Abstract
Background.
Acute respiratory infections (ARIs) are the most common symptomatic reason to seek ambulatory care, but many ARI visits may not be necessary.
Objective.
To measure the proportion of primary care ARI visits that may not require an office visit.
Methods.
We identified 58398 ARI visits to 14 primary care practices between May 2011 and May 2012 and randomly selected 500 visits, 439 of which were new ARI visits. We separated non-visit-required information [e.g. history of present illness (HPI), past medical history, etc.] from information that required an office visit (e.g. physical exam, testing, etc.). Reviewing non-visit-required information, we identified the diagnosis (HPI diagnosis) and whether office visit appeared necessary. Independently, we reviewed the visit-required information and determined if the visit changed antibiotic management.
Results.
Based on non-visit-required information, 72% (316/439) of visits did not appear to require an office visit. The most common diagnoses were non-specific upper respiratory infection (39%), sinusitis (24%) and acute bronchitis (22%). The HPI diagnosis was an exact match for clinicians’ diagnosis in 67% (213/316) of visits. After reviewing the visit-required information, antibiotic management did not change for 87% (276/316) of visits. For the remaining 13% (40/316) for which the visit changed management, the clinician prescribed an antibiotic for an antibiotic-appropriate diagnosis (65%; 26/40); prescribed an antibiotic for a non-antibiotic-appropriate diagnosis (25%; 10/40); or avoided an antibiotic prescription for patients with an HPI diagnosis of sinusitis (10%; 4/40).
Conclusion.
About two-thirds of primary care ARI visits may not be necessary for appropriate antibiotic management.
Key words. Antibacterial agents, clinical decision-making, health care costs, patient acceptance of health care, primary health care, respiratory tract infections.
Introduction
Acute respiratory infections (ARIs) include non-specific upper respiratory infections (NS URIs), otitis media, sinusitis, pharyngitis, acute bronchitis, influenza and pneumonia. Most ARIs are self-limited, do not require medical evaluation and can be managed with over-the-counter medications. Despite this, ARIs strain the health care system. ARIs are the most common reason patients seek ambulatory care in the USA, accounting for ~120 million visits per year or about 10% of all ambulatory visits (1).
For patients, clinic visits are inconvenient, requiring time and costing money (2). ARI visits also result in antibiotic prescriptions (3), many of which are inappropriate (4,5). ARIs account for 50% of antibiotic prescriptions to adults and 75% of antibiotic prescriptions to children (6). Unnecessary antibiotics increase health care costs, expose patients to adverse drug reactions and increase the prevalence of antibiotic-resistant bacteria (7,8).
Despite the fact that patients make visits for self-limited ARIs, ARI visits are inconvenient and expensive, and ARI visits often result in inappropriate antibiotic prescriptions, it is unknown what proportion of ARI visits are necessary. To measure the proportion of ARI visits that could have been managed without a visit, we conducted a retrospective chart review.
Methods
Setting and overview
The Brigham and Women’s Primary Care Practice-Based Research Network includes 14 academically affiliated practices in eastern Massachusetts staffed mainly by general internists who care for mostly adult patients. Patients who made visits in the network were 64% women, 66% White, 12% Black and 10% Latino; 67% had private insurance, 24% had Medicare and 8% had Medicaid. Staff clinicians in these practices saw ~10 patients per half-day in clinic and did not follow any formal clinical protocol in caring for patients with ARIs.
From these practices, we randomly selected 500 ARI visits to staff clinicians (i.e. not visits to residents or other trainees) from May 2011 to May 2012. From the visit documentation, we verified the visit was for a new ARI. We excluded visits if they had insufficient documentation (e.g. if the HPI did not contain any information about ARI symptoms), if they did not discuss ARI symptoms, if they were follow-up visits for ARIs or if they had symptom duration >30 days. From the remaining visits, we separated information that could be gathered without an office visit [e.g. history of present illness (HPI), past medical history, etc.] from information that required an office visit (e.g. physical exam findings, testing, etc.). Reviewing non-visit-required information, we determined the diagnosis (HPI diagnosis) and whether or not an office visit was preliminarily necessary. Independently, we reviewed the visit-required information to determine the clinician’s diagnosis and compared the HPI diagnosis to the clinician’s diagnosis. We determined that a visit had ultimately been unnecessary if there was a match between the HPI diagnosis and clinician’s diagnosis or, for cases with discrepant diagnoses, if no change in antibiotic management occurred based on the office visit.
