Abstract
Background
The “initial graft tension” applied at the time of graft fixation during ACL reconstruction surgery modulates joint contact mechanics, which in turn may promote post-traumatic osteoarthritis (OA). The objectives of this prospective randomized controlled trial were to compare clinical, functional, patient reported, and OA imaging outcomes between two different initial laxity-based graft tension cohorts and a matched uninjured control group, and to evaluate the effects of laxity-based graft tension on OA development at 84 months follow-up. The two laxity-based tension protocols were: 1) to restore normal anteroposterior (AP) laxity at the time of surgery relative to the contralateral uninjured knee (“low-tension” group), or 2) to over-constrain AP laxity by 2mm relative to the contralateral uninjured knee (“high-tension” group).
Hypothesis
We hypothesized that 1) the high-tension group would have improved outcomes and decreased OA compared to the low-tension group after 84-months, and 2) the outcomes for the high-tension group would be equivalent to an age, sex-, race-, and activity matched group of control subjects with normal knees.
Study Design
Randomized Controlled Trial (Level 1)
Methods
Patients were reconstructed either with a bone-patellar tendon-bone or a four-stranded hamstring autograft, and outcomes were compared to a matched control group recruited from the local area via advertising. Clinical, functional, patient reported and OA imaging outcomes were evaluated pre-operatively and at 60 and 84 months post-op. Repeated measures ANOVA were used to evaluate differences in outcomes between treatment groups and the control group.
Results
There were significant differences between the two tension groups in one of five KOOS outcomes (Sport, P=.04), and two of eight SF-36 scores (vitality and mental health, P<.04) at 84 and 60 months, respectively. Both tension groups scored significantly worse than the control group in IKDC exam (P<.001), 1-hop distance (P<=.017), KOOS Quality of Life and Symptoms (P<.03), and OARSI radiographic score (P<=.02) at 84 months. The low-tension group did worse than the control group in KOOS Pain (P=.03), SF-36 General Health and Social Functioning (P<.04), and the Whole-Organ MRI Score (P=.001), while the high-tension group was different than the control group in knee laxity (P<.001), radiographic joint space width (P=.003), OARSI score (P=.003), and had significantly more subsequent knee injuries (P=.02) at 84 months.
Conclusion
The results do not support our hypotheses that the high-tension group would have improved outcomes when compared to the low-tension group after 84 months of healing, and that the outcomes for the high-tension group would be equivalent to the matched control group. While there were minor differences in patient reported outcomes between the two laxity-based tension groups, all other outcomes were similar.
Key Terms: anterior cruciate ligament (ACL), autograft, reconstruction, tension, outcomes
INTRODUCTION
Anterior cruciate ligament (ACL) reconstruction is commonly performed to restore joint function. However evidence suggests that it may not reduce the risk of posttraumatic osteoarthritis (OA).1 The “initial graft tension” applied at the time of graft fixation modulates joint contact mechanics, which in turn, may promote knee OA. A study was previously published looking at the short-term (e.g., 36 month) outcomes of two different initial graft tension cohorts, using a “laxity-based” approach to set the initial graft tension.20 There were no detectable differences in clinical, functional, patient reported, and OA imaging outcomes between the two laxity-based graft tension groups, and neither group returned to those of the matched control group. However, it remained unknown whether these outcomes would continue to improve with time and become equivalent to those of the control group with long-term healing. Considering that the two laxity-based initial graft tension protocols produced different initial joint contact conditions,19 that autografts continue to remodel after 3 years of healing,7 and that sufficient time is required before OA can be detected,24 a long-term follow-up of these cohorts was needed.
The objectives of this prospective randomized controlled trial (NCT00434837) were to compare clinical, functional, patient reported, and OA imaging outcomes between two different initial laxity-based graft tension cohorts and a matched uninjured control group, and to evaluate the effects of laxity-based graft tension on OA development at 84 months (7 year) follow-up. The matched control group was included to provide baseline data to compare OA progression and other outcome measures. The two laxity-based tension protocols under investigation were: 1) to set the initial graft tension to restore normal anteroposterior (AP) laxity at the time of surgery relative to the contralateral uninjured knee (i.e., the “low-tension” group), or 2) to set the initial graft tension to constrain AP laxity by 2mm relative to the contralateral knee (i.e., the “high-tension” group). The clinical outcomes included the KT-1000,12 IKDC examination score,25 and the number of subsequent knee injuries. The functional outcomes included the 1-leg hop for distance36 and knee extensor torque.32 The patient reported outcomes included the KOOS,38 SF-36,42 and a patient satisfaction survey. The OA imaging outcomes included radiographic measures of joint space width,26 OARSI radiographic score,2 and the WORM (MRI) score.33 We hypothesized that: 1) the high-tension group would have improved clinical, functional, patient reported, and OA imaging outcomes compared to the low-tension group after 84 months, and 2) the outcomes for the high-tension group would be equivalent to a sex-, race-, and age-matched control group.
METHODS
Trial Design
The prospective randomized controlled trial is an extension of the short-term analysis20 and includes the follow-up data obtained at 60 and 84 months. The Institutional Review Boards of Rhode Island Hospital, Miriam Hospital, Memorial Hospital and Brown University approved the study and all subjects granted informed consent. The study was designed as an intent-to-treat analysis. The statistician performed the randomization. Although designed as a double-blind trial, the operating surgeon was informed of the randomization assignment at time of graft implantation. Although blinding was unveiled by the statistician to analyze the 36-month data, investigators were blinded to the subject group assignment for all 60 and 84 month follow-up assessments. An a priori power analysis determined that 45 subjects per group would be necessary to detect a mean difference in joint space width of 5% (1 − β = 0.80; α = 0.05).20 Based on this sample size, the study was powered to detect a 16% difference in AP laxity, 12% difference in International Knee Documentation Committee (IKDC) score, 12% difference in peak isokinetic torque, and 10% difference in the Knee Osteoarthritis Outcome Scores (KOOS).
