Abstract
Sternal variations and anomalies have been identified in the past during autopsy or cadaveric studies. Recently, an increasing number of minor sternal variations have been reported with the advent of multidetector computed tomography (CT). Although there are many sternal variations that occur with varying appearance and prevalence, most of them are not recognized or are underreported during routine imaging of thorax. Identification of sternal variations is important to differentiate from pathological conditions and to prevent fatal complications prior to sternal interventions like marrow aspiration or acupuncture. This article aims to describe the minor and asymptomatic sternal variations by multidetector CT and their clinical significance.
Keywords: Indian population, multidetector computed tomography, sternal cleft, sternal foramen, sternal variations, suprasternal ossicle, xiphoid foramen
Introduction
Sternal variations can occur in manubrium, body, or xiphoid. With the increasing use of multidetector computed tomography (MDCT), the sternal variations can be identified more frequently. In a large series, sternal variations and anomalies were characterized based on macroscopic[1] and radiographic[2] appearances in autopsy populations. In another series involving living subjects, the frequency of sternal anomalies has been described based on radiograph,[3,4] helical computed tomography (CT),[5,6] and magnetic resonance imaging (MRI)[7] appearances. Recently, sternal variations have been studied by MDCT in different populations.[8,9,10,11,12]
MDCT Protocol
MDCT examinations of chest were performed in our center using 128-slice CT scanner from the level of thoracic inlet to the level of adrenals in a cranio-caudal direction. The entire sternum including xiphoid process was included in all the cases. The common scanning parameters were: 120 kVp, 100-300 mA depending on body mass index, and 64 × 0.625 mm collimation. For isotropic resolution, we recommend 1 mm axial and multiplanar reconstruction image thickness. For better identification of sternal variations, images should be initially analyzed in axial, sagittal, and coronal multiplanar reconstruction (MPR) using bone algorithm followed by maximum intensity projection (MIP) and volume rendering (VR).
Embryology of Sternum
The sternal bone ossifies from a cartilaginous precursor. Beginning from the 5th month of prenatal life to shortly before birth, the ossification centers of manubrium and sternal body form on a cartilaginous plate on either side of midline in cranio-caudal direction. In manubrium, the ossification centers usually merge before birth. In sternal body, two or more ossification centers form on each segment of mesosternum referred as sternebrae. The ossification centers at each segment of the sternal body generally fuse to form single ossification center during 6-12 years of age [Figure 1]. The calcification and fusion of sternal body segments is usually complete by 25 years of age[8,11,13,14] [Figure 2]. Any failure in this developmental process results in sternal variations and anomalies.[1,2,15]
Figure 1.
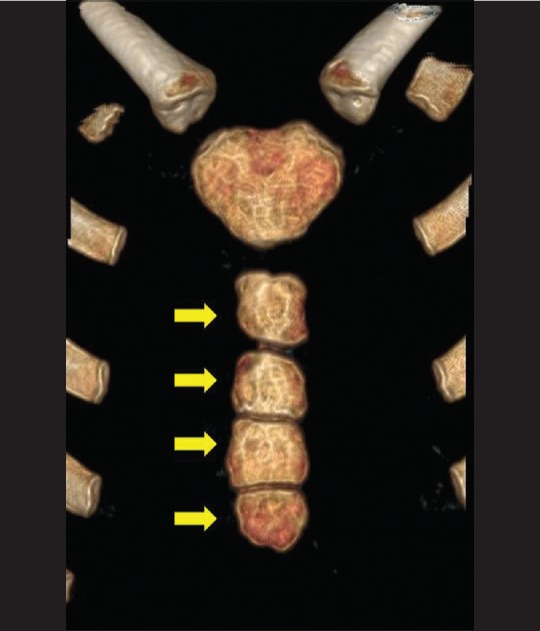
Coronal volume rendered image of sternum shows non fused sternal body segments in a 11 year old child (yellow arrows). This appearance is usually seen in children between 6-12 years of age. Note absence of xiphoid ossification
Figure 2.
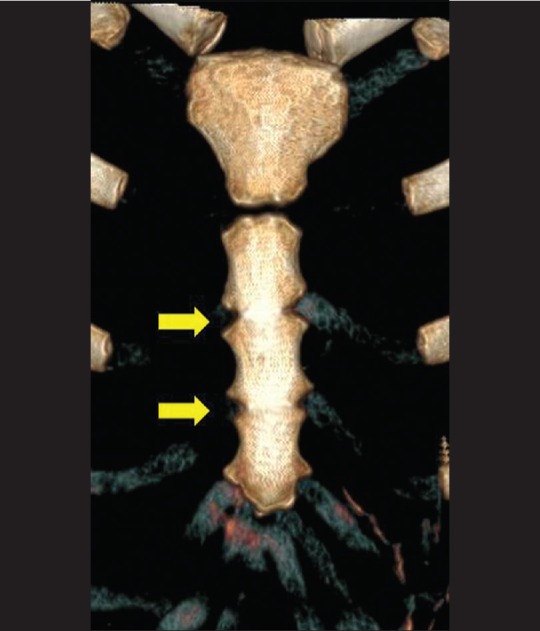
Coronal volume rendered image of sternum shows partial fusion of sternal body segments in a 17 year old (yellow arrows). The fusion of sternal body segments is usually complete by 25 years of age
Anatomy of Sternum
Sternum is a flat bone which consists of three parts: Manubrium, body, and xiphoid process [Figure 3]. Manubrium is the most cephalad and broadest segment. It has a superior central notch (suprasternal notch) and two lateral fossa (clavicular notch). Manubrium articulates with clavicles and the first two ribs laterally and with the body of sternum inferiorly (manubriosternal joint).[16,17,18,19]
Figure 3.
