Abstract
Objectives:
To evaluate the analgesic effect of transversus abdominis plane (TAP) block administered before varicocele surgery.
Methods:
This study was completed at the Faculty of Medicine, Çanakkale Onsekiz Mart University, Çanakkale, Turkey, between January 2011 and April 2013. In a prospective, double blind, randomized, placebo controlled clinical study, 40 male patients scheduled for elective varicocele operations were randomized to group T (treatment group) or group C (controls). After receiving general anesthesia, group T received a TAP block using 20 mL 0.25% bupivacaine on the operation side, whereas group C received a control block using 20 mL 0.9% Sodium chloride. During the first 24 hours after surgery, the patient pain was evaluated using the visual analogue scale (VAS) at rest and while coughing. Postoperative patient controlled analgesia morphine consumption, VAS scores, and side effects were recorded.
Results:
Of 34 patients, Group T (n=18) had significantly lower VAS pain scores than Group C (n=16) both at rest and while coughing. The total morphine consumed was lower (7.7 ± 4.0) versus 21.6 ± 12.4 mg, p<0.001) in the 24 hours after surgery.
Conclusion:
As part of a multimodal analgesic regime after varicocelectomy surgery, morphine consumption and VAS pain scores were significantly lower among those receiving 20 mL 0.25% bupivacaine administered for a TAP block than among controls.
As part of multi-model analgesic techniques for reducing postoperative pain, recent research has focused on the transversus abdominis plane (TAP) block, a regional anesthesia technique first defined by Rafi1 in 2001 as a local anesthesia injected between the transversus abdominis and internal oblique muscles in the petit triangle.1 Administered using real time ultrasound (US) imaging greater reliability is achieved; therefore, the preference is to use US guided transversus abdominis block (USG-TAP).2 Aiming to block the nerves in the abdominal anterolateral wall when used as part of a multimodal postoperative pain treatment, TAP has been shown to be a very effective analgesic regime for surgeries such as cesarean section,3 inguinal hernia,4 total abdominal hysterectomy,5 renal transplant,6 and open appendectomy.7 The only study to evaluate the efficiency of the TAP block for varicocele surgery was performed by Milone et al8 using 33 spinal surgery patients published in 2013. This study showed that the TAP block was an effective and applicable anesthetic method for retroperitoneal varicocelectomy. Studies exploring the efficacy of the TAP block in patients under general anesthesia for planned varicoselectomy seem to be lacking from the literature. We hypothesize that applying the TAP block before varicocele surgery would reduce patient pain in the postoperative period. The primary aim of this study was to compare the pain scores at rest and during movement (coughing) among those receiving a TAP block and controls during the first 24 hours after surgery. The secondary aim was to assess the amount of opioids consumed during this period.
Methods
This study was carried out in the Anesthesiology and Reanimation Department and the Urology Department, Medical Faculty Hospital Çanakkale Onsekiz Mart University, Çanakkale, Turkey between January 2011 and April 2013. Permission was granted by the Çanakkale Onsekiz Mart University Medical Faculty Ethics Committee. Patients with planned elective varicocele operations and who provided informed consent were included in the study. Our study was conducted according to the Helsinki declaration principles on human clinical studies. It was a prospective, double blind, randomized, placebo controlled clinical study. In addition, it complies with the design and layout requirements of the Consolidated Standards of Reporting Clinical Trials (CONSORT).9
Patients
Patients between 18 and 65 years, classified as American Society of Anesthesiologists (ASA) groups I or II, and scheduled for planned, elective varicocele operations were included in the study. Exclusion criteria were: (i) reduced mental capacity or psychiatric disease; (ii) excessive sensitivity to the agents used; (iii) cardiovascular, liver, or renal disease; (iv) alcohol or drug addiction or history of chronic painkiller or anesthetic material use; (v) tricyclic antidepressant, opioid analgesics, or corticosteroid use over the prior 24 hours; (vi) diagnosis of pain syndrome; (vii) obesity (body weight >30 kg/m2); and (viii) recurring varicocele.
Anesthesia
All patients undergoing operation were administered the same anesthetic protocol: 0.02 mg/kg midazolam, 1 µg/kg fentanyl, and 2 mg/kg propofol intravenous for anesthesia induction. After 0.1 mg/kg vecuronium was given and the muscles had relaxed sufficiently, tracheal intubation was performed. To maintain anesthesia, 5% to 6% desflurane and 1:1 nitrous oxide and oxygen were administered. Under general anesthesia, prior to initiation of surgery, all patients were given an injection in the TAP appropriate for the protocol. At the end of surgery, 20 mg tenoxicam was administered intravenously to all patients, and each was given intravenous patient controlled analgesia (IVPCA) 20 minutes prior to the end of the operation. If no complaint was made, antiemetics were not administered.