Participants and Entry Criteria
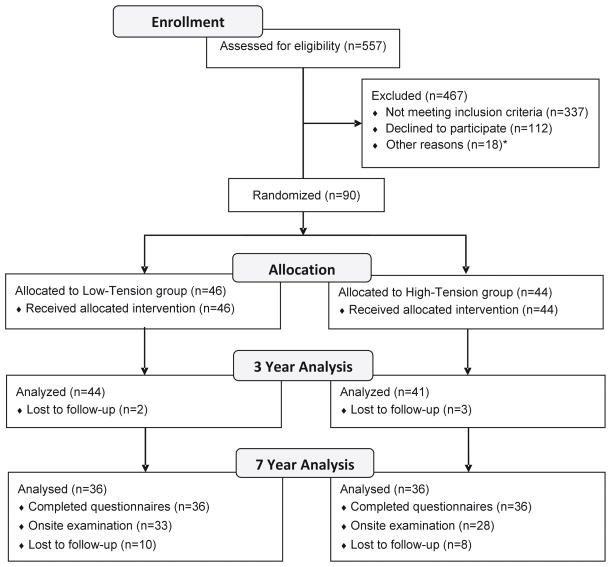
All patients who presented with an isolated unilateral ACL injury in the clinics of three surgeons over three years (02/2004 to 02/2007) were assessed for eligibility as previously described.20 In short, male and female patients between 15 and 50 years of age with a unilateral ACL injury who were candidates for surgical reconstruction with bone-patellar tendon-bone or 4-stranded hamstring tendon autograft were included. Patients presenting with an ACL injury more than 12 months old, significant concomitant injury to the menisci or other ligaments, a previous knee injury or evidence of OA were excluded. Of the 557 patients screened, 355 were excluded as they did not meet the inclusion criteria and 112 declined to participate.20 Of the 90 patients randomized between the two tension groups (low-tension, n=46; high-tension, n=44), eighteen (20%) were lost to follow-up at 84 months (Fig. 1). Of the remaining 72 patients, 100% filled out the questionnaires, and 86% returned for the on-site follow-up examination. An uninjured control group, comprised of 60 subjects, who were matched by age, sex, race, and activity level, was also recruited from the local area via advertisement.20 Control subjects were excluded if they had a previous knee injury, increased knee laxity, or evidence of OA.20 Twenty-five (42%) of the controls were lost to follow-up at 84 months, 32 returned for their 84 month exams and 3 sent in their questionnaires.
Fig. 1.
CONSORT diagram of the study design, patient allocation and loss to follow-up through 7 years.20
ACL Reconstruction/Initial Graft Tension Protocols
Patients were reconstructed either with a bone-patellar tendon-bone autograft obtained from the central third of the ipsilateral patellar tendon, or a four-stranded semitendinosis and gracilis autograft.20 Patients selected the graft type and all surgeons followed the same operative procedures. Grafts were preconditioned with 20 manual tension cycles prior to fixation. For the patellar tendon grafts, the bone blocks were secured using interference screws. The hamstring tendon grafts were fixed with cortical fixation on the femur and a biodegradable interference screw on the tibia backed up at the surgeon’s discretion with a screw and spiked soft tissue washer. For those patients receiving the low-tension assignment, the grafts were tensioned by firmly pulling on the distal graft with the knee at 0° of knee flexion.19 For those receiving the high-tension assignment, the grafts were firmly tensioned with the knee at 30° of knee flexion.19,20 Tibial fixation was partially engaged for both graft types and AP laxity at 20° of flexion was checked using the KT-1000S (MEDmetrics Inc; San Diego CA) and compared to that of the contralateral knee under anesthesia. If the targeted laxity value was not achieved within 1 mm, the fixation was released, and the tensioning procedure was repeated. The laxity value was rechecked once the fixation procedure was completed, and this value was used for all subsequent analyses. Post-operatively, all subjects followed a standardized rehabilitation program designed to get them back to sport within 6 months.6
Clinical Outcomes
AP laxity values for both knees were measured using the KT-1000 Knee Arthrometer (MEDMetric Corporation, San Diego CA) pre-operatively and at all post-operative time points.12 Trained sports physical therapists dedicated to the project performed the KT-1000/KT-1000S measurements. Three manual maximum tests were performed and the displacement readings averaged. The difference between legs was reported.
Clinical outcome was assessed using the 2000 IKDC Knee Examination Score (http://www.sportsmed.org).25 The IKDC scores evaluate four categories: 1) function, 2) symptoms, 3) range of knee motion, and 4) clinical examination. The IKDC score rates knees as normal (A), nearly normal (B), abnormal (C), and severely abnormal (D), with the final IKDC rating based on the score of the worst category. Subsequent knee injuries to the ipsilateral or contralateral knee were determined by patient questioning and medical record review at each follow-up visit. Trained sports physical therapists administered all clinical examinations.
Functional Outcomes
Subjects performed the 1-leg hop test for distance three times and the trials were averaged.36 The mean hop distance of the injured leg was normalized to that of the uninjured contralateral leg. Isokinetic strength testing (Biodex 2; Biodex Medical Systems, Inc. Shirley NY) was performed at 60°/sec to assess the strength of the extensor muscles of each knee.32 Peak torques for five repetitions were averaged and normalized with respect to bodyweight and height.
Patient-Reported Outcomes
The KOOS38 and the SF-36v242 were implemented to assess patient reported outcomes. The KOOS evaluates five domains: 1) knee related quality of life (KOOS-QOL), 2) sports and recreation function (KOOS-sport), 3) activity of daily living (KOOS-ADL), 4) symptoms (KOOS-symptoms), and 5) pain (KOOS-pain). For this study, the composite KOOS model developed by Englund et al was additionally used to identify subjects with joint arthrosis.18 Subjects with a KOOS-QOL≤87.5, and who did not meet the thresholds of at least two of the other subscales (i.e., KOOS-pain≤86.1, KOOS-symptoms≤85.7, KOOS-ADL≤86.8, and KOOS sport≤85) were designated as having OA using this model.18,43 The SF-36 evaluates general health related to physical function, role limitations, bodily pain, vitality, social functioning, emotional role, mental health, and health transition.42
Activity levels were monitored at time of recruitment and at each follow-up using the Tegner activity scale.39 A supplemental survey, in which subjects were asked if they had any subsequent knee injuries that required a doctor’s visit, how satisfied they were with their baseline surgical outcome (scale of 1, not satisfied, to 10, very satisfied), and if they would elect to have ACL reconstruction surgery again, was mailed after they completed their 84 month follow-up.
OA Imaging Outcomes
Medial minimum joint space width (JSW) measurements were obtained from standardized radiographs pre- and post-operatively using a posterior-anterior view of the semi-flexed knee.8,26 The knee flexion angle was standardized across patients by placing the metatarsal phalangeal joint of the foot in the same plane as the image intensifier and the knee was flexed forward until the patella touched the image intensifier as previously described.8,20 The minimum JSW of the medial compartment was calculated using a validated automated algorithm,13,14 which was recently used to measure JSW changes in the MOON “nested” cohort following ACL reconstruction,26,27 and has been recently shown to be more reliable than the method originally used in the 36-month follow-up of the current study.20
The overall condition of the joint was assessed pre- and post-operatively using the modified Osteoarthritis Research Society International (OARSI) radiographic grading scale.22 Using posterior-anterior and lateral radiographs of both knees, a grade of 0 (normal) to 4 (severe) was assigned to two radiographic features: osteophyte formation and joint space narrowing. In addition, sclerosis, attrition, and ligament calcification were assessed on a dichotomous scale. An experienced musculoskeletal radiologist (GAT) scored all films while blinded to the treatment group.
