Abstract
Objective
Evidence suggests interdependence between cancer patients’ and their caregivers’ physical and mental health. However, the extent to which caregivers’ health relates to their patients’ recovery, or patients’ health affects their caregivers’ outcomes, is largely unknown. This dyadic investigation reports the relations between cancer patients’ and their caregivers’ physical and mental health trajectories during the year following diagnosis.
Design
Ninety-two colorectal cancer patient-caregiver dyads completed questionnaires at two, six, and twelve months post-diagnosis.
Outcome Measures
Self-reported physical and mental health using the Medical Outcomes Study Short Form Health Survey-12.
Results
Patients reported improved physical health over the year following their diagnosis, whereas caregivers reported declining physical health. Patients with lower mental health at diagnosis had stagnated physical health recovery. Caregivers’ physical health declined most noticeably among those reporting low mental health at diagnosis and whose patients reported low physical health at diagnosis.
Conclusion
Findings suggest targeting health interventions to cancer patients and caregivers reporting poor mental health at diagnosis may mitigate their long-term physical morbidity. Limited evidence of dyadic interdependence between patients’ and caregivers’ physical and mental health trajectories suggests future studies are warranted to identify psychosocial and medical characteristics moderating the relations between patients’ and caregivers’ health.
Keywords: cancer, caregiving, physical health, mental health, actor partner interdependence model, latent growth model
Introduction
Recovering physical health during the first year following a cancer diagnosis is critical to patients’ survival (Patterson et al., 2011). This goal is shared and influenced by patients’ family and friends, constituting the estimated 4.6 million Americans providing informal care to an adult with cancer (National Alliance for Caregiving, 2009). The stresses of this critical time put these informal caregivers at significant risk for their own long-term physical health decline (Nijboer, Tempelaar, Triemstra, Sanderman, & van den Bos, 2001; Rohleder, Marin, Ma, & Miller, 2009), and also contribute to increased mental health burden among both patients (Massie, 2004; Mitchell et al., 2011; Pirl, 2004) and caregivers (Braun, Mikulincer, Rydall, Walsh, & Rodin, 2007; Janda et al., 2007).
Dyadic coping theory posits that patients and their caregivers react in tandem as an “emotional system” to shared stressful events such as cancer (Berg & Upchurch, 2007; Bodenmann, 2005). The interdependence between cancer patients’ and their caregivers’ mental health is well documented (Hagedoorn, Sanderman, Bolks, Tuinstra, & Coyne, 2008; Hodges, Humphris, & Macfarlane, 2005). The extent to which patients’ and their caregivers’ physical health trajectories also are interdependent has yet to be documented, as well as the extent to which their physical and mental health trajectories interrelate. Guided by dyadic coping and biopsychosocial theory, this study reports the first dyadic investigation of cancer patients’ and their caregivers’ physical and mental health trajectories during the year following the diagnosis, providing critical information to improve identification of patients and caregivers at greatest risk for poor health outcomes.
Background
During the year following the cancer diagnosis, patients’ physical ability to perform daily routines and social activities is frequently limited by disease symptoms and treatment side effects, such as fatigue (23–90% patients; Cella, Davis, Breitbart, & Curt, 2001; Pachman, Barton, Swetz, & Loprinzi, 2012; Yamagishi, Morita, Miyashita, & Kimura, 2009), pain (25–33%; Goudas, Bloch, Gialeli-Goudas, Lau, & Carr, 2005; National Comprehensive Cancer Network, 2012), and gastro-intestinal problems (9–23%; Esther Kim, Dodd, Aouizerat, Jahan, & Miaskowski, 2009; Meuser et al., 2001). These physical symptoms tend to lessen in severity after treatment is completed, yet some patients report persistent symptoms months to years following treatment (Bower & Lamkin, 2013; Pachman et al., 2012). Patients who self-report low physical health at diagnosis (Wong, Law, Wan, Poon, & Lam, 2014) and do not report improved physical health during the two years following treatment for cancer (Patterson et al., 2011) show elevated all-cause mortality, making self-reported physical health a critical indicator for patient outcomes.
Contrary to their patients’ physical health improvement during the year following diagnosis, caregivers exhibit physical health decline during the same period (Nijboer et al., 2001; Rohleder et al., 2009). Compared to demographically comparable non-caregivers, cancer caregivers self-report worse physical health (Li & Loke, 2013) and display increased risk for heart attacks and strokes (Ji, Zöller, Sundquist, & Sundquist, 2012). Recent evidence suggests that patients’ and their caregivers’ physical health trajectories are interdependent (Segrin & Badger, 2014). Declines in patients’ physical functioning translate into greater caregiving burden, which has been linked with caregivers’ physical health decline (Grunfeld et al., 2004; Pinquart & Sörensen, 2007). Caregivers’ own poor physical health increases their risk of engaging in poor caregiving behavior (Beach et al., 2005), which may be detrimental to patients’ health. However, no dyadic studies have yet examined the extent to which patients’ and their caregivers’ physical health trajectories relate during the critical year following diagnosis.
The mental health toll of cancer also contributes to disease burden among patients and caregivers. Patients report elevated symptoms of anxiety (10–49%; Mitchell et al., 2011; van't Spijker, Trijsburg, & Duivenvoorden, 1997) and depression (15–58%; Massie, 2004; Mitchell et al., 2011; Pirl, 2004) during the year following diagnosis, with the psychological turmoil of diagnosis and treatment often disrupting their daily life and social relationships. For caregivers, while most adapt effectively to the diagnosis during the first year (Hagedoorn et al., 2008; Pitceathly & Maguire, 2003), up to 40 percent of cancer caregivers report clinically significant symptoms of depression (Braun et al., 2007) and anxiety (Janda et al., 2007). For both patients and caregivers, although their psychological distress tends to decline over time, those reporting high distress around the time of diagnosis show prolonged elevations in distress across the cancer trajectory (Kim, Shaffer, Carver, & Cannady, 2014; Lambert, Jones, Girgis, & Lecathelinais, 2012; Milbury, Badr, Fossella, Pisters, & Carmack, 2013; Nordin, Berglund, Glimelius, & Sjöden, 2001; Palos et al., 2011). Moreover, dyadic analyses have documented interdependence between patients’ and their caregivers’ mental health following the cancer diagnosis both cross-sectionally (Hagedoorn et al., 2008; Hodges et al., 2005; Kim, Duberstein, Sörensen, & Larson, 2005) and over time (Kim, Ryn, et al., 2014; Moser, Künzler, Nussbeck, Bargetzi, & Znoj, 2013; Segrin, Badger, Dorros, Meek, & Lopez, 2007; Segrin et al., 2005).
Biopsychosocial models now highlight, however, that overall wellness must consider physical and mental health conjointly, with these elements being inextricably linked for both cancer patients and their caregivers. Patients expressing high levels of depressive symptoms (Hoppe et al., 2013; Pinquart & Duberstein, 2010; Satin, Linden, & Phillips, 2009) and stress (Chida, Hamer, Wardle, & Steptoe, 2008) have poorer physical health and treatment outcomes. Similarly for caregivers, those who report high levels of distress show elevated risk for premature morbidity and mortality (Kim, Carver, Shaffer, Gansler, & Cannady, 2015; Pinquart & Sörensen, 2007; Schulz & Beach, 1999; Vitaliano et al., 2002), whereas those reporting psychosocial benefits from caregiving show reduced mortality risk (Brown et al., 2009). Recent cross-sectional dyadic studies have linked patients’ physical health with their caregivers’ psychological health and vice versa: caregivers’ heightened psychological distress was concurrently related to their patients’ poorer physical functioning (Kim, Kashy, et al., 2008; Kim, Wellisch, & Spillers, 2008), and patients’ greater distress was concurrently related to their caregivers’ poorer physical health (Kim, van Ryn, et al., 2014). However, no studies have longitudinally studied the dyadic relations between patients’ and their caregivers’ physical and mental health trajectories.
