Abstract
Objectives
To assess how parents perceive long-term risks for developing obesity-related chronic health conditions.
Methods
A web-based nationally representative survey was administered to 502 U.S. parents with a 5–12 year old child. Parents reported whether their child was most likely to be at a healthy weight or overweight, and the probability that their child would develop hypertension, heart disease, depression, or type 2 diabetes in adulthood. Responses of parents of children with overweight and obesity were compared to those of healthy weight children using multivariate models.
Results
The survey had an overall response rate of 39.2%. The mean (SD) unadjusted parent predicted health risks were 15.4% (17.7%), 11.2% (14.7%), 12.5% (16.2%), and 12.1% (16.1%) for hypertension, heart disease, depression, and diabetes, respectively. Despite under-perceiving their child’s current BMI class, parents of children with obesity estimate their children to be at greater risk for obesity-related health conditions than parents of healthy weight children by 5–6 percentage points. Having a family history of a chronic disease, higher quality of care, and older parent age were also significant predictors of estimating higher risk probabilities.
Conclusions
Despite evidence that parents of overweight children may not perceive these children as being overweight, parents unexpectedly estimate greater future risk of weight-related health conditions for these children. Focusing communication about weight on screening for and reducing the risk of weight-related diseases may prove useful in engaging parents and children in weight management
Keywords: Childhood Obesity, Risk Perception, Risk Assessment, Risk Communication, Cardiovascular Disease, Mental Health, Diabetes
INTRODUCTION
One-third of U.S. children are overweight or obese. 1 Early obesity increases children’s risk for many chronic health conditions throughout their lifespan, including type 2 diabetes, cardiovascular disease, and depression.1, 2
In spite of the high prevalence and serious consequences of obesity, there is strong evidence that many parents do not recognize and/or express concern about obesity in their own families.3–5 Moreover, parents do not think their children will become obese adults.3, 6, 7 A 2013 poll found that only 15% of American parents were concerned about their child’s current weight, and of those concerned parents, 40% believed their child would “grow out of it.”3
Despite the robust evidence base around this topic, a key gap in the literature remains. While parents may construe the term “obesity” as a vague health state without tangible consequences, no studies have examined parent predictions that their child will develop specific obesity-related chronic health conditions.
Focusing pediatric clinical conversations on obesity-related health conditions in addition to obesity in general may change parents’ perceptions of their child’s health risks. Using chronic disease risk prediction tools (e.g. the Framingham risk score) has been shown to motivate behavior change in adults.8, 9 Accordingly, belief that a child is at risk for adverse chronic health effects in adulthood could be an important motivator for a parent to initiate healthful lifestyle behavior changes. Conversely, parents who see their child as immune to adverse health effects may be unlikely to engage in behavior changes. The objective of this study was to assess parent predictions that a child will be obese and/or develop obesity-related comorbidities in adulthood using a nationally-representative survey of parents. A secondary objective was to identify factors that were associated with higher parental chronic disease predictions, which may be future targets for health education and risk communication efforts.
METHODS
Study Population
GfK Custom Research was hired to administer an internet survey to members of their KnowledgePanel®, a nationally-representative panel recruited via probability sampling that covers 97% of the U.S. adult population and has been used to field many national surveys.10–13 Panel participants were identified using random digit dialing and address-based sampling. GfK provided participants with a computer and internet access if these were unavailable. Panel participants received a small incentive payment (< $5) from GfK for completing the survey. Parents with at least one child aged 5–12 years old were invited to complete the survey.
Survey
A 15 to 20 minute survey was administered in December 2014. Approximately 80% of surveys were administered in English, and 20% of surveys were administered in Spanish. If a parent had more than one 5–12 year old child, one child was randomly selected to be the focus of the survey. Parents were asked a series of questions about the child’s health, followed by questions about their level of numeracy, the family’s health, their assessments of the child’s long-term health risks, and the child’s quality of healthcare.
Survey Measures
Outcomes
Parents were asked whether they thought their child was most likely to be “underweight, about the right weight, or overweight” in adulthood (the parent’s age at the time of the survey). Parents were then asked to predict the chances that their child would develop clinical depression, type 2 diabetes, heart disease (congestive heart failure, coronary heart disease, angina, or heart attack), and hypertension in adulthood quantitatively on a visual analog scale ranging from 0% to 100% (Figure 1) and qualitatively on a 5-point Likert scale ranging from Very Likely to Very Unlikely.
Figure 1. Visual analog scale.
Parents were asked, “What do you think the chance is that [CHILD] will have [DISEASE] at age [PARENT’S CURRENT AGE]?” for each of the four health conditions on a visual analog scale (pictured). The scale reported numbers in terms of percentages and proportions and parents were able to see exactly what number they had chosen using the slider (any integer from 0 to 100) in the box underneath the scale.
Demographics
Data on the respondent’s race/ethnicity, family income, education, gender, age, household size, marital status, residence in a metropolitan statistical area (MSA), and census region were obtained from GfK KnowledgePanel® profile data. (Table 1)
Table 1.