OA was also assessed using the Whole Organ Magnetic Imaging Score (WORMS).34 The score utilizes MR sequences to grade 14 independent features; cartilage signal and morphology, sub-articular bone marrow abnormality, sub-articular cysts, sub-articular bone attrition, marginal osteophytes evaluated in 15 regions. The condition of the menisci, cruciate and collateral ligaments, synovitis, loose bodies, and periarticular cysts were also included. WORMS were performed by an experienced musculoskeletal radiologist (GAT) who was blinded to treatment.
Statistical Methods
Repeated measures ANOVAs were used to evaluate differences among treatment groups with respect to temporal changes in outcome variables. The statistical models included fixed factors representing treatment group (low-tension, high-tension and control) and time. For each control subject, a knee was randomly selected to represent the reconstructed knee for the outcome measures reported as differences or ratios between limbs. If significant interactions were detected, F-tests corresponding to simple effects were examined. Pairwise comparisons were performed using Fisher’s LSD. Chi-square tests were utilized to compare the frequency of subsequent injuries and the distributions of IKDC scores between groups. A chi-square test was also used to compare the percent of subjects within each group in which the composite KOOS model18,43 indicated the presence of OA. All means presented represent least square means and corresponding 95% confidence intervals (CI). P-values less than .05 were considered significant.
RESULTS
Patient Characteristics/Intraoperative Findings
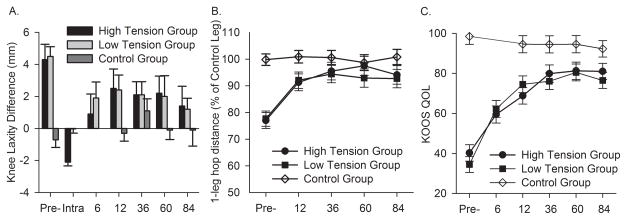
At the 84 month visit, ten low-tension, eight high-tension and twenty five control subjects were lost to follow-up. Patient sex (60% women vs 48% women), age (23 vs 24 years), weight (69 vs 73 kg), time between injury and index surgery (105 vs 114 days), percentage of patients receiving patellar tendon grafts (61% vs 67%), and the percentage of patients with minor meniscal injuries (41% vs 41%) or minor chondral lesions (23% vs 17%) were similar between the high- and low-tension initial laxity-based graft tension groups, respectively.20 Preoperatively, the AP laxity values between the two tension groups were not significantly different (P=.70) but they were significantly greater than the control group (Fig. 2A; P<.001).20
Fig. 2.
Examples of a A) clinical (KT-1000), B) functional (1-leg hop for distance), and C) a patient-oriented (KOOS-QOL) outcome over 84 months.
Clinical Outcomes
Immediately after graft fixation, AP laxity differences between limbs for the low-tension and high-tension treatments were 0.2±0.3 mm and 2.1±0.2 mm, respectively (P<.001), as intended by each initial graft tension protocol (Fig. 2A). The AP laxity values between the two initial graft tension groups were not significantly different at 60 months (P=.85) or 84 months (P=.83). At 84 months, there was a significant difference between the high-tension group laxity and that of the control group (P<.001), but no significant difference between the low-tension group and the control group (P=.06). As would be expected, there were no temporal changes in AP laxity in the control group (P=.23).
Preoperatively, the distributions of the IKDC examination scores between the two initial graft tension groups ranged from B (nearly normal) to D (severely abnormal), while the control group ranged from A (normal) to B (nearly normal) (Table 1). There was no significant difference in the distributions of the IKDC scores between the two initial graft tension groups (P=.68); however, they were significantly different from the control group (P<.001). Both the low- and high-tension groups remained significantly different from the control group 60 months (P=.04, P =.03) and 84 months (P<.001, P<.001) following surgery.
Table 1.
IKDC examination scores for the three experimental groups.
| IKDC Score | Low-tension | High-tension | Controls |
|---|---|---|---|
| Pre-operative | |||
| A | 0 (0.0%) | 0 (0.0%) | 58 (96.7%) |
| B | 27 (60.0%) | 27 (64.3%) | 2 (3.3%) |
| C | 17 (37.8%) | 13 (31.0%) | 0 (0.0%) |
| D | 1 (2.2%) | 2 (4.8%) | 0 (0.0%) |
| 36 month | |||
| A | 20 (60.6%) | 17 (53.1%) | 32 (86.5%) |
| B | 10 (30.3%) | 11 (34.4%) | 4 (10.8%) |
| C | 3 (9.1%) | 4 (10.8%) | 1 (2.7%) |
| D | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| 60 months | |||
| A | 13 (44.8%) | 10 (41.7%) | 21 (75.0%) |
| B | 13 (44.8%) | 12 (50.0%) | 7 (25.0%) |
| C | 3 (10.3%) | 2 (8.3%) | 0 (0.0%) |
| D | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| 84 months | |||
| A | 8 (25.0%) | 7 (24.1%) | 24 (75.0%) |
| B | 17 (53.1%) | 21 (72.4%) | 8 (25.0%) |
| C | 7 (21.9%) | 1 (3.5%) | 0 (0.0%) |
| D | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
Functional Outcomes
Preoperatively, the hop distances were not significantly different between the two initial graft tension groups (P=.59), but both were significantly less than the control group (P= .001) (Fig. 2B). After 84 months of healing, hop distances between the two initial graft tension groups were not significantly different from each other (P=.80). Both the low- (P=.008) and high- (P=.017) tension groups were significantly less than the control group. There were no temporal changes in hop distances within control patients (P=.79).
At 60 months, mean peak extension torques were 93.0±3.4%, 99.0±3.6% and 94.9±3.3%, and at 84 months were 99.7±3.3%, 102.4±3.6%, and 99.5±3.2% for the low-tension, high-tension and control groups, respectively. There were no significant differences between the treatment and control groups at 60 months (P=.22) or 84 months (P=.54).
Patient-Reported Outcomes
The pre-injury Tegner scores were 7.4±0.6, 7.8±0.6 and 6.4±0.6 for the low-tension, high-tension and control groups, respectively. At 60 months, these dropped to 5.4±0.7, 6.2±0.7, and 5.6±0.7, and at 84 months to 4.8±0.6, 5.6±0.6 and 5.5±0.6. There was a significant reduction in the mean Tegner activity scores over time in both tension groups as well as the control group (P<.009). There was no significant difference between the treatment groups at 60 months (P=.12) or 84 months (P=.06). Furthermore, the scores for the two initial graft tension groups were not significantly different from the control group at any postoperative time point (P>.12).
