Abstract
The NF-κB transcription factor pathway is a crucial regulator of inflammation and immune responses. Additionally, aberrant NF-κB signaling has been identified in many types of cancer. Downstream of key oncogenic pathways, such as RAS, BCR-ABL, and Her2, NF-κB regulates transcription of target genes that promote cell survival and proliferation, inhibit apoptosis, and mediate invasion and metastasis. The cancer stem cell model posits that a subset of tumor cells (cancer stem cells) drive tumor initiation, exhibit resistance to treatment, and promote recurrence and metastasis. This review examines the evidence for a role for NF-κB signaling in cancer stem cell biology.
Keywords: NF-κB, cancer, cancer stem cells, tumor-initiating cells, self-renewal
1. Introduction to NF-κB Signaling
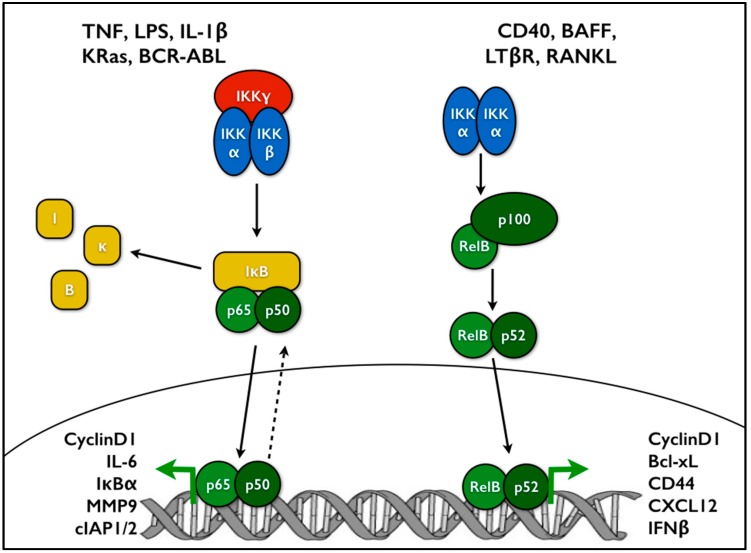
The NF-κB family of transcription factors consists of five members: p65 (RelA), RelB, c-Rel, p105/p50, and p100/p52. Each of these proteins contains a conserved N-terminal Rel homology domain which enables nuclear localization, DNA binding, and homo- and heterodimerization. p65, RelB, and c-Rel feature transcription activation domains as well, while p50 and p52 do not. The precursors p105 and p100 include ankyrin repeats which are proteolytically cleaved to produce the active subunits p50 and p52, respectively [1]. NF-κB signaling typically operates through two major pathways: the canonical and the non-canonical. Activation of the canonical pathway occurs downstream of many stimuli, including LPS and pro-inflammatory cytokines such as TNF or IL-1. Under basal conditions, p65-p50 dimers are bound by the inhibitor of κB proteins (IκBs), which shift the steady state localization of NF-κB to the cytosol, while still allowing nucleocytoplasmic shuttling [2,3,4,5]. Upon activation, the inhibitor of κB kinase (IKK) complex, which consists of the kinase subunits IKKα and IKKβ plus the regulatory subunit IKKγ (NEMO), phosphorylates IκBα, leading to its ubiquitination and proteasomal degradation. Loss of IκBα enhances NF-κB nuclear accumulation and DNA binding, promoting transcription of its target genes, including anti-apoptotic factors, cytokines such as IL-6, and proliferation factors such as cyclin D1 (Figure 1). One group of target genes includes negative regulators of NF-κB signaling, such as A20 and IκBα. By producing these components, NF-κB generates a negative feedback loop to add another dimension of control to this pathway. The non-canonical pathway is activated through developmental signals such as BAFFR, CD40, or LTβR. Here, p100 acts like an IκB molecule, holding RelB in the cytoplasm. Non-canonical signaling leads to stabilization of NF-κB-inducing kinase (NIK). NIK activates IKKα dimers, which subsequently phosphorylate p100. p100 phosphorylation leads to its cleavage into p52, producing an active RelB-p52 dimer that moves to the nucleus and regulates transcription (Figure 1) [6].
Figure 1.
NF-κB signaling consists of two main branches: canonical and non-canonical. On the left, canonical NF-κB is driven by the IKK complex containing IKKα, β, and γ subunits. Phosphorylation of IκBα leads to its degradation, allowing the p65-p50 dimer to accumulate in the nucleus and regulate transcription of target genes. On the right, non-canonical NF-κB is driven by IKKα homodimers, leading to p100 processing. Here the dimer consists of the RelB and p52 subunits. Canonical and non-canonical NF-κB subunits regulate expression of distinct and overlapping sets of target genes [7].
Given that NF-κB signaling is tightly intertwined with cytokine production and immune responses, it was natural to investigate a role for NF-κB in hematopoietic cells. Germline knockout of RelB resulted in mice with myeloid hyperplasia and extramedullary hematopoiesis [8]. Double knockout of cRel and RelA produced cells with impaired engraftment and erythropoiesis, along with deregulated granulocyte expansion [9], suggesting distinct, yet overlapping roles for different NF-κB subunits. Subsequent studies built on these findings to suggest that the level of NF-κB activation was tightly regulated in hematopoietic stem cells (HSCs). RelA deletion in HSCs leads to changes in gene expression consistent with decreased HSC maintenance and homeostasis with a concomitant increase in genes associated with lineage restricted cells [10]. Interestingly, non-canonical NF-κB was also found to contribute to HSC self-renewal, both intrinsically and through microenvironment interactions [11]. Others have found that activation of NF-κB, either through TLR activation or loss of miR-146, actually enhances myeloid differentiation of HSCs [12,13]. A similar paradigm is observed in embryonic stem cells, which are reported to have a low level of NF-κB activation. Nonetheless, inhibition of NF-κB drives differentiation of these cells [14,15]. Conversely, overexpression of p65 enhanced differentiation and loss of pluripotency in embryonic stem cells [16], consistent with the need for balanced NF-κB activity. Results in muscle stem cells show decreased canonical NF-κB signaling during differentiation, but a late induction of non-canonical NF-κB, demonstrating that these pathways can have distinct roles in stem cell biology [17,18,19]. Taken together, these studies illustrate the involvement of NF-κB signaling in the maintenance of a variety of stem cells, consistent with much of the literature on NF-κB in cancer stem cells.
2. NF-κB in Cancer
2.1. NF-κB Activation in Cancer
In addition to its roles in the innate immune system and inflammatory signaling, the NF-κB pathway has been extensively tied to cancer biology. The discovery of v-rel, the oncoprotein in an avian Rev-T virus responsible for reticuloendotheliosis, and its identification as the homolog of c-rel provided the first link between cancer and NF-κB [20,21]. Early efforts showed that NF-κB is activated downstream of oncogenic RAS and BCR-ABL, where it promotes the oncogenic phenotype [22,23,24]. Inhibition of NF-κB in oncogenic RAS+ cells leads to apoptosis, consistent with a role for NF-κB in driving an anti-apoptotic, pro-survival phenotype [25]. Many studies demonstrate that NF-κB and its target genes are upregulated in the majority of cancers—including both hematological malignancies and solid tumors. More recently, NF-κB has been shown to be activated downstream of loss of tumor suppressors such as p53, VHL, and PTEN [26,27,28,29,30,31,32,33,34]. While early efforts focused on analysis of canonical NF-κB signaling in cancer, recent studies indicate that non-canonical NF-κB signaling can also be found activated in different cancers [35,36,37,38,39,40,41]. Expression of the superrepressor form of IκBα (serines 32/36 mutated to alanines, preventing phosphorylation and degradation and leading to decreased NF-κB activity; IκBα-SR) and genetic deletion of IKKβ or RelA in RAS-driven lung tumor and melanoma models strongly suppressed tumor growth [42,43,44].
Once activated, NF-κB regulates a wide variety of target genes that overlap heavily with the hallmarks of cancer [45]. Proliferation is one of the most basic characteristics of a cancer cell and NF-κB is involved through regulation of CyclinD1, Cyclin E, and c-Myc. NF-κB promotes survival and inhibits apoptosis through several mechanisms [46]. These include transcriptional regulation of the cellular inhibitor of apoptosis (cIAPs) 1, 2 and XIAP, as well as Bcl-2 and Bcl-xL [47,48,49]. Perhaps, as expected, NF-κB regulates a number of cytokines that contribute to tumor-promoting inflammation such as: TNFα, IL-1, IL6, MCP1, COX2, and iNOS. Other NF-κB targets contribute to epithelial-mesenchymal transition (vimentin, Twist), remodeling the extracellular matrix through induction of angiogenesis (IL8, VEGF), and promotion of invasion and metastasis (MMP2, MMP9, uPA) [50].
The studies described above led to efforts to determine if human tumors feature genetic alterations in IKK/NF-κB components. Somewhat surprisingly, such mutations are not common. However, the level of coverage provided by next-generation sequencing has found examples of NF-κB-associated mutations in a low percentage of cancers, predominately hematological malignancies. Amplifications of c-rel, IKKβ, IKKγ, and the related kinase IKKε have been identified primarily in lymphomas and breast cancer [51,52,53]. Rearrangements of the NFKB2 locus (gene name for the p100 subunit) that lead to loss of the inhibitory IκB-like domain and increased p52 production are found in some B cell lymphomas [54]. C11orf95-RELA fusions have been described as driver events in ependymomas [55], while monoallelic deletions of IκBα were identified in a subset of glioblastoma [56]. Mutations in upstream proteins that lead to aberrant, constitutive NF-κB activation have been identified. For example, in certain subtypes of lymphoma, translocations can affect MALT1 and BCL10, while CARD11 features a variety of point mutations. All three of these proteins interact to form a complex that drives NF-κB activation [57]. Growth factor receptors, including EGFR and Her2, are frequently overexpressed in cancer and activate similar pathways, including NF-κB [58,59].
IKK exhibits NF-κB-independent functions that promote growth and survival functions important to a variety of cancer cells. For example, IKKα and IKKβ promote mTOR activation, via kinase activity [60,61,62,63]. Another example is that IKKα was found to phosphorylate the CDK inhibitor p27 downstream of Her2 to promote cancer stem cell self-renewal [64]. IKKβ was reported to phosphorylate the tumor suppressor p53 to promote its instability [65].
2.2. Chronic Inflammation as a Precursor to Cancer
Another line of research linking NF-κB with oncogenesis examines the connection between chronic inflammation and tumor development. The microenvironment surrounding a tumor includes fibroblasts, infiltrating immune cells, extracellular matrix proteins, and cytokines that interact with the tumor cells. In a mouse model of colitis-associated colon cancer with targeted IKKβ deletion in either the epithelial or myeloid compartments, NF-κB mediated survival of intestinal epithelial cells, while NF-κB activation in myeloid cells drove production of growth factors that promoted tumor proliferation [66]. In a model of hepatocellular carcinoma driven by treatment with the carcinogen diethylnitrosamine (DEN), NF-κB is again activated in the myeloid compartment, this time to drive IL6 production and subsequent STAT3 activation in the hepatocytes [67]. Interestingly, this model shows that deletion of IKKβ or IKKγ actually leads to enhanced tumor development. The liver initially shows more cell death following DEN treatment, however, because hepatocytes are highly regenerative, the cell death triggers proliferation of the remaining cells [68]. It is thought that a cycle of injury, cell death, and proliferation drives tumor formation in this model [69]. NF-κB was shown to be activated in cancer-associated fibroblasts promoting the expression of inflammatory cytokines, although the role of this response in promoting tumorigenesis is controversial [70,71,72]. Work examining tumor-associated macrophages has shown that NF-κB signaling maintains a tumor-promoting, immunosuppressive (or M2) phenotype and inhibits a tumor-suppressing (or M1) phenotype [73,74]. Taken together, these studies start to describe a complex microenvironment with multiple cell types interacting to drive tumorigenesis and place NF-κB as a central mediator between these various components.
