Abstract
OBJECTIVE
To evaluate the potential impact and value of applications (e.g., ordering levels, storage capacity, transportation capacity, distribution frequency) of data from demand forecasting systems implemented in a lower-income country’s vaccine supply chain with different levels of population change to urban areas.
MATERIALS AND METHODS
Using our software, HERMES, we generated a detailed discrete event simulation model of Niger’s entire vaccine supply chain, including every refrigerator, freezer, transport, personnel, vaccine, cost, and location. We represented the introduction of a demand forecasting system to adjust vaccine ordering that could be implemented with increasing delivery frequencies and/or additions of cold chain equipment (storage and/or transportation) across the supply chain during varying degrees of population movement.
RESULTS
Implementing demand forecasting system with increased storage and transport frequency increased the number of successfully administered vaccine doses and lowered the logistics cost per dose up to 34%. Implementing demand forecasting system without storage/transport increases actually decreased vaccine availability in certain circumstances.
DISCUSSION
The potential maximum gains of a demand forecasting system may only be realized if the system is implemented to both augment the supply chain cold storage and transportation. Implementation may have some impact but, in certain circumstances, may hurt delivery. Therefore, implementation of demand forecasting systems with additional storage and transport may be the better approach. Significant decreases in the logistics cost per dose with more administered vaccines support investment in these forecasting systems.
CONCLUSION
Demand forecasting systems have the potential to greatly improve vaccine demand fulfillment, and decrease logistics cost/dose when implemented with storage and transportation increases direct vaccines. Simulation modeling can demonstrate the potential health and economic benefits of supply chain improvements.
INTRODUCTION
Recent years have seen increasing interest in introducing demand forecasting systems to lower-income country supply chains to help anticipate demand for vaccines, to advise ordering, to allocate infrastructure, and to help supply meet demand [1]. In many lower-income countries, vaccine stockouts (i.e., immunization locations lacking vaccines to meet demand) continue to occur [2]. Demand forecasting systems prevent stockouts when substantial changes in vaccine demand occur (e.g., natural disasters, changing labor demand, and political unrest). Without demand forecasting systems, those managing a vaccine supply chain may have difficulty predicting changes in demand at immunization locations and consequently making the appropriate infrastructure (CCE) and supply compensatory changes [3]. Recently, various forecasting systems (e.g., Logistimo, Pipeline, SIGMED) have emerged to forecast demand [4–7]. One method is to track demand by having health workers enter stock levels or immunizations, and then extrapolate the trends in recent, past demand to anticipate upcoming demand. Another method is to record and store pregnancy and birth data, and then extrapolate when mothers and children reach the appropriate ages for each type of immunization. Having information systems that can help anticipate demand could theoretically allow workers to make adjustments in ordering, allocation of fixed and movable cold chain equipment, and transport frequencies to better tailor supply to demand.
However, installing and maintaining such systems is not trivial, especially in lower-income countries with limited resources [8]. Additionally, data collection is only successful if used to make appropriate changes. These countries face significant challenges in successful adoption of demand forecasting systems including the perceived burden of use, unfamiliarity, engagement of leadership, high cost for installation and maintenance, unreliable electricity in the supply chain, and lack of universal data standards [9–12]. Some systems, such as mobile phone-based systems, can overcome some of these challenges, such as unreliable power grids [9]. However, other challenges remain. Therefore, establishing the value of a demand forecasting system in public health supply chains is necessary for successful implementation.
Our Logistics Modeling Team developed a computational model of Niger’s vaccine supply chain using HERMES (Highly Extensible Resource for Modeling Supply Chains). Using this model, we evaluated the potential impact of applications of data from demand forecasting systems implemented in a lower-income country’s vaccine supply chain; specifically which applications (e.g., ordering levels, storage capacity, transportation capacity, distribution frequency) increased vaccine availability and had the most value when there were different levels of population change to urban areas.
MATERIALS AND METHODS
HERMES and the Niger Vaccine Supply Chain
Our team utilized HERMES, a software platform developed in Python using features provided by the SimPy package, to implement a detailed discrete event simulation model of the Niger World Health Organization (WHO) Expanded Programme on Immunization (EPI) vaccine supply chain. This virtual representation, described in detail in previous publications, represents the flow of all EPI vaccines upon entering the country through each storage location to vaccine administration locations over the course of one year of vaccine distribution in Niger [3, 13–19]. Every vaccine vial, order, and trip is individually tracked and reported. Each cold device has finite storage capacity that is a function of its size and utilization rate (percentage of physical space within the device usable for storage). Vaccine shipments between locations occur at frequencies specific to the transportation route and guided by country policies (Figure 1). Shipment size cannot exceed the available storage space in a vehicle or cold device(s). If demand for vaccine vials exceeds storage space, additional trips occur if vaccines are available and in line with country policies.
Figure 1.
