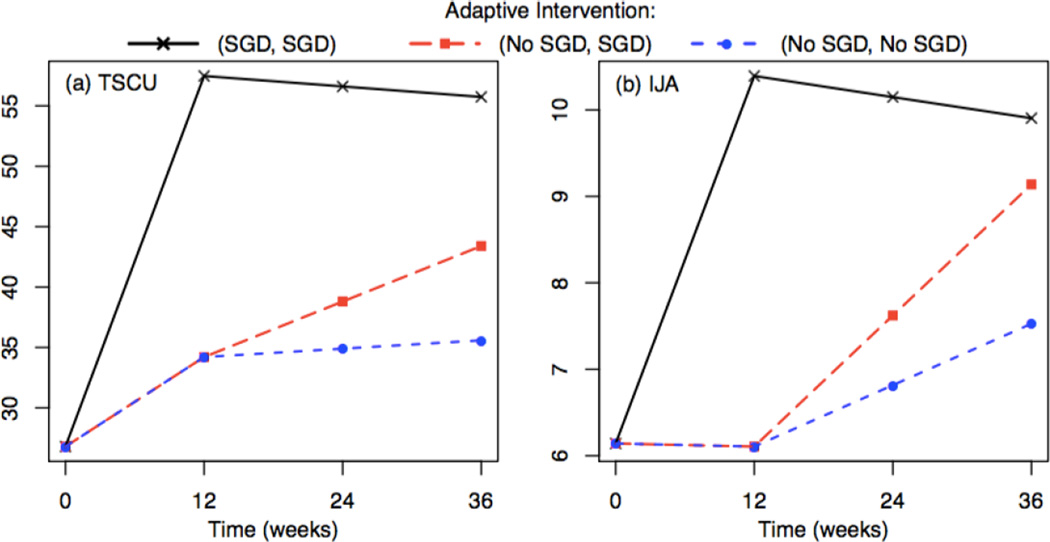
Stage-specific slope and AUC estimates are given in Table 3 for each of the three adaptive interventions. There were statistically significant differences in slopes (at stage 1 or stage 2) among the three adaptive interventions on two of the five outcomes considered: total spontaneous communicative utterances (TSCU, P<0.01) and initiated joint attention (IJA, P=0.046). Figure 2 shows the estimated average trajectories for each adaptive intervention, for these two outcomes. For each of these outcomes, (SGD, SGD) was the adaptive intervention with the largest estimated AUC value, (No SGD, SGD) had the second-largest estimated AUC, and (No SGD, No SGD) had the smallest estimated AUC value. In addition, the greatest change in each of these measures was with SGD during stage 1.
Table 3.
Estimates for the slope at each stage and AUC for the three embedded adaptive interventions.
| (No SGD, No SGD) | Estimate (95% CI) (No SGD, SGD) |
(SGD, SGD) | Test of No Differenc in Slopes** |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Stage 1 Slope* |
Stage 2 Slope |
AUC | Stage 2 Slope |
AUC | Stage 1 Slope |
Stage 2 Slope |
AUC | P-value | |
| Natural Language Sample |
|||||||||
| TSCU | 0.61 (−0.3,1.5) |
0.06 (−0.5,0.6) |
33.4 (25,42) |
0.38 (−0.2,1.0) |
36.0 (28,44) |
2.56 (1.6,3.5) |
−0.07 (−0.6,0.4) |
51.8 (43,60) |
<0.01 |
| NDWR | 0.60 (−0.05,1.2) |
0.0 (−0.3,0.3) |
21.7 (15.1,28.3) |
0.20 (−0.2,0.6) |
23.2 (16.6,29.9) |
1.39 (0.7,2.1) |
0.02 (−0.2,0.3) |
29.8 (23.4,36.1) |
0.12 |
| Early Social Communication Scale |
|||||||||
| IJA | 0 (−0.2,0.2) |
0.06 (−0.1,0.2) |
6.6 (5.0,8.2) |
0.13 (0.001,0.26) |
7.1 (5.5,8.7) |
0.35 (0.03,0.7) |
−0.02 (−0.2,0.1) |
9.5 (7.3,11.7) |
<0.05 |
| IBR | 0.19 (−0.1,0.5) |
0.06 (−0.1,0.2) |
16.1 (13.0,19.2) |
0.11 (−0.1,0.3) |
16.5 (13.2,19.8) |
0.36 (0.1,0.6) |
0.08 (−0.1,0.3) |
18.0 (14.8,21.2) |
0.31 |
| Structured Play Assessment |
|||||||||
| UPA | 0.17 (−0.1,0.4) |
−0.04 (−0.18,0.1) |
15.3 (13.2,17.5) |
−0.03 (−0.2,0.1) |
15.4 (13.2,17.5) |
0.06 (−0.2,0.3) |
0.1 (−0.03,0.2) |
15.4 (13.1,17.5) |
0.52 |
Notes.
