Abstract
Background:
Information in society and in health care is currently undergoing a transition from paper to digital formats, and the main source of information will probably be electronic in the future.
Objective:
To explore patients’ use and perceptions of the patient information leaflet included in the medication package, and their attitude towards a transition to an electronic version.
Methods:
The data was collected during October to November 2014 among individuals in South-Eastern Sweden, using a questionnaire (n=406, response rate 78%) and interviews (n=15).
Results:
The questionnaire showed that the majority of the respondents (52%) occasionally read the patient information leaflet, 37% always read it, and 11% never read it. Almost half of the patients (41%) were positive towards reading the patient information leaflet electronically while 32% were hesitant and 26% neutral. A majority of the patients would request to get the patient information leaflet printed at the pharmacy if it was not included in the package. There were differences in attitude related to age and gender. The interviews showed that patients had mixed views on a transition to an electronic patient information leaflet. The patients perceived several positive aspects with an electronic patient information leaflet but were concerned about elderly patients.
Conclusion:
Although many were positive towards reading the patient information leaflet electronically, the majority prefer the patient information leaflet in paper form. Providing appropriate and useful eHealth services for patients to access the patient information leaflet electronically, along with education, could prepare patients for a transition to electronic patient information leaflet.
Keywords: Drug Labeling, Telemedicine, Patient Medication Knowledge, Patient Education as Topic, Pharmacies, Surveys and Questionnaires, Qualitative Research, Sweden
INTRODUCTION
For safe, effective drug treatment, it is important that patients are well informed, understand which medicines they are supposed to take and how to use them, and understand the expected benefits and possible side effects of the drugs.1,2,3,4 Patient adherence to drug treatment is vital to reach the desired outcome. However, non-adherence to treatment is common for various reasons, such as adverse drug events and lack of motivation, knowledge or information.1,5,6 Patients often misunderstand or forget much of the information given by their physician or other healthcare professionals during consultation.7,8 Written information is known to increase the amount of information retained.9,10
In the EU, pharmaceutical companies are legally required to include a patient information leaflet in all medication packages.2,11 The patient information leaflet is also often referred to as the package information leaflet, the patient medication leaflet, consumer medicines information, the package leaflet, or the package insert. The content of the patient information leaflet should be in accordance with the Summary of Product Characteristics (SmPC). The purpose of the patient information leaflet is to communicate important information from the manufacturer to the patient in order to ensure that the medication is taken correctly and used as intended.12
Providing a patient information leaflet can improve patients’ knowledge about the medication, but reading the patient information leaflet can also result in non-adherence.2,11,13 Several studies have shown that the current patient information leaflets do not meet the needs of all patients.2,14,15,16 Problems that have been described include the text being too long and the font size too small, the presence of incomprehensible medical terms, the misinterpretation of benefits and risks, the complicated folding to fit it in the medication package, exclusion of ethnic minorities because of second language issues, and variations in the information between different brands of generically identical drugs. In Sweden, the patient information leaflets for all registered drugs are available online via www.fass.se, provided by LIF, a professional association representing research-based pharmaceutical companies in Sweden. The website www.fass.se is being increasingly used, with approximately four million visits each month; more than half of the visitors are patients and the rest are healthcare professionals.17 However, it is not known how Swedish patients feel about accessing or reading their medication information electronically compared with receiving the paper leaflet.
Today, patients are becoming increasingly engaged in their own health care, a development that is supported by the growth of information technology in our society.18,19 The internet is becoming an increasingly important source of health information; the majority of adults seek health information online, although the quality of this information is variable.10,19,20,21,22 Informed, motivated patients are more likely to continue using healthcare services, to value and maintain relationships with healthcare providers, to comply with treatment, and to take an active role in their own health care.23,24,25 During recent decades, the prescribing of medications and handling of information in the medication management process have gone through a major transition from paper-based to electronic.4,26 Medical information and services, communication, and education for patients are also becoming increasingly digitalised and mobile.27,28 For example, patients in Sweden can access information regarding current prescriptions online29 and, in some regions, patients can access their electronic health records online.30 Different countries vary in the degree to which eHealth services are implemented and in the use of the internet by their citizens.27,31 In Australia, the patient information leaflet (Consumer Medicine Information) is not required to be included in the medication package, and can be provided electronically instead, but the dissemination of the information is not as high as desirable.32
To meet the future needs of patients, it is desirable to improve the content of the patient information leaflet, but it is also important to investigate different forms for communicating the information to the patient, for example by providing the patient information leaflet online or integrated in other eHealth services.33 One positive impact with an electronic patient information leaflet is that the information can be instantly updated instead of it taking years for updates to reach the patient. Using an electronic patient information leaflet also offers opportunities for increased availability with mobile devices, and increased usability by allowing the patient to change the font size or use an audio version of the text, or to get difficult medical terms explained.34,35 Other possible effects are that more countries could share the same medication package, and that unnecessary disposal of medication could be minimised. Previous research internationally have explored different aspects of written medication information provided to patients, such as how to improve the content and format of the information as well as increasing the dissemination among patients.32,33,36,37 However, research with focus on patient attitudes towards receiving the information electronically compared with paper form is limited.
