Abstract
Aims/Introduction
Lifestyle management helps improve the clinical outcome of patients with type 2 diabetes. The present study aimed to obtain lifestyle data on the dietary and physical activity of adult type 2 diabetes patients in Zhejiang province of eastern China for better patient education and improvement of clinical management.
Materials and Methods
A cross‐sectional survey of 607 adult type 2 diabetes patients was carried out in 12 hospitals within eight cities of Zhejiang province. Data were collected for sex, age, basic physical measurement (blood pressure, height, weight, waist circumference and hip circumference), dietary favor and habit (vegetarian diets vs meat diets, preference of salty or light flavors), detailed dietary intake (24‐h recall method), as well as the weekly physical activity.
Results
The mean age of the patients in the analysis was 56.39 ± 12.29 years, and 38.71% of the patients had higher levels of body mass index than recommended. The average daily total energy intake was 1887.71 ± 575.10 kcal. The percentage of calories from carbohydrate, protein and fat were 61.36 ± 11.59%, 13.29 ± 3.37% and 25.35 ± 11.16%, respectively. For physical activity, the patients generally spent most of their daily time sitting and sleeping, and the time for moderate vigorous activity was limited.
Conclusions
Adult patients with type 2 diabetes in Zhejiang province have a relatively high carbohydrate and low protein diet, with very limited physical activity. Patient education to achieve a better lifestyle intervention needs to improve in this region.
Keywords: Dietary, Lifestyle, Type 2 diabetes
Introduction
With a dramatically increased incidence and prevalence, diabetes has become a major public health problem in China1. According to the latest epidemiological study, 11.6% of Chinese adults had diabetes, which accounts for approximately one‐quarter of diabetes patients worldwide, and the percentage for prediabetes was 50.1%2. This is a tremendous change when compared with the data from 20 years ago, when the prevalence of diabetes and impaired glucose tolerance in China were just 2.5% and 3.2%, respectively1, 3. As one of the major risk factors of disabling and life‐threatening complications from microvascular and macrovascular diseases and even cancer4, 5, 6, 7, this chronic disease is now more of a public health challenge than a health issue for individuals.
Increasing studies show that lifestyle changes after diagnosis can contribute to better clinical outcome in patients with type 2 diabetes. In a randomized controlled trial in Southwest England, changes in diet or diet plus physical activity improved the glycemic control, bodyweight and insulin resistance in newly diagnosed adult type 2 diabetes patients8. In Asia, a study of 2,484 patients with diabetes in Korea showed that diet modification helped to improve the blood lipid profile9. There are also meta‐analyses that conclude that aerobic and resistance exercise, as well as dietary intervention, are able to lower glycated hemoglobin A1c (HbA1c) levels10, 11, 12, 13, 14.
As the rapid increase in the prevalence of diabetes in China is thought to be associated with a shift in lifestyle, endocrinologists and diabetes centers in China are increasing their efforts to educate patients in nutrition therapy and promote exercise. These topics are an important component in general diabetes education. Zhejiang province is among the most economically developed regions in eastern China, where diabetes occurs at a relatively high incidence. Although there are some small or monocentric studies that provided some indications about the patients’ lifestyle in certain cities of this province, a comprehensive and multicenter study has been lacking. In the present cross‐sectional study, we collected detailed information about the dietary patterns and the duration of physical activity of 607 adult patients with type 2 diabetes from 12 medical centers within eight cities covering the entire province in order to provide comprehensive data of the patients’ dietary patterns and physical activity as background for reference in promoting better diabetes education and clinical management.
Materials and Methods
Questionnaire
The questionnaire comprised of three parts: (i) clinical characteristics; (ii) eating patterns and macronutrient distribution; and (iii) physical activity. In the first part, information regarding sex, age and basic physical measurement data (height, weight, waist circumference and hip circumference) of the participants were collected. Body mass index (BMI) was calculated as bodyweight in kilograms divided by squared body height in meters. Waist‐to‐hip ratio (WHR) was calculated as waist circumference divided by hip circumference. According to the World Health Organization standards, the measurement for waist circumference was made at the approximate midpoint between the lower margin of the last palpable rib and the top of the iliac crest, whereas the hip circumference measurement was taken around the widest portion of the buttocks. To describe the eating patterns and macronutrient distribution of the participants, dietary favor and habit (vegetarian or meat diets, preference for salty or light flavors), and detailed dietary intake (24‐h recall method) were recorded. The food diary was broken into six meal sections, which were: (i) breakfast; (ii) morning snack; (iii) lunch; (iv) afternoon snack; (v) dinner; and (vi) evening snack. Instructions including food atlas photographs to aid portion size estimation were located at the end of the food diary. The type and quantity of food or drink consumption were listed. In the last part, the duration of physical activity during the past week was recorded. The measurement of physical activity behavior was designed based on the international physical activity questionnaires short form. The activities were classified into the following categories: vigorous activity, moderate activity, walking, sitting and sleeping. Vigorous activities referred to activities that took hard physical effort leading the participants to breathe much harder than normal, these included heavy lifting, digging, aerobics or fast bicycling. Moderate activities referred to activities that took moderate physical effort and made the participants breathe somewhat harder than normal, such as carrying light loads, bicycling at a regular pace or playing doubles tennis. Walking was not included in moderate activity. The walking time recorded included walking at work and at home, walking for travel from place to place, and any other walking that the participants might do solely for recreation, sport, exercise or leisure. Sitting included time spent at work, at home, while doing course work and during leisure time. Sleeping time included the time when the participants were lying down. The survey was delivered by professional nurses for diabetes care who were trained for this survey in advance according to well‐established protocols.
