Abstract
Despite the high prevalence of HIV among men who have sex with men in South Africa, very little is known about their lived realities, including their social and sexual networks. Given the influence of social network structure on sexual risk behaviours, a better understanding of the social contexts of men who have sex with men is essential for informing the design of HIV programming and messaging. This study explored social network connectivity, an understudied network attribute, examining self-reported connectivity between friends, family and sex partners. Data were collected in Cape Town and Port Elizabeth, South Africa from 78 men who have sex with men who participated in in-depth interviews which included a social network mapping component. Five social network types emerged from the content analysis of these social network maps based on the level of connectivity between family, friends and sex partners, and ranged from disconnected to densely connected networks. The ways in which participants reported sexual risk-taking differed across the five network types revealing diversity in social network profiles. HIV programming and messaging for this population can greatly benefit from recognising the diversity in lived realities and social connections between men who have sex with men.
Keywords: Men who have sex with men, networks, HIV/AIDS, sexual risk, South Africa
Introduction
South Africa has the largest number of people living with HIV in the world, with an adult (15–49 years) population prevalence of 17.8% (Shisana 2012). After an early HIV outbreak among white gay-identified men in the 1980s, White men who have sex with men were thought to be disproportionately affected by the epidemic (Wilkinson and Engelbrecht 2009, Sher 1989). However, a second pattern of HIV transmission soon emerged revealing a larger, growing epidemic among Black heterosexual South Africans (Maartens et al. 1997, van Harmelen et al. 1997) which led to a re-characterisation of the epidemic as generalized, with heterosexual sex as the dominant transmission mode (South African National AIDS Council 2007). As a result, since then national HIV programmes have largely focused on heterosexual and mother-to-child transmission, to the exclusion of other high-risk groups (Rispel and Metcalf 2009). As the HIV landscape in South Africa matures, evidence continues to emerge suggesting a more diverse HIV epidemic, including concentrated epidemics among key populations including men who have sex with men. HIV prevalence estimates derived from observational studies enrolling urban men who have sex with men range between 10 and 50% (Sandfort et al. 2008, Burrell et al. 2010, Lane et al. 2011) and HIV prevalence among men who have sex with men has been estimated to be more than twice that of other reproductive age men (Beyrer et al. 2012, South African National AIDS Council 2011). These studies highlight the extent of the HIV epidemic among different sub-populations of men who have sex with men as well as variations in HIV-related risk among men who have sex with men sub-populations, particularly by race, locality and sexual identity (Sandfort et al. 2008, Burrell et al. 2010, Lane et al. 2011, Rispel et al. 2011). They have also helped underscore that Black township men who have sex with men, previously undocumented in the characterisation of the South African HIV epidemic, are a particularly vulnerable sub-population (Lane 2009).
Men who have sex with men in South Africa have often been considered a homogenous group confined to gay-identified and effeminate stereotypes (Reddy 2009). However research continues to suggest a socio-culturally complex population, comprised of men with variation in sexual identities, race, locality (Lane et al. 2008, Jewkes et al. 2006, Jobson et al. 2012) and sexual behaviours that drive HIV transmission (Lane et al. 2011, Lane 2009). Recognition and understanding of these different sociocultural and sexual identities is important as it creates differences in health needs and disparities in HIV risk profiles, and necessitates variation in programmatic approaches and health messaging. For instance, men who have sex with men residing in communities with higher levels of homophobia and HIV stigma, often more prevalent in township and rural areas, may be less likely to seek healthcare and would benefit from access to discreet, culturally appropriate messaging and healthcare facilities (Lane et al. 2008, Rebe KB 2013, Sandfort, Knox, et al. 2015). While some men who have sex with men identify as gay and only have sex with men, others may be straight- or non gay-identified and have sex with both men and women; each of these may have different HIV programmatic needs and could respond differently to heteronormative or overtly ‘gay’ public health campaigns (Masvawure et al. 2015, Sandfort, Lane, et al. 2015). Any effective response to the men who have sex with men HIV epidemic should understand the range of lived realities of these subgroups.
The composition and density of social networks held by men who have sex with men has been to shown to influence sexual risk-taking (Wright and Perry 2006). Men with a higher proportion of gay- or bisexual-identified male friends may have more opportunities for sexual partnering. Men reporting a higher overlap between their social and sexual networks have been shown to be at increased risk of HIV infection (Choi et al. 2007). However, increased network density, indicating higher familiarity between members, has been associated with a lower number of reported sex partners in the previous year (Smith et al. 2004), suggesting that denser networks may be subject to greater peer scrutiny thereby encouraging less risky sexual behaviour. The disclosure of same-sex behaviour and HIV sero-status is also influenced by social network composition. Men reporting emotionally supportive HIV-positive network members were more likely to have disclosed same-sex behaviour and HIV sero-status (Latkin et al. 2012). Failure to disclose HIV sero-status is a barrier to seeking healthcare and has been shown to be associated with negative mental health outcomes (Preston et al. 2007) and sexual risk-taking (Kalichman and Nachimson 1999, Olley, Seedat, and Stein 2004). Men reporting a higher proportion of their social network members being aware of their same-sex behaviour also report lower levels of sexual risk-taking, suggesting that increased social support may reduce sexual risk-taking (Finneran and Stephenson 2014).
Given the influence of social networks on sexual risk-taking and the limited social network research on South African men who have sex with men, we sought to further characterise the social networks of South African men who have sex with men by looking at the self-reported connectivity between friends, family and sex partners. A better understanding of the variation and context of these connections could provide insight for developing tailored prevention messaging for men who have sex with men.
Methods
Social network data were collected as part of a larger qualitative study which assessed health care access, uptake of and structural barriers to using prevention services, sexual behaviours and social networks among men who have sex with men in South Africa (Siegler, Sullivan, et al. 2014, Siegler, Voux, et al. 2014). The qualitative study took place over a 6-week period in 2012.