3. Cancer Stem Cells
Given the connections between the NF-κB pathway and the earliest events in oncogenesis, it follows that NF-κB signaling would be important in the tumor initiating cells. The cancer stem cell (CSC) model has been proposed to describe the cells which are responsible for tumor initiation. This phenomenon was first described in acute myeloid leukemia (AML), where cells from patients were transplanted into NOD/SCID mice and monitored for engraftment. Results from that study demonstrated that the CD34+ CD38− population of cells caused disease more frequently and at lower cell numbers than CD34− cells [75]. Subsequent to these findings, CSCs have been described in many solid tumors including those of the brain, prostate, breast, colon, and pancreas [76,77,78,79,80,81]. In addition to being responsible for primary tumor formation, CSCs are also generally thought to drive metastasis and exhibit increased resistance to radiation and chemotherapy. Due to their stem-like characteristics, these cells are also capable of differentiation into multiple lineages, which accounts for some of the heterogeneity seen in tumors [82]. While CSCs are frequently depicted at the top of a hierarchically arranged tumor, there is evidence that plasticity allows for the conversion of bulk tumor cells into CSCs [83].
Several assays allow for the study of CSCs. In vitro experiments focus on sphere formation under stem cell permissive conditions, such as serum-free media supplemented with essential growth factors and low-adherence plates. Ideally, these experiments are performed at limiting dilutions to best assess self-renewal from single cells. Additionally, in vivo assessments of tumor formation remain the gold standard for true CSC function, again preferably performed under limiting dilutions [84,85,86,87]. Frequently, prospective CSCs can be isolated from the bulk of the tumor cells based on one or more markers, either through the use of magnetic beads or fluorescence-activated cell sorting. Many markers have been proposed to distinguish CSCs from other tumor cells. While no individual marker is perfect, a few of the most commonly used markers include CD133, CD44 and EpCAM [76,78,79,81,88,89]. Once isolated, the populations can be compared in a number of phenotypic assays to dissect the differences between the cell types. Proliferation, survival, and gene expression analyses are commonly measured.
3.1. NF-κB Activation in CSCs
One of the earliest examples of NF-κB involvement in CSCs came from primary AML samples, where the CD34+ cells showed enhanced NF-κB DNA binding that was not seen in regular hematopoietic stem cells [90]. Since that initial report, elevated or constitutive NF-κB activity has been seen in many tumor types. Prostate CSCs were found to express higher levels of acetylated and total p65, as well as a decrease in IκBα expression when compared to parental tumors [91]. In glioblastoma, CSCs exhibited increased nuclear localization of p65 as compared with cells cultured under monolayer conditions [92]. Tumorsphere-forming cells showed increased phosphorylation of p65, again consistent with elevated NF-κB signaling in this population of cells. In that study, inhibition of NF-κB reduced self-renewal and blocked xenograft tumor growth using a limiting dilution approach [93]. In addition to direct evidence of preferential NF-κB activation in CSC subsets of tumors, several groups have taken an unbiased approach of profiling gene expression and defining CSC-associated signatures. This has revealed an inflammatory signature, which can frequently be tightly associated with NF-κB regulation, in a variety of tumors such as glioblastoma, breast, prostate, and ovarian cancers [94,95,96,97,98,99].
Perhaps not surprisingly, some of the same oncoproteins previously mentioned to activate NF-κB also participate in the CSC subpopulations of tumors. In mouse models of Her2-driven breast cancer, both canonical and non-canonical NF-κB pathways contribute to stemness and tumor formation. Expression of IκBα-SR impaired the formation of luminal epithelial tumors. Use of an NF-κB-GFP reporter allele localized activation to the luminal progenitors [100]. Another analysis of IκBα-SR in a Her2 mouse model found changes in a gene signature associated with stem cells, then specifically showed NF-κB-dependent changes in the specific stem cell factors Nanog and Sox2 (Figure 2) [101]. Knock-in of a kinase dead IKKα led to decreased self-renewal and senescence under mammary stem cell culture conditions [102]. In the Her2 breast cancer model, IKKα was found to phosphorylate p27 leading to its nuclear export and promoting CSC proliferation and expansion [64]. One of the canonical alterations that occurs during colorectal tumorigenesis is loss of APC. Myant and colleagues found that APC loss drives RAC1 activity to mediate ROS production and NF-κB activation, ultimately leading to an expansion of Lgr5+ CSCs [103].
Figure 2.
This diagram summarizes the various levels of NF-κB signaling in cancer stem cells. Both extracellular and intracellular sources of NF-κB activation are seen at the top. Either alone or in cooperation with other signaling pathways, NF-κB mediates a wide variety of transcriptional targets, which fall into several major categories such as cytokines and EMT factors. Ultimately, these targets mediate important aspects of CSC biology, including self-renewal, proliferation, and metastasis.
3.2. Connections between NF-κB Signaling, Cytokines, and CSCs
Signaling from toll-like receptors (TLRs) is known to drive traditional NF-κB activation in an inflammatory setting. In ovarian CSCs, TLR2-MyD88-driven NF-κB activity regulates expression of the stem cell associated genes CD44, Sox2 and Nanog [104]. TLR9 drives the propagation and self-renewal of androgen-independent prostate CSCs, largely through the co-activation of the NF-κB and STAT3 pathways, which in turn regulate expression of the crucial stem cell transcription factors NKX3.1 and KLF4 [105]. Numerous cytokines have also been associated with supporting CSC maintenance in an NF-κB-dependent manner. Chronic myeloid leukemia (CML) stem cells produce higher levels of TNFα than normal hematopoietic stem cells. Canonical NF-κB activation positively regulates expression of IL-3 and granulocyte/macrophage colony-stimulating factor common β-chain receptor (CSF2RB) to promote proliferation and survival of CML stem cells [106]. Similar findings in a mouse model of acute myeloid leukemia (AML) described a feedback loop between TNFα and NF-κB, confirmed by correlations in patient samples [107]. TNFα treatment of MCF7 breast cancer cells increased their mammosphere-forming capacity through upregulation of NF-κB and subsequently Slug (Figure 2) [108]. In colorectal cancer, levels of prostaglandin E2 (PGE2) correlated with CSC markers in human tumor samples. Treatment of either a genetic or xenograft mouse model with PGE2 led to CSC expansion through upregulation of several signaling pathways including NF-κB [109]. In glioblastoma, IL-17 receptor was found to be co-expressed with multiple CSC markers, including CD133, Nestin, and Sox2, as well as a source of NF-κB activation [110].
While several cytokines drive NF-κB signaling, NF-κB also controls the expression of a variety of other cytokines, particularly IL-6 and IL-8, which are heavily associated with CSC function. Iliopoulous and colleagues studied an inducible model of transformation by Src in mammary epithelial cells that led to rapid secretion of IL-6 and increased NF-κB activation. NF-κB positively regulates Lin28 transcription, which in turn decreases the level of let-7 microRNA. As IL-6 is one target of this microRNA, IL-6 expression increases even further, creating a positive feedback loop driving transformation and CSC expansion [111,112]. Interestingly, let-7 also targets KRas, and decreased levels of let-7 have been shown to drive mammosphere formation and size through Ras-NF-κB and Ras-MAPK-ERK pathways [113]. In basal-like breast cancer, NF-κB inhibition decreases mammosphere formation, but addition of exogenous IL-6 or IL-1β rescues the defect [93]. In CML, increased levels of IL-6 drive CML progenitors into the myeloid lineage, sustaining CML development [114]. IL-6, IL-8, and MCP1 similarly contribute to the survival and self-renewal of glioblastoma CSCs (Figure 2) [110,115].
3.3. Interactions between NF-κB and the Tumor Microenvironment
Given the close association between NF-κB and cytokines, it reasonably follows that NF-κB plays a role in modulating the microenvironment. CSCs are thought to occupy certain niches within tumors, much like their normal stem cell counterparts. For example in glioblastoma, CSCs have been localized to a perivascular niche, populated by an abundance of proliferating stromal and endothelial cells that support the growth of CSCs specifically [116,117]. As previously mentioned, preferential expression of IL-17 receptor is seen on glioblastoma CSCs. Relatedly, in ovarian cancer, macrophages and CD4+ T cells produce IL-17 to drive self-renewal of CSCs in vitro and tumor formation in vivo in an NF-κB- and p38-dependent manner [118]. Interestingly, there is evidence for CSCs promoting angiogenesis through secretion of endothelial factors like VEGF and IL-8 or through direct transdifferentiation [80,119,120,121]. Osteopontin is an oncoprotein that signals through integrins as well as CD44 family receptors, which have been used as a CSC marker in several tumor types. Hepatocellular carcinoma stem cells exhibit enhanced expression of osteopontin which drives a transcriptional cascade from NF-κB activation to HIF1α to BMI1 expression [122]. Periostin (POSTN) is a component of the extracellular matrix that has been identified in the niche of both normal and cancer stem cells. Generally thought to be produced by stromal fibroblasts, POSTN promotes metastasis to the lung in a breast cancer model by supporting the growth and expansion of CSCs [123]. Another group found that in vitro breast CSCs express higher levels of POSTN than their non-CSC counterparts. POSTN drives an ERK-NF-κB signaling axis, driving production of IL-6 and IL-8, which in turn contribute to CSC maintenance through STAT3 activation [124]. Breast cancer also exhibits a circuit of progestin-driven RANKL (receptor activator of NF-κB ligand) expression, leading to NF-κB activation. Deletion of the RANKL receptor RANK decreases the CD49fhi-CSC population and tumor incidence (Figure 2) [125].
3.4. Contributions by the NF-κB Pathway to Invasion and Metastasis
In addition to creating the proper niche for CSC survival and expansion, NF-κB also contributes to the invasive and metastatic capabilities of CSCs. This can occur through further modulation of the extracellular environment or through cell-intrinsic changes like epithelial-mesenchymal transition (EMT) which has been linked to CSC characteristics [126]. Work by several groups has shown NF-κB-mediated regulation of critical EMT factors including Snail [127,128], Slug [129,130], ZEB1/2 [131], and Twist1 [132,133,134,135,136] (reviewed in [137]). TNFα leads to NF-κB-dependent stabilization of Snail and transcriptional upregulation of Twist1, both of which enhanced invasion in vitro and metastasis in vivo [138,139]. Inhibition of NF-κB led to a reversal of EMT in mammary epithelial cells and decreased metastasis in an in vivo model [140]. In breast cancer, overexpression of RANK drives EMT and expansion of the CD44+/CD24− CSC population, ultimately leading to increased tumor growth and a substantially higher number of metastases [141]. Another study found overexpression of AXL in breast cancer stem cells; inhibition of AXL decreased NF-κB activity, expression of EMT-associated genes, invasion, and tumor formation [142]. In non-small cell lung cancer (NSCLC), Kumar and colleagues induced EMT through dual treatment with TNFα and TGF-β. The associated EMT transcription factors Twist1, Slug, and ZEB2 were upregulated in an NF-κB-dependent manner, followed by increases in multiple stem cell factors: KLF4, SOX2, POU5F1, MYCN, and KIT [130]. Subsequent studies found that NF-κB-mediated upregulation of Activin was required in order to maintain the mesenchymal phenotype of NSCLC CSCs [143]. There is also evidence that signaling through the NF-κB pathway and CXCR4 maintains stemness and promotes migration [144,145,146,147]. NF-κB has also been found to regulate the expression of matrix metalloproteinases (MMPs), which can degrade components of the extracellular matrix to increase invasion of tumor cells. Specifically, NF-κB directly regulates transcription of MMP9 [148,149,150], while indirectly increasing MMP2 activity [151,152,153]. Ovarian CSCs upregulate MMP9 expression to enable invasion and metastasis downstream of CCL5-NF-κB signaling [154]. NF-κB has also been shown to regulate VEGF and IL-8, which promote tumor formation and angiogenesis [155].
