Abstract
The number of women undergoing breast implant procedures is increasing exponentially. It is, therefore, imperative for a radiologist to be familiar with the normal and abnormal imaging appearances of common breast implants. Diagnostic imaging studies such as mammography, ultrasonography, and magnetic resonance imaging are used to evaluate implant integrity, detect abnormalities of the implant and its surrounding capsule, and detect breast conditions unrelated to implants. Magnetic resonance imaging of silicone breast implants, with its high sensitivity and specificity for detecting implant rupture, is the most reliable modality to asses implant integrity. Whichever imaging modality is used, the overall aim of imaging breast implants is to provide the pertinent information about implant integrity, detect implant failures, and to detect breast conditions unrelated to the implants, such as cancer.
Keywords: Breast implants, implant rupture, magnetic resonance imaging, mammography, ultrasonography
Introduction
There is a very high procedural demand for breast augmentation surgeries, the main indications being reconstruction after mastectomy, correction of congenital malformations, and cosmetic augmentation. With the evolution of implant devices and surgical options, the breast radiologist is faced with specific challenges such as identification of the type of implant, diagnosis of implant-related complications, as well as diagnosis and follow-up of additional breast lesions such as cancer. In this article, we illustrate the imaging appearances of commonly used breast implants and of complications encountered due to the implants. In the end, we describe the prominent role of magnetic resonance imaging (MRI) in both screening and diagnosing implant failures.
Breast Prosthesis
Breast augmentation was first attempted in 1895, when Vincenz Czerny transplanted a lumbar lipoma to enhance a patient's breast after excision of a large fibroadenoma.[1] Since then, a wide variety of breast augmentation techniques have evolved, with saline and silicone prototypes being the most commonly performed today.
Breast implants may have a single lumen or double lumen. Most commonly encountered are single lumen implants which contain either silicone or saline as the filling [Figures 1 and 2]. Other variations such as double lumen (silicone on the inside with an outer saline component) [Figure 3], reverse double lumen (saline on the inside with an outer silicone component), and stacked implants (presence of more than one implant per breast) may also be encountered. All implants have an outer silicone membrane or shell. After placement, a thin fibrous capsule normally forms around the prosthesis as a physiological response to foreign body (encapsulation). The main surgical planes for implant placement are subglandular (in front of pectoralis major muscle) or retropectoral (behind the pectoralis major muscle) planes [Figures 4 and 5].
Figure 1.
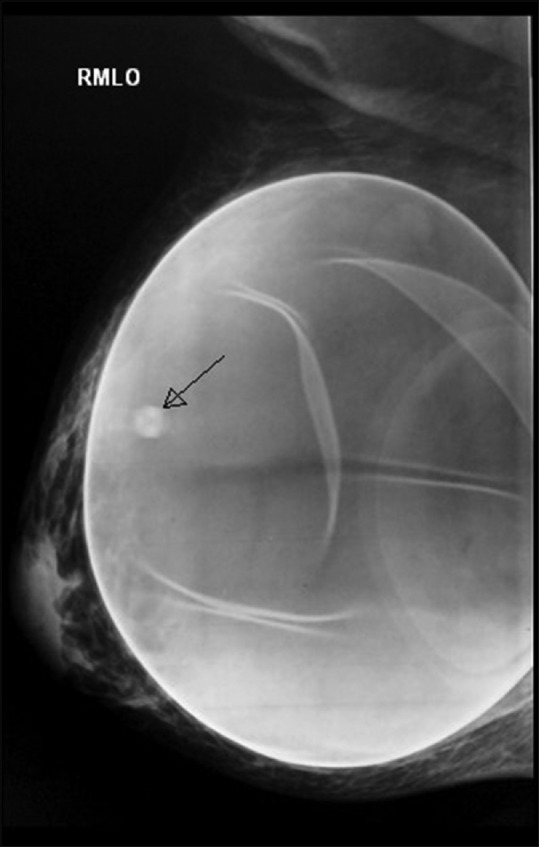
Mammogram showing single lumen saline breast implant. Right mediolateral oblique (MLO) view showing less radiodense saline implant. A valve is seen as a round density with a slightly lucent center superimposed on the implant (arrow)
Figure 2.
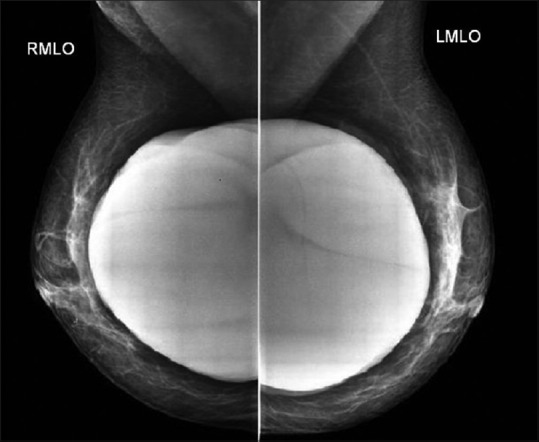
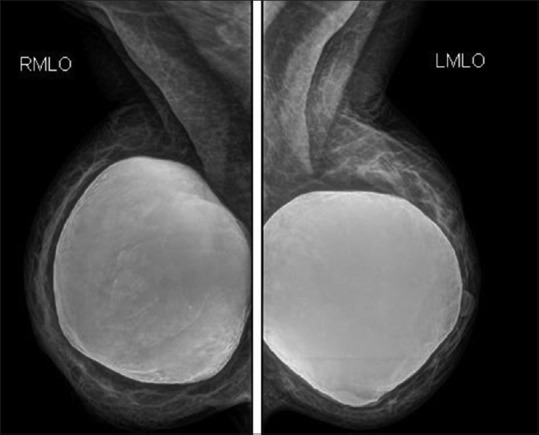
Mammogram showing single lumen silicone breast implants. Bilateral mediolateral oblique (MLO) views showing radiodense silicone implants with no visible distinction between the shell and the gel filler
Figure 3.