The aim of this study was to explore patients’ use and perceptions of the current patient information leaflets included in medication packages, as well as their attitudes to a potential transition to an electronic version.
METHODS
A mixed methods approach was used by collecting the data via a questionnaire and interviews. Both included similar questions regarding current usage of the patient information leaflet, and views on reading the patient information leaflet electronically in the future. However, while the questionnaire included only a few multiple choice questions, the interviews aimed to provide a greater understanding regarding views and preferences.
Questionnaire
The questionnaire was developed for this study based on previous research and experience with questionnaires. The questionnaire was reviewed by four researchers from different disciplines and tested among a few individuals before the large scale study. The questionnaire in Swedish comprised six questions along with those relating to the respondents’ age and gender, and also included a short description of what a patient information leaflet is (
).
Data was collected at seven pharmacies in South-Eastern Sweden from October 10th to November 14th 2014. The pharmacies of different sizes and in different types of location (i.e. small city, medium sized city, and hospital) were selected to capture a wide range of patients. One or two of the researchers visited each pharmacy for two to five hours at different times during the day to collect data using the questionnaires. All individuals visiting one of the participating pharmacies during one such occasion in order to collect prescription medication were included in the study, and asked to participate by filling out the questionnaire after being informed of the research. Before the study it was calculated that at least 384 answers were needed to answer the main question (How would you feel about reading the patient information leaflet electronically on a computer, phone or tablet?), for a population of more than 100 000, with a margin of error of 5% and a confidence level of 95%. It was decided that data was going to be collected until at least 400 answers to the questionnaire had been collected.
Interviews
The interviews followed a pre-defined interview guide comprising 19 questions (Online appendix). The semi-structured interviews were conducted face-to-face or via telephone during November 2014. Each interview lasted between 10 and 25 minutes, was recorded with the respondent’s permission and was transcribed.
The participants for the interviews were strategically selected from different settings in South-Eastern Sweden in order to include individuals of different ages, genders, and experience with medication. Participants were included until saturation in the answers were found and sufficient data were considered to be achieved. At the end of the interview, the respondents were presented a number of assumed benefits of an electronic patient information leaflet compared with the paper-based form: (1) instant updates can be made instead of waiting years for the updates to reach the patient, (2) there could be increased usability, allowing the patient to change the font size, use an audio version of the text, or have difficult medical terms explained, and (3) there could be environmental benefits because of decreased disposal of medication as a result of information updates. After receiving information of assumed benefits, the respondents were again asked for their views about accessing and reading the patient information leaflet online.
Analysis of data
The responses to the questionnaires were analysed using SPSS software (IBM SPSS statistics 22). The chi-squared test was used to analyse the relationship between the respondents’ answers and their age and gender, with p<0.05 as the level for a significant relationship. When analysing possible differences in attitude between age groups in this study, the respondents were divided in two (aged 55 or younger and over 55 years). The manifest content of the transcribed interviews was analysed using qualitative description method.38,39 The data were analysed and categorised using QSR NVivo 10 software. Representative quotes were selected for the main aspect of the interviews to exemplify the different perspectives. Quotes were then translated from Swedish to English. One researcher analysed all the interviews and the results were validated by two other researchers.
Ethical considerations
The ethical implications of the study were considered based on the guidelines of the Ethics Committee of South-East Sweden. Personal identifiers were removed or disguised, and data was handled in a way so that the respondents cannot be identified.
RESULTS
Questionnaire
In total, 523 pharmacy customers were included and asked to complete the questionnaire; 95 individuals declined and 406 accepted and thus responded to the questionnaire (response rate 78%). A summary of participant characteristics is given in Table 1. Approximately half of the respondents (49%, n=200) were aged 55 years or younger.
Table 1.
Respondents’ characteristics (n=406).
| Respondents | Respondents (%) |
|---|---|
| Gender | |
| Female | 253 (62%) |
| Male | 153 (38%) |
| Age (years) | |
| ≤ 25 | 28 (7%) |
| 26-55 | 172 (42%) |
| 56-85 | 203 (50%) |
| ≥ 86 | 3 (<1%) |
| Use of medications | |
| Continuously | 233 (57%) |
| Periodically | 61 (15%) |
| Occasionally | 112 (28%) |
The majority of the respondents (52%, n=213) occasionally read the patient information leaflet, 37% (n=150) always read it, and 11% (n=43) never read it. There was a significant difference between genders in how often they read the patient information leaflet (p<0.05), with females reading it more often than males, but there were no significant differences among age groups (Figure 1).
Figure 1.