Blinding and randomization
Patients were randomly divided into 2 groups using a random sample table. All medications were placed in the injectors by an anesthetist blind to the study conditions. A 10mL 0.5% bupivacaine (Marcaine® 0.5%, AstraZeneca, Istanbul, Turkey) added with 10 mL saline was prepared for the treatment group (group T). For control group (group C), 20 mL 0.9% NaCl was prepared.
Ultrasound-guided TAP block procedure
Each patient, under general anesthesia, was given a USG-TAP block under sterile conditions on the same side as the varicocele operation performed by the same researcher. A USG device and a 6-12-MHz linear transducer (GE LOGIQ C5 Premium®; GE, Jiangsu, China) were used. The USG probe was located in the axial plane at the center point of the iliac crest and costal margin. After an appropriate image was obtained (machine setting, depth, and gain), the external oblique, internal oblique, and transabdominal muscles, peritoneal, and intraperitoneal structures were differentiated. Guided by real time USG images, a 150mm long 20G nerve stimulator needle (Braun, Melsungen, Germany) was inserted between the internal oblique and transabdominal muscles under in-plane USG images. For the negative aspiration test, 1-2 mg 0.9% sodium chloride (NaCl) was administered, and the fluid distribution between the muscle layers was monitored on simultaneous USG images. Once the location of the needle was confirmed, depending on the protocol, local anesthetic (LA) or 0.9% NaCl was administered in a similar method by monitoring the accompanying images.
Surgical procedures
All surgical procedures were performed by the same surgeon. The surgical procedure for all patients was completed using the Ivanissevich varicocelectomy method.10,11 An appropriate incision was made in the symphysis pubis 2 cm above the internal and external inguinal ring between skin folds. Along the external oblique, using a fascia incision, the skin was opened taking care to protect the ilioinguinal nerve underneath. The spermatic cord was freed from the surrounding tissue and held by a Penrose drain. Above the spermatic cord, the cremasteric muscle was opened longitudinally, and the widened veins were found. The widened veins were freed one by one, tied with 4/0 silk suture, and cut. After bleeding was checked, the layers were closed according to the anatomic plan.
Postoperative procedures
On the day of the procedure, the visual analogue scale (VAS) and how it is scored was explained to all patients. A 10 cm long horizontal line was used, and represents no pain at the left end point and the most severe pain at the right end point. All patients were asked twice regarding the pain at rest and after coughing strongly to evaluate the pain in motion. All patients were given IV morphine (0.5 mg/mL) through a patient controlled analgesia (PCA) pump program for demand mode only with a basal rate of zero. It was set to administer 1 mg per bolus every 10 minutes as needed (up to 10 mg per 4 hours). Informed patients could demand analgesics from the first moment of postoperative pain by pressing the button on the IV PCA. The patient was prevented from consuming an overdose of morphine through the lock mechanism. In this situation, the patient’s requested and received amounts were recorded in the memory of the device. In the recovery room (postanesthesia care unit-PACU) 15 minutes after surgery, and in the ward on the first, second, fourth, eight, twelfth, and twenty-fourth hours patient pain was evaluated using the VAS. Our primary outcome was the comparison of the postoperative VAS pain scores between the 2 groups. The secondary outcome was comparison with the opioid consumption across the first 24 hours between the 2 groups. Simultaneously, sedation was evaluated on a Ramsey scale (0= patient is fully awake; 1= patient is somnolent and responds to verbal calls, 2 = patient is somnolent and responds to tactile stimuli, 3 = patient is drowsy and responds to pain stimuli, and 4 = patient cannot be woken). Nausea and vomiting were determined by a VAS (no symptoms to symptoms unbearably severe). When VAS pain scores exceeded 4, a 75 mg dose of diclofenac sodium was administered intramuscularly. When VAS nausea scores exceeded 4, or when vomiting occurred, 10 mg metoclopramide was administered intravenously. The anesthesia team that evaluated pain was blinded to the medications used.