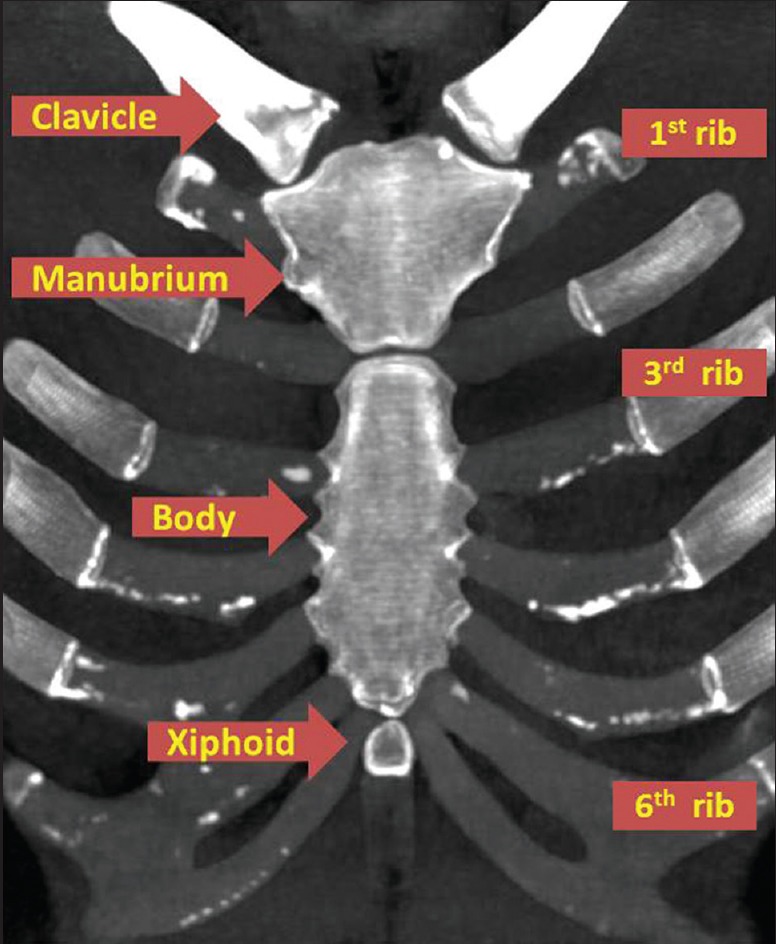
Coronal MIP image of sternum shows three parts including manubrium, sternal body and xiphoid (labelled). The relationship of clavicle and ribs to sternum is well depicted (labelled)
The body of the sternum is flat, with an irregular anterior surface. Superiorly, it articulates with the manubrium and inferiorly, it articulates with the xiphoid process at the sternoxiphoidal joint. The lateral borders of the sternum articulate with second to seventh ribs. The angle between the body and the manubrium (sternal angle) is a palpable clinical landmark.[16,17,18,19]
The xiphoid process is a thin and elongated bone that is subject to many variations. It is cartilaginous early in life and may become completely ossified and fused to the sternal body in old age.
Sternal Variations
Suprasternal or episternal ossicle or suprasternal bone
Suprasternal or episternal ossicle is a small accessory ossicle at the superior margin of manubrium that results from supernumerary ossification centers. It can be unilateral or bilateral.[8] The CT appearance is similar to any other accessory ossicle which occurs in human skeleton. In axial plane, it is well corticated, pyramidal or ovoid in shape, and seen adjoining the superior aspect of manubrium. Oblique coronal or sagittal planes are better in depicting the relation of suprasternal ossicles to manubrium and also to identify smaller or partially fused ossicles [Figure 4A and B]. The incidence of suprasternal ossicle in living subjects is found to vary as reported in previous studies, according to the sample population and ethnicity. In a study by Ogawa et al. (1979), suprasternal ossicle was seen in 6.9% of subjects, whereas in the studies by Stark et al. (1987) and Yekelar et al. (2006), it was seen in 1.5% and 4.1% of the subjects, respectively. The presence of these suprasternal ossicles is usually incidental, but they should be differentiated from vascular calcifications, calcified lymph nodes, fracture fragments, and foreign bodies.[9]
Figure 4 (A and B).
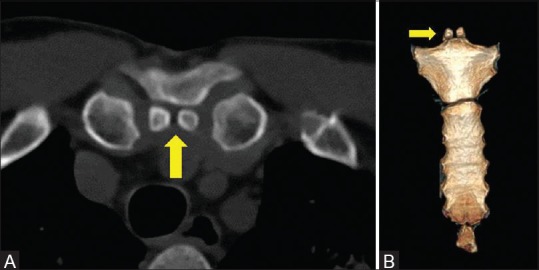
(A) Axial CT at the level of superior margin of manubrium shows two well defined ossicles consistent with suprasternal ossicles (yellow arrow) (B) Coronal volume rendered image of sternum shows bilateral suprasternal ossicles (yellow arrow)
Suprasternal tubercle
Suprasternal tubercle forms when a suprasternal ossicle fuses with manubrium.[3] Similar to suprasternal bone, it can be unilateral or bilateral. In CT, it usually appears as triangular or pyramidal bony projection in continuity with the superior margin of manubrium. It is better depicted in coronal and axial planes [Figure 5]. Previous studies have reported the incidence of suprasternal tubercle as 1.4% (Ogawa et al.) and 4% (Yekelar et al.). Occasionally, the suprasternal bone and tubercle occur in the same patient [Figure 6A and B].
Figure 5.
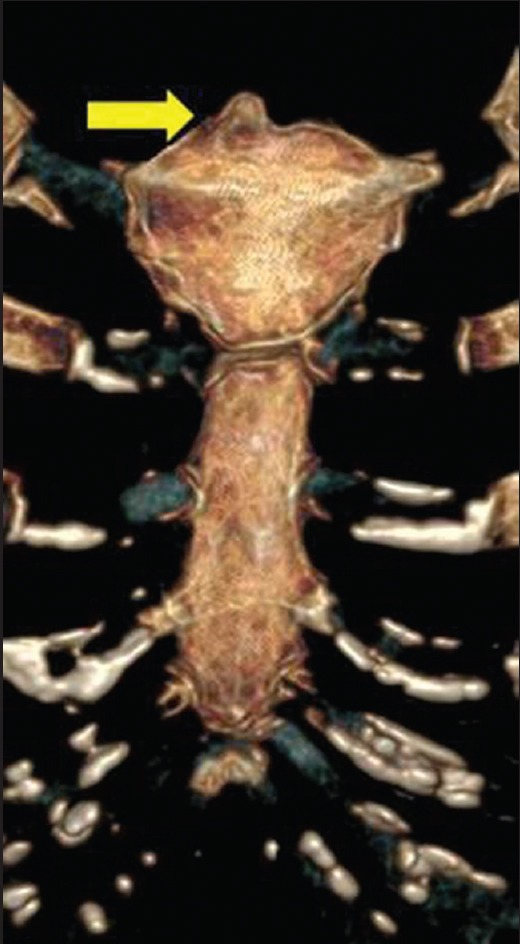
Coronal volume rendered image of sternum shows unilateral suprasternal tubercle (yellow arrow)
Figure 6 (A and B).