NF-κB frequently cooperates with additional signaling pathways to mediate these oncogenic effects. Coordinated activity between NF-κB and STAT3 has been previously mentioned in this review. Concurrent constitutive signaling from NF-κB and STAT3 in glioblastoma CSCs regulates expression of a set of genes (NOTCH1, HES5, JAG1, NUMBL, DTX3, DVL3, and RBPJ) that drive activation of Notch signaling, a third CSC-associated pathway (Figure 2) [92]. Another experiment, suggesting an important interaction between the CSCs and the bulk tumor cells, found that NF-κB activity in the non-CSCs upregulates JAG1 to stimulate Notch signaling in proximal breast CSCs [156].
The majority of the findings discussed here have focused on the canonical NF-κB pathway, particularly the p65 subunit. However, there is also evidence that the non-canonical pathway contributes to CSC phenotypes. In breast cancer, knockdown of IKKα, p100/p52, or RelB all produced a decrease in mammosphere formation [93]. Eva1, found to be overexpressed in glioblastoma CSCs, drives NIK stabilization and p100 processing, potentially by promoting ubiquitination and degradation of TRAF2 and cIAP [157]. RelB has been described as an oncogenic driver in mesenchymal glioma, regulating Olig2 expression and promoting tumor growth and invasion [39].
4. NF-κB as a Therapeutic Target
Given the extensive ties between NF-κB signaling and cancer biology, there has naturally been an interest in targeting the pathway therapeutically. In several of the studies previously mentioned, either knockdown of pathway components or targeted inhibitors produced a decrease in stem cell phenotypes in vitro as well as decreased tumor growth and/or metastasis in vivo. A combination of idarubicin and MG132, a proteasome inhibitor, induced cell death in AML stem cells, partially through NF-κB inhibition [158]. While proteasome inhibition will impact several pathways in a cell, NF-κB inhibition is a well-established effect of MG132 treatment as it blocks IκBα degradation, reducing NF-κB nuclear localization and DNA binding. The same group went on to identify the compound parthenolide as selectively inducing apoptosis in leukemia stem cells as opposed to normal hematopoietic stem cells, through a mechanism of increased reactive oxygen species, p53 activation, and NF-κB inhibition [159]. A subsequent in silico screen for additional drugs with specificity towards AML stem cells identified two other compounds, celastrol and 4-hydroxy-2-nonenal, and once again they found NF-κB inhibition to be part of the mechanism of action [160]. Parthenolide has also shown preferential activity in breast CSCs compared to the bulk tumor cells [161]. Use of SN50, a peptide inhibitor that blocks nuclear import of NF-κB and other transcription factors, decreases the sphere formation ability and tumorigenic capacity of glioma CSCs [162]. Others have found that inhibition of NF-κB promotes more rapid differentiation and progression to senescence in glioblastoma CSCs [163].
The activated B-cell subset of diffuse large B-cell lymphoma (DLBCL) has shown a distinct dependence on NF-κB signaling. Standard treatment for lymphoma patients includes rituximab, a monoclonal antibody against CD20. While this drug has many effects, one aspect includes inhibition of NF-κB signaling to induce apoptosis [164]. More recently, ibrutinib, a BTK inhibitor, has been found to improve patient outcome in clinical trials. While this drug does not specifically target IKK, BTK represents a key intermediate between B cell receptor and NF-κB, and ibrutinib treatment decreases NF-κB signaling [165]. Previously discussed studies have found an impact of IKK/NF-κB inhibition on tumor growth. While these efforts didn’t specifically analyze CSC effects, if CSCs are primarily driving tumor initiation, we could interpret these results as having some effect on the CSC population. Direct IKKβ inhibitors showed efficacy in a mutant KRas, p53-null model of lung cancer [166,167]. In addition to inhibitors targeting the kinase activity, the NF-κB pathway can be inhibited by peptides encompassing the NEMO-binding domain (NBD) that block association of the IKK catalytic subunits with NEMO/IKKγ. Recently, use of an NBD peptide slowed tumor growth in both a human glioma xenograft and a genetic mouse model of glioma [168]. The NBD peptide has also shown efficacy in a canine model of DLBCL [169,170].
NF-κB signaling also has ties to mediating resistance to radiation and chemotherapy, so there could be utility in combining NF-κB inhibition with traditional cancer therapies. Early work found that expression of IκBα-SR sensitized cancer cells to ionizing radiation, daunorubicin, and CPT-11 (a topoisomerase inhibitor) [171,172,173]. More recently, use of NF-κB inhibitors in combination with temozolomide, adriamycin, or radiation has shown increased apoptosis in glioblastoma cells [174,175,176]. Doxorubicin-resistant glioblastoma stem cells upregulated expression of MDR1 through a PI3K-NF-κB pathway [177]. In another study, KRas-NF-κB signaling mediated resistance to EGFR inhibitors in CSCs [178]. Upregulation of IRAK1 drives NF-κB activation and cytokine production, leading to CSC enrichment and paclitaxel resistance in breast cancer [179]. Taken together, these results suggest that not only could NF-κB inhibition be an effective treatment against CSCs, but it could also restore sensitivity to other therapeutic options.
5. Conclusions
The NF-κB pathway is integrated into many critical aspects of tumor biology. Its function in inflammation and immune responses often sets the stage for tumor development. Expression of several potent oncoproteins, including mutant RAS and BCR-ABL, leads to NF-κB activation early in tumorigenesis. Here, we have detailed crucial roles and contributions of NF-κB in cancer stem cells, which are driving tumor initiation, recurrence, and metastasis. NF-κB regulation of critical target genes—prominently including IAPs, cytokines, and EMT transcription factors—drive CSC phenotypes. In addition to direct NF-κB effects, there is also cooperation between other crucial CSC-associated pathways, such as STAT3, Notch, and TGF-β. Future work will need to determine if therapeutic targeting of the NF-κB pathway impacts tumor growth at the level of the cancer stem cells.
Acknowledgments
The authors wish to thank members of the Baldwin lab for their discussion and feedback on this review. The authors’ work is funded by NCI grant R35CA197684.
Abbreviations
The following abbreviations are used in this manuscript:
- AML
acute myeloid leukemia
- APC
adenomatous polyposis coli
- CML
chronic myeloid leukemia
- CSC
cancer stem cells
- DEN
diethylnitrosamine
- DLBCL
diffuse large B cell lymphoma
- ECM
extracellular matrix
- EGFR
epidermal growth factor receptor
- EMT
epithelial-mesenchymal transition
- HSC
hematopoietic stem cell
- IκBα
nuclear factor of κ light polypeptide gene enhancer in B-Cells inhibitor, α
- IKK
inhibitor of κB kinase
- LPS
lipopolysaccharide
- NBD
NEMO binding domain
- NF-κB
nuclear factor of κ light polypeptide gene enhancer in B-Cells
- NIK
NF-κB-inducing kinase
- POSTN
periostin
- RANK
receptor activator of NF-κB
- ROS
reactive oxygen species
- STAT
signal transducer and activator of transcription
- TLR
toll-like receptor
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Hayden M.S., Ghosh S. Shared Principles in NF-κB Signaling. Cell. 2008;132:344–362. doi: 10.1016/j.cell.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 2.Johnson C., Van Antwerp D., Hope T.J. An N-terminal nuclear export signal is required for the nucleocytoplasmic shuttling of IκBα. EMBO J. 1999;18:6682–6693. doi: 10.1093/emboj/18.23.6682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang T.T., Kudo N., Yoshida M., Miyamoto S. A nuclear export signal in the N-terminal regulatory domain of IκBα controls cytoplasmic localization of inactive NF-κB/IκBα complexes. Proc. Natl. Acad. Sci. USA. 2000;97:1014–1019. doi: 10.1073/pnas.97.3.1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carlotti F., Dower S.K., Qwarnstrom E.E. Dynamic Shuttling of Nuclear Factor-κB between the Nucleus and Cytoplasm as a Consequence of Inhibitor Dissociation. J. Biol. Chem. 2000;275:41028–41034. doi: 10.1074/jbc.M006179200. [DOI] [PubMed] [Google Scholar]
- 5.Birbach A., Gold P., Binder B.R., Hofer E., De Martin R., Schmid J.A. Signaling Molecules of the NF-κB Pathway Shuttle Constitutively between Cytoplasm and Nucleus. J. Biol. Chem. 2002;277:10842–10851. doi: 10.1074/jbc.M112475200. [DOI] [PubMed] [Google Scholar]
- 6.Ghosh S., Hayden M.S. Celebrating 25 years of NF-κB research. Immunol. Rev. 2012;246:5–13. doi: 10.1111/j.1600-065X.2012.01111.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bradford J.W., Baldwin A.S. IKK/Nuclear Factor-κB and Oncogenesis. Adv. Cancer Res. 2014;121:125–145. doi: 10.1016/B978-0-12-800249-0.00003-2. [DOI] [PubMed] [Google Scholar]
- 8.Weih F., Carrasco D., Durham S.K., Barton D.S., Rizzo C.A., Ryseck R.P., Lira S.A., Bravo R. Multiorgan inflammation and hematopoietic abnormalities in mice with a targeted disruption of RelB, a member of the NF-κ B/Rel family. Cell. 1995;80:331–340. doi: 10.1016/0092-8674(95)90416-6. [DOI] [PubMed] [Google Scholar]