Data sources
We identified all visits to 14 Brigham and Women’s Primary Care Practice-Based Research Network Clinics from May 2011 to May 2012 with one of the top three diagnoses representing an ARI visit based on International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9). We included NS URI (ICD-9 460, 464 and 465), acute bronchitis (ICD-9 466 and 490), influenza (ICD-9 487), non-streptococcal pharyngitis (ICD-9 462), streptococcal pharyngitis (ICD-9 034.0), otitis media (ICD-9 381 and 382), sinusitis (ICD-9 461 and 473) and pneumonia (ICD-9 481–486). From these visits, we randomly selected 500 visits to further analyze. During the review of 500 visits, we excluded visits for which the patient was not currently experiencing ARI symptoms, follow-up visits, visits for symptoms lasting longer than 30 days, or if there was insufficient information to determine if the patient made a new visit for an acute ARI.
Data extraction
We extracted inclusion and exclusion criteria and data about each ARI into a study-specific database (Microsoft Access 2010). We extracted the visit date, patient sex, age and co-morbidities (e.g. diabetes, congestive heart failure, chronic lung disease). We imported the corresponding visit documentation for each ARI visit from the online medical record and separated the visit documentation into two parts. The first part was information in the visit documentation that could be gathered without an office visit (non-visit-required information). This included the chief complaint, HPI, past medical history, medications, allergies, procedures, family and social history and review of systems when available. The second part was information that required an office visit (visit-required information). This included physical exam findings, labs, other tests that were ordered at the visit, interventions performed in-office and the physician’s assessment and plan.
Data extraction of non-visit-required information
We initially extracted data from the first part of the documentation for each visit—non-visit-required information. During this extraction, we gathered data on symptom duration (if noted) and the presence or absence of the following symptoms in the visit documentation: cough, cough with phlegm, cough with coloured sputum, chest congestion, sore throat, fevers, chills, ear pain, red eyes, headache, fatigue, myalgias, nasal symptoms, sinus symptoms, wheezing and shortness of breath.
We used the non-visit-required information, including patient age and co-morbidities, to preliminarily determine whether a visit was necessary or unnecessary for further management. For example, if a patient’s non-visit-required information led to a differential diagnosis that included both acute bronchitis and pneumonia, then the visit was labelled necessary in order to rule out pneumonia with a physical exam. If however non-visit-required information led to a differential of NS URI, then the visit was labelled as unnecessary for further management. We then selected a primary ARI diagnosis for each visit. We labelled this the primary ‘HPI diagnosis’ and chose from NS URI, otitis, sinusitis, pharyngitis, acute bronchitis, influenza and pneumonia. In addition, when relevant, we assigned secondary diagnoses and noted other reasons a visit might be indicated (e.g. age, co-morbidities or immunosuppressive medications).
A second reviewer determined the preliminary necessity of the office visit based on the HPI information for a randomly selected, 10% of the total visits and found 84% concordance (37/44) in visit necessity with the primary reviewer.
Data extraction of visit-required information
After analysis of the non-visit-required information was complete, we randomized the order of the visits and the same reviewer, blinded to previously extracted data, extracted the visit-required information. We extracted data on the presence or absence of the following physical exam findings: inflamed or enlarged tonsils, abnormal findings on auscultation, enlarged lymph nodes, fever, abnormal findings on ear exam, red/watery eyes, inflamed oropharynx/postnasal drip and sinus tenderness. We also extracted data on whether the following interventions were performed during the office visit: sputum culture, rapid influenza testing, rapid group A streptococcal testing, throat culture, blood work, nebulizer treatment and chest X-ray (CXR). For each ARI visit, we recorded whether the following occurred: an antibiotic prescription, a non-antibiotic prescription, referral to the emergency department, referral to a specialist, admission to the hospital and revisit to clinic within 2 weeks of initial appointment. Lastly, we extracted the clinician’s primary diagnosis, and secondary diagnosis if available, from the documented assessment and plan. We relied on the diagnosis in the visit documentation rather than the coded ARI billing diagnosis.