Population Demographic and Health Characteristics (n = 502)
| Demographic Characteristics | Percentage/Mean (SD) |
|---|---|
| Female Parent (%) | 54.8 |
| Parent Age (years (SD)) | 39.5 (7.8) |
| Child Age (years (SD)) | 8.5 (2.4) |
| Parent Race/ethnicity (%) | |
| White, non Hispanic | 60.8 |
| Black, non Hispanic | 10.7 |
| Hispanic | 19.9 |
| Other | 8.5 |
| Region (%) | |
| Northeast | 16.7 |
| Midwest | 22.1 |
| South | 36.5 |
| West | 24.7 |
| Residence in a Metropolitan Area (%) | 84.5 |
| Income (%) | |
| <$50,000 | 35.3 |
| $50,000–99,000 | 35.4 |
| >= $100,000 | 29.2 |
| Parent education (%) | |
| Less than High School | 12.7 |
| High School | 23.8 |
| Some College | 31.4 |
| Bachelor’s degree or higher | 32.1 |
| Parent Numeracy (# correct answers) | |
| 0 | 7.1 |
| 1 | 24.2 |
| 2 | 25.3 |
| 3 | 21.6 |
| 4 | 21.8 |
| Number of children in household (n (SD)) | 2.2 (1.1) |
| Health Characteristics | |
| Parent BMI Class, estimateda (%) | |
| Healthy Weight | 32.9 |
| Overweight | 30.4 |
| Obese | 36.7 |
| Child BMI Classa, (%) | |
| Healthy Weight | 64.8 |
| Overweight | 20.8 |
| Obese | 14.4 |
| Parent Assessment of Child BMI Class (%) | |
| Underweight | 12.8 |
| About the right weight | 79.0 |
| Overweight | 8.2 |
| Child has family history of (%) | |
| Depression | 15.1 |
| Diabetes | 28.0 |
| Heart Disease | 24.5 |
| Hypertension | 41.5 |
| Child health insurance (%) | |
| Private only | 60.9 |
| Any public | 35.3 |
| Uninsured | 2.1 |
| Don’t Know | 1.7 |
| Child healthcare utilization over the past 12 months (visits) (%) | |
| None | 14.7 |
| One | 28.9 |
| Two | 29.1 |
| Three or more | 27.2 |
| My child seems to be less healthy than other children I knowb (%) | 6.3 |
| I expect my child will live a very healthy lifeb (%) | 92.8 |
Notes: all percentages represent weighted estimates
SD = standard deviation
Height and weight used to calculate BMI were corrected for self-report biases.20, 22 For adults, healthy weight represents a BMI < 25 kg/m2, Overweight represents a BMI ≥ 25 kg/m2 and < 30 kg/m2, and Obese represents a BMI ≥ 30 kg/m2. For children, healthy weight represents a BMI < 85th percentile for age and sex, Overweight represents a BMI ≥ 85th percentile and < 95 percentile, and Obese represents a BMI ≥ 95th percentile.
“Definitely true” or “mostly true” versus “Don’t know,” “Mostly False,” and “Definitely False”
Numeracy
Parents were asked a series of four validated questions 14–16 (see Appendix A) to assess whether they could correctly interpret proportions and percentages. Parents got one point for each correct answer and the points were summed to create a continuous health numeracy scale ranging from 0 (no correct answers) to 4 (all answers correct) (Table 1).
Health and Healthcare
Parents reported whether they considered their child to be currently underweight, about the right weight, or overweight. (Table 1) Parents were asked to report the child’s birthdate, height, and weight, the last time the child had their height and weight measured, whether the child had personal or family history of any of the four health conditions, and child health care coverage information. Parents self-reported their own health conditions, height, and weight in the KnowledgePanel® profile data. Parents and children were classified as healthy (i.e. normal) weight, overweight, or obese by study authors using the zanthro package in Stata17 and in accordance with CDC guidelines.18, 19 Self-reported height and weight can be biased due to lack of knowledge, recall error, rounding, or social desirability; parents often underreport child height.20 Potential biases in adult and child height and weight were corrected using factors from the published literature. 20–23
Questions from the Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey were used to assess parent perceptions of their child’s current health and future health prospects, and the child’s frequency of healthcare utilization.24 CAHPS measures were also used to determine the quality of a child’s healthcare, defined as the number of best practice recommendations the usual care provider adhered to, ranging from 0 to 6 (see Appendix B for details).
Statistical Analyses
Subjective parent-predicted probabilities of a child being obese and/or developing the conditions of interest in adulthood were compared by child BMI class (healthy weight, overweight, and obese). The primary outcomes were the parent prediction of whether a child was most likely to be at a healthy weight or overweight, and the parent-predicted probability that a child would develop four obesity-related co-morbidities in adulthood. A secondary outcome was how likely parents perceived each risk to be on a Likert scale. Analyses were conducted separately for each health condition.
A logistic regression was used to assess which factors were associated with parent predictions of a child being overweight or obese in adulthood. For the other primary outcome of the parent-predicted probability that a child would develop four obesity-related co-morbidities in adulthood, various regression model specifications that could account for left-skewed outcomes were tested. A generalized linear model with a Poisson family and log link was chosen to evaluate which factors were associated with the primary outcome—the parent-predicted probability of a child developing one of the four specified health conditions in adulthood. For our secondary outcome measure of perceived likelihood on a categorical Likert scale, we used ordinal logistic regressions to assess what characteristics were associated with perceiving risks as being more likely. We also conducted a sensitivity analysis in which parents’ perceived child BMI class (as opposed to the child’s actual BMI weight class) was used in regressions of parent-predicted probabilities of a child developing an obesity-related comorbidity.