- 9.Grossmann M., Metcalf D., Merryfull J., Beg A., Baltimore D., Gerondakis S. The combined absence of the transcription factors Rel and RelA leads to multiple hemopoietic cell defects. Proc. Natl. Acad. Sci. USA. 1999;96:11848–11853. doi: 10.1073/pnas.96.21.11848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stein S.J., Baldwin A.S. Deletion of the NF-kappaB subunit p65/RelA in the hematopoietic compartment leads to defects in hematopoietic stem cell function. Blood. 2013;121:5015–5024. doi: 10.1182/blood-2013-02-486142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhao C., Xiu Y., Ashton J., Xing L., Morita Y., Jordan C.T., Boyce B.F. Noncanonical NF-κB Signaling Regulates Hematopoietic Stem Cell Self-Renewal and Microenvironment Interactions. Stem Cells. 2012;30:709–718. doi: 10.1002/stem.1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhao J.L., Rao D.S., O’Connell R.M., Garcia-Flores Y., Baltimore D. MicroRNA-146a acts as a guardian of the quality and longevity of hematopoietic stem cells in mice. Elife. 2013;2:e00537. doi: 10.7554/eLife.00537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhao J.L., Ma C., O’Connell R.M., Mehta A., DiLoreto R., Heath J.R., Baltimore D. Conversion of Danger Signals into Cytokine Signals by Hematopoietic Stem and Progenitor Cells for Regulation of Stress-Induced Hematopoiesis. Cell Stem Cell. 2014;14:445–459. doi: 10.1016/j.stem.2014.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Armstrong L., Hughes O., Yung S., Hyslop L., Stewart R., Wappler I., Peters H., Walter T., Stojkovic P., Evans J., et al. The role of PI3K/AKT, MAPK/ERK and NFκB signalling in the maintenance of human embryonic stem cell pluripotency and viability highlighted by transcriptional profiling and functional analysis. Hum. Mol. Genet. 2006;15:1894–1913. doi: 10.1093/hmg/ddl112. [DOI] [PubMed] [Google Scholar]
- 15.Deng P., Zhou C., Alvarez R., Hong C., Wang C.-Y. Inhibition of IKK/NF-κB Signaling Enhances Differentiation of Mesenchymal Stromal Cells from Human Embryonic Stem Cells. Stem Cell Rep. 2016 doi: 10.1016/j.stemcr.2016.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lüningschrör P., Stöcker B., Kaltschmidt B., Kaltschmidt C. miR-290 Cluster Modulates Pluripotency by Repressing Canonical NF-κB Signaling. Stem Cells. 2012;30:655–664. doi: 10.1002/stem.1033. [DOI] [PubMed] [Google Scholar]
- 17.Guttridge D.C., Albanese C., Reuther J.Y., Pestell R.G., Baldwin A.S. NF-κB controls cell growth and differentiation through transcriptional regulation of cyclin D1. Mol. Cell. Biol. 1999;19:5785–5799. doi: 10.1128/MCB.19.8.5785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Canicio J., Ruiz-Lozano P., Carrasco M., Palacin M., Chien K., Zorzano A., Kaliman P. Nuclear factor κB-inducing kinase and IκB kinase-α signal skeletal muscle cell differentiation. J. Biol. Chem. 2001;276:20228–20233. doi: 10.1074/jbc.M100718200. [DOI] [PubMed] [Google Scholar]
- 19.Bakkar N., Wang J., Ladner K.J., Wang H., Dahlman J.M., Carathers M., Acharyya S., Rudnicki M.A., Hollenbach A.D., Guttridge D.C. IKK/NF-κB regulates skeletal myogenesis via a signaling switch to inhibit differentiation and promote mitochondrial biogenesis. J. Cell Biol. 2008;180:787–802. doi: 10.1083/jcb.200707179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wilhelmsen K.C., Eggleton K., Temin H.M. Nucleic acid sequences of the oncogene v-rel in reticuloendotheliosis virus strain T and its cellular homolog, the proto-oncogene c-rel. J. Virol. 1984;52:172–182. doi: 10.1128/jvi.52.1.172-182.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kieran M., Blank V., Logeat F., Vandekerckhove J., Lottspeich F., Le Bail O., Urban M.B., Kourilsky P., Baeuerle P.A., Israel A. The DNA binding subunit of NF-κB is identical to factor KBF1 and homologous to the rel oncogene product. Cell. 1990;62:1007–1018. doi: 10.1016/0092-8674(90)90275-J. [DOI] [PubMed] [Google Scholar]
- 22.Finco T.S., Westwick J.K., Norris J.L., Beg A.A., Der C.J., Baldwin A.S. Oncogenic Ha-Ras-induced signaling activates NF-κB transcriptional activity, which is required for cellular transformation. J. Biol. Chem. 1997;272:24113–24116. doi: 10.1074/jbc.272.39.24113. [DOI] [PubMed] [Google Scholar]
- 23.Reuther J.Y., Reuther G.W., Cortez D., Pendergast A.M., Baldwin A.S. A requirement for NF-κB activation in Bcr-Abl-mediated transformation. Genes Dev. 1998;12:968–981. doi: 10.1101/gad.12.7.968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stein S.J., Baldwin A.S. NF-κB suppresses ROS levels in BCR-ABL(+) cells to prevent activation of JNK and cell death. Oncogene. 2011;45:4557–4566. doi: 10.1038/onc.2011.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mayo M.W., Wang C.Y., Cogswell P.C., Rogers-Graham K.S., Lowe S.W., Der C.J., Baldwin A.S. Requirement of NF-κB activation to suppress p53-independent apoptosis induced by oncogenic Ras. Science. 1997;278:1812–1815. doi: 10.1126/science.278.5344.1812. [DOI] [PubMed] [Google Scholar]
- 26.Weisz L., Damalas A., Liontos M., Karakaidos P., Fontemaggi G., Maor-Aloni R., Kalis M., Levrero M., Strano S., Gorgoulis V.G., et al. Mutant p53 Enhances Nuclear Factor-κB Activation by Tumor Necrosis Factor α in Cancer Cells. Cancer Res. 2007;67:2396–2401. doi: 10.1158/0008-5472.CAN-06-2425. [DOI] [PubMed] [Google Scholar]
- 27.Cooks T., Pateras I.S., Tarcic O., Solomon H., Schetter A.J., Wilder S., Lozano G., Pikarsky E., Forshew T., Rozenfeld N., et al. Mutant p53 Prolongs NF-κB Activation and Promotes Chronic Inflammation and Inflammation-Associated Colorectal Cancer. Cancer Cell. 2013;23:634–646. doi: 10.1016/j.ccr.2013.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Di Minin G., Bellazzo A., Dal Ferro M., Chiaruttini G., Nuzzo S., Bicciato S., Piazza S., Rami D., Bulla R., Sommaggio R., et al. Mutant p53 Reprograms TNF Signaling in Cancer Cells through Interaction with the Tumor Suppressor DAB2IP. Mol. Cell. 2014;56:617–629. doi: 10.1016/j.molcel.2014.10.013. [DOI] [PubMed] [Google Scholar]
- 29.Qi H., Ohh M. The von Hippel-Lindau tumor suppressor protein sensitizes renal cell carcinoma cells to tumor necrosis factor-induced cytotoxicity by suppressing the nuclear factor-κB-dependent antiapoptotic pathway. Cancer Res. 2003;63:7076–7080. [PubMed] [Google Scholar]
- 30.An J., Fisher M., Rettig M.B. VHL expression in renal cell carcinoma sensitizes to bortezomib (PS-341) through an NF-κB-dependent mechanism. Oncogene. 2004;24:1563–1570. doi: 10.1038/sj.onc.1208348. [DOI] [PubMed] [Google Scholar]
- 31.An J., Rettig M.B. Mechanism of von Hippel-Lindau Protein-Mediated Suppression of Nuclear Factor κB Activity. Mol. Cell. Biol. 2005;25:7546–7556. doi: 10.1128/MCB.25.17.7546-7556.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gustin J.A., Maehama T., Dixon J.E., Donner D.B. The PTEN Tumor Suppressor Protein Inhibits Tumor Necrosis Factor-induced Nuclear Factor-κB Activity. J. Biol. Chem. 2001;276:27740–27744. doi: 10.1074/jbc.M102559200. [DOI] [PubMed] [Google Scholar]
- 33.Asano T., Yao Y., Zhu J., Li D., Abbruzzese J.L., Reddy S.A.G. The PI 3-kinase/Akt signaling pathway is activated due to aberrant Pten expression and targets transcription factors NF-κB and c-Myc in pancreatic cancer cells. Oncogene. 2004;23:8571–8580. doi: 10.1038/sj.onc.1207902. [DOI] [PubMed] [Google Scholar]
- 34.Ying H., Elpek K.G., Vinjamoori A., Zimmerman S.M., Chu G.C., Yan H., Fletcher-Sananikone E., Zhang H., Liu Y., Wang W., et al. PTEN Is a Major Tumor Suppressor in Pancreatic Ductal Adenocarcinoma and Regulates an NF-κB-Cytokine Network. Cancer Discov. 2011;1:158–169. doi: 10.1158/2159-8290.CD-11-0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang X., Belguise K., Kersual N., Kirsch K.H., Mineva N.D., Galtier F., Chalbos D., Sonenshein G.E. Oestrogen signalling inhibits invasive phenotype by repressing RelB and its target BCL2. Nat. Cell Biol. 2007;9:470–478. doi: 10.1038/ncb1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xu Y., Josson S., Fang F., Oberley T.D., St Clair D.K., Wan X.S., Sun Y., Bakthavatchalu V., Muthuswamy A., St Clair W.H. RelB Enhances Prostate Cancer Growth: Implications for the Role of the Nuclear Factor-kappaB Alternative Pathway in Tumorigenicity. Cancer Res. 2009;69:3267–3271. doi: 10.1158/0008-5472.CAN-08-4635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wharry C.E., Haines K.M., Carroll R.G., May M.J. Constitutive noncanonical NFκB signaling in pancreatic cancer cells. Cancer Biol. Ther. 2014;8:1567–1576. doi: 10.4161/cbt.8.16.8961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thu Y.M., Su Y., Yang J., Splittgerber R., Na S., Boyd A., Mosse C., Simons C., Richmond A. NF-κB inducing kinase (NIK) modulates melanoma tumorigenesis by regulating expression of pro-survival factors through the β-catenin pathway. Oncogene. 2011;31:2580–2592. doi: 10.1038/onc.2011.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee D.W., Ramakrishnan D., Valenta J., Parney I.F., Bayless K.J., Sitcheran R. The NF-κB RelB Protein Is an Oncogenic Driver of Mesenchymal Glioma. PLoS ONE. 2013;8:16. doi: 10.1371/journal.pone.0057489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Uno M., Saitoh Y., Mochida K., Tsuruyama E., Kiyono T., Imoto I., Inazawa J., Yuasa Y., Kubota T., Yamaoka S. NF-κB Inducing Kinase, a Central Signaling Component of the Non-Canonical Pathway of NF-κB, Contributes to Ovarian Cancer Progression. PLoS ONE. 2014;9:16. doi: 10.1371/journal.pone.0088347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Li Y., Zhou Q.-L., Sun W., Chandrasekharan P., Cheng H.S., Ying Z., Lakshmanan M., Raju A., Tenen D.G., Cheng S.-Y., et al. Non-canonical NF-κB signalling and ETS1/2 cooperatively drive C250T mutant TERT promoter activation. Nat. Cell Biol. 2015;17:1327–1338. doi: 10.1038/ncb3240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Meylan E., Dooley A.L., Feldser D.M., Shen L., Turk E., Ouyang C., Jacks T. Requirement for NF-κB signalling in a mouse model of lung adenocarcinoma. Nature. 2009;461:104–107. doi: 10.1038/nature08462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bassères D.S., Ebbs A., Levantini E., Baldwin A.S. Requirement of the NF-κB subunit p65/RelA for K-Ras-induced lung tumorigenesis. Cancer Res. 2010;70:3537–3546. doi: 10.1158/0008-5472.CAN-09-4290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yang J., Splittgerber R., Yull F.E., Kantrow S., Ayers G.D., Karin M., Richmond A. Conditional ablation of Ikkb inhibits melanoma tumor development in mice. J. Clin. Invest. 2010;120:2563–2574. doi: 10.1172/JCI42358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hanahan D., Weinberg R.A. Hallmarks of Cancer: The Next Generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 46.Baldwin A.S. Regulation of cell death and autophagy by IKK and NF-κB: Critical mechanisms in immune function and cancer. Immunol. Rev. 2012;246:327–345. doi: 10.1111/j.1600-065X.2012.01095.x. [DOI] [PubMed] [Google Scholar]