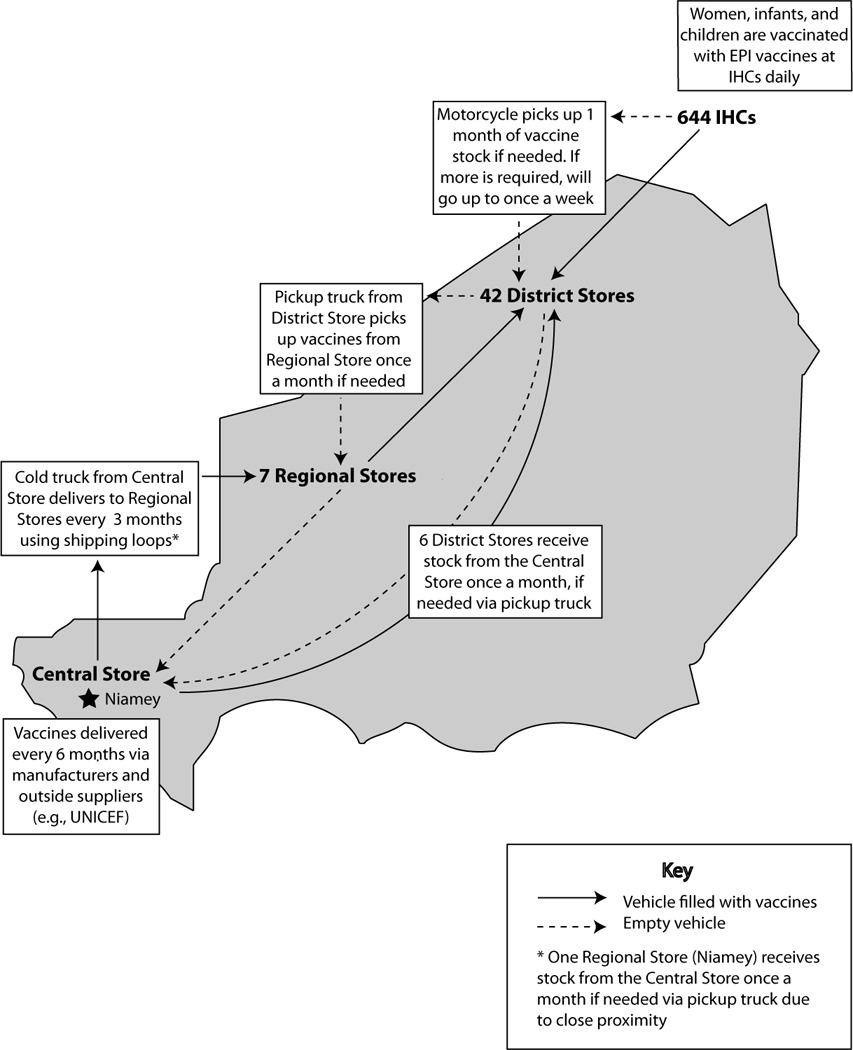
The Niger Supply Chain
Vaccine Demand
In the model, patients arrive for vaccination sessions at integrated health clinics (IHCs). These populations are derived from the 2005 Nigerien census and scaled to match projected 2012 pregnant woman/newborn/infant cohorts to yield a 2012 population estimate of how many in each area will need vaccines each month [20]. The model assumes a patient presents to their nearest IHC for immunization when they reach the appropriate ages for relevant vaccines. Vaccine orders are calculated based on how many doses, and thus vials, are predicted to be required for each session based on this census-based population estimate and with a 25% vial buffer added to stock levels. The 25% ordering buffer used in Niger and many other countries allows for some variation in population demand in the system, compared to the baseline census population. The six different vaccines given at IHCs in Niger and their schedules are shown in Table 1 [20]. All doses in multi-doses vials are not necessarily used; Bacillus Calmette-Guerin, Measles, and Yellow Fever vials are discarded six hours after opening, while Oral Polio Vaccine and Tetanus Toxoid vials can be used for 28 days after opening. Unused doses in partially used vials are quantified as open vial waste (OVW), which is the percentage of doses in a multi-dose vial that are unused and wasted due to the vial being opened and subsequently discarded at expiration.
Table 1.