Final determination of the necessity of the visit
We determined that a visit had ultimately been unnecessary if one of two criteria was met. First, we compared the HPI diagnosis to the clinician’s diagnosis. If there was an exact match between the HPI diagnosis and clinician’s diagnosis, we determined the visit was ultimately unnecessary. Second, we examined visits that had a discrepancy between the HPI diagnosis and clinicians’ diagnosis to determine whether the visit resulted in a change in antibiotic management. If there was no change in antibiotic management, we determined the visit was ultimately unnecessary. For example, a visit may have been assigned an HPI diagnosis of NS URI and the clinician’s diagnosis was acute bronchitis without an antibiotic prescription. Because there was no change in antibiotic management that occurred during the office visit this visit could have been managed without office visit. On the other hand, a visit assigned an HPI diagnosis of NS URI and a clinician’s diagnosis of sinusitis with antibiotic prescription had a change in antibiotic management and therefore required office visit for appropriate management.
If the HPI diagnosis indicated a need for a visit, then we determined that a visit was necessary, regardless of the clinician’s diagnosis.
We considered pneumonia, sinusitis (with prolonged, severe or worsening symptoms), streptococcal pharyngitis and otitis media ‘antibiotic-appropriate diagnoses’ (there are no US guidelines for the treatment of adults with otitis media, which is rare and usually treated with antibiotics) (9–11). We considered NS URI, acute bronchitis, sinusitis (without prolonged, severe or worsening symptoms), viral pharyngitis and influenza ‘non-antibiotic-appropriate diagnoses’.
Results
Visit flow
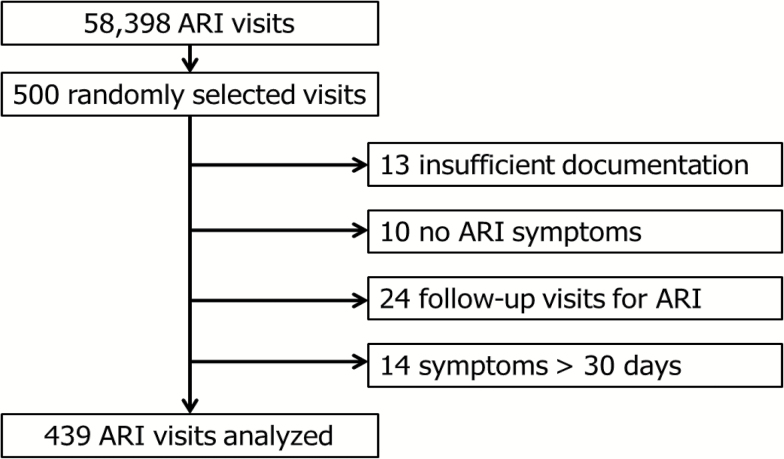
During the study period from May 2011 to May 2012, there were 58398 visits to the 14 primary care practices with an ARI diagnosis. We randomly selected 500 of these visits. We excluded 61 of these visits for the following reasons: 13 with insufficient documentation; 10 without ARI symptoms; 24 were follow-up visits for ARIs; and 14 visits had symptom duration >30 days. After these exclusions, there were 439 new ARI visits available for data extraction and analysis (Fig. 1).
Figure 1.
Visit flow.
Visit characteristics
Among the 439 visits, the average age of the patients in the sample was 45 years. The sample was 71% women. Sampled visits included 31 (7%) patients with diabetes, 3 (<1%) with congestive heart failure and 62 (14%) with chronic lung disease, most commonly asthma. The mean duration of ARI symptoms was 8 days.