- 47.Chu Z.L., McKinsey T.A., Liu L., Gentry J.J., Malim M.H., Ballard D.W. Suppression of tumor necrosis factor-induced cell death by inhibitor of apoptosis c-IAP2 is under NF-κB control. Proc. Natl. Acad. Sci. USA. 1997;94:10057–10062. doi: 10.1073/pnas.94.19.10057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang C.Y., Mayo M.W., Korneluk R.G., Goeddel D.V., Baldwin A.S. NF-κB antiapoptosis: Induction of TRAF1 and TRAF2 and c-IAP1 and c-IAP2 to suppress caspase-8 activation. Science. 1998;281:1680–1683. doi: 10.1126/science.281.5383.1680. [DOI] [PubMed] [Google Scholar]
- 49.Ramakrishnan P., Kahn D.A., Baltimore D. Anti-apoptotic effect of hyperglycemia can allow survival of potentially autoreactive T cells. Cell Death Differ. 2010;18:690–699. doi: 10.1038/cdd.2010.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bassères D.S., Baldwin A.S. Nuclear factor-κB and inhibitor of κB kinase pathways in oncogenic initiation and progression. Oncogene. 2006;25:6817–6830. doi: 10.1038/sj.onc.1209942. [DOI] [PubMed] [Google Scholar]
- 51.Beroukhim R., Mermel C.H., Porter D., Wei G., Raychaudhuri S., Donovan J., Barretina J., Boehm J.S., Dobson J., Urashima M., et al. The landscape of somatic copy-number alteration across human cancers. Nature. 2010;463:899–905. doi: 10.1038/nature08822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Boehm J.S., Zhao J.J., Yao J., Kim S.Y., Firestein R., Dunn I.F., Sjostrom S.K., Garraway L.A., Weremowicz S., Richardson A.L., et al. Integrative Genomic Approaches Identify IKBKE as a Breast Cancer Oncogene. Cell. 2007;129:1065–1079. doi: 10.1016/j.cell.2007.03.052. [DOI] [PubMed] [Google Scholar]
- 53.Orlowski R.Z., Baldwin A.S. NF-κB as a therapeutic target in cancer. Trends Mol. Med. 2002;8:385–389. doi: 10.1016/S1471-4914(02)02375-4. [DOI] [PubMed] [Google Scholar]
- 54.Neri A., Chang C.C., Lombardi L., Salina M., Corradini P., Maiolo A.T., Chaganti R.S., Dalla-Favera R. B cell lymphoma-associated chromosomal translocation involves candidate oncogene lyt-10, homologous to NF-κB p50. Cell. 1991;67:1075–1087. doi: 10.1016/0092-8674(91)90285-7. [DOI] [PubMed] [Google Scholar]
- 55.Parker M., Mohankumar K.M., Punchihewa C., Weinlich R., Dalton J.D., Li Y., Lee R., Tatevossian R.G., Phoenix T.N., Thiruvenkatam R., et al. C11orf95–RELA fusions drive oncogenic NF-κB signalling in ependymoma. Nature. 2014;506:451–455. doi: 10.1038/nature13109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bredel M., Scholtens D.M., Yadav A.K., Alvarez A.A., Renfrow J.J., Chandler J.P., Yu I.L.Y., Carro M.S., Dai F., Tagge M.J., et al. NFKBIA Deletion in Glioblastomas. N. Engl. J. Med. 2011;364:627–637. doi: 10.1056/NEJMoa1006312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lim K.-H., Yang Y., Staudt L.M. Pathogenetic importance and therapeutic implications of NF-κB in lymphoid malignancies. Immunol. Rev. 2012;246:359–378. doi: 10.1111/j.1600-065X.2012.01105.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Merkhofer E.C., Cogswell P., Baldwin A.S. Her2 activates NF-κB and induces invasion through the canonical pathway involving IKKα. Oncogene. 2010;29:1238–1248. doi: 10.1038/onc.2009.410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tanaka K., Babic I., Nathanson D., Akhavan D., Guo D., Gini B., Dang J., Zhu S., Yang H., De Jesus J., et al. Oncogenic EGFR Signaling Activates an mTORC2-NF-κB Pathway That Promotes Chemotherapy Resistance. Cancer Discov. 2011;1:524–538. doi: 10.1158/2159-8290.CD-11-0124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dan H.C., Adli M., Baldwin A.S. Regulation of Mammalian Target of Rapamycin Activity in PTEN-Inactive Prostate Cancer Cells by IκB Kinase α. Cancer Res. 2007;67:6263–6269. doi: 10.1158/0008-5472.CAN-07-1232. [DOI] [PubMed] [Google Scholar]
- 61.Dan H.C., Cooper M.J., Cogswell P.C., Duncan J.A., Ting J.P.Y., Baldwin A.S. Akt-dependent regulation of NF-κB is controlled by mTOR and Raptor in association with IKK. Genes Dev. 2008;22:1490–1500. doi: 10.1101/gad.1662308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Xu Y., Lai E., Liu J., Lin J., Yang C., Jia C., Li Y., Bai X., Li M. IKK interacts with rictor and regulates mTORC2. Cell. Signal. 2013;25:2239–2245. doi: 10.1016/j.cellsig.2013.07.008. [DOI] [PubMed] [Google Scholar]
- 63.Dan H.C., Ebbs A., Pasparakis M., Van Dyke T., Bassères D.S., Baldwin A.S. Akt-dependent Activation of mTORC1 Complex Involves Phosphorylation of mTOR (Mammalian Target of Rapamycin) by IκB Kinase α (IKKα) J. Biol. Chem. 2014;289:25227–25240. doi: 10.1074/jbc.M114.554881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhang W., Tan W., Wu X., Poustovoitov M., Strasner A., Li W., Borcherding N., Ghassemian M., Karin M. A NIK-IKKα Module Expands ErbB2-Induced Tumor-Initiating Cells by Stimulating Nuclear Export of p27/Kip1. Cancer Cell. 2013;23:647–659. doi: 10.1016/j.ccr.2013.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Xia Y., Padre R.C., De Mendoza T.H., Bottero V., Tergaonkar V.B., Verma I.M. Phosphorylation of p53 by IκB kinase 2 promotes its degradation by beta-TrCP. Proc. Natl. Acad. Sci. USA. 2009;106:2629–2634. doi: 10.1073/pnas.0812256106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Greten F.R., Eckmann L., Greten T.F., Park J.M., Li Z.-W., Egan L.J., Kagnoff M.F., Karin M. IKKβ Links Inflammation and Tumorigenesis in a Mouse Model of Colitis-Associated Cancer. Cell. 2004;118:285–296. doi: 10.1016/j.cell.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 67.Maeda S., Kamata H., Luo J.-L., Leffert H., Karin M. IKKβ Couples Hepatocyte Death to Cytokine-Driven Compensatory Proliferation that Promotes Chemical Hepatocarcinogenesis. Cell. 2005;121:977–990. doi: 10.1016/j.cell.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 68.Sakurai T., Maeda S., Chang L., Karin M. Loss of hepatic NF-κB activity enhances chemical hepatocarcinogenesis through sustained c-Jun N-terminal kinase 1 activation. Proc. Natl. Acad. Sci. USA. 2006;103:10544–10551. doi: 10.1073/pnas.0603499103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.DiDonato J.A., Mercurio F., Karin M. NF-κB and the link between inflammation and cancer. Immunol. Rev. 2012;246:379–400. doi: 10.1111/j.1600-065X.2012.01099.x. [DOI] [PubMed] [Google Scholar]
- 70.Erez N., Truitt M., Olson P., Hanahan D. Cancer-Associated Fibroblasts Are Activated in Incipient Neoplasia to Orchestrate Tumor-Promoting Inflammation in an NF-κB-Dependent Manner. Cancer Cell. 2010;17:135–147. doi: 10.1016/j.ccr.2009.12.041. [DOI] [PubMed] [Google Scholar]
- 71.Koliaraki V., Pasparakis M., Kollias G. IKKbeta in intestinal mesenchymal cells promotes initiation of colitis-associated cancer. J. Exp. Med. 2015;205:331. doi: 10.1084/jem.20150542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Pallangyo C.K., Ziegler P.K., Greten F.R. IKKbeta acts as a tumor suppressor in cancer-associated fibroblasts during intestinal tumorigenesis. J. Exp. Med. 2015;223:162. doi: 10.1084/jem.20150576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Saccani A., Schioppa T., Porta C., Biswas S.K., Nebuloni M., Vago L., Bottazzi B., Colombo M.P., Mantovani A., Sica A. p50 Nuclear Factor-κB Overexpression in Tumor-Associated Macrophages Inhibits M1 Inflammatory Responses and Antitumor Resistance. Cancer Res. 2006;66:11432–11440. doi: 10.1158/0008-5472.CAN-06-1867. [DOI] [PubMed] [Google Scholar]
- 74.Hagemann T., Lawrence T., McNeish I., Charles K.A., Kulbe H., Thompson R.G., Robinson S.C., Balkwill F.R. “Re-educating” tumor-associated macrophages by targeting NF-κB. J. Exp. Med. 2008;205:1261–1268. doi: 10.1084/jem.20080108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bonnet D., Dick J.E. Human acute myeloid leukemia is organized as a hierarchy that originates from a primitive hematopoietic cell. Nat. Med. 1997;3:730–737. doi: 10.1038/nm0797-730. [DOI] [PubMed] [Google Scholar]
- 76.Singh S.K., Clarke I.D., Terasaki M., Bonn V.E., Hawkins C., Squire J., Dirks P.B. Identification of a cancer stem cell in human brain tumors. Cancer Res. 2003;63:5821–5828. [PubMed] [Google Scholar]
- 77.Singh S.K., Hawkins C., Clarke I.D., Squire J.A., Bayani J., Hide T., Henkelman R.M., Cusimano M.D., Dirks P.B. Identification of human brain tumour initiating cells. Nature. 2004;432:396–401. doi: 10.1038/nature03128. [DOI] [PubMed] [Google Scholar]
- 78.Al-Hajj M., Wicha M.S., Benito-Hernandez A., Morrison S.J., Clarke M.F. Prospective identification of tumorigenic breast cancer cells. Proc. Natl. Acad. Sci. USA. 2003;100:3983–3988. doi: 10.1073/pnas.0530291100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Collins A.T. Prospective Identification of Tumorigenic Prostate Cancer Stem Cells. Cancer Res. 2005;65:10946–10951. doi: 10.1158/0008-5472.CAN-05-2018. [DOI] [PubMed] [Google Scholar]
- 80.Ricci-Vitiani L., Lombardi D.G., Pilozzi E., Biffoni M., Todaro M., Peschle C., De Maria R. Identification and expansion of human colon-cancer-initiating cells. Nature. 2006;445:111–115. doi: 10.1038/nature05384. [DOI] [PubMed] [Google Scholar]
- 81.Li C., Heidt D.G., Dalerba P., Burant C.F., Zhang L., Adsay V., Wicha M., Clarke M.F., Simeone D.M. Identification of Pancreatic Cancer Stem Cells. Cancer Res. 2007;67:1030–1037. doi: 10.1158/0008-5472.CAN-06-2030. [DOI] [PubMed] [Google Scholar]
- 82.Reya T., Morrison S.J., Clarke M.F., Weissman I.L. Stem cells, cancer, and cancer stem cells. Nature. 2001;414:105–111. doi: 10.1038/35102167. [DOI] [PubMed] [Google Scholar]
