Abstract
Background:
Clozapine is an antipsychotic medication used in treatment resistant schizophrenia. However, clozapine is associated with a significant adverse effect profile and extensive monitoring is required to optimise consumer safety. Traditionally, clozapine can only be prescribed by a psychiatrist and dispensed at a hospital or hospital affiliated pharmacy in Australia. These restrictions could result in significant treatment burden for consumers taking clozapine.
Objective:
To identify (1) the different models of supply that exist for people living in the community taking clozapine in Australia and compare to those in New Zealand and the United Kingdom, and (2) explore how these supply models may impact on consumer burden from the perspective of professionals involved in the supply of clozapine.
Method:
Key informants were interviewed (n=8) from Australia, New Zealand and the United Kingdom regarding how consumers, who lived in the community, accessed clozapine. Data were analysed and led to the development of four clozapine supply models. These four models were further validated by an online survey of a wider sample (n=30). Data were analysed thematically and via simple descriptive statistics.
Results:
Clozapine supply varied depending on location. A secondary care model was utilised in the United Kingdom compared to a community based (primary care) model in New Zealand; Australia utilised a mixture of both secondary and primary care. A key theme from all study participants was that community pharmacy should be utilised to dispense clozapine to consumers living in the community, provided adequate training and safeguards are in place. It was noted that the utilisation of community pharmacies could improve access and flexibility, thereby reducing treatment burden for these consumers.
Conclusion:
There are predominately two models for supply of clozapine to consumers living in the community in Australia, New Zealand and the United Kingdom. One model utilises secondary care facilities and the other community services. Community pharmacy is ideally placed to increase access to clozapine for consumers living in the community, provided appropriate training and support is given to pharmacists providing this professional service.
Keywords: Clozapine, Health Services Accessibility, Community Pharmacy Services, Pharmacies, Schizophrenia, Qualitative Research, Australia
INTRODUCTION
Schizophrenia is a complex mental illness, involving a range of symptoms including cognitive, behavioural and emotional dysfunctions. This includes a combination of positive (e.g. hallucinations and delusions), and negative symptoms (e.g. lack of motivation and social withdrawal), which typically begins in late teenage years and early twenties and for many people continues as a prolonged illness with distressing symptoms.1 Second generation antipsychotics are the first-line treatment for schizophrenia.2 However, if a consumer is either intolerant of, or does not respond adequately to, at least two first-line treatment options, their condition is regarded as treatment resistant. When this occurs the empirical treatment of choice is clozapine.2,3 There are nearly 12,000 people currently taking clozapine in Australia, accounting for approximately 19% of all people with schizophrenia.4
Clozapine is associated with a significant adverse effect profile, such as agranulocytosis and blood dyscrasias.3,5 Consequently, extensive and ongoing monitoring is required for consumer safety, e.g. metabolic, cardiac and haematological testing.6 This can place a significant burden on consumers taking clozapine who live in the community, i.e. stable consumers. In Australia, consumers must come to a hospital pharmacy within a specified time-frame, i.e. 48 hours, after their blood test every 28 days. The combination of monitoring requirements and the restrictive supply arrangements for clozapine, such as the need to attend clinics and to collect medication from a hospital or hospital affiliated pharmacy, could significantly impact on a consumer’s ability to access clozapine. Consequently treatment burden for this group of consumers would be expected to be high.
Treatment burden is a multifaceted concept that relates to the impact that the treatment of a condition has on the consumer. This includes the costs of treatment, time and travel burden, burden of medication or other therapeutic interventions, and access to healthcare services.7 This is an important concept to consider, as it has a direct impact on medication adherence, and subsequently, illness management and wellbeing. Consumers with schizophrenia are prone to a significant number of physical health comorbidities, e.g. diabetes and cardiovascular disease.8 Therefore, it is likely that these consumers may be taking concomitant medication, which can also increase treatment burden through increased medication expense, time to take medication and having to attend multiple health services. This includes the utilisation of both hospital and community pharmacies.
With over 5000 community pharmacies in Australia9, pharmacists are an accessible health professional equipped with extensive pharmacotherapy knowledge to aid in the optimisation of treatment.10 A key finding of a recent Australian Government funded study exploring the role of community pharmacy in supporting mental health consumers was that community pharmacy could play a larger role in this area.11 This study showed that the use of an ongoing, flexible and individualised service improved consumer outcomes, particularly in relation to illness perception, treatment satisfaction and quality of life.11 Furthermore, consumer engagement with the service improved how the consumer viewed their own health, treatment adherence and raised their expectation of what pharmacy could do to support them.11 Empowering a mental health consumer to be involved in their treatment is also critical, and can improve adherence and quality of life.12 Philpott reported that community pharmacists are ideally positioned to provide support and guidance to consumers experiencing mental illness, particularly in relation to issues of treatment adherence and efficacy.13 By accessing the extensive community pharmacy network, which has longer opening hours, no need for an appointment, predominantly free parking and close proximity to people’s homes, consumers can experience increased access to holistic treatment and advice.