Patients
The survey was carried out from August 2012 to August 2013. A total of 12 hospitals from eight different cities across the Zhejiang province participated. Participants who agreed to take part in this survey were randomly selected from the outpatient populations of these centers. The inclusion criteria were: (i) age of 18 years and older; (ii) not pregnant or breast‐feeding an infant; (iii) diagnosed as type 2 diabetes; (iv) being a local resident for at least six consecutive months before participation in the study; and (v) without mental disorder. The diagnostic criteria were: (i) fasting plasma glucose ≥7.0 mmol/L – fasting was defined as no caloric intake for at least 8 h; (ii) 2‐h plasma glucose ≥11.1 mmol/L during an oral glucose tolerance test carried out as described by the World Health Organization using a glucose load containing the equivalent of 75 g anhydrous glucose dissolved in water; or (iii) the patient presented with classic symptoms of hyperglycemia or hyperglycemic crisis, with a random plasma glucose ≥11.1 mmol/L. At the end, a total of 607 patients were recruited who completed the entire questionnaire. The patients were then divided into different groups according to age (young 18–39 years, middle aged 40–59 years, old ≥60 years), sex (male, female) or region (north: Hangzhou and Shaoxing; east: Ningbo, Wenzhou, Taizhou; midwest: Jinhua, Lishui and Quzhou) for statistical analysis. The study complied with the recommendations of the Declaration of Helsinki, and was approved by the Ethical Committee of the 2nd Affiliated Hospital, School of Medicine, Zhejiang University.
Statistical analysis
Dietary intake was analyzed using nourishment software (metabolic syndrome lifestyle intervention software v2.0; Zhejiang University, Zhejiang, China), which calculated total calories, and the amount of carbohydrates, fat and protein consumed. For each group, the mean age and the mean value of BMI, waist circumference and WHR were calculated. The percentages of patients who achieved the blood pressure control goal (under 140/90 mmHg, as recommended in the standard of medical care for diabetes provided by the American Diabetes Association [ADA] in 201515) and who had ever tried to control their diet were also evaluated. In the dietary intake analysis, the average level of total energy intake, and the percentage of calories from carbohydrate, protein and fat were calculated for each group. For the description of physical activity patterns, the average time of the activities the patients spent during 1 week was calculated. SPSS 16.0 (SPSS, Chicago, IL, USA) was used in all the data analysis. Non‐parametric test or one‐way anova was used for group comparisons. A P‐value <0.05 for two‐sided tests was considered as statistically significant.
Results
Sex, age and regional distribution of the participants enrolled
A total of 607 patients were included in the study, with 345 men (56.84%) and 262 women (43.16%). The mean age of the patients in the analysis was 56.39 ± 12.29 years. The majority of patients were in the age groups of 40–59 years and ≥60 years with percentages of 49.26% (299) and 42.34% (257), respectively. The number of the young patients (age 18–39 years) was 51, which accounted for 8.4% of the total cohort. Among the 12 hospitals that participated, six were from the northern part of Zhejiang province (city of Hangzhou and Shaoxing), which brought in 55.85% (339) of the participants, three were from the eastern regions (city of Ningbo, Wenzhou, Taizhou), which contributed 25.70% (156) of the participants, and the other three participating centers were from the midwest (city of Jinhua, Lishui, Quzhou), with 18.45% (112) of the participants. No significant difference of age was observed among these regions (Table 1).
Table 1.
