Summary
Background
Mortality within the first 6 months after initiating antiretroviral therapy (ART) is common in resource-limited settings and is often due to tuberculosis (TB) among patients with advanced HIV disease. Isoniazid preventive therapy (IPT) is recommended in HIV-infected adults, but sub-clinical TB can be difficult to diagnose. We hypothesized that empiric TB treatment would reduce early mortality compared to IPT in high-burden settings.
Methods
We conducted a multi-country randomized clinical trial comparing empiric TB therapy (Empiric) vs. isoniazid preventive therapy (IPT) in HIV-infected outpatients initiating ART with CD4 counts <50 cells/mm3. Individuals were screened for TB using a symptom screen, locally available diagnostics, and the GeneXpert MTB/RIF assay when available. The primary endpoint was survival (death or unknown status) at 24 weeks post randomization. Kaplan Meier estimates of the endpoint rates across arms were compared by the z-test. Registered at ClinicalTrials.gov (NCT01380080).
Findings
From October 31, 2011 until June 9, 2014, we randomized 850 participants (424 in Empiric arm and 426 in IPT arm); the median CD4 count at baseline was 18 cells/mm3 (IQR: 9, 32). At week 24, each arm had 22 primary endpoints, for rates of 5.2% in each arm (95% CI: 3.5% to 7.8% for Empiric and 3.4% to 7.8% for IPT; absolute risk difference of -0.06% (95% CI: −3.05% to 2.94%). Grade 3 or 4 signs or symptoms occurred in 50 (12%) in the Empiric arm and 46 (11%) in the IPT arm. Grade 3 or 4 laboratory abnormalities occurred in 99 (23%) in the Empiric arm and 97 (23%) in the IPT arm. Incident TB was more common in the Empiric arm (31 vs. 18 events, p=0.01).
Interpretation
Empiric TB therapy did not reduce mortality at 24 weeks in outpatient adults initiating ART with advanced HIV disease. The low mortality rate of the trial supports implementation of systematic TB screening and IPT in outpatients with advanced HIV disease.
Introduction
Introduction and expansion of antiretroviral therapy (ART) programs have saved millions of lives among HIV-infected individuals in resource-limited settings1. Despite these successes, persons with advanced HIV disease continue to present for care and up to 17% of adults die in the initial months after ART initiation2. Risk factors for early mortality after ART initiation include a low CD4 cell count, low body mass index (BMI), and anemia, with those having a CD4<50 cells/mm3 having the highest risk of any individual factor2.
Tuberculosis (TB) is the most common cause of mortality in HIV-infected individuals and both prevalent and incident TB infections are a major contributor to early mortality among patients presenting to outpatient settings to initiate ART3. Up to 70% of patients with TB in sub-Saharan Africa are HIV-infected, and TB incidence rates following ART initiation are high, particularly among those with advanced HIV disease4, 5. Autopsy studies from sub-Saharan Africa, South East Asia and the Americas confirm TB as the primary or contributing cause of mortality in the majority of cases with nearly half of the TB undiagnosed pre-mortem6. Strategies addressing TB in patients at high risk for early mortality across the globe are urgently needed.
Patients with HIV often lack classic symptoms and signs of TB, complicating diagnosis. The World Health Organization (WHO)-endorsed symptom screen for TB, based on cough, fever, weight loss and night sweats, misses two in ten TB cases in HIV-infected individuals7. In resource-limited settings where TB is common, patients with positive symptom screens are usually evaluated with sputum staining for acid fast bacilli (AFB), which has low sensitivity in HIV-infected individuals with low CD4 counts8. Likewise, patients with advanced HIV may have minimal changes on chest radiography. The GeneXpert MTB/RIF assay (Xpert MTB/RIF), has improved sensitivity in sputum9 but availability of this test remains limited10 and implementation of Xpert MTB/RIF alone has not decreased HIV and TB-associated mortality11–13. Limitations of existing diagnostics contribute to major ongoing challenges in diagnosing and treating HIV-associated TB in resource-limited settings.
Expanded use of empiric TB treatment, defined as treatment in absence of microbiologic confirmation of TB disease, has emerged as one potential approach to reduce TB-associated mortality. Currently, the WHO recommends that patients who screen negative for TB be placed on isoniazid preventive therapy (IPT), and empiric TB therapy only be used for seriously ill patients in peripheral settings in whom initial tests are negative14. However, the optimal approach for managing patients at high risk of HIV-associated TB and early mortality after ART initiation is uncertain. Recent studies have provided further evidence indicating that IPT alone may substantially reduce the risk of TB-associated mortality in HIV15, but concerns about tolerability of IPT and promotion of drug-resistance in patients with sub-clinical TB have limited the uptake of this intervention. For patients with advanced immunosuppression, an alternative strategy relevant to high-burden settings would be to empirically treat TB in all severely immunosuppressed patients who are not found to have TB after screening, even if not seriously ill. This approach could decrease early mortality by addressing undiagnosed, untreated TB and, via rifampin, increasing durability of TB preventive therapy as well as treating or preventing severe bacterial infections. The REMEMBER (Reducing Early Mortality and Early Morbidity by Empiric Tuberculosis Treatment Regimens) study, AIDS Clinical Trials Group (ACTG) Study A5274, hypothesized that empiric TB treatment will reduce early mortality compared to IPT among participants with advanced HIV disease presenting for ART initiation in settings where TB is common.
Methods
Study population
We enrolled HIV-infected ART-naïve individuals aged ≥13 years with CD4 counts <50 cells/mm3 who did not have evidence of active TB (as per criteria described below) and who were eligible for either IPT or empiric TB treatment. All 18 sites reported a TB incidence >100/100,000 person years and had ART programs with documented high early mortality rates (>10–20 per 100 person years) among outpatient populations. Inclusion criteria included having liver function tests ≤2.5x the upper limit of normal, a creatinine clearance ≥30mL/min, and a Karnofsky score ≥30 in order to facilitate inclusion of participants with advanced HIV presenting to ART clinics who were able to rapidly initiate both ART and TB treatment or IPT. To decrease the possible influence of HIV or TB drug resistance on outcomes, exclusion criteria included use of single dose nevirapine in the preceding 2 years, receipt of TB treatment or IPT within 96 and 48 weeks prior to study entry, respectively, and a history of household exposure to multidrug resistant (MDR)-TB. Full eligibility criteria are included in the study protocol (supplementary files).
Study sites generally followed local guidelines for ART initiation in their country programs. All 18 sites initiated ART for WHO stage 3 or 4 disease for those with CD4 counts < 350 cells/mm3. For standard of care TB screening, all 18 sites reported using sputum AFB screening and chest radiography, and 5 reported implementation of the Xpert MTB/RIF assay.
Study design
We compared 2 treatment strategies: ART + empiric TB therapy (Empiric arm) vs. ART+ IPT (IPT arm) in an open-label randomized 1:1 trial design. Randomization sequence was generated by a computer at the ACTG Data Management Center. Randomization was balanced by clinical trial unit and stratified according to CD4+ T cell count (<25 vs. ≥25 cells/mm3) and presence of any of the following prognostic factors: reportable hospitalization within the past 30 days, BMI <18.5 kg/m2, or anemia (hemoglobin <8 g/dl). Participants, site personnel, and study statisticians were not masked to group assignment. The open label pragmatic design was chosen to reflect actual field settings where ART would be combined with either Empiric 4 drug therapy or IPT.