Study Population and Recruitment
Ethical clearance for the study was provided by boards at Emory University, the University of Cape Town and the Human Sciences Research Council (HSRC). Eligible participants were aged ≥ 18 years, assigned male sex at birth, reported sex with a man in the last 6 months and lived in Cape Town or Port Elizabeth, South Africa. Approximately one-third of participants were recruited using pre-existing contact lists of men who have sex with men, gathered by collaborating community-based organisations Desmond Tutu HIV Foundation in Cape Town and HSRC in Port Elizabeth, while the remaining two-thirds were recruited by further snowball sampling from this initial list of men. Participants were contacted by telephone and screened for eligibility. Men who expressed interest were scheduled for an in-person interview at one of several private locations most convenient to the participant. All participants provided informed consent and were remunerated with 80 Rand (10 USD) for their time and travel expenses.
The median age was 30 years (range: 19–67 years). Almost two-thirds (60%) identified as Black, 18% as Coloured (South African term indicating mixed ancestry) and 19% as White. Almost all participants identified as gay (95%), with 4 identifying as bisexual (5%). Nineteen participants (26%) reported living with HIV; self-reported HIV status was not confirmed by testing.
Study Procedures
Given the evidence regarding the influence of social networks on sexual risk-taking among men who have sex with men and the lack of data on the social networks of men in South Africa, we wanted to fill this gap by looking at the variation in the self-reported connectivity among individuals in men’s networks (i.e., family, friends and sex partners), in relation to sexual risk behaviours. To achieve this goal, we conducted activity-based interviews which included a social network activity supplemented with a narrative provided by men. Interviews lasted approximately 90 minutes, were audio recorded and translated into English where applicable. Seventy-nine interviews, 40 in Cape Town and 39 in Port Elizabeth, were conducted.
The social network activity focused on the past 6 months of the participant’s life. Men were asked to “name the first names or nicknames of people you have felt closest to in the past 6 months” and then to indicate which “categories each of those people fall in” (i.e., friend, family or sex partner). Next, men were asked to indicate “which of these people know each other”. If men reported network members knowing one another, a line was drawn between these members to indicate a connection. Reported connections were recorded by trained interviewers in a graphical data collection form (Figure 1). There was no limit set on the number of friends, family or sex partners, men were allowed to list. Interviewers also used a semi-structured interview guide that addressed domains of sexual identity, lesbian, gay, bisexual and transgender (LGBT) community involvement, sexual partnerships and sexual practices.
Figure 1. Example of the social network mapping activity assessing connectivity across network subgroups.
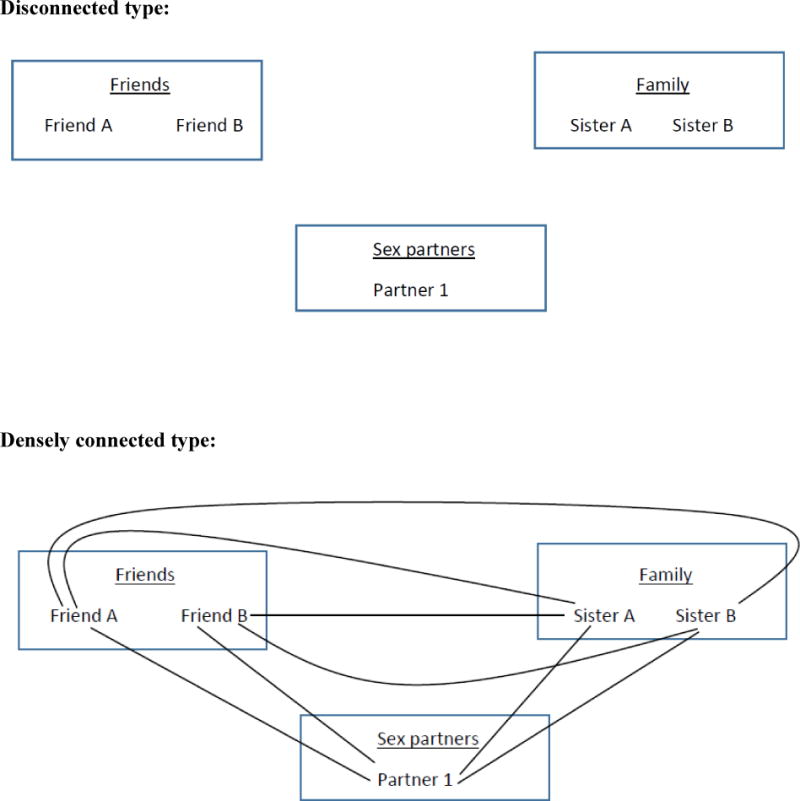
Note: Figure 1 includes an example from the Disconnected type where no connections are reported across network subgroups, and the Densely connected type where a connection is reported between every member of the social network.
Data Analysis
After excluding one participant due to missing social network data, 78 in-depth interviews (IDIs) were available for analysis. Since we expected data saturation to occur before all 78 IDIs were analysed, we employed a typical case purposive sampling strategy to identify a sub-sample of interviews for transcription (Patton 2002). Criteria outlined by Charmaz (Charmaz 2006) were used to determine at which point qualitative data saturation was reached, which included the analysis of the depth of themes across and within classifications. In addition, in order to obtain variation across major demographic groups, the subsample was targeted to be representative with respect to race (White, Coloured, Black), HIV status and age (18–25, >25). In total 34/78 interviews were sub-sampled and transcribed.
In order to create the social network typology, we counted the connections that men reported between individuals within their social network. Since two-thirds of our sample was recruited through snowball sampling we expected a number of men to report connections between friends as well as between friends and sex partners. Given this sampling bias we decided to consider the existence of connections between friends and family, between friends and sex partners and between family and sex partners in developing our network typology, with the possibility that no connections existed across these subgroups (Table 1). Key themes explored in more detail during the analysis were family and social network dynamics, sexual identity, sexual risk-taking behaviour, HIV testing behaviour and sex partner typologies.