Niger EPI Vaccine Characteristics
| Expanded Programme on Immunization (EPI) Vaccines |
Immunization schedule | Doses per person |
Doses per vial |
|---|---|---|---|
| Bacillus Calmette-Guérin (BCG) | Birth | 1 | 20 |
| Measles (M) | 9 months | 1 | 10 |
| Oral Polio Vaccine (OPV) | Birth, 6, 10, 14 weeks | 4 | 20 |
| Diphtheria-tetanus-pertussis - Hepatitis B - Haemophilus influenzae type B (DTP-HepB- Hib) |
6, 10, 14 weeks | 3 | 1 |
| Tetanus Toxoid (TT) | 1st contact, 4 weeks | 2 | 10 |
| Yellow Fever (YF) | 9 months | 1 | 10 |
Supply Chain Performance Indicators
In these simulations, we reported the following main outcomes: vaccine availability, doses administered, missed vaccination opportunities, total annual logistics costs, and logistics cost per dose administered. The logistics costs accrued (2012 USD) were calculated for storage equipment (energy usage, maintenance, depreciation), transportation (fuel usage, vehicle maintenance, depreciation, per diems), buildings (overhead, depreciation), and labor (personnel salaries). The calculations detailed below:
Experiments
Experiments explored the impact, and value over one year, of implementing a demand forecasting system to adjust ordering quantities of vaccines when population levels increase for urban clinics and decrease for rural clinics in Niger rather than relying on census-based population estimates. Increasing delivery frequencies and/or adding cold chain equipment (storage and/or transportation) across the supply chain could be implemented as well. Populations of pregnant women, newborns, and infants (0–11 months) were redistributed from rural districts in Niger to the 12 districts serving the largest cities for one year [21]. The redistribution decreased the population demand at the rural IHCs by a specific degree of movement (10%, 30%, or 50%) and proportionately relocated this population across all IHCs in the 12 urban districts.
Data from the demand forecasting system could be implemented to adjust ordering or increases of storage capacity, transportation capacity, transportation frequency, or a combination of the four. Increasing storage capacity added 7,192L of new cold storage capacity at facilities and increasing transportation capacity added 9,004L of new transportation capacity across the supply chain. These increases were in place for the full year to relieve bottlenecks based on need without population changes, as infrastructure improvements require implementation time. Increasing transportation frequency allowed deliveries up to monthly to Regional Stores, weekly to District Stores, and daily to IHCs. Each experiment consisted of running multiple realizations over one year with the average result reported. In all cases, the standard deviation was within 1% of the mean.
RESULTS
No Demand Forecasting System
Assuming no population changes and no demand forecasting system, the baseline Niger vaccine supply chain was unable to provide vaccines for a significant portion of its population, with a 69% average EPI vaccine availability (Table 2). At baseline, there is no demand forecasting system, leading to vaccine availability of 69%. The key constraints identified in the supply chain were storage and transport. Annual logistics operating costs were $1,893,422 and $0.25/dose administered.
Table 2.
Introducing a Demand Forecasting System with Single Concomitant Measures
| % of Rural Population Relocated to Urban Areas | ||||
|---|---|---|---|---|
| 0% | 10% | 30% | 50% | |
| No Demand Forecasting System | ||||
| Total | ||||
| Availability | 69% | 72% | 68% | 59% |
| Doses Given* | 7.54 | 7.87 | 7.34 | 6.42 |
| Doses Missed* | 3.31 | 2.99 | 3.52 | 4.44 |
| Urban/Rural | ||||
| Availability | 63% / 72% | 61% / 79% | 50% / 85% | 42% / 91% |
| Doses Given* | 2.05 / 5.49 | 2.46 / 5.41 | 2.79 / 4.56 | 2.97 / 3.45 |
| Doses Missed* | 1.19 / 2.11 | 1.55 / 1.44 | 2.74 / 0.78 | 4.08 / 0.36 |
| Demand Forecasting System | ||||
| Total | ||||
| Availability | N/A | 72% | 68% | 56% |
| Doses Given* | N/A | 7.87 | 7.35 | 6.14 |
| Doses Missed* | N/A | 3.00 | 3.51 | 4.72 |
| Urban/Rural | ||||
| Availability | N/A | 60% / 79% | 49% / 87% | 37% / 92% |
| Doses Given* | N/A | 2.41 / 5.45 | 2.71 / 4.64 | 2.62 / 3.52 |
| Doses Missed* | N/A | 1.59 / 1.41 | 2.82 / 0.69 | 4.42 / 0.30 |
| Demand Forecasting System & Storage Capacity | ||||
| Total | ||||
| Availability | N/A | 90% | 80% | 67% |
| Doses Given* | N/A | 9.75 | 8.73 | 7.24 |
| Doses Missed* | N/A | 1.12 | 2.14 | 3.62 |
| Urban/Rural | ||||
| Availability | N/A | 78% / 96% | 62% / 99% | 49% / 100% |
| Doses Given* | N/A | 3.14 / 6.61 | 3.44 / 5.28 | 3.43 / 3.80 |
| Doses Missed* | N/A | 0.87 / 0.25 | 2.08 / 0.05 | 3.62 / 0.01 |
| Demand Forecasting System & Transport Capacity | ||||
| Total | ||||
| Availability | N/A | 77% | 74% | 64% |
| Doses Given* | N/A | 8.42 | 8.02 | 6.95 |
| Doses Missed* | N/A | 2.45 | 2.84 | 3.90 |
| Urban/Rural | ||||
| Availability | N/A | 71% / 81% | 61% / 87% | 49% / 92% |
| Doses Given* | N/A | 2.84 / 5.58 | 3.39 / 4.63 | 3.45 / 3.50 |
| Doses Missed* | N/A | 1.17 / 1.28 | 2.14 / 0.71 | 3.60 / 0.31 |
| Demand Forecasting System & Increased Transport Frequency | ||||
| Total | ||||
| Availability | N/A | 98% | 97% | 92% |
| Doses Given* | N/A | 10.66 | 10.50 | 10.03 |
| Doses Missed* | N/A | 0.21 | 0.37 | 0.83 |
| Urban/Rural | ||||
| Availability | N/A | 96% / 99% | 94% / 99% | 88% / 99% |
| Doses Given* | N/A | 3.86 / 6.80 | 5.20 / 5.30 | 6.24 / 3.79 |
| Doses Missed* | N/A | 0.14 / 0.06 | 0.33 / 0.04 | 0.83 / 0.02 |
Number of doses in millions
When 30% and 50% of the rural population relocated, fewer vaccinations were successfully given, with decreased vaccine availabilities in both total and urban areas and increased MVOs (Table 2) with the larger inaccuracy in ordering. Rural vaccine availabilities increased with reduced demand at these locations.
