Abstract
Background
The prognostic value of p53 protein expression in esophageal cancer has been evaluated, but the results remain inconclusive and no consensus has yet been achieved. This meta-analysis was conducted to quantitatively assess the prognostic significance of p53 expression in esophageal cancer.
Methods
Publications that assessed the clinical or prognostic significance of p53 expression in esophageal cancer and were published before July 1, 2015 were identified by searching the PubMed and EMBASE databases. A meta-analysis was performed to clarify the association between p53 expression and the clinical outcomes.
Results
A total of 36 publications met the criteria and included 4577 cases. Analysis of these data showed that p53 expression in esophageal cancer was significantly associated with poorer 5-year survival (RR = 1.30, 95 % CI: 1.11–1.51, P = 0.0008). Subgroup analyses according to histological type, continent of the patients, and cut-off value revealed the similar results. The results also indicated that p53 expression was highly associated with advanced TNM stages (I/II vs. III/IV, OR = 0.74, 95 % CI: 0.55–0.99, P = 0.04), lymph node metastasis (OR = 0.77, 95 % CI: 0.66–0.90, P = 0.001), and distant metastasis (OR = 0.46, 95 % CI: 0.26–0.80, P = 0.006). However, p53 expression in the included studies was not significantly associated with tumor size (≤ 5 cm vs. > 5 cm, OR = 1.13, 95 % CI: 0.92–1.40, P = 0.24), tumor location (upper + middle vs. lower, OR = 0.91, 95 % CI: 0.70–1.17, P = 0.45), grade of differentiation (well + moderate vs. poor, OR = 1.10, 95 % CI: 0.90–1.34, P = 0.35), and the depth of invasion (T1/T2 vs. T3/T4, OR = 0.86, 95 % CI: 0.71–1.03, P = 0.09).
Conclusions
This meta-analysis showed that p53 expression may be a useful biomarker for predicting poorer prognosis in patients with esophageal cancer.
Keywords: p53, Esophageal cancer, Prognosis, Meta-analysis
Background
Esophageal cancer (EC), a highly aggressive and lethal malignancy, causes 400 200 deaths worldwide and is the sixth leading cause of cancer death in 2012 [1]. This malignancy includes two major histological types: esophageal squamous cell carcinoma (ESCC) and esophageal adenocarcinoma (EAC). Although the relevant diagnosis and treatment methods have dramatically improved in recent years, atypical early symptoms, middle-to-late stage diagnosis, low treatment remission rates, and high local recurrence rates continue to contribute to the poor prognosis of patients with EC [2]. The increasing incidence and poor prognosis of EC represent a major global public health problem [3]. Despite advancements in diagnostic and treatment methods in recent years, the prognosis of patients with EC remains not ideal. Only a small group of patients (15–30 %) survive five years after surgery [4, 5]. Therefore, the detailed molecular mechanisms involved in EC progression must be understood and prognostic factors should be identified to enable the precise prediction of survival and selection of better treatment and preventive measures for patients with EC.
A few biomarkers, including p53, vascular endothelial growth factor (VEGF) [6], and CXC chemokine receptor type 4 (CXCR4) [7], have recently emerged as prognostic or predictive factors in EC. p53, a tumor-suppressor gene, is located on the short arm of chromosome 17 and displays the highest correlation with human types of cancer uncovered thus far. This gene encodes the p53 protein, which acts as a transcription factor that plays a key role in cell cycle regulation, DNA synthesis inhibition, damaged DNA repair, and apoptosis [8, 9]. Under normal conditions, p53 levels are low; in some cases, they may even be undetectable [10]. However, the expression rate of p53 detected by immunohistochemistry (IHC) has been reported to range from 33 to 70 % in EC [11, 12]. p53 shows nuclear staining because of accumulation of mutant p53, which often has an increased stability and is resistant to degradation, making it detectable by IHC [13]. A cell without mutation is negative for IHC staining of p53 because no dye accumulation occurs in the cell [14]. Although accumulation of p53 detected by IHC does not necessarily imply gene mutation, p53 over-expression in most of cases (85 %) implies an underlying mutation [15]. Therefore, p53 expression may be regarded as an indicator of p53 gene mutation.
Over the past decade, numerous studies have evaluated the prognostic value of p53 protein expression in EC. However, the results of these reports remain inconclusive and no consensus has yet been achieved. Therefore, we conducted a systematic review and meta-analysis to address the association between p53 expression and the common clinical and pathological features of EC.
Methods
Search strategy
We considered all studies on the association between p53 and EC in this research. A systematic search was performed with the following keywords or their combinations: “p53” or “TP53” and “esophageal cancer” or “esophageal carcinoma.” The search was performed in the PubMed and EMBASE databases. The last search in this study was updated in July 2015.
Inclusion criteria
All of the original studies must meet the following criteria to be included in this meta-analysis: (1) Patients were confirmed as EC by pathological examination. (2) The expression of p53 in primary tumor tissues was detected by IHC. (3) None of patients had received radiation therapy or chemotherapy before surgery. (4) The sample size was greater than 20. (5) The association between p53 expression and overall survival (OS) of the patients with EC was evaluated. (6) Sufficient data were provided to allow the estimation of risk ratios (RRs) or odds ratios (ORs) and their corresponding 95 % confidence intervals (CI). (7) Only studies written in English and Chinese were included in this study.
Exclusion criteria
The search was broadened by browsing the related summary, methods, and references of retrieved articles. The title and abstract of each study identified in the search were scanned to exclude clearly irrelevant publications. The remaining articles were browsed to determine whether they contained information on the topic of interest. We excluded studies from this meta-analysis if they were: (1) review articles, case reports, familiar studies, duplicated publications, conference abstracts, and letters; (2) studies where p53 expression was evaluated by a method other than IHC; (3) studies with sample sizes less than 20; (4) studies without clinical data and the relationship between p53 expression and disease prognosis; (5) duplicate articles. For duplicate studies based on identical or overlapping patient populations, only the most recent and/or complete study was included in this meta-analysis.
Data extraction
Information was carefully and independently extracted from all eligible publications by two of the authors according to the inclusion criteria listed above. Disagreement was resolved by discussion between the two authors until a consensus was reached. Data tables were constructed to extract all relevant data from the text, tables, and figures of each included study, including the author, publication year, country of patient’s origin, tumor stage, number of patients, research technique, and cut-off value of p53 expression. When the prognosis was only plotted as a Kaplan–Meier curve in some articles, Engauge Digitizer 4.1 software (from https://sourceforge.net/projects/digitizer/) was applied to digitize and extract the data.