Table 1.
Social Network Types of men who have sex with men in Cape Town and Port Elizabeth, South Africa
| Social Network Type | Description |
|---|---|
| Disconnected | No connections between any friends, family or sex partners, only within network subgroups |
| Sparsely connected | Minimal connections between friends and family members and no connections between sex partners and friends or between sex partners and family |
| Connected | Most connections between friends and sex partners, or between friends and family, but none between sex partners and family |
| Well-connected | Connections between family and sex partners as well as friends and sex partners |
| Densely connected | Connection exists between every person in network |
Data were analysed using constant comparative method by comparing similarities and differences between emerging categories (Charmaz 2006, Strauss 1998). Independent analysis among three coders took place which was followed by consensus revisions and development of an inductive codebook. Codes were applied to text and the social networks created during the social network activity, leading to further characterisation of the social network types in relation to sexual risk-taking. Analysis was conducted using MAXQDA version 10 (Verbi Software, Berlin, Germany). Key quotes are presented using pseudonyms to protect the privacy of participants.
Results
Social Network Typology
Five social network types emerged based on the reporting of whether network sub-groups (i.e., family, friends and sex partners) knew each other. In the analytical sample there were 2 participants classified as Disconnected, 2 classified as Sparsely Connected, 20 classified as Connected, 8 classified as Well Connected and 2 classified as Densely Connected. In the total sample there were 2 Disconnected, 4 Sparsely Connected, 40 Connected, 27 Well Connected and 5 Densely Connected participants. The mean number of connections reported was 13 (range: 0–72). The mean number of sex partners, friends and family members reported was 4 (range: 1–42), 3 (range: 1–10) and 7 (range: 0–8) respectively.
Disconnected Type (N=2)
This type included men without any connections between friends, family or sex partners; only connections within subgroups existed (i.e., sex partners knew each other, but were not connected to friends or family). The Disconnected type had limited connectivity to LGBT organisations. Allan described belonging to LGBT organisations as difficult because ‘most of the organisations feel I must look a certain way to be gay… so I must just refrain from taking part’. (Allan, Black, 42, Cape Town) Even though both men in this type identified as gay, they described homonegative feelings. Ayanda regarded public displays of affection between men as outside of the norm.
Why must you walk hand in hand? I don’t think there’s a reason, why must you walk hand in hand and then kiss, like, eh, because imagine if it was me. If I must see other gay guy with another gay guy, and they are holding and kissing I would stare, it’s not normal. (Ayanda, Coloured, 22, Port Elizabeth)
Allan described engaging in sex with other men as an “indulgence”.
I think it was an exploration at first. Because then I ended up indulging in it. I ended up wanting more and more of it. I think that’s indulgence. (Allan, Black, 42, CT)
Both Allan and Ayanda had main partners – gay-identifying men that they felt emotionally connected to – as well as concurrent casual partnerships with straight-identifying men. Ayanda reported that separation between these concurrent partnerships was intentional and having straight-identifying casual partners meant they were both invested in keeping his extramarital sexual partnerships hidden from his husband and gay-identified friends.
I don’t go with gay guys, because gay guys talk, they gossip. And that’s why I’d rather go with the straight guys so tomorrow, you don’t know me, I don’t know you. (Ayanda, Coloured, 22, PE)
Sex within these casual partnerships happened in public spaces (i.e., the taxi rank or mall toilets), but sex with main partners took place at the participant or partner’s home. These public venues were either a function of convenience (i.e., partners were encountered in these spaces) or indicative of the secrecy of the partnership. All sexual encounters in the past six months were unprotected by condoms and in some cases men reported paying for sex. While discussing lifetime sexual practices, Allan reported being less likely to use a condom if it wasn’t requested.
I: Can you tell me a little bit about why you used condoms with men?
P: Sometimes it’s requested. I could use a condom
I: And then when would you not use a condom
P: If not requested or under the influence. (Allan, Black, 42, CT)
HIV testing behaviours were also different between these two participants. Allan tested annually, while Ayanda reported risk-based HIV testing, having had his first test at the age of 21 years after discovering that his sex partner had been diagnosed HIV positive.
I: When did you, when did you first test for HIV?
P: That was, 2 years ago. Cause I was cheating [LAUGH]. And my one friend told me that this guy has HIV and we didn’t use a condom. (Ayanda, Coloured, 22, PE)
Sparsely Connected Type (N=2)
This type included men with minimal connections between friends and family and no connections between sex partners and friends or between sex partners and family. Unlike the Disconnected type, almost all men in the Sparsely Connected type reported connectivity to LGBT organisations. Safer sex practices in this type were mixed. One participant was a male sex worker who reported inconsistent condom use across clients and other sex partners; while one participant reported only one condom-protected anal sex experience in his lifetime. HIV testing behaviours were mixed with men testing regularly either as a result of their participation in a men’s health study or at their private healthcare provider.
Connected Type (N=20)
This type included men with connections between friends and family and between friends and sex partners, but no connections between sex partners and family. The Connected type had a large proportion of participants from one township in Port Elizabeth, most of who reported connectivity to the same local LGBT group.
Some participants described homophobia within their families and a large number of participants had non-disclosing partners who were in concurrent relationships with women. These participants spoke about keeping their sexual relationships hidden from their families because of straight-identified sex partners in concurrent relationships with women, referred to as “after nines” (referring to men who were only available to meet for sex at night unbeknownst to their female sexual partners). Bongani described the difficulty in finding an openly gay sex partner and the struggle with having to maintain these secret relationships.
‘It’s difficult for us to have a guy who would show himself. Many of the times, we have to hide. If you slept over, we must wake up early at 4 so that people will not see you slept together.’ (Bongani, Black, 23, PE)
Participants spoke about having to accept that their partners have to maintain these concurrent relationships and mitigating the risk of HIV infection by insisting on condoms each time they have sex. Some of these men experienced adverse mental health outcomes including depression and alcoholism as they struggled to deal with maintaining these secret relationships.