All regression analyses controlled for the child’s BMI class, the child’s family history of the health condition, the parent’s BMI class, and other health and demographic characteristics. (Table 1) Model covariates were chosen using a backward elimination approach. Stata (version 12) was employed for all analyses with an a priori alpha level of 0.05.25 The survey package was used to adjust for the complex KnowledgePanel® sampling design.25 The study protocol was approved by the Western Institutional Review Board (#1148257).
RESULTS
GfK invited 1,279 KnowledgePanel® members to complete the survey. From this group, 644 members (50.4%) responded to the invitation and were asked to report the height, weight, birthdate, and gender for all 5–12 year old children in their household; those that were unwilling to provide those data or who provided estimates where the z-scores for height, weight, or BMI were ≥ 5 or ≤ −5 were deemed ineligible. Of the 1,279 invited participants, 502 (39.2% of invited members and 77.9% of those who responded to the invitation) completed the survey. The sample was 61% non-Hispanic white, 11% non-Hispanic Black, 20% Hispanic and 8% other race, and 35% had an annual income below $50,000. (Table 1) KnowledgePanel® parents who were invited to, but did not complete the survey were significantly less likely than survey participants to have obtained a Bachelor’s degree, to be married, to be white, to have an annual income above $50,000, and were on average 2 years younger than survey completers (p < 0.001; Appendix Table 1).
Appendix Table 1.
Demographic characteristics of survey responders and non-responders
| Category | Participants n=502 | Non-participants* n = 777 | p |
|---|---|---|---|
| Female Parent (%) | 42.8 | 38.8 | 0.16 |
| Parent Age (years (SD)) | 39.5 (789) | 37.3 (8.0) | < 0.001 |
| Parent Race/ethnicity (%) | < 0.001 | ||
| White, non Hispanic | 66.5 | 46.7 | |
| Black, non Hispanic | 7.4 | 15.4 | |
| Hispanic | 18.5 | 31.8 | |
| Other | 7.6 | 6.0 | |
| Region (%) | 0.37 | ||
| Northeast | 15.3 | 14.1 | |
| Midwest | 23.5 | 20.5 | |
| South | 33.8 | 28.3 | |
| West | 27.3 | 27.2 | |
| Residence in a Metropolitan Area (%) | 88.1 | 84.2 | 0.06 |
| Income (%) | < 0.001 | ||
| <$50,000 | 31.5 | 48.6 | |
| $50,000–99,000 | 37.0 | 27.9 | |
| >= $100,000 | 31.5 | 23.5 | |
| Parent education (%) | < 0.001 | ||
| Less than High School | 7.2 | 15.9 | |
| High School | 22.9 | 27.2 | |
| Some College | 25.3 | 32.1 | |
| Bachelor’s degree or higher | 44.6 | 24.9 | |
| Number of children in household (n (SD)) | |||
| Age 0–1 | 0.1 (0.3) | 0.1 (0.4) | 0.49 |
| Age 2–5 | 0.5 (0.7) | 0.5 (0.7) | 0.13 |
| Age 6–12 | 1.3 (0.9) | 1.2 (0.8) | 0.03 |
| Age 13–17 | 0.4 (0.7) | 0.4 (0.7) | 0.18 |
| Number of people in household (n (SD)) | 4.4 (1.3) | 4.4 (1.3) | 0.55 |
| Respondent is married (%) | 82.3 | 68.9 | <0.001 |
Note: Percentages are unweighted and may therefore differ from estimates in Table 1
777 non-participants includes 635 of the 1,279 invited participants who did not respond to the invitation; 97 of the participants who responded to the survey invitation, but who refused to provide required child height, weight, or age data; and 45 of the participants who responded to the survey invitation, but provided data where the height, weight, or BMI z-scores were ≥ 5 or ≤ −5.
Approximately 51% of survey respondents reported that their child’s height and weight was measured in the last three months, and 76% of children were measured within the last 6 months. After corrections to parent-reported height and weight were applied20, 22, BMI in this weighted sample of respondents was nationally representative; 35% of 5–12 year old children and 67% of parents were classified as currently overweight or obese, compared to national estimates of 34% and 69%, respectively for similarly aged groups.26 (Table 1)
A majority (81.2%) of parents of children with overweight and obesity misperceived their child to currently be underweight (5.5%) or about the right weight (75.7%). (Appendix Table 2) Regression analyses adjusted for parent BMI, age, race, and numeracy found that parents of children with obesity, whether or not the parents reported perceiving their child to be overweight or obese, were more likely than parents of healthy weight children to be among the 8% of all parents who predicted that their child would be overweight or obese in adulthood (OR= 2.4, 95% CI: 1.3, 4.7). A parent being obese (OR = 2.2, 95% CI: 1.1, 4.1), being of Hispanic ethnicity (OR = 2.1, 95% CI: 1.1, 4.3), each additional year of parent age (OR = 1.1, 95% CI: 1.0–1.1), and each additional point in the numeracy score (OR = 1.3, 95% CI: 1.0, 1.6) significantly increased the odds of a parent predicting that their children would be overweight or obese in adulthood. (Appendix Table 3)
Appendix Table 2.