Statistical analysis
ORs with 95 % CI were used to evaluate the association between p53 expression and clinicopathological factors, including the tumor TNM stage, tumor size, tumor location, grade of differentiation, depth of invasion, lymph node involvement, and distant metastasis. To stratify data for analysis, the p53 expression and clinicopathological factors were combined into single categories with comparable clinicopathological relevance: tumor TNM staging (I/II vs. III/IV), lymph node (negative or positive), distant metastasis (negative or positive), tumor size (≤ 5 cm vs. > 5 cm), tumor location (upper + middle vs. lower), grade of differentiation (well + moderate vs. poor), and depth of invasion (T1/T2 vs. T3/T4). RRs with 95 % CI were used to assess the association between p53 expression and the combined survival outcome over several studies. The presence of heterogeneity among studies was evaluated by the Dersimonian and Laird’s Q test. I2 was used to quantify heterogeneity, and an I2 value > 50 % was considered to represent substantial heterogeneity between studies [16]. Compared with fixed-effects models, random-effects models were found to be more appropriate for the current study because of the heterogeneity revealed by the forest plots. Heterogeneity often cannot be revealed by the Q test because of its low power. The influence of individual studies on the estimated summary effect was displayed in the sensitivity analysis. In addition, funnel plots were used to estimate the possible publication bias. Cochrane Review Manager version 5.2 (Cochrane Library) was used to calculate the ORs and RRs, as well as their variations, from each investigation.
Results
Description of studies
A total of 36 publications met the criteria for the analysis (Fig. 1). The total number of patients was 4577, with 33–775 patients per study. The main characteristics of the eligible studies, including the cut-off definition for p53-positive results, are summarized in Table 1. All of the studies determined the OS, and some reports included clinicopathological factors. IHC was the only method used to evaluate p53 expression in EC specimens.
Fig. 1.
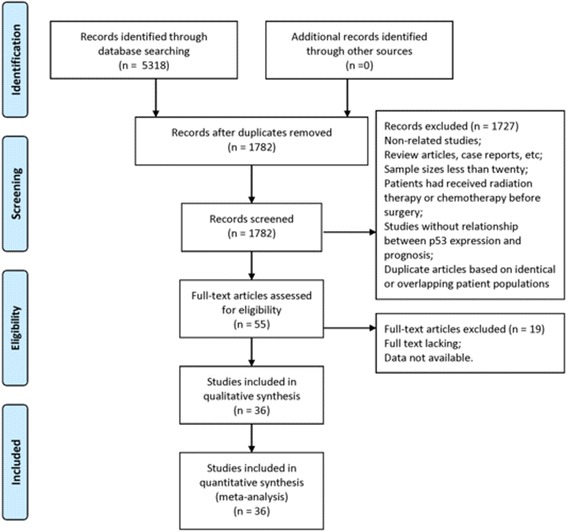
Literature search strategy and selection of articles
Table 1.
Characteristics of studies included in this meta-analysis
| Study | Country | Type | Source | Cases | p53 positive rate (%) | IHC Cut off (nuclear positivity) |
|---|---|---|---|---|---|---|
| Madani K, 2010 [12] | Canada | EAC | esophagectomy | 142 | 33.8 | >10 % |
| Casson AG, 1998 [28] | Canada | ESCC/EAC | esophagectomy | 61 | 39 | >10 % |
| Rosa AR, 2003 [29] | Brazil | ESCC | esophagectomy | 47 | 53.2 | >10 % |
| Bahnassy AA, 2005 [30] | Egypt | ESCC/UC | esophagectomy | 50 | 68 | >10 % |
| Egashira A, 2011 [31] | Japan | ESCC | esophagectomy | 94 | 56.4 | >10 % |
| Chanvitan A, 1995 [32] | Canada | ESCC | esophagectomy | 80 | 50 | >10 % |
| Murata, A, 2013 [33] | Japan | ESCC | esophagectomy | 266 | 52 | weak-to-strong |
| Wang DY, 1994 [34] | China | ESCC | esophagectomy | 100 | 65 | >30 % |
| Kato H, 2001 [35] | Japan | ESCC | esophagectomy | 89 | 55.1 | >10 % |
| Flejou JF, 1994 [36] | France | EAC | esophagectomy | 62 | 66 | ND |
| Shimaya K, 1993 [37] | Japan | ESCC | esophagectomy | 105 | 53 | any nuclear positivity |
| Huang K, 2014 [38] | China | ESCC | esophagectomy | 118 | 49.2 | >10 % |
| Lam KY, 1999 [39] | China | ESCC | esophagectomy | 153 | 64.1 | >25 % |
| Chyczewski L, 1999 [40] | Poland | ESCC | esophagectomy | 33 | 45 | >10 % |
| Cavazzola LT, 2009 [41] | Brazil | EAC | esophagectomy | 38 | 52.2 | >10 % |
| Shang L, 2014 [42] | China | ESCC | esophagectomy | 590 | 43 | >10 % |
| Yasuda M, 2000 [27] | Japan | EC | esophagectomy | 35 | 48.5 | dark brown |
| Kuwahara M, 1999 [43] | Japan | EC | esophagectomy | 64 | 48.4 | >10 % |