Clinical characteristics of the patients
| n | Age (years) | BMI (kg/m2) | Waist (cm) | WHR | BP target achievement | Diet control rate | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | P | Mean ± SD | P | Mean ± SD | P | Mean ± SD | P | Mean ± SD | P | Mean ± SD | P | ||
| Total | 607 | 56.39 ± 12.29 | 23.73 ± 3.68 | 85.56 ± 10.37 | 0.91 ± 0.07 | 79.08% | 68.70% | ||||||
| Sex | 0.088 | <0.001 | <0.001 | <0.001 | 0.571 | 0.005 | |||||||
| Male | 345 | 55.73 ± 12.73 | 24.32 ± 3.53 | 88.08 ± 9.91 | 0.93 ± 0.07 | 78.26% | 64.06% | ||||||
| Female | 262 | 57.27 ± 11.64 | 22.94 ± 3.73 | 82.24 ± 10.03 | 0.90 ± 0.08 | 80.15% | 74.81% | ||||||
| Age | / | 0.865 | 0.182 | 0.089 | <0.001 | 0.023 | |||||||
| 18–39 | 51 | 32.47 ± 5.63 | 23.60 ± 4.25 | 84.42 ± 11.50 | 0.90 ± 0.08 | 88.24% | 18–39 vs 40–59: <0.001 | 62.75% | 18–39 vs 40–59: 0.03 | ||||
| 40–59 | 299 | 50.84 ± 5.47 | 23.76 ± 3.48 | 85.08 ± 10.02 | 0.91 ± 0.07 | 84.28% | 40–59 vs ≥60: 0.018 | 64.55% | 40–59 vs ≥60: >0.05 | ||||
| ≥60 | 257 | 67.60 ± 6.36 | 23.71 ± 3.80 | 86.33 ± 10.52 | 0.92 ± 0.08 | 71.21% | 18–39 vs ≥60: <0.001 | 74.71% | 18–39 vs ≥60: 0.03 | ||||
| Region | 0.552 | 0.163 | 0.053 | <0.001 | <0.001 | 0.069 | |||||||
| North | 339 | 56.74 ± 12.43 | 23.59 ± 3.83 | 84.87 ± 10.46 | 0.91 ± 0.07 | North vs east: >0.05 | 83.78% | North vs east: 0.001 | 72.57% | ||||
| East | 156 | 56.42 ± 11.92 | 24.16 ± 3.54 | 85.79 ± 10.33 | 0.90 ± 0.07 | East vs midwest: <0.001 | 80.77% | East vs midwest: <0.001 | 64.10% | ||||
| Midwest | 112 | 55.29 ± 12.40 | 23.54 ± 3.34 | 87.30 ± 10.01 | 0.94 ± 0.08 | North vs midwest: <0.001 | 62.50% | North vs midwest: 0.001 | 63.39% | ||||
Data presented as mean ± standard deviation (SD) or as percentage. Basic characteristics, such as body mass index (BMI), waist circumference and waist‐to‐hip ratio (WHR) are shown. The percentage of patients whose blood pressure (BP) was under 140/90 mmHg was recorded as ‘BP target achievement’ for each group. The percentage of patients who had ever tried to control their daily diets was recorded as ‘diet control rate’ for each group.
BMI, waist circumference, WHR and BP control goals
The mean BMI level of the male patients was 24.32 ± 3.53 kg/m2, and 22.94 ± 3.73 kg/m2 for female patients. A total of 39.42% of the male patients did not reach the control goal of <25 kg/m2, and a similar rate was observed in the female patients (38%). No significant differences were observed for the BMI levels across the three regions, even though patients from the midwest showed the highest WHR level (north 0.91 ± 0.07, east 0.90 ± 0.07, midwest 0.94 ± 0.08, P < 0.001). According to the standards of medical care for diabetes provided by the ADA in 2015, the blood pressure of patients with diabetes should be controlled under 140/90 mmHg15. In the present study, the percentage of patients who achieved the blood pressure control goal were 78.26% and 80.15% for men and women, respectively, without significant difference. However, this rate of blood pressure goal achievement decreased along with age, from 88.24% in young patients to 71.21% in old patients (P < 0.001). In the midwest, the control rate was the lowest compared with the northern and eastern regions (midwest 62.50%, eastern 80.77%, northern 83.78%, P < 0.001; Table 1).
Dietary favor and habit
Information about the dietary favor and habit of the participants was collected. We found that vegetarian diets were more common in the older group. Approximately 43.19% of the patients aged over 60 years preferred vegetarian diets, and this proportion was approximately twofold when compared with young patients. The highest proportion with meat diets was observed in the middle‐aged group (Figure 1a). From the region distribution point of view, more patients from the eastern part of the province, where seafood is quite common, were found to prefer meat diets. In the midwest, people with vegetarian diets occupied the largest proportion (Figure 1a). For salty or light (not salty) flavors, the situation was quite similar when comparing middle‐ and old‐aged patients, whereas more young patients preferred salty foods (Figure 1b). With regard to the different regions, 40.13% of the patients in the eastern region preferred light tastes, which was the highest among the three regions (Figure 1b).
Figure 1.
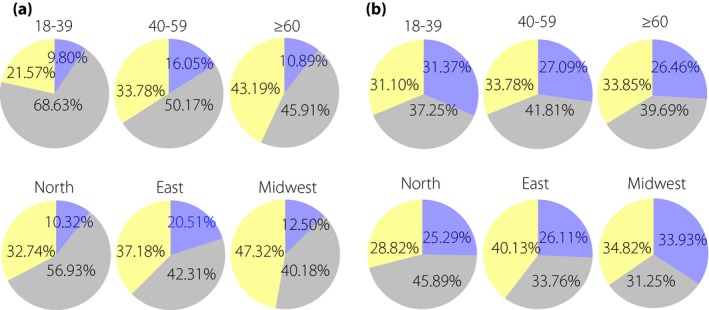
Dietary preferences of the patients. Data are shown in the percentage of the total population for each group. (a) Dietary preference for meat or vegetarian diets of the patients. Blue, patients who have meat diets; yellow, patients who have vegetarian diets; gray, patients who have moderate diets. (b) The preference for salty or light flavors of the patients. Blue, patients who prefer salty flavors; yellow, patients who prefer light flavors; gray, patients who prefer moderate flavors.