Preoperatively, all KOOS values for the graft tension groups were significantly different from the control group (P<.001) (Table 2). At 84 months, all low-tension KOOS scores were significantly less than the control group (P<.03), except for KOOS-ADL (P=.062). However, while the high-tension group scores for KOOS-QOL (Fig 2C) and KOOS-symptom were significantly less (P<.03) than the control group, there were no significant differences (P>.15) in KOOS-sport, KOOS-ADL, and KOOS-pain. Eight patients in the low-tension group, five patients in the high-tension group, and one subject in the control group had combined KOOS model outcomes indicative of symptomatic knee OA (Low-tension vs Control, p=.01; High-tension vs control group, p=.09).18,43
Table 2.
Scores of the Knee Osteoarthritis Outcome Score (KOOS) Subscales.
| Subscale | Time | Low-tension | High-tension | Control |
|---|---|---|---|---|
| Quality of Life (Tension treatment effect: p<.001; Tension time effect: p<.001) | ||||
| Pre-surgery | 34.5±5.5* | 40.3±5.7* | 98.5±5.6 | |
| 60 months | 80.5±5.9* | 81.3±6.0* | 94.6±6.0 | |
| 84 months | 76.5±5.6* | 81.1±5.7* | 92.3±5.8 | |
| Sports & Recreation (Tension treatment effect: p<.001; Tension time effect: p<.001) | ||||
| Pre-surgery | 55.4±5.2* | 59.6±5.4* | 98.0±5.2 | |
| 60 months | 85.3±5.5* | 89.2±5.6 | 93.9±5.6 | |
| 84 months | 79.9±5.2^* | 87.8±5.3^ | 93.3±5.4 | |
| Activities of Daily Living (Tension treatment effect: p<.001; Tension time effect: p<.001) | ||||
| Pre-surgery | 85.8±2.6* | 86.0±2.7* | 99.9±2.7 | |
| 60 months | 96.9±2.8 | 97.0±2.9 | 99.4±2.9 | |
| 84 months | 95.0±2.7t | 96.6±2.7 | 98.7±2.8 | |
| Symptoms (Tension treatment effect: p<.001; Tension time effect: p<.001) | ||||
| Pre-surgery | 69.6±4.2* | 73.0±4.3* | 96.3±4.2 | |
| 60 months | 85.3±4.4* | 85.8±4.5* | 93.0±4.5 | |
| 84 months | 82.5±4.2* | 85.8±4.3* | 92.4±4.3 | |
| Pain (Tension treatment effect: p<.001; Tension time effect: p<.001) | ||||
| Pre-surgery | 75.1±3.4* | 78.5±3.5* | 99.0±3.4 | |
| 60 months | 91.4±3.6t | 94.3±3.7 | 96.0±3.7 | |
| 84 months | 90.6±3.4* | 92.9±3.5 | 96.3±3.5 | |
Values are expressed as mean±95% confidence interval. There was a significant difference between tension groups at 84 months in the Sports & Recreation subscale.
There were differences between the two initial graft tension groups and the control group at most time points.
p<.05
p<.05
p<.10
Two of the eight SF-36 health domains (vitality, mental health) in the low-tension group were significantly lower than the high-tension group (P<.04) at 60 months but not at 84 months. The high-tension group scored better than the control group (P=.02) in one health domain (mental health) at 60 months, but there were no significant differences at 84 months. There were no significant differences between low-tension and control group at 60 months, however two of the health domains (general health, social functioning) scored significantly lower than the control group (P<.04) at 84 months (Table 3).
Table 3.
SF-36v2 Scores.
| Time | Low-tension | High-tension | Control |
|---|---|---|---|
| Physical Functioning (Tension treatment effect: p<.001; Tension time effect: p<.001) | |||
| Pre-surgery | 71.6±2.0* | 73.3±2.1* | 97.8±2.0 |
| 60 months | 94.2±2.1 | 96.6±2.2 | 96.5±2.1 |
| 84 months | 92.4±2.0t | 95.14±2.0 | 97.8±2.1 |
| Role Physical (Tension treatment effect: p<.001; Tension time effect: p<.001) | |||
| Pre-surgery | 61.7±5.5* | 58.2±2.9* | 97.0±2.8 |
| 60 months | 97.5±3.1 | 96.7±3.1 | 97.2±3.1 |
| 84 months | 94.8±2.9 | 97.6±2.9 | 96.6±2.9 |
| Bodily Pain (Tension treatment effect: p=.02; Tension time effect: p<.001) | |||
| Pre-surgery | 63.5±2.7* | 62.9±2.8* | 84.8±2.8 |
| 60 months | 82.5±3.0 | 88.3±3.0 | 82.3±3.0 |
| 84 months | 78.2±2.8#,t | 85.5±2.8 | 85.6±2.9 |
| General Health (Tension treatment effect: p=.22; Tension time effect: p=.68) | |||
| Pre-surgery | 81.4±2.1 | 85.4±2.1 | 85.8±2.1 |
| 60 months | 83.3±2.2 | 86.0±2.3 | 85.7±2.2 |
| 84 months | 80.7±2.1* | 84.1±2.1 | 86.9±2.2 |
| Vitality (Tension treatment effect: p=.19; Tension time effect: p=.02) | |||
| Pre-surgery | 62.3±2.6* | 66.1±2.7 | 71.8±2.7 |
| 60 months | 67.9±2.8^ | 76.3±2.9t | 68.9±2.8 |
| 84 months | 69.2±2.7 | 72.2±2.7 | 71.7±2.8 |
| Social Functioning (Tension treatment effect: p<.001; Tension time effect: p<.001) | |||
| Pre-surgery | 82.2±2.3* | 77.2±2.4* | 97.0±2.4 |
| 60 months | 92.4±2.5 | 94.6±2.6 | 97.3±2.5 |
| 84 months | 90.3±2.4#,* | 96.5±2.4 | 97.2±2.5 |
| Role Emotional (Tension treatment effect: p=.15; Tension time effect: p<.001) | |||
| Pre-surgery | 83.8±2.4* | 83.7±2.5* | 97.1±2.4 |
| 60 months | 93.25±2.6 | 96.0±2.7 | 96.7±2.6 |
| 84 months | 95.5±2.5 | 95.6±2.5 | 97.2±2.5 |
| Mental Health (Tension treatment effect: p=.06; Tension time effect: p<.001) | |||
| Pre-surgery | 73.4±2.2* | 75.1±2.2* | 83.9±2.2 |
| 60 months | 78.4±2.3^ | 87.7±2.4* | 80.0±2.3 |
| 84 months | 80.5±2.2 | 85.0±2.2 | 85.0±2.3 |
There was a significant difference between the mean±95% CI for the two tension groups at 60 months in the Vitality and Mental Health subscales.