Current Study and Hypotheses
Findings thus far suggest the mutual, dyadic impact of cancer patients’ and their caregivers’ physical and mental health on the other’s health outcomes. However, to date, no studies have prospectively documented the interrelationship of patients’ and caregivers’ physical and mental health changes over the first year following diagnosis, when the burdens of treatment and caregiving as well as psychological distress are greatest among both patients and caregivers. Better understanding the dyadic relations between patients’ and caregivers’ health trajectories holds both theoretical implications for the extension of dyadic stress theory to patients’ and caregivers’ physical health, as well as clinical implications for determining risk factors for those patients and caregivers at risk for poor long-term health outcomes.
To fill this gap in the literature, the current study undertook a novel dyadic examination of patients’ and their caregivers’ physical and mental health adjustment across the year following the cancer diagnosis. We first examined physical health trajectories among both patients and caregivers at individual and dyadic levels, hypothesizing that patients’ and their caregivers’ physical health trajectories would be positively related (i.e., greater physical health decline among patients would be related to greater physical health decline among caregivers). Then similarly, we examined patient and caregiver mental health trajectories, hypothesizing that patients’ and caregivers’ mental health trajectories would also be positively related. Last, we examined the relations between physical and mental health trajectories among both patients and caregivers at individual and dyadic levels, hypothesizing that patients’ mental health trajectories would be positively related both to their own and their caregivers’ physical health trajectories, and vice versa for physical health to mental health, as well as from caregivers’ health to patients’ health.
Method
Participants
Cancer patients were eligible and invited to participate if they were 18 years or older, able to read and speak English, diagnosed with colon or rectal cancer in stage I to IV for the first time during the two months prior to study participation, and lived within 50 miles of the study hospital. Patients identified family members or close friends from whom they expected to receive consistent help through their cancer experience. These caregivers were eligible and invited to participate in the study if they were 18 years or older, able to read and speak English, and lived within 50 miles of the study hospital.
In total, 116 patients and 195 caregivers completed questionnaires for at least one of three assessment time points at two (T1), six (T2), and twelve months (T3) post-diagnosis. To estimate dyadic effects, patients and caregivers were only included in analyses if they had a partner (i.e., caregiver or patient, respectively) participating with them. For patients with more than one participating caregiver (N= 43), the caregiver with the most complete data on study variables was selected for data analyses. A total of 92 patient-caregiver dyads were included in analyses. Patients and caregivers excluded from analyses (Ns= 24 and 103, respectively) did not differ from those included in the analyses on any study or demographic variable (ps> .11) with three exceptions: a marginally greater proportion of excluded patients were female (52 vs. 32 percent, p= .06), excluded patients had marginally lower mental health at T3 (Ms= 49.99 vs. 53.75, p= .08), and excluded caregivers were significantly younger (49.65 vs. 55.64 years, p= .01).
Procedure
This prospective, observational study was approved by and complied with the Institutional Review Boards of all five hospitals in Atlanta, Georgia from which participants were recruited. Eligible participants were typically recruited in-person at the hospital clinics; however, some were recruited via letter or telephone by the project manager who introduced the study and invited them to participate. Returned signed consent forms and completed surveys evidenced informed consent to participate. Each participant was compensated with a $20 gift card for each completed survey.
Measures
Physical and mental health
At each time point, self-reported physical health and mental health were assessed using the 12-item Medical Outcomes Study Short Form (MOS SF-12: Ware, Kosinski, & Keller, 1996). The physical health component score (PCS) represents a weighted composite of physical functioning, physical limitations to role requirements, bodily pain, and general health subscales. The mental health component score (MCS) represents a weighted composite of vitality, social functioning, emotional limitations to role requirements, and mental health subscales. Both scores have been normalized (US population normalized M= 50), with higher scores reflecting better mental and physical health (Ware et al., 1996).
This measure has been previously used to measure physical and mental health in dyadic studies of cancer patients and their caregivers (Kim, van Ryn, et al., 2014; Kim, Wellisch, & Spillers, 2008; Lambert et al., 2012; Moser et al., 2013). Poorer physical health scores have been related to cancer recurrence and mortality among colorectal cancer patients (Wong et al., 2014), and a prior study of colorectal cancer patients averaging three years post-diagnosis reported poorer physical health yet better mental health compared to healthy adults (Wong, Lam, Poon, & Kwong, 2013). Among caregivers, studies have previously found no difference between average caregivers’ scores with the U.S. population norm at two to eight years post-diagnosis (Kim & Spillers, 2010; Kim, Shaffer, Carver, & Spillers, 2015).
Covariate: Age
Due to the relations of age with physical and mental health (Ware et al., 1995), patient age was controlled from all patient latent variables and caregiver age was controlled from all caregiver latent variables. Patients and caregivers self-reported their date of birth, and age was calculated at date of survey completion.
Data Analysis
Means, standard deviations, and ranges of study variables were computed for the patient and caregiver samples separately. Mean differences between patients’ and caregivers’ physical and mental health were tested using paired t tests, and the strength of the relations between patients’ and caregivers’ scores were estimated using Pearson correlation coefficients. For all analyses, two-tailed tests were used, and p-values less than .05 were considered significant. Although power analyses specific to actor-partner interdependence modeling (APIM) have yet to be developed, APIM is regression-based and therefore F test power analyses may be used (Chung, Moser, Lennie, & Rayens, 2009). Given the current sample, power was approximately 82% to detect a significant prediction model with a small-to-medium effect (power estimates obtained using G*Power 3.1.9.2, Faul, 2014).
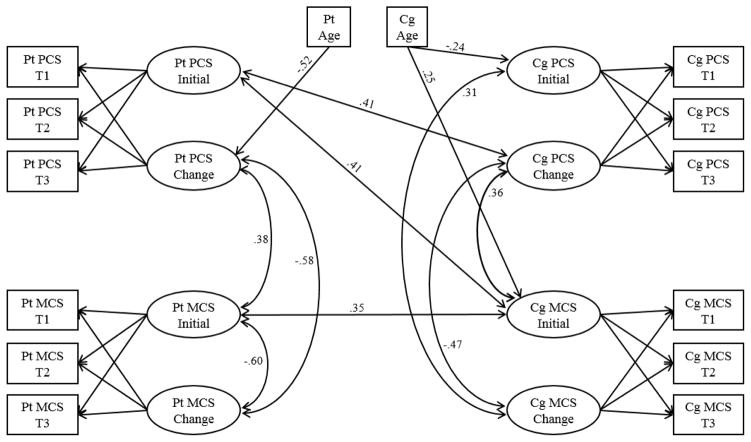
Central aims of the study were analyzed by combining latent growth modeling (LGM) with APIM within a structural equation modeling framework (Mplus 7; Muthén & Muthén, 2012). Four LGMs were specified, one each for patient physical health, patient mental health, caregiver physical health, and caregiver mental health, using three repeated measures of the variable of interest (e.g., patient self-reported physical health at T1, T2, and T3). Each LGM estimated two latent parameters: initial level of health (intercept) and change in health (slope) across the three assessments (Bollen & Curran, 2006; Muthén & Curran, 1997; Willett & Sayer, 1994). Linear change was estimated in all four LGMs by fixing loadings for the three health indicators to their respective intercept latent variable to 1 and to their respective slope latent variable to 0, 1, and 2 for T1 through T3, respectively (see Figure 1). To facilitate interpretation of results, all health indicator observed variables were centered at 50 (i.e., normalized mean for the US population), and age variables were centered to the sample mean (i.e., patient age centered at 61.56, caregiver age centered at 55.64).