Eating patterns and macronutrient distribution
We further investigated to what degree patients paid attention to diet control. The data showed that 74.81% of the female participants had made some effort to control their diets. This proportion was approximately 10% lower in the male participants (P = 0.005). Furthermore, older patients took this issue more seriously than the younger patients. The proportion went up from 62.75% in the 18–39 years age group to 74.71% in ≥60 years age group (P = 0.023). Although not statistically significant, it is still worth noting that the percentage in the northern part of the province was the highest, as 72.57% of the patients claimed that they had tried to make their eating pattern healthier, and this proportion was approximately 8–9% higher than the other two regions (Table 1).
To investigate the patients’ dietary intake in more detail, we used the 24‐h recall method to record the type and amount of food. The average total energy our participants consumed everyday was 1887.71 ± 575.10 kcal. The percentage of calories from carbohydrate, protein, and fat were 61.36 ± 11.59%, 13.29 ± 3.37% and 25.35 ± 11.16%, respectively (Table 2). The male patients consumed more calories than the female patients, and this significant difference could be found in both the total energy and the energy from the three nutrient contents (P < 0.001). However, the constituent ratios of the three macronutrients were quite similar between the two groups, with only a slightly greater protein composition in male patients (P = 0.003). In the analysis of the different age groups, we noticed that the young patients aged <40 years consumed more carbohydrate than patients aged >60 years (P = 0.026), although there was no significant difference of the macronutrient distribution among the three groups. From a region point of view, no statistical difference was observed for the amount of energy consumed (both total energy and the energy from carbohydrate, protein, and fat) across the three regions. For the proportion of the energy provided by the three macronutrients, we found that patients from the northern areas consumed more fat (P = 0.044), but less protein (P < 0.001) than the patients from the midwest (Table 2).
Table 2.
Eating patterns and macronutrient distribution of the patients
| n | Total energy (kcal) | Carbohydrate (kcal) | Protein (kcal) | Fat (kcal) | Percentage of total energy | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Carbohydrate | Protein | Fat | |||||||||||||
| Mean ± SD | P | Mean ± SD | P | Mean ± SD | P | Mean ± SD | P | Mean ± SD | P | Mean ± SD | P | Mean ± SD | P | ||
| Total | 607 | 1887.71 ± 575.10 | 1144.59 ± 381.36 | 249.07 ± 98.70 | 494.05 ± 285.79 | 61.36 ± 11.59% | 13.29 ± 3.37% | 25.35 ± 11.16% | |||||||
| Sex | <0.001 | <0.001 | <0.001 | 0.001 | 0.964 | 0.003 | 0.644 | ||||||||
| Male | 345 | 2027.28 ± 598.93 | 1223.80 ± 392.47 | 274.23 ± 107.31 | 529.25 ± 296.69 | 61.09 ± 11.41% | 13.62 ± 3.47% | 25.29 ± 10.83% | |||||||
| Female | 262 | 1703.93 ± 485.26 | 1040.27 ± 339.76 | 215.95 ± 74.18 | 447.70 ± 264.24 | 61.71 ± 11.83% | 12.85 ± 3.20% | 25.44 ± 11.60% | |||||||
| Age | 0.039 | 0.040 | 0.097 | 0.205 | 0.784 | 0.303 | 0.502 | ||||||||
| 18–39 | 51 | 2060.18 ± 772.69 | 18–39 vs 40–59: >0.05 | 1256.00 ± 521.06 | 18–39 vs 40–59: >0.05 | 284.47 ± 133.55 | 519.71 ± 305.30 | 61.61 ± 10.28% | 13.73 ± 3.36% | 24.66 ± 9.70% | |||||
| 40–59 | 299 | 1923.47 ± 567.48 | 40–59 vs ≥60: >0.05 | 1161.30 ± 375.12 | 40–59 vs ≥60: >0.05 | 251.73 ± 102.34 | 510.44 ± 288.87 | 61.02 ± 11.98% | 13.18 ± 3.59% | 25.80 ± 11.31% | |||||
| ≥60 | 257 | 1811.88 ± 527.50 | 18–39 vs ≥60: 0.014 | 1103.04 ± 350.59 | 18–39 vs ≥60: 0.026 | 238.96 ± 83.81 | 469.89 ± 277.42 | 61.70 ± 11.40% | 13.34 ± 3.12% | 24.96 ± 11.26% | |||||
| Region | 0.064 | 0.370 | 0.579 | 0.077 | 0.368 | <0.001 | 0.049 | ||||||||
| North | 339 | 1916.52 ± 523.01 | 1156.31 ± 354.64 | 246.04 ± 95.86 | 514.17 ± 283.84 | 61.03 ± 11.39% | 12.87 ± 3.28% | North vs east: >0.05 | 26.10 ± 11.21% | North vs east: >0.05 | |||||
| East | 156 | 1844.57 ± 529.85 | 1113.92 ± 331.37 | 245.05 ± 82.40 | 485.60 ± 277.25 | 61.16 ± 11.49% | 13.52 ± 3.58% | East vs midwest: >0.05 | 25.32 ± 10.71% | East vs midwest: >0.05 | |||||
| Midwest | 112 | 1860.62 ± 758.17 | 1151.82 ± 505.85 | 263.86 ± 124.3 | 444.94 ± 299.10 | 62.62 ± 12.32% | 14.25 ± 3.16% | North vs midwest: <0.001 | 23.13 ± 11.42% | North vs midwest: 0.044 | |||||
Data are presented as mean ± standard deviation (SD). The detailed dietary intake for 1 day was recorded using the 24‐h recall method. The amount of the carbohydrate, protein and fat containing in the food was calculated and shown in the table in the form of calories. Total energy was calculated as a sum of the calories from the three macronutrients. The macronutrient distribution was shown as the percentage of the total energy.
