Abstract
Aim/Introduction
Waist circumference (WC) is the most important parameter for diagnosis of metabolic syndrome. The present study was carried out to obtain optimal WC cut‐off values for diagnosis of metabolic syndrome in a Japanese population based on the measurement of total intra‐abdominal visceral fat volume (VFV), which could be expected to reflect visceral obesity more precisely than visceral fat area.
Materials and Methods
A total of 405 Japanese persons undergoing health screening were investigated. visceral fat volume was calculated from the data in 700–800 computed tomography slices from the top of the liver to the floor of the pelvic cavity. Then, receiver operating characteristic analysis was used to determine the cut‐off value of the VFV/height ratio. Subsequently, the corresponding WC value was obtained by linear regression analysis.
Results
The cut‐off value of the VFV/height ratio was 2,317 cm3/m in men and 1,425 cm3/m in women. The sensitivity and specificity of the ratio were 52.9 and 86.4% in men vs 63.4 and 82.2% in women, respectively. The corresponding cut‐off value of WC was 86.0 cm in men and 80.9 cm in women.
Conclusions
The proposed cut‐off values of WC for metabolic syndrome are 85 cm in Japanese men and 80 cm in Japanese women.
Keywords: Metabolic syndrome, Visceral fat volume, Waist circumference
Introduction
Persons with metabolic syndrome (MetS) are twice as likely to develop cardiovascular disease and five times more likely to develop type 2 diabetes mellitus than persons without MetS1. The features of MetS include: (i) elevation of triglycerides (TG); (ii) reduction of high‐density lipoprotein cholesterol (HDL‐C); (iii) elevation of blood pressure (BP); (iv) elevation of fasting glucose (FG); and (v) visceral obesity. Along with excessive accumulation of intrahepatic and/or intramuscular fat, visceral obesity is known as a major cause of insulin resistance, and it is closely associated with the other four features of MetS through an imbalance between adipokines and insulin2. To precisely assess the visceral fat volume (VFV), abdominal computed tomography (CT) or magnetic resonance imaging needs to be carried out, but these methods are not suitable for a mass screening program for MetS because of time and cost considerations. Instead, waist circumference (WC) is used as a simple indicator of visceral obesity, and the MetS diagnostic criteria include WC as an obligatory feature of this syndrome3.
However, the prevalence of visceral obesity and the WC value associated with a high risk of the development of type 2 diabetes mellitus or cardiovascular disease are influenced by ethnicity, age, sex and other factors4, and various WC values have already been proposed as indicators of MetS over the past decade3, 5, 6, 7, 8, 9. Against this background, the Joint Scientific Statement on diagnostic criteria for MetS was recently published by a group of six organizations including the International Diabetes Federation Task Force on Epidemiology and Prevention; the National Heart, Lung, and Blood Institute; the American Heart Association; the World Heart Federation; the International Atherosclerosis Society; and the International Association for the Study of Obesity10. This statement covered three main points. First, WC was not the essential diagnostic criterion for MetS, but was one of five features (TG, HDL‐C, BP, FG and WC), and the presence of any three of the five features was sufficient for diagnosis of MetS. Second, cut‐off values for the four features other than WC would be set as: TG ≥150 mg/dL, HDL‐C < 40 mg/dL (men) and <50 mg/dL (women), systolic BP ≥130 mmHg and/or diastolic BP ≥85 mmHg, FG ≥100 mg/dL. Third, the cut‐off value of WC required further study, so national or regional values for WC could be used in the interim.
Regarding the cut‐off value of WC in Asia, the International Diabetes Federation recommended 90 cm for men and 80 cm for women11. In contrast, the Japan Society for the Study of Obesity (JASSO) has recommended that the appropriate cut‐off values of WC for detecting visceral obesity are 85 cm in Japanese men and 90 cm in Japanese women from the general population12, and these values are widely used for diagnosis of MetS in Japan. As the JASSO cut‐off value of WC is higher for women than men, unlike the criteria used in other Asian countries, reassessment of the cut‐off values for Japanese persons has been carried out previously, and different values have been proposed13, 14, 15, 16, 17, 18, 19. However, these previous Japanese studies were based on WC and/or the visceral fat area (VFA) at the umbilicus determined by CT scanning. To precisely assess the accumulation of visceral fat, it might be preferable to measure the total VFV in the abdominal cavity. In addition, the cut‐off value of WC for MetS should be considered in relation to the cut‐off value of VFV for MetS.
We have developed a new method for evaluating VFV by analysis of 700–800 CT slices obtained from the top of the liver to the pelvic floor20, 21. Although the VFA at the umbilicus has been widely used to identify visceral obesity13, 14, 15, 16, 17, 18, 19, we previously showed that the maximal VFA was not at the umbilicus, but was widely distributed from L1 to L520, 21.