Power analysis
We sought to investigate the analgesic efficiency of the USG-TAP block used for varicocele surgeries. The main results of the study were postoperative VAS pain scores. The sample size estimation was based on the VAS assumed scores (5.2 ± 1.14) of a similar study performed by Soylemez et al.12 To detect a 20% change in VAS with an error of 0.05 and a power of 85%, the minimum sample size was found to be 15 patients per group. The sample size estimation was performed using Power Calculator (Department of Statistics, University of California, Los Angeles, CA, USA)
Statistical analysis
Statistical analyses were performed using the Statistical Package for the Social Sciences version 15.0 for Windows (SPSS Inc, Chicago, IL, USA). Descriptive statistics included the mean ± standard deviation for numerical data, and numbers and percentages for categorical data. The Kolmogorov Smirnov test was used to examine normality in the data. The Mann Whitney test was used to compare the averages of continuous measures such as age, weight, height, VAS, and morphine requirements. The Wilcoxon signed rank test was used to compare intragroup repeated measures, and the Chi-square test was used to compare data that denoted frequency, such as gender and ASA risk category. Statistical significance was recognized when p<0.05.
Results
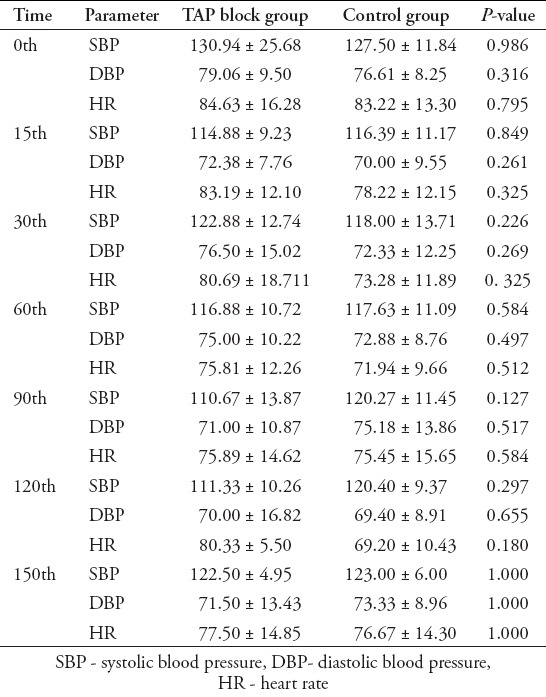
While 50 patients were screened for the enrollment, 34 patients were included in the analysis (18 in group T and 16 in group C; Figure 1). No statistical differences were found in the clinical and demographic variables of the groups (Table 1). The VAS pain scores when coughing and at rest were significantly lower in group T at all measured time points (p<0.05; Table 2). Group T consumed significantly less morphine than group C at all measured time points, except on admission to the PACU (Table 3). The total dose given to group C was 21.6 ± 12.4 mg; it was 7.7±4.0 mg for group T (Table 3). Among those who received unilateral repairs, a significant difference was observed in morphine consumption between the patients who underwent TAP block and the patients who did not undergo TAP block (p<0.05), except at PACU admission (p=0.563). Among those who received bilateral repairs, a significant difference between the groups was not found at any measured time point (Table 4). The need for diclofenac sodium was significantly higher in group C than in group T (p<0.001 at PACU and p=0.039 at 15th minute). No differences were found in hemodynamics between groups T and C (p<0.05; Table 5). In each group, one patient experienced nausea in the 15th minute postoperatively in the PACU; both were given 10 mg metoclopramide intravenously. No patient reported itching. No surgical, or anesthesia related complications were observed.
Figure 1.
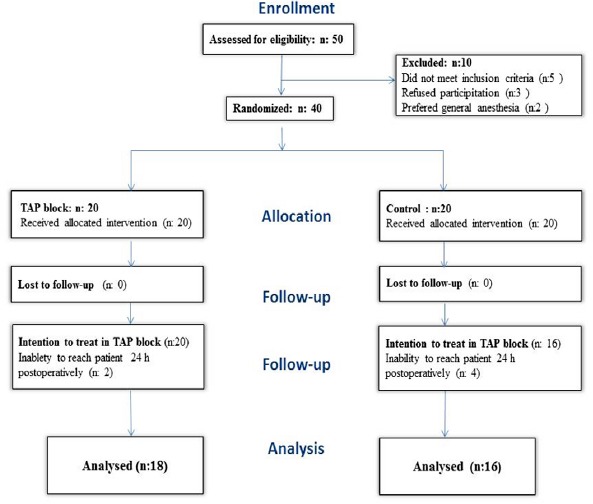
Flow chart of 50 patients were screened for a study on the efficacy of ultrasound-guided transversus abdominis plane (USG-TAP) in varicocelectomy.