However, when only 10% of the rural population moved to urban areas, vaccine availability increased in all areas with a decrease in MVOs (Figure 2). The 25% ordering buffer of extra vaccine vials provided sufficient compensation, despite increased ordering inaccuracy and demand at urban locations. Also, this reduced OVW, allowing more doses to be used from multi-dose vials. More doses were used from each vial, but only one vial per vaccination session was still needed for Measles, BCG, and Yellow Fever multi-dose vaccines, which previously had high open vial wastage. Logistics costs/dose administered increased as the percentage of rural population moved increased (Table 4).
Figure 2.
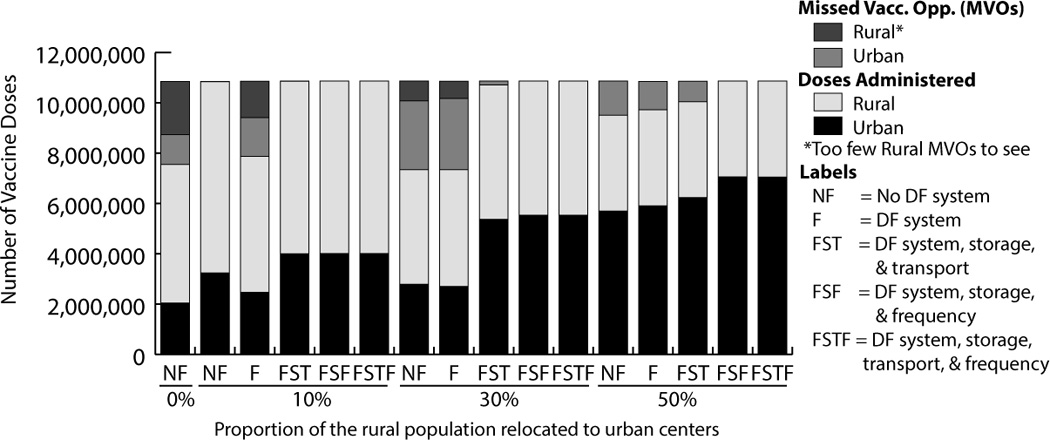
Vaccinations Administered with Demand Forecasting (DF) System
Table 4.
Logistics Costs with Introduction of Demand Forecasting Systems
| % of Rural Population Relocated to Urban Areas | ||||||||
|---|---|---|---|---|---|---|---|---|
| 0% | 10% | 30% | 50% | |||||
| No Demand Forecasting System | ||||||||
| Total Logistics Cost | $ | 1,893,422 | $ | 1,843,681 | $ | 1,808,060 | $ | 1,736,710 |
| Doses Given* | 7.54 | 7.87 | 7.35 | 6.42 | ||||
| Logistics Cost Per Dose | $ | 0.25 | $ | 0.23 | $ | 0.24 | $ | 0.27 |
| Demand Forecasting System | ||||||||
| Total Logistics Cost | N/A | $ | 1,825,166 | $ | 1,768,370 | $ | 1,709,372 | |
| Doses Given* | N/A | 7.87 | 7.35 | 6.14 | ||||
| Logistics Cost Per Dose | N/A | $ | 0.23 | $ | 0.24 | $ | 0.28 | |
| Demand Forecasting System & Storage Capacity | ||||||||
| Total Logistics Cost | N/A | $ | 1,958,177 | $ | 1,897,616 | $ | 1,855,844 | |
| Doses Given* | N/A | 9.75 | 8.73 | 7.24 | ||||
| Logistics Cost Per Dose | N/A | $ | 0.20 | $ | 0.22 | $ | 0.26 | |
| Demand Forecasting System & Transport Capacity | ||||||||
| Total Logistics Cost | N/A | $ | 1,970,992 | $ | 1,942,871 | $ | 1,947,235 | |
| Doses Given* | N/A | 8.42 | 8.02 | 6.95 | ||||
| Logistics Cost Per Dose | N/A | $ | 0.23 | $ | 0.24 | $ | 0.28 | |
| Demand Forecasting System & Transport Frequency | ||||||||
| Total Logistics Cost | N/A | $ | 1,900,409 | $ | 1,905,445 | $ | 1,914,718 | |
| Doses Given* | N/A | 10.66 | 10.50 | 10.03 | ||||
| Logistics Cost Per Dose | N/A | $ | 0.18 | $ | 0.18 | $ | 0.19 | |
| Demand Forecasting System, Storage Capacity, & Transport Capacity | ||||||||
| Total Logistics Cost | N/A | $ | 1,949,219 | $ | 2,009,821 | $ | 2,068,158 | |
| Doses Given* | N/A | 10.86 | 10.71 | 10.04 | ||||
| Logistics Cost Per Dose | N/A | $ | 0.18 | $ | 0.19 | $ | 0.21 | |
| Demand Forecasting System, Storage Capacity, & Transport Frequency | ||||||||
| Total Logistics Cost | N/A | $ | 1,956,329 | $ | 1,958,990 | $ | 1,986,062 | |
| Doses Given* | N/A | 10.87 | 10.87 | 10.86 | ||||
| Logistics Cost Per Dose | N/A | $ | 0.18 | $ | 0.18 | $ | 0.19 | |
| Demand Forecasting System, Transport Capacity, & Transport Frequency | ||||||||
| Total Logistics Cost | N/A | $ | 2,077,285 | $ | 2,102,022 | $ | 2,141,215 | |