‘No we broke up when I was in Port Elizabeth. I was drinking too much because I was so frustrated. I was so depressed and stressed. My mum said, ‘Why don’t you try to go to your family in Cape Town. You will change whatever, because your behaviour, now here in Port Elizabeth, I don’t like it. It worries me because you drink a lot.’ Everything was just messed up now.’ (David, Black, 43, Cape Town)
Jason and Kabelo were very careful to keep their same-sex partnerships from their disapproving families. These men were financially dependent on and living with their families and felt forced to maintain separate networks. To appease his family, Jason had a female partner concurrent to his male relationship. Jason described his frustration with having to maintain these separate networks.
Sometimes I just pray to God to end up with this world, because I will get sick of it. I get concerned that my brother will find out that I’m gay. But, sometimes, it goes up in my head to tell my brothers ‘Man this is me’, you know? But at the same time, I’m like OK, if I tell them, they’re obviously going to tell mum. And then mom she’s going to be like, what a disappointment.’ (Jason, Black, 23, Cape Town)
Kabelo described emotionally inhibited relationships with their male sexual partners.
‘Look, with my dad every day I feel like I’m moving forward with him. I would slip up and do something and just leave it. You know what, you’ve got to be yourself. I mean, I’m almost 40 and I still haven’t had a serious relationship because I’m still dealing with so much. I still can’t give anything. In a relationship you give 50/50. I feel like I can’t give if I don’t know what I’m giving, if I’m so inhibited in so many ways.’ (Kabelo, White, 30, PE)
Sexual risk behaviours described by Jason and Kabelo were low, with only one or two recent sexual encounters, all of which were condom-protected. This may be due to limited sexual opportunities given their secretive lifestyles. Jason reported consistent condom use with all sex partners and only non-penetrative thigh sex with his male partner.
Men in the Connected type preferred short-term casual partnerships. Some ascribed this to a matter of convenience, while one participant cited bad past experiences with abusive long-term relationships as the main reason. Kagiso preferred not to introduce these casual ‘hookups’ to his family and described these casual hookups as ‘stress free’, not having to be concerned with whether the partner was in a concurrent relationship.
‘Having a booty call is stress free. You don’t have to explain yourself.’ (Kagiso, Black, 21, PE)
Reporting of safer sex practices was mixed. Two participants in this type were HIV positive and reported inconsistent condom use. Lefa spoke disapprovingly about the disregard that people in his community have for HIV, despite not practising safer sex himself and admitting to being ‘reckless’. He had not disclosed his HIV status to any of his sex partners.
In this community, the issue of one’s status isn’t an issue. When you go to bed with a person, very seldom that you talk about condom use or that you talk about HIV status. It’s as if it doesn’t exist. There’s a lot of carelessness so much that I think that the rate of HIV infection must be very high here. If the people that you’re going to interview after me are honest, you will see what I’m talking about. I think over the past 13 years, there may be only 3 or 4 people who ask for a condom. (Lefa, Black, 60, Port Elizabeth)
Both sex workers preferred to exclusively engage in oral sex to minimise the risk of HIV infection and reported consistent condom use when their sex partner insisted on anal sex. The remaining participants also reported consistent condom use with their sex partners.
Well-connected Type (N=8)
The Well-connected type included men with connections between family and sex partners, and between friends and sex partners. Unlike the Connected type, a large number of men in this type reported a main partner, although this was not always the only sex partner reported in the past six months. Connections between sex partners and family were more likely to occur with main partners.
Condom use among these men varied depending on the type of sex partner. A number of men reported ceasing condom use with main partners, despite not having had a recent HIV test or being unaware of their partner’s sero-status. Transactional sex was reported by a number of participants who either identified as a sex worker or by ‘tagging’ their sex partners which involved buying them clothing or giving them money. Matthew did not use a condom with one of his regular clients because the client was married and as a result he trusted him more.
I: OK. What about condoms? Do you use condoms with [NAME]?
P: No, [NAME] he don’t like condoms. Especially I know I’m not positive, and that I trust him just because he is married. (Matthew, Black, 25, CT)
Two participants who were married to one another used condoms consistently because one partner was HIV positive.
Densely Connected Type (N=2)
The Densely Connected type included men who had connections between every person in their social network, including connections between family and sex partners and between friends and sex partners. LGBT connectivity in this type was in stark contrast to the Disconnected type. Peter was the founder of a local LGBT group which supported men coming out to their families. His house was a favourite meeting spot for local gay men in support groups and also served as a place for him to meet new sex partners.
P: Or we can all sometimes have orgies, like say it’s 3 of us here in the room, we call boys and then it’s BAH!
I: OK, and this is at your place?
P: Yeah
(Peter, Black, 31, Port Elizabeth)
A number of men in the Densely Connected type reported connectivity to the same support group in Port Elizabeth.
Condom use in this type was inconsistent and men reported a number of casual partners also in concurrent relationships. Similar to the Well-connected type, condom use varied by the type of sex partner and type of sex, with condom use less likely with casual partners and exclusively oral sex encounters. Men reported being more likely to use a condom if they were unfamiliar with the partner or if the partner requested it. Peter rationalised why partners would request condom use and seemed eager to concede when asked.
I: Do you ever ask [NAME], why do you want to use condoms? Is it because you think you’re HIV positive? Do ever have a conversation about that?
P: No, it doesn’t bother me because really they’re younger than me and obviously maybe because I’ve been around a lot longer than them, so they just want to protect themselves against something that they don’t know. That’s how I take it so I don’t really want to ask them any questions.
I: And you said that when you were younger you had the same idea.