Abbreviations: SGD—Speech generating device; TSCU—Total socially communicative utterances; NDWR— Number of direct word roots; IJA—Initiating joint attention; IBR—Initiating behavioral regulation; UPA—Unique play acts; AUC—the average area under the estimated longitudinal curve from baseline to week 36 (has the interpretation as the average outcome over the course of the study).
Slopes with a 95% confidence interval that does not include zero are boldfaced
The two adaptive interventions beginning with No SGD have identical stage. 1 slopes; hence, we only report it once under (No SGD, No SGD).
This is the hypothesis test that there is no difference in slopes between the three adaptive interventions, at any C stage; note that no difference in slopes implies that there is no difference in AUC
Figure 2.
Estimated average trajectories under each of the embedded adaptive interventions.
Notes. See Table 1 and Figure 1 to understand how the three adaptive interventions are defined. Trajectories are shown for the two significant outcomes: (a) total spontaneous communicative utterances (TSCU) and (b) initiating joint attention (IJA). Abbreviations: SGD—Speech generating device.
Table 4 provides additional detail concerning estimates of the pairwise differences in slopes and AUC (and associated standardized effect sizes) among the three adaptive interventions. For the primary outcome TSCU, there was a moderate-large difference in stage 1 slope (estimate, 1.94; 95%CI, 0.7 to 3.2; effect size, 0.8) between (SGD, SGD) and adaptive interventions beginning with No SGD. The difference in stage 2 slope between the two adaptive interventions beginning without SGD was small (estimate, 0.33; 95%CI, −0.05 to 0.8; effect size, 0.13). Based on AUC for TSCU, we find moderate differences suggesting that (SGD, SGD) > (No SGD, No SGD) (estimate, 18.6; 95%CI, 8 to 29; effect size, 0.67) and (SGD, SGD) > (No SGD, SGD) (estimate, 15.7 95%CI, 6 to 25; effect size, 0.58), yet little evidence that (No SGD, SGD) differed from (No SGD, No SGD) (estimate, 2.6; 95%CI, 0.4 to 5.6; small effect size, 0.1). For completeness, we descriptively examined the percentage of TSCU that were comments (TCOM) or requests (SPRQ); we did this at each time point, among children with TSCU>0. The average proportion of comments and requests stayed relatively stable over time, with comments accounting for 19.4–21.4% and requests accounting for 28.6–33.8% of TSCU.
Table 4.
Differences in slopes at each stage and AUC between the three embedded adaptive interventions.
| Difference / Effect Size (95% CI for Difference) | |||||||
|---|---|---|---|---|---|---|---|
| (SGD, SGD) vs (No SGD, No SGD) |
(SGD, SGD) vs (No SGD, SGD) |
(No SGD, SGD) vs (No SGD, No SGD) |
|||||
| Stage 1 Slope* |
Stage 2 Slope |
AUC | Stage 2 Slope |
AUC | Stage 2 Slope** |
AUC | |
| Natural Language Sample |
|||||||
| TSCU |
1.94 / 0.8 (0.7,3.2) |
−0.13 / −0.05 (−0.9,0.6) |
18.6 / 0.67 (8,29) |
−0.46 / −0.18 (−1.2,0.3) |
15.7 / 0.58 (6,25) |
0.33 / 0.13 (−0.05,0.8) |
2.6 / 0.1 (−0.4,5.6) |
| NDWR | 0.79 / 0.46 (−0.1,1.7) |
0.01 / 0.01 (−0.33,0.37) |
8.1 / 0.37 (−0.2,16.3) |
−0.18 / −0.13 (−0.62,0.27) |
6.5 / 0.30 (−1.7,14.8) |
0.19 / 0.13 (−0.05,0.43) |
1.5 / 0.07 (−0.4,3.4) |
| Early Social Communication Scale |
|||||||
| IJA |
0.36 / 0.43 (0.02,0.7) |
−0.08 / −0.1 (−0.28,0.13) |
2.9 / 0.43 (0.39,5.5) |
−0.15 / −0.18 (−0.36,0.06) |
2.4 / 0.35 (−0.1,4.8) |
0.07 / 0.08 (0.004,0.13) |
0.54 / 0.08 (0.03,1.0) |
| IBR | 0.17 / 0.21 (−0.2,0.6) |
0.03 / 0.03 (−0.21,0.27) |
1.9 / 0.24 (−0.7,4.5) |
−0.03 / −0.03 (−0.28,0.22) |
1.5 / 0.19 (−1.3,4.3) |
0.05 / 0.06 (−0.05,0.15) |
0.4 / 0.05 (−0.4,1.1) |
| Structured Play Assessment |
|||||||
| UPA | −0.11 / −0.16 (−0.4,0.2) |
0.14 / 0.24 (−0.05,0.3) |
0.03 / 0 (−2.1,2.1) |
0.13 / 0.23 (−0.07,0.33) |
−0.03 / 0 (−2.2,2.2) |
0.01 / 0.01 (−0.07,0.09) |
0.06 / 0.01 (−0.6,0.7) |
Notes.