Physical activity
In order to assess the physical activity of the patients, we classified routine activity into five different types: (i) vigorous physical activity; (ii) moderate physical activity; (iii) walking; (iv) sitting; and (v) sleeping. The time spent on each of these activities for the week before the survey was carefully recorded for each patient. We found that almost all the patients spent the majority of their daily time sitting and sleeping. Vigorous or moderate physical activity only took a negligible proportion. Just 30.64% of the patients spent more than 150 min/week on moderate to vigorous physical activity, and 60.46% of the patients did not take any activity of this intensity during the whole week. Even in the young group, the percentage of the patients who were absent for moderate vigorous activities was as high as 50.98%. In the analysis of different groups, we observed that the male patients spent more time in vigorous activity, as well as in sitting, than the female patients (Figure 2a; P < 0.001). Patients of different age groups and region groups did not show any difference in the daily schedule (Figure 2b,c).
Figure 2.
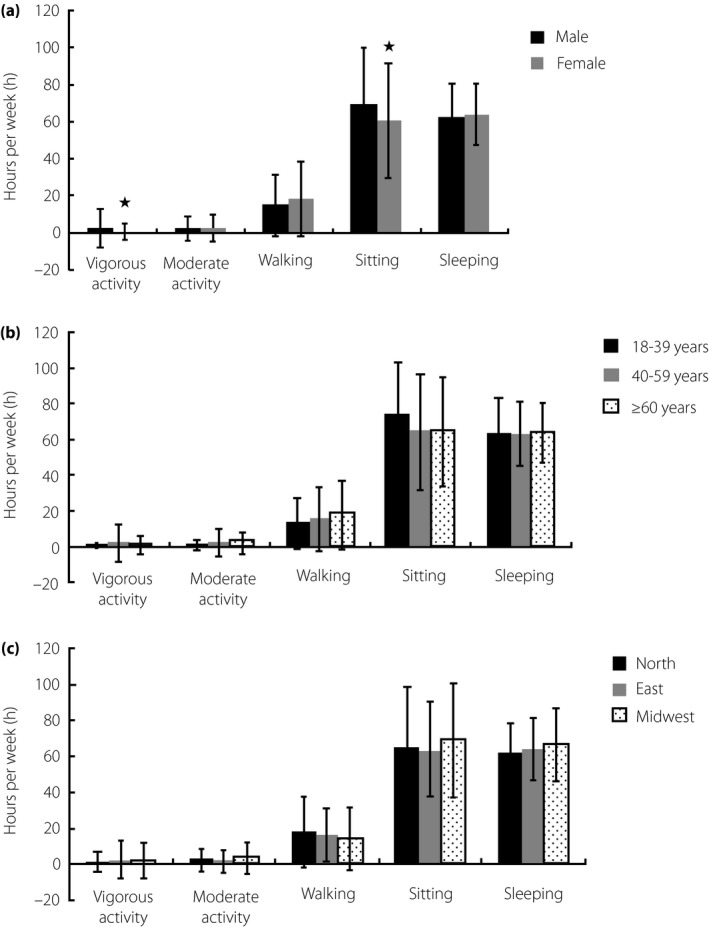
The physical activity of the patients. The time spent carrying out activities for 1 week was evaluated. Patients were classified into different groups according to sex, age or region. The sitting and sleeping mode are shown here as the dominant routine style. (a). Analysis between male and female patients. The male patients spent more time carrying out vigorous activity as well as sitting than the female patients. Analysis among (b) different age groups and (c) different region groups did not show any significant difference. *P < 0.05.
Discussion
As recommended by the ADA, nutrition therapy and physical activity are two key components for the management of diabetes16. Early in 1999, the Institute of Medicine reported that effective nutrition therapy helped to improve the clinical outcome of patients while decreasing the total cost of medical management16, 17. Several nutrition intervention studies have shown that appropriate lifestyle counseling contributes to good glycemic control8, 18, 19, 20. However, even in the USA, the percentage of diabetes patients who receive diabetes education is only approximately 50%, and even fewer patients see a registered dietitian21. With an increasing incidence and prevalence, diabetes is now gaining more and more attention in China, and the endocrinologists in China are putting more effort into promoting nutrition therapy and exercise, and now strongly support their implementation. This provided the rationale for a cross‐sectional study in order to obtain more specific information for a better understanding of the dietary and energy‐spending pattern of adult type 2 diabetes in this province.