| Doses Given* | N/A | 10.59 | 10.44 | 10.03 | ||||
| Logistics Cost Per Dose | N/A | $ | 0.20 | $ | 0.20 | $ | 0.21 | |
| Demand Forecasting System, Storage Capacity, Transport Capacity, & Transport Frequency | ||||||||
| Total Logistics Cost | N/A | $ | 2,039,842 | $ | 2,076,403 | $ | 2,149,395 | |
| Doses Given* | N/A | 10.87 | 10.87 | 10.86 | ||||
| Logistics Cost Per Dose | N/A | $ | 0.19 | $ | 0.19 | $ | 0.20 | |
Number of doses in millions
Demand Forecasting Alone
Use of a demand forecasting system to only adjust ordering did not improve the countrywide performance of the storage-constrained vaccine supply chain, and at times worsened it. Overall vaccine availability decreased with the use of a demand forecasting system when both 30% and 50% of the rural population relocated (Figure 2, Table 2). Logistics costs/dose administered were similar to those with no demand forecasting system (Table 4).
Increasing Storage Capacity
Increasing storage capacity with ordering adjustment from the demand forecasting system did not improve the performance of the vaccine supply chain compared to only adding storage capacity because there were still significant transportation bottlenecks. Overall vaccine availability increased by 20–29% across scenarios compared to no interventions but decreased slightly (0–6%) compared to only increasing storage (Table 2). Logistics cost/dose decreased 8–16% as the percentage of rural population moved increased.
Increasing Transportation Capacity
Overall vaccine availability increased with ordering adjustment plus increased transportation capacity compared to no interventions but decreased slightly compared to only increasing transportation capacity. Improvements were less than when storage capacity was added with ordering adjustment from the demand forecasting system. Logistics cost/dose were similar to only adjusting ordering.
Increasing Transportation Frequency
Implementing a demand forecasting system to adjust ordering with increased transportation frequency increased vaccine availability to >92% for all scenarios but had slightly lower vaccine coverage for multi-dose vials than scenarios only increasing transportation frequency because of unaddressed storage bottlenecks. Increasing transportation frequency alone increased vaccine availability more and had lower logistics cost/dose ($0.18–$0.19) than any other single factor intervention.
Increasing Storage and Transportation Capacities
Utilizing the demand forecasting system to adjust ordering with increased storage and transport capacities yielded 92–100% vaccine availability. When 10% of the rural population moved, overall vaccine availability increased by 38% compared to no demand forecasting system (Table 3). Even when 50% of the rural population moved, overall vaccine availability was 92%. Logistics cost/dose administered decreased by 36% compared to no demand forecasting system.
Table 3.