Figure 1. Change in Physical and Mental Health Among Patients and Caregivers.
Note. Only significant (p< .05) paths with standardized estimates are shown; PCS = Physical Health Component Scale of the MOS SF-12; MCS = Mental Health Component Scale of the MOS SF-12; latent factor loadings for initial latent variable were set to 1 across T1 through T3; latent factor loadings for change latent variable were set at 0, 1, and 2 for T1, T2, and T3, respectively.
APIM (Cook & Kenny, 2005; Kashy & Kenny, 2000; Kenny & Cook, 1999; Kenny, Kashy, & Cook, 2006) was used to test the relations between patients’ and caregivers’ initial levels and changes in physical and mental health. In this model, patients’ actor effects represent the individual relations between their own initial levels and changes in physical and mental health (e.g., Figure 1, line connecting patient initial and change in mental health); similarly, caregivers’ actor effects represent the individual relations between their own initial levels and changes in their physical and mental health. Partner effects in this model constitute the dyadic interrelations between patients’ initial levels and changes in physical and mental health with that of their caregivers (e.g., Figure 1, line connecting patient and caregiver initial mental health).
Three model fit indices are reported: the chi-square value, the comparative fit index (CFI), and the standardized root mean square residual (SRMR). Chi-square significance values greater than .05, CFI greater than .95, and SRMR less than .08 reflect adequate fit of a specified model to the data (Hu & Bentler, 1999; Kline, 2011).
Results
As shown in Table 1, the sample was almost evenly divided between African American and white ethnicities and was diverse in terms of educational attainment and household income. Patients were diagnosed primarily with localized or regional colon cancer. A greater proportion of the patient sample was male compared to the caregiver sample. Patients and caregivers reported comparable education, income, and ethnicity.
Table 1.
Demographic and Medical Characteristics of Study Sample (N= 92)
| Patients | Caregivers | ρ | t or χ2 | df | |
|---|---|---|---|---|---|
|
| |||||
| N (%) | N (%) | ||||
| Gender (female) | 29 (31.5) | 74 (80.4) | −.43*** | 44.66*** | 1 |
| Education | .24* | 0.63 | 2 | ||
| High school degree or less | 32 (34.8) | 27 (29.3) | |||
| Vocational or Some college | 26 (28.3) | 28 (30.4) | |||
| College or greater | 34 (37.0) | 37 (40.2) | |||
| Household Income | .32** | 5.37 | 3 | ||
| < $20,000 | 17 (18.5) | 11 (12.0) | |||
| $20,000 ~ $39,999 | 23 (25.0) | 17 (18.5) | |||
| ≥ $40,000 | 40 (43.5) | 47 (51.0) | |||
| Prefer not to answer | 12 (13.1) | 17 (18.5) | |||
| Ethnicity | .88*** | 0.26 | 2 | ||
| African American | 39 (42.4) | 38 (41.3) | |||
| Non-Hispanic White | 46 (50.0) | 49 (53.3) | |||
| Other | 7 (7.6) | 5 (5.5) | |||
| Relationship to Patient | |||||
| Spouse/Partner | - | 48 (52.2) | |||
| Child/Child-in-law | - | 18 (19.6) | |||
| Other | - | 26 (28.2) | |||
| Stage of Cancer | |||||
| Localized | 42 (45.7) | – | |||
| Regional | 33 (35.9) | – | |||
| Distant | 12 (13.3) | – | |||
| Unstaged/Unknown | 5 (5.4) | ||||
| Cancer Diagnosis | |||||
| Colon | 62 (67.4) | – | |||
| Rectal | 24 (26.1) | – | |||
| Both | 3 (3.3) | – | |||
| Unknown | 3 (3.3) | ||||
p < .05
p < .01
p < .001
Table 2 presents descriptive information on the study variables for patients and caregivers. Compared to their caregivers, patients were older, reported poorer physical health at T1 and T2, and better mental health at T1. Patients’ and their caregivers’ physical health reports were unrelated at each time point, whereas their mental health reports were positively associated to a small-to-moderate degree at each time point.
Table 2.
Descriptives and Paired t-tests of Age and Physical and Mental Health of Patients and Caregivers
| Patients
|
Caregivers
|
Paired t-test
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | M | SD | Range | N | M | SD | Range | t | df | r | |
| Age | 87 | 61.56 | 12.13 | 37.58–88.47 | 83 | 55.64 | 13.25 | 28.61–93.26 | 3.65*** | 80 | .28* |
| PCS at T1 | 85 | 38.10*** | 11.29 | 9.22–59.23 | 77 | 49.07 | 10.05 | 8.40–68.67 | −6.75*** | 72 | .10 |
| PCS at T2 | 66 | 41.04*** | 9.89 | 20.65–56.15 | 73 | 46.66** | 11.18 | 15.35–66.59 | −3.45*** | 60 | .21 |
| PCS at T3 | 65 | 42.74*** | 10.44 | 19.98–57.65 | 70 | 46.23** | 11.40 | 11.65–65.88 | −1.40 | 57 | .15 |
| MCS at T1 | 85 | 50.27 | 9.94 | 28.92–72.57 | 77 | 47.69† | 10.91 | 10.00–66.17 | 2.63** | 72 | .33** |
| MCS at T2 | 66 | 50.48 | 9.54 | 23.23–65.78 | 73 | 49.15 | 9.57 | 16.64–63.56 | 0.01 | 60 | .30* |
| MCS at T3 | 65 | 49.99 | 10.15 | 24.60–65.83 | 70 | 49.41 | 10.18 | 15.32–62.49 | −0.09 | 57 | .29* |
p <.10
p < .05
p < .01
p < .001
Note. PCS = Physical Health Component Scale of the MOS SF-12; MCS = Mental Health Component Scale of the MOS SF-12; T1 = 2 months post-diagnosis; T2 = 6 months post-diagnosis; T3= 12 months post-diagnosis; markings following mean scores indicate mean values differ from the US population normed mean of 50 per one-sample t-test.
Also shown in Table 2, data were missing at each time point between 8 to 29 percent for patients and caregivers on study variables. Correlates of missingness were investigated (Enders, 2010): missingness on study variables was unrelated to any demographic variable (ps> .16), with the exception that white patients and caregivers were more likely to have physical and mental health data at T2 and T3 (.04 <ps< .08). Therefore, ethnicity was included as an auxiliary variable in the models to reduce bias in the estimates produced by the Full Information Maximum Likelihood (FIML) estimation in MPlus (Enders, 2006; Schafer & Graham, 2002).