The most common symptoms were cough in 282 (64%) visits, sore throat in 241 (55%) visits and nasal symptoms such as runny nose or stuffy nose in 208 (47%) visits. The most common findings on physical exam involved the oropharynx (redness, postnasal drip) in 130 (30%) visits, nasal mucosal abnormalities in 89 (20%) visits and abnormal findings on auscultation in 68 (15%) visits. Clinicians ordered rapid testing for group A streptococci in 80 (18%) visits and CXRs in 37 (8%) visits. Other less commonly used office interventions included throat culture in 26 (6%) visits and blood tests in 24 (5%) visits. Patients were referred to specialists in 20 (5%) visits, with 17 of these referrals to otorhinolaryngology. The most common reasons for referral to otorhinolaryngology were recurrent sinus symptoms (eight), severe otitis media (three) and throat discomfort (three). Clinicians prescribed antibiotics in 213 (49%) visits and non-antibiotic prescriptions were given in 123 (28%) visits.
Visit classification
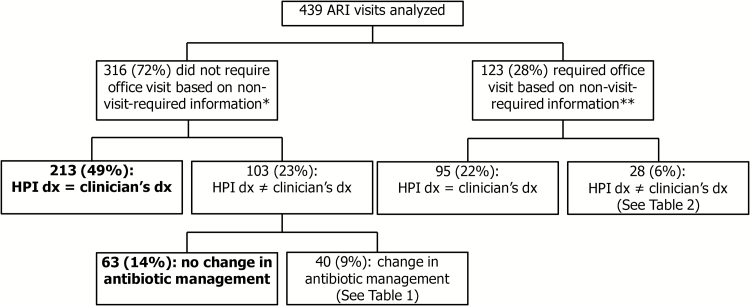
Based on the non-visit-required information, 72% (316/439) of visits did not preliminarily require an office visit (Fig. 2). The most common diagnoses were NS URI (39%), sinusitis (24%) and acute bronchitis (22%). The HPI diagnosis was an exact match with the clinician’s diagnosis in 67% (213/316) of these visits.
Figure 2.
Visit classification. *The most common diagnoses for the 316 visits that did not require an office visit based on non-visit-required information were non-specific upper respiratory infection (122; 39%), sinusitis (76; 24%) and acute bronchitis (70; 22%). **The most common diagnoses for the 123 visits that required office visit based on non-visit-required information were otitis media (39; 32%), pneumonia (39; 32%) and pharyngitis (35; 28%). Dx = diagnosis.
There were 33% (103/316) of visits for which the HPI diagnosis and the clinician’s diagnosis were not an exact match. Of these 103 visits, 61% (63/103) of visits had no change in antibiotic management despite a mismatch between HPI diagnosis and the clinician’s diagnosis. Combining these 63 visits with the 213 visits for which there was an exact match between HPI diagnosis and clinician’s diagnosis, 87% (276/316) of visits not requiring office visit based on non-visit-required information indeed could have been managed without an office visit. Overall, 63% (276/439; 95% confidence interval, 58–67%) of all analyzed visits could have been managed without an office visit (bolded boxes in Fig. 2).
This left 13% (40/316) of visits that, based on non-visit-required information, did not preliminarily require an office visit, but for which an office visit resulted in a change in antibiotic management (Table 1). In 50% (20/40) of these visits, the HPI diagnosis was NS URI, while the clinicians’ diagnoses were acute bronchitis (8), sinusitis (6), otitis (3), pharyngitis (2) and pneumonia (1); all these visits resulted in an antibiotic prescription. In 28% (11/40) of visits, the HPI diagnosis was acute bronchitis without antibiotic prescription, while the clinicians’ diagnoses were sinusitis (5), pneumonia (3), NS URI (2) and otitis (1); all these visits resulted in an antibiotic prescription.
Table 1.