Potential participants were referred to study clinics from local ART clinics, many of which were co-located and some of which were fully integrated within the ART program. At the study clinics, potential participants were screened for TB prior to study entry using a symptom screen that included the following: cough ≥2 weeks, any current fever >38°C, hemoptysis, night sweats within the past 2 weeks, unintentional weight loss >10% in the past 30 days, or enlarged axillary or cervical lymph nodes. Any positive screen required further workup per local standard of care. All sites had capacity to perform AFB smear, chest radiograph, ultrasound, mycobacterial culture, and Gene Xpert, however the use of specific tests was left up to the site’s clinicians. Persons who were strongly suspected to have TB, or for whom screening procedures identified confirmed or probable TB were excluded. The study did not collect information on the outcomes of persons excluded from study entry. In response to a June 2013 Data Safety Monitoring Board (DSMB) review, the protocol was modified to require the addition of sputum Xpert MTB/RIF assay testing for all potential participants during screening. Participants with negative symptom screens or positive screens but no microbiologic or presumptive diagnosis of TB were eligible for enrollment in the study.
All participants received efavirenz-containing ART with either study-provided tenofovir/emtricitibine (Truvada®; donated by Gilead) or locally available nucleoside reverse transcriptase inhibitors. Participants in the Empiric arm received self-administered, weight-adjusted fixed-dose combination rifampin/isoniazid/ethambutol/ pyrazinamide for 8 weeks, followed by fixed-dose combination rifampin/isoniazid for 16 weeks, beginning within 7 days after ART initiation. Participants in the IPT arm received 300mg of isoniazid daily for 24 weeks, beginning within 7 days of ART. All participants received pyridoxine. Participants are followed for 96 weeks; results through week 24 are reported here. Participants attended study visits at screening, enrollment, and weeks 1, 2, 4, 8, 12, 16, 20, and 24. Signs and symptoms, ART modifications, concomitant medications, and clinical events as defined by AIDS Clinical Trials Group (ACTG) Appendix 60 were collected at each visit. Blood was collected for CD4 and HIV-1 RNA at study entry, weeks 4 and 24, and blood for safety laboratories (liver function, hematology, and renal function) was collected at all visits except week 1. A sputum sample was collected and stored at study entry. After the DSMB review requiring real time Xpert MTB/RIF testing, the available stored samples collected prior to this requirement were retrospectively tested using the Xpert MTB/RIF assay. Participants in both arms who developed signs or symptoms of TB had TB investigations performed as per locally available diagnostics, which included sputum culture and, for those with positive cultures, drug susceptibility testing. Those with drug-sensitive TB received weight-adjusted fixed-dose combination rifampin/isoniazid/ethambutol/ pyrazinamide for 8 weeks, followed by fixed-dose combination rifampin/isoniazid for 16 weeks. Any participant with drug resistant TB was treated according to local standard of care. In the event of missed visits, participants were traced by phone calls and home visits if they or their contacts could not be reached by phone. Those who could not be contacted after this process were defined as lost to follow-up.
Study oversight
The study was funded by the National Institutes of Allergy and Infectious Diseases (NIAID) through the ACTG. An NIAID international DSMB monitored the study semi-annually. Sites obtained approval from local ethics committees. Participants had to provide written informed consent.
Statistical analysis
The primary endpoint was survival (death or unknown vital status) 24 weeks post randomization. The target sample size of 836 was selected to detect a 7.5% difference in the primary event probabilities (15% for IPT and 7.5% for Empiric) between arms based on a two-sided test of binomial probabilities with 90% power, 5% alpha level, and 5% inflation of the estimated sample size for interim analyses. For the primary endpoint analysis, an intent-to-treat (ITT) approach was used with all randomized participants regardless of receiving treatment, except for one participant who was enrolled inadvertently due to an incorrect CD4 count at screening (n=850). The final analysis was conducted with a significance level of 5% which does not account for the number of interim analyses since the original sample size was inflated by 5% for the interim analyses. On and off study deaths and participants with unknown survival status were included as events in the primary endpoint analysis. Kaplan Meier estimates of the endpoint probabilities across arms were compared by the z-test. Participants who withdrew consent (n=8) were censored at the time of their last visit. Secondary endpoints included death and AIDS progression, confirmed or probable TB, grade 3 or 4 signs/symptoms, and grade 3 or 4 lab abnormalities. AIDS progression was defined as any new WHO stage 3 or 4 event occurring greater than 2 weeks after study entry. Incident TB was defined as any diagnosis occurring after entry. Similar methods were used to compare the secondary endpoint probabilities of death or AIDS progression, and confirmed or probable TB between arms. Time to any primary and secondary endpoint was compared by the log-rank test. For the supplemental analyses, a per-protocol approach was used with all participants who completed the 24 week assessments (n=842). The Cochran-Mantel-Haenszel test was used to compare the primary endpoint probabilities between arms after stratification by randomization phase (before and after implementation of screening Xpert MTB/RIF testing) and by the prognostic stratification factors described above. Additionally, we evaluated the impact of excluding any participants with a positive enrollment sputum Xpert MTB/RIF sample as determined by retrospective testing. For the safety analysis, all randomized participants were included (n=851) and Chi-square test was used to compare the probabilities of safety and tolerability of ART and TB treatment. Safety outcomes included all signs, symptoms, and laboratory abnormalities meeting Grade 3 or 4 criteria per the Division of AIDS toxicity table. All causes of death, AIDS progression events, and TB cases were externally verified. All analyses were conducted in SAS Version 9.4. This study is registered in ClincalTrial.gov as trial number NCT01380080.
Results
Patient characteristics
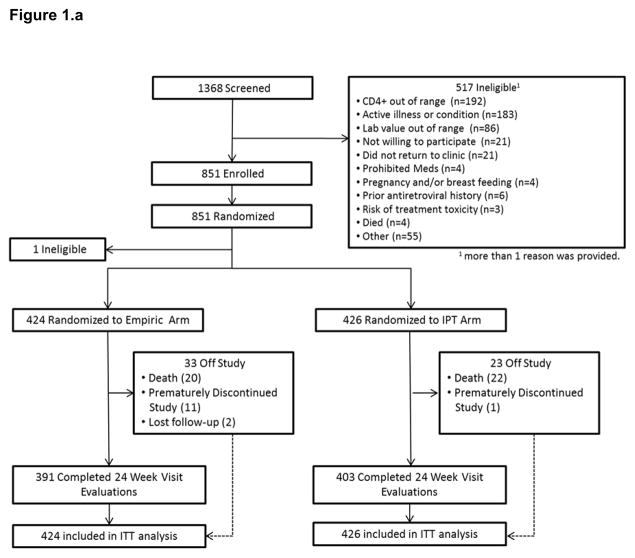
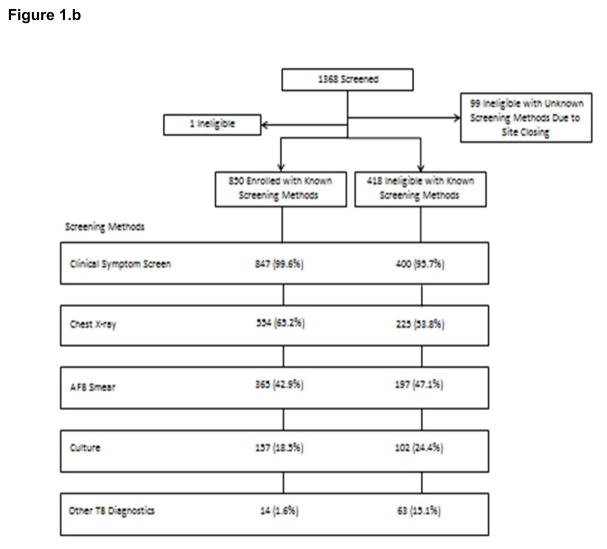
From October 31, 2011 until June 9, 2014, a total of 1368 candidates were screened and 851 (62%) were randomized (Figure 1.a.). One participant who was randomized to the IPT arm was later found to be ineligible and was discontinued at day 10 due to having a screening CD4 count value ≥ 50 cells/mm3. Participants were enrolled at 18 sites in 10 countries (Malawi, South Africa, Haiti, Kenya, Zambia, India, Brazil, Zimbabwe, Peru, and Uganda), with 77% (n=658) of the enrollment occurring in Sub-Saharan Africa. The most common screening failure reason was having a CD4 count value ≥ 50 cells/mm3 (n=192; 33%), followed by presence of suspected or confirmed TB (n=183; 32%) and having laboratory values out of range (n=86; 15%). Patients who were not enrolled were slightly more likely to have AFB smear, ultrasound, and culture performed at screening compared to those who were enrolled (Figure 1.b.). Among screening failures, the number excluded due to TB suspicion varied across sites 0% in Eldoret (Kenya) and Rio de Janeiro (Brazil) to 56% (n=10) in Port-au-Prince (Haiti). Overall, 10/18 sites excluded >30% of screen failures due to confirmed or probable TB. Among participants screened for the study, 98% (n=1247) had protocol mandated symptom screening, chest radiograph was performed in 61% (n=779), sputum AFB smear in 44% (n=562), culture in 20% (n=259), and other diagnostics in 6% (n=77). Of those screened, 26 patients were excluded because of a positive Xpert MTB/RIF assay. Among those enrolled, approximately 85% could produce sputum at baseline.