- 83.Chen R., Nishimura M.C., Bumbaca S.M., Kharbanda S., Forrest W.F., Kasman I.M., Greve J.M., Soriano R.H., Gilmour L.L., Rivers C.S., et al. A Hierarchy of Self-Renewing Tumor-Initiating Cell Types in Glioblastoma. Cancer Cell. 2010;17:362–375. doi: 10.1016/j.ccr.2009.12.049. [DOI] [PubMed] [Google Scholar]
- 84.Bruce W.R., van der Gaag H. A Quantitative Assay for the Number of Murine Lymphoma Cells Capable of Proliferation in vivo. Nature. 1963;199:79–80. doi: 10.1038/199079a0. [DOI] [PubMed] [Google Scholar]
- 85.Reynolds B.A., Weiss S. Generation of neurons and astrocytes from isolated cells of the adult mammalian central nervous system. Science. 1992;255:1707–1710. doi: 10.1126/science.1553558. [DOI] [PubMed] [Google Scholar]
- 86.Hemmati H.D., Nakano I., Lazareff J.A., Masterman-Smith M., Geschwind D.H., Bronner-Fraser M., Kornblum H.I. Cancerous stem cells can arise from pediatric brain tumors. Proc. Natl. Acad. Sci. USA. 2003;100:15178–15183. doi: 10.1073/pnas.2036535100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Nguyen L.V., Vanner R., Dirks P., Eaves C.J. Cancer stem cells: An evolving concept. Nat. Rev. Cancer. 2012;12:133–143. doi: 10.1038/nrc3184. [DOI] [PubMed] [Google Scholar]
- 88.Dalerba P., Dylla S.J., Park I.-K., Liu R., Wang X., Cho R.W., Hoey T., Gurney A., Huang E.H., Simeone D.M. Phenotypic characterization of human colorectal cancer stem cells. Proc. Natl. Acad. Sci. USA. 2007;104:10158–10163. doi: 10.1073/pnas.0703478104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Sales K.M., Winslet M.C., Seifalian A.M. Stem Cells and Cancer: An Overview. Stem Cell Rev. 2007;3:249–255. doi: 10.1007/s12015-007-9002-0. [DOI] [PubMed] [Google Scholar]
- 90.Guzman M.L., Neering S.J., Upchurch D., Grimes B., Howard D.S., Rizzieri D.A., Luger S.M., Jordan C.T. Nuclear factor-κB is constitutively activated in primitive human acute myelogenous leukemia cells. Blood. 2001;98:2301–2307. doi: 10.1182/blood.V98.8.2301. [DOI] [PubMed] [Google Scholar]
- 91.Rajasekhar V.K., Studer L., Gerald W., Socci N.D., Scher H.I. Tumour-initiating stem-like cells in human prostate cancer exhibit increased NF-κB signalling. Nat. Commun. 2011;2:162. doi: 10.1038/ncomms1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Garner J.M., Fan M., Yang C.H., Du Z., Sims M., Davidoff A.M., Pfeffer L.M. Constitutive Activation of Signal Transducer and Activator of Transcription 3 (STAT3) and Nuclear Factor-κB Signaling in Glioblastoma Cancer Stem Cells Regulates the Notch Pathway. J. Biol. Chem. 2013;288:26167–26176. doi: 10.1074/jbc.M113.477950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Song L., Liu L., Wu Z., Li Y., Ying Z., Lin C., Wu J., Hu B., Cheng S.-Y., Li M., Li J. TGF-β induces miR-182 to sustain NF-κB activation in glioma subsets. J. Clin. Invest. 2012;122:3563–3578. doi: 10.1172/JCI62339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Tafani M., Di Vito M., Frati A., Pellegrini L., De Santis E., Sette G., Eramo A., Sale P., Mari E., Santoro A., et al. Pro-inflammatory gene expression in solid glioblastoma microenvironment and in hypoxic stem cells from human glioblastoma. J. Neuroinflamm. 2011;8:32. doi: 10.1186/1742-2094-8-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Murohashi M., Hinohara K., Kuroda M., Isagawa T., Tsuji S., Kobayashi S., Umezawa K., Tojo A., Aburatani H., Gotoh N. Gene set enrichment analysis provides insight into novel signalling pathways in breast cancer stem cells. Br. J. Cancer. 2009;102:206–212. doi: 10.1038/sj.bjc.6605468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Liu R., Wang X., Chen G.Y., Dalerba P., Gurney A., Hoey T., Sherlock G., Lewicki J., Shedden K., Clarke M.F. The prognostic role of a gene signature from tumorigenic breast-cancer cells. N. Engl. J. Med. 2007;356:217–226. doi: 10.1056/NEJMoa063994. [DOI] [PubMed] [Google Scholar]
- 97.Birnie R., Bryce S.D., Roome C., Dussupt V., Droop A., Lang S.H., Berry P.A., Hyde C.F., Lewis J.L., Stower M.J., et al. Gene expression profiling of human prostate cancer stem cells reveals a pro-inflammatory phenotype and the importance of extracellular matrix interactions. Genome Biol. 2008;9:R83. doi: 10.1186/gb-2008-9-5-r83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Leizer A.L., Alvero A.B., Fu H.H., Holmberg J.C., Cheng Y.-C., Silasi D.-A., Rutherford T., Mor G. Regulation of Inflammation by the NF-κB Pathway in Ovarian Cancer Stem Cells. Am. J. Reprod. Immunol. 2010;65:438–447. doi: 10.1111/j.1600-0897.2010.00914.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Korkaya H., Liu S., Wicha M.S. Regulation of Cancer Stem Cells by Cytokine Networks: Attacking Cancer’s Inflammatory Roots. Clin. Can. Res. 2011;17:6125–6129. doi: 10.1158/1078-0432.CCR-10-2743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Pratt M.A.C., Tibbo E., Robertson S.J., Jansson D., Hurst K., Perez-Iratxeta C., Lau R., Niu M.Y. The canonical NF-κB pathway is required for formation of luminal mammary neoplasias and is activated in the mammary progenitor population. Oncogene. 2009;28:2710–2722. doi: 10.1038/onc.2009.131. [DOI] [PubMed] [Google Scholar]
- 101.Liu M., Sakamaki T., Casimiro M.C., Willmarth N.E., Quong A.A., Ju X., Ojeifo J., Jiao X., Yeow W.-S., Katiyar S., et al. The canonical NF-κB pathway governs mammary tumorigenesis in transgenic mice and tumor stem cell expansion. Cancer Res. 2010;70:10464–10473. doi: 10.1158/0008-5472.CAN-10-0732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Cao Y., Luo J.-L., Karin M. IκB kinase α kinase activity is required for self-renewal of ErbB2/Her2-transformed mammary tumor-initiating cells. Proc. Natl. Acad. Sci. USA. 2007;104:15852–15857. doi: 10.1073/pnas.0706728104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Myant K.B., Cammareri P., McGhee E.J., Ridgway R.A., Huels D.J., Cordero J.B., Schwitalla S., Kalna G., Ogg E.-L., Athineos D., et al. ROS Production and NF-κB Activation Triggered by RAC1 Facilitate WNT-Driven Intestinal Stem Cell Proliferation and Colorectal Cancer Initiation. Cell Stem Cell. 2013;12:761–773. doi: 10.1016/j.stem.2013.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Chefetz I., Alvero A., Holmberg J., Lebowitz N., Craveiro V., Yang-Hartwich Y., Yin G., Squillace L., Gurrea Soteras M., Aldo P., et al. TLR2 enhances ovarian cancer stem cell self-renewal and promotes tumor repair and recurrence. Cell Cycle. 2014;12:511–521. doi: 10.4161/cc.23406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Moreira D., Zhang Q., Hossain D.M.S., Nechaev S., Li H., Kowolik C.M., D’Apuzzo M., Forman S., Jones J., Pal S.K., et al. TLR9 signaling through NF-κB/RELA and STAT3 promotes tumor-propagating potential of prostate cancer cells. Oncotarget. 2015;6:17302–17313. doi: 10.18632/oncotarget.4029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Gallipoli P., Pellicano F., Morrison H., Laidlaw K., Allan E.K., Bhatia R., Copland M., Jørgensen H.G., Holyoake T.L. Autocrine TNF-α production supports CML stem and progenitor cell survival and enhances their proliferation. Blood. 2013;122:3335–3339. doi: 10.1182/blood-2013-02-485607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kagoya Y., Yoshimi A., Kataoka K., Nakagawa M., Kumano K., Arai S., Kobayashi H., Saito T., Iwakura Y., Kurokawa M. Positive feedback between NF-κB and TNF-α promotes leukemia-initiating cell capacity. J. Clin. Invest. 2014;124:528–542. doi: 10.1172/JCI68101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Storci G., Sansone P., Mari S., D’Uva G., Tavolari S., Guarnieri T., Taffurelli M., Ceccarelli C., Santini D., Chieco P., et al. TNFα up-regulates SLUG via the NF-κB/HIF1α axis, which imparts breast cancer cells with a stem cell-like phenotype. J. Cell. Physiol. 2010;225:682–691. doi: 10.1002/jcp.22264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Wang D., Fu L., Sun H., Guo L., DuBois R.N. Prostaglandin E2 Promotes Colorectal Cancer Stem Cell Expansion and Metastasis in Mice. Gastroenterology. 2015;149:1884–1895. doi: 10.1053/j.gastro.2015.07.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Parajuli P., Anand R., Mandalaparty C., Suryadevara R., Sriranga P.U., Michelhaugh S.K., Cazacu S., Finniss S., Thakur A., Lum L.G., et al. Preferential expression of functional IL-17R in glioma stem cells: Potential role in self-renewal. Oncotarget. 2016;7:6121–6135. doi: 10.18632/oncotarget.6847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Iliopoulos D., Hirsch H.A., Struhl K. An epigenetic switch involving NF-κB, Lin28, Let-7 MicroRNA, and IL6 links inflammation to cell transformation. Cell. 2009;139:693–706. doi: 10.1016/j.cell.2009.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Iliopoulos D., Hirsch H.A., Wang G., Struhl K. Inducible formation of breast cancer stem cells and their dynamic equilibrium with non-stem cancer cells via IL6 secretion. Proc. Natl. Acad. Sci. USA. 2011;108:1397–1402. doi: 10.1073/pnas.1018898108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Xu C., Sun X., Qin S., Wang H., Zheng Z., Xu S., Luo G., Liu P., Liu J., Du N., et al. Let-7a regulates mammosphere formation capacity through Ras/NF-κB and Ras/MAPK/ERK pathway in breast cancer stem cells. Cell Cycle. 2015;14:1686–1697. doi: 10.1080/15384101.2015.1030547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Reynaud D., Pietras E., Barry-Holson K., Mir A., Binnewies M., Jeanne M., Sala-Torra O., Radich J.P., Passegué E. IL-6 controls leukemic multipotent progenitor cell fate and contributes to chronic myelogenous leukemia development. Cancer Cell. 2011;20:661–673. doi: 10.1016/j.ccr.2011.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wang H., Lathia J.D., Wu Q., Wang J., Li Z., Heddleston J.M., Eyler C.E., Elderbroom J., Gallagher J., et al. Targeting Interleukin 6 Signaling Suppresses Glioma Stem Cell Survival and Tumor Growth. Stem Cells. 2009;27:2393–2404. doi: 10.1002/stem.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Calabrese C., Poppleton H., Kocak M., Hogg T.L., Fuller C., Hamner B., Oh E.Y., Gaber M.W., Finklestein D., Allen M., et al. A Perivascular Niche for Brain Tumor Stem Cells. Cancer Cell. 2007;11:69–82. doi: 10.1016/j.ccr.2006.11.020. [DOI] [PubMed] [Google Scholar]