Differences in Child Actual BMI Class and Parent-Perceived BMI Class
| Actual child BMI class^ | Parent-perceived BMI class | ||
|---|---|---|---|
| Underweight | About the right weight | Overweight | |
| Healthy weight | 16.7% | 80.9% | 2.4% |
| Overweight or Obese | 5.5% | 75.7% | 18.8% |
Actual child BMI class calculated using parent-reported height and weight estimates. Height and weight used to calculate BMI were corrected for self-report biases.20, 22 For children, healthy weight represents a BMI < 85th percentile for age and sex, Overweight represents a BMI ≥ 85th percentile and < 95 percentile, and Obese represents a BMI ≥ 95th percentile.
Appendix Table 3.
Model Coefficients for Logistic Regression on Parent Predicting Child Would be Overweight/Obese in Adulthood
| OR | 95% CI | |
|---|---|---|
| Child BMI | ||
| Healthy weight | ref | |
| Overweight | 0.95 | [0.49, 1.79] |
| Obese | 2.44** | [1.26, 4.73] |
| Parent BMI | ||
| Healthy weight | ref | |
| Overweight | 1.16 | [0.59, 2.25] |
| Obese | 2.17* | [1.14, 4.13] |
| Parent Age (years) | 1.07*** | [1.04, 1.11] |
| Parent Race | ||
| White | ref | |
| Black | 2.00 | [0.73, 5.49] |
| Hispanic | 2.12* | [1.05, 4.28] |
| Other | 0.87 | [0.35, 2.17] |
| Numeracy (0–4) | 1.28* | [1.02, 1.61] |
| Constant | 0.003 | [0.001, 0.02] |
Notes: Child age, child gender, child frequency of healthcare utilization, quality of child healthcare, child health insurance, census region, residence in an MSA, family income, parent numeracy, parent education, and household size were tested, but ultimately dropped from the model due to lack of significance.
Statistically significant at P = 0.05
Statistically significant at P = 0.01
Statistically significant at P = 0.001
BMI: Body Mass Index; MSA: Metropolitan Statistical Area; OR: Odds Ratio
The mean (SD) unadjusted parent predicted health risks were 15.4% (17.7%), 11.2% (14.7%), 12.5% (16.2%), and 12.1% (16.1%) for hypertension, heart disease, depression, and diabetes, respectively. Roughly 17–20% of parents estimated that their child would have zero risk of developing the four health conditions of interest in adulthood. In unadjusted bivariate analyses, neither parent nor child current BMI class were predictive of parents estimating that their child would have zero risk of developing one of the health conditions in adulthood.
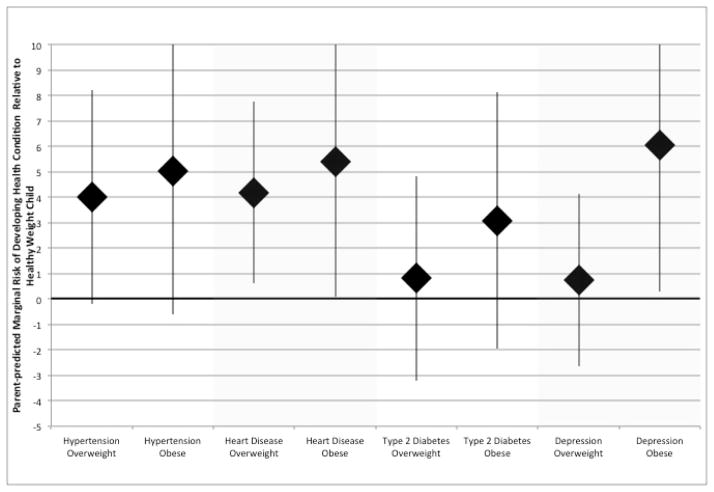
In multivariate regression analyses that adjusted for family history of disease, residence in an MSA, quality of healthcare, parent BMI class, parent age, parent race, and census region, parents of children who were overweight and obese estimated some higher disease risks than parents of healthy weight children. Parents of children with overweight estimated future disease risks for hypertension that were higher by +3.99 percentage points (95% CI: −0.19, +8.19) for hypertension and +4.18 percentage points (95% CI: +0.61, +7.76) for heart disease compared to parents of healthy weight children. Parents of children with obesity estimated future disease risks that were higher by +5.01 percentage points (95% CI: −0.62, +10.63) for hypertension, by +5.38 percentage points (95% CI: +0.10, +10.66) for heart disease, and by +6.04 percentage points (95% CI: +0.31, +11.78) for depression compared to parents of healthy weight children. Parents children with overweight and obesity did not estimate higher diabetes risks than parents of healthy weight children. (Figure 2)
Figure 2. Marginal difference in parent-predicted child health risk by BMI class (mean and 95% CI).
Regression models examining the relationship between parent-predicted risk and child current BMI were adjusted for, family history of disease, residence in an MSA, quality of healthcare, parent BMI class, parent age, parent race, and census region.
Parents of children with a family history of disease were found to have reported risk estimates for all four conditions of interest that were 5.1–8.6 percentage points higher (p < 0.05) than the predictions of those without a family history of disease. Having higher quality of care (0.69–1.2 percentage points for each additional standard of care met) and older parent age (0.21–0.44 percentage points for each additional year of parent age) were also predictors of predicting higher risk probabilities (p < 0.05). Hispanic parents were more likely to estimate lower risks for hypertension, heart disease and depression compared to White parents (−4.5 to −3.6 percentage points, p < 0.05). The parent’s BMI class was not associated with risk estimates.