Figure 1.
Figure 1.a Consort Diagram
Figure 1.b Screening Methods for Enrolled and Ineligible Participants
Baseline characteristics of 850 enrolled participants (424 in Empiric arm and 426 in IPT arm) were similar across arms (Table 1). Overall, 53% (n=450) were male, 90% (n=768) were black; median (IQR, range) age was 36 (30–42, 18–70) years. Participants had highly advanced HIV disease with a median (IQR) CD4 count of 18 cells/mm3 (9–32). Forty-two (5%) had reportable hospitalization within 30 days before study entry, 248 (29%) had a BMI less than 18.5 kg/m2, and 44 (5%) had a hemoglobin less than 8 g/dL. Of 448 (53%) who were enrolled prior to required sputum Xpert MTB/RIF assay screening, 379 (45%) had retrospective testing using Xpert MTB/RIF and 6 (2%) were positive, 3 in each arm. Among the 850 enrolled participants, 502 (59%) had at least one positive result on symptom screen prior to enrollment in the trial, with unintentional weight loss being the most commonly reported symptom (among 415, or 49%), followed by cough > 2 weeks (reported by 139, or 16%) (Table 1).
Table 1.
Baseline characteristics of study participants
| Characteristic | Empiric (n=424) | IPT (n=426) | All Participants (n=850) |
|---|---|---|---|
| Male | 224 (53%) | 226 (53%) | 450 (53%) |
| Race | |||
| Black African or Black of African Origin | 380 (90%) | 388 (91%) | 768 (90%) |
| Others | 44 (10%) | 38 (9%) | 82 (10%) |
| Age (years) | 36 (30–42) | 35 (30–42) | 36 (30–42) |
| Country | |||
| Malawi | 95 (22%) | 98 (23%) | 193 (23%) |
| South Africa | 86 (20%) | 90 (21%) | 176 (21%) |
| Kenya | 77 (18%) | 75 (18%) | 152 (18%) |
| Haiti | 53 (13%) | 56 (13%) | 109 (13%) |
| Zimbabwe | 25 (6%) | 27 (6%) | 52 (6%) |
| Uganda | 25 (6%) | 24 (6%) | 49 (6%) |
| Peru | 20 (5%) | 19 (5%) | 39 (5%) |
| Zambia | 17 (4%) | 19 (5%) | 36 (4%) |
| India | 17 (4%) | 12 (3%) | 29 (3%) |
| Brazil | 9 (2%) | 6 (1%) | 15 (2%) |
| CD4 count (cells/mm3) | 18 (9–31) | 19 (9–33) | 18 (9–32) |
| HIV-1 RNA log10(cp/mL) | 5.4 (5.0–5.7) | 5.3 (4.9–5.7) | 5.3 (4.9–5.7) |
| Stratification Factors | |||
| < 25 CD4 count cells/mm3 | 253 (60%) | 257 (60%) | 510 (60%) |
| Hospitalized within the past 30 days | 19 (4%) | 23 (5%) | 42 (5%) |
| < 18.5 kg/m2 Body Mass Index | 120 (28%) | 128 (30%) | 248 (29%) |
| Anemia (hemoglobin <8 g/dl) | 28 (7%) | 16 (4%) | 44 (5%) |
| WHO stages * | |||
| No stages 3 or 4 event | 305 (72%) | 309 (73%) | 614 (72%) |
| Stage 3 | 85 (20%) | 77 (18%) | 162 (19%) |
| Stage 4 | 34 (8%) | 40 (9%) | 74 (9%) |
| Clinical Symptoms | |||
| Cough lasting for 2 or more weeks | 66 (16%) | 73 (17%) | 139 (16%) |
| Fever ≥38° Celsius | 27 (6%) | 22 (5%) | 49 (6%) |
| Hemoptysis in the past 2 weeks | 0 (0%) | 1 (<1%) | 1 (<1%) |
| Night sweats in the past 2 weeks | 32 (8%) | 43 (10%) | 75 (9%) |
| Unintentional weight loss in the past 30 days | 195 (46%) | 220 (52%) | 415 (49%) |
| Enlarged axillary or cervical lymph nodes | 38 (9%) | 43 (10%) | 81 (10%) |
| At least one TB symptom reported | 237 (56%) | 265 (62%) | 502 (59%) |
Data are n(%) or median (IQR).
Number of participants who had at least one event at baseline.
Primary Outcome
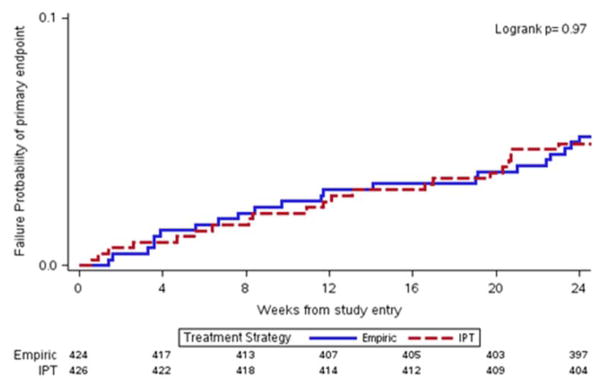
At week 24, both arms had 22 primary events resulting in the same primary endpoint rate of 5.2% (95% CI: 3.5% to 7.8% for Empiric arm and 3.4% to 7.8% for IPT arm; p-value = 0.97) and resulting in an absolute risk difference of −0.06% (95% CI: −3.05% to 2.94%). All primary endpoints were deaths except for 2 unknown vital status events in the Empiric arm. The death rates between the study arms remained not significantly different after treating the two participants as censored cases in sensitivity analysis (n=20, 4.8% for the Empiric arm and n=22, 5.2% for the IPT arm; p-value = 0.78). Among the 10 countries with at least one site, eight reported at least one death and the primary endpoint rates by arm were generally similar across countries. While mortality was higher among those with a CD4 count <25 cells/mm3 and those with poor prognostic factors, the event rates were similar across arms for the stratification factors as well as before and after implementation of sputum Xpert MTB/RIF testing or after excluding participants with retrospectively identified positive sputum Xpert MTB/RIF tests (Table 2). There was no difference in time to the primary event across arms (Figure 2.a).