Any intervention that improves consumer access to medication has the potential to reduce treatment burden, increase adherence and optimisation of treatment. However, there is a dearth of information on access issues for consumers taking antipsychotics, particularly how clozapine is accessed by people in Australia. Most research focuses on interventions such as motivational interviewing to improve adherence in consumers with schizophrenia, rather than focusing on issues of access.14 At the commencement of this research, clozapine was dispensed in Australian hospital pharmacies unless special arrangements existed. As of July 1st 2015, regulatory changes have allowed clozapine to be dispensed in community pharmacies to stable or maintenance therapy consumers. This will make it possible for clozapine to be more readily accessible in the community setting via community pharmacies. Whilst there is limited information on how many community pharmacies are dispensing clozapine since the regulatory changes, feedback is that uptake has been very low suggesting implementation barriers. Subsequently, knowledge of current processes is both timely and relevant; it is expected that most consumers are still obtaining their clozapine via the traditional hospital pharmacy pathway.
The aim of this research was to: (1) describe the different models of access that exist for consumers taking clozapine in the community, and (2) explore how these models of supply may impact on consumer burden from the perspective of professionals involved in the supply of clozapine. The study sought to compare the clozapine supply arrangements that exist in Australia to those of New Zealand (NZ) and the United Kingdom (UK), as well as explore perceptions about community pharmacy’s role in working with clozapine consumers.
METHODS
This study utilised a mixed methods approach and was conducted in two stages: model development via semi-structured interviews with key informants, and model validation by a survey with a larger participant sample (Figure 1). Participants were coded by method of enquiry, I for interview and S for survey and their country of practice e.g. S29NZ= Survey 29 New Zealand. Ethics approval was obtained from the Griffith University Human Research Ethics Committee (PHM/02/2014/HREC).
Figure 1.
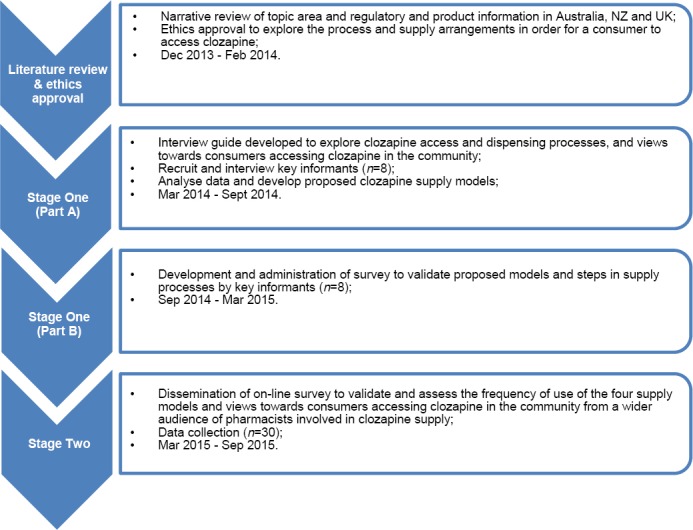
Study Overview
NZ=New Zealand, UK=United Kingdom
Stage One
A review of the literature focusing on current supply practices of clozapine to consumers living in the community yielded limited information. Consequently, a semi-structured interview guide was developed to be exploratory in nature; questions were reviewed and discussed by the research team. A pilot interview was conducted to trial the questions and interview structure. This process highlighted a number of areas for improvement and subsequently the interview guide was adapted to include several questions that were more specific to the processes surrounding clozapine dispensing such as: how recent do blood tests need to be? Participants were purposively sampled to include pharmacists, mental health pharmacists or clozapine coordinators within their respective health service or place of employment, in three study regions (Australia, NZ and the UK). Participants were invited because of their expertise in clozapine use through collegial networks and snowballing. This sampling process yielded a total of eight key informants for Stage One of the study. Semi-structured interviews were conducted with the eight key informants, via phone, in person or by Skype™ and lasted between 30 to 45 minutes.