In sensitivity analyses that utilized parent-perceived current child BMI class instead of the child’s actual current BMI class, parents who considered their child to be currently overweight or obese estimated disease risks that were higher by +8.17 percentage points (95% CI: 1.47, 14.87) for hypertension and +7.03 percentage points (95% CI: −0.33, 14.39) for heart disease relative to parents who considered their child to be currently at a healthy weight or underweight. There were no differences in type 2 diabetes or depression risk prediction between groups.
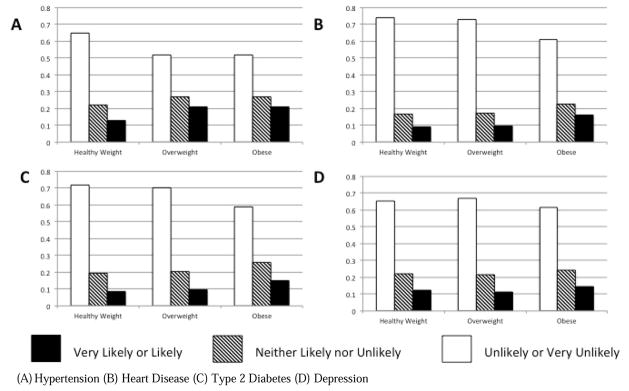
Overall, 10–16% of parents categorized their child’s future health risks as likely or very likely. (Appendix Figure 1) In our ordinal logistic regression that examined characteristics associated with perceiving risks as being more likely, adjusted for family medical history, residence in an MSA, quality of healthcare, parent BMI class, parent age, parent race, and census region, parents of children with overweight were more likely to rank their predicted risk as being in a higher category (unlikely or very unlikely vs. neither likely or unlikely vs. likely or very likely) for hypertension (OR = 1.19, 95% CI: 1.1, 3.3) relative to parents of healthy weight children. Parents of children with obesity were more likely to rank their predicted risk as being in a higher category for hypertension (OR = 1.9, 95% CI: 0.97, 3.8), heart disease (OR = 2.26, 95% CI: 1.1, 4.7), and type 2 diabetes (OR = 2.2, 95% CI: 1.1, 4.4) relative to parents of healthy weight children.
Appendix Figure 1.
Parent perception of risk likelihood by child BMI class (unadjusted)
(A) Hypertension (B) Heart Disease (C) Type 2 Diabetes (D) Depression
DISCUSSION
This is the first study to assess the parent-perceived risk that a child will develop obesity-related health conditions in adulthood, and factors associated with higher risk estimates. Our results suggest that obesity-related comorbidity risks are perceived differently than obesity itself. Similar to prior studies 6, 7, 27, we found that most parents of children with overweight and obesity underestimate their child’s current BMI class. While parents of children with obesity were more likely than parents of healthy weight children to predict that their child would be overweight in adulthood, our parent sample as a whole was unlikely to predict that their child would be overweight or obese in adulthood. Considering these findings,, we surprisingly found that parents of children with obesity estimated their children to be at greater risk for developing obesity-related diseases in adulthood compared to parents of healthy weight children, by 5 to 6 percentage points. Parents of children with obesity also perceived their children to be at higher risk than parents of healthy weight children on a Likert Scale.
Accurate parental perception of long-term health risks could motivate a family to engage in behavior change to improve a child’s BMI. A recent study by Peyer et al. found that parents who perceived their child to be heavier expressed more concern about child weight.27 Additionally, parents who engage in childhood obesity treatment programs cite a desire to improve their child’s long-term health outcomes as motivation to initiate behavior change.28, 29 The evidence on the relationship between risk perception and behavior change among adults is mixed8, 30, 31, but little is known about this relationship in child populations. Future research should assess whether more accurate health risk perception around specific obesity-related comorbidities would improve health behaviors.
Parents of children with obesity did not estimate higher type 2 diabetes risks than parents of healthy weight children. One explanation for parent reluctance to report that their child was likely to become obese and/or develop diabetes may be stigma around those conditions.32, 33 While depression is also generally stigmatized, it may not be as strongly associated with obesity as diabetes. The severity of the four conditions did not seem to affect parent responses; respondents in a recent poll reported considering heart disease to be more serious than diabetes, but parents of children with obesity were not more reluctant than parents of healthy weight children to predict high heart disease-related risks.34
Parents whose children had high quality healthcare and consistent with another study, whose children had a family history of disease 35, estimated higher disease risks than their counterparts. These findings suggest that improving physician communication about a child’s physical and emotional development and focusing counseling on conditions for which there is a family history may have some benefit. Collection of family medical history is recommended by the American Academy of Pediatrics.36 Future studies should assess the impact of incorporating these techniques into clinical care on risk perception and patient health behavior.
Hispanic parents were more likely to predict that their child would be overweight or obese in adulthood, but unexpectedly predicted significantly lower cardiovascular and depression risks compared to White parents. This antithetical relationship has also been documented among Hispanic parents of preschool-aged children. Parents reported an awareness of weight-related adverse health outcomes, but a lack of concern specific to that age group. 37
In the absence of longitudinal studies that follow children from early childhood to late adulthood, mathematical simulation models are a frequently used and the most feasible method for assessing the impact of early obesity intervention on long-term pediatric risks.38–41 Future work should compare parents’ risk estimates collected in this survey to risk estimates forecasted by validated simulation models to assess whether parents are underestimating their children’s long-term health risks.
Finally, this analysis focuses on health-related risk assessment, but obesity also affects social and emotional development throughout the life course.42 Future research may assess parent predictions of outcomes such as marriage and educational attainment. Risk communication related to these non-health outcomes may also affect uptake of behavior change.