Discrepancies between history of present illness diagnoses and clinician diagnoses for unnecessary visits based on non-visit-required information with changes in antibiotic management (n = 40) at 14 primary care practices from May 2011 to May 2012
| Primary HPI diagnosis | Clinician diagnosis | Antibiotics prescribed by treating clinician |
|---|---|---|
| 20 NS URI | 8 Acute bronchitis | Yes |
| 6 Sinusitis | ||
| 3 Otitis | ||
| 2 Pharyngitis | ||
| 1 Pneumonia | ||
| 11 Acute bronchitis | 5 Sinusitis | Yes |
| 3 Pneumonia | ||
| 2 NS URI | ||
| 1 Otitis | ||
| 4 Non-streptococcal pharyngitis | 3 Pharyngitis | Yes |
| 1 Sinusitis | ||
| 4 Sinusitis | 4 NS URI | No |
| 1 Influenza | 1 Otitis | Yes |
HPI, history of present illness; NS URI, non-specific upper respiratory infection.
Considered together, for the 13% (40/316) for which the visit changed management, the treating clinician prescribed an antibiotic for a potentially antibiotic-appropriate diagnosis (65%; 26/40); prescribed an antibiotic for a non-antibiotic-appropriate diagnosis (25%; 10/40); or avoided an antibiotic prescription for patients with an HPI diagnosis of sinusitis (10%; 4/40).
For the 28% (123/439) of visits preliminarily requiring an office visit based on non-visit-required information, the most common diagnoses were otitis media (32%), pneumonia (32%) and pharyngitis (28%). The HPI diagnosis matched the clinician’s diagnosis for 77% (95/123) of these visits. This left 23% (28/123) of visits with a mismatch between the HPI diagnosis and clinicians’ diagnosis (Table 2). Most of these visits were for antibiotic-appropriate diagnoses such as otitis media or pneumonia or non-antibiotic-appropriate diagnoses with secondary diagnoses or co-morbidities which made a visit necessary.
Table 2.
Discrepancies between history of present illness diagnoses and clinician diagnoses for necessary visits based on non-visit- required information (n = 28) at 14 primary care practices from May 2011 to May 2012
| Primary HPI diagnosis and secondary diagnoses | Clinician diagnosis | Antibiotics prescribed by treating clinician |
|---|---|---|
| 8 Otitis | 4 NS URI | No |
| 2 Pharyngitis | No | |
| 1 Pharyngitis | Yes | |
| 1 Sinusitis | Yes | |
| 6 Sinusitis | 6 NS URI | No |
| Secondary diagnoses | ||
| 3 Otitis | ||
| 2 Pneumonia | ||
| 1 Asthma | ||
| 4 Pneumonia | 2 Acute bronchitis | Yes |
| 1 NS URI | No | |
| 1 Pharyngitis | No | |
| 4 NS URI | 2 Acute bronchitis | Yes |
| Secondary diagnoses | 1 Sinusitis | Yes |
| 1 Pneumonia | 1 Pharyngitis | No |
| 1 Otitis | ||
| 1 Symptoms for 30 days | ||
| 1 Immunosuppressive medications | ||
| 3 Acute bronchitis | 2 NS URI | Yes |
| Secondary diagnoses | 1 NS URI | No |
| 3 Pneumonia | ||
| 2 Influenza | 1 Sinusitis | Yes |
| Secondary diagnoses | 1 Acute bronchitis | No |
| 2 Pneumonia | ||
| 1 Possible streptococcal pharyngitis | 1 NS URI | No |
HPI, history of present illness; NS URI, non-specific upper respiratory infection.
Discussion
In this retrospective chart review of randomly selected ARI visits, we initially determined that 72% did not require an office visit based on information that could be collected without a visit. Of these, after reviewing information collected at the visit, the visit neither resulted in a change in the diagnosis or a change in antibiotic management for 87%. The remaining 13% of visits had a change in antibiotic management, but some of the antibiotic prescribing was for non-antibiotic-appropriate diagnoses. Overall, 63% (276/439) of all visits were determined to be unnecessary for appropriate antibiotic management.