In the present study, we measured VFV in Japanese persons undergoing health screening, and attempted to determine the cut‐off value of VFV for separating metabolically normal Japanese persons without any of the four features of MetS in the Joint Scientific Statement other than WC (high TG, low HDL‐C, high BP, high FG)10 from persons with one or more of these four features. We also determined the cut‐off value of WC corresponding to the cut‐off value of VFV by linear regression analysis.
Methods
Participants
The study participants were 405 Japanese persons (239 men and 166 women) from the general population who underwent health screening at the International University of Health and Welfare Hospital (Nasushiobara, Tochigi). We excluded women who were pregnant or breast‐feeding, and persons with a history of cardiovascular disease, hepatic disease or other factors that made them inappropriate for this study (e.g., persons who had undergone CT several times recently). Persons with normal values for four features of MetS (TG, HDL‐C, BP and FG) in the Joint Scientific Statement10 were defined as metabolically normal. Persons on drug treatment for hyperlipidemia, hypertension or diabetes were defined as having the corresponding features of MetS.
Measurements
Height and bodyweight were determined by automated measurement (BF‐220; Tanita Co. Ltd., Tokyo, Japan). WC was measured at the umbilicus in the standing position during quiet breathing by using an inelastic tape measure. In participants with marked periumbilical fat accumulation, measurement was carried out at a point midway between the lower margin of the ribs and the anterior superior iliac spine. BP was measured in the sitting position by one of two automatic devices (UA‐786; A&D Co Ltd., Saitama, Japan; or Kentaro HBP‐9020; Omron Co. Ltd., Kyoto, Japan).
Laboratory tests
A blood sample was collected in the morning while fasting. Free fatty acids (FFA) and immunoreactive insulin (IRI) were measured by an enzymatic method (LSI Medience Co. Ltd., Tokyo, Japan) and a chemiluminescence immunoassay (LSI Medience Co. Ltd.), respectively. Glycated hemoglobin (National Glycohemoglobin Standardization Program) was measured by the latex agglutination method, and other tests were carried out by standard methods (SRL Co. Ltd., Tokyo, Japan).
CT measurement of abdominal fat volume
All participants underwent CT scanning in the supine position with both arms raised above the head after urination. A 16‐row multidetector CT unit (Aquillion™ 16; Toshiba Medical Systems Corp., Tokyo, Japan) was used with scanning conditions of 120 kV, 250–300 mA and 0.5‐s rotation. The protocol involved acquisition of 700–800 images with a slice thickness of 0.5 mm at 8‐mm intervals from the top of liver to the floor of the pelvic cavity. Adipose tissue was identified as the pixels ranging from –190 to –30 Hounsfield units, as reported previously22. All imaging data were transferred to a PC workstation for analysis of the total abdominal fat volume. Visceral fat volume and the subcutaneous abdominal fat volume (SFV) were calculated with SYNAPSE VINCENT® software (Fuji Film, Tokyo, Japan). VFA was calculated at the mid‐umbilical level. To prevent an interobserver variation, assessment of adipose tissue was carried out by the same examiner.
Adjustment of VFV for physique
The VFV/height ratio and VFV/abdominal length ratio were calculated to adjust VFV for the influence of body height or the length of the abdomen, respectively. Then the area under the receiver operating characteristic (ROC) curve was calculated for each index to compare their relative ability to correctly classify the participants.
Statistical analysis
Results are presented as the mean ± standard deviation. Comparison of mean values between the groups was carried out by Student's t‐test. Correlations among VFV, anthropometric measurements, and laboratory data were evaluated by Pearson's univariate multiple regression analysis. ROC analysis was carried out to determine the sensitivity, specificity and area under the curve for each potential index of MetS. All statistical analyses were carried out with EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan) and graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria), a modified version of R commander that includes statistical functions frequently used in biostatistics. Statistical significance was accepted at P < 0.05.
The present study was carried out according to the principles of the Declaration of Helsinki, and was approved by the ethics review board of the International University of Health and Welfare. Informed consent was obtained from all of the participants.
Results
The demographic and clinical characteristics of the participants are presented in Table 1. While age did not differ between the sexes, height, bodyweight, body mass index (BMI), WC and abdominal length were significantly larger in men than in women. The VFA, VFV, VFV/height ratio and VFV/abdominal length ratio were all larger in men than in women, whereas SFV was smaller. VFV was larger than SFV in men (3,736 ± 1,633 vs 3,370 ± 1,618 cm3, P < 0.05), whereas it was smaller than SFV in women (2,309 ± 1,195 vs 4,576 ± 2,032 cm3, P < 0.001). When participants who had no features of MetS except for a high WC were assessed, there was a significantly lower percentage of such persons among men than among women (27.6 vs 44.0%, P < 0.001).
Table 1.