Table 1.
Baseline clinical and demographic of 34 patients included in a study on the efficacy of USG-TAP in varicocelectomy.
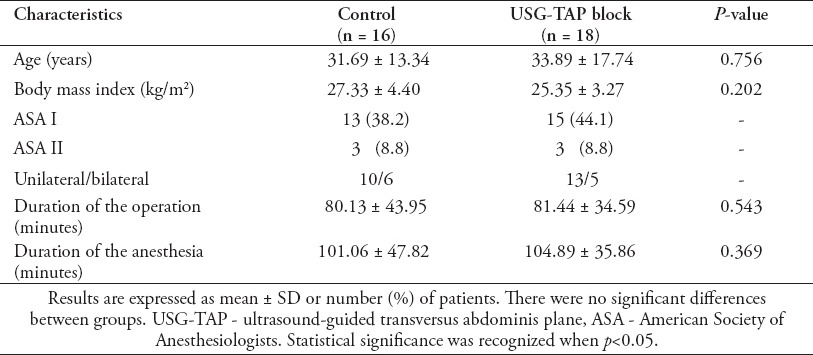
Table 2.
Pain intensity at various times during the postoperative period among 34 patients included in the study.
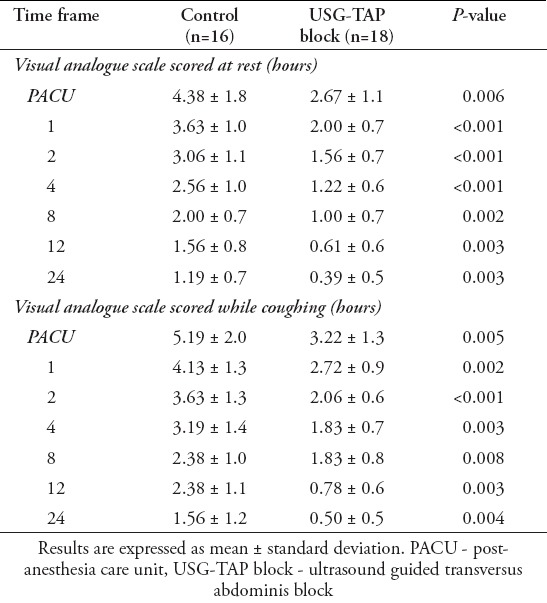
Table 3.
Postoperative morphine requirements of 34 patients included in the study.
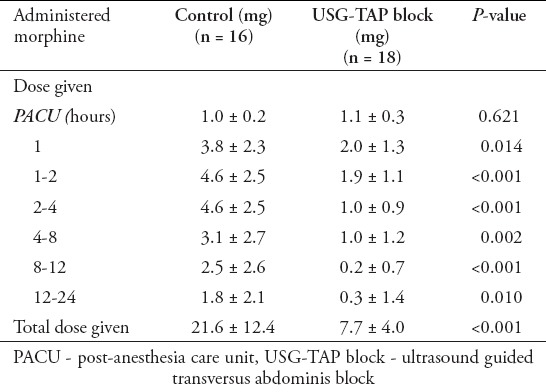
Table 4.
Postoperative morphine requirements among patients who received bilateral repairs among 34 patients included in the study.
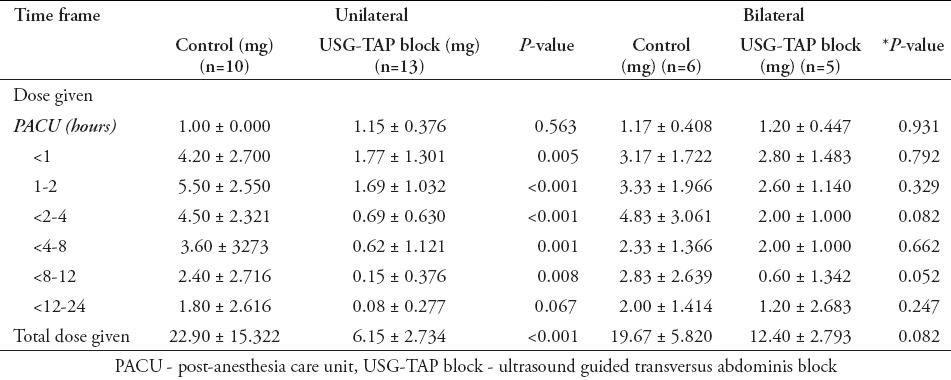
Table 5.