The interviews were not recorded due to planned participant validation of results; extensive notes were taken and at the conclusion of each interview a summary of key points was documented and findings discussed by the research team. Three participants were re-contacted to clarify points or responses given such as specific training requirements and to confirm the actual order of events in the clozapine supply process. As the interview questions were structured around collecting particular information, data were categorised into the following areas:
Regulatory requirements and dispensing protocols
Current clozapine dispensing by community pharmacists and associated requirements
Advantages and disadvantages to community dispensing
Prescriber role, monitoring, and blood parameters
Extra dose provisions and supply issues
Other information, e.g. consumer numbers, funding issues, district variations
Differences in processes between geographic areas were identified, resulting in four different clozapine supply models. These were generated solely from participant responses and not from regulatory frameworks. Models were described and developed from sequencing events in clozapine supply, from prescriber involvement to consumer clozapine collection. Points of interest included: which professionals were able to prescribe clozapine, what pathology services were utilised, who was responsible for authorising or checking blood results, where clozapine was dispensed and collected by consumers whom lived in the community. The four proposed models were discussed and reviewed by the research team.
The four models were returned to Stage One key informants for validation alongside a supplementary survey. The survey included questions relating to prescribers, collection, review and validity of blood tests, frequency of consumer follow-up, and any additional comments on clozapine access in community pharmacy. These questions were asked to ensure the consistent collection of key information from participants, including those involved in Stage Two. The data from the completed surveys was tabulated and compared to previous results to ensure accurate interpretation of participant responses.
Stage Two
The clozapine supply models required wider verification due to the small Stage One purposive sample size. An expanded version of the survey was developed to verify the models of clozapine supply and to gather the opinion of practitioners involved in this process about how their supply processes impacted on consumers who lived in the community. The survey was delivered online to promote participation. Stage Two participants were pharmacists involved in the dispensing of clozapine in either a community or hospital setting, in Australia, NZ and the UK. Participants were recruited through advertising, cold calling and snowballing. In Australia, advertisements were placed on the Pharmaceutical Society of Australia Early Career Pharmacist Facebook© page and the Society of Hospital Pharmacists e-newsletter. The research team also rang hospital pharmacies in Australia and attempted to speak with the pharmacists responsible for clozapine supply to invite them to participate; snow-balling requests were made during this contact for additional people. In NZ and the UK email advertising was sent to relevant mental health pharmacy special interest groups inviting participation.
Survey data were de-identified and sorted to include all eligible and completed responses. Data analysis involved basic descriptive analysis and, where appropriate, thematic analysis of comments. Thematic analysis was chosen to interpret the comments in order to identify common themes regarding participant opinions of the role of community pharmacy working with clozapine consumers who lived in the community.15
RESULTS
Participants
Stage One key informants (n=8) were experts involved in clozapine supply; three people from Australia, two from NZ and three from the UK. All participants had been in their current role for more than 12 months, with seven being hospital-based pharmacists and one participant was a non-pharmacist clozapine coordinator. There were 50 responses to the Stage Two survey, of which 32 (64%) were complete and useable; a further two responses were excluded as they had participated in Stage One. The majority of Stage Two participants (Table 1) worked in a hospital setting (n=28, 93%), all were pharmacists and had an average of 8.3 years’ experience in their current role (range: 7 months to 28 years). Participants were primarily working in Australia (n=24, 80%) with three each from NZ and the UK.
Table 1.
Stage two participant location and workplace
| Country Region |
Participants | Workplace setting | ||||
|---|---|---|---|---|---|---|
| Hospital | Community | |||||
| n | % | n | % | n | % | |
| Australia New South Wales Northern Territory Queensland South Australia Tasmania Victoria Western Australia |
10 1 3 2 1 4 3 |
33.3 3.3 10 6.7 3.3 13.3 10 |
10 1 3 1 1 4 3 |
33.3 3.3 10 3.3 3.3 13.3 10 |
- - - 1 - - - |
- - - 3.3 - - - |
| United Kingdom England |
3 | 10 | 3 | 10 | - | - |
| New Zealand | 3 | 10 | 2 | 6.6 | 1 | 3.3 |
| Total | 30 | 100 | 28 | 93.4 | 2 | 6.6 |
The models – Stage One
Initial clozapine supply models were developed from commonalities in the data generated from the Stage One semi-structured interviews. The models comprised of a six or seven step process beginning with a prescriber review and ending with clozapine collection by the consumer. To assist readers, the final validated models are provided in Figure 2.
Figure 2.