Demographic and clinical characteristics of the subjects
| n (%) | Total | Men | Women | P | |
|---|---|---|---|---|---|
| 405 (100) | 239 (59) | 166 (41) | |||
| Age | years | 53.8 ± 10.2 | 54.0 ± 10.6 | 53.5 ± 9.7 | 0.59 |
| Height | cm | 164.4 ± 8.5 | 169.6 ± 6.1 | 157.1 ± 5.6 | <0.001 |
| Weight | kg | 64.0 ± 12.0 | 69.3 ± 10.6 | 56.4 ± 9.6 | <0.001 |
| Body mass index (BMI) | kg/m2 | 23.6 ± 3.4 | 24.1 ± 3.2 | 22.9 ± 3.6 | <0.001 |
| Waist circumference (WC) | cm | 83.7 ± 9.1 | 85.3 ± 8.1 | 81.4 ± 10.0 | <0.001 |
| Abdominal length (AL) | cm | 48.2 ± 3.5 | 48.9 ± 3.5 | 47.3 ± 3.3 | <0.001 |
| Triglycerides | mg/dl | 112.3 ± 74.4 | 126.9 ± 79.9 | 91.3 ± 59.9 | <0.001 |
| HDL cholesterol | mg/dl | 57.0 ± 13.4 | 53.5 ± 12.9 | 62.1 ± 12.6 | <0.001 |
| Systolic blood pressure | mmHg | 117.8 ± 14.5 | 119.4 ± 12.6 | 115.5 ± 16.6 | <0.001 |
| Diastolic blood pressure | mmHg | 72.9 ± 9.6 | 74.3 ± 8.8 | 70.8 ± 10.3 | <0.001 |
| Fasting plasma glucose | mg/dl | 100.7 ± 17.4 | 102.7 ± 19.7 | 97.8 ± 12.9 | <0.001 |
| Total cholesterol | mg/dl | 199.4 ± 31.1 | 199.2 ± 30.9 | 199.6 ± 31.5 | 0.89 |
| LDL cholesterol | mg/dl | 121.0 ± 27.7 | 122.6 ± 27.0 | 118.7 ± 28.5 | 0.15 |
| Hemoglobin A1c | % | 5.6 ± 0.6 | 5.6 ± 0.6 | 5.6 ± 0.5 | 0.94 |
| HOMA‐R | 1.6 ± 3.4 | 1.8 ± 4.4 | 1.4 ± 0.7 | 0.22 | |
| VFA | cm2 | 113.8 ± 56.3 | 130.6 ± 57.7 | 89.6 ± 44.2 | <0.001 |
| SFV | cm3 | 3,864 ± 1,889 | 3,370 ± 1,618 | 4,576 ± 2,023 | <0.001 |
| VFV | cm3 | 3,151 ± 1,627 | 3,736 ± 1,633 | 2,309 ± 1,195 | <0.001 |
| VFV/height ratio | cm3/m | 1,905 ± 952 | 2,207 ± 958 | 1,471 ± 758 | <0.001 |
| VFV/AL ratio | cm3/m | 6,444 ± 3,093 | 7,572 ± 3,055 | 4,828 ± 2,345 | <0.001 |
| Features of MetS | |||||
| Elevated triglycerides | % | 33.9 | 37.8 | 28.3 | 0.05 |
| HDL‐C | % | 14.6 | 12.6 | 17.5 | 0.19 |
| Elevated blood pressure | % | 33.2 | 37.4 | 27.1 | 0.031 |
| Elevated fasting glucose | % | 41.6 | 48.3 | 31.9 | 0.001 |
| No features | % | 34.3 | 27.6 | 44.0 | <0.001 |
| Two or more features | % | 38.8 | 44.8 | 30.1 | 0.004 |
Values are presented as the mean ± SD or number (%) VFA, abdominal visceral fat area; SFV, abdominal subcutaneous fat volume; VFV, abdominal visceral fat volume. P values were calculated by the t‐test for continuous variables and Fisher's exact test for categorical variables.
The area under the ROC curve was calculated to compare the ability of each index of visceral obesity to correctly classify the participants. As shown in Table 2, the WC had the smallest area and the VFV/height ratio had the largest area among the indices. In addition, the cut‐off values of the indices were generally higher in men than in women. ROC curves for identifying metabolically normal persons with various cut‐off values of VFV are shown in Figure 1a (men) and b (women). According to ROC data, the cut‐off value yielding the maximal sensitivity plus specificity was 3,885 cm3 in men and 2,321 cm3 in women. With these cut‐off values, the sensitivity and specificity were 53.8 and 84.8% in men vs 60.2 and 82.2% in women, respectively. ROC curves for the VFV/height ratio are shown in Figure 2. The cut‐off value with the maximum sensitivity plus specificity was 2,317 cm3/m in men and 1,425 cm3/m in women. With these cut‐off values, the sensitivity and specificity were 52.9 and 86.4% in men vs 63.4 and 82.2% in women, respectively.
Table 2.