Limitations
There were significant differences in the demographic characteristics of survey responders and non-responders. Potential respondents were only shown information about the subject (health) and the length of the survey (20 minutes); lower socioeconomic status populations may have limited time to complete long surveys. However, survey responses were weighted to be nationally-representative using probability sample weights. Probability-based internet samples like the one employed in this study have been found to provide the optimal combination of representativeness and self-report accuracy relative to random digit-dialing telephone and online volunteer survey samples.43 Shorter surveys may improve response rates among low socioeconomic status families.
Results did not include Bonferroni adjustments for multiple comparisons, as this method assumes that the outcomes are independent. Because our outcomes are expected to be correlated with each other, this correction would be too conservative. Instead, we have chosen to report our results with multiple p-values (< 0.05; < 0.01; <0.001) and report the 95% confidence interval, which provides additional information about the magnitude of our effects.
The web-based modality of survey administration may have affected parent responses. On one hand, parents may have been more honest in this anonymous forum, and on the other hand, parents may have also been more likely to misreport their child’s height, weight, and perceived weight class. Due to the web-based nature of this survey, there was no way for us to validate parent responses. We were able to correct reported height and weight measurements for self-report biases. Still, given these limitations, it may be helpful to replicate this survey using different modalities (i.e. in-person or by phone). Additionally, if these results are adapted for clinic-based interventions, researchers should consider that responses may differ in face-to-face versus web- or tablet-based interactions.
CONCLUSION
Some parents of children with obesity do not consider their children to be overweight or obese, but parents of children with obesity in our sample are more likely to estimate their children to be at increased long-term risk for some chronic health conditions compared to parents of healthy weight children. Providers may consider talking with parents about specific comorbidity risks as opposed to obesity in general in order to increase risk perception and subsequent action. Future work should assess whether improved risk assessment leads to better engagement in behavior change to reduce a child’s risk for developing obesity-related co-morbidities in adulthood.
What’s New.
Although most parents think their children are unlikely to become obese adults, parents of children with obesity estimate their children to be at higher risk for developing obesity-related comorbidities in adulthood relative to parents of healthy weight children.
Acknowledgments
Funding Source: Financial support for this study was provided by a grant from the University of Washington Nutrition Obesity Research Center (P30 DK035816). The funding agreement ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report. Dr. Dawson-Hahn’s time was supported by the Rush L. Kirschstein National Research Service Award (T32HP10002). Dr. Wright’s time was supported by The University of Washington Institute for Translational Health Sciences (UL1 TR000423).
This work was funded by the University of Washington Nutrition Obesity Research Center (P30 DK035816). The University of Washington Nutrition Obesity Research Center had no role in the study design, data analysis, or interpretation of study findings. The research presented in this paper is that of the authors and does not reflect the official policy of the funders.
Abbreviations
- BMI
body mass index
- MSA
metropolitan statistical area
Appendix A: Numeracy
Four questions were used to assess parents’ health numeracy, parent’s ability to interpret percentages and proportions. These questions were adapted from questions previously used in the literature.14–16
Imagine that we flip a fair coin 1,000 times. What is your best guess about how many times the coin would come up heads in 1,000 flips?
In the BIG BUCKS LOTTERY, the chance of winning a $50 prize is 1%. What is your best guess about how many people would win a $50 prize if 1,000 people each buy a single ticket to BIG BUCKS?
In ACME PUBLISHING SWEEPSTAKES, the chance of winning a car is 1 in 1,000. What percent of tickets to ACME PUBLISHING SWEEPSTAKES will win a car?
Maria drives to work and takes the same route every day. On her way to work, there is a 1 in 96 chance that Maria will drive past a house that is painted blue and a 1 in 57 chance that Maria will drive past a house that is painted white. Which is bigger, Maria’s chance of driving past a blue house or her chance of driving past a white house?
Appendix B: Quality of Care
Healthcare quality was assessed using questions derived from CAHPS measures. 24 The survey asked parents the following questions:
-
In the last 12 months, how often do [CHILD’s] doctors or other health providers explain things in a way that was easy to understand?
Never
Sometimes
Usually
Always
Don’t Know
-
In the last 12 months, has a doctor or other health provider ever discussed [CHILD’s] eating or exercise behaviors with you?
Yes
No
Don’t Know
-
In the last 12 months, did you seek information or advice about changing [CHILD’s] eating or exercise behaviors form a doctor or other health provider?
Yes
No
Don’t Know
-
In the last 12 months, has a doctor or other health care provider ever talked to you about [CHILD’s]
Learning ability
Age-appropriate behaviors
Moods and emotions
How much time [CHILD] spends on a computer and in front of TV
Physical development
How [CHILD] gets along with others
To improve the efficiency of the survey, Question 4 was presented in a grid, and parents answered “Yes,” “No,” or “Don’t Know.” Don’t Know responses were categorized as missing.
The responses to question #4 were dichotomized, where a score of 1 was assigned to “yes” responses and a score of 0 was assigned to “no” responses. The six responses were summed to create a scale for quality of care, ranging from 0 (low quality, health provider met no standard of care items) to 6 (high quality, health provider met all standard of care items). This measure composite measure was used as a proxy for quality of care in statistical analyses.