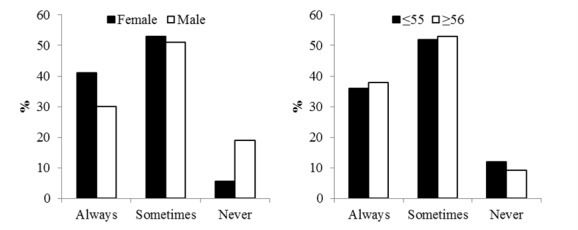
Answers to the question “How often do you read the information on the patient information leaflet?”, according to gender (left) and age group (right).
The majority of respondents (55%, n=225) preferred to read the patient information leaflet in its current form included in the medication package, 17% (n=69) would prefer it in electronic form, 13% (n=52) preferred it printed at the pharmacy, 11% had no opinion and 4% gave more than one answer (Figure 2).
Figure 2.
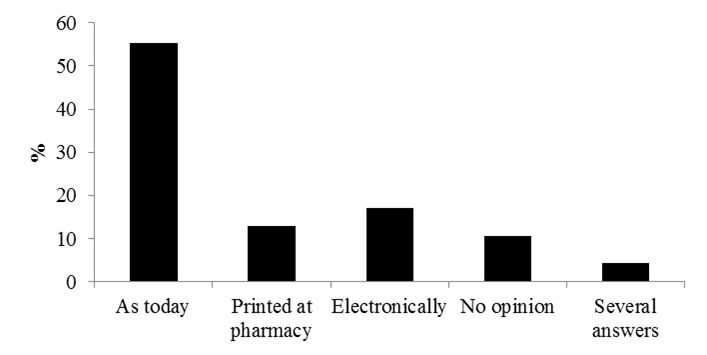
Answers to the multiple-choice question “How would you prefer to receive the information currently provided in the patient information leaflet?” with four alternatives. Some of the respondents chose several alternatives.
When asked how they would feel about reading the patient information leaflet electronically on a computer, phone or tablet, almost half of the participants were positive (41%, n=168) while 32% (n=131) were hesitant/uncertain and 26% (n=107) were neutral. For this question, there was a significant difference (p<0.05) in attitudes between respondents aged 55 years or younger and those aged 56 years or older; the younger respondents were more positive (Figure 3), but there was no significant difference between the genders.
Figure 3.
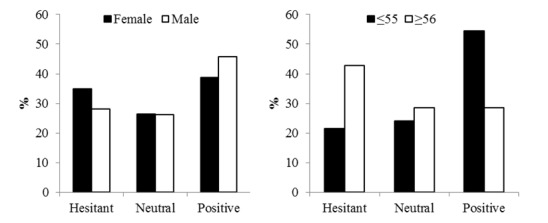
Answers to the question “How would you feel about reading the patient information leaflet electronically on a computer, phone or tablet?” according to gender (left) and age group (right).
If the patient information leaflet was not included in the package, more than half (54%, n=220) stated that they would ask to get the patient information leaflet printed at the pharmacy, 26% (n=104) stated that they would not, and 20% (n=81) said that they did not know. There was a significant (p<0.05) difference between the two age groups, with those aged 56 years or older more often stating that they would ask to get the patient information leaflet printed (Figure 4), but there was no significant difference between the genders.
Figure 4.
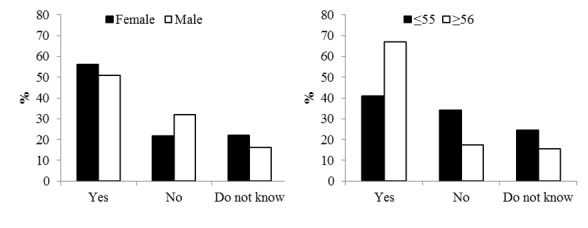
Answers to the question “If the patient information leaflet was not included in the medication package, would you ask to get it printed at the pharmacy?” according to gender (left) and age group (right).
Interviews
Fifteen respondents participated in the interviews (eight female and seven male); they were aged between 24 and 89 years with a mean age of 49 years. The respondents’ experience with medications varied; some used medications daily and some only occasionally. A few respondents also helped another family member with their medication.
Information regarding medications:
The respondents obtained information regarding medications from the prescriber, pharmacists at the pharmacy, a family member with more knowledge regarding medications, the patient information leaflet included in the package, online information sources, or advertisements.
“I get the information from the patient information leaflet and, of course, first of all from the physician.” (female, 67 years)
“Primarily online via fass.se, and secondarily I turn to my doctor” (female, 52 years)
Many of the respondents used the internet to find information regarding medications, but a few had never felt the need or been able to use the internet for this reason. The most commonly mentioned source of information online was www.fass.se but several said that they used Google to find the information they wanted.
“I have read fass.se sometimes, if there was something I wanted to investigate more deeply.” (female, 45 years)
“I’d probably just ‘google’ it and see what came up, see what was believable. Often there are forums where people have written about similar side effects or whatever I want to know about regarding the drug, and then you can probably find your way there.” (female, 24 years)
Usage of and perceptions about the patient information leaflet included in medication packages:
Almost all the respondents answered that they read the patient information leaflet included in the medication package, at least occasionally. Some said that they almost always read the patient information leaflet to find out more about their treatment and gain a better understanding of it. The reasons for reading the patient information leaflet among those who only read it sometimes included: the medication was new to them, the type of medication, questions regarding use during pregnancy, suspicion of adverse effects, reports in the mass media regarding the medication, or questions regarding mixing the medication with alcohol.