| Nita ME, 1999 [44] | Brazil | ESCC | esophagectomy | 62 | 50 | >10 % |
| Ikeguchi M, 2000 [45] | Japan | ESCC | esophagectomy | 191 | 44.5 | >50 % |
| Furihata M, 1993 [46] | Japan | ESCC | esophagectomy | 71 | 33.8 | ND |
| Ahn MJ, 2002 [47] | Korea | ESCC/BSCC | esophagectomy | 81 | 51.9 | >10 % |
| Hashimoto N, 1999 [48] | Japan | ESCC | esophagectomy | 73 | 64 | >5 % |
| Makoto O, 2002 [49] | Japan | ESCC | esophagectomy | 96 | 46 | >10 % |
| Hsu PK, 2008 [50] | China | ESCC | esophagectomy | 68 | 63.2 | >25 % |
| Kanamoto A,1999 [51] | Japan | ESCC | esophagectomy | 239 | 48.1 | >10 % |
| Hardwick RH, 1997 [52] | UK | ESCC/EAC | esophagectomy | 78 | 66.7 | >10 % |
| Vijeyasingam R, 1994 [53] | England | ESCC/EAC | esophagectomy | 60 | 68.3 | >5 % |
| Inada S, 1999 [54] | Japan | ESCC | esophagectomy | 40 | 52.5 | >10 % |
| Nakamura T, 1995 [55] | Japan | ESCC | esophagectomy | 61 | 52 | ND |
| Cheng TH, 2009 [56] | China | ESCC | esophagectomy | 119 | 51.3 | >10 % |
| Yao W, 2014 [57] | China | ESCC | esophagectomy or endoscopy | 136 | 41.9 | weak-to-strong |
| Takeno S, 2002 [58] | Germany | ESCC | esophagectomy | 71 | 36.6 | >10 % |
| Xu XL, 2014 [59] | China | ESCC | esophagectomy | 775 | 35.9 | >10 % |
| Takahashi Y, 2006 [60] | Japan | ESCC | esophagectomy | 180 | 61.7 | >10 % |
| Goukon Y, 1994 [61] | Japan | ESCC | esophagectomy | 49 | 59 | any nuclear positivity |
UC undifferentiated carcinoma, BSCC basaloid squamous cell carcinoma, ND not documented
Correlation of p53 expression with clinicopathological parameters
The association between p53 and several clinicopathological parameters are illustrated in Fig. 2 and Table 2. The p53 expression was highly correlated with more advanced TNM stages (I/II vs. III/IV, OR = 0.74, 95 % CI: 0.55–0.99, P = 0.04, Fig. 2a), lymph node metastasis (OR = 0.77, 95 % CI: 0.66–0.90, P = 0.001, Fig. 2b), and distant metastasis (OR = 0.46, 95 % CI: 0.26–0.80, P = 0.006, Fig. 2c). However, p53 expression was not significantly associated with tumor size (≤ 5 cm vs. > 5 cm, OR = 1.13, 95 % CI: 0.92–1.40, P = 0.24), tumor location (upper + middle vs. lower, OR = 0.91, 95 % CI: 0.70–1.17, P = 0.45), grade of differentiation (well + moderate vs. poor, OR = 1.10, 95 % CI: 0.90–1.34, P = 0.35), and depth of invasion (T1/T2 vs. T3/T4, OR = 0.86, 95 % CI: 0.71–1.03, P = 0.09; Table 2).
Fig. 2.
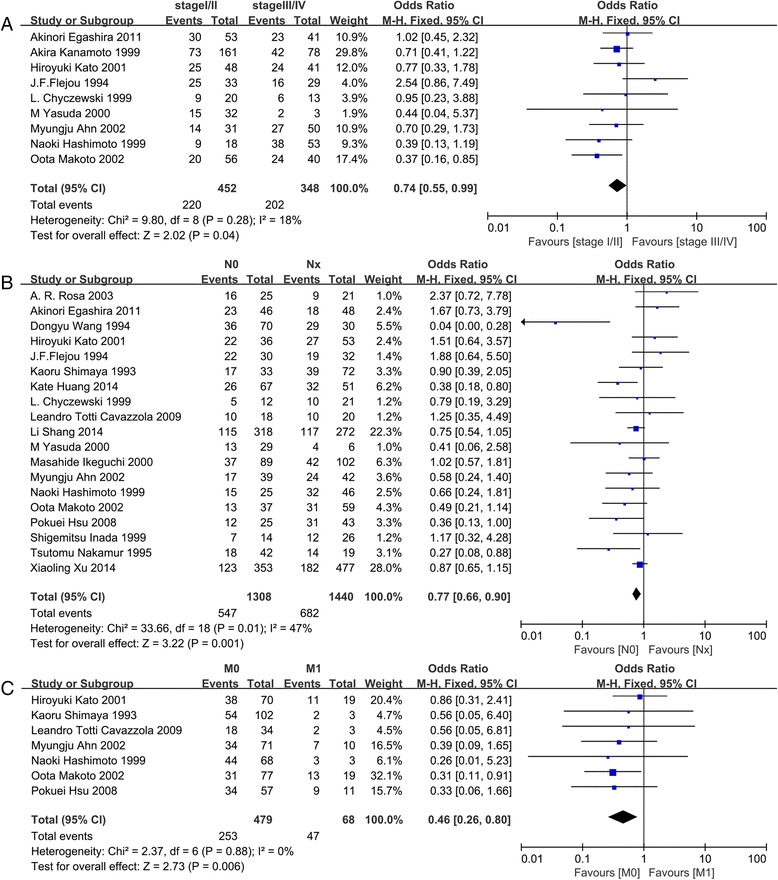
Forest plot of p53 expression and OR for clinicopathological features. The investigated clinicopathological parameters are TNM stage (a), lymph node metastasis (b), and distant metastasis (c). ORs with the corresponding confidence intervals are shown
Table 2.
Meta-analysis of p53 expression and clinicopathological features of EC
| Clinicopathological features | N | Cases | Analytical model | Pooled OR (95 % CI) | P value | Heterogeneity | |
|---|---|---|---|---|---|---|---|
| I2 (%) | P value | ||||||
| Tumor size (≤ 5 cm vs. > 5 cm) | 4 | 1515 | FEM | 1.13 (0.92–1.40) | 0.24 | 0 | 0.96 |
| Tumor location (upper + middle vs. lower) | 8 | 1205 | FEM | 0.91 (0.70–1.17) | 0.45 | 0 | 0.80 |
| Grade of differentiation (well + moderate vs. poor) | 16 | 2328 | FEM | 1.10 (0.90–1.34) | 0.35 | 17 | 0.26 |
| Depth of invasion (T1/T2 vs. T3/T4) | 13 | 2262 | FEM | 0.86 (0.71–10.3) | 0.09 | 0 | 0.67 |
N number of studies, FEM fixed-effect model
p53 expression and five-year survival outcome
Based on the methods described above, the OS of 4577 patients in 36 studies were analyzed. The 5-year OS rate was extracted from 32 studies. Meta-analysis of the 32 studies for the prognostic value of p53 expression showed that increased expression was associated with poorer OS. This trend was obtained from the M–H random-effects model with a value of 1.30 (95 % CI: 1.11–1.51, P = 0.0008; Fig. 3), although heterogeneity between studies was noted (I2 = 66 %, Ph < 0.00001).
Fig. 3.