P: Yes. So, I just don’t want to jeopardise what I have with them by asking like, why do you want to use a condom. Maybe that’ll give them, give them another mindset about me.
(Peter, Black, 31, Port Elizabeth)
All but one participant reported straight-identified or bisexual casual partners, while the main partners tended to publicly identify as gay. Similar to the Connected type, men in the Densely Connected type expressed frustration with partners in concurrent relationships with women.
Most of the participants in the Densely Connected type only had one lifetime HIV test, with one participant living with HIV. Participants were either tested as part of their screening intake prior to medical male circumcision, because of suspected STI symptoms, or because of encouragement to get tested as part of a larger group of friends.
Discussion
Participants in our study were classified into five social network types based on self-reported connectivity between their friends, family and sex partners. At the one end of the spectrum, the Disconnected type showed signs of struggling with their sexual identity and feelings of homonegativity. Both men in the Disconnected type reported a main partner and concurrent casual sex partners. These casual partnerships were secretive and with straight-identifying men in concurrent relationships with women. Sex occurred in public spaces, was unprotected and sometimes transactional. This public nature and anonymity has been reported to be more prevalent in sexual encounters with straight-identifying partners, where the urgency of the encounter and risk of being caught is not amenable to condom use (Dladla 2013). Men also reported feelings of internalised homophobia, which has been shown to increase the likelihood of unprotected sexual encounters (Berg et al. 2013, Wright and Perry 2006, Ross et al. 2008).
At the other end of the spectrum, men in the Densely Connected type reported being more comfortable with their sexual identity. Men in the Densely Connected type also reported greater involvement with LGBT organisations. However, increased connectivity and LGBT involvement did not translate into safer risk profiles. A number of men reported multiple casual sexual encounters not protected by condoms. Larger and more connected networks have been shown to be associated with riskier sexual profiles by presenting more sexual partnering opportunities and exposing men to more varied sexual practices including condomless anal sex and transactional sex (Beyrer et al. 2012, Finneran and Stephenson 2014, Choi et al. 2007).
Reporting of the types and contexts of sexual risk behaviours varied across the five social network types. The Densely Connected type were more likely to report concurrent relationships, which is in contrast to findings that familiarity between sexual partners and friends was associated with a 52% reduction in concurrency among young South Africans (14–25 years) in the general population (Kenyon et al. 2010). Interestingly, the same study reported higher concurrency among Black men whose partner knew the family of the respondent (Kenyon et al. 2010). Other studies have reported knowing that one’s partner is in a concurrent relationship and emotional and sexual dissatisfaction as predictors of this behaviour – which were also reported by the Densely Connected type (Kenyon et al. 2010, Cox et al. 2014, Mah and Halperin 2010). The high prevalence of concurrency is concerning since it has been shown to be associated with higher levels of condomless anal sex among men who have sex with men and may be significant for HIV transmission within the setting of dense, overlapping networks (Rosenberg, Khosropour, and Sullivan 2012, Doherty et al. 2006, Mah and Halperin 2010).
Although the Densely Connected type reported greater comfort with their sexual identity and visibility in their community, their health-seeking behaviours were limited with most men reporting only one lifetime HIV test. The majority of the Densely Connected type were township residents. Challenges such as limited healthcare infrastructure and stigma is more pervasive within the township setting (Lane et al. 2008, Knox et al. 2011), suggesting that they still represent significant barriers to HIV preventative behaviours.
Men in the Well-connected type, with connections between all subgroups including family and sex partners, were more likely to be in a monogamous relationship. These men had the lowest median number of sex partners, but were more likely to cease condom use with their main partner, despite not having had a recent HIV test or not knowing their partners’ status. These men reported feeling pressured to cease using condoms with their main partners, suggesting that benefit can still be derived from dyadic-level interventions such as couples HIV counselling and testing (Stephenson et al. 2012, Sullivan et al. 2014).
The Connected type exhibited the most intragroup variability in HIV risk behaviours and social context, with men in this type having a range of different reasons for keeping their sex partners disconnected from their families. The Connected type included men experiencing family homophobia and men in relationships with non-disclosing partners. Participants experiencing familial homophobia felt forced to maintain dual identities and reported a lower number of, mostly protected, sexual encounters. This finding is in contrast to studies reporting that familial discrimination and a need to maintain a heterosexual identity are associated with high risk behaviours (Diaz, Ayala, and Bein 2004, Ryan et al. 2009). Since both men experiencing familial homophobia lived with their families, the lower number of sexual encounters may be as a result of limited sexual opportunities and may also be a strategy employed by these men to limit being in stigmatising situations (Choi et al. 2011).
The qualitative characterisation of these social network types sheds light on the role that social context may play on prevailing sexual norms and sexual risk behaviours. The Disconnected type exploited homonegative norms by only engaging in casual partnerships with non-disclosing straight-identifying partners, thereby hiding same-sex behaviours. The Connected type were forced to keep their relationships hidden because their partners were in concurrent relationships with women and minimised their risk by insisting on condoms. Men in the Connected type reported feeling constrained in their ability to have open and emotionally satisfying relationships with these partners and many reported adverse mental health outcomes such as depression and suicidal ideation.
There are several limitations to the current study. First, recruitment methods likely limited diversity in participants, over-sampling those who were connected to community-based organisations. These men may be systematically different to other men who have sex with men; for example, the majority of our sample was gay-identified. In addition, the network data collection focused on the last six months and may not be completely representative of the participant’s social network. We also examined only self-reported social networks; it is possible that social desirability led men to report only the connections they felt comfortable with reporting. Additionally, our sample contained a small number of men who reported participating in transactional sex. The number was too small to analyse their data separately and their self-reported networks did not differ significantly to other men who have sex with men.