The survey covered eight cities distributed across the whole province, which provides more comprehensive information than previous studies reporting the situation in this province. We recruited 607 adult type 2 diabetes patients with an average age of 56.39 ± 12.29 years. More than two‐thirds of the patients achieved the blood pressure control goal, which is under 140/90 mmHg, and approximately 68.70% of the patients had ever tried to control their diet. Although the glycemic levels and information about other metabolic targets were not included, we see room for improvement of general diabetes education, as only approximately one‐third of the patients were aware of nutrition therapy or did not take it seriously. This is similar to the results reported by Zhong et al.22, who carried out a cross‐sectional study of 365 participants with type 2 diabetes for their awareness and practice of self‐management in Anhui province, China. Their data showed that fewer than half of the participants had a basic knowledge of the disease and practiced adequate self‐management22. In the dietary analysis, we found that the average total energy our participants consumed everyday was 1887.71 ± 575.10 kcal, and the percentage of calories from carbohydrate, protein, and fat were 61.36 ± 11.59%, 13.29 ± 3.37% and 25.35 ± 11.16%, respectively, and there was no obvious group difference for the macronutrient distribution. This could be considered as a diet containing relatively high carbohydrate and low protein. Currently, there is no ideal macronutrient distribution for all people with diabetes, according to the ADA recommendations for nutrition therapy16. For example, some studies showed better glycemic control and insulin sensitivity in patients taking lower levels of carbohydrate23, 24, 25, whereas some others showed no difference26, 27. Conflicting results were also reported by various studies regarding the clinical outcomes in patients having higher or usual protein intake28, 29, 30, 31. Eating plans and nutrition therapy goals should be set collaboratively with individual needs including the patients’ metabolic targets, personal and cultural preferences, literacy and economic capability, as well as their ability and willingness to change16. Further studies are required to check if diets containing lower carbohydrate or higher protein can contribute to better glycemic control and reduction of diabetes‐related complications, and to define a suitable dietary pattern for patients in this region.
Meanwhile, we also compared the situation between different age groups. According to a national study among Chinese adults, the prevalence of diabetes increased with age (3.2%, 11.5%, and 20.4% among persons who were aged 20–39, 40–59 and ≥60 years)1. In our randomly recruited participants, we found that the percentage of the patients who were aged 18–39, 40–59, and ≥60 years were 8.4%, 49.26% and 42.34%, respectively. Although the middle‐ and old‐aged patients still represented the majority of participants in the study, young‐onset diabetes should be given special attention. In the survey, we showed that the percentage of patients who had ever tried to make a diet control was the lowest in this age group. Although no significant difference was observed for the nutrition intake distribution of carbohydrate, protein and fat among different age groups, the average amount of the three macronutrients as well as total energy consumed by the young patients was the largest. Approximately 31.37% of the young patients prefer salty flavors, which is also the highest compared with 27.09% in middle‐age patients and 26.46% in old‐age patients. Although not statistically significant, the average time the young patients spent on moderate to vigorous activity and walking per week was the shortest. They also spent longer time on average sitting. So the young patients showed a lifestyle of a relatively high‐energy intake and less physical activity in this province. In a study of metabolic control or the burden of associated complications in adult diabetes in Asia (the Joint Asia Diabetes Evaluation cohort), Yeung et al.32 showed that approximately 18% of the diabetes were young‐onset (diagnosed before 40 years‐of‐age). They had longer disease duration, higher mean concentrations of HbA1c and low‐density lipoprotein cholesterol and higher prevalence of retinopathy than those of late‐onset diabetes (diagnosed at 40 years‐of‐age or older)32. Genetic variants in genes, such as DACH1, might give some explanations of why young diabetics are characterized by obesity and increased risk for cardiovascular disease33, their unique way of life might also contribute to the worse clinical outcome. This special group of patients should not be neglected in the education program.
In the comparison across different regions, we found that the patients from the midwest of the province (patients of city Jinhua, Lishui and Quzhou) showed the highest level of average WHR (P < 0.001), and the lowest percentage of patients who achieved the blood pressure target (P < 0.001), compared with the other two regions. With regard to eating habits, more patients from this region preferred salty flavors, which is 33.93% compared with 25.29% in the north and 26.11% in the east. It would be interesting to carry out further studies to see whether these differences are related to the disease prevalence and clinical outcomes. In addition, this region is relatively less developed, and this could lead to less diabetes education input in the clinical management.
With regard to physical activity, no significant difference was observed between different age groups and across different regions. Patients spent most of their daily time sitting and sleeping (including the time when the patients were lying down). The time for moderate and vigorous activity was short, with an average time of 2.53 ± 6.71 h and 1.70 ± 8.03 h, respectively. As recommended by the standards of medical care provided by the ADA in 2015, adult diabetics should carry out at least 150 min/week of moderate‐intensity aerobic physical activity15. In the present study, just 30.64% of patients spent more than 150 min/week on moderate to vigorous physical activities, and 60.46% of the patients did not carry out any activity of this intensity during the whole week. Although some patients might not be able to engage in certain activities because of their medical conditions, it is still meaningful to point out that even in the young group, 50.98% of the patients were absent for moderate‐vigorous activities. In another survey from Hunan province of central China, Zhou et al.34 recruited 163 diabetes patients to investigate their self‐care practices. They reported that just 9% of the patients were most active, whereas more than half the patients were least active in total daily life34. This ‘lazy’ lifestyle is obviously not satisfying, which calls for more effort on education for physical activity and better self‐management of patients.