“A new medication means that I will read the patient information leaflet.” (female, 45 years)
“It can depend on the type of medication. If it is something I expect or believe has side effects, I am more anxious to check them than the medication I believe or expect is more harmless. In that case I may not care as much about looking at the patient information leaflet at all.” (male, 32 years)
When asked which information they read in the patient information leaflet, almost all the respondents mentioned information regarding adverse effects. Other issues mentioned were information regarding dosage and user instructions. The respondents generally thought the current patient information leaflet was good, but most of them also perceived problems including: the text is too small, it can be difficult to find the information they are searching for, or the language is difficult to understand. Other negative aspects included that the current patient information leaflet in paper form is difficult to get back into the package once they had read it, and that it was easily lost because of that. Most of the respondents did not lack any information in the patient information leaflet, but one respondent was missing information regarding interactions with other medications.
“A lot of text, often written in small letters, and it can be difficult to find just what you’re looking for.” (female, 24 years)
“It’s difficult to get it back into the package once you’ve unfolded it. It gets wrinkled and messy or you throw it away and then it’s not there the next time you need it.” (female, 34 years) Preferred format for medication information:
More than half of the respondents regarded the electronic format as more practical, but some preferred to read the patient information leaflet in paper form (included in the package), or to get the patient information leaflet printed at the pharmacy. Even among those who preferred reading the information electronically, some still wanted the patient information leaflet to be included in the medication package. Some preferred the electronic form for themselves but did not think it would work for all patient groups, for example the elderly.
“I would like to have it in my mobile phone, I think.” (male, 24 years)
“I think that it is probably good to have it as it is today in paper form but also to have it on Fass.se online. I believe there are different target groups, elderly people, for example, who may not have access to the Internet.” (female, 24 years)
Perceptions of a possible transition to electronic patient information leaflets:
Most of the respondents felt positive about reading the patient information leaflet electronically, for example on a computer, smart phone or tablet, but a few were more hesitant or negative. Possible problems with electronic patient information leaflets described by the respondents included worries about the elderly not being able to access the medication electronically, problems related to privacy, or trouble finding the right information for their specific medication.
“It would be wonderful! And I’d be more curious!” (male, 48 years)
“If I look to myself, it would be more convenient to get it online. But for my parents, it would be a disaster. They have no computer and need the paper form.” (female, 52 years)
Some respondents said that if the information was going to be relayed electronically, they wanted some form of guidance to find the right information, for example by getting an email, a link, or an SMS (text message), or via a chip (e.g. NFC, near field communication) or code (e.g. QR, quick response) on the medication package.
“The dream would be to get it in an email when I’ve received a prescription.” (female, 45 years)
“Maybe it’s not super easy to go to fass.se and find it there. One could imagine a QR code on the package that you can scan, or maybe an NFC chip on the package. There should be some kind of link between the medicine I receive in my hand, and the information I get. It is easy to confuse two similar names, which might have serious consequences if you receive the wrong information.” (male, 32 years)
The respondents described several benefits associated with an electronic patient information leaflet: being able to increase the font size, being able to access other visual instructions, or it being easier to find the information they seek without having to read the whole patient information leaflet.
“I can come up with several uses and benefits. If some medicines need more instructions, there is the possibility of adding pictures or instructional videos.” (male, 32 years)
“From an environmental point of view I think computers are better, and it might be easier to find exactly the information you want without having to read a lot of unnecessary text, and it might be faster.” (female, 34 years)
After receiving the information regarding the possible benefits of an electronic patient information leaflet, most respondents had a more positive view on the possible transition to an electronic patient information leaflet. However, their previously described problems or worries remained the same.
DISCUSSION
The study showed that although most patients read the patient information leaflets included in medication packages at least sometimes, they perceived several weaknesses associated with this format. Many patients use electronic medication information to some extent. The patients had mixed views on a future transition to electronic patient information leaflets. Although many were positive towards reading the patient information leaflet electronically, the majority still prefer paper patient information leaflet included in the medication package. Patients saw several positive aspects associated with an electronic patient information leaflet, but were concerned about elderly patients who they believe depend on paper-based information. The majority of patients stated that they would ask to get the patient information leaflet printed at the pharmacy if it was not included in the package. The results indicated differences in attitude related to age and gender.