In conclusion, this typology emphasises the diversity in the social networks and lived realities of men who have sex with men in two South African cities, and offers an alternative lens through which to view the ways in which sexual risk is manifested. Furthermore, our results reiterate the limitations of treating men who have sex with men as a homogenous risk group and underscore the importance of reframing public health messaging according to the specific contexts in which men live. Findings from this study demonstrate the utility of social network mapping as an exposure assessment tool when evaluating sexual risk e.g., assessing social network connectivity may help identify men that more prone to depressive behaviours or feelings of internalised homonegativity. During HIV counselling and testing, counselors could consider asking about the degree of social support available and network connectivity, which can in turn tailor the counseling and referral process. The way in which HIV prevention messages are delivered to men needs to be tailored: disconnected and sparsely connected men may benefit from more generic public health campaigns or discreet healthcare facilities tailored to men who have sex with men, while densely connected men may prefer more explicit and overtly men who have sex with men focused campaigns. Understanding social contexts and the reasons men have such varied social connections is fundamental for providing targeted and nuanced HIV prevention work.
Table 2.
Characteristics of 34 men who have sex with men, Cape Town and Port Elizabeth, South Africa
| All, % (N) | Disconnected (N=2) | Sparsely connected (N=2) | Connected (N=18) | Well-connected (N=10) | Densely connected (N=2) | |
|---|---|---|---|---|---|---|
| Age (years) | ||||||
| 18–25 | 50 (17) | 50 (1) | – | 44 (8) | 70 (7) | 50 (1) |
| 26–35 | 29 (10) | – | – | 33 (6) | 30 (3) | 50 (1) |
| >35 | 21 (7) | 50 (1) | 100 (2) | 22 (4) | – | – |
| Race | ||||||
| Black | 62 (21) | 50 (1) | 50 (1) | 67 (12) | 50 (5) | 100 (2) |
| Coloured | 21 (7) | 50 (1) | 50 (1) | 17 (3) | 20 (2) | – |
| White | 18 (6) | – | – | 17 (3) | 30 (3) | – |
| Self-reported HIV status | ||||||
| HIV negative | 76 (26) | 100 (2) | 50 (1) | 72 (13) | 70 (7) | 100 (2) |
| HIV positive | 24 (8) | – | 50 (1) | 28 (5) | 30 (3) | – |
| Educational attainment | ||||||
| Primary or less | 29 (10) | 50 (1) | 100 (2) | 39 (7) | – | – |
| Secondary | 53 (18) | 50 (9) | 70 (7) | 100 (2) | ||
| College or higher | 18 (6) | 50 (1) | 11 (2) | 30 (3) | – | |
| Current employment status | ||||||
| Unemployed | 47 (16) | 50 (1) | 50 (1) | 61 (11) | 10 (1) | 100 (2) |
| Employed | 41 (14) | 50 (1) | 50 (1) | 33 (6) | 50 (5) | – |
| Student | 12 (4) | 6 (1) | 40 (4) | – | ||
| Current relationship status | ||||||
| Single | 15 (5) | 100 (2) | 17 (3) | – | – | |
| Dating | 29 (10) | 39 (7) | 30 (3) | – | ||
| Monogamous partnership | 47 (16) | 50 (1) | 44 (8) | 50 (5) | 100 (2) | |
| Married | 9 (3) | 50 (1) | – | 20 (2) | – | |
| Sex partners, median (IQR) | 3 (1–7) | 11 (10–11) | 7 (2–15) | 3 (1–5) | 1 (1–3) | 3 (3–7) |
Acknowledgments
The authors would like to thank the participants for their valuable time and participation, and Ayesha McAdams-Mahmoud for her work in the study implementation and data collection.
Funding
This work was supported by the US National Institute of Allergy and Infectious Diseases under Grant [1R01AI094575–01]; and was facilitated by the Center for AIDS Research at Emory University, P30AI050409.
References
- Berg RC, Ross MW, Weatherburn P, Schmidt AJ. Structural and environmental factors are associated with internalised homonegativity in men who have sex with men: findings from the European MSM Internet Survey (EMIS) in 38 countries. Social Science & Medicine. 2013;78:61–9. doi: 10.1016/j.socscimed.2012.11.033. [DOI] [PubMed] [Google Scholar]
- Beyrer C, Baral SD, van Griensven F, Goodreau SM, Chariyalertsak S, Wirtz AL, Brookmeyer R. Global epidemiology of HIV infection in men who have sex with men. Lancet. 2012;380(9839):367–77. doi: 10.1016/S0140-6736(12)60821-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burrell E, Mark D, Grant R, Wood R, Bekker LG. Sexual risk behaviours and HIV-1 prevalence among urban men who have sex with men in Cape Town, South Africa. Sexual Health. 2010;7(2):149–53. doi: 10.1071/SH09090. [DOI] [PubMed] [Google Scholar]
- Charmaz K. Constructing Grounded Theory. In: Silverman D, editor. Introducing Qualitative Methods. SAGE; 2006. [Google Scholar]
- Choi KH, Han CS, Paul J, Ayala G. Strategies for managing racism and homophobia among U.S. ethnic and racial minority men who have sex with men. AIDS Education and Prevention. 2011;23(2):145–58. doi: 10.1521/aeap.2011.23.2.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi KH, Ning Z, Gregorich SE, Pan QC. The influence of social and sexual networks in the spread of HIV and syphilis among men who have sex with men in Shanghai, China. Journal of Acquired Immune Deficiency Syndrome. 2007;45(1):77–84. doi: 10.1097/QAI.0b013e3180415dd7. [DOI] [PubMed] [Google Scholar]
- Cox CM, Babalola S, Kennedy CE, Mbwambo J, Likindikoki S, Kerrigan D. Determinants of concurrent sexual partnerships within stable relationships: a qualitative study in Tanzania. British Medical Journal Open. 2014;4(2):e003680. doi: 10.1136/bmjopen-2013-003680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diaz RM, Ayala G, Bein E. Sexual risk as an outcome of social oppression: data from a probability sample of Latino gay men in three U.S. cities. Cultural Diversity & Ethnic Minority Psychology. 2004;10(3):255–67. doi: 10.1037/1099-9809.10.3.255. [DOI] [PubMed] [Google Scholar]