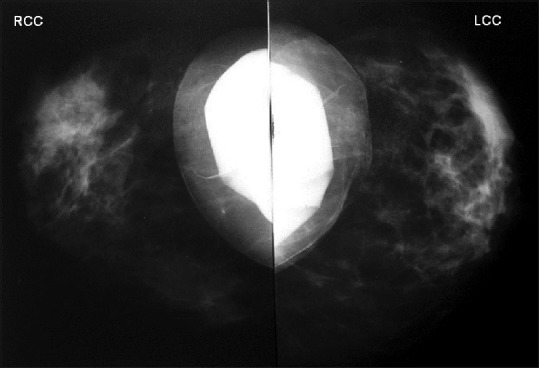
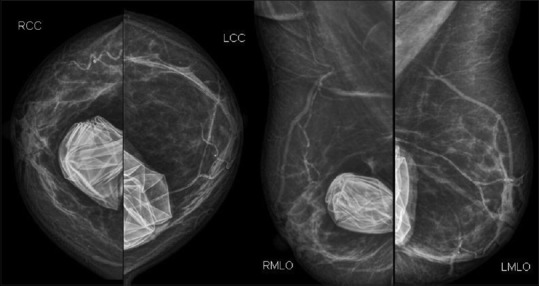
Mammogram showing double lumen breast implants. Bilateral craniocaudal (CC) views showing double lumen breast implants with an inner silicone lumen and saline on the outside
Figure 4.
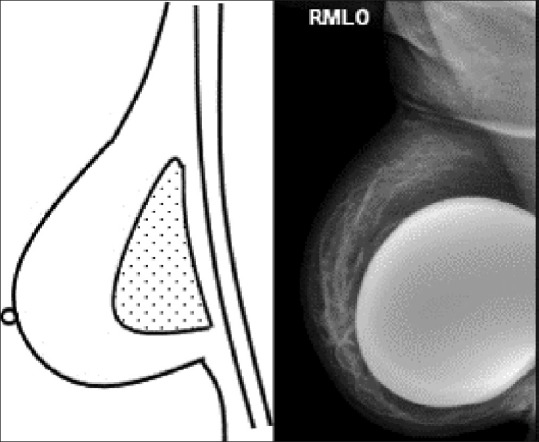
Schematic representation and mammogram showing a subglandular silicone breast implant. The pectoralis major muscle is seen diving posterior to the implant. In the right mediolateral oblique (MLO) view, the implant is seen anterior to pectoralis major muscle
Figure 5.
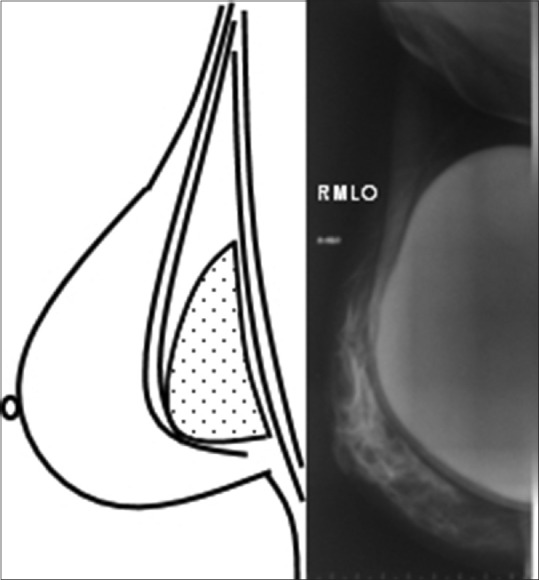
Schematic representation and mammogram showing a retropectoral silicone breast implant. The pectoralis major muscle overlies the implant in the diagram. In the right mediolateral oblique (MLO) view, the pectoralis major muscle is seen anterior to the implant
On mammography, saline implants appear as oval masses with a dense outer silicone envelope and a less radio-opaque center. Often a valve is visible, which is used to fill the saline implant [Figure 1]. Normal membrane foldings may be seen, as also partially the glandular tissue may be seen through the implant depending on the penetration used. Silicone implants are seen as dense oval masses, so that a separate envelope or accompanying folds are not visualized on mammography [Figure 2]. The screening mammogram should include implant displaced (Eklund technique), craniocaudal (CC), and mediolateral oblique (MLO) views, in addition to the standard CC and MLO views[2] [Figure 6]. Displacing the implant allows more breast tissue to be visualized than the standard compression views.
Figure 6 (A and B).