Differences in the results between the questionnaire and the interviews
There were some differences in attitude to electronic patient information leaflets between the findings of the questionnaire and those of the interviews, with the interviews indicating a more positive attitude. There are several possible explanations for this. The interviews allowed the respondents to explain their concerns regarding electronic patient information leaflets, revealing that many respondents were positive towards reading them electronically themselves but were worried about the elderly being unable to read them electronically. Perhaps the more negative attitude seen in the questionnaires reflected worries about others rather than themselves. The interviews also indicated that a negative attitude might not reflect on the electronic format itself, but rather on insecurities about how to find the right patient information leaflet, which could be managed if there was a way to guide the patient to the correct patient information leaflet for their medication, for example via an SMS, email, chip or digital barcode, or even including the patient information leaflet with other eHealth patient services such as their online list of current medications. The interviews also showed that providing information on the possible benefits of electronic patient information leaflets could lead to a more positive attitude. Because electronic patient information leaflets have probably not been considered by most patients before, this short questionnaire without any background information could have increased the likelihood of patients being in favour of the current form rather than opening up to something new.
Respondents’ perceptions of current information sources
The sources the respondents used to obtain information regarding their medications were similar to those mentioned in other studies.40,41,42,43 Online sources are becoming increasingly important for health information19-21, but some of the respondents in this study were unsure of how to find correct, reliable information about their medications. The questionnaire showed that the majority of respondents wanted the patient information leaflet printed at the pharmacy if it was not included in the package. However, if a similar question had been included asking if the respondents would want, for example, an email with their patient information leaflet sent to them, perhaps a large proportion would prefer that. The findings regarding usage and perceptions of the patient information leaflet were in line with those of other studies, and the problems associated with the patient information leaflet were also similar to those described in other studies.2,13,34,44 There are a large number of studies internationally on how to improve the content and format of written information about individual medications to meet the need of patients.33,45,46
The results showed that patients aged 56 years or older had a more negative attitude towards reading the patient information leaflet electronically. The study also indicated that females read the patient information leaflets more often than males, and that males might be more positive towards an electronic patient information leaflet than females. Problems related to the elderly being excluded or affected negatively when information or services are digitalised are often discussed when introducing eHealth services.47 However, some of the weaknesses associated with the current patient information leaflet format, like small font size, too much information, and difficult language, represent major issues for the elderly.2,14 Thus, the potential for increased usability with electronic information may be beneficial for the elderly as well. In addition, problems with the elderly being excluded from the digital society are an issue that will decrease with the passage of time.
Transition towards electronic information formats
Information in society and in health care is currently undergoing a transition from paper to digital formats, and the main source of information will probably be electronic in the future. Digital information provides several benefits, such as increased availability, mobility, usability and individualisation, instant updates, and benefits for the environment as a result of the decreased use of paper and wastage of drugs. At the same time, current information available online from different sources varies in quality and reliability, and requires the patient to know how to find the information.
It seems very likely that patient information leaflets will primarily be provided in an electronic format in the future. For example, in Australia, pharmaceutical companies are no longer obliged to provide consumer medicine information in the medication package, as long as it is provided online or is printed at the pharmacy.32 However, the dissemination and use of the written medicines information in Australia is lower than desired and there are several studies on how to improve this.32,45 Our results show that the majority of patients prefer the patient information leaflet included in the medication package, but many are interested in and ready to use electronic sources. As with other new interventions, it may take time to prepare users for the transition. Before, during, and after such a transition, it is important to help and educate patients to find the correct information and to provide alternatives such as a patient information leaflet printed at the pharmacy. Providing good services for patients to be able to access the patient information leaflet electronically, perhaps integrated with other eHealth services such as the patients’ list of current medications, could make patients less dependent on the paper patient information leaflet included in the medication package and prepare them for a future transition to an electronic patient information leaflet.
Methodological strengths and limitations
The mixed methods approach used in this study is one of its strengths, with the questionnaire providing quantitative results, and the interviews providing deeper insight to prevailing attitudes. However, a larger population might have revealed significant differences between age groups and genders for more questions and made it possible to detect differences related to experience with medications or the type of pharmacies the patients are visiting. The participants for both the questionnaire and the interviews were recruited from a population in South-Eastern Sweden in small and medium-sized cities, thus limiting generalisation of the results to large cities and other countries. The inclusion of respondents who visit a pharmacy is known to result in a slightly unrepresentative population, since some patient groups (such as the elderly) may not visit the pharmacy themselves but instead send a relative or caretaker.48 Some respondents helped older relatives with their medication and their answers seemed to reflect concerns from the perspective of the elderly as well. However, future research should be designed to collect information directly from older patients.
Future studies
Future research should study patient needs related to the content, form, and design of the patient information leaflet. Different approaches for providing the patient information leaflet electronically to patients should be evaluated, such as directing patients to the correct online information using an SMS, an email, a chip or a QR code on the medication package. Other approaches that could be explored include integrating the patient information leaflet into other patient services related to their medication. Studies similar to this one should be performed when new services have been provided and patients are more used to reading the patient information leaflet electronically.
Practical implications
It seems likely that the main format for the patient information leaflet will be electronic in the future. In order to prepare patients for a future transition to electronic patient information leaflets it is desirable that health care provide appropriate services so that patients can access the patient information leaflet electronically, perhaps integrated with other eHealth services, along with increasing the available information and education resources regarding electronic services.