Preoperatively, low tension and high tension were significantly different from control in 7 and 6 out of the 8 subscales, respectively.
p<.05
p<.10
p<.05
p<.10
While there were no significant differences in the number of subsequent knee injuries between treatment groups at 84 months (P=.53), there was a significant difference between high-tension and control groups (P=.02). In the ACL-reconstructed knees, there was a total of four knee injuries (2 graft tears, and 2 meniscus tears) in the low-tension group, and seven knee injuries (2 graft tears, 4 meniscal tears, and 1 graft+meniscus tear) in the high-tension group. In the contralateral knee, there was a total of three knee injuries (2 ACL tears, 1 meniscal tear) in the low-tension group and three knee injuries (3 ACL tears) in the high-tension group. There were 4 knee injuries (1 ACL tear, 1 MCL tear, 1 meniscus tear, 1 patellar dislocation) in the control group.
From the patients that filled out the supplemental questionnaire, it was found that the low- and high-tension groups were very satisfied with their surgical outcome with scores of 9.10±1.7 and 9.30±1.3 out of ten, respectively (P=.67). Twenty out of 21 low-tension respondents and nineteen out of 20 high-tension respondents indicated they would elect to have ACL reconstruction surgery again if it were needed.
Imaging Outcomes
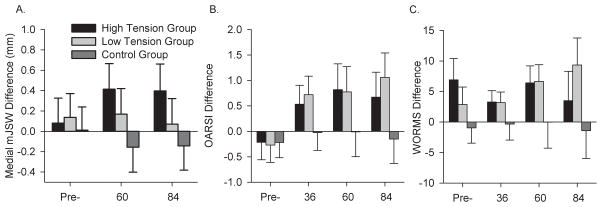
There were no significant differences in the mean medial minimum joint space width of the injured knee between treatment groups at 60 months (P=0.17) or 84 months (P=.08). The medial joint space width of the high-tension group was significantly greater than the control group at both 60 (P=.002) and 84 months (P=.003), however the low-tension group was not (P=.07, P=.22, respectively; Fig 3A).
Fig. 3.
The mean differences (±95% confidence intervals) between the surgical limb and the contralateral control knee for each group over 84 months for A) minimum JSW of the medial compartment, B) OARSI score, C) WORM score are shown. A positive value indicates that the surgical knee is greater than the contralateral knee.
The mean differences in the OARSI scores of the injured knee minus the contralateral knee between tension groups were not significant at 60 months (P=0.29) or 84 months (P=.23), however there was a significant increase (i.e. worse score) between the low-tension and the control groups at both 60 (P=.03) and 84 months (P<.001), and between the high-tension and control groups at 84 months (P=.02) (Fig. 3B).
The mean WORMS for the injured knee were greater (i.e., worse) than those of the control group both preoperatively and after 84 months (Fig 3C). The mean WORMS differences (injured – contralateral knee) were not significantly different between the two initial graft tension treatment groups preoperatively (P=.15), at 60 months (P=.69) or at 84 months (P=.08). Both the high- and low-tension groups were significantly greater than the control group at 60 months (P=.03, P=.01). The low-tension group remained significantly different than the control group at 84 months (P=.001), however there was no significant difference between the high-tension and control groups (P=.14).
DISCUSSION
The most important findings of this study were that, in general, there was little difference in the clinical, functional, and patient reported outcomes for the two initial graft tension groups. Furthermore, most outcomes of both groups were inferior to those of the control group at 84 months. Thus, the results do not support the hypotheses that the high-tension group would have better outcomes than the low-tension group and that the outcomes of the high-tension group would be equivalent to those of the control group. Nonetheless, the long-term follow-up has shown the emergence of differences in the KOOS sport and two of the SF-36 scores between the two tension groups, with the high-tension group faring greater than 8 points better than the low-tension group for all three scores, differences that were not present at 36 months.20 An 8 point difference in the KOOS is thought to be clinically relevant.37 The reason for this is unclear but could possibly be the result of degenerative changes that are not detectable in the early stages of healing. Furthermore, the imaging outcomes evaluating OA suggest that knee arthrosis is progressing 84 months post-operatively in both treatment groups relative to the age-, sex-, race- and activity-matched control group.
While several of the clinical and functional outcomes between the two tension groups were not significantly different, there were a few trends worth noting. First, there was a trend (P=.089) that the IKDC examination score distribution for the high-tension was superior to that of the low tension group (1 “C” rating versus 7 “C” ratings, respectively) at 84 months. It is also interesting to note the trend that the mean Tegner score for the high-tension group was greater than that of the low tension group at 84 months (P=.06). The activity level of the high-tension group was equivalent to the control group while the low-tension group was less active. For the low-tension group, all of the KOOS scores except for KOOS-ADL were significantly less than those of the control group while for the high-tension group only the KOOS-symptom and KOOS-QOL scores were less than that of the control group. It should be noted that eight of the patients in the low-tension group and five in the high-tension group had the KOOS scores indicative of symptomatic knee OA according to the combined KOOS model of Englund et al in which the low-tension group reached statistical significance.18 While many of the outcomes are only trends, these were not present at the 36-month follow-up,20 and further suggest that differences are emerging. Long-term follow-up will be required to determine the implications of these trends.
The imaging outcomes for OA suggest that on average knee arthrosis is progressing 84 months post-operatively. The minimum joint space width of the medial compartment was measured with the validated method used by the Osteoarthritis Initiative.14,15 While not significant, there was a trend (P=.08) indicating that the minimum joint space width of the surgical knee of the high tension group was greater than those of the low-tension group at 84 months. These findings suggest that the cartilage thickness was increasing in the high-tension group but not changing in the low-tension group. While advanced OA is typically marked by a decrease in articular cartilage thickness, an increase in cartilage thickness has been reported in the early stages of OA progression, and thought to be due to the breakdown of proteoglycan, which attracts water into the articular cartilage.10,35 A mean increase in articular cartilage thickness in ACL reconstructed knees relative to the uninjured contralateral control knee has been reported by Jones et al two years after surgery.26 They also found that ACL reconstructed knees that also underwent partial meniscectomy had narrower JSW measurements relative to the contralateral uninjured knee than knees of patients that underwent an isolated ACL reconstruction, suggesting the knees with concomitant meniscal damage are further along the disease process.26 It may be that the low tension group is normal or that we are seeing OA development at different stages in both groups (i.e., the high-tension group at an earlier stage of OA progression). Additional study is warranted.