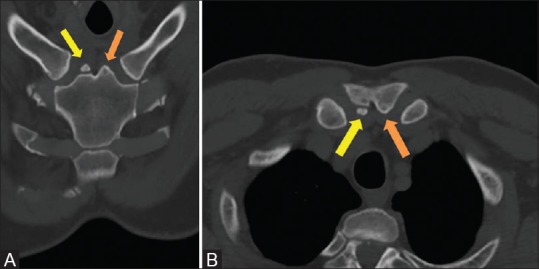
(A) Oblique coronal CT of manubrium shows suprasternal ossicle on right (yellow arrow) and suprasternal tubercle on left side (orange arrow) (B) Oblique axial CT of manubrium shows suprasternal ossicle on right (yellow arrow) and suprasternal tubercle on left side (orange arrow)
Manubriosternal and sternoxiphoidal fusion
Manubriosternal and sternoxiphoidal fusion can be partial or complete. It is best seen in sagittal and oblique coronal planes [Figures 7 and 8]. Complete fusion can be seen in younger and older patients. Manubriosternal fusion in the older age group due to degeneration can be associated with bridging osteophytes.[20] Inflammatory arthritis (especially ankylosing spondylitis) can lead to similar fusion of manubriosternal joint.[18,21] But this pathological ankylosis can be differentiated by its clinical features, involvement of other joints (including sternoclavicular joint and spine), and biochemical markers. In the study by Yekelar et al. (2006), 20% of subjects with complete fusion of manubriosternal and sternoxiphoidal joints were less than 45 years of age and the youngest subject was 20 years old. Similarly, we have encountered complete fusion of manubriosternal joint in a 19-year-old male [Figure 9A and B]. This implies that developmental fusion without osteodegeneration can occur in younger age group and should be differentiated from pathological bony ankylosis.[8]
Figure 7.
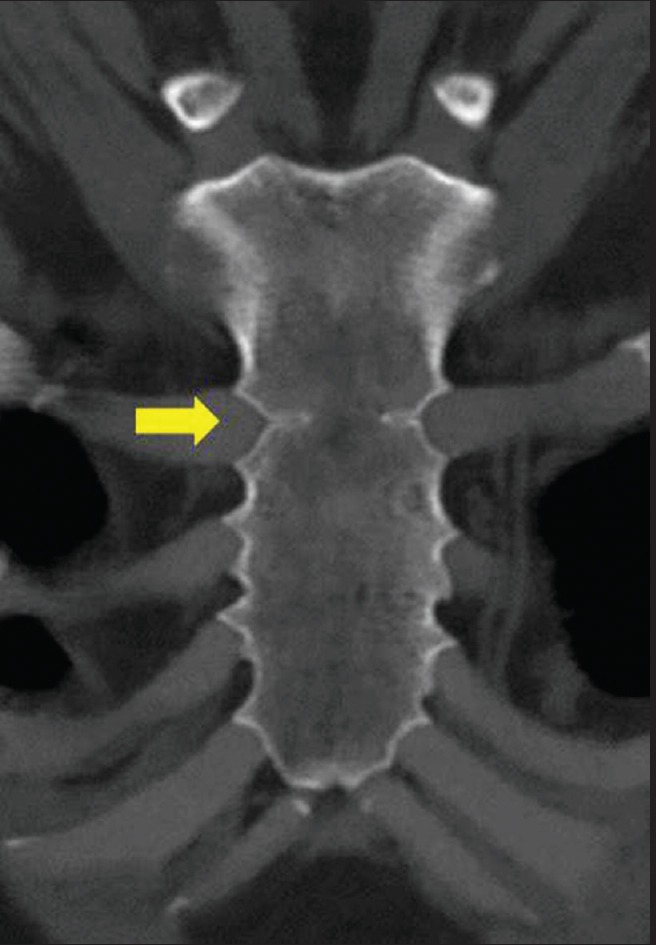
Coronal CT of sternum shows partial fusion of manubriosternal joint (yellow arrow) in 36 year old
Figure 8 (A and B).
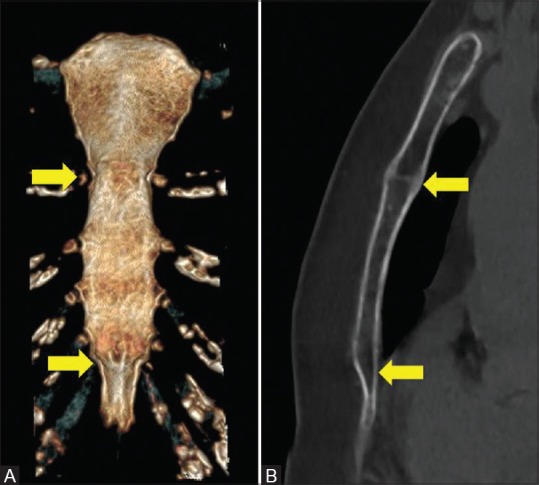
(A) Volume rendered image of sternum shows complete fusion of manubriosternal and sternoxiphoidal joint (yellow arrows) (B) Reformatted sagittal CT of sternum shows complete fusion of manubriosternal and sternoxiphoidal joint (yellow arrows)
Figure 9 (A and B).
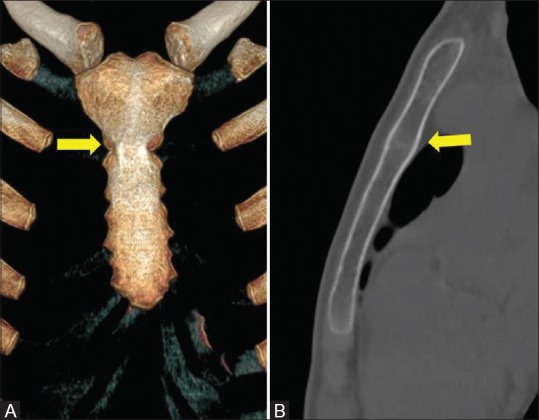
(A) Coronal volume rendered image of sternum shows complete fusion of manubriosternal joint (yellow arrow) in a 19 year old male. Note absence of xiphoid ossification (B) Reformatted sagittal CT of sternum shows complete fusion of manubriosternal joint (yellow arrow) in a 19 year old male
Sternal and xiphoid foramen
Sternal foramen occurs from incomplete fusion of a pair of sternebrae.[8] It can be single or multiple and is usually seen in lower part of the sternal body. CT shows a well-corticated, round to oval-shaped defect in the midline of the sternal body with an average diameter of 6 mm.[8] In axial plane, it has a bow-tie appearance[18] [Figures 10–12]. Previous studies show the incidence of sternal foramen to be around 4.5% of the population.[5,8] Sometimes, the sternal foramen can mimic a lytic lesion, especially in bone scintigraphy where it appears as a focal defect.[22] In such cases, cross-sectional imaging can have a vital role in diagnosis. Lytic lesions of the sternum, secondary to infection, primary malignancy, or metastases usually have irregular margins, erosions, and a soft tissue component. Identification of such variations is important to prevent fatal complications during sternal marrow aspiration and acupuncture. Since mediastinal structures are unprotected, complications like cardiac tamponade can occur.[23,24,25] Similarly, xiphoid foramen can occur, but is of lesser clinical significance [Figure 12].