Table 2.
Proportions of death or unknown survival status at week 24
| Study Population and Stratification Factors | No. of Participants | No. (%) of Death or Unknown Survival Status | 95% CI for Estimated Difference in Endpoint Rates (KM Approach) | P Value | |
|---|---|---|---|---|---|
| Empiric | IPT | ||||
| All Participants | 850 | 22 (5.2%) | 22 (5.2%) | −3.05, 2.94 | 0.97 |
| All Participants excluding 6 | 844 | 21 (5.0%) | 21 (5.0%) | −3.00, 2.89 | 0.97 |
| Xpert MTB/RIF Positive at Baseline | |||||
| Stratification Factors1 | |||||
| Pre-Mandated Sputum Xpert MTB/RIF | 444 | 13 (5.8%) | 13 (5.9%) | NA | 0.96 |
| Post-Mandated Sputum Xpert MTB/RIF | 398 | 9 (4.6%) | 9 (4.4%) | ||
| CD4 < 25 cells/mm3 | 504 | 17 (6.9%) | 17 (6.6%) | NA | 0.92 |
| CD4 ≥25 cells/mm3 | 338 | 5 (2.9%) | 5 (3.0%) | ||
| Poor Prognostic Factor 2 | 284 | 13 (9.4%) | 8 (5.5%) | NA | 0.94 |
| No Poor Prognostic Factor | 558 | 9 (3.2%) | 14 (5.0%) | ||
A total of 842 participants were included as 8 participants who withdrew consent at or before week 24 were excluded.
Poor prognostic factor was defined as presence of at least one of the following: reportable hospitalization within the past 30 days, body mass index [BMI] <18.5, or anemia [hemoglobin <8 g/dl]
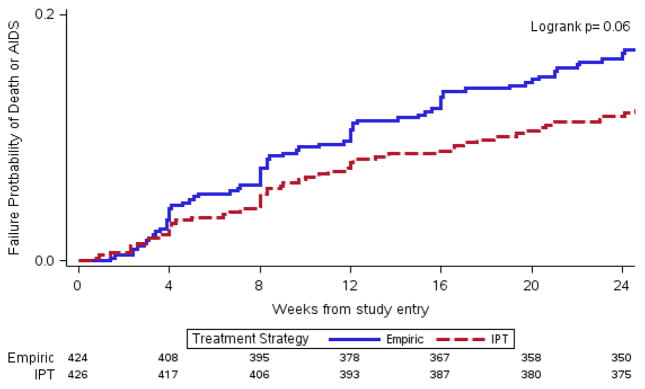
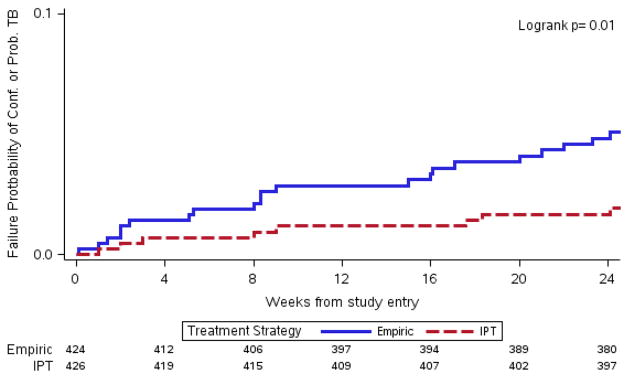
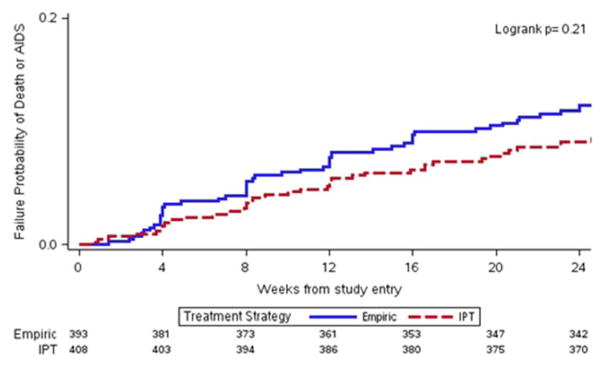
Figure 2. Kaplan Meier plots for time to primary and secondary endpoint.
a) Time to primary endpoint (death or unknown status) by treatment strategy
b) Time to death or AIDS progression by treatment strategy
c) Time to confirmed or probable Tuberculosis by treatment strategy
d) Time to death or AIDS progression (Excluding confirmed and probable TB) by treatment strategy
Causes of death included HIV-associated infections (17 in Empiric arm, 11 in IPT arm), non-HIV diagnoses (5 in IPT arm), renal toxicity attributed to tenofovir (1 in IPT arm), unknown in 6 cases (2 in Empiric arm, 4 in IPT arm), and motor vehicle accident (1 in the IPT arm) (supplemental Table 1). Cryptococcal meningitis (4), Kaposi’s sarcoma (3), and extrapulmonary TB (3) were the most common HIV-associated causes of death.
Secondary Outcomes
By week 24, the Empiric arm had a higher rate of death or AIDS progression (17.1% (n=72) vs. 12.5% (n=53); p=0.06) and the time to death or AIDS progression was more rapid in the Empiric arm (Figure 2.b). The result was due primarily to an increased incidence of TB (31 and 18 participants in the Empiric and IPT arms, respectively p=0.01), including both pulmonary and extrapulmonary disease (supplemental Table 2). The time to confirmed or probable TB in the Empiric arm was also more rapid (Figure 2.c). There was no difference in time to death or AIDS progression if confirmed or probable TB was excluded (Figure 2.d). Self-reported adherence to study medications was similar across arms at all weeks except the Empiric arm had lower reported 100% adherence to TB drugs at week 8 (88% (n=360) vs. 93% (n=383) , p=0.03). The Empiric arm also experienced more premature discontinuations of TB drugs by week 24 (47 Empiric vs. 18 IPT discontinuations). A viral load <400 copies/mL was achieved by 84% (n=309) and 85% (n=322) of participants in the Empiric and IPT arms, respectively. The median CD4 change at 24 weeks was 96 (IQR: 55–147) in the Empiric arm and 102 (IQR: 60–159) in the IPT arm (p=0.25 by Wilcoxon test).
Safety measures were also similar across arms. Grade 3 or 4 signs or symptoms occurred in 50 (12%) in the Empiric arm and 46 (11%) in the IPT arm. Grade 3 or 4 laboratory abnormalities occurred in 23% (n=99 and 97 for Empiric and IPT, respectively) in both arms (Table 4). Hematology abnormalities were most common, occurring in 15% (n=124) overall (15% (n=65) in Empiric arm, 14% (n=59) in IPT arm) followed by hepatic abnormalities, occurring in 6% (n=55) overall (6% (n=26 ) in Empiric arm, 7% (n=29) in IPT arm). Of the 49 incident cases of TB, there was no evidence of differential increased drug resistance by study arm. Drug resistance to at least one TB drug occurred in 6 participants, 3 in each arm. In the Empiric arm, the resistance profiles of the 3 participants were Isoniazid/ethambutol, isoniazid/rifampin/ethambutol, and Streptomycin /rifampin/isoniazid/ethambutol while in the IPT arm, the resistance profiles of the 3 participants were isoniazid only, Streptomycin /rifampin/isoniazid/ethambutol, and Streptomycin /rifampin/isoniazid/ethambutol/pyrazinamide. The participants switched to appropriate TB treatment per local guidelines after the resistance was identified.