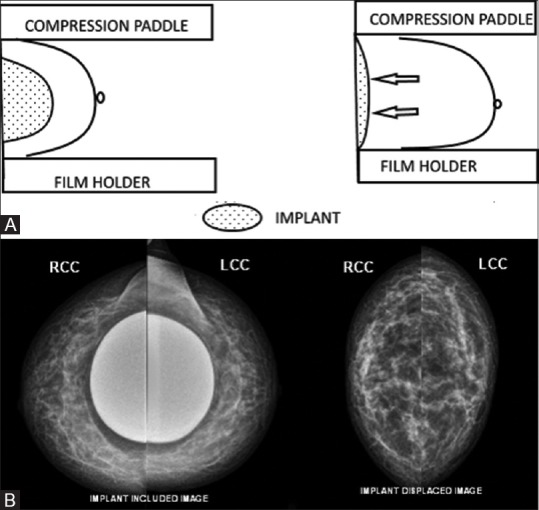
Schematic diagram showing Eklund technique (A). The displacement technique introduced by Eklund to facilitate mammography in women with implants allows slightly more tissue to be visualized with displacement (arrows) (on the left) than with standard compression mammography (on the right). Bilateral craniocaudal (CC) views showing implant included and implant displaced images (B)
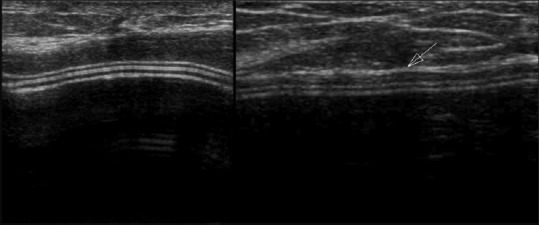
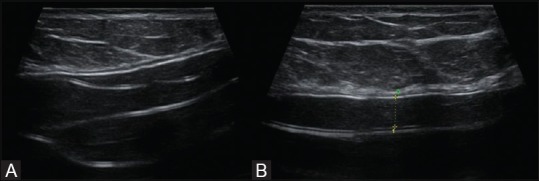
Ultrasound (USG) evaluation of breast implants includes assessing the morphology, contour, content, and peri-implant tissues and axillae. The transverse to longitudinal ratio of the implant is calculated; the smooth undulations of the envelope (radial folds), the homogeneity of the implant lumen, and signs of free silicone or silicone granulomas in the axillae or breast tissue are checked. On USG, saline and silicone implants have a similar appearance. They appear anechoic surrounded by a linear echogenic envelope [Figure 7]. Low-level echoes may be seen within the implant. Reverberation artifacts seen anteriorly and echoes produced behind the implant may be confused with loss of implant integrity by an inexperienced interpreter. The implant shell may be seen as a single echogenic line or parallel echogenic lines. The fibrous capsule is visualized as two parallel echogenic lines superficial to the implant surface [Figure 8]. Normal undulations of the envelope may be seen as wavy echogenic lines with or without minimal intervening fluid [Figure 9].
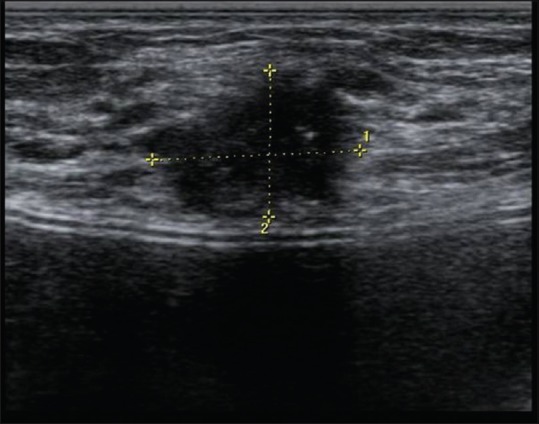
Figure 7.
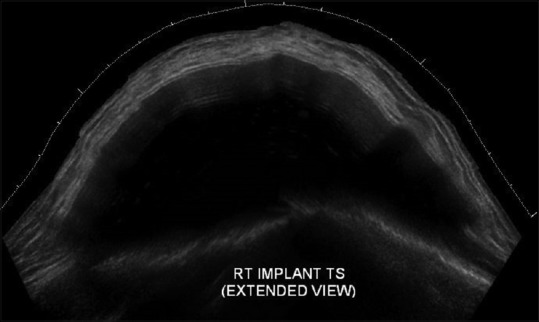
Ultrasound image (extended field of view) of a woman with intact implant depicting an ellipsoid shape of the implant with an anterior convex shape of the anterior and posterior margins of the implant
Figure 8.
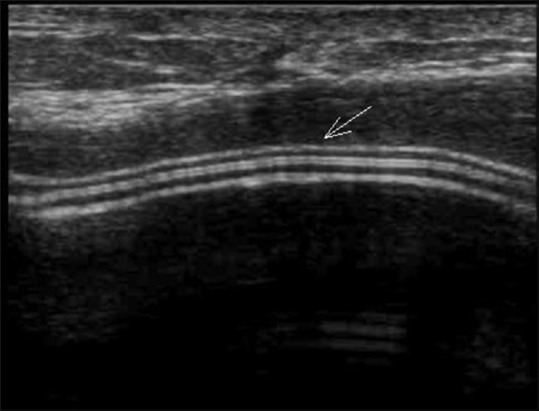
Transverse ultrasound image of a woman with intact implant. Normal contour of the implant is seen with the implant shell and the fibrous capsule visualized as parallel echogenic lines (arrowed)
Figure 9.
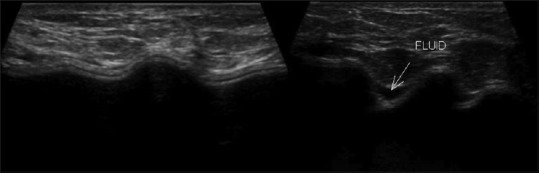
Transverse ultrasound images of a woman with intact implant showing normal undulations and minimal fluid (arrow) between the implant shell and the capsule
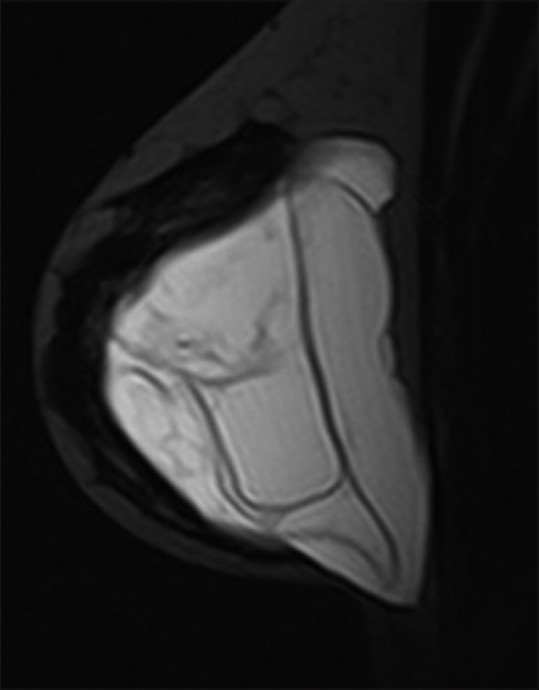
Apart from its high spatial and soft tissue resolution and lack of ionizing radiation, the ability of MRI to suppress or emphasize the signal from water, fat, or silicone makes it the most ideal modality for evaluating breast implants.[3] A dedicated breast coil should be used to obtain high-resolution images. Saline implants follow fluid signal on all sequences. However, MRI is not used for assessing the integrity of saline implants because a ruptured saline implant is a clinical diagnosis presenting as an acute reduction in breast size.[4] Silicone appears hypointense on T1-weighted image and hyperintense on T2-weighted image. The envelope and capsule have low signal on all sequences. MRI often shows low signal intensity radial folds extending to the periphery of the implant. Radial folds and periprosthetic fluid are considered normal findings and should not be mistaken for rupture[5] [Figure 10].