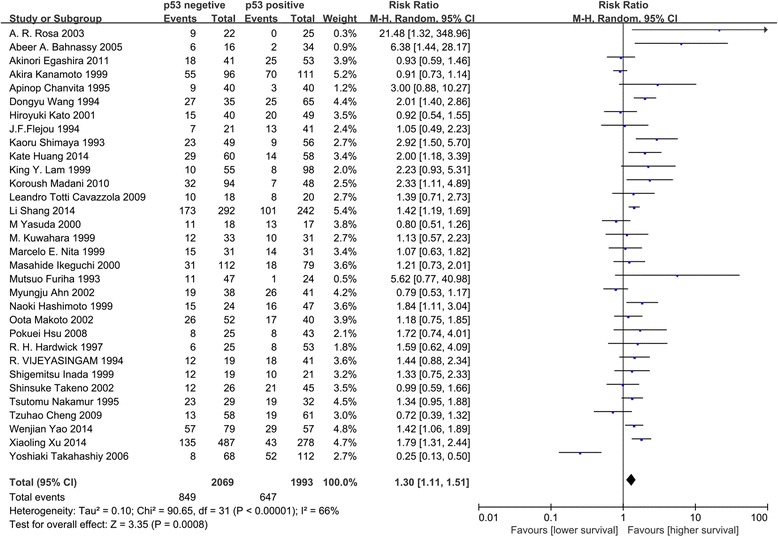
Analysis of p53 expression and survival of EC patients. Forest plot of RR for the OS included studies. Combined RR was calculated by a random model
Subgroup analyses were conducted to address the heterogeneity observed in the correlation between p53 overexpression and decreased OS in EC patients, according to histological type of EC, continent of the patients, and cut-off value of IHC (Table 3). Results showed the similar clinical significance of p53 expression in each of the two major histological types (pure ESCC cohorts: RR = 1.32, 95 % CI: 1.10–1.57, P = 0.002; pure EAC cohorts: RR = 1.61, 95 % CI: 1.05–2.47, P = 0.03). The association between p53 overexpression and poorer OS in EC patients appeared to be greater among studies involving patients from Europe and America (RR = 1.54, 95 % CI: 1.22–1.94, P = 0.0003) compared with studies involving patients from Asia (RR = 1.24, 95 % CI: 1.04–1.48, P = 0.02), and studies setting a none-10 % cut-off value (RR = 1.56, 95 % CI: 1.35–1.81, P <0.00001) compared with studies with a cut-off value of 10 % (RR = 1.18, 95 % CI: 0.96–1.45, P = 0.12).
Table 3.
Subgroup meta-analyses of p53 expression and survival according to histological type, continent and cut-off value
| Subgroup | N | Cases | Pooled RR (95 % CI) | P value | Analytical model | Heterogeneity | |
|---|---|---|---|---|---|---|---|
| I2 (%) | P value | ||||||
| Histological type | |||||||
| ESCC only | 23 | 3454 | 1.32 (1.10–1.57) | 0.002 | REM | 70 | < 0.00001 |
| EAC only | 3 | 242 | 1.61 (1.05–2.47) | 0.03 | FEM | 16 | 0.3 |
| Continent | |||||||
| Asia | 22 | 3372 | 1.24 (1.04–1.48) | 0.02 | REM | 72 | < 0.00001 |
| Europe and America | 9 | 640 | 1.54 (1.22–1.94) | 0.0003 | FEM | 30 | 0.18 |
| Cut-off value | |||||||
| 10 % | 20 | 2949 | 1.18 (0.96–1.45) | 0.12 | REM | 71 | < 0.00001 |
| None-10 % | 12 | 1113 | 1.56 (1.35–1.81) | < 0.00001 | FEM | 44 | 0.05 |
N number of studies, FEM fixed-effect model, REM random-effect model
Sensitivity analysis
To test for bias introduced by the low number of available eligible publications, we performed a sensitivity analysis. A single study in the meta-analysis was omitted from each round of analysis to investigate the influence of the individual data set of a particular study on the pooled ORs. We found that the corresponding pooled ORs were not essentially altered by the subtraction of any study (data not shown), thereby indicating that our results were statistically robust.
Publication bias
Funnel plots were performed to assess the publication bias in this meta-analysis. The shape of the funnel plots did not reveal obvious evidence of asymmetry (Fig. 4).
Fig. 4.
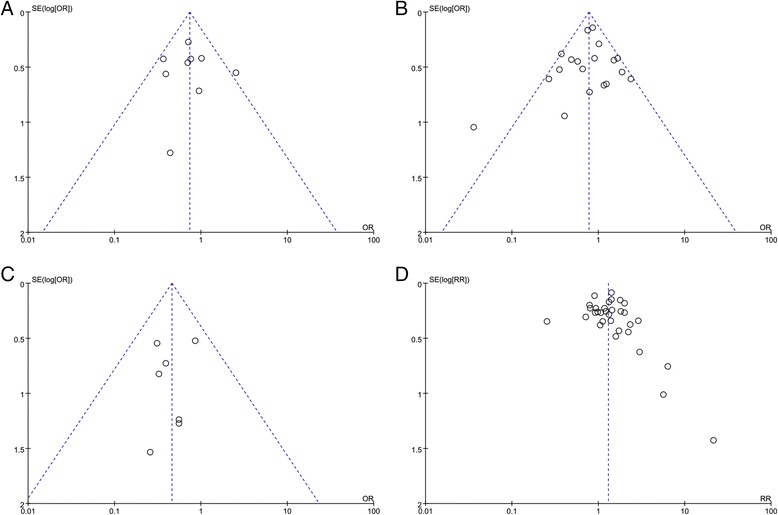
Publication bias determination using funnel plot. Funnel plots of TNM stage (a), lymph node metastasis (b), distant metastasis (c), and 5-year survival (d)
Discussion
The clinical significance and prognostic value of p53 expression in EC has recently been reported by several investigators. In the present meta-analysis, we assess the association between p53 expression and survival, as well as the clinicopathological features in EC. A total of 36 relevant studies comprised of 4577 cases were subjected to the final analysis.