Footnotes
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Clinical Trial Registration: N/A
Contributor’s Statements
Dr. Wright (University of Washington & Seattle Children’s Research Institute) had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Dr. Wright conceptualized and designed the study, obtained funding, analyzed and interpreted the data, and wrote the initial manuscript. Dr. Paula Lozano (Group Health Research Institute), Dr. Elizabeth Dawson-Hahn (University of Washington & Seattle Children’s Research Institute), Dr. Dimitri Christakis (University of Washington & Seattle Children’s Research Institute), Ms. Wren Haaland (Seattle Children’s Research Institute), and Dr. Anirban Basu (University of Washington) all contributed to the study design and interpretation of data, and critically reviewed and revised the manuscript. Dr. Dawson Hahn’s time was supported by the Ruth L. Kirschstein National Research Service Award (#T32HP10002). Ms. Wren Haaland’s (Seattle Children’s Research Institute) time was supported by the Seattle Children’s Research Institute.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Skinner AC, Skelton JA. Prevalence and Trends in Obesity and Severe Obesity Among Children in the United States, 1999–2012. JAMA Pediatr. 2014 doi: 10.1001/jamapediatrics.2014.21. [DOI] [PubMed] [Google Scholar]
- 2.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337:869–873. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 3.RWJF, NPR, Harvard School of Public Health. A Poll About Children and Weight: Crunch Time During the American Work and School Week-- 3 pm to Bed. 2013. [Google Scholar]
- 4.Katz DL. Oblivobesity: looking over the overweight that parents keep overlooking. Child Obes. 2015;11:225–226. doi: 10.1089/chi.2015.1131. [DOI] [PubMed] [Google Scholar]
- 5.Duncan DT, Hansen AR, Wang W, Yan F, Zhang J. Change in Misperception of Child’s Body Weight among Parents of American Preschool Children. Child Obes. 2015 doi: 10.1089/chi.2014.0104. [DOI] [PubMed] [Google Scholar]
- 6.Parry LL, Netuveli G, Parry J, Saxena S. A systematic review of parental perception of overweight status in children. J Ambul Care Manage. 2008;31:253–268. doi: 10.1097/01.JAC.0000324671.29272.04. [DOI] [PubMed] [Google Scholar]
- 7.Rietmeijer-Mentink M, Paulis WD, van Middelkoop M, Bindels PJ, van der Wouden JC. Difference between parental perception and actual weight status of children: a systematic review. Matern Child Nutr. 2013;9:3–22. doi: 10.1111/j.1740-8709.2012.00462.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Colkesen EB, Ferket BS, Tijssen JG, Kraaijenhagen RA, van Kalken CK, Peters RJ. Effects on cardiovascular disease risk of a web-based health risk assessment with tailored health advice: a follow-up study. Vascular health and risk management. 2011;7:67–74. doi: 10.2147/VHRM.S16340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Edwards A, Hood K, Matthews E, et al. The effectiveness of one-to-one risk communication interventions in health care: a systematic review. Med Decis Making. 2000;20:290–297. doi: 10.1177/0272989X0002000305. [DOI] [PubMed] [Google Scholar]
- 10.GfK Knowledge Networks. http://www.gfk.com/us/Solutions/consumer-panels/Pages/GfK-KnowledgePanel.aspx2014.
- 11.American National Election Studies; Studies UoMCfP, editor. The ANES Guide to Public Opinion and Electoral Behavior. Ann Arbor: University of Michigan Center for Political Studies; [Google Scholar]
- 12.McAfee T, Davis KC, Alexander RL, Jr, Pechacek TF, Bunnell R. Effect of the first federally funded US antismoking national media campaign. Lancet. 2013;382:2003–2011. doi: 10.1016/S0140-6736(13)61686-4. [DOI] [PubMed] [Google Scholar]
- 13.Time-Sharing Experiments for the Social Sciences. Introducing TESS. 2015;2015 [Google Scholar]
- 14.Woloshin S, Schwartz LM, Byram S, Fischhoff B, Welch HG. A new scale for assessing perceptions of chance: a validation study. Med Decis Making. 2000;20:298–307. doi: 10.1177/0272989X0002000306. [DOI] [PubMed] [Google Scholar]
- 15.Weller J, NFD, MT, Mertz C, WJB, Peters E. Development and Testing of an Abbreviated Numeracy Scale: A Rasch Analysis Approach. Journal of Behavioral Decision Making. 2013;26:198–212. doi: 10.1002/bdm.1751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schwartz LM, Woloshin S, Black WC, Welch HG. The role of numeracy in understanding the benefit of screening mammography. Ann Intern Med. 1997;127:966–972. doi: 10.7326/0003-4819-127-11-199712010-00003. [DOI] [PubMed] [Google Scholar]
- 17.Vidmar S, Carlin J, Hesketh K. Standardizing anthropometric measures in children and adolescents with new functions for egen. The Stata Journal. 2004;4:50–55. [Google Scholar]
- 18.Centers for Disease Control and Prevention. About BMI for Adults. Mar 9, 2015. [Google Scholar]
- 19.Centers for Disease Control and Prevention. About BMI for Children and Teens. Vol. 2015. Atlanta: 2014. [Google Scholar]