Reducing ARI visits could decrease a significant source of burden on the health care system. ARI visits are not individually complex or expensive, but because they collectively account for about 10% of ambulatory visits, reducing ARI visits could liberate much needed primary care capacity. Reduction in the number of ARI visits could decrease a portion of outpatient care costs, which account for 41% of total health care costs (12). Avoiding unnecessary ARI visits could be part of paying for value-based health care, shifting the focus from volume and profitability of services provided by physicians to patients’ needs and outcomes achieved.
Fewer ARI visits could save valuable time and money for patients. For the typical visit, patients spend an average of 28 minutes waiting in clinic and an additional 15 minutes with the physician (13,14). Factoring in travel time and missed work, ARI visits place a burden on patients seeking care when office visits may not be necessary. Unnecessary visits may contribute to inappropriate antibiotic prescribing (4,5) which increase health care costs, expose patients to adverse drug reactions and increase the prevalence of antibiotic-resistant bacteria (7,8).
Attempted solutions to reduce ARI visits have shown mixed results. A Cold Self-Care Center established to promote self-reliance for patients with minor upper respiratory diseases found a decrease in visits and costs for common colds (15). Patients were able to assess their own symptoms using a checklist or modified algorithm, and if no serious symptoms were present, they were given information on home remedies and over the counter medications for symptom relief. Cold Self-Care patients were satisfied with convenience, speed and ease of use. In contrast, a practice that implemented a URI clinical guideline for initial telephone assessment of patients found that only 13% of patients were eligible due to underlying conditions, prolonged or severe symptoms, or symptoms suggestive of a specific diagnosis other than URI. The guideline failed to decrease clinic visits, antibiotic use or cost of care (16).
When implementing a clinical intervention to triage patients with ARI, it is important to understand the reason why patients seek care. A major reason is antibiotics; patients who visit a physician for ARI desire antibiotics at rates as high as 60–75% (17–19). However, we previously found that 39% of patients visiting an urgent care centre desired antibiotics, suggesting that patients may be seeking care for reasons other than antibiotic prescriptions (20). Other reasons for seeking care included patient’s desire for a diagnosis; reassurance from a physician; get a non-antibiotic treatment recommendation or prescription; have testing; or get a prognosis (20). Improved, accurate, reliable previsit triage and management could reduce the burden of ARI office visits on primary care and the health care system. Interventions must also address clinician concerns. In a largely fee-for-service health care setting, there are financial incentives that encourage office visits.
Although such a model for ARI has yet to be documented, telephone encounters for management of depression (21), asthma (22) and urinary tract infections (23) have been successfully implemented. These telephone encounters work best when a patient–physician relationship already exists and physical examination is unnecessary.
Online communication is another promising area with one study finding that two-thirds of respondents would be interested in an e-mail visit for management of a simple medical problem (24). Internet-based medical visits, or E-Visits, allow patients to seek diagnosis and treatment from their doctor over a secure website without physician office visit. E-Visit may decrease costs without increasing the risk of inappropriate or incomplete care (25,26), but concerns have been raised about equitable access and increased antibiotic prescribing (27,28). E-Visits are gaining in popularity due to patients’ desire for electronic access to health care providers, but there is a lack of published research on outcomes associated with these visits.
Our study has limitations that should be considered. First, we used billing codes to identify potential ARI visits. The visits we reviewed had been, in effect, prescreened to be likely to contain an ARI visit. True, de novo visits might include additional uncertainty. However, we previously found billing codes to have a high sensitivity (98%), specificity (96%) and positive predictive value (96%) (29). For the present study, we found a high positive predictive value for new ARI visits (88%; 439/500), but cannot comment on sensitivity or specificity. In addition, for ARI visits that we ‘missed’ because they had non-ARI billing codes, we cannot comment on the necessity of the visit or the accuracy of the HPI diagnosis. In actual, prospective non-visit-based clinical care, clinicians will be able to identify ‘red flags’ that should indicate the necessity of a visit.