Results of receiver operating characteristic (ROC) analysis
| ROC curve | Cut‐off value | Area | 95%CI |
|---|---|---|---|
| Men | |||
| WC (cm) | 82.1 | 0.669 | 0.589–0.748 |
| VFA (cm2) | 107.2 | 0.725 | 0.655–0.795 |
| VFV (cm3) | 3,885 | 0.746 | 0.678–0.814 |
| VFV/AL ratio (cm3/m) | 6,791 | 0.754 | 0.687–0.820 |
| VFV/Height ratio (cm3/m) | 2,317 | 0.756 | 0.689–0.822 |
| Women | |||
| WC (cm) | 78.0 | 0.739 | 0.664–0.814 |
| VFA (cm2) | 98.3 | 0.770 | 0.698–0.841 |
| VFV (cm3) | 2,321 | 0.762 | 0.690–0.834 |
| VFV/AL ratio (cm3/m) | 4,812 | 0.771 | 0.669–0.842 |
| VFV/Height ratio (cm3/m) | 1,425 | 0.772 | 0.701–0.843 |
Figure 1.
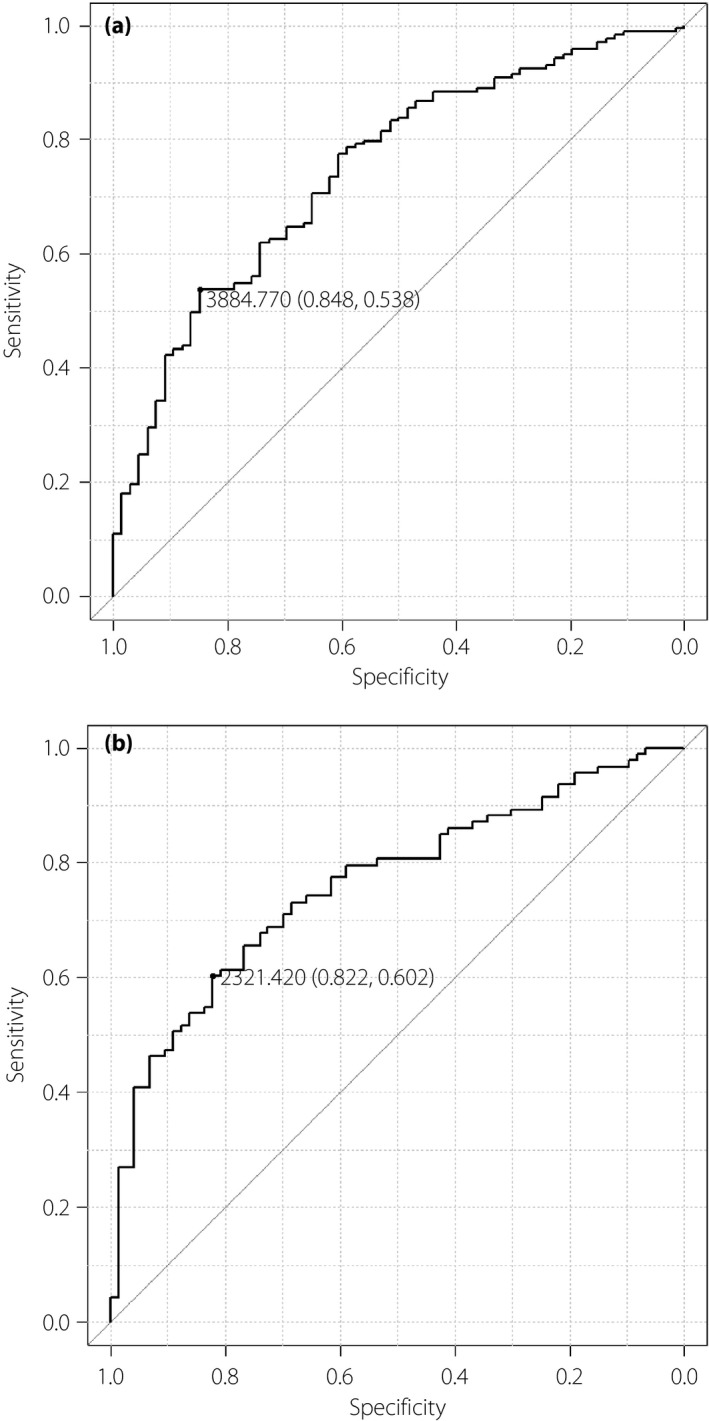
Receiver operating characteristic (ROC) curves for identifying metabolically normal persons with various cut‐off values of visceral fat volume (VFV) in (a) men and (b) women. ●, Cut‐off visceral fat volume yielding the maximum sensitivity + specificity for predicting risk factors for metabolic syndrome.
Figure 2.