Abbreviations: SGD—Speech generating device; TSCU—Total socially communicative utterances; NDWR— Number of direct word roots; IJA—Initiating joint attention; IBR—Initiating behavioral regulation; UPA— Unique play acts; AUC—the average area under the estimated longitudinal curve from baseline to week 36 (has the interpretation as the average outcome over the course of the study).
Comparisons with a 95% confidence interval that does not include zero are boldfaced.
The stage 1 slopes comparison for (SGD, SGD) vs (No SGD, No SGD) and (SGD, SGD) vs (No SGD, SGD) are identical; hence we report it only once in the (SGD, SGD) vs (No SGD, No SGD) column.
The two adaptive interventions beginning with No SGD have identical stage 1 slopes; hence, for the (No SGD, SGD) vs (No SGD, No SGD) comparison, we only report a stage 2 pair-wise comparison.
The differences in trends among the three adaptive interventions were especially interesting for the social outcome IJA (Figure 2). Introducing the SGD initially (for all children) or delaying its introduction until later (for slower responders, only) led to comparable AUC, such that (SGD, SGD) > (No SGD, No SGD) (estimate, 2.9; 95% CI, 0.39 to 5.5; moderate effect size, 0.43) and (No SGD, SGD) > (No SGD, No SGD) (estimate, 0.54; 95% CI, 0.03 to 1.0; small effect size, 0.08), yet there was less evidence that (SGD, SGD) differed from (No SGD, SGD). This was, in part, due to slightly greater change in IJA in stage 2 by introducing the device versus intensifying JASP+EMT (estimated difference in stage 2 slopes, 0.07; 95% CI, 0.004 to 0.13; small effect size, 0.08).
While there was no evidence of between-group differences in slopes (and therefore, AUC) in novel words (NDWR; P=0.12), there was evidence of stage 1 improvement in novel words for all children, on average (overall stage 1 slope estimate, 0.99; 95% CI, 0.5 to 1.5; P<0.01). Similarly, while there was no evidence of between-group differences in slopes in initiating behavioral regulation (IBR; P=0.31), there was evidence of stage 1 improvement in initiating behavioral regulation for all children, on average (overall stage 1 slope estimate, 0.28; 95% CI, 0.07 to 0.49; P=0.01). The two preceding results—which represent average time-trends in the outcome, rather than between-group differences in trends—are not provided in Table 3. For unique play actions (UPA), there was no evidence of between-group differences in slopes/AUC (P=0.52), nor evidence of overall or within-group differences in change.
DISCUSSION
This manuscript presents results of a secondary data analysis of sixty-one minimally-verbal children ages 5 to 8 with ASD who participated in a sequential multiple-assignment randomized trial (SMART; Kasari et al., 2014) The goal of this analysis was to compare three adaptive interventions involving different provisions of an SGD in the context of a naturalistic, developmental behavioral intervention, JASP+EMT for increasing spoken language. The three, two-stage adaptive interventions were compared in terms of their trajectories and area under the curve from baseline to week 36 on five key communication outcomes including two verbal outcomes (TSCU and NDWR) and three non-linguistic outcomes (IJA, IBR and UPA).