- 117.Charles N., Ozawa T., Squatrito M., Bleau A.-M., Brennan C.W., Hambardzumyan D., Holland E.C. Perivascular nitric oxide activates notch signaling and promotes stem-like character in PDGF-induced glioma cells. Cell Stem Cell. 2010;6:141–152. doi: 10.1016/j.stem.2010.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Xiang T., Long H., He L., Han X., Lin K., Liang Z., Zhuo W., Xie R., Zhu B. Interleukin-17 produced by tumor microenvironment promotes self-renewal of CD133+ cancer stem-like cells in ovarian cancer. Oncogene. 2013;34:165–176. doi: 10.1038/onc.2013.537. [DOI] [PubMed] [Google Scholar]
- 119.Alvero A.B., Fu H.H., Holmberg J., Visintin I., Mor L., Marquina C.C., Oidtman J., Silasi D.-A., Mor G. Stem-Like Ovarian Cancer Cells Can Serve as Tumor Vascular Progenitors. Stem Cells. 2009;27:2405–2413. doi: 10.1002/stem.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Wang R., Chadalavada K., Wilshire J., Kowalik U., Hovinga K.E., Geber A., Fligelman B., Leversha M., Brennan C., Tabar V. Glioblastoma stem-like cells give rise to tumour endothelium. Nature. 2010;468:829–833. doi: 10.1038/nature09624. [DOI] [PubMed] [Google Scholar]
- 121.Soda Y., Marumoto T., Friedmann-Morvinski D., Soda M., Liu F., Michiue H., Pastorino S., Yang M., Hoffman R.M., Kesari S., Verma I.M. Transdifferentiation of glioblastoma cells into vascular endothelial cells. Proc. Natl. Acad. Sci. USA. 2011;108:4274–4280. doi: 10.1073/pnas.1016030108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Cao L., Fan X., Jing W., Liang Y., Chen R., Liu Y., Zhu M., Jia R., Wang H., Zhang X., et al. Osteopontin promotes a cancer stem cell-like phenotype in hepatocellular carcinoma cells via an integrin-NF-κB-HIF-1α pathway. Oncotarget. 2015;6:6627–6640. doi: 10.18632/oncotarget.3113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Malanchi I., Santamaria-Martínez A., Susanto E., Peng H., Lehr H.-A., Delaloye J.-F., Huelsken J. Interactions between cancer stem cells and their niche govern metastatic colonization. Nature. 2011;481:85–89. doi: 10.1038/nature10694. [DOI] [PubMed] [Google Scholar]
- 124.Lambert A.W., Wong C.K., Ozturk S., Papageorgis P., Raghunathan R., Alekseyev Y., Gower A.C., Reinhard B.M., Abdolmaleky H.M., Thiagalingam S. Tumor Cell-Derived Periostin Regulates Cytokines That Maintain Breast Cancer Stem Cells. Mol. Cancer Res. 2016;14:103–113. doi: 10.1158/1541-7786.MCR-15-0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Schramek D., Leibbrandt A., Sigl V., Kenner L., Pospisilik J.A., Lee H.J., Hanada R., Joshi P.A., Aliprantis A., Glimcher L., et al. Osteoclast differentiation factor RANKL controls development of progestin-driven mammary cancer. Nature. 2010;468:98–102. doi: 10.1038/nature09387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Mani S.A., Guo W., Liao M.-J., Eaton E.N., Ayyanan A., Zhou A.Y., Brooks M., Reinhard F., Zhang C.C., Shipitsin M., et al. The Epithelial-Mesenchymal Transition Generates Cells with Properties of Stem Cells. Cell. 2008;133:704–715. doi: 10.1016/j.cell.2008.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Barberà M.J., Puig I., Domínguez D., Julien-Grille S., Guaita-Esteruelas S., Peiró S., Baulida J., Francí C., Dedhar S., Larue L., et al. Regulation of Snail transcription during epithelial to mesenchymal transition of tumor cells. Oncogene. 2004;23:7345–7354. doi: 10.1038/sj.onc.1207990. [DOI] [PubMed] [Google Scholar]
- 128.Kim H.J., Litzenburger B.C., Cui X., Delgado D.A., Grabiner B.C., Lin X., Lewis M.T., Gottardis M.M., Wong T.W., Attar R.M., et al. Constitutively Active Type I Insulin-Like Growth Factor Receptor Causes Transformation and Xenograft Growth of Immortalized Mammary Epithelial Cells and Is Accompanied by an Epithelial-to-Mesenchymal Transition Mediated by NF-κB and Snail. Mol. Cell. Biol. 2007;27:3165–3175. doi: 10.1128/MCB.01315-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Belguise K., Guo S., Yang S., Rogers A.E., Seldin D.C., Sherr D.H., Sonenshein G.E. Green Tea Polyphenols Reverse Cooperation between c-Rel and CK2 that Induces the Aryl Hydrocarbon Receptor, Slug, and an Invasive Phenotype. Cancer Res. 2007;67:11742–11750. doi: 10.1158/0008-5472.CAN-07-2730. [DOI] [PubMed] [Google Scholar]
- 130.Kumar M., Allison D.F., Baranova N.N., Wamsley J.J., Katz A.J., Bekiranov S., Jones D.R., Mayo M.W. NF-κB Regulates Mesenchymal Transition for the Induction of Non-Small Cell Lung Cancer Initiating Cells. PLoS ONE. 2013;8:16. doi: 10.1371/journal.pone.0068597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Chua H.L., Bhat-Nakshatri P., Clare S.E., Morimiya A., Badve S., Nakshatri H. NF-κB represses E-cadherin expression and enhances epithelial to mesenchymal transition of mammary epithelial cells: Potential involvement of ZEB-1 and ZEB-2. Oncogene. 2006;26:711–724. doi: 10.1038/sj.onc.1209808. [DOI] [PubMed] [Google Scholar]
- 132.Wang S.M., Coljee V.W., Pignolo R.J., Rotenberg M.O., Cristofalo V.J., Sierra F. Cloning of the human twist gene: Its expression is retained in adult mesodermally-derived tissues. Gene. 1997;187:83–92. doi: 10.1016/S0378-1119(96)00727-5. [DOI] [PubMed] [Google Scholar]
- 133.Kanegae Y., Tavares A.T., Izpisúa Belmonte J.C., Verma I.M. Role of Rel/NF-κB transcription factors during the outgrowth of the vertebrate limb. Nature. 1998;392:611–614. doi: 10.1038/33429. [DOI] [PubMed] [Google Scholar]
- 134.Takeda K., Takeuchi O., Tsujimura T., Itami S., Adachi O., Kawai T., Sanjo H., Yoshikawa K., Terada N., Akira S. Limb and skin abnormalities in mice lacking IKKα. Science. 1999;284:313–316. doi: 10.1126/science.284.5412.313. [DOI] [PubMed] [Google Scholar]
- 135.Šošić D., Richardson J.A., Yu K., Ornitz D.M., Olson E.N. Twist regulates cytokine gene expression through a negative feedback loop that represses NF-κB activity. Cell. 2003;112:169–180. doi: 10.1016/S0092-8674(03)00002-3. [DOI] [PubMed] [Google Scholar]
- 136.Pham C.G., Bubici C., Zazzeroni F., Knabb J.R., Papa S., Kuntzen C., Franzoso G. Upregulation of Twist-1 by NF-κB Blocks Cytotoxicity Induced by Chemotherapeutic Drugs. Mol. Cell. Biol. 2007;27:3920–3935. doi: 10.1128/MCB.01219-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Min C., Eddy S.F., Sherr D.H., Sonenshein G.E. NF-κB and epithelial to mesenchymal transition of cancer. J. Cell. Biochem. 2008;104:733–744. doi: 10.1002/jcb.21695. [DOI] [PubMed] [Google Scholar]
- 138.Wu Y., Deng J., Rychahou P.G., Qiu S., Evers B.M., Zhou B.P. Stabilization of Snail by NF-κB Is Required for Inflammation-Induced Cell Migration and Invasion. Cancer Cell. 2009;15:416–428. doi: 10.1016/j.ccr.2009.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Li C.W., Xia W., Huo L., Lim S.O., Wu Y., Hsu J.L., Chao C.H., Yamaguchi H., Yang N.K., Ding Q., et al. Epithelial-Mesenchymal Transition Induced by TNF-α Requires NF-κB-Mediated Transcriptional Upregulation of Twist1. Cancer Res. 2012;72:1290–1300. doi: 10.1158/0008-5472.CAN-11-3123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Huber M.A., Azoitei N., Baumann B., Grünert S., Sommer A., Pehamberger H., Kraut N., Beug H., Wirth T. NF-κB is essential for epithelial-mesenchymal transition and metastasis in a model of breast cancer progression. J. Clin. Invest. 2004;114:569–581. doi: 10.1172/JCI200421358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Palafox M., Ferrer I., Pellegrini P., Vila S., Hernandez-Ortega S., Urruticoechea A., Climent F., Soler M.T., Munoz P., Vinals F., et al. RANK Induces Epithelial-Mesenchymal Transition and Stemness in Human Mammary Epithelial Cells and Promotes Tumorigenesis and Metastasis. Cancer Res. 2012;72:2879–2888. doi: 10.1158/0008-5472.CAN-12-0044. [DOI] [PubMed] [Google Scholar]
- 142.Asiedu M.K., Beauchamp-Perez F.D., Ingle J.N., Behrens M.D., Radisky D.C., Knutson K.L. AXL induces epithelial-to-mesenchymal transition and regulates the function of breast cancer stem cells. Oncogene. 2013;33:1316–1324. doi: 10.1038/onc.2013.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Wamsley J.J., Kumar M., Allison D.F., Clift S.H., Holzknecht C.M., Szymura S.J., Hoang S.A., Xu X., Moskaluk C.A., Jones D.R., et al. Activin Upregulation by NF-κB Is Required to Maintain Mesenchymal Features of Cancer Stem-like Cells in Non-Small Cell Lung Cancer. Cancer Res. 2015;75:426–435. doi: 10.1158/0008-5472.CAN-13-2702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Es-haghi M., Soltanian S., Dehghani H. Perspective: Cooperation of Nanog, NF-κB, and CXCR4 in a regulatory network for directed migration of cancer stem cells. Tumor Biol. 2015 doi: 10.1007/s13277-015-4690-6. [DOI] [PubMed] [Google Scholar]
- 145.Singh A.P., Arora S., Bhardwaj A., Srivastava S.K., Kadakia M.P., Wang B., Grizzle W.E., Owen L.B., Singh S. CXCL12/CXCR4 Protein Signaling Axis Induces Sonic Hedgehog Expression in Pancreatic Cancer Cells via Extracellular Regulated Kinase- and Akt Kinase-mediated Activation of Nuclear Factor-κB: Implications for Bidirectional Tumor-Stromal Interactions. J. Biol. Chem. 2012;287:39115–39124. doi: 10.1074/jbc.M112.409581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Helbig G., Christopherson K.W., Bhat-Nakshatri P., Kumar S., Kishimoto H., Miller K.D., Broxmeyer H.E., Nakshatri H. NF-κB Promotes Breast Cancer Cell Migration and Metastasis by Inducing the Expression of the Chemokine Receptor CXCR4. J. Biol. Chem. 2003;278:21631–21638. doi: 10.1074/jbc.M300609200. [DOI] [PubMed] [Google Scholar]
- 147.Zhi Y., Duan Y., Zhou X., Yin X., Guan G., Zhang H., Dong Q., Yang K. NF-κB signaling pathway confers neuroblastoma cells migration and invasion ability via the regulation of CXCR4. Med. Sci. Monit. 2014;20:2746–2752. doi: 10.12659/MSM.892597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Himelstein B.P., Lee E.J., Sato H., Seiki M., Muschel R.J. Transcriptional activation of the matrix metalloproteinase-9 gene in an H-ras and v-myc transformed rat embryo cell line. Oncogene. 1997;14:1995–1998. doi: 10.1038/sj.onc.1201012. [DOI] [PubMed] [Google Scholar]