CONCLUSIONS
The study showed that most patients read the patient information leaflets included in medication packages at least sometimes but perceived several weaknesses associated with this paper form. The patients had mixed views on transitioning to an electronic patient information leaflet. They saw several positive aspects associated with a future electronic patient information leaflet, but were concerned about elderly patients depending on paper-based information. Although many patients were positive about reading the patient information leaflet electronically, the majority still prefer the patient information leaflet in paper form as currently included in the medication package. A future transition to electronic patient information leaflet should therefore be supported by extensive information and education to patients regarding electronic services.
ACKNOWLEDGEMENTS
The authors would like to thank Ulrika Lönnbom for assistance during the design of questionnaires and interviews, and participating in the collecting of data. The authors would also like to thank Professor Göran Petersson for valuable feedback on the manuscript.
Footnotes
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Funding: The study was funded by grants from the trade association for the research-based pharmaceutical industry in Sweden, “Läkemedelsindustriföreningen” (LIF). The study was designed and conducted independent of the funding organisation.
Contributor Information
Tora Hammar, Researcher. eHealth Institute, Department of Medicine and Optometry, Linnaeus University. Kalmar (Sweden). tora.hammar@lnu.se.
Anna-Lena Nilsson, Researcher. eHealth Institute, Department of Medicine and Optometry, Linnaeus University. Kalmar (Sweden). anna-lena.nilsson@lnu.se.
Bo Hovstadius, Associate professor, research fellow. eHealth Institute, Department of Medicine and Optometry, Linnaeus University. Kalmar (Sweden). bo.hovstadius@lnu.se.
References
- 1.Kuntz JL, Safford MM, Singh JA, Phansalkar S, Slight SP, Her QL, Lapointe NA, Mathews R, O’Brien E, Brinkman WB, Hommel K, Farmer KC, Klinger E, Maniam N, Sobko HJ, Bailey SC, Cho I, Rumptz MH, Vandermeer ML, Hornbrook MC. Patient-centered interventions to improve medication management and adherence: a qualitative review of research findings. Patient Educ Couns. 2014;97(3):310–326. doi: 10.1016/j.pec.2014.08.021. doi: 10.1016/j.pec.2014.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schwappach DL, Mulders V, Simic D, Wilm S, Thurmann PA. Is less more? Patients’ preferences for drug information leaflets. Pharmacoepidemiol Drug Saf. 2011;20(9):987–995. doi: 10.1002/pds.2212. doi: 10.1002/pds.2212. [DOI] [PubMed] [Google Scholar]
- 3.Ekedahl A, Hoffman M. Patients’ information on their prescribed current treatment. J Pharm Health Serv Res. 2012;3(2):79–84. doi: 10.1111/j.1759-8893.2012.00086.x. [Google Scholar]
- 4.Hammar T. eMedication –improving medication management using information technology. [Doctoral dissertation] Kalmar: Linnaeus University; 2014. [Google Scholar]
- 5.Topinkova E, Baeyens JP, Michel JP, Lang PO. Evidence-based strategies for the optimization of pharmacotherapy in older people. Drugs Aging. 2012;29(6):477–494. doi: 10.2165/11632400-000000000-00000. doi: 10.2165/11632400-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 6.Vermeire E, Hearnshaw H, Van Royen P, Denekens J. Patient adherence to treatment: three decades of research. A comprehensive review. J Clin Pharm Ther. 2001;26(5):331–342. doi: 10.1046/j.1365-2710.2001.00363.x. [DOI] [PubMed] [Google Scholar]
- 7.Kessels RP. Patients’ memory for medical information. J R Soc Med. 2003;96(5):219–222. doi: 10.1258/jrsm.96.5.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kenny T, Wilson RG, Purves IN, Clark J, Sr, Newton LD, Newton DP, Moseley DV. A PIL for every ill? Patient information leaflets (PILs): a review of past, present and future use. Fam Pract. 1998;15(5):471–479. doi: 10.1093/fampra/15.5.471. [DOI] [PubMed] [Google Scholar]
- 9.Koo MM, Krass I, Aslani P. Factors influencing consumer use of written drug information. Ann Pharmacother. 2003;37(2):259–267. doi: 10.1177/106002800303700218. [DOI] [PubMed] [Google Scholar]
- 10.Treweek SP. Computer-generated Patient Education Materials: Do They Affect Professional Practice?: A Systematic Review. J Am Med Inform Assoc. 2002;9(4):346–358. doi: 10.1197/jamia.M1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bjerrum L, Foged A. Patient information leaflets-helpful guidance or a source of confusion? Pharmacoepidemiol Drug Saf. 2003. 12(1):55–59. doi: 10.1002/pds.795. [DOI] [PubMed] [Google Scholar]