Among the three adaptive interventions that were compared, the (SGD, SGD) adaptive intervention was found to be superior. This adaptive intervention is made up of the following intervention components: (i) treatment begins with JASP+EMT+SGD twice per week for 12 weeks; (ii) responder status is assessed at the end of week 12 (see the Methods, Adaptive Interventions section for details on this intervention component); (iii) children showing an early response to treatment at the end of 12 weeks continue with JASP+EMT+SGD for an additional 12 weeks; and (iv) children exhibiting a slower response by the end of 12 weeks receive intensified JASP+EMT+SGD from twice per week to three times per week. This adaptive intervention led to improved spontaneous spoken communicative utterances and initiating joint attention relative to the (No SGD, No SGD) adaptive intervention, with moderate AUC effect sizes of 0.43 and 0.67, respectively. Relative to the (No SGD, SGD) adaptive intervention, (SGD, SGD) led to improved spontaneous spoken communicative utterances with a slightly more attenuated AUC effect size of 0.58. A separate analysis of participant and therapist communication interactions during the intervention sessions found that children in the (SGD, SGD) adaptive intervention demonstrated greater increases in the amount of time that they spent engaged in reciprocal communication with the therapist (DiStefano, Shih, Kaiser, Landa, & Kasari, under review). Taken together, these results may suggest that using an SGD within an effective naturalistic behavioral developmental intervention may facilitate longer and more frequent reciprocal communication interactions, leading to gains in verbal and non-linguistic communication skills. It is interesting to note that within this intervention, the therapist did not provide direct instruction to the child to use the SGD and the child was never required to use the SGD—indeed, providing the SGD did not lead to children using the SGD to communicate (see page 643 of Kasari et al., 2014). Instead, the therapist (i) consistently used the SGD (along with spoken language) and (ii) responded to child use of the SGD. This raises the possibility that the communication gains made by children in the (SGD, SGD) adaptive intervention (relative to the other adaptive interventions) could be explained by the therapist modeling SGD use, with or without child SGD use. Future work is needed to examine this and other potential mechanisms.
While there was no evidence in this analysis of a statistically significant difference in novel words between the three adaptive interventions (P=0.12), it was estimated that, on average over the course of the six month study, children would have eight additional novel words (95%CI, −0.2 to 16.3; effect size, 0.37) under the (SGD, SGD) adaptive intervention (AUC=29.8) relative to the (No SGD, No SGD) adaptive intervention (AUC=21.7), and six additional novel words (95%CI, −1.7 to 14.8; effect size, 0.3) under (SGD, SGD) relative to the (No SGD, SGD) adaptive intervention (AUC=23.2). Developing and evaluating interventions that improve novel words is an important challenge for researchers, given that this represents a higher bar relative to changing the total number of spontaneous communicative utterances. Increases in spontaneous communicative utterances may represent a child using the same small set of words more frequently, while increases in novel words indicates that the child has developed an expanded expressive vocabulary. A difference over time of eight novel words between (SGD, SGD) versus (No SGD, No SGD), a moderate-small effect size of 0.37, coupled with an overall estimated change of one novel word per week during stage 1 (slope averaged over SGD and No SGD, 0.99; 95% CI, 0.51 to 1.48) is both clinically significant and encouraging. Future ASD interventions research could benefit from larger sample sizes in order to detect moderate-small changes in NDWR of the kind observed here.
A significant gain in initiating joint attention in stage 2 was observed under the (No SGD, SGD) adaptive intervention (slope, 0.13; 95%CI, 0.001 to 0.26), which provided SGD access at week 12 only to slow responders to JASP+EMT. While this gain was (in absolute terms) slower than the gain in IJA observed during stage 1 under the (SGD, SGD) adaptive intervention (slope, 0.35; 95%CI, 0.03 to 0.7), children under the (No SGD, SGD) adaptive intervention on average appear to “catch up” to peers who followed the (SGD, SGD) adaptive intervention, which provided SGD from the beginning (see Figure 2). This finding is important because while all children who received the (SGD, SGD) intervention had access to the SGD over 24 weeks in total, only an estimated 40% of children (12/30) who received the (No SGD, SGD) intervention had access to the SGD and only for last 12 weeks; yet, IJA outcomes were on average similar at week 36 under both of these adaptive interventions.
There was no evidence in this analysis of a statistically significant difference in initiating behavioral regulation (IBR; P=0.31) among the three adaptive interventions. Although requests are a part of JASP+EMT (in addition to comments) especially when it seemed developmentally appropriate, JASPER places a heavier focus on social commenting (IJA) over requesting (IBR). It is not surprising, then, that the provision of the SGD alongside JASP+EMT did not have an effect on IBR. Nevertheless, it is encouraging that overall positive changes in IBR were observed among the minimally verbal children in this study, given that initiating behavioral regulation would be expected to increase as children gain additional communication skills, even without being specifically targeted.