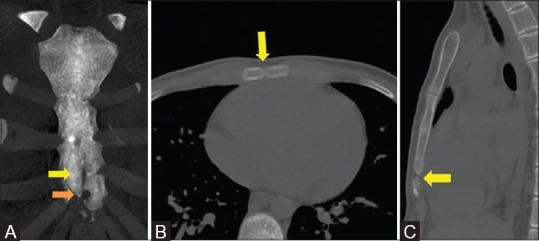
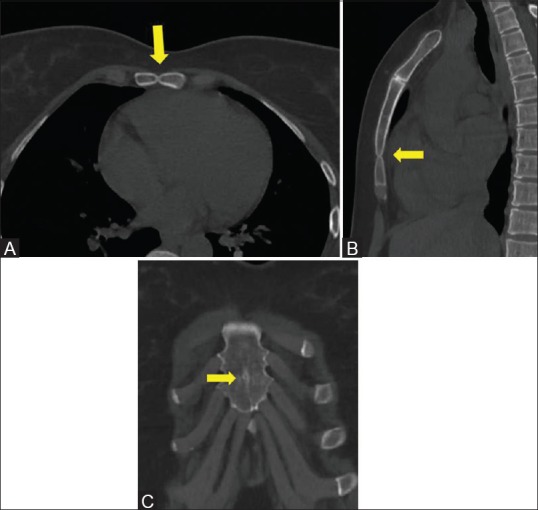
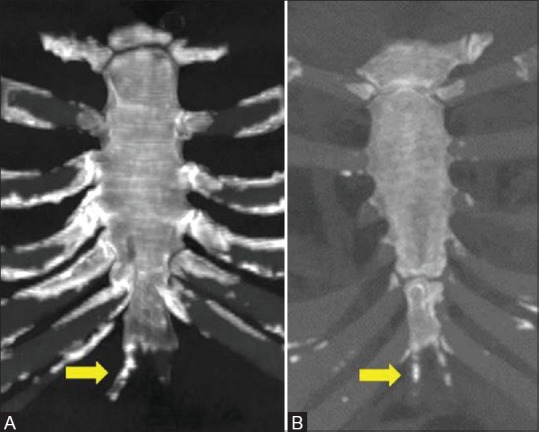
Figure 10 (A-C).
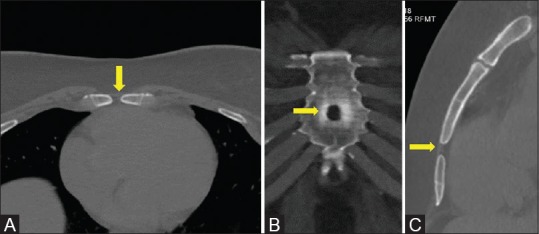
(A) Axial CT of body of sternum shows a typical bow-tie appearance of sternal foramen (yellow arrow) (B) Oblique coronal CT of sternal body shows a typical sternal foramen with sclerotic margins (yellow arrow) (C) Reformatted sagittal CT of sternum shows well defined sternal foramen (yellow arrow)
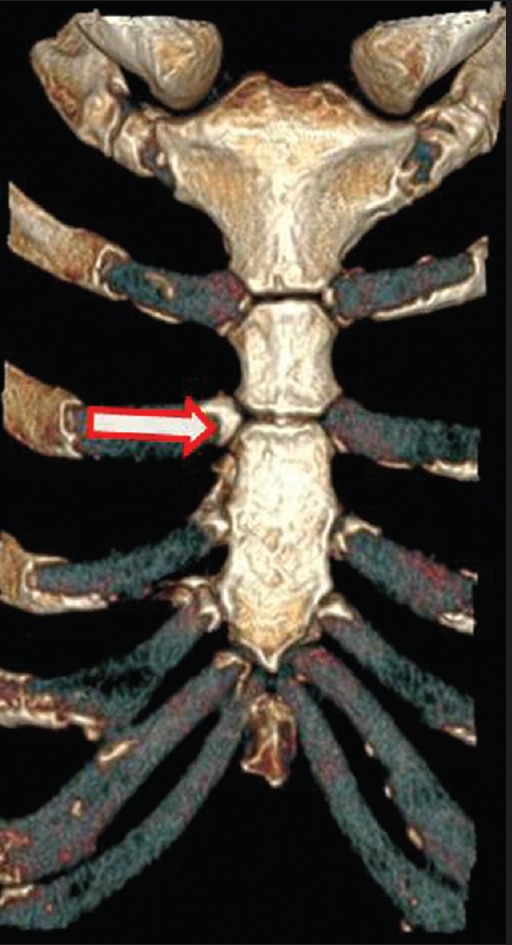
Figure 12.
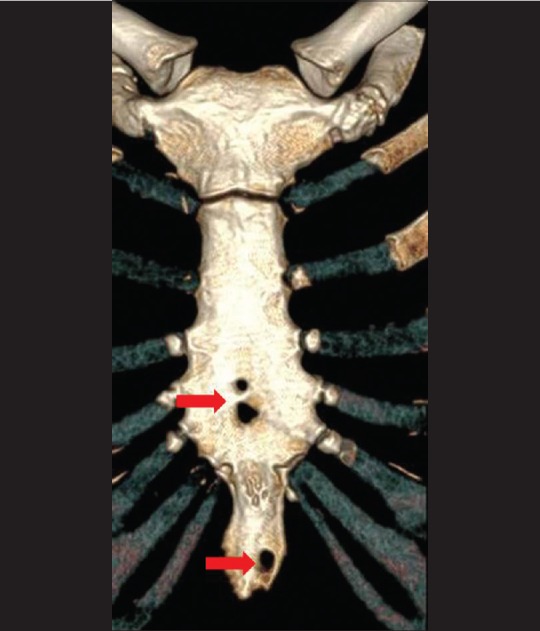
Coronal volume rendered image of sternum shows multiple foramina in sternal body and xiphoid (red arrows)
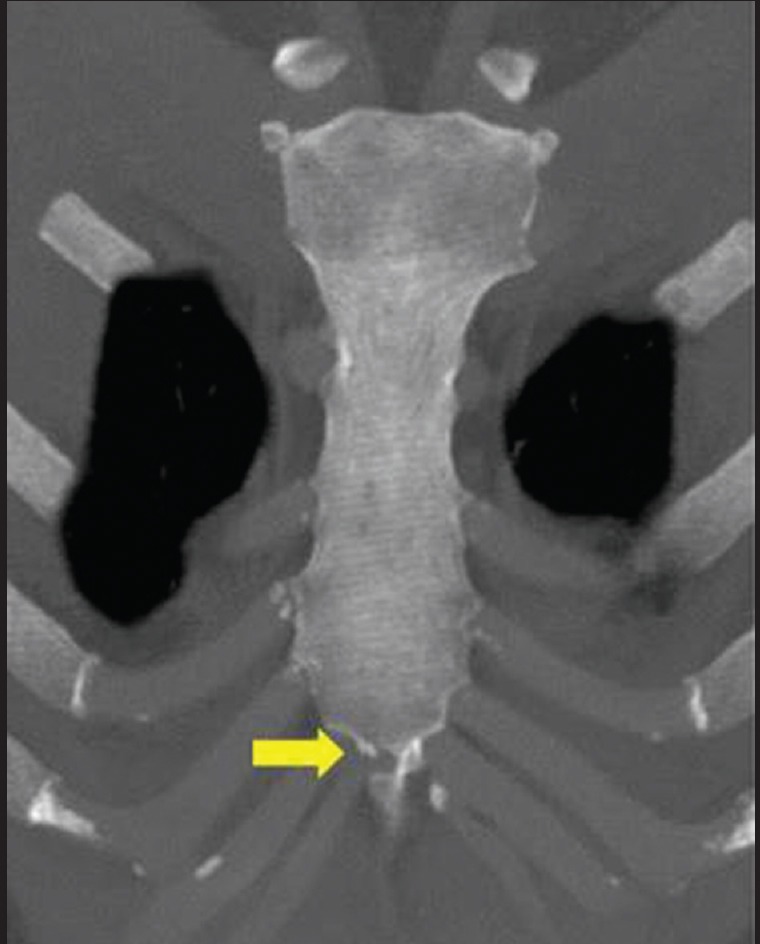
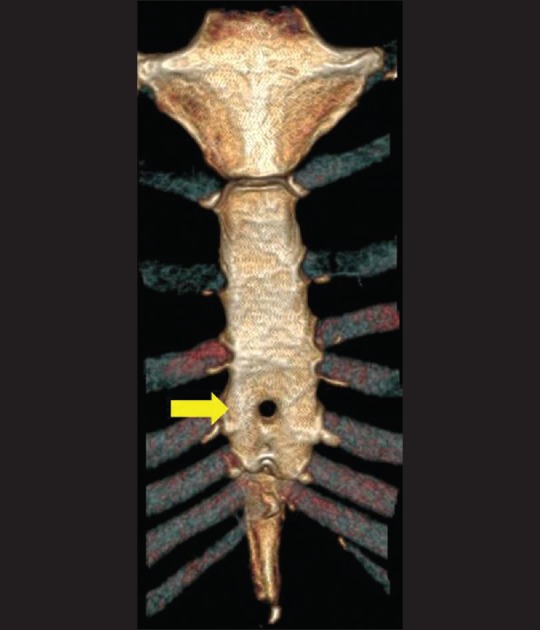
Figure 11.
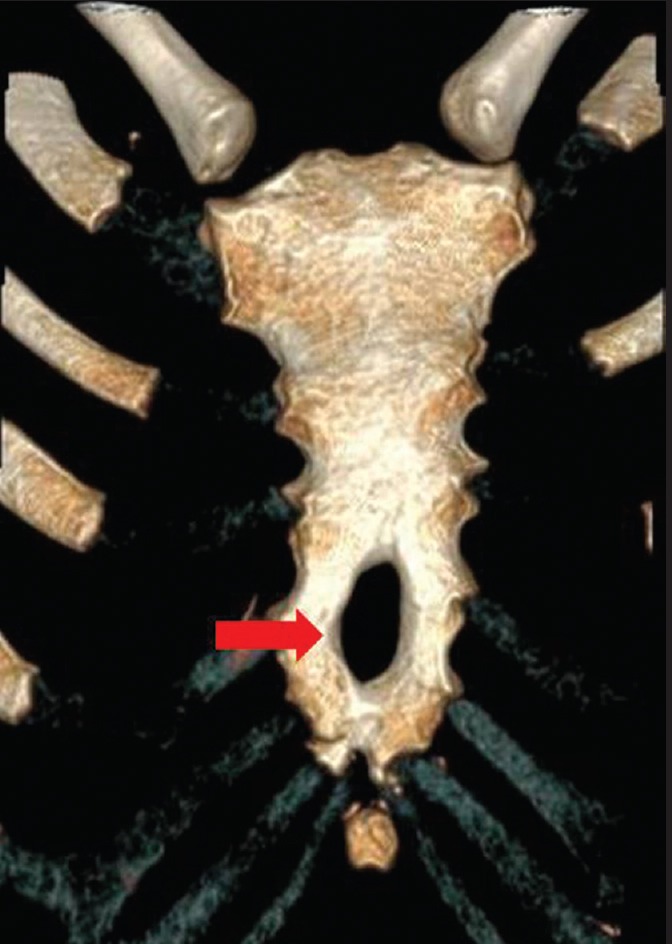
Coronal volume rendered image of sternum shows a large foramen measuring 11 mm (Red arrow)
Sternal cleft and band
These vertically oriented midline congenital defects are seen at the junction of the sternal bars.[8,15,18,26] Sternal cleft occurs due to failure or incomplete fusion of sternal segments. The sternal defects can vary from a linear fissure to larger defects with complete or partial separation of sternum. The larger defects can be associated with ectopia cordis, omphalocele, or occur as part of complex syndromes (Cantrell's pentalogy, PHACE syndrome which includes posterior fossa malformations, hemangiomas, arterial anomalies, coarctation of aorta and cardiac defects, eye abnormalities).