Second, this was a retrospective study, dependent on documentation. The documentation does not always neatly reflect the clinicians’ thought process during the office visit. Documentation may also be subject to confirmation bias. Although we conceived of the HPI diagnosis and the clinicians’ diagnosis as separate, their documentation are not independent. Third, in reality, diagnoses are subject to uncertainty (30), but we considered the HPI diagnosis and clinicians’ diagnoses definitive. Fourth, a single reviewer determined visit necessity and the HPI diagnosis for most visits. However, a duplicate review of 10% of visits showed 84% concordance in determining visit necessity. Fifth, although we considered otitis media an antibiotic-appropriate diagnosis, most cases, especially in children, do not require antibiotic treatment. Despite these limitations, our study shows that a majority of ARI may not require office visit for diagnosis and antibiotic management.
Conclusion
In conclusion, we found that ~63% of primary care visits for ARI may be unnecessary for appropriate management. A robust system of previsit triage and management, by telephone, internet or some other modality, could help determine which patients could be managed without office visit and ensure appropriate follow-up. Interventions to reduce ARI visits have the potential to decrease inappropriate antibiotic prescribing, reduce the burden of ARI office visits on the health care system and offer more convenience for patients.
Declaration
Funding: National Institutes of Health (RC4 AG039115 to JAL); National Institute of Allergy and Infectious Diseases (R21 AI097759 to JAL); Agency for Healthcare Research and Quality (R18 HS018419 to JAL).
Ethical approval: this project was approved by the Partners Health Care Human Research Committee.
Conflict of interest: Dr Linder received funding from Astellas Pharma, Inc. on an unrelated topic.
Acknowledgements
Oral presentation at the 2014 New England Society of General Internal Medicine Regional Meeting on 7 March 2014.
References
- 1. Centers for Disease Control and Prevention. National Center for Health Statistics, National Health Care Surveys. http://www.cdc.gov/nchs/dhcs.htm (accessed on 23 February 2015). [Google Scholar]
- 2. Fendrick AM, Monto AS, Nightengale B, Sarnes M. The economic burden of non-influenza-related viral respiratory tract infection in the United States. Arch Intern Med 2003; 163: 487–94. [DOI] [PubMed] [Google Scholar]
- 3. Grijalva CG, Nuorti JP, Griffin MR. Antibiotic prescription rates for acute respiratory tract infections in US ambulatory settings. J Am Med Assoc 2009; 302: 758–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Barnett ML, Linder JA. Antibiotic prescribing for adults with acute bronchitis in the United States, 1996-2010. J Am Med Assoc 2014; 311: 2020–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Barnett ML, Linder JA. Antibiotic prescribing to adults with sore throat in the United States, 1997-2010. JAMA Intern Med 2014; 174: 138–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Steinman MA, Gonzales R, Linder JA, Landefeld CS. Changing use of antibiotics in community-based outpatient practice, 1991-1999. Ann Intern Med 2003; 138: 525–33. [DOI] [PubMed] [Google Scholar]
- 7. Gandhi TK, Weingart SN, Borus J, et al. Adverse drug events in ambulatory care. N Engl J Med 2003; 348: 1556–64. [DOI] [PubMed] [Google Scholar]
- 8. Shehab N, Patel PR, Srinivasan A, Budnitz DS. Emergency department visits for antibiotic-associated adverse events. Clin Infect Dis 2008; 47: 735–43. [DOI] [PubMed] [Google Scholar]
- 9. Chow AW, Benninger MS, Brook I, et al. ; Infectious Diseases Society of America. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis 2012; 54: e72–112. [DOI] [PubMed] [Google Scholar]
- 10. Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, et al. Clinical practice guideline (update): adult sinusitis. Otolaryngol Head Neck Surg 2015; 152 (suppl 2): S1–39. [DOI] [PubMed] [Google Scholar]
- 11. Shulman ST, Bisno AL, Clegg HW, et al. ; Infectious Diseases Society of America. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin Infect Dis 2012; 55: 1279–82. [DOI] [PubMed] [Google Scholar]