For all outcomes considered, except for play, children in the (SGD, SGD) adaptive intervention demonstrated, on average, a rapid stage 1 increase that then stabilized in stage 2 and maintained ?through follow-up. Recall that under the (SGD, SGD) intervention, all children received JASP+EMT+SGD initially, slower responders received intensified JASP+EMT+SGD, and responders continued on JASP+EMT+SGD. The lack of positive change under the (SGD, SGD) adaptive intervention from week 12 onward (on all outcomes) may suggest areas for improvement. Future studies may develop and evaluate approaches for extending the gains under JASP+EMT+SGD. For example, strategic introduction of new play materials and activities along with expanded SGD symbol displays may help to extend the novelty of the intervention context and SGD, as well as introduce new vocabulary. This in turn could facilitate continued motivation for social communication. Future studies may also evaluate other alternatives for slower responders to JASP+EMT+SGD. One approach may be to blend JASP+EMT+SGD with other existing behavioral interventions designed to improve spoken communication, such as with core principles of discrete trial training (DTT; Smith, 2001), and similar to the priming used in earlier versions of JASPER (Kasari et al, 2006).
At study entry, children demonstrated a low rate of socially communicative utterances. Interestingly, on average children demonstrated both spontaneous requests and comments at entry although communication occurred at low rates initially. The current paper highlights an important measurement distinction when examining the form and function of social communication. All too often, composite outcome variables including both requesting and joint attention skills are presented. In such cases, the reader is not able to discern which behaviors are changing and if change in only one function are driving the overall changes in the children’s outcomes. In contrast, the transcription and coding systems utilized in this study allowed for clear differentiation of children’s communication by function including communication to request and more challenging, communication to share (joint attention, commenting). The current findings uniquely highlight that children who are minimally verbal can make gains over time in both requesting skills, as well as social sharing—a challenging outcome to move forward.
Total unique play acts was the only outcome of the five for which there was no evidence of differences among the three adaptive interventions, nor evidence of significant change over time overall or under any one of the adaptive interventions. Across treatment arms, play was targeted within the same developmental framework from early simple cause and effects actions on objects through symbolic pretend play (Kasari & Chang, 2014). Therefore, within the sessions not only was children’s play diversity (number of unique types of acts) targeted but also advances in the level of children’s play. Although no significant change within groups was noted in children’s play diversity (UPA) as measured by the Structured Play Assessment, it is possible that children made gains in play skills that were not captured by this variable within an assessment context. Further examination of overall gains in play, including gains in specific type of play (e.g., symbolic versus pre-symbolic) are examined in greater detail by Chang et al. (under review).
To our knowledge, this is the first study to examine the longitudinal effects of different sequences of decision rules (i.e., adaptive interventions) guiding the provision of JASP+EMT and a SGD among children with ASD who are minimally verbal. Both the SMART study design used to collect the data, as well as the longitudinal statistical methods employed in this analysis (Lu et al., 2015), are novel. The SMART design allowed us to compare the effectiveness of three adaptive interventions—two that introduce the SGD at different time points (and for different children) and one that does not provide an SGD to any child. The analyses allowed us to examine how outcome trajectories differ at the time points where the adaptive interventions differ (i.e., at baseline and week 12). More common alternative research designs do not provide the appropriate data for answering this question (e.g., a two-arm randomized trial in which children are randomized to JASP+EMT+SGD versus JASP+EMT does not provide data on the provision of SGD in the context of an adaptive intervention) or are not as efficient as the SMART in addressing this question (e.g., a three-arm randomized trial in which children are randomized to one of the three adaptive interventions).
While there is much interest in adaptive interventions, and in the use of SMART designs to develop empirically-based adaptive interventions, additional substantive and methodological work is needed. Future substantive work in children with ASD who are minimally verbal could focus on identifying the type of children at baseline who would benefit more or less or equally from one adaptive intervention over another (i.e., moderators analysis). For example, building on the novelty argument above, it may be that the effect of the SGD is minimized for children who have previous experience with an SGD, or for minimally verbal children who have a relatively larger number of spontaneous communicative utterances at baseline. In addition, we conjecture that children with lower non-verbal IQ will benefit more from (No SGD, SGD) because their ability to understand and use the SGD will likely be increased by waiting until the JASP+EMT context has become more familiar, whereas children with higher non-verbal IQ would benefit more from (SGD, SGD). Such additional analyses would have clear clinical implications in that they could be used to develop more deeply-tailored sequences of interventions for children with ASD who are minimally verbal by taking advantage of the heterogeneous disposition of these children at baseline. As noted above, future substantive work could also focus on further examining the mechanisms by which the (SGD, SGD) adaptive intervention led to improved outcomes relative to the other adaptive interventions. There is also a need for additional methodological advancements. Many state-of-the-art methods that we have become accustomed to using—such as random effects models (Verbeke & Molenberghs, 2009) to extend the longitudinal analyses presented here by examining longitudinal variance components, or mediation analyses (MacKinnon & Fairchild, 2009) for examining mechanism(s) by which the (SGD, SGD) adaptive intervention led to improved outcomes relative to the other adaptive interventions—have not been developed or applied for use with data arising from a SMART.