The present study had several limitations. First, more detailed information about the composition of the macronutrients, such as the glucose categories and percentage of saturated fatty in total fat consumption, was not included. Second, some clinical data, such as blood glucose or HbA1c level, blood lipid profile and complication occurrence, were not included, which to a large extent was due to the difficulty in unifying the different test standards among different centers. As a result, we were not able to clearly define the dietary patterns, and determine the association between certain living habit and clinical outcomes. Third, our data were obtained from patients seeking care from top hospitals in the selected cities, which might not be able to present the situations among patients who usually visit community hospitals for diabetes care. The education and income levels of the participants were not taken into consideration, which could lead to bias in our analysis. Future studies are required to examine the relative contributions of dietary and exercise pattern to diabetes prevalence, as well as blood glucose control and complication risks in this region.
Here, we conclude that in Zhejiang province, more female type 2 diabetes patients achieved blood pressure control goal and they paid more attention to diet control than the male patients. Most of the patients had diets that were high in carbohydrate and fat, but low in protein. Among almost all the patients, the predominant daily routine was sitting or sleeping, and the time for moderate‐vigorous activity was insufficient.
Disclosure
The authors declare no conflict of interest.
Acknowledgments
This work was supported by Zhejiang Province Key Science and Technology Innovation Team (grant number: 2013TD13), Zhejiang Provincial Natural Science Foundation of China (grant number: LQ16H160007) and the Project of the Dietary Intervention for Type 2 Diabetes (grant number: Y201225325). We thank Professor Peter Nelson and Daniel Peng for critical review and editing of the manuscript.
J Diabetes Investig 2016; 7: 529–538
Xiaowen He, Jie Pan and Mingxia Pan contributed equally to this manuscript.
Mingxia Pan is an on‐the‐job postgraduate student.
References
- 1. Yang W, Lu J, Weng J, et al Prevalence of diabetes among men and women in China. N Engl J Med 2010; 362: 1090–1101. [DOI] [PubMed] [Google Scholar]
- 2. Chan JC, Zhang Y, Ning G. Diabetes in China: a societal solution for a personal challenge. Lancet Diabetes Endocrinol 2014; 2: 969–979. [DOI] [PubMed] [Google Scholar]
- 3. Pan XR, Yang WY, Li GW, et al Prevalence of diabetes and its risk factors in China, 1994. National Diabetes Prevention and Control Cooperative Group. Diabetes Care 1997; 20: 1664–1669. [DOI] [PubMed] [Google Scholar]
- 4. Sarwar N, Gao P, Seshasai SR, et al Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta‐analysis of 102 prospective studies. Lancet 2010; 375: 2215–2222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Yang X, So W, Ko GT, et al Independent associations between low‐density lipoprotein cholesterol and cancer among patients with type 2 diabetes mellitus. CMAJ 2008; 179: 427–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Yang X, So WY, Ma RC, et al Diabetes and cancer: the mechanistic implications of epidemiological analyses from the Hong Kong Diabetes Registry. Diabetes Metab Res Rev 2012; 28: 379–387. [DOI] [PubMed] [Google Scholar]
- 7. Xu CX, Zhu HH, Zhu YM. Diabetes and cancer: associations, mechanisms, and implications for medical practice. World J Diabetes 2014; 5: 372–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Andrews RC, Cooper AR, Montgomery AA, et al Diet or diet plus physical activity versus usual care in patients with newly diagnosed type 2 diabetes: the Early ACTID randomised controlled trial. Lancet 2011; 378: 129–139. [DOI] [PubMed] [Google Scholar]
- 9. Cho Y, Shin MJ, Chung HK. Effects of diet modification on meal quality and quality of life in Korean diabetic patients: data from Korea national health and nutrition examination survey (2007–2011). Clin Nutr Res 2014; 3: 106–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Snowling NJ, Hopkins WG. Effects of different modes of exercise training on glucose control and risk factors for complications in type 2 diabetic patients: a meta‐analysis. Diabetes Care 2006; 29: 2518–2527. [DOI] [PubMed] [Google Scholar]
- 11. Thomas DE, Elliott EJ, Naughton GA. Exercise for type 2 diabetes mellitus. Cochrane Database Syst Rev 2006; CD002968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Boule NG, Haddad E, Kenny GP, et al Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus: a meta‐analysis of controlled clinical trials. JAMA 2001; 286: 1218–1227. [DOI] [PubMed] [Google Scholar]