Hemodynamic variables during perioperative period 34 patients included in the study.
Discussion
This study shows that, as part of a multimodal analgesic regime for Ivanissevich varicocelectomy operations, 20 mL 0.25% bupivacaine administered by USG-TAP block provides effective analgesia in the postoperative period and reduces the need for opioids, compared with controls. In the first 24 hours postoperatively, pain was significantly less, both at rest and with coughing (Table 2). Also, except during PACU admission, the requested and administered morphine were significantly lower (Table 3). Many studies have assessed the efficacy of TAP blocks under various conditions, assessing the medication, dose, timing, location, and size of the surgical site, and application of general, or regional anesthesia. Most reported that the TAP block affects postoperative pain scores and opioid requirements in the first 24 hours after abdominal surgery, reducing the need for additional analgesics and increasing the time to the first rescue analgesic dose.3-8 While varicocele is observed in 15-22% of the adult male population, it is detected in 30-40% of those treated for infertility; it is the most frequent pathology in male infertility.13 It is treated using laparoscopic, or radiological (sclerotherapy or embolization) methods, but the gold standard is open surgery.11 Varicocelectomy is one of the most performed surgeries in urology clinics, and anesthetists use either general or regional anesthesia. Studies report successful TAP blocks from T6-L1 and sometimes up to L3, depending on the location of administration with dermatome involvement,14,15 but only the techinique by Milone et al8 uses it for varicocelectomy. Using 33 patients undergoing Palomo varicocelectomy under spinal anesthesia with a TAP block, they reported significantly lower VAS scores at rest and in motion, compared with controls. Although there was no significant difference at the end of the first 24 hour recovery period, they also required less analgesia. We similarly found that, while patients were given general anesthesia during that time frame, VAS values both at rest and while coughing as well as the IV PCA administered morphine, were significantly lower using the USG-TAP block. The rescue analgesic dose was significantly higher in the control group. In a study of ASA III patients with cardiovascular disease undergoing abdominal surgery, Tsuchiya et al16 compared hemodynamic stability and recovery in patients who received general anesthesia with and without a TAP block. They found that patients who received the TAP block maintained better intraoperative hemodynamic control and had shorter recovery times, associated with lower consumption of anesthetics, fewer opioid doses, and lower severity of postoperative pain. Similarly, successful cases in which general anesthesia and TAP block have been used together for critical patients with serious renal, cardiovascular, or severe respiratory difficulties have been reported.14-17 However, we found no difference in hemodynamics between the treatment and control groups.
Transversus abdominis plane blocks have a wide range of use during intra and postoperative periods. For a patient with severe chronic obstructive pulmonary disease and left ventricular hypokinesis who presented with a femoral neck fracture, Stuart-Smith et al14 completed hemiarthroplasty with a TAP block and sedation. They first placed the needle just above the iliac crest posterior to the middle axillary line and administered the TAP block to widen the TAP block’s effect in the lower segments of L1. Next, an LA was administered at a high volume and high dose (20 mL 1% lidocaine and 20 mL 0.5% bupivacaine) to provide a wider paravertebral distribution, achieving a loss of sensation to pain in the T11-L3 dermatomes, covering the surgical area. Because L1 segment coverage is sufficient for varicocele surgery, we selected the posterior line of the classic Petit’s triangle and a 20 mL volume for the TAP block.
In another study,4 patients undergoing outpatient Lichtenstein hernia repairs received an LA with, or without a TAP block and found that those receiving the TAP block showed a higher efficacy from the LA as well as better pain control postoperatively. These reports raise the question as to whether, with an appropriate dose suited to the correct anatomical structures, varicocelectomy using only a TAP block and sedation could be possible. However, additional studies are required to assess the effectiveness of this approach.