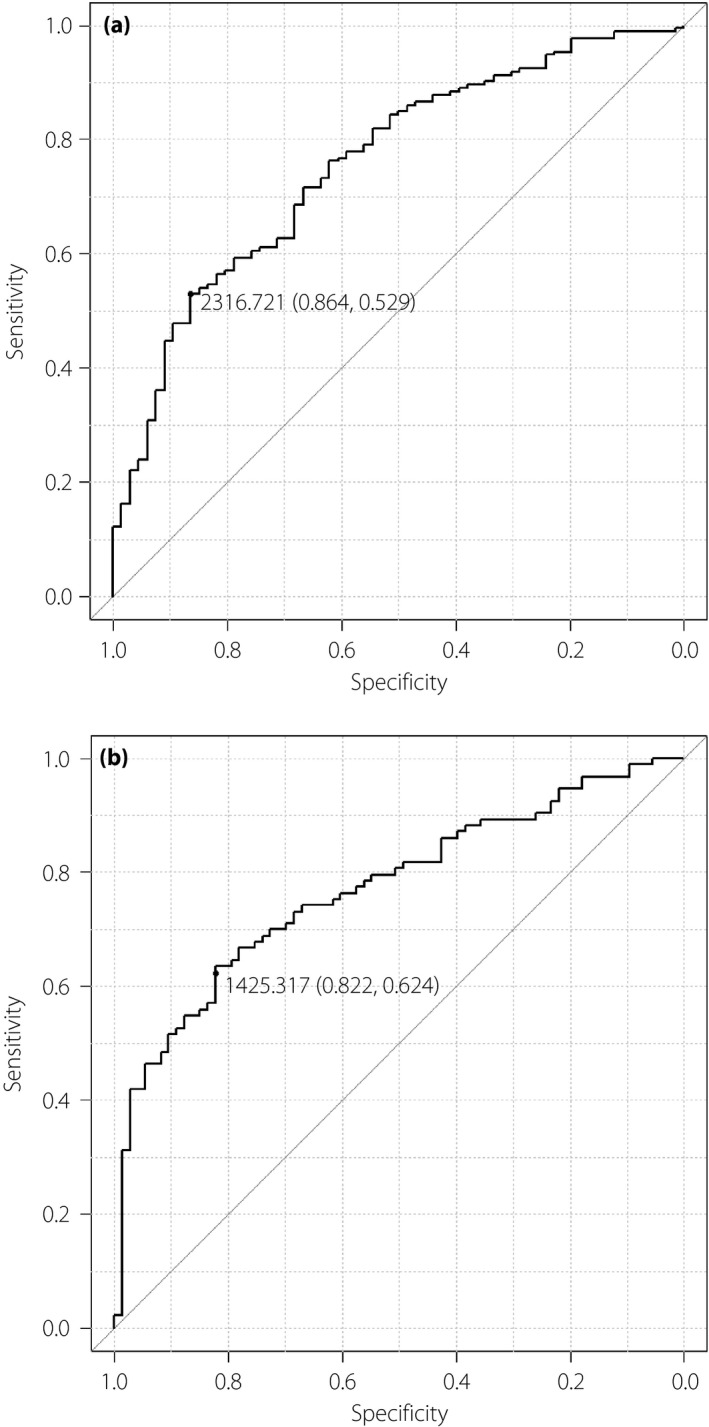
Receiver operating characteristic curves for identifying metabolically normal persons with various cut‐off values of visceral fat volume/height ratio in (a) men and (b) women. ●, Cut‐off visceral fat volume/height ratio yielding the maximum sensitivity + specificity for predicting risk factors for metabolic syndrome.
Scatter plots of the VFV/height ratio (x‐axis) vs WC (y‐axis) are shown in Figure 3a for men and Figure 3b for women. Linear regression analysis of the VFV/height ratio vs WC yielded a y‐intercept of 70.20 and a slope of 0.0068 in men, whereas the y‐intercept was 65.60 and the slope was 0.010 in women. There was a strong positive correlation between these two variables in both sexes, with a correlation coefficient (r) of 0.812 (95% CI 0.764–0.851) in men and 0.816 (95% CI 0.758–0.861) in women. The WC corresponding to a VFV/height ratio of 2,317 cm3/m was 86.0 cm in men, whereas the WC corresponding to a ratio of 1,425 cm3/m was 80.9 cm in women. Then we will simplify them for clinical convenience and propose the cut‐off point of WC for the criteria of metabolic syndrome in the Japanese population to be 85 cm in men and 80 cm in women. When the cut‐off values of WC were set at 85 cm in men and 80 cm in women, the sensitivity and the specificity for identifying MetS with the presence of any three of the five features were 69.3 and 93.4% in men vs 61.5 and 90.9% in women.
Figure 3.