The tumor suppressor gene p53 and its wild-type protein play multiple functions in regulating cell cycle progression, apoptosis, autophagy, differentiation, senescence, and DNA repair functions, as well as influences cell metabolic pathways and cytokines [17]. However, if p53 is mutated, the mutant p53 protein can accumulate in the cell nucleus [18], although in some cases, nonsense mutations or a quickly degraded mutant protein can cause lack of expression [13]. Therefore, p53 over-expression is generally associated with the inactivation of p53 [19]. Based on its functions, positive p53 expression in cancer cells may promote cell migration, invasion, and metastasis, finally leading to poor prognosis [20]. In human cancers, the p53 gene is the most commonly mutated gene; positive expression of p53 has been correlated with the clinicopathological features and prognosis of breast cancer [21], bladder cancer [22], and other types of cancer.
The results of the overall pooled analysis in the present study on the association of p53 expression with survival in EC patients suggested that positive p53 expression was significantly related to poorer OS (RR = 1.30, 95 % CI: 1.11–1.51). These findings demonstrated the significance of p53 expression in the prognosis of patients with EC and agreed with the theoretical inference that patients with positive p53 expression, which is often cause by mutation, could have poorer clinical prognosis than those with negative p53 expression. The same results have been reported in the meta-analyses of gastric cancer [23], osteosarcoma [24], hepatocellular carcinoma [25], and other tumors.
We also analyzed the relationship between p53 and clinicopathological parameters; the results showed that p53 expression was significantly associated with more advanced TNM stages (I/II vs. III/IV, OR = 0.74, 95 % CI: 0.55–0.99), lymph node metastasis (OR = 0.77, 95 % CI: 0.66–0.90), and distant metastasis (OR = 0.46, 95 % CI: 0.26–0.80). Given that a more advanced TNM stage, positive lymph node metastasis, and distant metastasis are adverse prognostic features, the present results may explain why positive p53 expression is associated with poor 5-year survival in patients with EC. However, no significant associations were observed between p53 expression and tumor size, tumor location, grade of differentiation, and depth of invasion in this study.
The current study presented several limitations that should be considered. First, the heterogeneity across studies was high for some parameters of this disease. Therefore, even if the random-effects models are used to take heterogeneity into account and several heterogeneity analyses were performed, some estimates should be interpreted with caution. The second limitation involves the lacking of a defined standardized protocol and evaluation system to measure p53 expression by IHC in various studies; several factors, such as differences in types of antibodies, concentrations, and cut-off values used may lead to potential bias. Nevertheless, the sensitivity of IHC to assess p53 mutations through protein accumulation is generally poor; some mutations, such as truncated mutant, can lead to complete loss of p53 staining and be missed by IHC [13, 26, 27]. Combining IHC and other widely applicable techniques, which could detect p53 gene aberrations, would potentially improve the accuracy of p53 as a clinical biomarker for predicting EC progression. Third, the full text of studies in this meta-analysis were published only in English or Chinese. Non-significant or negative findings are usually not published and other potential eligible studies may have been excluded; these factors also contribute to bias. We included the data of 4577 patients in this meta-analysis to provide a foundation for a larger prospective study.
Conclusions
In conclusion, our findings indicate that positive p53 expression is independently and significantly associated with poorer 5-year survival, more advanced TNM stages, lymph node metastasis, and distant metastasis in patients with EC. The expression of p53 may be a useful biomarker to predict a poorer prognosis for EC patients. However, to strengthen our findings, larger prospective studies with better standardized methods are needed to provide a comprehensive conclusion regarding the prognostic role of p53 expression in EC.
Abbreviations
BSCC, basaloid squamous cell carcinoma; CI, confidence interval; EAC, esophageal adenocarcinoma; EC, esophageal cancer; ESCC, esophageal squamous cell carcinoma; FEM, fixed-effect model; IHC, immunohistochemistry; N, number of studies; ND, not documented; OR, odds ratio; OS, overall survival; RR, risk ratio; UC, undifferentiated carcinoma
Acknowledgments
Not applicable.
Funding
This work was supported by grants from the National Natural Science Foundation of China (No.81460416, 81560399), the Ministry of Science and Technology of China (2012AA02A503), and the Scientific Research Start-up Capital for High-level Talents of Shihezi University (RCZX201444, RCZX201229).
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article.
Authors’ contributions
LW, JH and FL conceived the study. XY and ZZ searched the databases and extracted the data. LW, XY, JL and JH assembled and analyzed the data. LW and LJ gave advice on meta-analysis methodology. XY wrote the draft of the paper. LW, JH and LF revised the manuscript. All authors have read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Contributor Information
Lianghai Wang, Email: wizard@virology.com.cn.
Xiaodan Yu, Email: 840055318@qq.com.
Jing Li, Email: 826625461@qq.com.
Zhiyu Zhang, Email: 810383911@qq.com.
Jun Hou, Email: houjun229@163.com.
Feng Li, Email: lifeng7855@126.com.