The specified model combining the four LGMs for patient and caregiver physical and mental health with APIM was first tested for model fit. Small out-of-bounds negative residual variances and residual covariances were set to 0. The resulting model fit the data: χ2(54)= 59.44, p= .28, CFI= .99, SRMR= .08. Model identification and significant paths are shown in Figure 1. Means and variances of latent variables, as well as path estimates, are reported in Table 3.
Table 3.
Latent Growth and Actor-Partner Interdependence Model Results for Patient and Caregiver Physical and Mental Health
| M | [95% CI] | p | s2 | [95% CI] | p | |
|---|---|---|---|---|---|---|
| Patient PCS Initial | −11.61 | [−13.88, −9.33] | <.001 | 59.80 | [21.47, 98.14] | .002 |
| Patient PCS Change | 2.11 | [0.90, 3.33] | .001 | 12.31 | [2.50, 22.11] | .014 |
| Caregiver PCS Initial | −1.53 | [−3.72, 0.67] | .174 | 97.76 | [66.32, 129.21] | <.001 |
| Caregiver PCS Change | −1.45 | [−2.45, −0.45] | .004 | 16.71 | [10.36, 23.05] | <.001 |
| Patient MCS Initial | 0.98 | [−1.11, 3.08] | .358 | 91.02 | [62.82, 119.21] | <.001 |
| Patient MCS Change | −0.41 | [−1.66, 0.84] | .520 | 25.71 | [16.21, 35.22] | <.001 |
| Caregiver MCS Initial | −2.00 | [−4.38, 0.37] | .098 | 85.25 | [41.77, 128.73] | <.001 |
| Caregiver MCS Change | 0.41 | [−0.88, 1.70] | .533 | 21.47 | [8.19, 34.75] | .002 |
| Unstandardized
|
Standardized
|
|||
|---|---|---|---|---|
| B | [95% CI] | β | p | |
| Physical Health Patient Actor Effects | ||||
| Pt Age→ Pt PCS Initial | 0.08 | [−0.10, 0.27] | .13 | .383 |
| Pt Age→ Pt PCS Change | −0.18 | [−0.28, −0.07] | −.52 | .001 |
| Pt PCS Initial ↔ Pt PCS Change | −2.14 | [−18.58, 14.31] | −.08 | .799 |
| Physical Health Caregiver Actor Effects | ||||
| Cg Age → Cg PCS Initial | −0.19 | [−0.35, −0.03] | −.24 | .024 |
| Cg Age → Cg PCS Change | 0.03 | [−0.05, 0.11] | .10 | .454 |
| Cg PCS Initial ↔ Cg PCS Change | −6.24 | [−16.78, 4.30] | −.15 | .246 |
| Physical Health Patient and Caregiver Partner Effects | ||||
| Pt PCS Initial ↔ Cg PCS Initial | 3.54 | [−20.49, 27.58] | .05 | .773 |
| Pt PCS Initial ↔ Cg PCS Change | 12.80 | [0.99, 24.62] | .41 | .034 |
| Cg PCS Initial ↔ Pt PCS Change | 5.54 | [−7.00, 18.09] | .16 | .387 |
| Pt PCS Change ↔ Cg PCS Change | −3.92 | [−9.72, 1.88] | −.27 | .185 |
| Mental Health Patient Actor Effects | ||||
| Pt Age → Pt MCS Initial | 0.08 | [−0.09, 0.24] | .10 | .371 |
| Pt Age → Pt MCS Change | 0.03 | [−0.07, 0.13] | .07 | .568 |
| Pt MCS Initial ↔ Pt MCS Change | −29.01 | [−42.29, −15.74] | −.60 | <.001 |
| Mental Health Caregiver Actor Effects | ||||
| Cg Age → Cg MCS Initial | 0.18 | [0.01, 0.35] | .25 | .034 |
| Cg Age → Cg MCS Change | −0.02 | [−0.12, 0.08] | −.07 | .648 |
| Cg MCS Initial ↔ Cg MCS Change | −13.66 | [−33.94, 6.61] | −.32 | .187 |
| Mental Health Patient and Caregiver Partner Effects | ||||
| Pt MCS Initial ↔ Cg MCS Initial | 30.81 | [7.24, 54.37] | .35 | .010 |
| Pt MCS Initial ↔ Cg MCS Change | −2.74 | [−14.59, 9.11] | −.06 | .651 |
| Cg MCS Initial ↔ Pt MCS Change | −2.71 | [−17.56, 12.15] | −.09 | .721 |
| Pt MCS Change Cg MCS Change | 4.52 | [−3.63, 12.68] | .19 | .277 |
| Physical and Mental Health Patient Actor Effects | ||||
| Pt PCS Initial ↔ Pt MCS Initial | 7.24 | [−14.85, 29.33] | .10 | .521 |
| Pt PCS Initial ↔ Pt MCS Change | 10.41 | [−2.80, 23.62] | .27 | .122 |
| Pt MCS Initial ↔ Pt PCS Change | 12.77 | [0.95, 24.59] | .38 | .034 |
| Pt PCS Change ↔ Pt MCS Change | −10.39 | [−17.35, -3.43] | −.58 | .003 |
| Physical and Mental Health Caregiver Actor Effects | ||||
| Cg PCS Initial ↔ Cg MCS Initial | −11.10 | [−35.70, 13.50] | −.12 | .377 |
| Cg PCS Initial ↔ Cg MCS Change | 13.97 | [0.29, 27.65] | .31 | .045 |
| Cg MCS Initial ↔ Cg PCS Change | 13.56 | [1.56, 25.55] | .36 | .027 |
| Cg PCS Change ↔ Cg MCS Change | −8.89 | [−15.50, −2.28] | −.47 | .008 |
| Physical and Mental Health Patient and Caregiver Partner Effects | ||||
| Pt PCS Initial ↔ Cg MCS Initial | 29.41 | [1.78, 57.03] | .41 | .037 |
| Pt PCS Initial ↔ Cg MCS Change | −13.41 | [−28.85, 2.04] | −.37 | .089 |
| Cg PCS Initial ↔ Pt MCS Change | −10.48 | [−23.42, 2.46] | −.21 | .112 |
| Pt MCS Initial ↔ Cg PCS Initial | 16.51 | [−4.78, 37.79] | .18 | .128 |
| Pt MCS Initial ↔ Cg PCS Change | 6.12 | [−3.25, 15.49] | .16 | .200 |
| Cg MCS Initial ↔ Pt PCS Change | −11.91 | [−27.04, 3.22] | −.37 | .123 |
| Pt PCS Change ↔ Cg MCS Change | 1.66 | [−6.60, 9.91] | .10 | .694 |
| Cg PCS Change ↔ Pt MCS Change | 1.72 | [−4.11, 7.55] | .08 | .563 |
Note. Unstandardized estimates reported for latent growth parameter means and variances; PCS= Physical Health Component Scale of the MOS SF-12; MCS= Mental Health Component Scale of the MOS SF-12; indicator values were centered at 50 (i.e., normalized mean for the US population) prior to analyses; p-values for unstandardized estimates; significant paths (p< .05) are bolded and shown in bold in Figure 1; Pt= Patients; Cg= Caregivers; age variables were centered at the patient and caregiver mean values, respectively, prior to analyses.