Despite potential benefits of rifampin on severe bacterial infections, the incidence of such infections did not differ significantly by arm [37 (9%) for the Empiric arm and 52 (12%) for the IPT arm; p-value = 0.095; Supplemental Table 2)]. TB-immune reconstitution inflammatory syndrome (IRIS) was adjudicated using ACTG definitions by the external endpoint panel. A total of 19 TB-IRIS cases (2%) were reported (9 in the Empiric arm and 10 in the IPT arm). Of these 19 cases, 13 were confirmed ART ‘unmasking’ TB-associated TB-IRIS (6 in the Empiric arm and 7 in the IPT arm), and 5 were probable ART ‘unmasking’ TB-associated TB-IRIS (2 in the Empiric arm and 3 in the IPT arm), and 1 was probable paradoxical TB-associated TB-IRIS (in the Empiric arm).
Discussion
In this large, multi-site randomized clinical trial, empiric TB therapy did not reduce early mortality compared to administration of IPT in individuals with highly advanced HIV disease initiating ART in outpatient settings where TB incidence is high. Furthermore, despite enrolling participants with extremely low CD4 cell counts, we observed a mortality rate that was substantially lower than that observed in previous studies from similar settings2. We also observed an increased risk of AIDS progression and specifically TB in the Empiric arm. Taken together, the results support the use of standardized TB screening procedures in patients with advanced HIV disease presenting for ART initiation and indicate that, in those without a diagnosis of TB after screening, there is no added benefit of empiric TB therapy compared to provision of IPT alone. Indeed, this study effectively demonstrates that the combination of IPT with ART is safe when used to prevent TB and early mortality in very advanced HIV disease.
We had hypothesized that empiric TB therapy would more effectively treat those with subclinical active TB and thereby reduce early mortality. Numerous studies done pre- and post-mortem have identified TB as the major cause of mortality in those with advanced HIV disease who are initiating ART in sub-Saharan Africa, India, Haiti and parts of South America, where our study took place2, 6. An additional hypothesized effect of empiric TB therapy relates to a potentially more durable TB preventive impact of isoniazid and rifampin compared to isoniazid alone16. Lastly, by virtue of the use of rifampin, empiric TB treatment could also plausibly provide benefit in terms of prevention or early treatment of severe bacterial infections. However, we found a definitive lack of benefit of empiric therapy on mortality outcomes. This finding likely resulted in part from the exclusion of many TB cases by the study’s systematic TB screening approach, as one-third of screened participants were excluded for suspected active TB. Furthermore, although the median CD4 count of the study population was extremely low, systematic non-referral of sicker patients or those with very high TB suspicion to the study may have resulted in exclusion of candidates with poor prognosis. Interestingly, our study still encountered substantial incident TB but we also observed that fewer participants diagnosed with TB after ART initiation died during 24 weeks of follow-up across both arms. This contrasts sharply with the strong association previously observed between prevalent and incident TB after ART initiation and early mortality among HIV-infected outpatients initiating ART3, 17. This lower mortality is notable, given the highly advanced HIV disease of the cohort, but provides solid evidence that empiric TB therapy does not provide a mortality benefit over IPT even among outpatients with profound immunosuppression who remain without a TB diagnosis after screening.
Other observational studies and clinical trials have documented early mortality rates of 15% or higher2, 18, 19 which is substantially greater than the 5% documented in this study. In addition to possible effects of screening and referral patterns mentioned above, this low mortality rate may also relate to the fact that all participants received INH, a rapidly bactericidal agent20 which can reduce the risk of TB in HIV-infected patients21–23. Although INH’s effect on survival is uncertain in patients with severe HIV immunosuppression, two observational studies from South Africa and a cluster-randomized trial in Brazil found that IPT reduced early mortality and incidence of a combined endpoint of TB and mortality in HIV-infected individuals24–26. More recently, the TEMPRANO study, a randomized, 2 x 2 factorial designed clinical trial evaluating ART and IPT in adults with median baseline CD4 count of approximately 460 cells/mmm3, found that IPT resulted in a 35% reduction in severe HIV morbidity15. To date, no other trial including IPT and ART initiation among HIV-infected individuals has examined a similarly large population of individuals with highly advanced HIV disease. This distinguishing characteristic of the A5274 trial is important, because although IPT is recommended by WHO for HIV-infected adults, its uptake and implementation has been very low due in part to concerns about excluding active TB in advanced HIV disease, and associated fears of generating drug resistance. Deferring IPT for some months among advanced patients has been proposed to address any potential resistance risk associated with early incident TB27. However, while the number of incident TB cases in this study limits formal analyses of isoniazid resistance, the prescribed 6-month course of IPT was well tolerated and discontinuations were rare when initiated near the time of ART initiation. Thus, while our study did not include a placebo arm, these results indicate that IPT plus ART can be safely implemented in patients with highly advanced HIV disease who are not diagnosed with TB after screening. This is in keeping with the WHO’s latest guidance to provide IPT regardless of CD4 count for all HIV-infected adults and adolescents14. Repeated symptom screening for TB at follow-up visits after IPT initiation, also recommended by WHO14, should also be implemented to detect incident TB as early as possible on ART.
The increased risk of AIDS progression and specifically TB seen in the Empiric arm was unexpected. Provision of 4-drug TB therapy to patients without a known TB diagnosis plausibly could lead to adverse events and reduced adherence to anti-tubercular therapy or ART, either of which could result in an increased risk of AIDS progression. Although self-reported adherence to TB therapy and ART, as well as virologic and immunologic responses to ART, were similar across arms for all visits except week 8, premature TB drug discontinuation rates were more common in the Empiric arm. A previous study has suggested that the combination of isoniazid/rifampin may have more potent and durable protection against the development of TB and death than isoniazid alone, but multi-drug regimens for treatment of latent TB infection are also associated with increased risk of discontinuation21. Another potential explanation for the increased rate of TB in the empiric arm is diagnostic suspicion bias, where knowledge of TB treatment status led to more aggressive use of TB diagnostics or more liberal TB diagnosis in participants randomized to the Empiric arm. Unmasking TB-IRIS was also uncommon in both arms and does not appear to explain this difference in incident TB. Nonetheless, given the lack of clinical benefit of the empiric therapy, the finding of potential harm should be carefully considered by providers when evaluating similar patient populations.
Notably our study population of adults with advanced HIV (CD4<50 cells/mm3) disease continues to be encountered in HIV programs globally despite the evolving guidance to start ART at higher CD4 cell counts. Currently, the median CD4 count in ART programs in low- and middle-income settings remains below 200 cells/mm3, 28. This low CD4 population is the group at highest risk of developing and dying from TB. By focusing on individuals with advanced HIV disease, our study provides valuable evidence that systematic screening for TB using standard measures that may or may not include Gene Xpert may enable safe and effective initiation of IPT and ART together in settings with a high burden of HIV and TB.