References
- 1.Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 2.Chen J, Wu F, Pei HL, Gu WD, Ning ZH, Shao YJ, Huang J. Analysis of the correlation between P53 and Cox-2 expression and prognosis in esophageal cancer. Oncol Lett. 2015;10(4):2197–2203. doi: 10.3892/ol.2015.3624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Belkhiri A, El-Rifai W. Advances in targeted therapies and new promising targets in esophageal cancer. Oncotarget. 2015;6(3):1348–1358. doi: 10.18632/oncotarget.2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jemal A, Simard EP, Dorell C, Noone AM, Markowitz LE, Kohler B, Eheman C, Saraiya M, Bandi P, Saslow D, et al. Annual Report to the Nation on the Status of Cancer, 1975–2009, featuring the burden and trends in human papillomavirus(HPV)-associated cancers and HPV vaccination coverage levels. J Natl Cancer Inst. 2013;105(3):175–201. doi: 10.1093/jnci/djs491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morita M, Yoshida R, Ikeda K, Egashira A, Oki E, Sadanaga N, Kakeji Y, Yamanaka T, Maehara Y. Advances in esophageal cancer surgery in Japan: an analysis of 1000 consecutive patients treated at a single institute. Surgery. 2008;143(4):499–508. doi: 10.1016/j.surg.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 6.Peng J, Shao N, Peng H, Chen LQ. Prognostic significance of vascular endothelial growth factor expression in esophageal carcinoma: a meta-analysis. J BUON. 2013;18(2):398–406. [PubMed] [Google Scholar]
- 7.Wu J, Wu X, Liang W, Chen C, Zheng L, An H. Clinicopathological and prognostic significance of chemokine receptor CXCR4 overexpression in patients with esophageal cancer: a meta-analysis. Tumour Biol. 2014;35(4):3709–3715. doi: 10.1007/s13277-013-1490-8. [DOI] [PubMed] [Google Scholar]
- 8.Soussi T. The p53 pathway and human cancer. Br J Surg. 2005;92(11):1331–1332. doi: 10.1002/bjs.5177. [DOI] [PubMed] [Google Scholar]
- 9.Kastan MB, Onyekwere O, Sidransky D, Vogelstein B, Craig RW. Participation of p53 protein in the cellular response to DNA damage. Cancer Res. 1991;51(23 Pt 1):6304–6311. [PubMed] [Google Scholar]
- 10.Wang X, Simpson ER, Brown KA. p53: protection against tumor growth beyond effects on cell cycle and apoptosis. Cancer Res. 2015;75(23):5001–5007. doi: 10.1158/0008-5472.CAN-15-0563. [DOI] [PubMed] [Google Scholar]
- 11.Patel DD, Bhatavdekar JM, Chikhlikar PR, Patel YV, Shah NG, Ghosh N, Suthar TP, Balar DB. Clinical significance of p53, nm23, and bcl-2 in T3-4N1M0 oesophageal carcinoma: an immunohistochemical approach. J Surg Oncol. 1997;65(2):111–116. doi: 10.1002/(SICI)1096-9098(199706)65:2<111::AID-JSO7>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 12.Madani K, Zhao R, Lim HJ, Casson AG. Prognostic value of p53 mutations in oesophageal adenocarcinoma: final results of a 15-year prospective study. Eur J Cardiothorac Surg. 2010;37(6):1427–1432. doi: 10.1016/j.ejcts.2009.12.018. [DOI] [PubMed] [Google Scholar]
- 13.Davelaar AL, Calpe S, Lau L, Timmer MR, Visser M, Ten Kate FJ, Parikh KB, Meijer SL, Bergman JJ, Fockens P, et al. Aberrant TP53 detected by combining immunohistochemistry and DNA-FISH improves Barrett’s esophagus progression prediction: a prospective follow-up study. Genes Chromosomes Cancer. 2015;54(2):82–90. doi: 10.1002/gcc.22220. [DOI] [PubMed] [Google Scholar]
- 14.Pietrantonio F, De Braud F, Da Prat V, Perrone F, Pierotti MA, Gariboldi M, Fanetti G, Biondani P, Pellegrinelli A, Bossi I, et al. A review on biomarkers for prediction of treatment outcome in gastric cancer. Anticancer Res. 2013;33(4):1257–1266. [PubMed] [Google Scholar]
- 15.Baas IO, Mulder JW, Offerhaus GJ, Vogelstein B, Hamilton SR. An evaluation of six antibodies for immunohistochemistry of mutant p53 gene product in archival colorectal neoplasms. J Pathol. 1994;172(1):5–12. doi: 10.1002/path.1711720104. [DOI] [PubMed] [Google Scholar]
- 16.Lin J, Albers AE, Qin J, Kaufmann AM. Prognostic significance of overexpressed p16INK4a in patients with cervical cancer: a meta-analysis. PLoS One. 2014;9(9):e106384. doi: 10.1371/journal.pone.0106384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levine AJ, Oren M. The first 30 years of p53: growing ever more complex. Nat Rev Cancer. 2009;9(10):749–758. doi: 10.1038/nrc2723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dowell SP, Wilson PO, Derias NW, Lane DP, Hall PA. Clinical utility of the immunocytochemical detection of p53 protein in cytological specimens. Cancer Res. 1994;54(11):2914–2918. [PubMed] [Google Scholar]
- 19.Cordon-Cardo C, Dalbagni G, Saez GT, Oliva MR, Zhang ZF, Rosai J, Reuter VE, Pellicer A. p53 mutations in human bladder cancer: genotypic versus phenotypic patterns. Int J Cancer. 1994;56(3):347–353. doi: 10.1002/ijc.2910560309. [DOI] [PubMed] [Google Scholar]
- 20.Muller PA, Vousden KH, Norman JC. p53 and its mutants in tumor cell migration and invasion. J Cell Biol. 2011;192(2):209–218. doi: 10.1083/jcb.201009059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bourdon JC, Khoury MP, Diot A, Baker L, Fernandes K, Aoubala M, Quinlan P, Purdie CA, Jordan LB, Prats AC, et al. p53 mutant breast cancer patients expressing p53gamma have as good a prognosis as wild-type p53 breast cancer patients. Breast Cancer Res. 2011;13(1):R7. doi: 10.1186/bcr2811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhou X, Zhang G, Tian Y. p53 Status correlates with the risk of recurrence in non-muscle invasive bladder cancers treated with Bacillus Calmette-Guerin: a meta-analysis. PLoS One. 2015;10(3):e0119476. doi: 10.1371/journal.pone.0119476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wei K, Jiang L, Wei Y, Wang Y, Qian X, Dai Q, Guan Q. The prognostic significance of p53 expression in gastric cancer: a meta-analysis. J Cancer Res Clin Oncol. 2015;141(4):735–748. doi: 10.1007/s00432-014-1844-7. [DOI] [PubMed] [Google Scholar]