Recently, the TAP block has been used to relieve postoperative pain. In one case, treatment of long term pain developing after thoracotomy surgery was treated with a USG-TAP block using 20 mL 0.5% levobupivacaine for pain involving T7-10 dermatomes.18 Four 15-mL injections of 2.5 mg/mL bupivacaine were administered in the lateral medial plane for postoperative pain in patients with large open or laparoscopic abdominal surgeries, resulting in a clear reduction in VAS pain scores; the patients could be mobilized within the first 6 hours.19 In this study, a bilateral 4 point single shot technique in the upper (T6-T9) and lower (T10-T12) abdominal wall was used to provide effective postoperative analgesia. This new 4 point single shot technique was effective at reducing severe pain after major abdominal surgery. Another study used MRI to investigate the distribution of local anesthetics and the relationship between this distribution and the obtained sensory dermatomal anesthesia after performing USG-TAP blocks on volunteers. To attain full anterior abdominal wall (T6-T12) anesthesia, a low volume (15 mL) double injection was sufficient, whereas the same total volume (30 mL) in a single injection was not.20 We found that 20 mL 0.5% bupivacaine administered in a single injection was sufficient for a TAP block in patients undergoing varicocelectomy and clearly reduced postoperative VAS pain scores and morphine requirements (Tables 2 & 3). Neither a higher volume nor additional injections were required. Though the contribution of TAP blocks to various abdominal surgeries has been shown, a consensus on the optimal doses and distribution of the administered medications has not been reached. A study performed in healthy volunteers identified an irregular area of cutaneous sensory block, contradicting the idea of non-dermatomal spread.21 As shown in a study performed in cadavers, this situation can be explained by the presence of a plexus of nerves instead of special nerves located in the abdominal transverse plane on the anterior abdominal wall.15 Similarly, Stoving et al22 compared a USG-TAP block using 20 mL 7.5 mg/mL ropivacaine with placebo in healthy volunteers and reported that the medication distribution was nondermatomal, did not cross the medial line, and exhibited greater caudal and lateral involvement and less medial involvement; they suggested that this approach may not be successful for surgeries with incisions on the medial line. These results remind us once again of the importance of the volume and injection points for block activity. We observed that a TAP block using 20 mL bupivacaine at the midpoint of the midaxillary line between the iliac crest and costal margin reduced opioid requirements and provided effective analgesia after varicocelectomy. Stoving et al22 also reported that all lateral abdominal muscle layers significantly thinned, and the abdominal circumference increased much more during maximal voluntary contraction than the relaxed condition on the blocked side. The clinical benefits of abdominal muscle layer relaxation and the effects on intra abdominal pressure changes have not been established, and further studies are required. The USG-TAP block increases the success rate and reduces the number of attempt at TAP block administration and real time observation of the needle and LA distribution reduces the complication rate. In a study in which investigators were blind to needle position, Weintraud et al23 found that when LA was applied between the inner oblique and transversus abdominis muscles, accuracy, as confirmed by an experienced ultrasonographer, was acceptable only 14% of the time. In all other cases, the LA was injected in the surrounding tissue, and 84% of the time, it spread through more than one anatomic layer. Overall, only 45% did not reach the criteria for success. Using US, we were able to successfully administer the LA and increase its distribution in the correct area. Performing the TAP block without US or with blind administration of the LA can result in intrahepatic injection,24 transient femoral nerve palsy,25 or abdominal wall hematoma.26 Rarely, systemic neurotoxicity,27,28 liver lacerations, and later peritonitis29 have developed after a USG-TAP block. By using an appropriate USG device that shows the deep tissue with good images and by following the needle tip carefully without disturbing deep tissue, an experienced operator can assure short duration of the TAP block, fewer attempts, and less complications.30 We experienced no complications among our patients.
Study limitations
First, although the USG-TAP block was performed with real time images, the patients were under general anesthesia; therefore an evaluation of the sensory block could not be made. Second, use of a larger volume of LA may have increased our success rate, but others have reported that a larger total volume (40 mL) leads to increased paravertebral distribution. Our relatively large sample size could be more appropriate for comparing unilateral with bilateral varicocele procedures.
In conclusion, as part of a multimodal analgesic regime for Ivanissevich varicocelectomy operations, 20 mL 0.25% bupivacaine administered by a USG-TAP block can provide effective analgesia in the postoperative period and reduce the need for opioids. Thus, in varicocelectomy patients, a USG-TAP block may represent a safe and effective method for postoperative pain control. However, more advanced studies are required to determine the most appropriate LA, volume, concentration, and timing for the TAP block in varicocelectomy operations.