While minimum joint space width is a surrogate for articular cartilage thickness, the secondary cartilage imaging outcomes (OARSI radiographic and WORM scores) reflect overall joint health as it relates to OA since it is a disease that affects the whole joint. The OARSI scores were primarily influenced by osteophyte formation at 84 months. The WORM scores were affected by cartilage signal and osteophyte formation at 84 months, whereas at the time of injury (pre-op assessment) they were being driven by bone marrow edema, meniscus status, and ACL integrity. Longer-term follow-up is required to determine if joint arthrosis will continue to progress in this cohort of ACL reconstructed patients with isolated ACL injuries and minimal meniscal damage at time of surgery. It is important to focus the study on subjects with isolated ACL injuries as concomitant meniscal injury has been shown to accelerate post-traumatic OA in ACL injured patients.26
There have been several randomized trials evaluating the effects of initial graft tension on clinical outcomes after single-bundle ACL reconstruction. For hamstring tendon grafts, Yasuda et al reported mean side-to-side differences in anterior laxity were significantly less when the graft was tensioned to 80 N compared to 20 N two or more years post-surgery.47 However, Kim et al found no significant differences in knee laxity when the grafts were tensioned to 78, 117 and 146 N after one year.28 For patellar tendon grafts, Nicholas et al reported significant improvements in knee laxity when the grafts were tensioned to 90 N as compared to 45 N.31a However, Yoshiya48 and van Kampen40 found no differences in knee laxity. While two of these studies showed differences in knee laxity, no differences in any other outcomes were found. In an evidence-based review, it was concluded that “there is no clear trend in terms of statistically significant or clinically relevant differences in the amount of tension to apply to the graft during graft fixation”.4 Likewise, in the present study, there were no significant differences in most of the outcomes between the two laxity-based initial graft tension protocols through 84-months. The comparison to the control group, which was unique to the current study, also indicated that many of the outcome measures were inferior to those of the matched control group despite the initial graft tension level.
A laxity-based initial graft tensioning protocol was selected for study instead of a “force-based” approach.19 The laxity-based approach implies that the tension in the graft is adjusted to produce an AP laxity value that is equal to or less than that of the contralateral normal knee. A force-based approach (e.g. 20N, 40N, etc.) was not used for this study because the amount of force required to restore AP knee laxity is subject specific,9 and prone to error.21,41 Although a laxity-based tensioning approach may require a variety of tension levels across patients within a treatment group, the tension applied to the graft in an effort to recreate normal AP knee laxity would be less than that required to over-constrain the joint within the same patient, hence the terminology of “low-tension” versus “high-tension”.
For this trial, the grafts were tensioned to match normal AP laxity or over-constrain it by 2 mm. The desired initial conditions were achieved, however both grafts stretched out over time. After 7 years of healing, the mean difference between the surgical limb and the contralateral control limb across the two treatment groups was approximately 1.5 mm, while the knees of the control group did not stretch out over time (Fig. 2A). Most of the increase occurred over the first six months of healing. The amount of increase observed was similar to those reported for other clinical studies of ACL reconstruction.5,29. Although the results suggest that the differences in AP knee laxity between the two laxity-based initial graft tension conditions are minimal at 84 months, differences in joint contact conditions immediately after surgery may still impact long-term joint health. Recent evidence suggests that the inflammatory response after ACL injury may have a negative impact on the articular cartilage,22,30 which in turn may compromise a primary lubricating mechanism of the joint.16,17 Although the details about the interactions between inflammatory cytokines, degradative enzymes, lubrication and OA remain to be worked out, the cartilage is thought to be at high risk for damage in the early days following injury.3,11,22 Surgery also adds a second inflammatory insult, which could exacerbate the problem.23 High contact stresses and increased shear motion during early healing, when catabolic enzymes are present in synovial fluid, could promote OA.3 Thus, it is likely that initial differences in joint contact mechanics would influence long-term joint health. At this time, it appears that OA may be progressing in both initial graft tension groups compared to the uninjured control group.
There are several limitations to this study. As with any long term follow-up, the number of subjects that drop out will introduce bias. However, the number of patients that dropped out of the tension cohorts at 84 months was only 20%. Loss to follow-up would also affect the power of the study, however the change was minimal as the study was power to detect an 18% difference in knee laxity, 13.5% change in IKDC score, 13.5% change in peak torque, and a 12% change in KOOS score with the reduced number. The dropout rate for control group was higher, however we over-recruited the control group by 15 subjects to compensate for the expected higher loss to follow-up. While the control group was relatively small (n=35), matching by age, sex, race and activity was performed to try to construct a representative control population for comparison. It should also be noted that the supplemental patient satisfaction questionnaire was completed by only 41 of the 72 eligible subjects, as it was mailed out after all subjects had received their original questionnaires.
Structural assessments of joint space width via radiography are not very sensitive measures to detect changes in the early stages of OA.36 While joint space narrowing in the medial compartment did not occur on average in our cohort at 84 months, the OARSI radiographic score,2 and WORM score,34 are outcomes that focus on the whole joint and not just cartilage alone. These latter measures are starting to show differences between the experimental groups. It is likely that joint space narrowing will follow given enough time. While the radiologist was blinded to treatment group, it is possible that the presence of screws and tunnels in the surgical knee could bias scoring of the radiographs or MR images. However, he would be unable to distinguish images between the contralateral knees of the treatment group and the knees of the control group, or between reconstructed knees of the two graft tension groups.
In this study, our objective was to establish the progression of OA in the ACL reconstructed knee following isolated ACL injury while accounting for confounding variables including graft type, graft placement, concomitant injuries, and post-operative rehabilitation. Therefore, only patients receiving autografts were enrolled, all surgeons used the same drill guide system, subjects with concomitant injuries (other than a minor meniscal tear) were excluded, and all patients were prescribed the same post-operative rehabilitation program. A limitation is that we included both patellar tendon and 4-stranded hamstring tendon autografts in the study. Due to the popularity of these two autografts, the participating surgeons felt it was important to give the patient their choice. This was not seen as a significant limitation as previous biomechanical and clinical studies found them to be equivalent.31,44,45 However, a recent meta-analysis suggests that the radiographic incidence of OA following ACL reconstruction is greater for bone-patellar tendon-bone compared to hamstring tendon autografts.46 As graft type was not randomized in this study, and because only a third of the patients received a hamstring tendon graft, the study was not powered to address the question. Nonetheless, the ratio of graft types in both treatment groups was similar, which would minimize bias.20
In conclusion, the results do not support our hypotheses that the high-tension group would have improved outcomes when compared to the low-tension group after 84 months of healing, and that the outcomes for the high-tension group would be equivalent to the matched control group. While there were minor differences in patient reported outcomes between the two laxity-based tension groups, all other outcomes were similar. Long-term data are still needed to reconcile these findings.
Acknowledgments
The project was funded by the National Institutes of Health (2R01-AR047910 from NIAMS) and the Lucy Lippitt Endowed Professorship.
The authors gratefully acknowledge the assistance of Melanie Westwell, Nabil Mehta, Alison Biercevicz, Emily Robbins, Heidi Oksendahl, Daniel Acuri, Lynn Fanella, and David Dimascio. The MRI scans were acquired at the MRI Research Facility (Brown University, Providence, Rhode Island) and the Osteoarthritis Initiative MRI Facility (Southeastern Medical Center, Memorial Hospital, Pawtucket, Rhode Island).
Footnotes
Investigation performed at Rhode Island Hospital, Providence, Rhode Island
Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NIAMS of the NIH.