- 13. Thomas D, Elliott EJ. Low glycaemic index, or low glycaemic load, diets for diabetes mellitus. Cochrane Database Syst Rev 2009; CD006296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Nield L, Moore HJ, Hooper L, et al Dietary advice for treatment of type 2 diabetes mellitus in adults. Cochrane Database Syst Rev 2007; CD004097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. The American Diabetes Association . Standards of medical care in diabetes–2015: summary of revisions. Diabetes Care 2015; 38 (Suppl): S4. [DOI] [PubMed] [Google Scholar]
- 16. Evert AB, Boucher JL, Cypress M, et al Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care 2013; 36: 3821–3842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Institute of Medicine . The Role of Nutrition in Maintaining Health in the Nation's Elderly: Evaluating Coverage of Nutrition Services for the Medicare Population. National Academies Press, Washington, DC, 2000. [PubMed] [Google Scholar]
- 18. Wolf AM, Conaway MR, Crowther JQ, et al Translating lifestyle intervention to practice in obese patients with type 2 diabetes: improving control with activity and nutrition (ICAN) study. Diabetes Care 2004; 27: 1570–1576. [DOI] [PubMed] [Google Scholar]
- 19. Al‐Shookri A, Khor GL, Chan YM, et al Effectiveness of medical nutrition treatment delivered by dietitians on glycaemic outcomes and lipid profiles of Arab, Omani patients with Type 2 diabetes. Diabet Med 2012; 29: 236–244. [DOI] [PubMed] [Google Scholar]
- 20. Coppell KJ, Kataoka M, Williams SM, et al Nutritional intervention in patients with type 2 diabetes who are hyperglycaemic despite optimised drug treatment–lifestyle over and above drugs in diabetes (LOADD) study: randomised controlled trial. BMJ 2010; 341: c3337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ali MK, Bullard KM, Saaddine JB, et al Achievement of goals in U.S. diabetes care, 1999–2010. N Engl J Med 2013; 368: 1613–1624. [DOI] [PubMed] [Google Scholar]
- 22. Zhong X, Tanasugarn C, Fisher EB, et al Awareness and practices of self‐management and influence factors among individuals with type 2 diabetes in urban community settings in Anhui Province, China. Southeast Asian J Trop Med Public Health 2011; 42: 185–186, 184, 187–196. [PubMed] [Google Scholar]
- 23. Stern L, Iqbal N, Seshadri P, et al The effects of low‐carbohydrate versus conventional weight loss diets in severely obese adults: one‐year follow‐up of a randomized trial. Ann Intern Med 2004; 140: 778–785. [DOI] [PubMed] [Google Scholar]
- 24. Elhayany A, Lustman A, Abel R, et al A low carbohydrate Mediterranean diet improves cardiovascular risk factors and diabetes control among overweight patients with type 2 diabetes mellitus: a 1‐year prospective randomized intervention study. Diabetes Obes Metab 2010; 12: 204–209. [DOI] [PubMed] [Google Scholar]
- 25. Shai I, Schwarzfuchs D, Henkin Y, et al Weight loss with a low‐carbohydrate, Mediterranean, or low‐fat diet. N Engl J Med 2008; 359: 229–241. [DOI] [PubMed] [Google Scholar]
- 26. Wolever TM, Gibbs AL, Mehling C, et al The Canadian trial of carbohydrates in diabetes (CCD), a 1‐y controlled trial of low‐glycemic‐index dietary carbohydrate in type 2 diabetes: no effect on glycated hemoglobin but reduction in C‐reactive protein. Am J Clin Nutr 2008; 87: 114–125. [DOI] [PubMed] [Google Scholar]
- 27. Davis NJ, Tomuta N, Schechter C, et al Comparative study of the effects of a 1‐year dietary intervention of a low‐carbohydrate diet versus a low‐fat diet on weight and glycemic control in type 2 diabetes. Diabetes Care 2009; 32: 1147–1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gannon MC, Nuttall FQ, Saeed A, et al An increase in dietary protein improves the blood glucose response in persons with type 2 diabetes. Am J Clin Nutr 2003; 78: 734–741. [DOI] [PubMed] [Google Scholar]
- 29. Parker B, Noakes M, Luscombe N, et al Effect of a high‐protein, high‐monounsaturated fat weight loss diet on glycemic control and lipid levels in type 2 diabetes. Diabetes Care 2002; 25: 425–430. [DOI] [PubMed] [Google Scholar]
- 30. Wycherley TP, Noakes M, Clifton PM, et al A high‐protein diet with resistance exercise training improves weight loss and body composition in overweight and obese patients with type 2 diabetes. Diabetes Care 2010; 33: 969–976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Brinkworth GD, Noakes M, Parker B, et al Long‐term effects of advice to consume a high‐protein, low‐fat diet, rather than a conventional weight‐loss diet, in obese adults with type 2 diabetes: one‐year follow‐up of a randomised trial. Diabetologia 2004; 47: 1677–1686. [DOI] [PubMed] [Google Scholar]
- 32. Yeung RO, Zhang Y, Luk A, et al Metabolic profiles and treatment gaps in young‐onset type 2 diabetes in Asia (the JADE programme): a cross‐sectional study of a prospective cohort. Lancet Diabetes Endocrinol 2014; 2: 935–943. [DOI] [PubMed] [Google Scholar]
- 33. Ma RC, Lee HM, Lam VK, et al Familial young‐onset diabetes, pre‐diabetes and cardiovascular disease are associated with genetic variants of DACH1 in Chinese. PLoS One 2014; 9: e84770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Zhou Y, Liao L, Sun M, et al Self‐care practices of Chinese individuals with diabetes. Exp Ther Med 2013; 5: 1137–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]