Figure 10 (A-C).
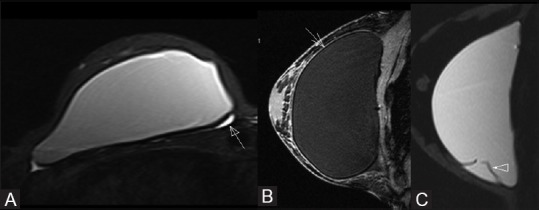
MRI of intact implants. The axial T2-weighted TIRM image (A) of the breast shows minimal normal periprosthetic fluid collection (closed arrow). The low signal intensity capsule (open arrow) can be very well appreciated in the sagittal T2-weighted image (B). Sagittal T2-weighted TIRM image of breast demonstrating a silicone gel implant with normal radial folds (arrowhead) (C). Periprosthetic fluid and radial folds are not in themselves indicative of rupture
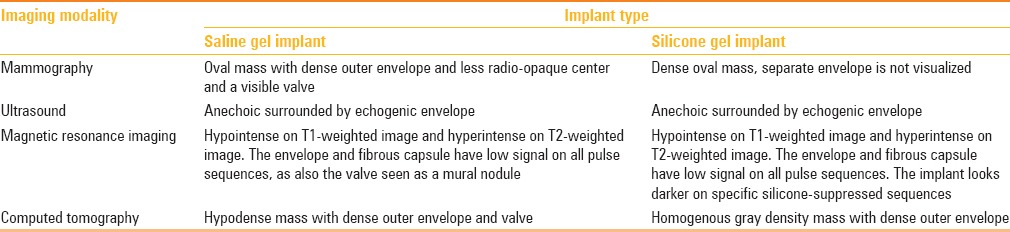
Table 1 summarizes the imaging features of saline and silicone breast implants.
Table 1.
Summary of imaging appearance of breast implants
Implants placed for congenital abnormalities such as Poland syndrome may have an asymmetric appearance and should not be confused with malpositioning [Figure 11].
Figure 11.
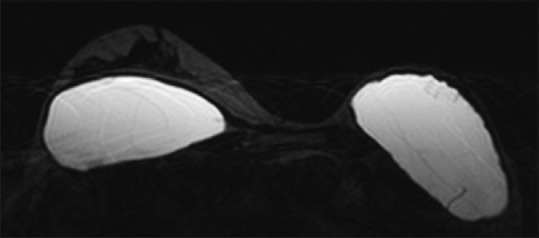
Bilateral breast MRI of a woman with Poland syndrome. Right sided retropectoral and left sided subglandular silicone gel implants placed for cosmesis in the patient with Poland syndrome. Note the absence of left breast tissue and chest wall muscle
Implant Complications
Early post-surgical complications are infection and hematoma. Delayed complications include capsular contracture, implant rupture, and gel bleed. In 2006, the Food and Drug Administration (FDA) recommended that women with silicone gel breast implants receive MRI screening 3 years after they receive a new implant and every 2 years after that.[6] However, the cost of these screening examinations over the lifetime is very high.
Infection
Infection is a significant complication related to breast implants. After breast esthetic surgery, up to 2.9% of patients develop a surgical site infection with an even higher rate of 1–53% noted after breast reconstruction surgery.[7] The majority of the cases occur in the early postoperative period presenting with breast pain, swelling, and erythema. USG may reveal an abscess visualized as irregular hypoechoic fluid collection with internal debris. MRI findings suggestive of implant infection include skin thickening, edema, and capsular enhancement. Peri-implant complex fluid collections may also be seen.
Hematoma
Breast implant surgery can be complicated by hematoma formation with a majority of cases occurring in the early postoperative period or it could be post-traumatic. On mammography, well-defined hyperdense or heterogeneous density masses may be seen. USG, computed tomography (CT), and MRI can be used to demonstrate the hematoma.
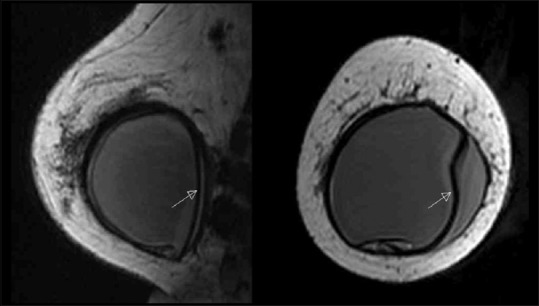
Capsular contracture
Capsular contracture is the most common delayed complication noted in patients with smooth-walled silicone prosthesis. It is the abnormal constriction of the fibrous capsule that surrounds the breast implant resulting in hardening and deformity of the implant. Predominantly a clinical diagnosis, it presents with a distorted, tough and sometimes painful breast. On mammography, the implant may appear spherical rather than oval in shape with transverse diameter measuring less than two times the anteroposterior diameter of the implant[8] [Figure 12]. It may develop unusual areas of bulging, irregularity, or tenting. On USG and MRI, loss of the normal triangular configuration of the implants may be seen with an increased anteroposterior diameter of the implant [Figures 13 and 14]. Thickening of the echogenic fibrous capsule and increase in the number of radial folds [Figures 15 and 16] may be noted. Peri-implant calcifications may be seen [Figure 17].