- Dladla S. Sexual behaviors and HIV protective practices amongst men who have sex with men (MSM) and men who have sex with men and women (MSMW) in Soweto. MPH, Faculty of Health Sciences University of Witwatersrand; 2013. [Google Scholar]
- Doherty IA, Shiboski S, Ellen JM, Adimora AA, Padian NS. Sexual bridging socially and over time: a simulation model exploring the relative effects of mixing and concurrency on viral sexually transmitted infection transmission. Sexually Transmitted Diseases. 2006;33(6):368–73. doi: 10.1097/01.olq.0000194586.66409.7a. [DOI] [PubMed] [Google Scholar]
- Finneran C, Stephenson R. Social network composition and sexual risk-taking among gay and bisexual men in Atlanta, GA. AIDS & Behavior. 2014;18(1):59–68. doi: 10.1007/s10461-013-0569-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jewkes R, Dunkle K, Nduna M, Levin J, Jama N, Khuzwayo N, Koss M, Puren A, Duvvury N. Factors associated with HIV sero-positivity in young, rural South African men. International Journal of Epidemiology. 2006;35(6):1455–60. doi: 10.1093/ije/dyl217. [DOI] [PubMed] [Google Scholar]
- Jobson G, de Swardt G, Rebe K, Struthers H, McIntyre J. HIV Risk and Prevention Among Men Who Have Sex with Men (MSM) in Peri-Urban Townships in Cape Town, South Africa. AIDS & Behavior. 2012;Suppl 1:S12–22. doi: 10.1007/s10461-012-0328-5. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Nachimson D. Self-efficacy and disclosure of HIV-positive serostatus to sex partners. Health Psychology. 1999;18(3):281–7. doi: 10.1037//0278-6133.18.3.281. [DOI] [PubMed] [Google Scholar]
- Kenyon C, Boulle A, Badri M, Asselman V. “I don’t use a condom (with my regular partner) because I know that I’m faithful, but with everyone else I do”: The cultural and socioeconomic determinants of sexual partner concurrency in young South Africans. SAHARA Journal. 2010;7(3):35–43. doi: 10.1080/17290376.2010.9724967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knox J, Sandfort T, Yi H, Reddy V, Maimane S. Social vulnerability and HIV testing among South African men who have sex with men. International Journal of STD & AIDS. 2011;22(12):709–13. doi: 10.1258/ijsa.2011.010350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane T. HIV research among township men who have sex with men in South Africa. In: Reddy V, Sandfort T, Rispel L, editors. From Social Silence to Social Science: Same-sex sexuality, HIV & AIDS and Gender in South Africa. South Africa: HSRC Press; 2009. [Google Scholar]
- Lane T, Mogale T, Struthers H, McIntyre J, Kegeles SM. “They see you as a different thing”: the experiences of men who have sex with men with healthcare workers in South African township communities. Sexually Transmitted Infections. 2008;84(6):430–3. doi: 10.1136/sti.2008.031567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane T, Raymond HF, Dladla S, Rasethe J, Struthers H, McFarland W, McIntyre J. High HIV prevalence among men who have sex with men in Soweto, South Africa: results from the Soweto Men’s Study. AIDS & Behavior. 2011;15(3):626–34. doi: 10.1007/s10461-009-9598-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin C, Yang C, Tobin K, Roebuck G, Spikes P, Patterson J. Social network predictors of disclosure of MSM behavior and HIV-positive serostatus among African American MSM in Baltimore, Maryland. AIDS & Behavior. 2012;16(3):535–42. doi: 10.1007/s10461-011-0014-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maartens G, Wood R, O’Keefe E, Byrne C. Independent epidemics of heterosexual and homosexual HIV infection in South Africa–survival differences. Quarterly Journal of Medicine. 1997;90(7):449–54. doi: 10.1093/qjmed/90.7.449. [DOI] [PubMed] [Google Scholar]
- Mah TL, Halperin DT. Concurrent sexual partnerships and the HIV epidemics in Africa: evidence to move forward. AIDS & Behavior. 2010;14(1):11–6. doi: 10.1007/s10461-008-9433-x. dicussion 34–7. [DOI] [PubMed] [Google Scholar]
- Masvawure TB, Sandfort TG, Reddy V, Collier KL, Lane T. ’They think that gays have money’: gender identity and transactional sex among Black men who have sex with men in four South African townships. Culture, Health & Sexuality. 2015;17(7):891–905. doi: 10.1080/13691058.2015.1007168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olley BO, Seedat S, Stein DJ. Self-disclosure of HIV serostatus in recently diagnosed patients with HIV in South Africa. African Journal of Reproductive Health. 2004;8(2):71–6. [PubMed] [Google Scholar]
- Patton MQ. Qualitative research & evaluation methods. 3rd. Thousand Oaks, CA: SAGE; 2002. [Google Scholar]
- Preston DB, D’Augelli AR, Kassab CD, Starks MT. The relationship of stigma to the sexual risk behavior of rural men who have sex with men. AIDS Education and Prevention. 2007;19(3):218–30. doi: 10.1521/aeap.2007.19.3.218. [DOI] [PubMed] [Google Scholar]
- Rebe KB, De Swardt G, Struthers H, McIntyre JA. Towards ’men who have sex with men appropriate’ health services in South Africa. South African Journal of HIV Medicine. 2013;14(2):52–57. [Google Scholar]
- Reddy V, Sandfort T, Rispel L. From Social Silence to Social Science: Same-sex sexuality. In: Reddy V, Sandfort T, Rispel L, editors. HIV & AIDS and Gender in South Africa. HSRC Press; 2009. [Google Scholar]