Acknowledgments
Clinical Trials Number: NCT01013545. We would like to thank the families and children who participated in this study. We would also like to thank the team of interventionists, coders, transcribers, and data analysts at our three sites: UCLA—Kathryne Krueger, Dalia Kabab, Caitlin McCracken, Julia Kim, Alison Holbrook, Abbey Hye, Kelsey Johnson; Vanderbilt University—Stephanie Jordan, Courtney Wright, Blair Burnette, Jennifer Nietfeld; KKI—Philip Menard, Emily Watkins, Kerry Buechler, Christine Hess, Sarah Gardner.
FUNDING
This study was funded by Autism Speaks grant #5666, Characterizing Cognition in Nonverbal Individuals with Autism, awarded to the last author. We would also like to acknowledge funding from the National Institutes of Health: R01DA039901 (Almirall, Nahum-Shani), R03MH097954 (Almirall), P50DA039838 (Almirall), and R01HD073975 (Kasari, Kaiser, Almirall, Shire, Lu, Nahum-Shani); and the Autism Speaks Mexiner Postdoctoral Fellowship in Translational Research (DiStefano).
Contributor Information
Daniel Almirall, Email: daniel.almirall@gmail.com.
Charlotte DiStefano, Email: cmucchetti@gmail.com.
Ya-Chih Chang, Email: ya-chih.chang27@calstatela.edu.
Stephanie Shire, Email: stephpatterson25@gmail.com.
Ann Kaiser, Email: ann.kaiser@vanderbilt.edu.
Xi Lu, Email: luxi@umich.edu.
Inbal Nahum-Shani, Email: inbal@umich.edu.
Rebecca Landa, Email: landa@kennedykrieger.org.
Pamela Mathy, Email: pamela.mathy@hsc.utah.edu.
Connie Kasari, Email: kasari@gseis.ucla.edu.
REFERENCES
- Almirall D, Compton SN, Rynn MA, Walkup JT, Murphy SA. SMARTer discontinuation trial designs for developing an adaptive treatment strategy. Journal of child and adolescent psychopharmacology. 2012;22(5):364–374. doi: 10.1089/cap.2011.0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almirall D, Nahum-Shani I, Sherwood NE, Murphy SA. Introduction to SMART designs for the development of adaptive interventions: with application to weight loss research. Translational Behavioral Medicine. 2014;4(3):260–274. doi: 10.1007/s13142-014-0265-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson DK, Lord C, Risi S, DiLavore PS, Shulman C, Thurm A, Pickles A. Patterns of growth in verbal abilities among children with autism spectrum disorder. Journal of Consulting and Clinical Psychology. 2007;75(4):594. doi: 10.1037/0022-006X.75.4.594. [DOI] [PubMed] [Google Scholar]
- Buuren S, Groothuis-Oudshoorn K. MICE: Multivariate imputation by chained equations in R. Journal of statistical software. 2011;45(3) [Google Scholar]
- Chakraborty B. Dynamic treatment regimes for managing chronic health conditions: A statistical perspective. American journal of public health. 2011;101(1):40. doi: 10.2105/AJPH.2010.198937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakraborty B, Moodie EE. Statistical Methods for Dynamic Treatment Regimes: Reinforcement Learning, Causal Inference, and Personalized Medicine. New York: Springer-Verlag; 2013. [Google Scholar]
- Chang YC, Shih W, Kaiser AP, Landa R, Kasari C. Older Minimally Verbal Children with Autism: Learning to play. (under review) [Google Scholar]
- Cohen J. Statistical power for the behavioral sciences. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Cress CJ, Marvin CA. Common questions about AAC services in early intervention. Augmentative and alternative communication. 2003;19(4):254–272. [Google Scholar]
- DiStefano C, Shih W, Kaiser A, Landa R, Kasari C. Communication growth in minimally verbal children with ASD: The importance of interaction. doi: 10.1002/aur.1594. (under review) [DOI] [PubMed] [Google Scholar]
- Frost L, Bondy A. The picture exchange communication system training manual: Pyramid Educational Products, Incorporated. 2002 [Google Scholar]
- Gast DL, Ledford JR. Single-subject research methodology in behavioral sciences. Routledge; 2009. [Google Scholar]
- Hancock T, Kaiser A. Enhanced Milieu Teaching. In: McAuley RJ, Fey ME, editors. Treatment of language disorders in children. Baltimore, MD: Paul H. Brookes Publishing Co; 2006. [Google Scholar]