Physical Health Trajectories at Individual and Dyadic Levels
Patient actor effects
Patients’ average initial level of physical health was significantly lower than the US population norm of 50. On average, patients reported significant improvement in their physical health over the year following their diagnosis, by approximately four points. Patients’ age was unrelated to their initial level of physical health, but was significantly negatively related to their change in physical health: older patients reported less improvement in their physical health over the year following their diagnosis. Patients’ initial level of physical health was unrelated to their change in physical health over the following year.
Caregiver actor effects
Caregivers’ average initial level of physical health did not significantly differ from the US population norm of 50. On average, caregivers reported a significant decline in their physical health over the year following their patients’ diagnosis by approximately three points. Caregivers’ age was significantly negatively related to their initial level of physical health: older caregivers reported lower physical health around the time of their patients’ diagnosis. Caregivers’ age and initial level of physical health were unrelated to their change in physical health over the following year.
Patient and caregiver partner effects
Patients’ initial level of physical health was significantly positively related to their caregivers’ change in physical health: patients’ lower levels of physical health around the time of diagnosis were associated with their caregivers’ greater decline in physical health over the following year. No other partner effects of physical health were significant.
Mental Health Trajectories at Individual and Dyadic Levels
Patient actor effects
Patients’ average initial level of mental health did not significantly differ from the US population norm of 50. On average, patients reported no significant change in their mental health over the year following their diagnosis. Patients’ age was unrelated to both their initial level and change in mental health. However, patients’ initial level of mental health was significantly negatively related to their change in mental health: patients who reported low mental health around the time of diagnosis showed greater improvement in mental health over the following year.
Caregiver actor effects
Caregivers’ average initial level of mental health was marginally lower than the US population norm of 50. On average, caregivers reported no significant change in their mental health over the year following their patients’ diagnosis. Caregivers’ age was significantly positively related to their initial level of mental health: older caregivers reported higher mental health around the time of their patients’ diagnosis. Caregivers’ age and initial level of mental health were unrelated to their change in mental health over the following year.
Patient and caregiver partner effects
Patients’ and their caregivers’ initial levels of mental health were significantly positively related: patients’ lower levels of mental health around the time of diagnosis were concurrently associated with their caregivers’ lower levels of mental health. No other partner effects of mental health were significant.
Relations Between Physical and Mental Health Trajectories at Individual and Dyadic Levels Patient actor effects
Patients’ initial level of physical health was unrelated to both their initial level of mental health and their change in mental health over the following year. However, patients’ initial level of mental health was significantly positively related to their change in physical health: patients reporting low initial mental health around the time of diagnosis showed less improvement in physical health over the following year. Patients’ changes in physical and mental health were significantly negatively related: patients who showed less improvement in their physical health conversely showed greater improvement in their mental health over the year following diagnosis.
Caregiver actor effects
Caregivers’ initial level of physical health was unrelated to their initial level of mental health. However, caregivers’ initial level of physical health was significantly positively related to their change in mental health: caregivers reporting low physical health around the time of their patients’ diagnosis showed greater decline in mental health over the following year. Similarly, caregivers’ initial level of mental health was significantly positively related to their change in physical health: caregivers reporting low mental health around the time of their patients’ diagnosis showed greater decline in physical health over the following year. Caregivers’ changes in physical and mental health were significantly negatively related: caregivers who showed greater decline in their physical health showed greater improvement in their mental health over the year following diagnosis.
Patient and caregiver partner effects
Patients’ initial level of physical health was significantly positively related to their caregivers’ initial level of mental health: patients’ lower levels of physical health around the time of diagnosis were concurrently associated with their caregivers’ lower levels of mental health. No other partner effects of physical with mental health were significant.
Discussion
This study examined levels and changes of physical and mental health among cancer patients and their informal caregivers across the year following diagnosis. Although initial levels and changes in physical and mental health were related for both patients and caregivers at an individual level, results provided limited evidence of dyadic interdependence between patients’ and their caregivers’ health trajectories.
Physical Health Trajectories
Relative to the physical health of the general US population, patients reported significantly poorer physical health around the time of their diagnosis, whereas caregivers did not differ. However, patients reported significant improvement in their physical health across the year following diagnosis (as expected with cancer treatment), while their caregivers reported significant deterioration in their physical health. Results showed that caregivers’ physical health decline was strongly related to their patients’ poorer physical health at diagnosis, supporting interdependence between patients’ and their caregivers’ physical health. This association may be due in part to caregiving burden rising proportionally with patients’ physical limitations (Grunfeld et al., 2004), thus increasing caregivers’ risk for their own physical health decline (Kim et al., 2015; Pinquart & Sörensen, 2007). Mechanisms linking caregivers’ physical health with their patients’ physical health warrant further study. With caregivers at increased risk for premature disease development relative to non-caregivers (Ji et al., 2012; Rohleder et al., 2009; Vitaliano et al., 2002), targeted preventive interventions to curb caregivers’ physical health decline will be critical to reducing this health disparity, with particular attention paid to caregivers whose patients’ physical health is poor at the time of diagnosis.
Mental Health Trajectories
Relative to the mental health of the general US population, neither patients nor caregivers differed at the time of the patient’s diagnosis. In addition, no significant change in mental health was seen among patients or caregivers over the following year, on average. For patients, however, those reporting low mental health at diagnosis showed a rebound in their mental health over the following year. While earlier work showed that patients’ high distress at diagnosis predicted continued elevations in their distress six months later (Nordin et al., 2001), the current study suggests that these elevations in distress may tend to alleviate over a longer course of time. This mental health rebound was not seen among caregivers, however. Findings that caregivers did not report significant mental health impairment at diagnosis or show significant change in mental health over the following year concur with prior studies: the average caregiver tends to adapt effectively to the role, yet those caregivers who do experience mental health impairment tend not to recover over the following few years (Kim, Shaffer, et al., 2014; Lambert et al., 2012; Palos et al., 2011).
Interdependence among patients’ and caregivers’ mental health was only documented at diagnosis, with a moderate, positive correlation concurring with previous findings (Hodges et al., 2005). However, the present study did not show a significant correlation between patients’ and caregivers’ mental health changes across the following year. These results contrast with those from previous studies reporting prospective relations between breast cancer patients’ and their caregivers’ depression (Segrin et al., 2005) and anxiety (Segrin et al., 2007). Notably, Segrin and colleagues (2005, 2007) reported on dyads from a psychosocial intervention trial, with primary cross-over between patients’ and caregivers’ mental health occurring from the end of the intervention to a four-week follow-up. In contrast, the current study reports on naturalistic, observational data provided by cancer patients and their caregivers. Reconciling these findings suggests the possibility that dyadic psychosocial interventions may strengthen the adaptive emotional system between patients and caregivers. An enhanced dyadic coping system may account in part for patients’ improved health outcomes when their caregivers are included in psychosocial interventions compared to patient-only interventions (Martire, 2005; Martire, Lustig, Schulz, Miller, & Helgeson, 2004).
Relations Between Mental and Physical Health Trajectories
For both patients and caregivers, poorer mental health at the time of diagnosis related to their own more pronounced physical health decline over the following year. These findings are consistent with prior results for both patients (Chida et al., 2008; Hoppe et al., 2013) and caregivers (Pinquart & Duberstein, 2010; Satin et al., 2009; Vitaliano et al., 2002). Also for both patients and caregivers, change in physical health was inversely associated with change in mental health. These inverse associations are likely due to the findings that, among those with low mental health at diagnosis, their mental health tended to rebound whereas their physical health tended to worsen.