References
- 1.Ajuied A, Wong F, Smith C, et al. Anterior cruciate ligament injury and radiologic progression of knee osteoarthritis: A systematic review and meta-analysis. Am J Sports Med. 2014;42:2242–2252. doi: 10.1177/0363546513508376. [DOI] [PubMed] [Google Scholar]
- 2.Altman RD, Gold GE. Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthritis Cartilage. 2007;15:A1–A56. doi: 10.1016/j.joca.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 3.Anderson DD, Chubinskaya S, Guilak F, et al. Post-traumatic osteoarthritis: Improved understanding and opportunities for early intervention. J Orthop Res. 2011;29:802–809. doi: 10.1002/jor.21359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arneja S, McConkey MO, Mulpuri K, et al. Graft tensioning in anterior cruciate ligament reconstruction: a systematic review of randomized controlled trials. Arthroscopy. 2009;25:200–207. doi: 10.1016/j.arthro.2008.07.010. [DOI] [PubMed] [Google Scholar]
- 5.Beynnon BD, Johnson RJ, Naud S, et al. Accelerated versus nonaccelerated rehabilitation after anterior cruciate ligament reconstruction: a prospective, randomized, double-blind investigation evaluating knee joint laxity using roentgen stereophotogrammetric analysis. Am J Sports Med. 2011;39:2536–2548. doi: 10.1177/0363546511422349. [DOI] [PubMed] [Google Scholar]
- 6.Beynnon BD, Uh BS, Fleming BC, et al. Rehabilitation following anterior cruciate ligament reconstruction; A prospective, randomized, double-blind comparison of accelerated versus non-accelerated rehabilitation. Am J Sports Med. 2005;33:347–359. doi: 10.1177/0363546504268406. [DOI] [PubMed] [Google Scholar]
- 7.Biercevicz AM, Akelman MR, Fadale PD, et al. MRI volume and signal intensity of ACL graft predict clinical, functional, and patient-oriented outcome measures after ACL reconstruction. Am J Sports Med. 2015;43:693–699. doi: 10.1177/0363546514561435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buckland-Wright JC, Wolfe F, Ward RJ. Substantial superiority of semiflexed (MTP) views in knee osteoarthritis: a comparative radiographic study, without fluoroscopy, of standing extended, semiflexed (MTP), and schuss views. J Rheumatol. 1999;26:2664–2674. [PubMed] [Google Scholar]
- 9.Burks RT, Leland R. Determination of graft tension before fixation in anterior cruciate ligament reconstruction. Arthroscopy. 1988;4:260–266. doi: 10.1016/s0749-8063(88)80041-0. [DOI] [PubMed] [Google Scholar]
- 10.Calvo E, Palacios I, Delgado E, et al. Histopathological correlation of cartilage swelling detected by magnetic resonance imaging in early experimental osteoarthritis. Osteoarthritis Cartilage. 2004;12:878–886. doi: 10.1016/j.joca.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 11.Catterall JB, Stabler TV, Flannery CR, Kraus VB. Changes in serum and synovial fluid biomarkers after acute injury ( NCT00332254) Arthritis Res Ther. 2010;12:R229. doi: 10.1186/ar3216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Daniel DM, Malcom LL, Losse GM, Stone ML, Sachs R, Burks RT. Instrumented measurement of anterior laxity of the knee. J Bone Joint Surg Am. 1985;67:720–726. [PubMed] [Google Scholar]
- 13.Duryea J, Li J, Peterfy CG, Gordon C, Genant HK. Trainable rule-based algorithm for the measurement of joint space width in digital radiographic images of the knee. Med Phys. 2000;27:580–591. doi: 10.1118/1.598897. [DOI] [PubMed] [Google Scholar]
- 14.Duryea J, Neumann G, Niu J, et al. Comparison of radiographic joint space width with magnetic resonance imaging cartilage morphometry: analysis of longitudinal data from the Osteoarthritis Initiative. Arthritis Care Res (Hoboken) 2010;62:932–937. doi: 10.1002/acr.20148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Duryea J, Zaim S, Genant HK. New radiographic-based surrogate outcome measures for osteoarthritis of the knee. Osteoarthritis Cartilage. 2003;11:102–110. doi: 10.1053/joca.2002.0866. [DOI] [PubMed] [Google Scholar]
- 16.Elsaid KA, Jay GD, Chichester CO. Reduced expression and proteolytic susceptibility of lubricin/superficial zone protein may explain early elevation in the coefficient of friction in the joints of rats with antigen-induced arthritis. Arthritis Rheum. 2007;56:108–116. doi: 10.1002/art.22321. [DOI] [PubMed] [Google Scholar]
- 17.Elsaid KA, Machan JT, Waller K, Fleming BC, Jay GD. The impact of anterior cruciate ligament injury on lubricin metabolism and the effect of inhibiting tumor necrosis factor alpha on chondroprotection in an animal model. Arthritis Rheum. 2009;60:2997–3006. doi: 10.1002/art.24800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Englund M, Roos EM, Lohmander LS. Impact of type of meniscal tear on radiographic and symptomatic knee osteoarthritis: A sixteen-year followup of meniscectomy with matched controls. Arthritis Rheum. 2003;48:2178–2187. doi: 10.1002/art.11088. [DOI] [PubMed] [Google Scholar]
- 19.Fleming BC, Brady MF, Bradley MP, Banerjee R, Hulstyn MJ, Fadale PD. Tibiofemoral compression force differences using laxity- and force-based initial graft tensioning techniques in the anterior cruciate ligament-reconstructed cadaveric knee. Arthroscopy. 2008;24:1052–1060. doi: 10.1016/j.arthro.2008.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fleming BC, Fadale PD, Hulstyn MJ, et al. The effect of initial graft tension after anterior cruciate ligament reconstruction: A randomized clinical trial with 36-month follow-up. Am J Sports Med. 2013;41:25–34. doi: 10.1177/0363546512464200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fleming BC, Peura GD, Beynnon BD. Factors influencing the output of an implantable force transducer. J Biomech. 2000;33:889–893. doi: 10.1016/s0021-9290(00)00019-1. [DOI] [PubMed] [Google Scholar]
- 22.Haslauer CM, Elsaid KA, Fleming BC, Proffen BL, Johnson VM, Murray MM. Loss of extracellular matrix from articular cartilage is mediated by the synovium and ligament after anterior cruciate ligament injury. Osteoarthritis Cartilage. 2013;21:1950–1957. doi: 10.1016/j.joca.2013.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Heard BJ, Solbak NM, Achari Y, et al. Changes of early post-traumatic osteoarthritis in an ovine model of simulated ACL reconstruction are associated with transient acute post-injury synovial inflammation and tissue catabolism. Osteoarthritis Cartilage. 2013;21:1942–1949. doi: 10.1016/j.joca.2013.08.019. [DOI] [PubMed] [Google Scholar]