- Howlin P, Goode S, Hutton J, Rutter M. Adult outcome for children with autism. Journal of Child Psychology and Psychiatry. 2004;45(2):212–229. doi: 10.1111/j.1469-7610.2004.00215.x. [DOI] [PubMed] [Google Scholar]
- Kaiser AP, Roberts MY. Parent-implemented enhanced milieu teaching with preschool children who have intellectual disabilities. Journal of Speech, Language, and Hearing Research. 2013;56(1):295–309. doi: 10.1044/1092-4388(2012/11-0231). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasari C, Chang YC. Handbook of Autism and Pervasive Developmental Disorders. Fourth 2014. Play development in children with Autism Spectrum Disorders: skills, object play, and interventions. [Google Scholar]
- Kasari C, Freeman S, Paparella T. Joint attention and symbolic play in young children with autism: A randomized controlled intervention study. Journal of Child Psychology and Psychiatry. 2006;47(6):611–620. doi: 10.1111/j.1469-7610.2005.01567.x. [DOI] [PubMed] [Google Scholar]
- Kasari C, Kaiser A, Goods K, Nietfeld J, Mathy P, Landa R, Almirall D. Communication Interventions for Minimally Verbal Children With Autism: A Sequential Multiple Assignment Randomized Trial. Journal of the American Academy of Child & Adolescent Psychiatry. 2014;53(6):635–646. doi: 10.1016/j.jaac.2014.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasari C, Paparella T, Freeman S, Jahromi LB. Language outcome in autism: randomized comparison of joint attention and play interventions. Journal of Consulting and Clinical Psychology. 2008;76(1):125. doi: 10.1037/0022-006X.76.1.125. [DOI] [PubMed] [Google Scholar]
- Kasari C, Tager-Flusberg H, Cooper J. NIH Workshop on Nonverbal School-aged Children with Autism; Paper presented at the National Institutes of Health; Rockville, Maryland. 2010. [Google Scholar]
- Lavori PW, Dawson R. A design for testing clinical strategies: biased adaptive within-subject randomization. Journal of the Royal Statistical Society: Series A (Statistics in Society) 2000;163(1):29–38. [Google Scholar]
- Lavori PW, Dawson R. Dynamic treatment regimes: practical design considerations. Clinical trials. 2004;1(1):9–20. doi: 10.1191/1740774s04cn002oa. [DOI] [PubMed] [Google Scholar]
- Lavori PW, Dawson R. Introduction to Dynamic Treatment Strategies and Sequential Multiple Assignment Randomization. Clinical trials. 2014;11(4):393–399. doi: 10.1177/1740774514527651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavori PW, Dawson R, Rush AJ. Flexible treatment strategies in chronic disease: clinical and research implications. Biological psychiatry. 2000;48(6):605–614. doi: 10.1016/s0006-3223(00)00946-x. [DOI] [PubMed] [Google Scholar]
- Lord C. Commentary: achievements and future directions for intervention research in communication and autism spectrum disorders. Journal of autism and developmental disorders. 2000;30(5):393–398. doi: 10.1023/a:1005591205002. [DOI] [PubMed] [Google Scholar]
- Lord C, Risi S, Lambrecht L, Cook EH, Jr, Leventhal BL, DiLavore PC, Rutter M. The Autism Diagnostic Observation Schedule—Generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of autism and developmental disorders. 2000;30(3):205–223. [PubMed] [Google Scholar]
- Lu X, Nahum-Shani I, Kasari C, Lynch KG, Oslin DW, Pelham WE, Almirall D. Comparing dynamic treatment regimes using repeated-measures outcomes: modeling considerations in SMART studies. Statistics in Medicine. 2015 doi: 10.1002/sim.6819. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ. Current directions in mediation analysis. Current directions in psychological science. 2009;18(1):16–20. doi: 10.1111/j.1467-8721.2009.01598.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller J, Chapman R. Systematic analysis of language transcripts. Madison, WI: Language Analysis Laboratory; 1985. [Google Scholar]
- Moodie EE, Richardson TS, Stephens DA. Demystifying optimal dynamic treatment regimes. Biometrics. 2007;63(2):447–455. doi: 10.1111/j.1541-0420.2006.00686.x. [DOI] [PubMed] [Google Scholar]
- Mundy P, Delgado C, Block J, Venezia M, Hogan A, Seibert J. A Manual for the Early Social Communication Scales (ESCS) 2013 Retrieved from University of California at Davis: http://education.ucdavis.edu/sites/main/files/file-attachments/escs_manual_2003_2013.pdf.