- 24.Yao D, Cai GH, Chen J, Ling R, Wu SX, Li YP. Prognostic value of p53 alterations in human osteosarcoma: a meta analysis. Int J Clin Exp Pathol. 2014;7(10):6725–6733. [PMC free article] [PubMed] [Google Scholar]
- 25.Liu J, Ma Q, Zhang M, Wang X, Zhang D, Li W, Wang F, Wu E. Alterations of TP53 are associated with a poor outcome for patients with hepatocellular carcinoma: evidence from a systematic review and meta-analysis. Eur J Cancer (Oxford, England : 1990) 2012;48(15):2328–2338. doi: 10.1016/j.ejca.2012.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fichter CD, Herz C, Munch C, Opitz OG, Werner M, Lassmann S. Occurrence of multipolar mitoses and association with Aurora-A/-B kinases and p53 mutations in aneuploid esophageal carcinoma cells. BMC Cell Biol. 2011;12:13. doi: 10.1186/1471-2121-12-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yasuda M, Kuwano H, Watanabe M, Toh Y, Ohno S, Sugimachi K. p53 expression in squamous dysplasia associated with carcinoma of the oesophagus: evidence for field carcinogenesis. Br J Cancer. 2000;83(8):1033–1038. doi: 10.1054/bjoc.2000.1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Casson AG, Tammemagi M, Eskandarian S, Redston M, McLaughlin J, Ozcelik H. p53 alterations in oesophageal cancer: association with clinicopathological features, risk factors, and survival. Mol Pathol. 1998;51(2):71–79. doi: 10.1136/mp.51.2.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rosa AR, Schirmer CC, Gurski RR, Meurer L, Edelweiss MI, Kruel CD. Prognostic value of p53 protein expression and vascular endothelial growth factor expression in resected squamous cell carcinoma of the esophagus. Dis Esophagus. 2003;16(2):112–118. doi: 10.1046/j.1442-2050.2003.00309.x. [DOI] [PubMed] [Google Scholar]
- 30.Bahnassy AA, Zekri ARN, Abdallah S, El-Shehaby AMR, Sherif GM. Human papillomavirus infection in Egyptian esophageal carcinoma: correlation with p53, p21waf, mdm2, C-erbB2 and impact on survival. Pathol Int. 2005;55(2):53–62. doi: 10.1111/j.1440-1827.2005.01804.x. [DOI] [PubMed] [Google Scholar]
- 31.Egashira A, Morita M, Yoshida R, Saeki H, Oki E, Sadanaga N, Kakeji Y, Tsujitani S, Maehara Y. Loss of p53 in esophageal squamous cell carcinoma and the correlation with survival: analyses of gene mutations, protein expression, and loss of heterozygosity in Japanese patients. J Surg Oncol. 2011;104(2):169–175. doi: 10.1002/jso.21920. [DOI] [PubMed] [Google Scholar]
- 32.Chanvitan A, Nekarda H, Casson AG. Prognostic value of DNA index, S-phase fraction and p53 protein accumulation after surgical resection of esophageal squamous-cell carcinomas in Thailand. Int J Cancer. 1995;63(3):381–386. doi: 10.1002/ijc.2910630314. [DOI] [PubMed] [Google Scholar]
- 33.Murata A, Baba Y, Watanabe M, Shigaki H, Miyake K, Karashima R, Imamura Y, Ida S, Ishimoto T, Iwagami S, et al. P53 immunohistochemical expression and patient prognosis in esophageal squamous cell carcinoma. Med Oncol. 2013;30(4):728. doi: 10.1007/s12032-013-0728-z. [DOI] [PubMed] [Google Scholar]
- 34.Wang DY, Xiang YY, Tanaka M, Li XR, Li JL, Shen Q, Sugimura H, Kino I. High prevalence of p53 protein overexpression in patients with esophageal cancer in Linxian, China and its relationship to progression and prognosis. Cancer. 1994;74(12):3089–3096. doi: 10.1002/1097-0142(19941215)74:12<3089::AID-CNCR2820741205>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 35.Kato H, Yoshikawa M, Miyazaki T, Nakajima M, Fukai Y, Tajima K, Masuda N, Tsukada K, Fukuda T, Nakajima T, et al. Expression of p53 protein related to smoking and alcoholic beverage drinking habits in patients with esophageal cancers. Cancer Lett. 2001;167(1):65–72. doi: 10.1016/S0304-3835(01)00461-X. [DOI] [PubMed] [Google Scholar]
- 36.Flejou JF, Paraf F, Potet F, Muzeau F, Fekete F, Henin D. p53 protein expression in Barrett’s adenocarcinoma: a frequent event with no prognostic significance. Histopathology. 1994;24(5):487–489. doi: 10.1111/j.1365-2559.1994.tb00561.x. [DOI] [PubMed] [Google Scholar]
- 37.Shimaya K, Shiozaki H, Inoue M, Tahara H, Monden T, Shimano T, Mori T. Significance of p53 expression as a prognostic factor in oesophageal squamous cell carcinoma. Virchows Arch A Pathol Anat Histopathol. 1993;422(4):271–276. doi: 10.1007/BF01608335. [DOI] [PubMed] [Google Scholar]
- 38.Huang K, Chen L, Zhang J, Wu Z, Lan L, Wang L, Lu B, Liu Y. Elevated p53 expression levels correlate with tumor progression and poor prognosis in patients exhibiting esophageal squamous cell carcinoma. Oncol Lett. 2014;8(4):1441–1446. doi: 10.3892/ol.2014.2343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lam KY, Law S, Tin L, Tung PH, Wong J. The clinicopathological significance of p21 and p53 expression in esophageal squamous cell carcinoma: an analysis of 153 patients. Am J Gastroenterol. 1999;94(8):2060–2068. doi: 10.1111/j.1572-0241.1999.01278.x. [DOI] [PubMed] [Google Scholar]
- 40.Chyczewski L, Kozlowski M, Niklinski J, Szyszko J, Laudanski J, Niklinska W. p53 protein expression in resected invasive esophageal cancer. Neoplasma. 1999;46(3):150–155. [PubMed] [Google Scholar]
- 41.Cavazzola LT, Rosa AR, Schirmer CC, Gurski RR, Telles JP, Mielke F, Meurer L, Edelweiss MI, Kruel CD. Immunohistochemical evaluation for P53 and VEGF (Vascular Endothelial Growth Factor) is not prognostic for long term survival in end stage esophageal adenocarcinoma. Rev Col Bras Cir. 2009;36(1):24–34. doi: 10.1590/S0100-69912009000100007. [DOI] [PubMed] [Google Scholar]