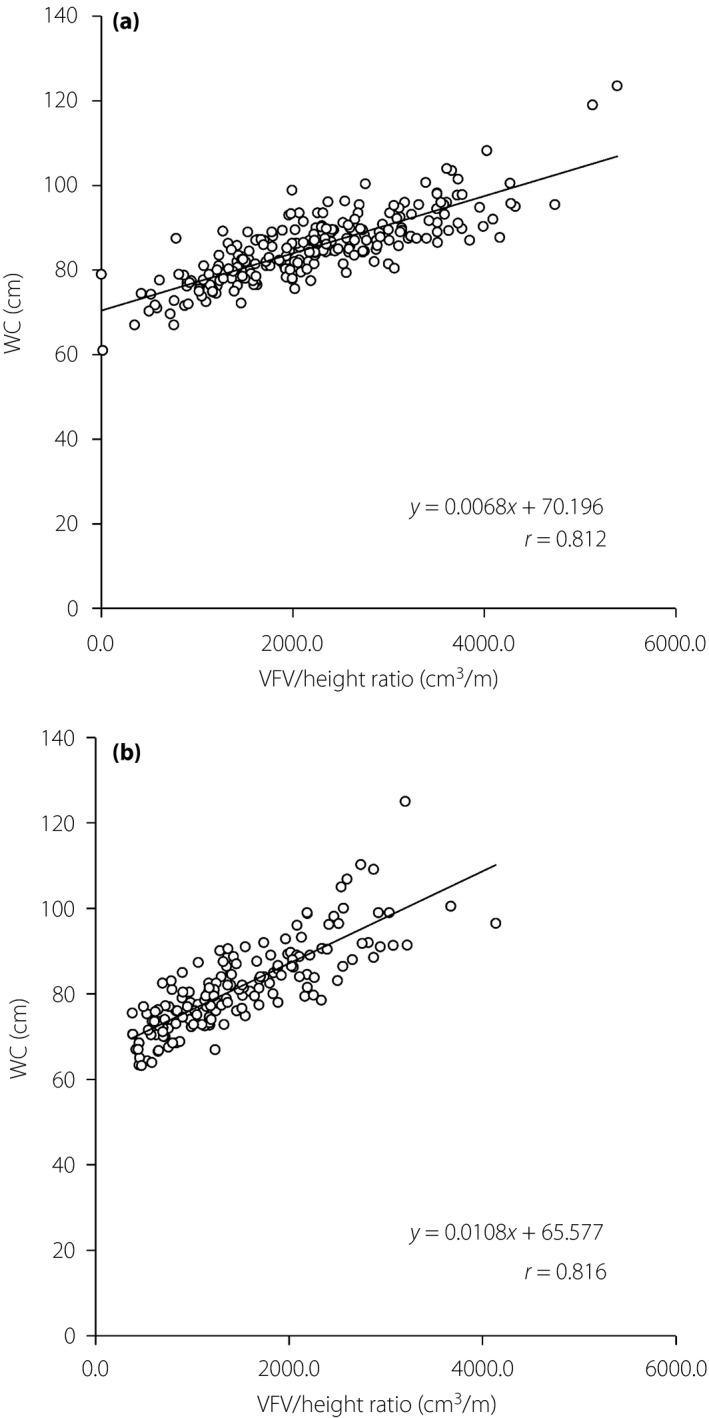
Scatter plots of the visceral fat volume (VFV)/height ratio (x‐axis) vs waist circumference (WC; y‐axis) in (a) men and (b) women.
Discussion
Three main findings were obtained in the present study. First, VFA, VFV, VFV/height ratio and VFV/abdominal length ratio were larger in men than in women, whereas SFV was smaller in men. Also, VFV was larger than SFV in men, but was smaller than SFV in women. Second, the cut‐off values of VFV and the VFV/height ratio that separated metabolically normal persons from persons with at least one feature of MetS (except a high WC) were approximately 3,900 cm3 and 2,300 cm3/m in men vs 2,300 cm3 and 1,400 cm3/m in women, respectively. Third, the cut‐off values of WC corresponding to these VFV/height ratios were 85 cm in men and 80 cm in women.
We previously evaluated the sex difference of the SFV/VFV ratio in 131 Japanese persons by using the same method of whole abdominal CT scanning, and we found a significantly higher SFV/VFV ratio in women than in men (1.78 ± 0.83 vs 1.08 ± 0.54, P < 0.001), despite no difference of BMI or WC20. However, the sex difference of SFV and VFV has not been fully investigated. Fox et al.13 compared the partial (not total) abdominal visceral and subcutaneous fat volumes in 1,649 men and 1,452 women from the Framingham Heart Study cohort by analyzing a region of 125 mm above S1 on CT scans. They reported that the mean VFV was 1.6‐fold larger than the subcutaneous fat volume in men, whereas the mean subcutaneous fat volume was 1.2‐fold larger than the VFV in women, with BMI and WC both being slightly higher in men. These resu‐lts are consistent with our present findings, and suggest a sex difference in the distribution of abdominal fat that should be considered when selecting the optimal WC value for identification of visceral obesity.
The present study is the first to propose cut‐off values of VFV and the VFV/height ratio for separating metabolically normal Japanese persons from those with one or more risk factors for MetS. We found that a VFV of 3,900 cm3 and a VFV/height ratio of 2,300 cm3/m might be useful markers of visceral obesity in Japanese men, whereas the corresponding values were 2,300 cm3 and 1,400 cm3/m in women. To precisely measure the entire volume of visceral fat has been methodologically difficult, but we used commercially available software to calculate VFV and SFV by analysis of CT data in the present study. Although our method can also analyze subtle regional changes of visceral and subcutaneous fat, and might be useful for investigation of obesity, exposure to radiation is problematic. The approximate exposure to radiation with whole abdominal examination by a 16‐row multidetector CT scanner was 8–10 mSv in the present study, and it might be 10–15 mSv with the new 64‐row multidetector CT scanners. Thus, we need to choose subjects for VFV analysis carefully by considering this point.