Footnotes
References
- 1.Rafi AN. Abdominal field block: a new approach via the lumbar triangle. Anaesthesia. 2001;56:1024–1026. doi: 10.1046/j.1365-2044.2001.02279-40.x. [DOI] [PubMed] [Google Scholar]
- 2.McDermott G, Korba E, Mata U, Jaigirdar M, Narayanan N, Boylan J, et al. Should we stop doing blind transversus abdominis plane blocks? Br J Anaesth. 2012;108:499–502. doi: 10.1093/bja/aer422. [DOI] [PubMed] [Google Scholar]
- 3.Abdallah FW, Halpern SH, Margarido CB. Transversus abdominis plane block for postoperative analgesia after Caesarean delivery performed under spinal anaesthesia?A systematic review and meta-analysis. Br J Anaesth. 2012;109:679–687. doi: 10.1093/bja/aes279. [DOI] [PubMed] [Google Scholar]
- 4.Milone M, Di Minno MN, Musella M, Maietta P, Salvatore G, Iacovazzo C, et al. Outpatient inguinal hernia repair under local anaesthesia: feasibility and efficacy of ultrasound-guided transversus abdominis plane block. Hernia. 2013;17:749–755. doi: 10.1007/s10029-012-1022-2. [DOI] [PubMed] [Google Scholar]
- 5.Bhattacharjee S, Ray M, Ghose T, Maitra S, Layek A. Analgesic efficacy of transversus abdominis plane block in providing effective perioperative analgesia in patients undergoing total abdominal hysterectomy: a randomized controlled trial. Journal of Anaesthesiology, Clinical Pharmacology. 2014;30:391–396. doi: 10.4103/0970-9185.137274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Soltani Mohammadi S, Dabir A, Shoeibi G. Efficacy of transversus abdominis plane block for acute postoperative pain relief in kidney recipients: a double-blinded clinical trial. Pain Med. 2014;15:460–464. doi: 10.1111/pme.12311. [DOI] [PubMed] [Google Scholar]
- 7.Cho S, Kim YJ, Kim DY, Chung SS. Postoperative analgesic effects of ultrasound guided transversus abdominis plane block for open appendectomy. Journal of the Korean Surgical Society. 2013;85:128–133. doi: 10.4174/jkss.2013.85.3.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Milone M, Di Minno MN, Musella M, Maietta P, Iacovazzo C, Milone F. Ultrasound-guided transversus abdominis plane block for retroperitoneal varicocele repair. Could it be an anesthesia method? Updates Surg. 2013;65:225–230. doi: 10.1007/s13304-013-0211-6. [DOI] [PubMed] [Google Scholar]
- 9.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Int J Surg. 2011;9:672–677. doi: 10.1016/j.ijsu.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 10.Ivanissevich O. Left varicocele due to reflux;experience with 4,470 operative cases in forty-two years. J Int Coll Surg. 1960;34:742–755. [PubMed] [Google Scholar]
- 11.González R. Proposal for describing procedures to correct varicocele. A new terminology. Front Pediatr. 2014;30:47. doi: 10.3389/fped.2014.00047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Soylemez H, Penbegul N, Atar M, Bozkurt Y, Sancaktutar AA, Altunoluk B. Comparison of laparoscopic and microscopic subinguinal varicocelectomy in terms of postoperative scrotal pain. JSLS. 2012;16:212–217. doi: 10.4293/108680812X13427982376220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cayan S, Kadıoglu A. Derleme: Variloselin tedavisinde güncel yaklaşımlar. [Review: current approaches in the diagnosis and treatment of varicocele] Turk J Urol. 2005;31:57–63. [Google Scholar]
- 14.Stuart-Smith K. Hemiarthroplasty performed under transversus abdominis plane block in a patient with severe cardiorespiratory disease. Anaesthesia. 2013;68:417–420. doi: 10.1111/anae.12108. [DOI] [PubMed] [Google Scholar]
- 15.Rozen WM, Tran TM, Ashton MW, Barrington MJ, Ivanusic JJ, Taylor GI. Refining the course of the thoracolumbar nerves: a new understanding of the innervation of the anterior abdominal wall. Clin Anat. 2008;21:325–333. doi: 10.1002/ca.20621. [DOI] [PubMed] [Google Scholar]