- 42.Shang L, Liu HJ, Hao JJ, Jiang YY, Shi F, Zhang Y, Cai Y, Xu X, Jia XM, Zhan QM, et al. A panel of overexpressed proteins for prognosis in esophageal squamous cell carcinoma. PLoS One. 2014;9(10):e111045. doi: 10.1371/journal.pone.0111045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kuwahara M, Hirai T, Yoshida K, Yamashita Y, Hihara J, Inoue H, Toge T. p53, p21(Waf1/Cip1) and cyclin D1 protein expression and prognosis in esophageal cancer. Dis Esophagus. 1999;12(2):116–119. doi: 10.1046/j.1442-2050.1999.00034.x. [DOI] [PubMed] [Google Scholar]
- 44.Nita ME, Nagawa H, Tominaga O, Tsuno N, Hatano K, Kitayama J, Tsuruo T, Domene CE, Muto T. p21Waf1/Cip1 expression is a prognostic marker in curatively resected esophageal squamous cell carcinoma, but not p27Kip1, p53, or Rb. Ann Surg Oncol. 1999;6(5):481–488. doi: 10.1007/s10434-999-0481-x. [DOI] [PubMed] [Google Scholar]
- 45.Ikeguchi M, Oka S, Gomyo Y, Tsujitani S, Maeta M, Kaibara N. Combined analysis of p53 and retinoblastoma protein expressions in esophageal cancer. Ann Thorac Surg. 2000;70(3):913–917. doi: 10.1016/S0003-4975(00)01719-7. [DOI] [PubMed] [Google Scholar]
- 46.Furihata M, Ohtsuki Y, Ogoshi S, Takahashi A, Tamiya T, Ogata T. Prognostic significance of human papillomavirus genomes (type-16, -18) and aberrant expression of p53 protein in human esophageal cancer. Int J Cancer. 1993;54(2):226–230. doi: 10.1002/ijc.2910540211. [DOI] [PubMed] [Google Scholar]
- 47.Ahn MJ, Jang SJ, Park YW, Choi JH, Oh HS, Lee CB, Paik HK, Park CK. Clinical prognostic values of vascular endothelial growth factor, microvessel density, and p53 expression in esophageal carcinomas. J Korean Med Sci. 2002;17(2):201–207. doi: 10.3346/jkms.2002.17.2.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hashimoto N, Tachibana M, Dhar DK, Yoshimura H, Nagasue N. Expression of p53 and RB proteins in squamous cell carcinoma of the esophagus: their relationship with clinicopathologic characteristics. Ann Surg Oncol. 1999;6(5):489–494. doi: 10.1007/s10434-999-0489-2. [DOI] [PubMed] [Google Scholar]
- 49.Makoto O, Takeda A, Ting-Leig L, Shinnichi O, Hisahiro M, Yutaka F, Yoshihiro N, Kobayashi S, Gunji Y, Suzuki T, et al. Prognostic significance of thymidine phosphorylase and p53 co-expression in esophageal squamous cell carcinoma. Oncol Rep. 2002;9(1):23–28. [PubMed] [Google Scholar]
- 50.Hsu PK, Li AF, Wang YC, Hsieh CC, Huang MH, Hsu WH, Hsu HS. Reduced membranous beta-catenin protein expression is associated with metastasis and poor prognosis in squamous cell carcinoma of the esophagus. J Thorac Cardiovasc Surg. 2008;135(5):1029–1035. doi: 10.1016/j.jtcvs.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 51.Kanamoto A, Kato H, Tachimori Y, Watanabe H, Nakanishi Y, Kondo H, Yamaguchi H, Gotoda T, Muro K, Matsumura Y. No prognostic significance of p53 expression in esophageal squamous cell carcinoma. J Surg Oncol. 1999;72(2):94–98. doi: 10.1002/(SICI)1096-9098(199910)72:2<94::AID-JSO10>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 52.Hardwick RH, Barham CP, Ozua P, Newcomb PV, Savage P, Powell R, Rahamin J, Alderson D. Immunohistochemical detection of p53 and c-erbB-2 in oesophageal carcinoma; no correlation with prognosis. Eur J Surg Oncol. 1997;23(1):30–35. doi: 10.1016/S0748-7983(97)80139-4. [DOI] [PubMed] [Google Scholar]
- 53.Vijeyasingam R, Darnton SJ, Jenner K, Allen CA, Billingham C, Matthews HR. Expression of p53 protein in oesophageal carcinoma: clinicopathological correlation and prognostic significance. Br J Surg. 1994;81(11):1623–1626. doi: 10.1002/bjs.1800811120. [DOI] [PubMed] [Google Scholar]
- 54.Inada S, Koto T, Futami K, Arima S, Iwashita A. Evaluation of malignancy and the prognosis of esophageal cancer based on an immunohistochemical study (p53, E-cadherin, epidermal growth factor receptor) Surg Today. 1999;29(6):493–503. doi: 10.1007/BF02482343. [DOI] [PubMed] [Google Scholar]
- 55.Nakamura T, Ide H, Eguchi R, Hayashi K, Hanyu F, Nagasako K, Yukawa M, Asaka K, Fujimori T, Maeda S. Expression of p53 protein related to human papillomavirus and DNA ploidy in superficial esophageal carcinoma. Surg Today. 1995;25(7):591–597. doi: 10.1007/BF00311431. [DOI] [PubMed] [Google Scholar]
- 56.Cheng TH, Hsu PK, Li AF, Hung IC, Huang MH, Hsu HS. Correlation of p53, MDM2 and p14(ARF) protein expression in human esophageal squamous cell carcinoma. J Cancer Res Clin Oncol. 2009;135(11):1577–1582. doi: 10.1007/s00432-009-0605-5. [DOI] [PubMed] [Google Scholar]
- 57.Yao W, Qin X, Qi B, Lu J, Guo L, Liu F, Liu S, Zhao B. Association of p53 expression with prognosis in patients with esophageal squamous cell carcinoma. Int J Clin Exp Pathol. 2014;7(10):7158–7163. [PMC free article] [PubMed] [Google Scholar]
- 58.Takeno S, Noguchi T, Kikuchi R, Uchida Y, Yokoyama S, Muller W. Prognostic value of cyclin B1 in patients with esophageal squamous cell carcinoma. Cancer. 2002;94(11):2874–2881. doi: 10.1002/cncr.10542. [DOI] [PubMed] [Google Scholar]
- 59.Xu XL, Zheng WH, Tao KY, Li XX, Xu WZ, Wang Y, Zhu SM, Mao WM. p53 is an independent prognostic factor in operable esophageal squamous cell carcinoma: a large-scale study with a long follow-up. Med Oncol. 2014;31(11):1–7. doi: 10.1007/s12032-014-0257-4. [DOI] [PubMed] [Google Scholar]
- 60.Takahashi Y, Noguchi T, Takeno S, Kimura Y, Okubo M, Kawahara K. Reduced expression of p63 has prognostic implications for patients with esophageal squamous cell carcinoma. Oncol Rep. 2006;15(2):323–328. [PubMed] [Google Scholar]
- 61.Goukon Y, Sasano H, Nishihira T, Nagura H, Mori S. p53 overexpression in human esophageal carcinoma: A correlation with tumor DNA ploidy and two parameter flow cytometric study. Anticancer Res. 1994;14(3 B):1305–1312. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets supporting the conclusions of this article are included within the article.