Based on the present findings, we proposed 85 cm for Japanese men and 80 cm for Japanese women as the WC values identifying MetS. The joint Scientific Statement published in 2009 recommended that separate cut‐off values of WC should be set for different ethnic groups10. The Statement also mentioned that several different WC values have been proposed in Japan, ranging from >85–90 cm for men and >80 cm for women in recent studies23, 24, 25, in contrast to the JASSO cut‐off values of ≥85 cm for men and ≥90 cm for women9. Although the JASSO cut‐off value is consistent with our present value for men, the value we obtained for women was 10‐cm smaller than the JASSO value. To explain this discrepancy, three points might be considered. First, the original JASSO cut‐off values of ≥85 cm for men and ≥90 cm for women were based on the common VFA cut‐off value of ≥100 cm2 for identifying visceral obesity in both men and women, as analysis of the VFA value separating normal persons from those with one or more features of MetS was carried out in men and women combined12. However, the WC corresponding to the same VFA value might be higher in women than in men, because the SFV/VFV ratio is much higher in women, as discussed above. In contrast, we analyzed each sex separately, and we found that the cut‐off values of both VFV and the VFV/height ratio were higher in men (3,885 cm3 and 2,317 cm3/m) than in women (2,321 cm3 and 1,425 cm3/m). Similarly, Oka et al.16 proposed 132.6 cm2 and 91.5 cm2 as the cut‐off values of VFA in men and women, respectively. We also assessed various cut‐off values of WC according to different approaches. The cut‐off values of WC in men were greater than those in women in any conditions (Table S1). Second, the definitions of each feature of MetS were different. We used the values in the 2009 joint Scientific Statement10, whereas the JASSO study12 used the following values: TG ≥150 mg/dL, HDL‐C < 40 mg/dL (in both men and women), systolic BP ≥140 mmHg, diastolic BP ≥90 mmHg, FG ≥110 mg/dL and also included total cholesterol ≥220 mg/dL in the features of dyslipidemia. Third, the correlations between VFA and WC were weaker in the JASSO study (r = 0.68 in men [n = 775] and r = 0.65 in women [n = 418]) than those between the VFV/height ratio and WC in the present study (r = 0.81 in men [n = 239] and r = 0.82 in women [n = 166]), despite the larger number of participants in the earlier study. When we assessed the correlation between VFA and WC in the present study, we obtained even stronger relationships (r = 0.81 in men and r = 0.80 in women). The reason for this discrepancy is unclear, but progress in software used for analysis and the resolution of CT scanners might be involved.
The present study had several limitations. First, as aforementioned, our method was associated with radiation exposure and high cost. This might be a hurdle to studying a large population, and the number of participants we assessed was smaller than in some of the previous studies23, 24, 25. In addition, the present study was limited to residents of Tochigi prefecture in an area located approximately 150 km north of Tokyo, and it is unclear whether they were representative of the general Japanese population. Despite these limitations and the potential for bias, the present results suggest that consideration should be given to modifying the previous cut‐off values.
In conclusion, we propose a VFV/height ratio of 2,300 cm3/m in Japanese men and 1,400 cm3/m in Japanese women as cut‐off values for MetS, as well as WC values of 85 cm in men and 80 cm in women. Further investigations on a larger scale and in wider regions of Japan would be required to confirm these results.
Disclosure
The authors declare no conflict of interest.
Supporting information
Table S1¦ Optimal cut‐off values, area under the receiver operating characteristic curve, sensitivity and specificity predicting metabolic syndrome.