- 12.Herber OR, Gies V, Schwappach D, Thurmann P, Wilm S. Patient information leaflets: informing or frightening? A focus group study exploring patients’ emotional reactions and subsequent behavior towards package leaflets of commonly prescribed medications in family practices. BMC Fam Pract. 2014;15:702. doi: 10.1186/1471-2296-15-163. doi: 10.1186/1471-2296-15-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nathan JP, Zerilli T, Cicero LA, Rosenberg JM. Patients’ use and perception of medication information leaflets. Ann Pharmacother. 2007;41(5):777–782. doi: 10.1345/aph.1H686. [DOI] [PubMed] [Google Scholar]
- 14.Liu F, Abdul-Hussain S, Mahboob S, Rai V, Kostrzewski A. How useful are medication patient information leaflets to older adults? A content, readability and layout analysis. Int J Clin Pharm. 2014;36(4):827–834. doi: 10.1007/s11096-014-9973-2. doi: 10.1007/s11096-014-9973-2. [DOI] [PubMed] [Google Scholar]
- 15.Pander Maat H, Lentz L. Improving the usability of patient information leaflets. Patient Educ Couns. 2010;80(1):113–119. doi: 10.1016/j.pec.2009.09.030. doi: 10.1016/j.pec.2009.09.030. [DOI] [PubMed] [Google Scholar]
- 16.Berry DC, Raynor DK, Knapp P, Bersellini E. Patients’ understanding of risk associated with medication use: impact of European Commission guidelines and other risk scales. Drug Saf. 2003;26(1):1–11. doi: 10.2165/00002018-200326010-00001. [DOI] [PubMed] [Google Scholar]
- 17.Hammar T, editor. communication with Kristina von Sydow, manager FASS, LIF (de forskande läkemedelsföretagen) 2015 [Google Scholar]
- 18.Powell JA, Darvell M, Gray JA. The doctor, the patient and the world-wide web: how the internet is changing healthcare. J R Soc Med. 2003;96(2):74–76. doi: 10.1258/jrsm.96.2.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bylund CL, Gueguen JA, Sabee CM, Imes RS, Li Y, Sanford AA. Provider-patient dialogue about Internet health information: an exploration of strategies to improve the provider-patient relationship. Patient Educ Couns. 2007;66(3):346–352. doi: 10.1016/j.pec.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 20.Kim KY, Metzger A, Wigle PR, Choe PJ. Evaluation of online consumer medication information. Res Social Adm Pharm. 2011;7(2):202–207. doi: 10.1016/j.sapharm.2010.04.003. doi: 10.1016/j.sapharm.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 21.McMullan M. Patients using the Internet to obtain health information: how this affects the patient-health professional relationship. Patient Educ Couns. 2006;63(1-2):24–28. doi: 10.1016/j.pec.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 22.Eysenbach G, Powell J, Kuss O, Sa ER. Empirical studies assessing the quality of health information for consumers on the world wide web: a systematic review. JAMA. 2002;287(20):2691–2700. doi: 10.1001/jama.287.20.2691. [DOI] [PubMed] [Google Scholar]
- 23.Naik Panvelkar P, Saini B. Measurements of patient satisfaction with community pharmacy services: A review. Pharm World Sci. 2009;31(5):525–537. doi: 10.1007/s11096-009-9311-2. doi: 10.1007/s11096-009-9311-2. [DOI] [PubMed] [Google Scholar]
- 24.Asadi-Lari M, Tamburini M, Gray D. Patients’ needs, satisfaction, and health related quality of life: towards a comprehensive model. Health Qual Life Outcomes. 2004;2:702. doi: 10.1186/1477-7525-2-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Robben S, van Kempen J, Heinen M, Zuidema S, Olde Rikkert M, Schers H, Melis R. Preferences for receiving information among frail older adults and their informal caregivers: a qualitative study. Fam Pract. 2012;29(6):742–747. doi: 10.1093/fampra/cms033. doi: 10.1093/fampra/cms033. [DOI] [PubMed] [Google Scholar]
- 26.Odukoya OK, Chui MA. e-Prescribing: characterisation of patient safety hazards in community pharmacies using a sociotechnical systems approach. BMJ Qual Saf. 2013;22(10):816–825. doi: 10.1136/bmjqs-2013-001834. doi: 10.1136/bmjqs-2013-001834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kreps GL, Neuhauser L. New directions in eHealth communication: opportunities and challenges. Patient Educ Couns. 2010;78(3):329–336. doi: 10.1016/j.pec.2010.01.013. doi: 10.1016/j.pec.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 28.Mosa AS, Yoo I, Sheets L. A systematic review of healthcare applications for smartphones. BMC Med Inform Decis Mak. 2012;12:702. doi: 10.1186/1472-6947-12-67. doi: 10.1186/1472-6947-12-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hammar T, Nyström S, Petersson G, Åstrand B, Rydberg T. Patients satisfied with ePrescribing in Sweden: a survey of a nationwide implementation. J Pharm Health Serv Res. 2011;2(2):97–105. doi: 10.1111/j.1759-8893.2011.00040.x. [Google Scholar]