- 24.Hunter DJ, Arden N, Conaghan PG, et al. Definition of osteoarthritis on MRI: results of a Delphi exercise. Osteoarthritis Cartilage. 2011;19:963–969. doi: 10.1016/j.joca.2011.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Irrgang JJ, Ho H, Harner CD, Fu FH. Use of the International Knee Documentation Committee Guidelines to assess outcome following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 1998;6:107–114. doi: 10.1007/s001670050082. [DOI] [PubMed] [Google Scholar]
- 26.Jones MH, Spindler KP, Fleming BC, et al. Meniscus treatment and age associated with narrower radiographic joint space width 2 – 3 years after ACL reconstruction: Data from the MOON onsite cohort. Osteoarthritis Cartilage. 2015;23:581–588. doi: 10.1016/j.joca.2014.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jones MH, Spindler KP, Fleming BC, et al. Predictors of lateral compartment joint space difference two or more years after ACL reconstruction: Data from the MOON onsite cohort. Osteoarthritis Cartilage. 2015;23:A280. doi: 10.1016/j.joca.2014.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim SG, Kurosawa H, Sakuraba K, Ikeda H, Takazawa S. The effect of initial graft tension on postoperative clinical outcome in anterior cruciate ligament reconstruction with semitendinosus tendon. Arch Orthop Trauma Surg. 2006;126:260–264. doi: 10.1007/s00402-005-0045-x. [DOI] [PubMed] [Google Scholar]
- 29.Magnussen RA, Carey JL, Spindler KP. Does autograft choice determine intermediate-term outcome of ACL reconstruction? Knee Surg Sports Traumatol Arthrosc. 2011;19:462–472. doi: 10.1007/s00167-010-1277-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McNulty AL, Rothfusz NE, Leddy HA, Guilak F. Synovial fluid concentrations and relative potency of interleukin-1 alpha and beta in cartilage and meniscus degradation. J Orthop Res. 2013;31:1039–1045. doi: 10.1002/jor.22334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mohtadi NG, Chan DS, Dainty KN, Whelan DB. Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2011:CD005960. doi: 10.1002/14651858.CD005960.pub2. [DOI] [PMC free article] [PubMed]
- 31a.Nicholas SJ, D’Amato MJ, Mullaney MJ, Tyler TF, Kolstad K, McHugh MP. A prospective randomized double-blind study on the effects of initial graft tension on knee stability after anterior cruciate ligament reconstruction. A, J Sports Med. 2004;32:1881–1886. doi: 10.1177/0363546504265924. [DOI] [PubMed] [Google Scholar]
- 32.Patel RR, Hurwitz DE, Bush-Joseph CA, Bach BR, Andriacchi TP. Comparison of clinical and dynamic knee function in patients with anterior cruciate ligament deficiency. Am J Sports Med. 2003;31:68–74. doi: 10.1177/03635465030310012301. [DOI] [PubMed] [Google Scholar]
- 33.Peterfy C, Li J, Zaim S, et al. Comparison of fixed-flexion positioning with fluoroscopic semi-flexed positioning for quantifying radiographic joint-space width in the knee: test-retest reproducibility. Skeletal Radiology. 2003;32:128–132. doi: 10.1007/s00256-002-0603-z. [DOI] [PubMed] [Google Scholar]
- 34.Peterfy CG, Guermazi A, Zaim S, et al. Whole-organ magnetic resonance imaging score (WORMS) of the knee in osteoarthritis. Osteoarthritis Cartilage. 2004;12:177–190. doi: 10.1016/j.joca.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 35.Qazi AA, Folkesson J, Pettersen PC, Karsdal MA, Christiansen C, Dam EB. Separation of healthy and early osteoarthritis by automatic quantification of cartilage homogeneity. Osteoarthritis and Cartilage. 2007;15:1199–1206. doi: 10.1016/j.joca.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 36.Reinke EK, Spindler KP, Lorring D, et al. Hop tests correlate with IKDC and KOOS at minimum of 2 years after primary ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:1806–1816. doi: 10.1007/s00167-011-1473-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1:64. doi: 10.1186/1477-7525-1-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)--development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28:88–96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- 39.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Rel Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 40.van Kampen A, Wymenga AB, van der Heide HJL. The effect of different graft tensioning in anterior cruciate ligament reconstruction: A prospective randomized study. Arthroscopy. 1998;14:845–850. doi: 10.1016/s0749-8063(98)70022-2. [DOI] [PubMed] [Google Scholar]
- 41.Ventura CP, Wolchok J, Hull ML, Howell SM. An implantable transducer for measuring tension in an anterior cruciate ligament graft. J Biomech Engin. 1998;120:327–333. doi: 10.1115/1.2797998. [DOI] [PubMed] [Google Scholar]
- 42.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 43.Wasserstein D, Huston LJ, Nwosu S, Group M, Spindler KP. KOOS pain as a marker for significant knee pain two and six years after primary ACL reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) prospective longitudinal cohort study. Osteoarthritis Cartilage. 2015;23:1674–1684. doi: 10.1016/j.joca.2015.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wilson TW, Zafuta MP, Zobitz M. A biomechanical analysis of matched bone-patellar tendon-bone and double-looped semitendinosus and gracilis tendon grafts. Am J Sports Med. 1999;27:202–207. doi: 10.1177/03635465990270021501. [DOI] [PubMed] [Google Scholar]
- 45.Woo SL-Y, Kanamori A, Zeminski J, Yagi M, Papageorgiou CD, Fu FH. The effectiveness of reconstruction of the anterior cruciate ligament with hamstrings and patellar tendon - A cadaveric study comparing anterior tibial and rotational loads. J Bone Joint Surg Am. 2002;84:907–914. doi: 10.2106/00004623-200206000-00003. [DOI] [PubMed] [Google Scholar]
- 46.Xie X, Xiao Z, Li Q, et al. Increased incidence of osteoarthritis of knee joint after ACL reconstruction with bone-patellar tendon-bone autografts than hamstring autografts: a meta-analysis of 1,443 patients at a minimum of 5 years. Eur J Orthop Surg Traumatol. 2015;25:149–159. doi: 10.1007/s00590-014-1459-3. [DOI] [PubMed] [Google Scholar]
- 47.Yasuda K, Tsujino J, Tanabe Y, Kaneda K. Effects of initial graft tension on clinical outcome after anterior cruciate ligament reconstruction - Autogenous doubled hamstring tendons connected in series with polyester tapes. Am J Sports Med. 1997;25:99–106. doi: 10.1177/036354659702500120. [DOI] [PubMed] [Google Scholar]
- 48.Yoshiya S, Kurosaka M, Ouchi K, Kuroda R, Mizuno K. Graft tension and knee stability after anterior cruciate ligament reconstruction. Clin Orthop Rel Res. 2002;394:154–160. doi: 10.1097/00003086-200201000-00018. [DOI] [PubMed] [Google Scholar]