Our study has some limitations. Study treatment was not blinded to providers or participants such that knowledge of study arm could both influence patient acceptance of a multi-drug combination treatment or providers’ diagnostic suspicion for TB. However, the unblinded approach enabled a pragmatic assessment of how this treatment strategy might work in non-trial settings, where participants without TB after screening would be asked to initiate four-drug TB therapy. The conduct of the study in multiple sites where early mortality rates are high and TB is endemic is a major strength, but the results may not be generalizable to settings where systematic TB screening is not performed or where limited resources prevent close follow-up and early TB diagnosis after ART initiation. In addition, the results from this study among outpatients initiating ART may be not be generalizable to sicker inpatient populations with higher mortality rates, where the prevalence of TB at autopsy has approached 50%6. However, randomized trials of empiric TB therapy in highly advanced patients in inpatient settings would address a different research question, and may have different concerns regarding equipoise. Another limitation was that we did not collect data on all eligible patients who could have potentially enrolled but who were not referred to the trial, limiting our ability to place this strategy in a broader context of care. Nonetheless, similarly low mortality rates may be achievable in routine care settings, given that the study’s screening methods and follow-up schedule were based largely on WHO and local treatment guidelines14. Importantly, while many settings may not have universal access to the Xpert MTB/RIF assay, mortality rates in this study were similar before and after mandatory sputum Xpert MTB/RIF testing at screening was implemented and after excluding TB cases identified retrospectively using the Xpert MTB/RIF assay. This result is consistent with data indicating that the use of the Xpert MTB/RIF assay may not reduce mortality in patients with HIV11–13. Furthermore, the rationale for empiric TB therapy is based primarily on high rates of undiagnosed TB in patients presenting for care, which in part depends upon the availability of accurate TB diagnostics and assessments performed prior to ART initiation, along the entire cascade of HIV care. Novel TB diagnostics such as the urinary lipoarabinomannan (LAM) assay, which has approximately 67% sensitivity in patients with CD4 counts <50 cells/mm3 29, has recently been shown to reduce mortality as well as the use of empiric TB treatment among hospitalized patients when used as an additional diagnostic test30 and may decrease the rationale for empiric TB therapy.
In summary, our study found that empiric TB treatment did not reduce early mortality in outpatients with advanced HIV disease compared to provision of IPT. Among patients with advanced HIV disease in settings where TB incidence is high, systematic TB screening prior to ART initiation and implementation of IPT near the time of ART initiation should be urgently pursued.
Supplementary Material
Table 3.
New laboratory events of Grade 3 or higher by week 24
| Empiric (N=424) | IPT (N=426) | All Participants (N=851) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Grade | Grade | Grade | |||||||
| Laboratory Event | 3 | 4 | All | 3 | 4 | All | 3 | 4 | All |
| Any Chemistry | 21 (5 %) | 5 (1 %) | 26 (6%) | 20 (5 %) | 9 (2%) | 29 (7 %) | 41 (5 %) | 14 (2 %) | 55 (6 %) |
| Any Chemistry, Gases | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 |
| Hydrogen Ion Concentration | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 |
| Any Chemistry, General | 20 | 5 | 25 | 20 | 9 | 29 | 40 | 14 | 54 |
| Albumin | 11 | 0 | 11 | 6 | 0 | 6 | 17 | 0 | 17 |
| Alkaline Phosphatase | 1 | 0 | 1 | 10 | 1 | 11 | 11 | 1 | 12 |
| Bicarbonate | 2 | 0 | 2 | 0 | 0 | 0 | 2 | 0 | 2 |
| Calcium | 1 | 0 | 1 | 2 | 0 | 2 | 3 | 0 | 3 |
| Carbon Dioxide | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 |
| Sodium | 10 | 5 | 15 | 9 | 7 | 16 | 19 | 12 | 31 |
| Any Endocrine | 1 (0 %) | 0 (0 %) | 1 (0 %) | 0 (0 %) | 0 (0 %) | 0 (0 %) | 1 (0 %) | 0 (0 %) | 1 (0 %) |
| Any Endocrine, General | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 |
| Uric Acid | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 |
| Any Hematology | 38 (9 %) | 27 (6 %) | 65 (15 %) | 46 (11 %) | 13 (3 %) | 59 (14 %) | 84 (10 %) | 40 (5 %) | 124 (15 %) |
| Any Hematology, Coagulation | 0 | 2 | 2 | 3 | 1 | 4 | 3 | 3 | 6 |
| Platelets | 0 | 2 | 2 | 3 | 1 | 4 | 3 | 3 | 6 |
| Any Hematology, RBC | 12 | 9 | 21 | 20 | 4 | 24 | 32 | 13 | 45 |
| Hemoglobin | 12 | 9 | 21 | 20 | 4 | 24 | 32 | 13 | 45 |
| Any Hematology, WBC/Differential | 31 | 18 | 49 | 28 | 9 | 37 | 59 | 27 | 86 |
| Absolute Neutrophil Count | 33 | 16 | 49 | 26 | 9 | 35 | 59 | 25 | 84 |
| White Blood Cells | 6 | 2 | 8 | 4 | 1 | 5 | 10 | 3 | 13 |
| Any Liver/Hepatic | 17 (4 %) | 9 (2 %) | 26 (6 %) | 18 (4 %) | 11 (3 %) | 29 (7 %) | 35 (4 %) | 20 (2 %) | 55 (6 %) |
| SGOT | 16 | 4 | 20 | 16 | 8 | 24 | 32 | 12 | 44 |
| SGPT | 7 | 6 | 13 | 14 | 6 | 20 | 21 | 12 | 33 |
| Total Bilirubin | 4 | 2 | 6 | 0 | 3 | 3 | 4 | 5 | 9 |
| Any Renal | 2 (0 %) | 1 (0 %) | 3 (1 %) | 3 (1 %) | 2 (0 %) | 5 (1 %) | 5 (1 %) | 3 (0 %) | 8 (1 %) |
| Creatinine | 2 | 1 | 3 | 3 | 2 | 5 | 5 | 3 | 8 |
| ANY EVENT | 59 (14 %) | 40 (9 %) | 99 (23 %) | 66 (15 %) | 31 (7 %) | 97 (23 %) | 125 (15 %) | 71 (8 %) | 196 (23 %) |
Data are n (%).
Research in Context.
Evidence before this study
We searched PubMed for articles published up to February 9th, 2016, in any language, that used a randomized trial design to test the hypothesis that empirically treating HIV-infected individuals with TB treatment who did not have clinical or microbiologic evidence of TB disease would reduce early mortality after antiretroviral therapy (ART) initiation using the search terms: “HIV-1”, “tuberculosis”, “mortality”, “antiretroviral therapy”, “empiric therapy”, and “randomized trial”. No published randomized trials of empiric TB therapy were identified. Management of HIV and TB co-infection is a longstanding challenge with respect to morbidity, mortality and disease prevention and control programs. A major issue relates to the complexity of adequately detecting TB in patients with advanced HIV disease who are presenting for antiretroviral therapy (ART) initiation. These patients are at very high risk of TB-associated morbidity and mortality but tests commonly used for TB diagnosis in resource-limited settings, including sputum staining for acid-fast bacilli (AFB), have low sensitivity in these individuals. Furthermore, autopsy studies reveal that TB is the major cause of HIV-associated mortality in these settings. Thus, high rates of mortality within ART programs in resource-limited settings, particularly among those with advanced HIV disease, have been largely attributed to under-diagnosed TB. Strategies to reduce mortality in this vulnerable population are urgently needed.
WHO guidelines currently advocate use of symptom screening and IPT for 6 to 36 months in HIV-infected individuals in whom TB is not found after screening. However, IPT is poorly implemented in most settings due in part to data showing that patients with HIV/TB may have minimal symptoms, which could result in treating patients with sub-clinical TB with a single drug. Additionally, while the WHO recommends the Cepheid GeneXpert MTB/RIF (Xpert MTB/RIF) assay as a diagnostic tool to improve identification of TB and TB drug resistance in HIV-associated TB, availability remains limited and implementation of the test has not been associated with reduced mortality in randomized trials to date. Empiric TB treatment, based on clinical symptoms without microbiologic confirmation in those at high risk of TB and death, is an alternative approach to managing these patients and has been recommended for study by the WHO. At the time of study inception, however, no randomized studies had evaluated this strategy for reducing early ART mortality among HIV-infected outpatients presenting for ART initiation.