Limited evidence supported interdependence between patients’ and caregivers’ health trajectories. It was found, however, that patients’ physical health at the time of diagnosis was positively associated with caregivers’ concurrent level of mental health as well as their change in physical health over time. Overall, results suggest the relevance of psychosocial interventions targeted to distressed patients and caregivers during the year following diagnosis to improve patients’ clinical outcomes (Pirl, 2004) and to mitigate caregivers’ physical health decline (Northouse, Katapodi, Song, Zhang, & Mood, 2010).
Limitations and Future Directions
In the current study, sample size was small and effect sizes were modest. Those participants who were unable to be included in the current study differed marginally from the included sample in terms of gender, mental health, and age, limiting the generalizability of findings. Another limitation is that all variables from the current study were self-reported and therefore may be affected by social desirability concerns. Inclusion of objective markers of physical health (e.g., salivary cortisol, pro-inflammatory cytokines) and psychological health (e.g., clinical assessment, medical record review for mental health diagnoses) will be important next steps to understanding patients’ and caregivers’ adjustment across the cancer trajectory. Ecological measures of dyadic coping (e.g., linguistic analysis, behavioral paradigm coding) paired with these objective physiological and psychological health outcomes may provide even more nuanced understanding of the impact of the dyadic emotional system on patients’ and caregivers’ adjustment to chronic illness.
Future research into dyadic adjustment between cancer patients and their caregivers across the course of cancer may also benefit from examining factors that may moderate associations between patient and caregiver health trajectories. Berg and Upchurch (2007) discuss both distal (e.g., sociocultural) and proximal (e.g., relationship) context factors that relate to the strength and success of dyadic adjustment to chronic illness. The sociocultural diversity in the present study represents a study strength in terms of generalizing findings for both white and African American dyads, dyads of varying relationships (e.g., spousal, parent-child), and to persons from diverse socioeconomic backgrounds. However, this diversity may also obscure patterns of dyadic adjustment occurring within specific subgroups of patients and caregivers. For example, dyadic coping is likely strongest between spousal couples due to the uniqueness of the marital bond and shared living environment—follow-up analysis of the current data supports dyadic interdependence may be stronger among spousal couples compared to non-spousal dyads (data not shown). Further study of relationship type and other moderators of dyadic interdependence is therefore warranted.
Conclusion
Despite limitations, this study provides novel evidence regarding important risk factors relevant to cancer patients’ and their caregivers’ physical and mental health. Patients’ and caregivers’ own physical and mental health assessments at diagnosis were most relevant to predicting their own changes in health across the year following the patients’ cancer diagnosis, yet future study is warranted to examine moderating factors that may enhance interdependence among patients’ and caregivers’ health trajectories. For both patients and caregivers, poor mental health at diagnosis posed significant risk to their physical health: distressed patients showed stagnated physical health recovery, and distressed caregivers showed accelerated physical health decline. Results suggest the importance of targeting interventions to both patients and caregivers reporting poor mental health at diagnosis to mitigating their long-term physical morbidity.
Acknowledgments
This work was supported by the American Cancer Society National Home Office, intramural research, and the National Cancer Institute under Grant 1 F31 CA189431-01A1.
Footnotes
The authors declare that they have no conflict of interest.
References
- Beach SR, Schulz R, Williamson GM, Miller LS, Weiner MF, Lance CE. Risk factors for potentially harmful informal caregiver behavior. Journal of the American Geriatrics Society. 2005;53(2):255–261. doi: 10.1111/j.1532-5415.2005.53111.x. [DOI] [PubMed] [Google Scholar]
- Berg CA, Upchurch R. A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychological Bulletin. 2007;133(6):920. doi: 10.1037/0033-2909.133.6.920. [DOI] [PubMed] [Google Scholar]
- Bevans M, Sternberg EM. Caregiving burden, stress, and health effects among family caregivers of adult cancer patients. Journal of the American Medical Association. 2012;307(4):398–403. doi: 10.1001/jama.2012.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodenmann G. Dyadic coping and its significance for marital functioning. In: Revenson T, Kayser K, Bodenmann G, editors. Couples Coping with Stress: Emerging Perspectives on Dyadic Coping. Washington, D.C., US: American Psychological Association; 2005. pp. 33–49. [Google Scholar]
- Bollen KA, Curran PJ. Latent Curve Models: A Structural Equation Approach. New Jersey, US: John Wiley & Sons; 2006. Wiley Series on Probability and Mathematical Statistics. [Google Scholar]
- Bower JE, Lamkin DM. Inflammation and cancer-related fatigue: Mechanisms, contributing factors, and treatment implications. Brain, Behavior, and Immunity. 2013;30:S48–S57. doi: 10.1016/j.bbi.2012.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun M, Mikulincer M, Rydall A, Walsh A, Rodin G. Hidden morbidity in cancer: Spouse caregivers. Journal of Clinical Oncology. 2007;25(30):4829–4834. doi: 10.1200/JCO.2006.10.0909. [DOI] [PubMed] [Google Scholar]
- Brown SL, Smith DM, Schulz R, Kabeto MU, Ubel PA, Poulin M, … Langa KM. Caregiving behavior is associated with decreased mortality risk. Psychological Science. 2009;20(4):488–494. doi: 10.1111/j.1467-9280.2009.02323.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cella D, Davis K, Breitbart W, Curt G. Cancer-related fatigue: prevalence of proposed diagnostic criteria in a United States sample of cancer survivors. Journal of Clinical Oncology. 2001;19(14):3385–3391. doi: 10.1200/JCO.2001.19.14.3385. [DOI] [PubMed] [Google Scholar]
- Chida Y, Hamer M, Wardle J, Steptoe A. Do stress-related psychosocial factors contribute to cancer incidence and survival? Nature Clinical Practice Oncology. 2008;5(8):466–475. doi: 10.1038/ncponc1134. [DOI] [PubMed] [Google Scholar]
- Cook WL, Kenny DA. The Actor–Partner Interdependence Model: A model of bidirectional effects in developmental studies. International Journal of Behavioral Development. 2005;29(2):101–109. [Google Scholar]
- Enders C. A primer on the use of modern missing-data methods in psychosomatic medicine research. Psychosomatic medicine. 2006;68(3):427–436. doi: 10.1097/01.psy.0000221275.75056.d8. [DOI] [PubMed] [Google Scholar]
- Enders C. Applied missing data analysis. Guilford Press; 2010. [Google Scholar]