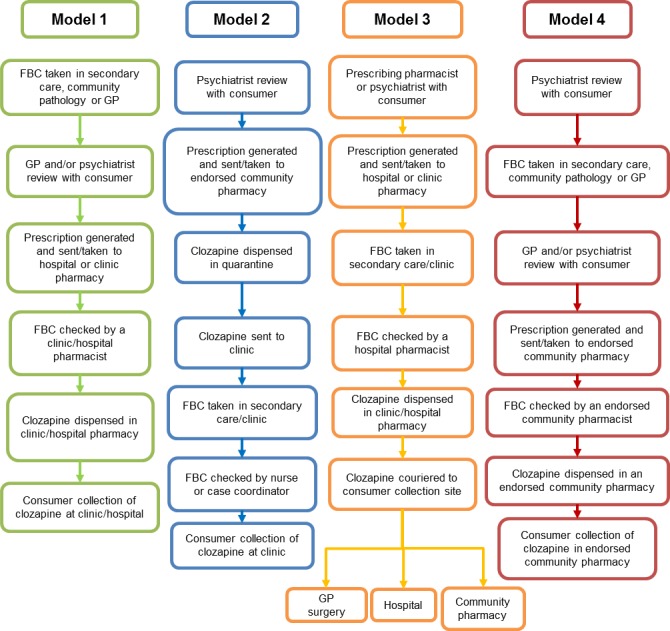
Clozapine supply models
FBC: Full blood count
Three of the four models (Models 1, 3 and 4) involved a similar process in terms of consumer follow-up by a prescriber and prescription generation, the collection and monitoring of blood samples, and finally, the dispensing and collection of clozapine. Differences existed in terms of the prescriber involved, where the blood test was taken, who had the responsibility to check blood tests and where the consumer collected the clozapine.
Model 2 was markedly different as clozapine was dispensed prior to consumer review and blood monitoring, in either a secondary care or community pharmacy setting, and then signed over to a clozapine clinic. The blood results were checked in real time at the point of care and clozapine provided to the consumer if blood tests were in range.
Clozapine prescriptions were predominantly written by psychiatrists. Four participants reported that only psychiatrists were able to prescribe clozapine (Models 2 and 4), with remaining participants describing a combination of prescribers working under the guidance of a psychiatrist. This included shared care arrangements with general practitioners (Model 4) and use of psychiatrist, pharmacist or nurse prescribers in a mental health clinic (Models 1 and 3).
The frequency of consumer review by a prescriber depended on the procedures in each location. Time points for review included monthly, quarterly, semi-annually and annual reviews. In addition, the number of prescription repeats varied from none to a 12-month supply at 28-day intervals. Community pathology services were utilised in all but two areas where consumers who lived in the community had to attend a hospital or clinic for blood tests (Models 2 and 3). Five participants noted that prescribers or general practitioners were required to review blood test results regardless of whether this was also checked by a pharmacist or other medical personnel. Notably, Model 2 differed significantly with a clinic nurse responsible for checking blood tests prior to the consumer accessing their clozapine. According to the two clozapine protocols in Australia (one for each registered brand), everything from blood sample collection to clozapine dispensing must occur within a 48 hour window.16,17 Yet, how long blood tests were valid varied between two to 42 days (Table 2).18 In the UK a maximum of 42 days’ supply of clozapine is possible from the date of the most recent blood test with a monthly FBC that is within range.18 If a new blood test is not conducted within 42 days of the previous test, clozapine supply is prohibited.19 In New Zealand the Community Pharmacy Service Agreement states that dispensing of medication should occur within 24 to 72 hours of a blood test but may vary from location to location.20
Table 2.
Stage one validation survey
| Participant model validation | Model 1 | Model 2 | Model 3 | Model 4 |
|---|---|---|---|---|
| n=1 | n=1 | n=1 | n=5 | |
| Prescriber | ||||
| Psychiatrist only | - | 1 | - | 3 |
| Psychiatrist/GP | - | - | - | 1 |
| Other a | 1 | - | 1 | 1 |
| Pathology service | ||||
| Community | - | - | - | 5 |
| Hospital/clinic | - | 1 | 1 | - |
| Both | 1 | - | - | - |
| Is a doctor required to review FBC regardless of pharmacist check? | ||||
| Yes | 1 | 1 | - | 3 |
| No | - | - | 1 | 2 |
| Prescriber review b | monthly | 6 monthly | 6-12 months | 1-6 months |
| Validity of FBC | 28-42 days | 28 days | 28-42 days | 4-42 days |
| Maximum number of prescription repeats | 1 | 0 | 11 | 2-5 |
nurse or pharmacist prescriber;
of stable (28 day) consumer; FBC: Full blood count; GP: General practitioner.