Introducing a Demand Forecasting System with Multiple Concomitant Measures
| % of Rural Population Relocated to Urban Areas | ||||
|---|---|---|---|---|
| 0% | 10% | 30% | 50% | |
| Demand Forecasting System, Storage Capacity, & Transport Capacity | ||||
| Total | ||||
| Availability | N/A | 100% | 99% | 92% |
| Doses Given* | N/A | 10.86 | 10.71 | 10.04 |
| Doses Missed* | N/A | 0.00 | 0.16 | 0.82 |
| Urban/Rural | ||||
| Availability | N/A | 100% / 100% | 97% / 100% | 88% / 100% |
| Doses Given* | N/A | 4.00 / 6.86 | 5.37 / 5.34 | 6.23 / 3.81 |
| Doses Missed* | N/A | 0.00 / 0.00 | 0.16 / 0.00 | 0.82 / 0.00 |
| Demand Forecasting System, Storage Capacity, & Transport Frequency | ||||
| Total | ||||
| Availability | N/A | 100% | 100% | 100% |
| Doses Given* | N/A | 10.87 | 10.87 | 10.86 |
| Doses Missed* | N/A | 0.00 | 0.00 | 0.00 |
| Urban/Rural | ||||
| Availability | N/A | 100% / 100% | 100% / 100% | 100% / 100% |
| Doses Given* | N/A | 4.01 / 6.86 | 5.53 / 5.34 | 7.05 / 3.81 |
| Doses Missed* | N/A | 0.00 / 0.00 | 0.00 / 0.00 | 0.00 / 0.00 |
| Demand Forecasting System, Transport Capacity, & Transport Frequency | ||||
| Total | ||||
| Availability | N/A | 97% | 96% | 92% |
| Doses Given* | N/A | 10.59 | 10.44 | 10.03 |
| Doses Missed* | N/A | 0.28 | 0.43 | 0.83 |
| Urban/Rural | ||||
| Availability | N/A | 95% / 99% | 93% / 99% | 89% / 99% |
| Doses Given* | N/A | 3.83 / 6.76 | 5.16 / 5.28 | 6.25 / 3.78 |
| Doses Missed* | N/A | 0.18 / 0.10 | 0.37 / 0.05 | 0.80 / 0.03 |
| Demand Forecasting System, Storage Capacity, Transport Capacity, & Transport Frequency | ||||
| Total | ||||
| Availability | N/A | 100% | 100% | 100% |
| Doses Given* | N/A | 10.87 | 10.87 | 10.86 |
| Doses Missed* | N/A | 0.00 | 0.00 | 0.00 |
| Urban/Rural | ||||
| Availability | N/A | 100% / 100% | 100% / 100% | 100% / 100% |
| Doses Given* | N/A | 4.01 / 6.86 | 5.53 / 5.34 | 7.05 / 3.81 |
| Doses Missed* | N/A | 0.00 / 0.00 | 0.00 / 0.00 | 0.00 / 0.00 |
Number of doses in millions
Only adding storage and transport capacities resulted in lower vaccine availabilities than adding storage and transport capacities with the demand forecasting system ranging from 88–100% as 0–50% of rural population moved. Logistics costs/dose administered were slightly higher than when the ordering was adjusted by the demand forecasting system with increased storage and transportation frequency.
Increasing Storage Capacity and Transport Frequency
Using the demand forecasting system to adjust ordering with both increased storage capacity and transportation frequency increased vaccine availability by 38–77% while decreasing logistics cost/dose by 29–52% compared to no intervention across all scenarios. 100% vaccine availability occurred for all scenarios with both storage and transport bottlenecks addressed. For 30% and 50% rural population movement, total logistics costs ($1,958,990 and $1,986,062, respectively) and cost/dose ($0.18) were lower for this scenario than any other intervention. Increasing storage capacity and transportation frequency without adjusting ordering led to 99–100% vaccine availability.
Increasing Transportation Capacity and Transportation Frequency
Implementing a demand forecasting system to adjust ordering with increased transportation capacity and frequency increased, was similar to only increasing transport frequency with vaccine availability >92% for all scenarios but had slightly lower vaccine coverage for multi-dose vials than without the demand forecasting system because of storage bottlenecks. Total logistics costs and logistics cost/dose were higher than only increasing transportation frequency despite similar vaccine availabilities.
Increasing Storage Capacity, Transport Capacity, and Transportation Frequency
Using the demand forecasting system to adjust ordering with increased storage capacity, transport capacity, and transportation frequency resulted in 100% vaccine availability occurred for all scenarios, but had higher costs/dose than other interventions of similar efficacy.
DISCUSSION
Demand forecasting systems can guide appropriate interventions that successfully increase vaccine coverage and decrease logistics cost/dose when populations relocate to urban areas. Demand forecasting systems are most successful when used to adjust ordering quantities, increase storage capacity, and increase transportation frequency with >99% vaccine availabilities and up to 34% decreases in costs. Vaccine availability increased from 69% to 100% at baseline when the demand forecasting system was implemented with increases in storage and transportation frequency. With 50% rural population movement, vaccine availability increased from 59% to 100%, indicating that these concomitant changes allowed the supply chain to support a substantial shift in population. Significant decreases (34%) in the logistics cost/dose from implementing the demand forecasting system with additional storage capacity and increased transport help make the case for investment in these forecasting systems. If resources are limited and only a single adjustment can be made to the supply chain, then transportation frequency should be increased. Increasing transportation had the highest vaccine availabilities with lowest costs.
Certainly, implementing a demand forecasting system in a supply chain can provide many potential benefits to vaccine delivery, but applying its data to only a single aspect of the supply chain (e.g., a demand forecasting system only adjusting the allocation of vaccines) could actually lead to negative results. More successful information systems integrate collected data between relevant health programs and policy makers to maximize impact [22]. As our study suggests, the most significant gains in vaccine availability and decreases in logistics cost/dose from implementing a demand forecasting system may only be realized if there are simultaneous adjustments in both storage and transport.