- 12. Bradford JW, Knott DJ, Levine EH, Zemmel RW. Accounting for the Cost of U.S. Health Care: Pre-reform Trends and the Impact of the Recession. McKinsey Center for U.S. Health System Reform. McKinsey & Company, 2011. [Google Scholar]
- 13. Tak HJ, Hougham GW, Ruhnke A, Ruhnke GW. The effect of in-office waiting time on physician visit frequency among working-age adults. Soc Sci Med 2014; 118: 43–51. [DOI] [PubMed] [Google Scholar]
- 14. Tai-Seale M, McGuire TG, Zhang W. Time allocation in primary care office visits. Health Serv Res 2007; 42: 1871–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zapka J, Averill BW. Self care for colds: a cost-effective alternative to upper respiratory infection management. Am J Public Health 1979; 69: 814–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. O’Connor PJ, Amundson G, Christianson J. Performance failure of an evidence-based upper respiratory infection clinical guideline. J Fam Pract 1999; 48: 690–7. [PubMed] [Google Scholar]
- 17. Hamm RM, Hicks RJ, Bemben DA. Antibiotics and respiratory infections: are patients more satisfied when expectations are met? J Fam Pract 1996; 43: 56–62. [PubMed] [Google Scholar]
- 18. Dosh SA, Hickner JM, Mainous AG, III, Ebell MH. Predictors of antibiotic prescribing for nonspecific upper respiratory infections, acute bronchitis, and acute sinusitis. An UPRNet study. Upper Peninsula Research Network. J Fam Pract 2000; 49: 407–14. [PubMed] [Google Scholar]
- 19. Ray DA, Rohren CH. Characteristics of patients with upper respiratory tract infection presenting to a walk-in clinic. Mayo Clin Proc 2001; 76: 169–73. [DOI] [PubMed] [Google Scholar]
- 20. Linder JA, Singer DE. Desire for antibiotics and antibiotic prescribing for adults with upper respiratory tract infections. J Gen Intern Med 2003; 18: 795–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Simon GE, VonKorff M, Rutter C, Wagner E. Randomised trial of monitoring, feedback, and management of care by telephone to improve treatment of depression in primary care. Br Med J 2000; 320: 550–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Pinnock H, Bawden R, Proctor S, et al. Accessibility, acceptability, and effectiveness in primary care of routine telephone review of asthma: pragmatic, randomised controlled trial. Br Med J 2003; 326: 477–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Barry HC, Hickner J, Ebell MH, Ettenhofer T. A randomized controlled trial of telephone management of suspected urinary tract infections in women. J Fam Pract 2001; 50: 589–94. [PubMed] [Google Scholar]
- 24. Grover F, Jr, Wu HD, Blanford C, Holcomb S, Tidler D. Computer-using patients want Internet services from family physicians. J Fam Pract 2002; 51: 570–2. [PubMed] [Google Scholar]
- 25. Albert SM, Shevchik GJ, Paone S, Martich GD. Internet-based medical visit and diagnosis for common medical problems: experience of first user cohort. Telemed J E Health 2011; 17: 304–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Rohrer JE, Angstman KB, Adamson SC, et al. Impact of online primary care visits on standard costs: a pilot study. Popul Health Manag 2010; 13: 59–63. [DOI] [PubMed] [Google Scholar]
- 27. Mehrotra A, Paone S, Martich GD, Albert SM, Shevchik GJ. Characteristics of patients who seek care via eVisits instead of office visits. Telemed J E Health 2013; 19: 515–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mehrotra A, Paone S, Martich GD, Albert SM, Shevchik GJ. A comparison of care at e-visits and physician office visits for sinusitis and urinary tract infection. JAMA Intern Med 2013; 173: 72–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Linder JA, Bates DW, Williams DH, Connolly MA, Middleton B. Acute infections in primary care: accuracy of electronic diagnoses and electronic antibiotic prescribing. J Am Med Inform Assoc 2006; 13: 61–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Whaley LE, Businger AC, Dempsey PP, Linder JA. Visit complexity, diagnostic uncertainty, and antibiotic prescribing for acute cough in primary care: a retrospective study. BMC Fam Pract 2013; 14: 120. [DOI] [PMC free article] [PubMed] [Google Scholar]