Model Validation – Stage Two
Model 1 was the most commonly selected clozapine supply model (n=15, 51%). Seven participants confirmed the use of Model 4 (25%), with Models 2 and 3 recognised by only one participant each. Six participants replied that they had different procedures to the four models described. However, their descriptions of processes were aligned with Models 3 or 4. The three participant responses that aligned with Model 3 noted differences in the prescriber, i.e. psychiatrist only or junior doctors. The other three participants replied that their system was similar to Model 4, but that the prescriber could be a GP or the use of a shared care arrangement. This was also consistent across comments made by participants who had selected Model 4. Overall, Model 1 accounted for 50.0% of responses, Model 4 by 33.3%, Model 3 by 13.3% and Model 2 by 3.3%. Geographically, Australian participants reported to predominantly utilise Models 1 and 4, NZ participants exclusively used Model 4 and UK participants reported using Models 1 and 3.
Psychiatrists were reported to be the primary clozapine prescribers. Additionally, over half of the Australian participants (n=14, 58%) and all NZ participants identified that GP’s were able to prescribe clozapine. UK respondents reported that although GP prescribing was theoretically possible, it was not current practice. Results verified that monthly clinical review by prescribers was the most common practice (n=24, 83%). Other time-frames were limited, with one response for quarterly review (NZ) and two responses for six monthly prescriber reviews (one each from NZ and the UK). Monthly reviews by the prescriber were consistent across the model types, however Model 4 or other accounted for all 3, 6 or 12 monthly reviews.
With respect to repeat prescription supply, Models 1 and 4 respondents described two repeat supply options; five monthly repeats (giving a total of six months’ supply per prescription), or two monthly repeats (giving a total of three months’ supply per prescription). A Model 3 respondent from NZ described the possibility of unlimited repeats. Whilst this study did not verify the models against regulatory documentation or prescribing guidelines in different localities, it should be noted that unlimited repeat supply on a community prescription is not funded in NZ as a prescription can supply a maximum of 3 months or 90 days of medication.21 The majority of Australian participants noted that no repeats were provided (n=21, 87%). One NZ participant stated that multiple repeats were ideal, however convincing some prescribers to do this was difficult.
Blood monitoring could be done in a secondary care environment (n=17, 58%) such as a hospital or mental health clinic, community pathology service (n=23, 79%) or by a GP (n=9, 31%). Only secondary care services were used in the UK, NZ did not utilise GP’s for collecting blood samples and Australia used a combination of service providers. Stage Two participants confirmed Stage One results in relation to validity of blood tests and prescriber review. Both UK participants noted that blood tests were valid for 42 days compared to 3-28 days in NZ. In Australia, the validity of blood tests ranged from two days (n=15), within 28 days (n=5), or 3, 5, 7 or 30 days. In the UK a maximum of 42-day supply of clozapine is possible from the date of the most recent blood test with a monthly FBC that is within range.18,19 Blood monitoring was typically undertaken by a doctor or medical officer (n=23, 79%), and that this had to be done regardless of whether a pharmacist or other medical personnel would review the results.
Perceptions of clozapine dispensing in community pharmacy
Utilisation of community pharmacy to dispense clozapine varied among the respondents, however, nearly all Stage Two survey participants (n=18, 62%) acknowledged that enabling consumers living in the community to access clozapine in community pharmacies would be beneficial and normalised care:
Totally agree with community pharmacies dispensing clozapine. They have information about all the other meds [medication] the pt. [patient] is taking for their physical health hence can pick interactions etc… This definitely has benefits for the pt [patient]… (S29NZ)
The positive attitude to the utilisation of the community pharmacy network was related to the alleviation of burden and an improvement in flexibility and convenience for the consumer:
It is a significant burden to the patient to be required to present to the hospital pharmacy. This is in addition to the significant burden clozapine places on the hospital dispensary. (S14AUS)
Having community pharmacies supply clozapine provides increased flexibility for the consumer. It provides an increased level of independence in managing mental illness… (S18AUS)
It was also noted that alongside reducing stigma, the use of community pharmacy had the potential to improve medication access and adherence:
I believe it offers the client better accessibility. I would advocate for making the [clozapine] supply as easy and convenient as possible. Compliance is such an important factor in maintaining this patient group. (S23AUS)
Consumers ought to be able to access clozapine for maintenance therapy in their community, close to where they live, instead of having to deal with returning to the hospital, which may be difficult/ have a negative impact for them, e.g. due to stigma they may experience if they are forced to return to a hospital every month. These patients have treatment-resistant schizophrenia, are often not well-organised & are a vulnerable group of patients, at risk of non-compliance, so the clozapine collection system needs to be as easy as possible for them. They ought to be able to collect their clozapine where they collect all of their other regular medications. (S22AUS)
Participants who reported the value of community pharmacy based clozapine supply did so on the proviso that training or certification should be completed prior to providing this service. Approximately half of participants made statements regarding the need for adequate training (n=14, 48%):
Community pharmacists need to be properly trained re [regarding] dispensing clozapine, what side effects to be aware of, problems with non-compliance etc. They dispense many other potent, problematic medicines, so why not clozapine? (S29NZ)
It should be fine assuming the pharmacists are appropriately trained and are fully cognisant of the importance and ramifications of the monitoring system. (S21AUS)
The need for training was also expressed along with concern for the consumer if adequate safeguards were not in place:
I think if not adequately resourced, with training provided…patients may be placed at risk, particularly when not continuing to use a single nominated pharmacy. (S3AUS)
There were concerns raised that the provision of clozapine in community pharmacy had the potential to cause harm. This related to themes including staff changes, locum use, and insufficient understanding of the condition, the medication and its monitoring requirements. One participant noted that it was not a service that everyone should be involved in due to the contacts with associated support personal, secondary care providers and knowledge required. Furthermore, remuneration was seen as an extra barrier to the provision of clozapine services by community pharmacies as it is labour intensive in both the paperwork involved and consumer interaction.