- Mundy P, Newell L. Attention, joint attention, and social cognition. Current directions in psychological science. 2007;16(5):269–274. doi: 10.1111/j.1467-8721.2007.00518.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mundy P, Sigman M, Kasari C. A longitudinal study of joint attention and language development in autistic children. Journal of autism and developmental disorders. 1990;20(1):115–128. doi: 10.1007/BF02206861. [DOI] [PubMed] [Google Scholar]
- Mundy P, Sigman M, Ungerer J, Sherman T. Defining the social deficits of autism: The contribution of non-verbal communication measures. Journal of Child Psychology and Psychiatry. 1986;27(5):657–669. doi: 10.1111/j.1469-7610.1986.tb00190.x. [DOI] [PubMed] [Google Scholar]
- Murphy SA. An experimental design for the development of adaptive treatment strategies. Statistics in Medicine. 2005;24(10):1455–1481. doi: 10.1002/sim.2022. [DOI] [PubMed] [Google Scholar]
- Murphy SA, Almirall D. Dynamic treatment regimens. In: Kattan M, editor. Encyclopedia of Medical Decision Making. Thousand Oaks, CA: Sage Publications; 2009. [Google Scholar]
- Nahum-Shani I, Qian M, Almirall D, Pelham WE, Gnagy B, Fabiano G, Murphy SA. Experimental Design and Primary Data Analysis for Developing Adaptive Interventions. Psychological methods. 2012;17(4):457. doi: 10.1037/a0029372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Research Council. Educating children with autism. Washington, D.C: National Academy Press; 2001. [Google Scholar]
- Orellana L, Rotnitzky A, Robins JM. Dynamic regime marginal structural mean models for estimation of optimal dynamic treatment regimes, part I: main content. The International Journal of Biostatistics. 2010;6(2) Article 8. [PubMed] [Google Scholar]
- Rutter M. Diagnosis and definition of childhood autism. Journal of autism and childhood schizophrenia. 1978;8(2):139–161. doi: 10.1007/BF01537863. [DOI] [PubMed] [Google Scholar]
- Schafer JL. Multiple imputation: A primer. Statistical Methods in Medical Research. 1999;8:3–15. doi: 10.1177/096228029900800102. [DOI] [PubMed] [Google Scholar]
- Shire SY, Goods K, Shih W, Distefano C, Kaiser A, Wright C, Kasari C. Parents’ Adoption of Social Communication Intervention Strategies: Families Including Children with Autism Spectrum Disorder Who are Minimally Verbal. Journal of autism and developmental disorders. 2014;45:1712–1724. doi: 10.1007/s10803-014-2329-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shortreed SM, Laber E, Stroup ST, Pineau J, Murphy SA. A multiple imputation strategy for sequential multiple assignment randomized trials. Statistics in Medicine. 2014;33(24):4202–4214. doi: 10.1002/sim.6223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith T. Discrete trial training in the treatment of autism. Focus on autism and other developmental disabilities. 2001;16(2):86–92. [Google Scholar]
- Tager-Flusberg H, Kasari C. Minimally Verbal School-Aged Children with Autism Spectrum Disorder: The Neglected End of the Spectrum. Autism Research. 2013;6(6):468–478. doi: 10.1002/aur.1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ungerer JA, Sigman M. Symbolic play and language comprehension in autistic children. Journal of the American Academy of Child Psychiatry. 1981;20(2):318–337. doi: 10.1016/s0002-7138(09)60992-4. [DOI] [PubMed] [Google Scholar]
- van der Meer LA, Rispoli M. Communication interventions involving speech-generating devices for children with autism: A review of the literature. Developmental Neurorehabilitation. 2010;13(4):294–306. doi: 10.3109/17518421003671494. [DOI] [PubMed] [Google Scholar]
- Verbeke G, Molenberghs G. Linear mixed models for longitudinal data. New York: Springer-Verlag; 2009. [Google Scholar]
- Wodka EL, Mathy P, Kalb L. Predictors of phrase and fluent speech in children with autism and severe language delay. Pediatrics. 2013;131(4):e1128–e1134. doi: 10.1542/peds.2012-2221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan J, Hojsgaard S, Halekoh U. geepack: Generalized estimating equation package. 2015 Retrieved from https://cran.r-project.org/web/packages/geepack/geepack.pdf.
- Zhang B, Tsiatis AA, Laber EB, Davidian M. Robust estimation of optimal dynamic treatment regimes for sequential treatment decisions. Biometrika. 2013 doi: 10.1093/biomet/ast014. e-pub ahead of print. Retrieved from http://biomet.oxfordjournals.org/content/early/2013/05/30/biomet.ast014. [DOI] [PMC free article] [PubMed]