Three clinical trials evaluating empiric TB therapy have been implemented and are ongoing. These include 1) the Systematic Empirical vs. Test-guided Anti-TB Treatment Impact in Severely Immunosuppressed HIV-infected Adults Initiating ART With CD4 Cell Counts <100/mm3 (STATIS; NCT020577); 2) the TB Fast Track Study (ISRCTN35344604) and 3) ACTG A5274, Reducing Early Mortality and Early Morbidity by Empiric Tuberculosis Treatment (REMEMBER), of which the 24-week results are presented here. While the design of each of these studies is different, all include HIV-infected populations at high risk for early mortality and use of empiric TB treatment. The REMEMBER study addresses the question of whether outpatients with advanced HIV disease who are not diagnosed with TB after screening using existing methodologies should be empirically treated for TB or started on IPT as recommended by WHO. A5274/REMEMBER is the only randomized empiric TB treatment trial that includes an IPT arm.
Added value of this study
REMEMBER is the first completed clinical trial that addresses whether outpatients with advanced HIV disease living in settings with a high burden of TB who screen negative for TB should initiate IPT or be treated empirically for TB. The study was performed at 18 diverse sites in 10 countries that likely reflect conditions encountered by clinicians attempting to diagnose and treat TB in patients with advanced HIV disease in resource-limited settings. We found no beneficial effect of empiric treatment on mortality. Overall, the mortality rate in the study was lower than what ART programs have reported in observational studies, likely reflecting the clinical trial care setting. There was a suggestion of possible harm in the empiric arm with respect to incident TB and HIV disease progression. IPT was safe and well-tolerated.
Implications of all the available evidence
In settings where routine symptom screening is conducted among outpatients presenting to initiate ART, diagnostics are accessible, and close follow-up is possible, there is no benefit to empiric TB treatment over the current WHO recommendation of the use of IPT. Additionally, this trial demonstrates that IPT can be safely given to HIV-infected individuals with advanced disease. The results strongly suggest that ART programs should enhance routine TB symptom screening and implementation of IPT, even for individuals with low CD4 counts.
Acknowledgments
Presented in part at the 8th IAS conference on HIV Pathogenesis Treatment and prevention Conference, Vancouver Canada, July 18–22, 2015. Research reported in this publication was supported by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under Award Number UM1 AI068634, UM1 AI068636 and UM1 AI106701. Dr. Bao’s effort was funded by the National Institute of Allergy and Infectious Diseases, National Institutes of Health, Department of Health and Human Services (contract no. HH-SN272200800014C).
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Pharmaceutical support was provided by Gilead Sciences but Gilead had no influence in the study design or the analysis of the data. Disclosure forms provided by the authors are available with the full text of this article.
Footnotes
Author Contributions
Mina C. Hosseinipour: literature search, study design, participant recruitment, data collection, data interpretation, manuscript drafting, manuscript revision and intellectual contribution
Gregory P. Bisson: literature search, study design, data collection, data interpretation, manuscript drafting, manuscript revision and intellectual contribution
Sachiko Miyahara: figures, data analysis, data interpretation, manuscript drafting, manuscript revision and intellectual contribution
Xin Sun: figures, data analysis, data interpretation, manuscript drafting, manuscript revision and intellectual contribution
Agnes Moses: participant recruitment, data collection, data interpretation, manuscript revision and intellectual contribution
Cynthia. Riviere, participant recruitment, data collection, data interpretation, manuscript revision and intellectual contribution
F.K. Kirui, participant recruitment, data collection, data interpretation, manuscript revision and intellectual contribution
Sharla. Badal-Faesen, participant recruitment, data collection, data interpretation, manuscript revision and intellectual contribution
David. Lagat, participant recruitment, data collection, data interpretation, manuscript revision and intellectual contribution
Mulinda. Nyirenda, participant recruitment, data collection, data interpretation, manuscript revision and intellectual contribution
K. Naidoo, participant recruitment, data collection, data interpretation, manuscript revision and intellectual contribution
James. Hakim, participant recruitment, data collection, data interpretation, manuscript revision and intellectual contribution
Peter. Mugyenyi, participant recruitment, data collection, data interpretation, manuscript revision and intellectual contribution
German. Henostroza, participant recruitment, data collection, data interpretation, manuscript revision and intellectual contribution
P.D. Leger, participant recruitment, data collection, data interpretation, manuscript revision and intellectual contribution
Javier.R. Lama, participant recruitment, data collection, data interpretation, manuscript revision and intellectual contribution
Lerato. Mohapi, participant recruitment, data collection, data interpretation, manuscript revision and intellectual contribution
Jorge. Alave, participant recruitment, data collection, data interpretation, manuscript revision and intellectual contribution,
V. Mave, participant recruitment, data collection, data interpretation, manuscript revision and intellectual contribution
Valdilea.G. Veloso: participant recruitment, data collection, data interpretation, manuscript revision and intellectual contribution
Sandy. Pillay: participant recruitment, data collection, data interpretation, manuscript revision and intellectual contribution
Nagalingeswaran Kumarasamy: participant recruitment, data collection, data interpretation, manuscript revision and intellectual contribution
Jing. Bao: study design, data interpretation, manuscript revision and intellectual contribution
Lynne Jones: data management, manuscript revision and intellectual contribution
Evelyn. Hogg: study design, data interpretation, manuscript revision and intellectual contribution
Andrew Zolopa: literature search, study design, data interpretation, manuscript drafting, manuscript revision and intellectual contribution
Johnstone Kumwenda: literature search, study design, data interpretation, manuscript drafting, manuscript revision and intellectual contribution
Amita Gupta: literature search, study design, data interpretation, manuscript drafting, manuscript revision and intellectual contribution
References
- 1.UNAIDS. How AIDS changed everything: MDG 6: 15 YEARS, 15 LESSONS OF HOPE FROM THE AIDS ESPONSE. [accessed July 14 2015 2015];Fact Sheet. 2015 http://www.unaids.org/sites/default/files/media_asset/20150714_FS_MDG6_Report_en.pdf.