DISCUSSION
The aim of this study was to describe the different models by which consumers with schizophrenia living in the community access clozapine, how Australia’s arrangements compared to those in NZ and the UK, and how these supply models may impact on a consumer’s life. This study found that there were two main clozapine supply models, and that provided appropriate training and safeguards are in place, there was wide support for community pharmacy to supply clozapine to consumers living in the community. Results indicated that for this consumer group, NZ adopts a clozapine supply model that is decentralised and utilises community services, whereas the UK tends to use a more centralised, secondary care or mental health clinic based approach. Australia seems to sit somewhere in-between the two with the use of both centralised and decentralised approaches.
Utilisation of clozapine supply models varied depending on location. Models 1 and 4 were most widely used and primarily varied with respect to the prescriber, pathology service and where clozapine was collected by the consumer. Model 1 focused on the use of secondary care mental health services such as clinics and hospitals, yet GP’s could be involved as prescribers. This may be due to the utilisation of shared care arrangements in Australia. Alternatively, Model 4 utilised community services such as community pathology service and community pharmacy, and was used by all NZ and South Australian participants. This suggests that consumers who live in the community in these areas are managed predominantly in the primary care setting. South Australia has a range of protocols and resources to support health professionals to work with consumers taking clozapine.22 Conversely, the more restrictive models for supply, Models 1, 2 and 3, were predominantly used in the UK and accounted for approximately one third of Australian responses. Reasons for this are unclear, however, it is worth noting that all but two Stage Two participants worked in a secondary health care environment. This may influence the types of consumers that participants interact with as both participating community pharmacists discussed a Model 4 supply arrangement.
Utilisation of community pharmacy was deemed to be advantageous to the consumer as it promoted normalisation of care and had the potential to reduce treatment burden. These findings were consistent across both research stages. It was also noted that the utilisation of community pharmacy may be advantageous for adherence. Despite this, there was concern that if insufficient training or systems were in place there was a significant potential for an increased risk to consumers, due to the nature of clozapine and its adverse effect profile. Currently, in all three countries, any pharmacist who is eligible to dispense clozapine must be registered with the appropriate clozapine patient monitoring service and linked to a registered pharmacy.16,17 Pharmacist registration to a service, e.g. ClopineCentral® or the Clozaril Patient Monitoring System® (CPMS), recognises that the pharmacist will follow the relevant protocols when dispensing clozapine. Yet, there is limited evidence of wide spread formal training programs associated with dispensing clozapine in the community pharmacy setting. Several study participants stated that secondary care providers did provide training to linked community pharmacies and pharmacists, and that support programs were in place. This study highlighted that participants, while confident in the ability for community pharmacy to supply clozapine, believe that the need for training and formal certification was important and necessary to ensure the quality and safe use of clozapine.
A study by O’Reilly et al. found that pharmacists who had low levels of stigma and high literacy levels regarding schizophrenia were much more likely to provide medication counselling to consumers with schizophrenia.23 Studies such as this, combined with our findings, give credence to the need for understanding not only clozapine as a medication, but schizophrenia as a long term condition and the social issues surrounding serious mental illness. Outcomes for our research centre on the perception that the use of community pharmacy to supply clozapine would be advantageous provided adequate and appropriate support and training are in place. It is recommended that a training or certification package for community pharmacy staff be designed, that incorporates information beyond that of clozapine monitoring requirements alone. Further research is needed to assess the roll-out of clozapine supply for community-based consumers into a community setting to ensure proper safeguards are monitored.