Only implementing the demand forecasting system to adjust ordering or only changing storage or transport with ordering changes actually decreased vaccine availability compared to similar scenarios when ordering wasn’t adjusted because the storage and transport constrained system could not effectively accommodate shifts in vaccine flow to fulfill demand. In essence, by redirecting vaccines, the demand forecasting system without adjusted storage and transport shifted or created new bottlenecks in the system. This would be analogous to introducing new traffic lights to redirect traffic without first ensuring that the roads are wide enough to handle added traffic. The constrained storage and transport in the supply chain prevented additional vaccines from being delivered to address increasing demand at many urban facilities.
In HERMES, when the vaccine supply is constricted and only a fraction of the requested doses can be delivered or stored, the number of vials delivered is uniformly reduced across all needed vaccine types to the volume fitting in the cold device displacing some highly utilized multi-dose vials with large single-dose vials. This caused a net drop in the number of vaccinations delivered, as seen in the urban areas when large populations moved. Other options include prioritizing exclusion of vaccines to fit in the cold device. However, regardless of the option picked there will always be undelivered, necessary vaccines in a constrained system, resulting in lower vaccination coverage. This speaks to the necessity of using from a demand forecasting system to address both storage and transport.
As vaccine supply chains are complex systems, interweaving many facilities, vehicles, equipment, and personnel, a single change, such as adjusting ordering from data received a demand forecasting system, can have multiple reverberating effects that are not always easy to anticipate [19]. Doing so can be difficult without simulation modeling. Implementing multiple changes at once can consume considerable time, effort, and resources. Mistakes may not be easy to correct. A model can serve as a virtual laboratory to test the effects of various changes before they are implemented in the field. In fact, there may be a fair amount of synergy between the demand forecasting system and vaccine supply chain models. The latter can help design appropriate demand forecasting systems and identify the information that such a system should collect. The former can then provide additional data to help further refine the models. The models can also utilize the demand forecasting system provided information to make better forecasts and run various scenarios. This type of arrangement already occurs in other industries such as meteorology and air traffic control: an active link between data collection systems and models.
Limitations
Our computational model is a representation of real life [23]. Experiments were conducted using data from Niger collected in 2005 and 2008 and were extrapolated to the present, and thus may not reflect current country conditions. In addition, our experiments were limited to variations in demand, distribution frequencies, and cold chain equipment presenting a best-case scenario and are not related to feasibility of implementation; presumably, information systems speaking to other components of the supply chain may further optimize vaccine availability. Notably, while more accurate population prediction from demand forecasting systems could allow adjustment of distribution frequencies and storage and transport capacities necessary to alleviate these constraints, in reality there are potentially other constraints that could limit this activity. Our model operates under the assumption that all transport and CCE is available and in working order, though maintenance costs are included in costing. In actuality, this may not always be the case, resulting in lower vaccine availability. Although our model accounts for storage and transport constraints, other factors such as personnel engagement, accuracy and standards of data recording, and reliable electricity were not taken into consideration, but would need consideration prior to actual implementation of a demand forecasting system.
CONCLUSIONS
Our study shows the benefits and value of demand forecasting systems to adjust ordering levels while increasing storage capacity and transportation during increases in urban demand. Vaccine availabilities can greatly increase along with lower logistics cost/doses when the demand forecasting system is used to adjust ordering with both additional storage capacity and transportation (capacity or frequency). Implementation of other applications may have some impact but, in certain circumstances, such as a storage and transport constrained supply chain, may hurt delivery. Therefore, implementing a demand forecasting system to advise increases in cold storage and transportation (frequency or capacity) may be the better approach. Systems modeling can assimilate data from demand forecasting systems to make these appropriate recommendations and demonstrate the potential health and economic benefits of supply chain improvements.
Highlights.
-
-
Demand forecasting systems can improve vaccine fulfillment if storage capacity and transportation are added to the supply chain.
-
-
Logistics cost per dose can decrease 34% with implementation of a demand forecasting system with increases in storage capacity and transportation frequency.
-
-
Isolated improvements may not help supply chain performance.
-
-
Simulation modeling can show the effects of concomitant supply chain improvements.