[15,27] Patients with larger defects can be clinically diagnosed at birth or early childhood and evaluated for associated anomalies. But isolated small clefts are found incidentally during imaging of chest. In CT, they are seen as a linear midline lucent defect with corticated margins in the coronal plane and slit-like defect in the axial plane [Figure 13a–c]. The smaller sternal clefts can be mistaken for a sternal fracture, but CT shows typical appearance of fracture as irregular lucency with non-sclerotic margins. Similar to sternal foramens, clefts should be recognized before any invasive procedure of sternum to prevent complications.
Figure 13 (A-C).
(A) Coronal MIP image of sternum shows a midline cleft (yellow arrow) and associated foramen at its lower end (orange arrow) (B) Axial CT of sternal body shows a slit like midline sternal defect (yellow arrow) (C) Reformatted sagittal CT of sternum shows the associated sternal foramen (yellow arrow)
Bands are generally found in the manubrium and sternal body, but not in the xiphoid process [Figures 14 and 15]. Sclerotic band in sternal body is usually seen in the inferior segment in the midline and can occasionally be associated with sternal cleft or foramen.[8] Although sclerotic bands are more common than cleft, they usually have no clinical significance.[8]
Figure 14 (A and B).
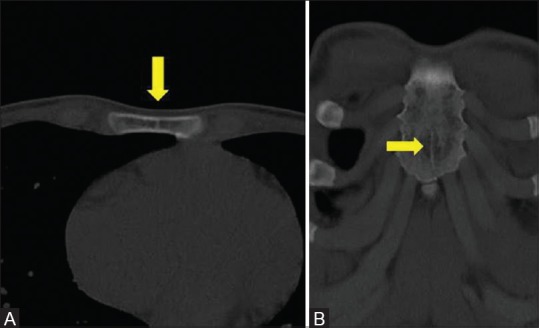
(A) Axial CT at the level of lower sternal body shows a midline sclerotic line consistent with sternal band (yellow arrow) (B) Reformatted oblique coronal CT of sternum shows a midline band in lower 1/3rd of body (yellow arrow)
Figure 15 (A and B).