Strengths and limitations
This exploratory study sought to describe current clozapine supply practices to community-based consumers by collecting responses from key pharmacists or clozapine coordinators. As such, participants were purposively sampled and represent key health professionals with expertise in this area. Study participants were predominantly hospital pharmacists and it is unclear at this stage how many community pharmacists currently dispense clozapine and their views on supply in a community setting. This should be considered for future research. It should also be noted that the Models generated were based on the responses of participants and not from regulatory frameworks. It is therefore possible that whilst respondents were invited to participate in the study as experts in this area, there may be discrepancies in the findings presented. It is also possible that despite piloting the data collection tools, that the survey questions were misinterpreted. This is exemplified by issues identified during the analysis process such as the ‘unlimited repeat supply’ identified by one respondent and with the use of the term ‘Full Blood Count (FBC) validity’. This question was intended to reflect how long blood tests were valid, in order to dispense a new supply of clozapine.
The results ranged from 2-42 days and this wide range is likely due to misinterpretation of the question and different wording used in the product information and protocols in Australia, NZ and the UK.16,17,20,24
The number of participants in Stage One was limited to eight as purposive sampling networks had been exhausted. Despite this limitation, Stage Two validated the models generated in Stage One and no further models of supply became apparent. The study included only a small number of responses from the UK and NZ to serve as a comparison for Australian practices. The overall low response rate makes it difficult to say that these findings are generalisable to the total practices in these locations, however the two-stage validation process strengthens the findings. Furthermore, this study is generalisable only to the perceptions of pharmacists closely involved in clozapine supply (most typically this was hospital pharmacists or pharmacists specialising in mental health) and clozapine coordinators as the perceptions of other health professionals (e.g. psychiatrists and/or GPs) were not explored.
CONCLUSIONS
Australia utilises multiple clozapine supply arrangements for consumers living in the community. These feature both secondary care and primary care arrangements, with commonalities with both UK and NZ practice. This study identified that pharmacists support the utilisation of community pharmacy to dispense and supply clozapine. Furthermore, it is proposed that the utilisation of community pharmacy would reduce consumer treatment burden by improving medication access. However, it was the strong recommendation of the study participants in this study that training or certification programs be developed to support the safe and quality use of clozapine in community pharmacy.
ACKNOWLEDGEMENTS
We thank all participants for their time and involvement in this study.
Footnotes
CONFLICT OF INTEREST
The authors declare that there are no conflicts of interest to declare.
Funding: This was an Honours student project supported by Griffith University.
Contributor Information
Sally-Anne Knowles, Griffith University. Nathan, QLD (Australia). sally.knowles@griffithuni.edu.au.
Sara S. Mcmillan, School of Pharmacy, Menzies Health Institute Queensland, Griffith University. Nathan, QLD (Australia). s.mcmillan@griffith.edu.au
Amanda J. Wheeler, Professor of Mental Health, Menzies Health Institute Queensland, Griffith University. Nathan, QLD (Australia). a.wheeler@griffith.edu.au
References
- 1.American Psychiatric Association. [accessed January 21 2016];Diagnostic and Statistical Manual of Mental Disorders Washington D.C.2013] 5th. Available at: http://dx.doi.org/10.1176/appi.books.9780890425596.dsm02 .