- 149.Farina A.R., Tacconelli A., Vacca A., Maroder M., Gulino A., Mackay A.R. Transcriptional up-regulation of matrix metalloproteinase-9 expression during spontaneous epithelial to neuroblast phenotype conversion by SK-N-SH neuroblastoma cells, involved in enhanced invasivity, depends upon GT-box and nuclear factor κB elements. Cell Growth Differ. 1999;10:353–367. [PubMed] [Google Scholar]
- 150.Ricca A., Biroccio A., Del Bufalo D., Mackay A.R., Santoni A., Cippitelli M. BCL-2 over-expression enhances NF-κB activity and induces mmp-9 transcription in human MCF7(ADR) breast-cancer cells. Int. J. Cancer. 2000;86:188–196. doi: 10.1002/(SICI)1097-0215(20000415)86:2<188::AID-IJC7>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 151.Han Y.P., Tuan T.L., Wu H., Hughes M., Garner W.L. TNF-α stimulates activation of pro-MMP2 in human skin through NF-κB mediated induction of MT1-MMP. J. Cell. Sci. 2001;114:131–139. doi: 10.1242/jcs.114.1.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Philip S., Bulbule A., Kundu G.C. Osteopontin stimulates tumor growth and activation of promatrix metalloproteinase-2 through nuclear factor-κB-mediated induction of membrane type 1 matrix metalloproteinase in murine melanoma cells. J. Biol. Chem. 2001;276:44926–44935. doi: 10.1074/jbc.M103334200. [DOI] [PubMed] [Google Scholar]
- 153.Connelly L., Robinson-Benion C., Chont M., Saint-Jean L., Li H., Polosukhin V.V., Blackwell T.S., Yull F.E. A transgenic model reveals important roles for the NF-κB alternative pathway (p100/p52) in mammary development and links to tumorigenesis. J. Biol. Chem. 2007;282:10028–10035. doi: 10.1074/jbc.M611300200. [DOI] [PubMed] [Google Scholar]
- 154.Long H., Xie R., Xiang T., Zhao Z., Lin S., Liang Z., Chen Z., Zhu B. Autocrine CCL5 Signaling Promotes Invasion and Migration of CD133+ Ovarian Cancer Stem-Like Cells via NF-κB-Mediated MMP-9 Upregulation. Stem Cells. 2012;30:2309–2319. doi: 10.1002/stem.1194. [DOI] [PubMed] [Google Scholar]
- 155.Huang S., Robinson J.B., Deguzman A., Bucana C.D., Fidler I.J. Blockade of nuclear factor-κB signaling inhibits angiogenesis and tumorigenicity of human ovarian cancer cells by suppressing expression of vascular endothelial growth factor and interleukin 8. Cancer Res. 2000;60:5334–5339. [PubMed] [Google Scholar]
- 156.Yamamoto M., Taguchi Y., Ito-Kureha T., Semba K., Yamaguchi N., Inoue J.-I. NF-κB non-cell-autonomously regulates cancer stem cell populations in the basal-like breast cancer subtype. Nat. Commun. 2013;4:2299. doi: 10.1038/ncomms3299. [DOI] [PubMed] [Google Scholar]
- 157.Ohtsu N., Nakatani Y., Yamashita D., Ohue S., Ohnishi T., Kondo T. Eva1 Maintains the Stem-like Character of Glioblastoma-Initiating Cells by Activating the Noncanonical NF-κB Signaling Pathway. Cancer Res. 2016;76:171–181. doi: 10.1158/0008-5472.CAN-15-0884. [DOI] [PubMed] [Google Scholar]
- 158.Guzman M.L., Swiderski C.F., Howard D.S., Grimes B.A., Rossi R.M., Szilvassy S.J., Jordan C.T. Preferential induction of apoptosis for primary human leukemic stem cells. Proc. Natl. Acad. Sci. USA. 2002;99:16220–16225. doi: 10.1073/pnas.252462599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Guzman M.L., Rossi R.M., Karnischky L., Li X., Peterson D.R., Howard D.S., Jordan C.T. The sesquiterpene lactone parthenolide induces apoptosis of human acute myelogenous leukemia stem and progenitor cells. Blood. 2005;105:4163–4169. doi: 10.1182/blood-2004-10-4135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Hassane D.C., Guzman M.L., Corbett C., Li X., Abboud R., Young F., Liesveld J.L., Carroll M., Jordan C.T. Discovery of agents that eradicate leukemia stem cells using an in silico screen of public gene expression data. Blood. 2008;111:5654–5662. doi: 10.1182/blood-2007-11-126003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Zhou J., Zhang H., Gu P., Bai J., Margolick J.B., Zhang Y. NF-κB pathway inhibitors preferentially inhibit breast cancer stem-like cells. Breast Cancer Res Treat. 2007;111:419–427. doi: 10.1007/s10549-007-9798-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Zhang L., Ren X., Cheng Y., Liu X., Allen J.E., Zhang Y., Yuan Y., Huang S.-Y., Yang W., Berg A., et al. The NFκB inhibitor, SN50, induces differentiation of glioma stem cells and suppresses their oncogenic phenotype. Cancer Biol. Ther. 2014;15:602–611. doi: 10.4161/cbt.28158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Nogueira L., Ruiz-Ontañon P., Vazquez-Barquero A., Lafarga M., Berciano M.T., Aldaz B., Grande L., Casafont I., Segura V., Robles E.F., et al. Blockade of the NFκB pathway drives differentiating glioblastoma-initiating cells into senescence both in vitro and in vivo. Oncogene. 2011;30:3537–3548. doi: 10.1038/onc.2011.74. [DOI] [PubMed] [Google Scholar]
- 164.Jazirehi A.R., Huerta-Yepez S., Cheng G., Bonavida B. Rituximab (chimeric anti-CD20 monoclonal antibody) inhibits the constitutive nuclear factor-κB signaling pathway in non-Hodgkin’s lymphoma B-cell lines: Role in sensitization to chemotherapeutic drug-induced apoptosis. Cancer Res. 2005;65:264–276. [PubMed] [Google Scholar]
- 165.Akinleye A., Chen Y., Mukhi N., Song Y., Liu D. Ibrutinib and novel BTK inhibitors in clinical development. J. Hematol. Oncol. 2013;6:59. doi: 10.1186/1756-8722-6-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Xue W., Meylan E., Oliver T.G., Feldser D.M., Winslow M.M., Bronson R., Jacks T. Response and Resistance to NF-κB Inhibitors in Mouse Models of Lung Adenocarcinoma. Cancer Discov. 2011;1:236–247. doi: 10.1158/2159-8290.CD-11-0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Bassères D.S., Ebbs A., Cogswell P.C., Baldwin A.S. IKK is a therapeutic target in KRAS-Induced lung cancer with disrupted p53 activity. Genes Cancer. 2014;5:41–55. doi: 10.18632/genesandcancer.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Friedmann-Morvinski D., Narasimamurthy R., Xia Y., Myskiw C., Soda Y., Verma I.M. Targeting NF-κB in glioblastoma: A therapeutic approach. Science Advances. 2016;2:e1501292–e1501292. doi: 10.1126/sciadv.1501292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Habineza Ndikuyeze G., Gaurnier-Hausser A., Patel R., Baldwin A.S., May M.J., Flood P., Krick E., Propert K.J., Mason N.J. A Phase I Clinical Trial of Systemically Delivered NEMO Binding Domain Peptide in Dogs with Spontaneous Activated B-Cell like Diffuse Large B-Cell Lymphoma. PLoS ONE. 2014;9:16. doi: 10.1371/journal.pone.0095404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Gaurnier-Hausser A., Patel R., Baldwin A.S., May M.J., Mason N.J. NEMO-Binding Domain Peptide Inhibits Constitutive NF-κB Activity and Reduces Tumor Burden in a Canine Model of Relapsed, Refractory Diffuse Large B-Cell Lymphoma. Clin. Can. Res. 2011;17:4661–4671. doi: 10.1158/1078-0432.CCR-10-3310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Wang C.Y., Mayo M.W., Baldwin A.S. TNF- and cancer therapy-induced apoptosis: Potentiation by inhibition of NF-κB. Science. 1996;274:784–787. doi: 10.1126/science.274.5288.784. [DOI] [PubMed] [Google Scholar]
- 172.Wang C.Y., Cusack J.C., Liu R., Baldwin A.S. Control of inducible chemoresistance: Enhanced anti-tumor therapy through increased apoptosis by inhibition of NF-κB. Nat. Med. 1999;5:412–417. doi: 10.1038/10577. [DOI] [PubMed] [Google Scholar]
- 173.Cusack J.C., Liu R., Houston M., Abendroth K., Elliott P.J., Adams J., Baldwin A.S. Enhanced chemosensitivity to CPT-11 with proteasome inhibitor PS-341: Implications for systemic nuclear factor-κB inhibition. Cancer Res. 2001;61:3535–3540. [PubMed] [Google Scholar]
- 174.Fukushima T., Kawaguchi M., Yorita K., Tanaka H., Takeshima H., Umezawa K., Kataoka H. Antitumor effect of dehydroxymethylepoxyquinomicin, a small molecule inhibitor of nuclear factor-κB, on glioblastoma. Neuro-Oncology. 2011;14:19–28. doi: 10.1093/neuonc/nor168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Brassesco M.S., Roberto G.M., Morales A.G., Oliveira J.C., Delsin L.E.A., Pezuk J.A., Valera E.T., Carlotti C.G., Rego E.M., de Oliveira H.F., et al. Inhibition of NF-κB by Dehydroxymethylepoxyquinomicin Suppresses Invasion and Synergistically Potentiates Temozolomide and γ-Radiation Cytotoxicity in Glioblastoma Cells. Chemother. Res. Pract. 2013;2013:1–16. doi: 10.1155/2013/593020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Shukla S., Pia Patric I.R., Thinagararjan S., Srinivasan S., Mondal B., Hegde A.S., Chandramouli B.A., Santosh V., Arivazhagan A., Somasundaram K. The NPTX2-PTEN-NFκB nexus is an essential component of a prognostic DNA methylation signature of glioblastoma. Cancer Res. 2013;73:6563–6573. doi: 10.1158/0008-5472.CAN-13-0298. [DOI] [PubMed] [Google Scholar]
- 177.Xi G., Hayes E., Lewis R., Ichi S., Mania-Farnell B., Shim K., Takao T., Allender E., Mayanil C.S., Tomita T. CD133 and DNA-PK regulate MDR1 via the PI3K- or Akt-NF-κB pathway in multidrug-resistant glioblastoma cells in vitro. Oncogene. 2015;35:241–250. doi: 10.1038/onc.2015.78. [DOI] [PubMed] [Google Scholar]
- 178.Seguin L., Kato S., Franovic A., Camargo M.F., Lesperance J., Elliott K.C., Yebra M., Mielgo A., Lowy A.M., Husain H., et al. An integrin β3-KRAS-RalB complex drives tumour stemness and resistance to EGFR inhibition. Nat. Cell Biol. 2014;16:457–468. doi: 10.1038/ncb2953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Wee Z.N., Yatim S.M.J.M., Kohlbauer V.K., Feng M., Goh J.Y., Yi B., Lee P.L., Zhang S., Wang P.P., Lim E., et al. IRAK1 is a therapeutic target that drives breast cancer metastasis and resistance to paclitaxel. Nat. Commun. 2015;6:8746. doi: 10.1038/ncomms9746. [DOI] [PMC free article] [PubMed] [Google Scholar]