(A) Axial CT of manubrium shows two sclerotic bands (yellow arrow) (B) Oblique coronal CT of manubrium shows two bands in midline (yellow arrow)
Sternal defect or notch
Focal defect or notch is usually seen in lower one-third of the body of sternum in the posterior aspect, with an incidence of 7.7% of the population. In some cases, it appears as recently closed or incomplete sternal foramen.[8] In CT, it appears as a round or wedge-shaped, well-corticated defect in the posterior sternal cortex [Figure 16A and B]. Although majority of such defects are seen in the posterior cortex, we encountered a case where there was both anterior and posterior cortical defect [Figure 17A–C]. Similar to sternal foramen, focal defect or notch can show photopenic area in bone scintigraphy.[22]
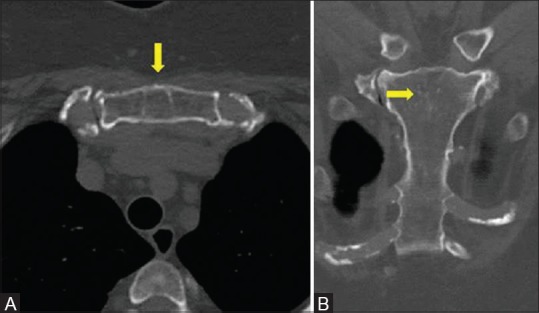
Figure 16 (A and B).
(A) Axial CT at lower 1/3rd of sternal body shows focal defect or notch in posterior cortex (yellow arrow) (B) Reformatted sagittal CT of sternum shows sternal defect or notch in posterior cortex (yellow arrow)
Figure 17 (A-C).
(A) Axial CT at the level of lower sternal body shows well defined defect involving anterior and posterior cortex (yellow arrow) (B) Reformatted sagittal CT of sternum shows sternal defect involving anterior and posterior cortex (yellow arrow) (C) Reformatted coronal CT of body of sternum shows the appearance of sternal defect in coronal plane (yellow arrow)
Xiphoid Ending, Ossification, and Xiphoid Ligament Calcification
Xiphoid ending is classified as single, double, or triple. The most common xiphoid ending is single, followed by double and triple ending[8,12] [Figure 18A–C]. In addition, xiphoid can vary in size (elongated process) and shape (e.g. ventral or dorsal deviation, hook like, reverse “S” shape).[12,28] We have encountered few cases of elongated xiphoid process measuring more than 4 cm in length, out of which one was reverse “S” shaped [Figures 19 and 20]. In another subject, the xiphoid process was laterally deviated, resembling a semilunar or “C” shape [Figure 21].
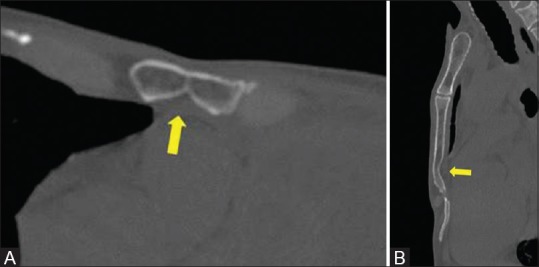
Figure 18 (A-C).
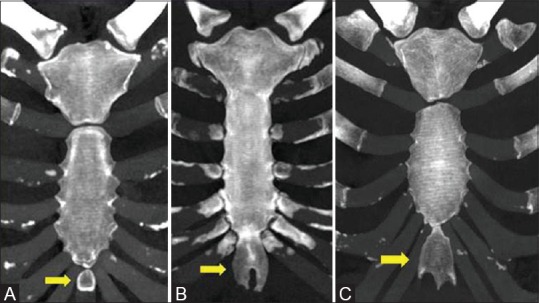
(A) Coronal MIP image of sternum shows single type of xiphoid ending (yellow arrow) (B) Coronal MIP image of sternum shows double type of xiphoid ending (yellow arrow) (C) Coronal MIP image of sternum shows triple type of xiphoid ending (yellow arrow)
Figure 19.
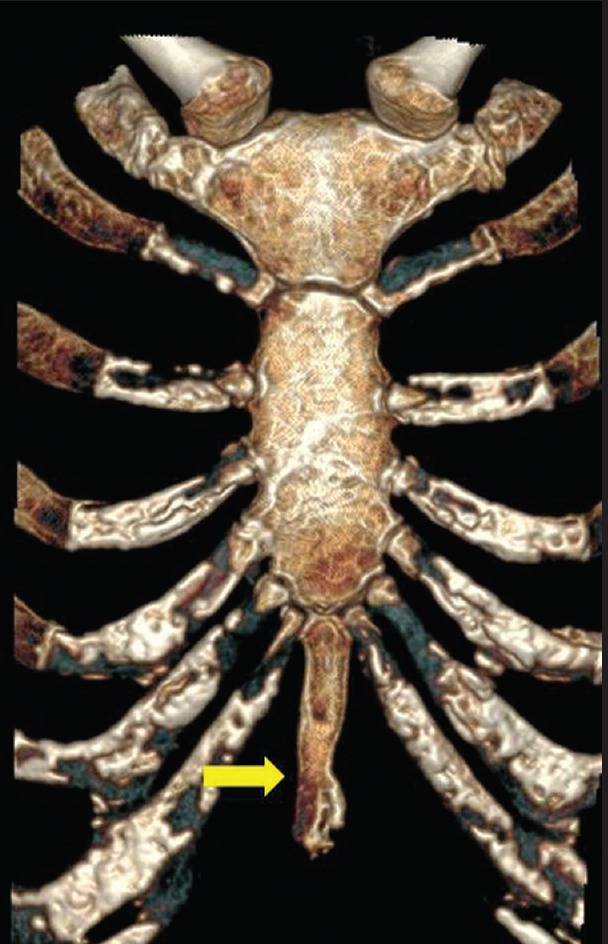
Coronal volume rendered image of sternum shows an elongated xiphoid process (yellow arrow)
Figure 20.