Figure 12.
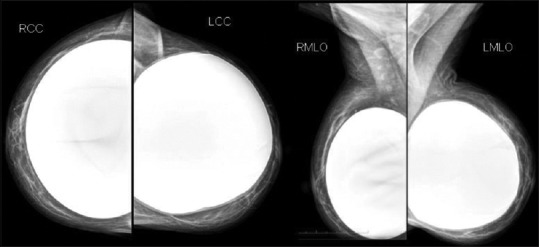
Bilateral mammography of a woman with left implant showing capsular contracture craniocaudal (CC) and mediolateral oblique (MLO) views. Bilateral craniocaudal (CC) and mediolateral oblique (MLO) views showing subglandular silicone gel implants. The left implant is spherical in shape as compared to the right implant
Figure 13.
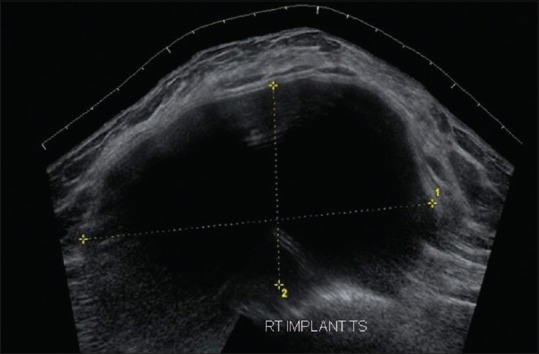
Transverse ultrasound image of a woman with capsular contracture of right implant. The implant appears spherical in shape with an increased anteroposterior diameter
Figure 14.
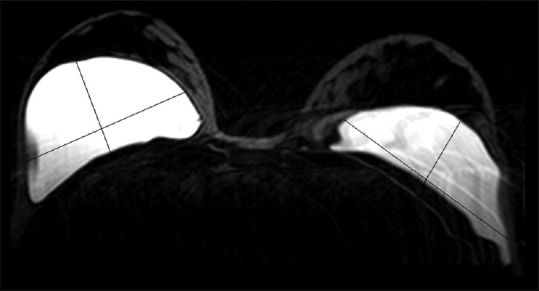
Bilateral breast MRI of a woman with capsular contracture of right implant. Axial STIR image demonstrates subglandular silicone gel implants. The left implant is oval in shape with transverse diameter more than anteroposterior diameter. Note the spherical shaped right implant with an increased anteroposterior diameter compared to its transverse diameter suggestive of capsular contracture
Figure 15.
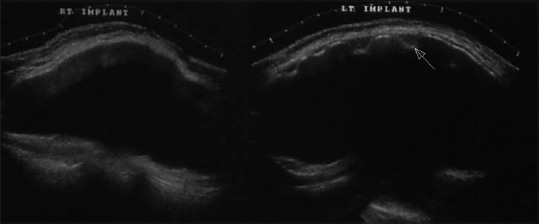
Transverse ultrasound image of a woman with capsular contracture. The left implant (arrow) shows increase in the number of radial folds suggestive of capsular contracture. The right implant is normal
Figure 16.
Transverse ultrasound image of a woman with capsular contracture. The image on the left shows normal thickness of the fibrous capsule. The image on the right shows increased thickness of the fibrous capsule (arrow) suggestive of capsular thickening in a patient with capsular contracture
Figure 17.
Bilateral mediolateral oblique views. Bilateral subglandular silicone gel implants are visualized with calcifications adherent to the fibrous capsule. The left breast implant shows a bulge inferiorly
Implant rupture
Rupture is one of the main complications of breast implants. The incidence of breast implant rupture increases with implant age with most implant ruptures occurring 10–15 years after placement.[8] Saline implant ruptures are easily diagnosed clinically as the implant significantly decreases in size with extrusion of fluid [Figure 18]. Silicone implant ruptures can be difficult to identify. Breast pain on physical examination of implants is a strong predictor of rupture, but absence of pain does not exclude rupture. The rupture is classified into two categories depending on the location of the silicone with respect to the fibrous capsule [Table 2].
Figure 18.
Bilateral craniocaudal (CC) and mediolateral oblique (MLO) views showing bilateral subglandular saline implants with collapsed and folded implant envelope
Table 2.