- Rispel LC, Metcalf CA. Breaking the silence: South African HIV policies and the needs of men who have sex with men. Reproductive Health Matters. 2009;17(33):133–42. doi: 10.1016/S0968-8080(09)33442-4. [DOI] [PubMed] [Google Scholar]
- Rispel LC, Metcalf CA, Cloete A, Reddy V, Lombard C. HIV prevalence and risk practices among men who have sex with men in two South African cities. Journal of Acquired Immune Deficiency Syndromes. 2011;57(1):69–76. doi: 10.1097/QAI.0b013e318211b40a. [DOI] [PubMed] [Google Scholar]
- Rosenberg ES, Khosropour CM, Sullivan PS. High prevalence of sexual concurrency and concurrent unprotected anal intercourse across racial/ethnic groups among a national, Web-based study of men who have sex with men in the United States. Sexually Transmitted Diseases. 2012;39(10):741–6. doi: 10.1097/OLQ.0b013e31825ec09b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross MW, Rosser BR, Neumaier ER, Team Positive Connections The relationship of internalized homonegativity to unsafe sexual behavior in HIV-seropositive men who have sex with men. AIDS Education and Prevention. 2008;20(6):547–57. doi: 10.1521/aeap.2008.20.6.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan C, Huebner D, Diaz RM, Sanchez J. Family rejection as a predictor of negative health outcomes in white and Latino lesbian, gay, and bisexual young adults. Pediatrics. 2009;123(1):346–52. doi: 10.1542/peds.2007-3524. [DOI] [PubMed] [Google Scholar]
- Sandfort TG, Knox J, Collier KL, Lane T, Reddy V. HIV testing practices of South African township MSM in the era of expanded access to ART. AIDS & Behavior. 2015;19(3):561–74. doi: 10.1007/s10461-014-0843-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandfort TG, Lane T, Dolezal C, Reddy V. Gender Expression and Risk of HIV Infection Among Black South African Men Who Have Sex with Men. AIDS & Behavior. 2015 doi: 10.1007/s10461-015-1067-1. First online 14 April. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandfort TG, Nel J, Rich E, Reddy V, Yi H. HIV testing and self-reported HIV status in South African men who have sex with men: results from a community-based survey. Sexually Transmitted Infections. 2008;84(6):425–9. doi: 10.1136/sti.2008.031500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sher R. HIV infection in South Africa, 1982–1988–a review. South African Medical Journal. 1989;76(7):314–8. [PubMed] [Google Scholar]
- Shisana O, Rehle T, Simbayi LC, Zuma K, Jooste S, Zungu N, Labadarios D, Onoya D. South African National HIV Prevalence, Incidence and Behaviour Survey. Cape Town: Human Sciences Research Council; 2012. [DOI] [PubMed] [Google Scholar]
- Siegler AJ, Sullivan PS, de Voux A, Phaswana-Mafuya N, Bekker LG, Baral SD, Winskell K, Kose Z, Wirtz AL, Brown B, Stephenson R. Exploring repeat HIV testing among men who have sex with men in Cape Town and Port Elizabeth, South Africa. AIDS Care. 2014;27(2):229–341. doi: 10.1080/09540121.2014.947914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegler Aaron J, Voux Alex de, Phaswana-Mafuya Nancy, Bekker Linda-Gail, Sullivan Patrick S, Baral Stefan D, Winskell Kate, Kose Zamakayise, Wirtz Andrea L, Stephenson Rob. Elements of Condom-Use Decision Making among South African Men Who Have Sex with Men. Journal of the International Association of Providers of AIDS Care. 2014 doi: 10.1177/2325957414535979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith AM, Grierson J, Wain D, Pitts M, Pattison P. Associations between the sexual behaviour of men who have sex with men and the structure and composition of their social networks. Sexually Transmitted Infections. 2004;80(6):455–8. doi: 10.1136/sti.2004.010355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- South African National AIDS Council. National Strategic Plan on HIV, STIs and TB 2007–2011 2007 [Google Scholar]
- South African National AIDS Council. End of Term Review of the NSP 2007–2011 2011 [Google Scholar]
- Stephenson R, Rentsch C, Sullivan P, McAdams-Mahmoud A, Jobson G, Struthers H, McIntyre J. Attitudes Toward Couples-Based HIV Counseling and Testing Among MSM in Cape Town, South Africa. AIDS & Behavior. 2012;17(Suppl 1):S43–50. doi: 10.1007/s10461-012-0293-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss AL, Corbin JM. Basics of qualitative research: Techniques and procedures for developing grounded theory. 2nd. Thousand Oaks: SAGE; 1998. [Google Scholar]
- Sullivan PS, Stephenson R, Grazter B, Wingood G, Diclemente R, Allen S, Hoff C, Salazar L, Scales L, Montgomery J, Schwartz A, Barnes J, Grabbe K. Adaptation of the African couples HIV testing and counseling model for men who have sex with men in the United States: an application of the ADAPT-ITT framework. Springerplus. 2014;3:249. doi: 10.1186/2193-1801-3-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Harmelen J, Wood R, Lambrick M, Rybicki EP, Williamson AL, Williamson C. An association between HIV-1 subtypes and mode of transmission in Cape Town, South Africa. AIDS. 1997;11(1):81–7. doi: 10.1097/00002030-199701000-00012. [DOI] [PubMed] [Google Scholar]
- Wilkinson E, Engelbrecht S. Molecular characterization of non-subtype C and recombinant HIV-1 viruses from Cape Town, South Africa. Infection, Genetics and Evolution. 2009;9(5):840–6. doi: 10.1016/j.meegid.2009.05.001. [DOI] [PubMed] [Google Scholar]
- Wright ER, Perry BL. Sexual identity distress, social support, and the health of gay, lesbian, and bisexual youth. Journal of Homosexuality. 2006;51(1):81–110. doi: 10.1300/J082v51n01_05. [DOI] [PubMed] [Google Scholar]