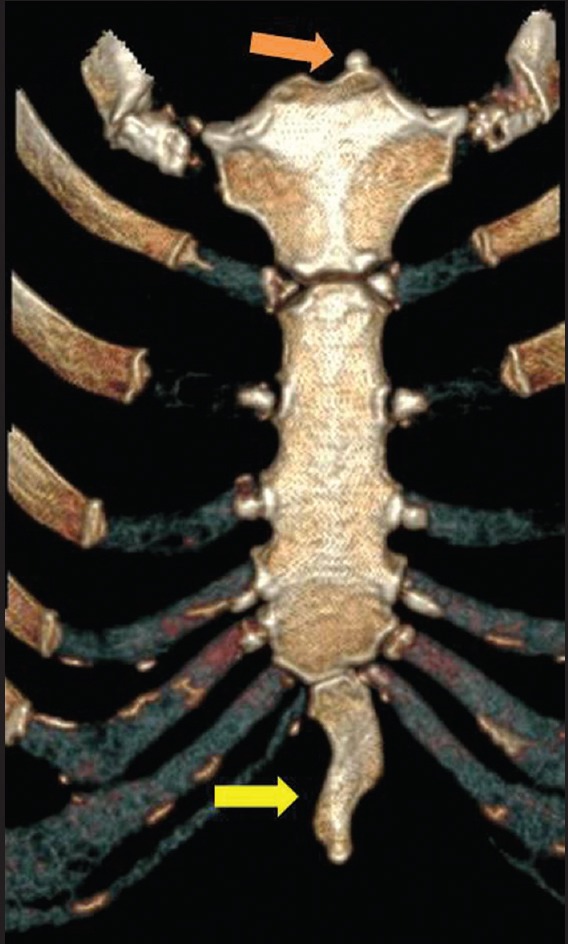
Coronal volume rendered image of sternum shows a elongated xiphoid process with reverse S shape (yellow arrow). Also note a suprasternal ossicle on left side (orange arrow)
Figure 21.

Coronal volume rendered image of sternum shows a semilunar or C shape Xiphoid process (yellow arrow)
Xiphoid ossification is usually complete in middle and older age. In one study, majority of subjects with no xiphoid ossification were under 30 years of age.[8] Xiphoid ligament calcification (unilateral and bilateral) is usually seen in older age group[8] (>50 years) [Figure 22A and B]. Xiphoid variations are usually of no clinical significance. However, review of literature shows elongated and ventrally deviated xiphoid process can be mistaken for an epigastric mass and cause pain[29,30] [Figure 23].
Figure 22 (A and B).
(A) Coronal MIP image of sternum shows unilateral xiphoid ligament calcification on right side (yellow arrow) (B) Coronal MIP image of sternum shows bilateral xiphoid ligament calcification (yellow arrow)
Figure 23.

Reformatted sagittal CT of sternum shows a elongated xiphoid process with ventral deviation (yellow arrow). Such variation can mimic an epigastric mass. Also note a sternal foramen (red arrow)
Sternal pseudoforamen and pseudocleft
Pseudoforamen and pseudocleft can be seen at manubriosternal and sternoxiphoidal junctions due to partial fusion [Figure 24]. They have no clinical significance.
Figure 24.
Coronal MIP image of sternum shows a pseudo foramen at sternoxiphoidal junction (yellow arrow)
Non-fusion of sternal body segments
Fusion of sternal body segments is usually complete by 25 years of age.[8,13] But non-fusion of sternal body segments can be seen in older age group [Figure 25].
Figure 25.
Coronal volume rendered image of sternum shows non fusion of upper and mid segment of sternal body in a 60 year old (white arrow)
Shape of sternal body
The body of sternum has three different shapes – longitudinal oval, flat, and “O” shape [Figures 26–28]. The shape is decided according to the proportion of basic and maximum breadths of the sternal body. The basic breadth is obtained as an average measurement of the upper and lower segments of the sternal body. The upper measurement is between second and third, whereas the lower measurement is between sixth and seventh costal notches, respectively.[11,31] In a cadaveric study by Selthofer et al., the longitudinal oval type was the standard shape of sternal body. Recently, in a study by Bayarogulları et al. that evaluated postnatal development of the sternum by MDCT, flat type was most commonly seen.
Figure 26.

Coronal volume rendered image of sternum shows longitudinal oval shape of sternal body
Figure 28.
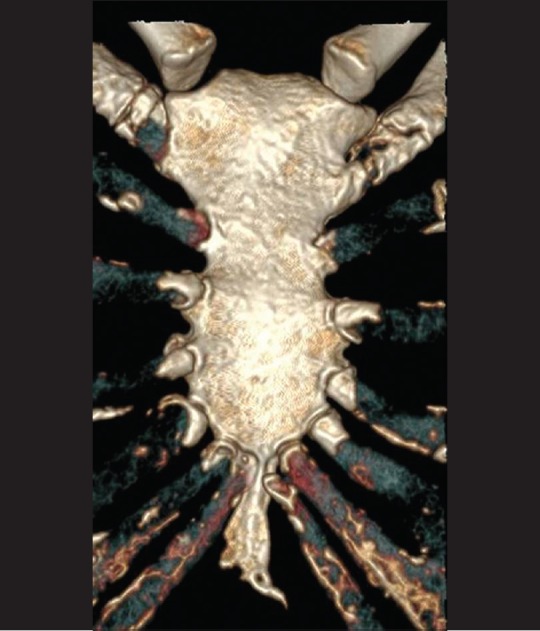
Coronal volume rendered image of sternum shows O shape of sternal body
Figure 27.
Coronal volume rendered image of sternum shows flat shape of sternal body. Also note the presence of sternal foramen (yellow arrow)
Conclusion
The use of multiplanar, curved reconstructions, MIP and VR images has made MDCT the primary imaging method of choice for the evaluation of sternum. Some of the key points regarding sternal variations are as follows.
Developmental fusion of manubriosternal joint in younger age group should not misinterpreted as pathological bony ankylosis
Identification of sternal foramen or cleft prior to invasive procedure of sternum prevents catastrophic complications
In bone scintigraphy, sternal foramen or defect can mimic lytic lesion
Elongated and ventrally deviated xiphoid process can present as an epigastric mass.