- Esther Kim JE, Dodd MJ, Aouizerat BE, Jahan T, Miaskowski C. A review of the prevalence and impact of multiple symptoms in oncology patients. Journal of Pain and Symptom Management. 2009;37(4):715–736. doi: 10.1016/j.jpainsymman.2008.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goudas LC, Bloch R, Gialeli-Goudas M, Lau J, Carr DB. The epidemiology of cancer pain. Cancer Investigation. 2005;23(2):182–190. [PubMed] [Google Scholar]
- Grunfeld E, Coyle D, Whelan T, Clinch J, Reyno L, Earle CC, … Janz T. Family caregiver burden: Results of a longitudinal study of breast cancer patients and their principal caregivers. Canadian Medical Association Journal. 2004;170(12):1795–1801. doi: 10.1503/cmaj.1031205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagedoorn M, Sanderman R, Bolks HN, Tuinstra J, Coyne JC. Distress in couples coping with cancer: a meta-analysis and critical review of role and gender effects. Psychological Bulletin. 2008;134(1):1. doi: 10.1037/0033-2909.134.1.1. [DOI] [PubMed] [Google Scholar]
- Hodges L, Humphris G, MacFarlane G. A meta-analytic investigation of the relationship between the psychological distress of cancer patients and their carers. Social Science & Medicine. 2005;60(1):1–12. doi: 10.1016/j.socscimed.2004.04.018. [DOI] [PubMed] [Google Scholar]
- Hoppe S, Rainfray M, Fonck M, Hoppenreys L, Blanc JF, Ceccaldi J, … Cany L. Functional decline in older patients with cancer receiving first-line chemotherapy. Journal of Clinical Oncology. 2013;31(31):3877–3882. doi: 10.1200/JCO.2012.47.7430. [DOI] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6(1):1–55. [Google Scholar]
- Janda M, Steginga S, Langbecker DH, Dunn J, Walker D, Eakin EG. Quality of life among patients with a brain tumor and their carers. Journal of Psychosomatic Research. 2007;63(6):617–623. doi: 10.1016/j.jpsychores.2007.06.018. [DOI] [PubMed] [Google Scholar]
- Ji J, Zöller B, Sundquist K, Sundquist J. Increased risks of coronary heart disease and stroke among spousal caregivers of cancer patients. Circulation. 2012;125(14):1742–1747. doi: 10.1161/CIRCULATIONAHA.111.057018. [DOI] [PubMed] [Google Scholar]
- Kashy DA, Kenny DA. The analysis of data from dyads and groups. Handbook of Research Methods in Social and Personality Psychology. 2000:451–477. [Google Scholar]
- Kenny DA, Cook W. Partner effects in relationship research: Conceptual issues, analytic difficulties, and illustrations. Personal Relationships. 1999;6(4):433–448. [Google Scholar]
- Kenny DA, Kashy DA, Cook WL. Dyadic Data Analysis. The Guilford Press; 2006. [Google Scholar]
- Kim Y, Carver CS, Shaffer KM, Gansler T, Cannady RS. Cancer caregiving predicts physical impairments: Roles of earlier caregiving stress and being a spousal caregiver. Cancer. 2015;121(2):302–310. doi: 10.1002/cncr.29040. [DOI] [PubMed] [Google Scholar]
- Kim Y, Duberstein PR, Sörensen S, Larson MR. Levels of depressive symptoms in spouses of people with lung cancer: Effects of personality, social support, and caregiving burden. Psychosomatics. 2005;46(2):123–130. doi: 10.1176/appi.psy.46.2.123. [DOI] [PubMed] [Google Scholar]
- Kim Y, Kashy DA, Wellisch DK, Spillers RL, Kaw CK, Smith TG. Quality of life of couples dealing with cancer: Dyadic and individual adjustment among breast and prostate cancer survivors and their spousal caregivers. Annals of Behavioral Medicine. 2008;35(2):230–238. doi: 10.1007/s12160-008-9026-y. [DOI] [PubMed] [Google Scholar]
- Kim Y, Spillers RL. Quality of life of family caregivers at 2 years after a relative's cancer diagnosis. Psycho-Oncology. 2010;19(4):431–440. doi: 10.1002/pon.1576. [DOI] [PubMed] [Google Scholar]
- Kim Y, Shaffer KM, Carver CS, Cannady RS. Quality of life of family caregivers 8 years after a relative's cancer diagnosis: follow-up of the National Quality of Life Survey for Caregivers. Psycho-Oncology. 2015 doi: 10.1002/pon.3843. [DOI] [PubMed] [Google Scholar]
- Kim Y, van Ryn M, Jensen RE, Griffin JM, Potosky A, Rowland J. Effects of gender and depressive symptoms on quality of life among colorectal and lung cancer patients and their family caregivers. Psycho-Oncology. 2014;24(1):95–105. doi: 10.1002/pon.3580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Y, Shaffer KM, Carver CS, Cannady RS. Prevalence and predictors of depressive symptoms among cancer caregivers 5 years after the relative’s cancer diagnosis. Journal of Consulting and Clinical Psychology. 2014;82(1):1–8. doi: 10.1037/a0035116. [DOI] [PubMed] [Google Scholar]
- Kim Y, Wellisch DK, Spillers RL. Effects of psychological distress on quality of life of adult daughters and their mothers with cancer. Psycho-Oncology. 2008;17(11):1129–1136. doi: 10.1002/pon.1328. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and Practice of Structural Equation Modeling. Guilford press; 2011. [Google Scholar]
- Lambert SD, Jones BL, Girgis A, Lecathelinais C. Distressed partners and caregivers do not recover easily: Adjustment trajectories among partners and caregivers of cancer survivors. Annals of Behavioral Medicine. 2012;44(2):225–235. doi: 10.1007/s12160-012-9385-2. [DOI] [PubMed] [Google Scholar]
- Li Q, Loke AY. A spectrum of hidden morbidities among spousal caregivers for patients with cancer, and differences between the genders: A review of the literature. European Journal of Oncology Nursing. 2013;17(5):578–587. doi: 10.1016/j.ejon.2013.01.007. [DOI] [PubMed] [Google Scholar]
- Martire LM. The “relative" efficacy of involving family in psychosocial interventions for chronic illness: Are there added benefits to patients and family members? Families, Systems, & Health. 2005;23(3):312–328. [Google Scholar]
- Martire LM, Lustig AP, Schulz R, Miller GE, Helgeson VS. Is it beneficial to involve a family member? A meta-analysis of psychosocial interventions for chronic illness. Health Psychology. 2004;23(6):599–611. doi: 10.1037/0278-6133.23.6.599. [DOI] [PubMed] [Google Scholar]
- Massie MJ. Prevalence of depression in patients with cancer. JNCI Monographs. 2004;2004(32):57–71. doi: 10.1093/jncimonographs/lgh014. [DOI] [PubMed] [Google Scholar]
- Meuser T, Pietruck C, Radbruch L, Stute P, Lehmann KA, Grond S. Symptoms during cancer pain treatment following WHO-guidelines: A longitudinal follow-up study of symptom prevalence, severity and etiology. Pain. 2001;93(3):247–257. doi: 10.1016/S0304-3959(01)00324-4. [DOI] [PubMed] [Google Scholar]
- Milbury K, Badr H, Fossella F, Pisters KM, Carmack CL. Longitudinal associations between caregiver burden and patient and spouse distress in couples coping with lung cancer. Supportive Care in Cancer. 2013;21(9):2371–2379. doi: 10.1007/s00520-013-1795-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell AJ, Chan M, Bhatti H, Halton M, Grassi L, Johansen C, Meader N. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: A meta-analysis of 94 interview-based studies. The Lancet Oncology. 2011;12(2):160–174. doi: 10.1016/S1470-2045(11)70002-X. [DOI] [PubMed] [Google Scholar]