- 16.Tsuchiya M, Takahashi R, Furukawa A, Suehiro K, Mizutani K, Nishikawa K. Transversus abdominis plane block in combination with general anesthesia provides better intraoperative hemodynamic control and quicker recovery than general anesthesia alone in high-risk abdominal surgery patients. Minerva Anestesiol. 2012;78:1241–1247. [PubMed] [Google Scholar]
- 17.Patil SS, Pawar SC, Divekar V, Bakhshi RG. Transversus abdominis plane block for an emergency laparotomy in a high-risk, elderly patient. Indian Journal of Anaesthestists. 2010;54:249–254. doi: 10.4103/0019-5049.65377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ekmekci P, Kazak Bengisun Z, Kazbek BK, Han S, Tuzuner F. Ultrasound guided TAP block for the treatment of postoperative prolonged pain-an alternative approach. Agri. 2012;24:191–193. doi: 10.5505/agri.2012.82905. [DOI] [PubMed] [Google Scholar]
- 19.Borglum J, Maschmann C, Belhage B, Jensen K. Ultrasound-guided bilateral dual transversus abdominis plane block: a new four-point approach. Acta Anaesthesiol Scand. 2011;55:658–663. doi: 10.1111/j.1399-6576.2011.02430.x. [DOI] [PubMed] [Google Scholar]
- 20.Borglum J, Jensen K, Christensen AF, Hoegberg LC, Johansen SS, Lonnqvist PA, et al. Distribution patterns, dermatomal anesthesia, and ropivacaine serum concentrations after bilateral dual transversus abdominis plane block. Reg Anesth Pain Med. 2012;37:294–301. doi: 10.1097/AAP.0b013e31824c20a9. [DOI] [PubMed] [Google Scholar]
- 21.Carney J, Finnerty O, Rauf J, Bergin D, Laffey JG, Mc Donnell JG. Studies on the spread of local anaesthetic solution in transversus abdominis plane blocks. Anaesthesia. 2011;66:1023–1030. doi: 10.1111/j.1365-2044.2011.06855.x. [DOI] [PubMed] [Google Scholar]
- 22.Stoving K, Rothe C, Rosenstock CV, Aasvang EK, Lundstrom LH, Lange KH. Cutaneous sensory block area, muscle-relaxing effect, and block duration of the transversus abdominis plane block: a randomized, blinded, and placebo-controlled study in healthy volunteers. Reg Anesth Pain Med. 2015;40:355–362. doi: 10.1097/AAP.0000000000000252. [DOI] [PubMed] [Google Scholar]
- 23.Weintraud M, Marhofer P, Bosenberg A, Kapral S, Willschke H, Felfernig M, et al. Ilioinguinal/iliohypogastric blocks in children: where do we administer the local anesthetic without direct visualization? Anesth Analg. 2008;106:89–93. doi: 10.1213/01.ane.0000287679.48530.5f. [DOI] [PubMed] [Google Scholar]
- 24.Farooq M, Carey M. A case of liver trauma with a blunt regional anesthesia needle while performing transversus abdominis plane block. Reg Anesth Pain Med. 2008;33:274–275. doi: 10.1016/j.rapm.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 25.Walker G. Transversus abdominis plane block: a note of caution! Br J Anaesth. 2010;104:265. doi: 10.1093/bja/aep387. [DOI] [PubMed] [Google Scholar]
- 26.Randall IM, Costello J, Carvalho JC. Transversus abdominis plane block in a patient with debilitating pain from an abdominal wall hematoma following Cesarean delivery. Anesth Analg. 2008;106:1928. doi: 10.1213/ane.0b013e318170baf3. [DOI] [PubMed] [Google Scholar]
- 27.Sakai T, Manabe W, Kamitani T, Takeyama E, Nakano S. Ropivacaine-induced late-onset systemic toxicity after transversus abdominis plane block under general anesthesia: successful reversal with 20% lipid emulsion. Masui. 2010;59:1502–1505. [PubMed] [Google Scholar]
- 28.Griffiths JD, Le NV, Grant S, Bjorksten A, Hebbard P, Royse C. Symptomatic local anaesthetic toxicity and plasma ropivacaine concentrations after transversus abdominis plane block for Caesarean section. Br J Anaesth. 2013;110:996–1000. doi: 10.1093/bja/aet015. [DOI] [PubMed] [Google Scholar]
- 29.Lancaster P, Chadwick M. Liver trauma secondary to ultrasound-guided transversus abdominis plane block. Br J Anaesth. 2010;104:509–510. doi: 10.1093/bja/aeq046. [DOI] [PubMed] [Google Scholar]
- 30.Petersen PL, Mathiesen O, Torup H, Dahl JB. The transversus abdominis plane block: a valuable option for postoperative analgesia?A topical review. Acta Anaesthesiol Scand. 2010;54:529–535. doi: 10.1111/j.1399-6576.2010.02215.x. [DOI] [PubMed] [Google Scholar]