Thus, the radiologist should be familiar about such variations of clinical importance to prevent complications and misdiagnosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Cooper PD, Stewart JH, McCormick WF. Development and morphology of the sternal foramen. Am J Forensic Med Pathol. 1988;9:342–7. doi: 10.1097/00000433-198812000-00016. [DOI] [PubMed] [Google Scholar]
- 2.Moore MK, Stewart JH, McCormick WF. Anomalies of the human chest plate area. Radiographic findings in a large autopsy population. Am J Forensic Med Pathol. 1988;9:348–54. doi: 10.1097/00000433-198812000-00017. [DOI] [PubMed] [Google Scholar]
- 3.Ogawa K, Fukuda H, Omori K. Suprasternal bone (author's translation) Nihon Seikeigeka Gakkai Zasshi. 1979;53:155–64. [PubMed] [Google Scholar]
- 4.Keats TE, Anderson MW. 7th ed. Chicago, IL: Year Book; 2001. Atlas of Normal Roentgenvariants that May Simulate Disease; pp. 438–49. [Google Scholar]
- 5.Stark P. Midline sternal foramen: CT demonstration. J Comput Assist Tomogr. 1985;9:489–90. doi: 10.1097/00004728-198505000-00013. [DOI] [PubMed] [Google Scholar]
- 6.Schratter M, Bijak M, Nissel H, Gruber I, Schratter-Sehn AU. The foramen sternale: A minor anomaly-great relevance. Rofo. 1997;166:69–71. doi: 10.1055/s-2007-1015380. [DOI] [PubMed] [Google Scholar]
- 7.Haje SA, Harcke HT, Bowen JR. Growth disturbance of the sternum and pectus deformities: Imaging studies and clinical correlation. Pediatr Radiol. 1999;29:334–41. doi: 10.1007/s002470050602. [DOI] [PubMed] [Google Scholar]
- 8.Yekeler E, Tunaci M, Tunaci A, Dursun M, Acunas G. Frequency of sternal variations and anomalies evaluated by MDCT. AJR Am J Roentgenol. 2006;186:956–60. doi: 10.2214/AJR.04.1779. [DOI] [PubMed] [Google Scholar]
- 9.Stark P, Watkins GE, Hildebrandt-Stark HE, Dunbar RD. Episternal ossicles. Radiology. 1987;165:143–4. doi: 10.1148/radiology.165.1.3628759. [DOI] [PubMed] [Google Scholar]
- 10.Babinski MA, de Lemos L, Babinski MS, Gonçalves MV, De Paula RC, Fernandes RM. Frequency of sternal foramen evaluated by MDCT: A minor variation of great relevance. Surg Radiol Anat. 2015;37:287–91. doi: 10.1007/s00276-014-1339-x. [DOI] [PubMed] [Google Scholar]
- 11.Bayaroğulları H, Yengil E, Davran R, Ağlagül E, Karazincir S, Balcı A. Evaluation of the postnatal development of the sternum and sternal variations using multidetector CT. Diagn Interv Radiol (Ank) 2014;20:82–9. doi: 10.5152/dir.2013.13121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Akin K, Kosehan D, Topcu A, Koktener A. Anatomic evaluation of the xiphoid process with 64-row multidetector computed tomography. Skeletal Radiol. 2011;40:447–52. doi: 10.1007/s00256-010-1022-1. [DOI] [PubMed] [Google Scholar]
- 13.Larsen WJ. 2nd ed. New York, NY: Churchill Livingstone; 1997. Human Embryology; pp. 77–8. [Google Scholar]
- 14.O’Neal ML, Dwornik JJ, Ganey TM, Ogden JA. Postnatal development of the human sternum. J Pediatr Orthop. 1998;18:398–405. [PubMed] [Google Scholar]
- 15.Fokin AA. Cleft sternum and sternal foramen. Chest Surg Clin N Am. 2000;10:261–76. [PubMed] [Google Scholar]
- 16.Goodman LR, Teplick SK, Kay H. Computed tomography of the normal sternum. AJR Am J Roentgenol. 1983;141:219–23. doi: 10.2214/ajr.141.2.219. [DOI] [PubMed] [Google Scholar]
- 17.Gray H, Williams PL, Bannister LH. New York, NY: Churchill Livingstone; 1995. Gray's Anatomy: The Anatomical Basis of Medicine and Surgery. [Google Scholar]
- 18.Restrepo CS, Martinez S, Lemos DF, Washington L, McAdams HP, Vargas D, et al. Imaging appearances of the sternum and sternoclavicular joints. Radiographics. 2009;29:839–59. doi: 10.1148/rg.293055136. [DOI] [PubMed] [Google Scholar]
- 19.Stark P, Jaramillo D. CT of the sternum. AJR Am J Roentgenol. 1986;147:72–7. doi: 10.2214/ajr.147.1.72. [DOI] [PubMed] [Google Scholar]
- 20.Sebes JI, Salazar JE. The manubriosternal joint in rheumatoid disease. AJR Am J Roentgenol. 1983;140:117–21. doi: 10.2214/ajr.140.1.117. [DOI] [PubMed] [Google Scholar]
- 21.Parker VS, Malhotra CM, Ho G, Jr, Kaplan SR. Radiographic appearance of the sternomanubrial joint in arthritis and related conditions. Radiology. 1984;153:343–7. doi: 10.1148/radiology.153.2.6333045. [DOI] [PubMed] [Google Scholar]
- 22.Ishii S, Shishido F, Miyajima M, Sakuma K, Shigihara T, Kikuchi K, et al. Causes of photopenic defects in the lower sternum on bone scintigraphy and correlation with multidetector CT. Clin Nucl Med. 2011;36:355–8. doi: 10.1097/RLU.0b013e31820aa41b. [DOI] [PubMed] [Google Scholar]
- 23.Wolochow MS. Fatal cardiac tamponade through congenital sternal foramen. Lancet. 1995;346:442. doi: 10.1016/s0140-6736(95)92814-6. [DOI] [PubMed] [Google Scholar]
- 24.Bhootra BL. Fatality following a sternal bone marrow aspiration procedure: A case report. Med Sci Law. 2004;44:170–2. doi: 10.1258/rsmmsl.44.2.170. [DOI] [PubMed] [Google Scholar]
- 25.Halvorsen TB, Anda SS, Naess AB, Levang OW. Fatal cardiac tamponade after acupuncture through congenital sternal foramen. Lancet. 1995;345:1175. doi: 10.1016/s0140-6736(95)91004-2. [DOI] [PubMed] [Google Scholar]
- 26.Biswas G, Khandelwal NK, Venkatramu NK, Chari PS. Congenital sternal cleft. Br J Plast Surg. 2001;54:259–61. doi: 10.1054/bjps.2000.3527. [DOI] [PubMed] [Google Scholar]
- 27.James PA, McGaughran J. Complete overlap of PHACE syndrome and sternal malformation-vascular dysplasia association. Am J Med Genet. 2002;110:78–84. doi: 10.1002/ajmg.10398. [DOI] [PubMed] [Google Scholar]
- 28.Xie YZ, Wang BJ, Yun JS, Chung GH, Ma ZB, Li XJ, et al. Morphology of the human xiphoid process: Dissection and radiography of cadavers and MDCT of patients. Surg Radiol Anat. 2014;36:209–17. doi: 10.1007/s00276-013-1163-8. [DOI] [PubMed] [Google Scholar]
- 29.Yapici Ugurlar O, Ugurlar M, Ozel A, Erturk SM. Xiphoid syndrome: An uncommon occupational disorder. Occup Med (Lond) 2014;64:64–6. doi: 10.1093/occmed/kqt132. [DOI] [PubMed] [Google Scholar]
- 30.Maigne JY, Vareli M, Rousset P, Cornelis P. Xiphodynia and prominence of the xyphoid process. Value of xiphosternal angle measurement: Three case reports. Joint Bone Spine. 2010;77:474–6. doi: 10.1016/j.jbspin.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 31.Selthofer R, Nikolić V, Mrcela T, Radić R, Leksan I, Rudez I, et al. Morphometric analysis of the sternum. Coll Antropol. 2006;30:43–7. [PubMed] [Google Scholar]