- Moser MT, Künzler A, Nussbeck F, Bargetzi M, Znoj HJ. Higher emotional distress in female partners of cancer patients: Prevalence and patient–partner interdependencies in a 3-year cohort. PsychoOncology. 2013;22(12):2693–2701. doi: 10.1002/pon.3331. [DOI] [PubMed] [Google Scholar]
- Muthén BO, Curran PJ. General longitudinal modeling of individual differences in experimental designs: A latent variable framework for analysis and power estimation. Psychological Methods. 1997;2(4):371. [Google Scholar]
- Muthén L, Muthén B. MPlus User's Guide. Los Angeles, CA: Muthén & Muthén; 2012. [Google Scholar]
- National Association for Caregiving. Caregiving in the US: A focused look at those caring for someone age 50 or older. Bethesda, MD: National Alliance for Caregiving; 2009. [Google Scholar]
- National Comprehensive Cancer Network. Clinical Practice Guidelines in Oncology: Adult Cancer Pain. Fort Washington, PA: National Comprehensive Cancer Network; 2012. [Google Scholar]
- Nijboer C, Tempelaar R, Triemstra M, Sanderman R, van den Bos GA. Dynamics in cancer caregiver's health over time: Gender-specific patterns and determinants. Psychology and Health. 2001;16(4):471–488. [Google Scholar]
- Nordin K, Berglund G, Glimelius B, Sjöden PO. Predicting anxiety and depression among cancer patients: A clinical model. European Journal of Cancer. 2001;37(3):376–384. doi: 10.1016/s0959-8049(00)00398-1. [DOI] [PubMed] [Google Scholar]
- Northouse L, Williams A, Given B, McCorkle R. Psychosocial care for family caregivers of patients with cancer. Journal of Clinical Oncology. 2012;30(11):1227–1234. doi: 10.1200/JCO.2011.39.5798. [DOI] [PubMed] [Google Scholar]
- Northouse LL, Katapodi MC, Song L, Zhang L, Mood DW. Interventions with family caregivers of cancer patients: Meta-analysis of randomized trials. CA: A Cancer Journal for Clinicians. 2010;60(5):317–339. doi: 10.3322/caac.20081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachman DR, Barton DL, Swetz KM, Loprinzi CL. Troublesome symptoms in cancer survivors: Fatigue, insomnia, neuropathy, and pain. Journal of Clinical Oncology. 2012;30(30):3687–3696. doi: 10.1200/JCO.2012.41.7238. [DOI] [PubMed] [Google Scholar]
- Palos GR, Mendoza TR, Liao KP, Anderson KO, Garcia-Gonzalez A, Hahn K, … Lynch GR. Caregiver symptom burden: The risk of caring for an underserved patient with advanced cancer. Cancer. 2011;117(5):1070–1079. doi: 10.1002/cncr.25695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson RE, Saquib N, Natarajan L, Rock CL, Parker BA, Thomson CA, Pierce JP. Improvement in self-reported physical health predicts longer survival among women with a history of breast cancer. Breast Cancer Research and Treatment. 2011;127(2):541–547. doi: 10.1007/s10549-010-1236-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart M, Duberstein P. Depression and cancer mortality: A meta-analysis. Psychological Medicine. 2010;40(11):1797. doi: 10.1017/S0033291709992285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart M, Sörensen S. Correlates of physical health of informal caregivers: A meta- analysis. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2007;62(2):P126–P137. doi: 10.1093/geronb/62.2.p126. [DOI] [PubMed] [Google Scholar]
- Pirl WF. Evidence report on the occurrence, assessment, and treatment of depression in cancer patients. JNCI Monographs. 2004;2004(32):32–39. doi: 10.1093/jncimonographs/lgh026. [DOI] [PubMed] [Google Scholar]
- Pitceathly C, Maguire P. The psychological impact of cancer on patients’ partners and other key relatives: A review. European Journal of Cancer. 2003;39(11):1517–1524. doi: 10.1016/s0959-8049(03)00309-5. [DOI] [PubMed] [Google Scholar]
- Rohleder N, Marin TJ, Ma R, Miller GE. Biologic cost of caring for a cancer patient: Dysregulation of pro-and anti-inflammatory signaling pathways. Journal of Clinical Oncology. 2009;27(18):2909–2915. doi: 10.1200/JCO.2008.18.7435. [DOI] [PubMed] [Google Scholar]
- Satin JR, Linden W, Phillips MJ. Depression as a predictor of disease progression and mortality in cancer patients. Cancer. 2009;115(22):5349–5361. doi: 10.1002/cncr.24561. [DOI] [PubMed] [Google Scholar]
- Schafer J, Graham J. Missing data: our view of the state of the art. Psychological Methods. 2002;7(2):147. [PubMed] [Google Scholar]
- Schulz R, Beach SR. Caregiving as a risk factor for mortality. Journal of the American Medical Association. 1999;282(23):2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- Segrin C, Badger T, Dorros SM, Meek P, Lopez AM. Interdependent anxiety and psychological distress in women with breast cancer and their partners. PsychoOncology. 2007;16(7):634–643. doi: 10.1002/pon.1111. [DOI] [PubMed] [Google Scholar]
- Segrin C, Badger TA. Psychological and physical distress are interdependent in breast cancer survivors and their partners. Psychology, Health & Medicine. 2014;19(6):716–723. doi: 10.1080/13548506.2013.871304. [DOI] [PubMed] [Google Scholar]
- Segrin C, Badger TA, Meek P, Lopez AM, Bonham E, Sieger A. Dyadic interdependence on affect and quality-of-life trajectories among women with breast cancer and their partners. Journal of Social and Personal Relationships. 2005;22(5):673–689. [Google Scholar]
- Ulrich B. Caring for the caregivers. Nephrology Nursing Journal. 2006;33(2):129. [PubMed] [Google Scholar]
- van't Spijker A, Trijsburg RW, Duivenvoorden HJ. Psychological sequelae of cancer diagnosis: a meta-analytical review of 58 studies after 1980. Psychosomatic Medicine. 1997;59(3):280–293. doi: 10.1097/00006842-199705000-00011. [DOI] [PubMed] [Google Scholar]
- Vitaliano PP, Scanlan JM, Zhang J, Savage MV, Hirsch IB, Siegler IC. A path model of chronic stress, the metabolic syndrome, and coronary heart disease. Psychosomatic Medicine. 2002;64(3):418–435. doi: 10.1097/00006842-200205000-00006. [DOI] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Medical Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Bayliss MS, McHorney CA, Rogers WH, Raczek A. Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: Summary of results from the Medical Outcomes Study. Medical Care. 1995;33(4 Suppl):AS264–AS279. [PubMed] [Google Scholar]
- Wong CK, Law WL, Wan YF, Poon JTC, Lam CLK. Health-related quality of life and risk of colorectal cancer recurrence and all-cause death among advanced stages of colorectal cancer 1-year after diagnosis. BMC Cancer. 2014;14(1):337. doi: 10.1186/1471-2407-14-337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong CK, Lam CLK, Poon JTC, Kwong DLW. Clinical correlates of health preference and generic health-related quality of life in patients with colorectal neoplasms. PLOS One. 2013;8(3):e58341. doi: 10.1371/journal.pone.0058341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willett JB, Sayer AG. Using covariance structure analysis to detect correlates and predictors of individual change over time. Psychological Bulletin. 1994;116:363–363. [Google Scholar]
- Yamagishi A, Morita T, Miyashita M, Kimura F. Symptom Prevalence and Longitudinal Follow-Up in Cancer Outpatients Receiving Chemotherapy. Journal of Pain and Symptom Management. 2009;37(5):823–830. doi: 10.1016/j.jpainsymman.2008.04.015. [DOI] [PubMed] [Google Scholar]