- 2.Therapeutic Guidlines Ltd. Schizophrenia and related psychoses eTG complete [internet] ed. Melbourne. 2015 [Google Scholar]
- 3.Bleakley S, Taylor D. Clozapine Handbook. Warwickshire United Kingdom: Llyod-Reinhold; 2013. [Google Scholar]
- 4.Malalagama G, Bastiampillai T, Dhillon R. Clozapine use in Australia. Australas Psychiatry. 2011;19(2):175. doi: 10.3109/10398562.2010.525646. doi: 10.3109/10398562.2010.525646. [DOI] [PubMed] [Google Scholar]
- 5.Fakra E, Azorin JM. Clozapine for the treatment of schizophrenia. Expert Opin Pharmacother. 2012;13(13):1923–1935. doi: 10.1517/14656566.2012.709235. doi: 10.1517/14656566.2012.709235. [DOI] [PubMed] [Google Scholar]
- 6.Asenjo Lobos C, Komossa K, Rummel-Kluge C, Hunger H, Schmid F, Schwarz S, Leucht S. Clozapine versus other atypical antipsychotics for schizophrenia. Cochrane Database Syst Rev. 2010;(11):722. doi: 10.1002/14651858.CD006633.pub2. doi: 10.1002/14651858.CD006633.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sav A, King MA, Whitty JA, Kendall E, McMillan SS, Kelly F, Hunter B, Wheeler AJ. Burden of treatment for chronic illness: a concept analysis and review of the literature. Health Expect. 2015 Jun;18(3):312–324. doi: 10.1111/hex.12046. doi: 10.1111/hex.12046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barnett AH, Chaudhry I, Farooqi A, Gadsby R, Heald A, Hill J, Jones PB, Mackin P, Millar H, Peveler R, Rees A, Singh V, Taylor D, Vora J. Minimising metabolic and cardiovascular risk in schizophrenia: diabetes, obesity and dyslipidaemia. J Psychopharmacol. 2007;21(4):357–373. doi: 10.1177/0269881107075509. [DOI] [PubMed] [Google Scholar]
- 9.Pharmacies in Australia: Market Research Report: IBISWorld; [accessed January 21 2016];2015 Available at: http://www.ibisworld.com.au/industry/default.aspx?indid=1878 .
- 10.Crump K, Boo G, Liew FS, Olivier T, So C, Sung JY, Wong CH, Shaw J, Wheeler AJ. New Zealand community pharmacists’ views of their roles in meeting medicine-related needs for people with mental illness. Res Social Adm Pharm. 2011;7(2):122–133. doi: 10.1016/j.sapharm.2010.03.006. doi: 10.1016/j.sapharm.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 11.Wheeler A, Fowler J, Hattingh L, Kelly F. [accessed January 21 2016];Exploring the role of community pharmacy in supporting mental health consumers and carers. [Research Report] Available from: http://6cpa.com.au/resources/fifth-agreement-rd/mental-health-project/
- 12.Thompson L, McCabe R. The effect of clinician-patient alliance and communication on treatment adherence in mental health care: a systematic review. BMC Psychiatry. 2012;12:722. doi: 10.1186/1471-244X-12-87. doi: 10.1186/1471-244X-12-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Philpott L. Mental health: Make a difference. Aust J Pharm. 2014;95(1133):36–40. [Google Scholar]
- 14.Zygmunt A, Olfson M, Boyer CA, Mechanic D. Interventions to improve medication adherence in schizophrenia. Am J Psychiatry. 2002;159(10):1653–1664. doi: 10.1176/appi.ajp.159.10.1653. [DOI] [PubMed] [Google Scholar]
- 15.Liamputtong P. Australia: Oxford University Press; 2013. Qualitative Research Methods. ISBN: 9780195518559. [Google Scholar]
- 16.Clozaril Patient Monitoring System Protocol. Novartis Pharmaceuticals. 2015 Available from Novartis Pharmaceuticals Australia. [Google Scholar]
- 17.Clopine Connect. Hospira. 2015 Available from Hospira. [Google Scholar]
- 18.Dixon M, Dada C. How clozapine patients can be monitored safely and effectively. Pharm J. 2014;6(5):131. [Google Scholar]
- 19.Monitoring Frequency and Overdue Notifications. Novartis Pharmaceutics. Available from Novartis Pharmaceuticals UK: 2014. [Cited d2016]. [Google Scholar]
- 20.Community Pharmacy Services Agreement. [accessed January 21 2016];TAS. 2012 Available at: http://centraltas.co.nz/assets/Publications/Pharmacy-Documents/Implementing-the-CPSA/Community+Pharmacy+Services+Agreement+generic+version.pdf .
- 21.Medicines Regulation of 1984 NZ. [accessed June 22 2016]; Available at: http://www.legislation.govt.nz/regulation/public/1984/0143/latest/DLM95668.html .
- 22.Treating patients on Clozapine [webpage] [accessed June 22 2016];South Australia Health. Available at: http://www.sahealth.sa.gov.au/wps/wcm/connect/public+content/sa+health+internet/clinical+resources/clinical+topics/medicines+and+drugs/clozapine/treating+patients+on+clozapine .
- 23.O’Reilly CL, Bell JS, Kelly PJ, Chen TF. Exploring the relationship between mental health stigma, knowledge and provision of pharmacy services for consumers with schizophrenia. Res Social Adm Pharm. 2015;11(3):e101–e109. doi: 10.1016/j.sapharm.2013.04.006. doi: 10.1016/j.sapharm.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 24.Clozaril Product Information AUSDI: Phoneix Medical Publishing Pty Limited [Google Scholar]