Intracapsular rupture versus extracapsular rupture
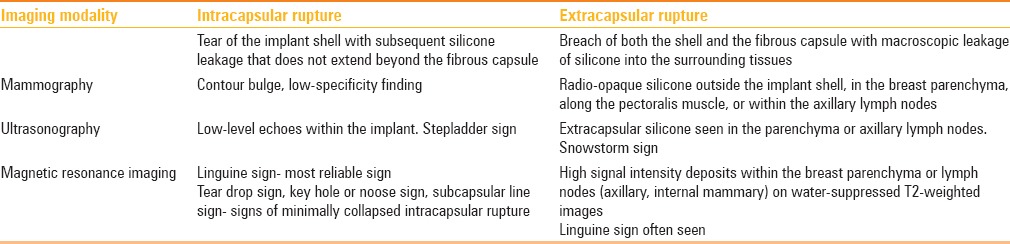
Intracapsular rupture
This is the most common type (77–89%).[9] The integrity of the implant is breached, but the fibrous capsule is intact; so the leaked silicone is confined within the fibrous capsule. Mammography does not confidently detect intracapsular rupture. A contour bulge may indicate intracapsular rupture; however, the differential diagnosis includes implant herniation. On USG, horizontally stacked echogenic lines traversing through the implant interior at various levels, termed the “stepladder sign” is seen [Figure 19]. Low-level echoes in the central portion of the prosthesis may be observed, but they can also be seen in intact silicone breast implants; therefore, they should be interpreted with caution. Isoechoic silicone may be found between the fibrous capsule and the implant surface, indicative of minimal prosthetic collapse; however, these findings should be confirmed with MRI [Figure 20]. The most reliable sign on MRI for intracapsular rupture is the presence of multiple curvilinear low signal intensity lines within the T2 bright silicone, called the “linguine sign” [Figure 21]. The curvilinear lines represent collapsed implant membrane floating within the silicone gel.[10] Signs of minimally collapsed intracapsular rupture include the “tear drop sign,” the “key hole or noose sign,” and the “subcapsular line sign.” The tear drop sign represents focal silicone invagination between the inner shell and the fibrous capsule, with the margins of the collapsing shell in contact with one another. The key hole or noose sign represents focal invagination of silicone, with the margins of the collapsing shell not in contact with one another [Figure 22]. Subcapsular line sign represents a thin layer of silicone between the shell and the fibrous capsule [Figure 23].
Figure 19.

Transverse ultrasound image of a woman with intracapsular rupture. The ultrasound image shows stacked echogenic lines corresponding to collapsed envelope of silicone implant termed the “step ladder” sign. This imaging finding is most reliable for intracapsular rupture
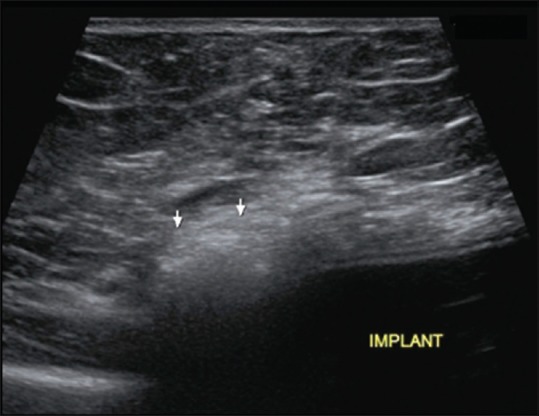
Figure 20 (A and B).
Transverse ultrasound image of a woman with intracapsular rupture. The ultrasound shows diffuse low level internal echoes within the implant (A). Isoechoic silicone between the fibrous capsule and the implant shell in the same patient (B). Although this sign may be observed in patients with intracapsular rupture, it may also be seen in intact silicone gel implants and this should be interpreted with caution
Figure 21.
MRI of a woman with intracapsular rupture. Sagittal T2-weighted TIRM image shows typical “linguine sign” representing collapsed implant shell seen as multiple curvilinear low signal intensity echoes within the bright T2 silicone
Figure 22.
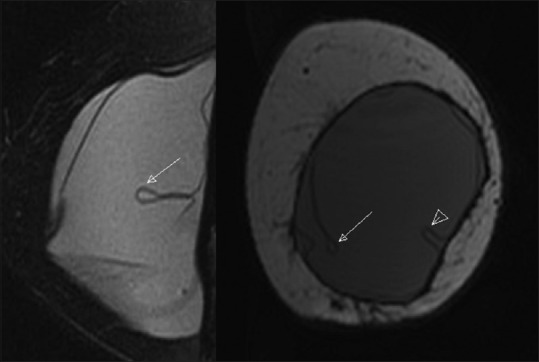
MRI of a woman with intracapsular rupture. Sagittal T2-weighted fat saturated image demonstrates a “teardrop sign” (arrow). When walls of collapsing implant shell abut each other and small quantity of silicone is identified between these layers, this MR appearance is termed “teardrop sign.” The coronal T2-weighted image demonstrates a “noose sign” (arrowhead) and a “teardrop sign” (arrow). This sign differs from teardrop sign in that the margins of the collapsing implant shell do not abut each other
Figure 23.
MRI of a woman with intracapsular rupture. Sagittal and axial T1-weighted image demonstrates a “subcapsular line” sign (arrow) representing a thin layer of silicone interposed between the shell and the fibrous capsule
Extracapsular rupture
Extracapsular rupture is defined as rupture of both the implant shell and the fibrous capsule with macroscopic silicone leakage that extends beyond the fibrous capsule into the surrounding tissues. On mammography, extracapsular rupture is seen as radiodense silicone extending away from the implant shell into the breast parenchyma along the pectoralis muscle or within the axillary lymph nodes [Figure 24]. On USG, large conglomerates of extracapsular silicone are seen as hyperechoic or anechoic masses, almost indistinguishable from cysts. More frequently, free silicone appears as an echogenic nodule with well-defined anterior margin and posterior dirty acoustic shadowing, termed as “snowstorm sign” [Figure 25]. On MRI, extracapsular free silicone is visualized as discrete foci of isointense to low signal intensity on T1 fat-suppressed images and of high signal intensity on water-suppressed T2-weighted images [Figure 26]. Silicone granulomas may have similar enhancement to breast carcinoma and sometimes require biopsy.
Figure 24.