Acknowledgments
Our HERMES Team would like to acknowledge the continuing guidance of Raja Rao, Senior Program Officer at the Bill and Melinda Gates Foundation. This work was supported by the Bill and Melinda Gates Foundation, the Agency for Healthcare Research and Quality (AHRQ) via grant R01HS023317, the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Office of Behavioral and Social Sciences Research (OBSSR) and the Global Obesity Prevention Center (GOPC) via grant U54HD070725, NICHD via grant U01 HD086861, and USAID via grant AID-OAA-A-15-00064. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Black A, Car J, Pagliari C, et al. The impact of eHealth on the quality and safety of healthcare: a systematic overview. PLoS Med. 2011;8:e1000387. doi: 10.1371/journal.pmed.1000387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Partnership for Supply Chain Management. [accessed 12 August 2013];The Hard Road to reliable LMIS: Lessons learned in providing access to accurate and timely data. 2010 [Online], available: http://scms.pfscm.org/scms/docs/papers/LMIS%20abstract.pdf. [Google Scholar]
- 3.Rajgopal J, Connor D, Assi T, et al. The optimal number of routine vaccines to order at health clinics in low or middle income countries. Vaccine. 2011;29:5512–5518. doi: 10.1016/j.vaccine.2011.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Logistimo. [accessed 12 August 2013];Products. 2011 [Online], available: http://www.logistimo.com/products. [Google Scholar]
- 5.Path & World Health Organization. [accessed 12 August 2013];Developing a vision for immunization supply systems. in 2020: landscape analysis summaries. 2011 [Online], available: http://www.path.org/publications/files/TS_opt_vision_2020.pdf. [Google Scholar]
- 6.John Snow, Inc & Usaid. [accessed 12 August 2013];Pipeline 5.1. 2010 [Online], available: http://www.deliver.jsi.com/dhome/resources/tools/softwaretools/pipeline. [Google Scholar]
- 7.Medict. [accessed 12 August 2013];Sigmed. [Online], available: http://www.medict.nl/Manual/introduction/content_001.htm. [Google Scholar]
- 8.Fraser H, Blaya J. Implementing medical information systems in developing countries, what works and what doesn't. AMIA Annu Symp Proc. 2010;2010:232–236. [PMC free article] [PubMed] [Google Scholar]
- 9.Usaid. [accessed 12 August 2013];Computerizing logistics management information systems: a program manager’s guide. 2012 [Online], available: http://deliver.jsi.com/dlvr_content/resources/allpubs/guidelines/CompLMIS_PMG.pdf. [Google Scholar]
- 10.Openlmis. [accessed 12 August 2013];Designing and deploying logistics management information systems that work. 2013 [Online], available: http://openlmis.org/designing-and-deploying-logistics-management-information-systems-that-work/ [Google Scholar]
- 11.Garrib A, Stoops N, McKenzie A, et al. An evaluation of district health information systems. S Afr Med J. 2008;98:549–552. [PubMed] [Google Scholar]
- 12.Gordon W, Jones A, Wecker J. Introducing multiple vaccines in low-and lower-middle-income countries: issues, opportunities and challenges. Health Policy Plan. 2012;27:ii17–ii26. doi: 10.1093/heapol/czs040. [DOI] [PubMed] [Google Scholar]
- 13.Assi T, Brown S, Djibo A, et al. Impact of changing the measles vaccine vial size on Niger's vaccine supply chain: a computational model. BMC Public Health. 2011;11:425. doi: 10.1186/1471-2458-11-425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Assi T, Rookkapan K, Rajgopal J, et al. How influenza vaccination policy may affect vaccine logistics. Vaccine. 2012;30:4517–4523. doi: 10.1016/j.vaccine.2012.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haidari L, Connor D, Wateska A, et al. Augmenting transport versus increasing cold storage to improve vaccine supply chains. PLoS ONE. 2013;8:e64303. doi: 10.1371/journal.pone.0064303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee B, Assi T, Rajgopal J, et al. Impact of introducing the pneumococcal and rotavirus vaccines into the routine immunization program in Niger. Am J Public Health. 2012;102:269–276. doi: 10.2105/AJPH.2011.300218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee B, Assi T, Rookkapan K, et al. Replacing the measles ten-dose vaccine presentation with the single-dose presentation in Thailand. Vaccine. 2011a;29:3811–3817. doi: 10.1016/j.vaccine.2011.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee B, Assi T, Rookkapan K, et al. Maintaining vaccine delivery following the introduction of the rotavirus and pneumococcal vaccines in Thailand. PLoS One. 2011b;6:e24673. doi: 10.1371/journal.pone.0024673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee B, Cakouros B, Assi T, et al. The impact of making vaccines thermostable in Niger's vaccine supply chain. Vaccine. 2012b;30:5637–5643. doi: 10.1016/j.vaccine.2012.06.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization. Comprehensive MultiYear Plan Niger 2011–2015. [accessed 1 May 2013];2011 [Online]. available: http://www.who.int/immunization_financing/countries/cmyp_doc.pdf.
- 21.Geonames. [accessed 27 February 2013];Biggest Cities Niger. 2013 [Online], available: http://www.geonames.org/NE/largest-cities-in-niger.html. [Google Scholar]
- 22.Chaulagai C, Moyo C, Koot J, et al. Design and Implementation of health management information system in Malawi: issues, innovations and results. Health Policy Plan. 2010;20:375–384. doi: 10.1093/heapol/czi044. [DOI] [PubMed] [Google Scholar]
- 23.Lee B. Digital decision making: computer models and antibiotic prescribing in the twenty-first century. Clin Infect Dis. 2008;46:1139–1141. doi: 10.1086/529441. [DOI] [PubMed] [Google Scholar]