J Diabetes Investig 2016; 7: 587–593
References
- 1. Grundy SM. Metabolic syndrome pandemic. Arterioscler Thromb Vasc Biol 2004; 28: 629–636. [DOI] [PubMed] [Google Scholar]
- 2. Assmann G, Guerra R, Fox G, et al Harmonizing the definition of the metabolic syndrome: Comparison of the criteria of the Adult Treatment Panel III and the International Diabetes Federation in United States American and European Populations. Am J Cardiol 2007; 99: 541–548. [DOI] [PubMed] [Google Scholar]
- 3. Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part1:Diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 1998; 15: 539–553. [DOI] [PubMed] [Google Scholar]
- 4. Klein S, Allison DB, Heymsfield SB, et al Waist circumference and cardiometabolic risk: A consensus statement from shaping America's health: association for Weight Management and Obesity Prevention; NAASO, the Obesity Society; the American Society for Nutrition; and the American Diabetes Association. Diabetes Care 2007; 30: 1647–1652. [DOI] [PubMed] [Google Scholar]
- 5. Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation 2004: 17: 35–44. [PubMed] [Google Scholar]
- 6. Kahn R, Buse JM, Ferrannini E, et al American Diabetes Association; European Association for the Study of Diabetes. The metabolic syndrome: Time for a critical appraisal: Joint statement from the American Diabetes Association and European Association for the Study of Diabetes. Diabetes Care 2005; 28: 2289–2304. [DOI] [PubMed] [Google Scholar]
- 7. Grundy SM, Cleeman JI, Daniels SR, et al Diagnosis and management of the metabolic syndrome; an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005; 112: 2735–2752. [DOI] [PubMed] [Google Scholar]
- 8. Alberti KG, Zimmet P, Shaw J, and for the IDF Epidemiology Task Force Consensus Group . The metabolic syndrome – a new worldwide definition. Lancet 2005; 366: 1059–1062. [DOI] [PubMed] [Google Scholar]
- 9. The Examination committee of criteria for Metabolic Syndrome . The definition and criteria of metabolic syndrome. J Jpn Soc Int Med 2005; 94: 794–809. [Google Scholar]
- 10. Alberti KG, Eckel RH, Grundy SM, et al Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009; 120: 1640–1645. [DOI] [PubMed] [Google Scholar]
- 11. Alberti KG, Zimmet P, Shaw J. Metabolic syndrome – a new world‐wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med 2006; 23: 469–480. [DOI] [PubMed] [Google Scholar]
- 12. Examination Committee of Criteria for ‘Obesity Disease’ in Japan. Japan Society for the Study of Obesity . New criteria for ‘obesity disease’ in Japan. Circ J 2002; 66: 987–992. [DOI] [PubMed] [Google Scholar]
- 13. Fox CS, Massaro JM, Hoffmann U, et al Abdominal visceral and subcutaneous adipose tissue compartments: Association with metabolic risk factors in Framingham Heart Study. Circulation 2007; 116: 39–48. [DOI] [PubMed] [Google Scholar]
- 14. Neeland IJ, Ayers CR, Rohatgi AK, et al Association of visceral and abdominal subcutaneous adipose tissue with markers of cardiac and metabolic risk in obese adults. Obesity 2013; 21: E439–E447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cornier MA, Despres JP, Davis N, et al Assessing adiposity: A scientific statement from the American Heart Association. Circulation 2011; 124: 1996–2019. [DOI] [PubMed] [Google Scholar]
- 16. Oka R, Kobayashi J, Yagi K, et al Reassessment of the cutoff values of waist circumference and visceral fat area for identifying Japanese subjects at risk for the metabolic syndrome. Diabetes Res Clin Pract 2008; 79: 474–481. [DOI] [PubMed] [Google Scholar]
- 17. Takahara M, Katakami N, Kaneto H, et al Contribution of visceral fat accumulation and adiponectin to the clustering of metabolic abnormalities in a Japanese population. J Atheroscler Thromb 2014; 21: 543–553. [PubMed] [Google Scholar]
- 18. Hiuge‐Shimizu A, Kishida K, Funahashi T, et al Coexistence of visceral fat and multiple risk factor accumulations in strongly associated with coronary artery disease in Japanese (the VACATION‐J study). J Atheroscler Thromb 2012; 19: 657–663. [DOI] [PubMed] [Google Scholar]
- 19. Hiuge‐shimizu A, Kishida K, Funahashi T, et al Reduction of visceral fat correlates with the decrease in the number of obesity‐related cardiovascular risk factors in Japanese with Abdominal Obesity (VACATION‐J Study). J Atheroscler Thromb 2012; 19: 1106–1118. [DOI] [PubMed] [Google Scholar]
- 20. Furukawa K, Katabami T, Nakajima Y, et al Evaluation of whole‐abdominal fat volume by 700‐slice fat area anthropometric indices. Obes Res Clin Pract 2010; 4: e111–e117. [DOI] [PubMed] [Google Scholar]
- 21. Sada Y, Katabami T, Asai S, et al Intrahepatic lipid content is linked to insulin resistance in obese subjects. Obes Res Clin Pract 2011; 5: e129–e136. [DOI] [PubMed] [Google Scholar]
- 22. Yoshizumi T, Nakamura T, Yamane M, et al Abdominal fat: Standardized technique for measurement at CT. Radiology 1999; 211: 283–286. [DOI] [PubMed] [Google Scholar]
- 23. Li G, Chen X, Jang Y, et al Obesity, coronary heart disease risk factors and diabetes in Chinese: An approach to the criteria of obesity in the Chinese population. Obes Rev 2002; 3: 167–172. [DOI] [PubMed] [Google Scholar]
- 24. Zhou BF. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults – study on optimal cut‐off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci 2002; 15: 83–96. [PubMed] [Google Scholar]
- 25. Hara K, Matsushita Y, Hotikoshi M, et al A proposal for the cutoff point of waist circumference for the diagnosis of metabolic syndrome in the Japanese population. Diabetes Care 2006; 29: 1123–1124. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1¦ Optimal cut‐off values, area under the receiver operating characteristic curve, sensitivity and specificity predicting metabolic syndrome.