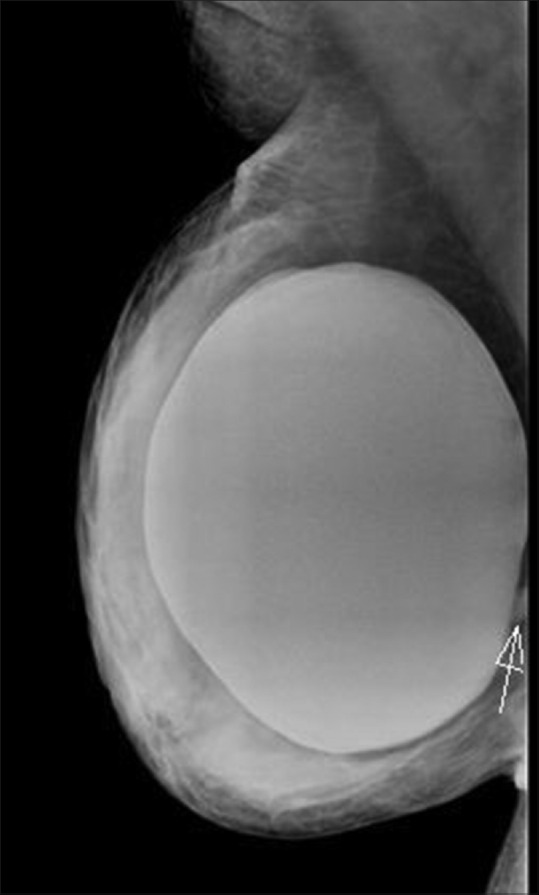
Right mediolateral oblique (MLO) view shows a blob of silicone (arrow) extruded into breast tissue in extracapsular rupture
Figure 25.
Transverse ultrasound image shows the classic “snowstorm sign” of extracapsular rupture. An echogenic mass (arrows) with dirty posterior shadowing is seen
Figure 26.
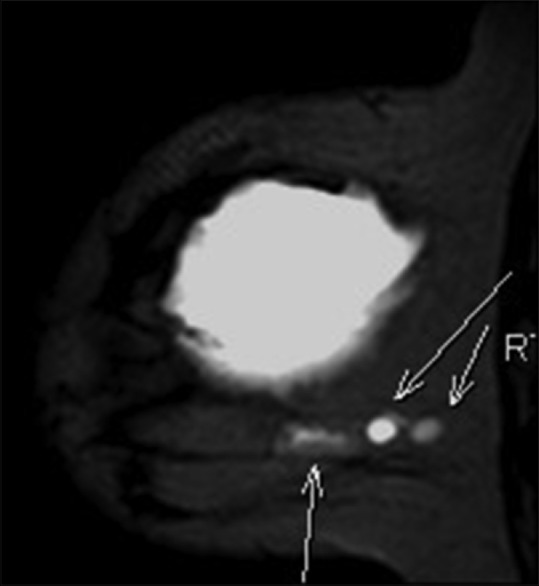
MRI of a woman with extracapsular rupture. Sagittal STIR image shows extracapsular free silicone conglomerates (arrows) in breast parenchyma
Mammography has limited value for assessing intracapsular rupture, but it is useful for detecting extracapsular rupture especially when the silicone has migrated away from the implant shell. The sensitivity of mammography in detecting implant ruptures varies between 25–30% and 68%.[11] USG has a better sensitivity than mammography in detecting implant ruptures. One limitation is the evaluation of posterior wall of breast implants and the tissue posterior to the implant. USG has a sensitivity of 50–77% and a specificity of 55–84% in detecting implant rupture.[11] Also, the silicone granulomas following an extracapsular rupture may hinder the evaluation of a new implant. MRI is the imaging test with the highest sensitivity and specificity to review the integrity of breast implants. It has a reported sensitivity of 72–94% and specificity of 85–100% in detecting implant rupture.[11] MRI has evolved to be most accurate tool in detecting free silicone, its relationship to surrounding structures, and in evaluating implant ruptures.[12]
Gel bleed
Gel bleed is the normal transudation of microscopic amounts of silicone through an intact breast prosthesis membrane into the surrounding tissues and lymphatics.[12] Gel bleed is difficult to identify on USG and MRI unless it is extensive.
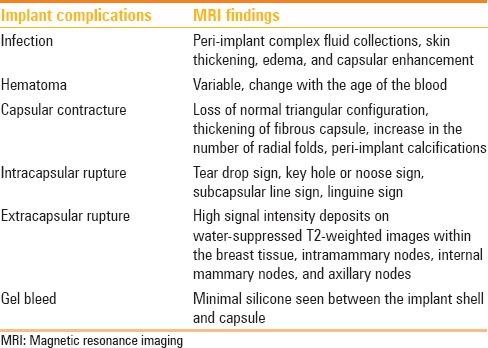
Table 3 provides a checklist of MRI findings in implant complications.
Table 3.
Magnetic resonance imaging findings in implant complications
Concurrent Breast Conditions
The remaining breast is a potential site for disease, benign or malignant. Cysts, fibroadenomas, cancer, all can occur. Cysts are a very common finding in the breast parenchyma with or without implants. Fibroadenomas have the same imaging appearance as in women without implants. Breast implants are not associated with an increased risk of breast carcinoma[13] [Figure 27]. There is no difference in survival rates in women with breast cancer and implants compared to those without implants. A few published cases have been reported about the associations between anaplastic large cell lymphoma (ALCL) and breast implants (both silicone and saline); however, more data is required to confirm its linkage with breast implants.[14] The presence of the implant may impair the ability of mammography or USG for cancer detection. A correlation between physical examination and mammography findings should be first done. Any palpable abnormality can then be subjected to a USG or contrast-enhanced MRI. Suspicious findings should be further evaluated with biopsy.
Figure 27.