- 20.Weden MM, Brownell PB, Rendall MS, Lau C, Fernandes M, Nazarov Z. Parent-Reported Height and Weight as Sources of Bias in Survey Estimates of Childhood Obesity. American Journal of Epidemiology. 2013:461–473. doi: 10.1093/aje/kws477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ezzati M, Martin H, Skjold S, Vander Hoorn S, Murray CJ. Trends in national and state-level obesity in the USA after correction for self-report bias: analysis of health surveys. J R Soc Med. 2006;99:250–257. doi: 10.1258/jrsm.99.5.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jain RB. Regression models to predict corrected weight, height and obesity prevalence from self-reported data: data from BRFSS 1999–2007. Int J Obes (Lond) 2010;34:1655–1664. doi: 10.1038/ijo.2010.80. [DOI] [PubMed] [Google Scholar]
- 23.Rendall MS, Weden MM, Lau C, Brownell P, Nazarov Z, Fernandes M. Evaluation of bias in estimates of early childhood obesity from parent-reported heights and weights. Am J Public Health. 2014;104:1255–1262. doi: 10.2105/AJPH.2014.302001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Homer CJ, Fowler FJ, Gallagher PM, et al. The Consumer Assessment of Health Plan Study (CAHPS) survey of children’s health care. Jt Comm J Qual Improv. 1999;25:369–377. doi: 10.1016/s1070-3241(16)30452-7. [DOI] [PubMed] [Google Scholar]
- 25.StataCorp. Stata Statistical Software: Release 12. College Station, TX: Statacorp LP; 2011. [Google Scholar]
- 26.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peyer KL, Welk G, Bailey-Davis L, Yang S, Kim JK. Factors Associated with Parent Concern for Child Weight and Parenting Behaviors. Child Obes. 2015 doi: 10.1089/chi.2014.0111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grow HM, Hsu C, Liu LL, et al. Understanding family motivations and barriers to participation in community-based programs for overweight youth: one program model does not fit all. J Public Health Manag Pract. 2013;19:E1–E10. doi: 10.1097/PHH.0b013e31825ceaf9. [DOI] [PubMed] [Google Scholar]
- 29.Gillespie J, Midmore C, Hoeflich J, Ness C, Ballard P, Stewart L. Parents as the start of the solution: a social marketing approach to understanding triggers and barriers to entering a childhood weight management service. J Hum Nutr Diet. 2014 doi: 10.1111/jhn.12237. [DOI] [PubMed] [Google Scholar]
- 30.Atlantis E, Barnes EH, Ball K. Weight status and perception barriers to healthy physical activity and diet behavior. Int J Obes (Lond) 2008;32:343–352. doi: 10.1038/sj.ijo.0803707. [DOI] [PubMed] [Google Scholar]
- 31.Wister A, Loewen N, Kennedy-Symonds H, McGowan B, McCoy B, Singer J. One-year follow-up of a therapeutic lifestyle intervention targeting cardiovascular disease risk. CMAJ: Canadian Medical Association journal = journal de l’Association medicale canadienne. 2007;177:859–865. doi: 10.1503/cmaj.061059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Puhl RM, Heuer CA. Obesity stigma: important considerations for public health. Am J Public Health. 2010;100:1019–1028. doi: 10.2105/AJPH.2009.159491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Browne JL, Ventura A, Mosely K, Speight J. ‘I call it the blame and shame disease’: a qualitative study about perceptions of social stigma surrounding type 2 diabetes. BMJ Open. 2013;3:e003384. doi: 10.1136/bmjopen-2013-003384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Oliver JE, Lee T. Public opinion and the politics of obesity in America. Journal of health politics, policy and law. 2005;30:923–954. doi: 10.1215/03616878-30-5-923. [DOI] [PubMed] [Google Scholar]
- 35.Nsiah-Kumi PA, Ariza AJ, Mikhail LM, Feinglass J, Binns HJ Pediatric Practice Research, G. Family history and parents’ beliefs about consequences of childhood overweight and their influence on children’s health behaviors. Acad Pediatr. 2009;9:53–59. doi: 10.1016/j.acap.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 36.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 37.Gauthier KI, Gance-Cleveland B. Hispanic Parental Perceptions of Child Weight in Preschool-Aged Children: An Integrated Review. Child Obes. 2015;11:549–559. doi: 10.1089/chi.2014.0152. [DOI] [PubMed] [Google Scholar]
- 38.Hall KD, Butte NF, Swinburn BA, Chow CC. Dynamics of childhood growth and obesity: development and validation of a quantitative mathematical model. The lancet. Diabetes & endocrinology. 2013;1:97–105. doi: 10.1016/s2213-8587(13)70051-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kristensen AH, Flottemesch TJ, Maciosek MV, et al. Reducing childhood obesity through U.S. federal policy: a microsimulation analysis. Am J Prev Med. 2014;47:604–612. doi: 10.1016/j.amepre.2014.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Levy DT, Mabry PL, Wang YC, et al. Simulation models of obesity: a review of the literature and implications for research and policy. Obes Rev. 2010 doi: 10.1111/j.1467-789X.2010.00804.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011;378:815–825. doi: 10.1016/S0140-6736(11)60814-3. [DOI] [PubMed] [Google Scholar]
- 42.Cheng Y-hA. Longer Exposure to Obesity, Slimmer Chance of College? Body Weight Trajectories, Non-Cognitive Skills, and College Completion. Youth & Society. 2014 0044118X14540183. [Google Scholar]
- 43.Chang L, Krosnick J. National surveys via RDD telephone interviewing versus the Internet: Comparing sample representativeness and response quality. Public Opiionn Quarterly. 2009;73:641–678. [Google Scholar]