- 30.Scandurra I, Holgersson J, Lind T, Myreteg G. Development of Patient Access to Electronic Health Records as a Step towards Ubiquitous Public eHealth. European Journal of ePractice. 2013;(20) [Google Scholar]
- 31.Kierkegaard P. E-Prescription across Europe. Health and Technology. 2012;3(3):205–219. [Google Scholar]
- 32.Hamrosi KK, Raynor DK, Aslani P. Pharmacist, general practitioner and consumer use of written medicine information in Australia: are they on the same page? Res Social Adm Pharm. 2014. 10(4):656–668. doi: 10.1016/j.sapharm.2013.10.002. doi: 10.1016/j.sapharm.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 33.Raynor DK, Blenkinsopp A, Knapp P, Grime J, Nicolson DJ, Pollock K, Dorer G, Gilbody S, Dickinson D, Maule AJ, Spoor P. A systematic review of quantitative and qualitative research on the role and effectiveness of written information available to patients about individual medicines. Health Technol Assess. 2007;11(5):1–160. doi: 10.3310/hta11050. [DOI] [PubMed] [Google Scholar]
- 34.Blanck A, Nyblom K. Package leaflets today: a betrayal of Europe's patients. Script Regul Aff. 2012 Aug;:16–17. [Google Scholar]
- 35.EFPIA. Position on shortcomings of the Summary of Product Characteristics and the Package Leaflet and proposals to resolve them. EFPIA (European Federation of Pharmaceutical Industries and Associations) 2014 [Google Scholar]
- 36.Hamrosi KK, Raynor DK, Aslani P. Enhancing provision of written medicine information in Australia: pharmacist, general practitioner and consumer perceptions of the barriers and facilitators. BMC Health Serv Res. 2014;14:702. doi: 10.1186/1472-6963-14-183. doi: 10.1186/1472-6963-14-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Peterson-Clark G, Aslani P, Williams KA. Pharmacists’ online information literacy: an assessment of their use of Internet-based medicines information. Health Info Libr J. 2010;27(3):208–216. doi: 10.1111/j.1471-1842.2010.00891.x. doi: 10.1111/j.1471-1842.2010.00891.x. [DOI] [PubMed] [Google Scholar]
- 38.Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–112. doi: 10.1016/j.nedt.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 39.Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000. 23(4):334–340. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 40.Holappa M, Ahonen R, Vainio K, Hameen-Anttila K. Information sources used by parents to learn about medications they are giving their children. Res Social Adm Pharm. 2012;8(6):579–584. doi: 10.1016/j.sapharm.2012.01.003. doi: 10.1016/j.sapharm.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 41.Narhi U. Sources of medicine information and their reliability evaluated by medicine users. Pharm World Sci. 2007;29(6):688–694. doi: 10.1007/s11096-007-9131-1. [DOI] [PubMed] [Google Scholar]
- 42.Thompson S, Stewart K. Older persons’ opinions about, and sources of, prescription drug information. The International journal of pharmacy practice. 2001;9(3):153–162. doi: 10.1111/j.2042-7174.2001.tb01043.x. [Google Scholar]
- 43.Trewin VF, Veitch GB. Patient sources of drug information and attitudes to their provision: a corticosteroid model. Pharm World Sci. 2003;25(5):191–196. doi: 10.1023/a:1025810603241. [DOI] [PubMed] [Google Scholar]
- 44.Gustafsson J, Kalvemark S, Nilsson G, Nilsson JL. Patient information leaflets-patients’ comprehension of information about interactions and contraindications. Pharm World Sci. 2005;27(1):35–40. doi: 10.1007/s11096-005-1413-x. [DOI] [PubMed] [Google Scholar]
- 45.Hamrosi KK, Aslani P, Raynor DK. Beyond needs and expectations: identifying the barriers and facilitators to written medicine information provision and use in Australia. Health Expect. 2014;17(2):220–231. doi: 10.1111/j.1369-7625.2011.00753.x. doi: 10.1111/j.1369-7625.2011.00753.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Raynor DK. User testing in developing patient medication information in Europe. Res Social Adm Pharm. 2013;9(5):640–645. doi: 10.1016/j.sapharm.2013.02.007. doi: 10.1016/j.sapharm.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 47.Chesser A, Burke A, Reyes J, Rohrberg T. Navigating the digital divide: a systematic review of eHealth literacy in underserved populations in the United States. Inform Health Soc Care. 2016;41(1):1–19. doi: 10.3109/17538157.2014.948171. doi: 10.3109/17538157.2014.948171. [DOI] [PubMed] [Google Scholar]
- 48.Frisk P, Kalvemark-Sporrong S, Wettermark B. Selection bias in pharmacy-based patient surveys. Pharmacoepidemiol Drug Saf. 2014;23(2):128–139. doi: 10.1002/pds.3488. doi: 10.1002/pds.3488. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