Transverse ultrasound image shows an irregular hypoechoic mass in a woman with breast implant, which was malignant
Role of Preoperative MRI-based Breast Volumetry for Immediate Breast Reconstruction
Restoring volumetric symmetry is one of the main objectives of breast esthetic and reconstructive surgery. Various methods for preoperative breast volume estimation have been described previously in the literature, including anthropometry, USG, mammography, CT, liquid volume displacement technique, thermoplastic methods, MRI, and three-dimensional breast surface imaging.[15] MRI-based breast volumetry is a simple and convenient solution to assessing breast volume and composition of breast tissue for initial operative planning and post-surgical follow-up and calculating the implant size in patients with missing documentation of a previously implanted device. Breast MRI has been shown to have the highest correlation with the actual breast volume.[16] The entire augmented breast with the elliptical implant in situ is traced onto axial slices. The breasts with the implant inside are traced on a bilateral axial slice and the borders of the implant are outlined. After marking all slices, a software program is used to determine the implant volume as well as the volume of the entire breast.
Conclusion
Since the number of breast implant procedures is increasing and an increasing number of patients present for assessing implant integrity, a radiologist should be familiar with the spectrum of appearances of the complications. The imaging appearances of the common breast implants and their complications are varied. MRI is the modality of choice for evaluation of silicone breast implant integrity. In symptomatic patients, after an initial evaluation with mammography and USG, non-contrast MRI is recommended to rule out the diagnosis of rupture. Dynamic contrast-enhanced MRI is indicated in patients with breast reconstruction surgeries after mastectomy for breast cancer or in breast implant patients with suspicious masses. MRI is not recommended as a screening modality for implant rupture in asymptomatic women with breast implants.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Champaneria MC, Wong WW, Hill ME, Gupta SC. The evolution of breast reconstruction: A historical perspective. World J Surg. 2012;36:730–42. doi: 10.1007/s00268-012-1450-2. [DOI] [PubMed] [Google Scholar]
- 2.Eklund GW, Busby RC, Miller SH, Job JS. Improved imaging of the augmented breast. AJR Am J Roentgenol. 1988;151:469–73. doi: 10.2214/ajr.151.3.469. [DOI] [PubMed] [Google Scholar]
- 3.Amano Y, Aoki R, Kumita S, Kumazaki T. Silicone-selective multishot echo-planar imaging for rapid MRI survey of breast implants. Eur Radiol. 2007;17:1875–8. doi: 10.1007/s00330-006-0533-6. [DOI] [PubMed] [Google Scholar]
- 4.Baek WY, Lew DH, Lee DW. A retrospective analysis of ruptured breast implants. Arch Plast Surg. 2014;41:734–9. doi: 10.5999/aps.2014.41.6.734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Venkataraman S, Hines N, Slanetz PJ. Challenges in mammography: Part 2, multimodality review of breast augmentation – Imaging findings and complications. AJR Am J Roentgenol. 2011;197:W1031–45. doi: 10.2214/AJR.11.7216. [DOI] [PubMed] [Google Scholar]
- 6.Chung KC, Malay S, Shauver MJ, Kim HM. Economic analysis of screening strategies for rupture of silicone gel breast implants. Plast Reconstr Surg. 2012;130:225–37. doi: 10.1097/PRS.0b013e318254b43b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rubino C, Brongo S, Pagliara D, Cuomo R, Abbinante G, Campitiello N, et al. Infections in breast implants: A review with a focus on developing countries. J Infect Dev Ctries. 2014;8:1089–95. doi: 10.3855/jidc.3898. [DOI] [PubMed] [Google Scholar]
- 8.Berg WA, Caskey CI, Hamper UM, Anderson ND, Chang BW, Sheth S, et al. Diagnosing breast implant rupture with MR imaging, US, and mammography. Radiographics. 1993;13:1323–36. doi: 10.1148/radiographics.13.6.8290727. [DOI] [PubMed] [Google Scholar]
- 9.Brown SL, Middleton MS, Berg WA, Soo MS, Pennello G. Prevalence of rupture of silicone gel breast implants revealed on MR imaging in a population of women in Birmingham, Alabama. AJR Am J Roentgenol. 2000;175:1057–64. doi: 10.2214/ajr.175.4.1751057. [DOI] [PubMed] [Google Scholar]
- 10.Gorczyca DP, DeBruhl ND, Mund DF, Bassett LW. Linguine sign at MR imaging: Does it represent the collapsed silicone implant shell? Radiology. 1994;191:576–7. doi: 10.1148/radiology.191.2.8153345. [DOI] [PubMed] [Google Scholar]
- 11.Moschetta M, Telegrafo M, Cornacchia I, Vincenti L, Ranieri V, Cirili A, et al. PIP breast implants: Rupture rate and correlation with breast cancer. G Chir. 2014;35:274–8. [PMC free article] [PubMed] [Google Scholar]
- 12.Lindenblatt N, El-Rabadi K, Helbich TH, Czembirek H, Deutinger M, Benditte-Klepetko H. Correlation between MRI results and intraoperative findings in patients with silicone breast implants. Int J Womens Health. 2014;6:703–9. doi: 10.2147/IJWH.S58493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bryant H, Brasher P. Breast implants and breast cancer – Reanalysis of a linkage study. N Engl J Med. 1995;332:1535–9. doi: 10.1056/NEJM199506083322302. [DOI] [PubMed] [Google Scholar]
- 14.Weathers WM, Wolfswinkel EM, Hatef DA, Lee EI, Hollier LH, Brown RH. Implant-associated anaplastic large cell lymphoma of the breast: Insight into a poorly understood disease. Can J Plast Surg. 2013;21:95–8. doi: 10.1177/229255031302100209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Herold C, Reichelt A, Stieglitz LH, Dettmer S, Knobloch K, Lotz J, et al. MRI-based breast volumetry-evaluation of three different software solutions. J Digit Imaging. 2010;23:603–10. doi: 10.1007/s10278-009-9264-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yoo A, Minn KW, Jin US. Magnetic resonance imaging-based volumetric analysis and its relationship to actual breast weight. Arch Plast Surg. 2013;40:203–8. doi: 10.5999/aps.2013.40.3.203. [DOI] [PMC free article] [PubMed] [Google Scholar]