- 2.Gupta A, Nadkarni G, Yang WT, et al. Early Mortality in Adults Initiating Antiretroviral Therapy (ART) in Low- and Middle-Income Countries (LMIC): A Systematic Review and Meta-Analysis. PLoS ONE. 2011;6(12):e28691. doi: 10.1371/journal.pone.0028691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gupta A, Wood R, Kaplan R, Bekker LG, Lawn SD. Prevalent and incident tuberculosis are independent risk factors for mortality among patients accessing antiretroviral therapy in South Africa. PLoS One. 2013;8(2):e55824. doi: 10.1371/journal.pone.0055824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lawn SD, Badri M, Wood R. Tuberculosis among HIV-infected patients receiving HAART: long term incidence and risk factors in a South African cohort. AIDS. 2005;19(18):2109–16. doi: 10.1097/01.aids.0000194808.20035.c1. [DOI] [PubMed] [Google Scholar]
- 5.Brinkhof MW, Egger M, Boulle A, et al. Tuberculosis after initiation of antiretroviral therapy in low-income and high-income countries. Clin Infect Dis. 2007;45(11):1518–21. doi: 10.1086/522986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gupta RK, Lucas SB, Fielding KL, Lawn SD. Prevalence of tuberculosis in post-mortem studies of HIV-infected adults and children in resource-limited settings: a systematic review and meta-analysis. AIDS. 2015;29(15):1987–2002. doi: 10.1097/QAD.0000000000000802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Getahun H, Kittikraisak W, Heilig CM, et al. Development of a standardized screening rule for tuberculosis in people living with HIV in resource-constrained settings: individual participant data meta-analysis of observational studies. PLoS Med. 2011;8(1):e1000391. doi: 10.1371/journal.pmed.1000391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singhal S, Mahajan SN, Diwan SK, Gaidhane A, Quazi ZS. Correlation of sputum smear status with CD4 count in cases of pulmonary tuberculosis and HIV co-infected patients--a hospital based study in a rural area of Central India. The Indian journal of tuberculosis. 2011;58(3):108–12. [PubMed] [Google Scholar]
- 9.Scott LE, McCarthy K, Gous N, et al. Comparison of Xpert MTB/RIF with other nucleic acid technologies for diagnosing pulmonary tuberculosis in a high HIV prevalence setting: a prospective study. PLoS Med. 2011;8(7):e1001061. doi: 10.1371/journal.pmed.1001061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fenner L, Ballif M, Graber C, et al. Tuberculosis in antiretroviral treatment programs in lower income countries: availability and use of diagnostics and screening. PLoS One. 2013;8(10):e77697. doi: 10.1371/journal.pone.0077697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Theron G, Zijenah L, Chanda D, et al. Feasibility, accuracy, and clinical effect of point-of-care Xpert MTB/RIF testing for tuberculosis in primary-care settings in Africa: a multicentre, randomised, controlled trial. Lancet. 2014;383(9915):424–35. doi: 10.1016/S0140-6736(13)62073-5. [DOI] [PubMed] [Google Scholar]
- 12.Churchyard GJ, Stevens WS, Mametja LD, et al. Xpert MTB/RIF versus sputum microscopy as the initial diagnostic test for tuberculosis: a cluster-randomised trial embedded in South African roll-out of Xpert MTB/RIF. The Lancet Global health. 2015;3(8):e450–7. doi: 10.1016/S2214-109X(15)00100-X. [DOI] [PubMed] [Google Scholar]
- 13.Cox HS, Mbhele S, Mohess N, et al. Impact of Xpert MTB/RIF for TB diagnosis in a primary care clinic with high TB and HIV prevalence in South Africa: a pragmatic randomised trial. PLoS Med. 2014;11(11):e1001760. doi: 10.1371/journal.pmed.1001760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization; WHO, editor. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: what’s new Policy brief. 2015. p. 20. [Google Scholar]
- 15.Temprano ANRS Study Group. A Trial of Early Antiretrovirals and Isoniazid Preventive Therapy in Africa. N Engl J Med. 2015 doi: 10.1056/NEJMoa1507198. [DOI] [PubMed] [Google Scholar]
- 16.Houben RM, Sumner T, Grant AD, White RG. Ability of preventive therapy to cure latent Mycobacterium tuberculosis infection in HIV-infected individuals in high-burden settings. Proc Natl Acad Sci U S A. 2014;111(14):5325–30. doi: 10.1073/pnas.1317660111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koenig SP, Riviere C, Leger P, et al. High mortality among patients with AIDS who received a diagnosis of tuberculosis in the first 3 months of antiretroviral therapy. Clin Infect Dis. 2009;48(6):829–31. doi: 10.1086/597098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mfinanga S, Chanda D, Kivuyo SL, et al. Cryptococcal meningitis screening and community-based early adherence support in people with advanced HIV infection starting antiretroviral therapy in Tanzania and Zambia: an open-label, randomised controlled trial. Lancet. 2015;385(9983):2173–82. doi: 10.1016/S0140-6736(15)60164-7. [DOI] [PubMed] [Google Scholar]
- 19.Dart Trial Team. Mugyenyi P, Walker AS, et al. Routine versus clinically driven laboratory monitoring of HIV antiretroviral therapy in Africa (DART): a randomised non-inferiority trial. Lancet. 2010;375(9709):123–31. doi: 10.1016/S0140-6736(09)62067-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jindani A, Dore CJ, Mitchison DA. Bactericidal and sterilizing activities of antituberculosis drugs during the first 14 days. Am J Respir Crit Care Med. 2003;167(10):1348–54. doi: 10.1164/rccm.200210-1125OC. [DOI] [PubMed] [Google Scholar]
- 21.Akolo C, Adetifa I, Shepperd S, Volmink J. Treatment of latent tuberculosis infection in HIV infected persons. Cochrane Database Syst Rev. 2010;(1):CD000171. doi: 10.1002/14651858.CD000171.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Samandari T, Agizew TB, Nyirenda S, et al. 6-month versus 36-month isoniazid preventive treatment for tuberculosis in adults with HIV infection in Botswana: a randomised, double-blind, placebo-controlled trial. Lancet. 2011;377(9777):1588–98. doi: 10.1016/S0140-6736(11)60204-3. [DOI] [PubMed] [Google Scholar]
- 23.Rangaka MX, Wilkinson RJ, Boulle A, et al. Isoniazid plus antiretroviral therapy to prevent tuberculosis: a randomised double-blind, placebo-controlled trial. Lancet. 2014;384(9944):682–90. doi: 10.1016/S0140-6736(14)60162-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Charalambous S, Grant AD, Innes C, et al. Association of isoniazid preventive therapy with lower early mortality in individuals on antiretroviral therapy in a workplace programme. AIDS. 2010;24(Suppl 5):S5–13. doi: 10.1097/01.aids.0000391010.02774.6f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Golub JE, Pronyk P, Mohapi L, et al. Isoniazid preventive therapy, HAART and tuberculosis risk in HIV-infected adults in South Africa: a prospective cohort. AIDS. 2009;23(5):631–6. doi: 10.1097/QAD.0b013e328327964f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Durovni B, Saraceni V, Moulton LH, et al. Effect of improved tuberculosis screening and isoniazid preventive therapy on incidence of tuberculosis and death in patients with HIV in clinics in Rio de Janeiro, Brazil: a stepped wedge, cluster-randomised trial. Lancet Infect Dis. 2013;13(10):852–8. doi: 10.1016/S1473-3099(13)70187-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lawn SD, Wood R, De Cock KM, Kranzer K, Lewis JJ, Churchyard GJ. Antiretrovirals and isoniazid preventive therapy in the prevention of HIV-associated tuberculosis in settings with limited health-care resources. Lancet Infect Dis. 2010;10(7):489–98. doi: 10.1016/S1473-3099(10)70078-5. [DOI] [PubMed] [Google Scholar]
- 28.IeDea, Collaborations ARTC. Avila D, et al. Immunodeficiency at the start of combination antiretroviral therapy in low-, middle-, and high-income countries. J Acquir Immune Defic Syndr. 2014;65(1):e8–16. doi: 10.1097/QAI.0b013e3182a39979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lawn SD, Kerkhoff AD, Vogt M, Wood R. Diagnostic accuracy of a low-cost, urine antigen, point-of-care screening assay for HIV-associated pulmonary tuberculosis before antiretroviral therapy: a descriptive study. Lancet Infect Dis. 2011 doi: 10.1016/S1473-3099(11)70251-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Peter JG, Zijenah LS, Chanda D, et al. The mortality impact of point-of-care urine lipoarabinomannan testing to guide tuberculosis treatment initiation in HIV-infected hospitalised patients: a multi-country randomised controlled trial. 46th World Conference on Lung Health of the International Union Against Tuberculosis and Lung Disease (The Union); 2015; Cape Town. 2015. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.