Abstract
[Purpose] The purpose of this study was to evaluate the relationship between malalignment and lower-extremity injury and to determine the optimal dynamic alignment of the lower extremity with wall squats. [Subjects and Methods] Healthy individuals from one therapy school were enrolled and assigned to a wall squat normal or abnormal group based on their forms during wall squats. The abnormal group was found to be more prone to lower-extremity injury on three-dimensional motion analysis. Eight students from each group were randomly chosen for the study. The effects of single-leg landing movements were assessed using three-dimensional motion analysis. [Results] In the sagittal plane, significant flexion of the hip and knee joints occurred 0.02 and 0.04 seconds after initial foot contact with the ground in the normal and abnormal groups, respectively. In the frontal plane, significant adduction of the hip joint occurred at 0.07 seconds in the abnormal group. [Conclusion] The abnormal group tended to display later flexion of the hip and knee joints and narrower hip, knee, and ankle range of motion than the normal group, suggesting that dynamic alignment of the lower extremity in the abnormal group likely made them susceptible to injury.
Key words: Squat, Lower extremity alignment, Single leg jump
INTRODUCTION
Several effective injury prevention programs for the lower extremity have recently been reported1, 2). These reports indicated that for appropriate injury prevention, it is essential to maintain appropriate alignment of the lower extremity while controlling the cervical region and trunk. Moreover, they suggest that movement needs to be performed in a symmetrical manner while maintaining the entire body in optimal alignment. Thus, during activities, there is a strong emphasis on maintaining the appropriate form and suitably executing movements.
At present, the squat exercise is an integral part of any injury prevention program3, 4). Squats are performed by diverse populations, from professional athletes to people who participate in irregular exercise irregularly, due to its similarity to the movements executed in sports activities. Moreover, it is used in medical practice, including postsurgical rehabilitation and rehabilitation in elderly individuals.
However, no study5,6,7) thus far has established a method for assessing squats while maintaining an appropriate alignment and controlling compensatory movements.
It is important that squats be executed while maintaining good mechanics and alignment; however, three-dimensional (3D) motion analysis and other equipment not readily available in training environments are essential to ensure that squats are performed appropriately. Hence, assessment of lower-extremity alignment during squats is often subjective and dependent on the view and experience of the athletes and trainers.
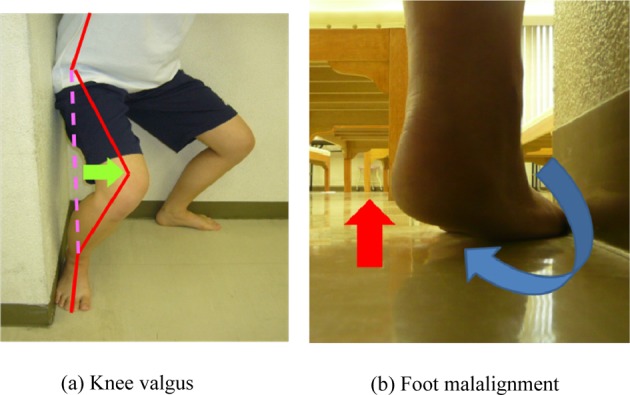
Individuals with good alignment and without any mechanical issues usually have a lower risk of injury during activities of daily living (ADLs) and in sports settings. However, individuals with malalignment are at a higher risk of injury, particularly under high threshold activities in training and sports settings. When such individuals perform squats, dynamic valgus and collapsing of the foot arch are common forms of malalignment, which could induce pain during ADLs or in sports settings. It can be assumed that many athletes train with malalignment and do not have any access to motion analysis devices, and hence, there is a need for a simple method to screen lower-extremity alignment objectively.
In the present study, the wall squat proposed by Watarai8) was used to evaluate the correlation between malalignment and lower-extremity injury as well as to determine the optimal dynamic alignment of the lower extremity.
SUBJECTS AND METHODS
Healthy individuals from a physical therapy school were enrolled and assigned to two groups based on their form during wall squats: wall squat abnormal (WSA) and wall squat normal (WSN). A total of eight students were randomly chosen from each group to participate in the study: three men and five women in the WSN group (mean age: 22 ± 1.7 years) and three men and five women in the WSA group (mean age: 21 ± 0 years).
A manual muscle test was conducted to ensure that all individuals had adequate strength for the test and did not demonstrate any major asymmetry. Prior to the study, all individuals were assessed for the absence of limited range of motion of the hip, knee, and ankle as well as for the lack of any underlying neuromuscular pathology. The participants were given detailed information about the study and provided informed consent prior to inclusion in the study. This study was approved by Ethic Comity for the Human subjects research in Graduate school of Sport system, Graduate school of Emergency Medical system, Kokushikan University.
The wall squat increases sensory input and enables better awareness of alignment. The use of a corner wall makes performance of the wall squat safe and reproducible. The wall squat can be performed in most training environments where there is a corner wall (including two vertical walls perpendicular to the floor and with each other) by placing the lateral aspects of the hips, thighs, lower legs, and the head of the fifth metatarsal against the wall; the heels are not placed against the wall. The subjects were requested to execute the wall squat while maintaining contact with the wall and consciously focusing on bearing weight on the long axis of the feet. During a wall squat, the upper body tilts forward along with the anterior pelvis, whereas the line connecting the acromion and hip joint remains parallel to the tibia.
Subjects who could complete a wall squat based on the conditions above were assigned to the WSN group (Fig. 1), whereas those who could not maintain contact and alignment during a squat were assigned to the WSA group (Fig. 2). The test was performed under supervision of physical therapists and athlete trainers licensed in Japan.
Fig. 1.

Wall squat normal (WSN)
Fig. 2.
Wall squat abnormal (WSA)
Three-dimensional motion analysis was performed using a 3D motion capture system from Vicon Motion Systems (Vicon MX), a force plate sensor from AMTI, and eight infrared cameras with a frame rate of 100 Hz. Moreover, a total of 16 reflective markers were used based on the instructions for a Plug-in-Gait model of the lower extremity. For the analysis, subjects were instructed to jump from a single leg from a 20 cm high platform and land on the same leg on a force plate (dimensions: 50 cm × 50 cm) placed in front of the platform. Landings in which the wrong foot was used to land or in which aberrant upper-body compensation was noted were excluded.
After sufficient practice, three successful landings on the right and left sides were included for analysis. Noise was removed from the measured coordinate values of the reflective markers by using a two-dimensional Butterworth filter (10 Hz). Moreover, the joint angles of the pelvis, hip, knee, and ankle were estimated using the VICON Plug-In-Gait Model.
Among the three single-leg jumps, only cases in which the landing met the appropriate criteria were included in the analysis. Based on the findings of previous studies9), the injury rate is high during the first 0.1 s after the initial foot contact with the ground. This 0.1 s was divided into 10 segments (0.01 s each) to trace and calculate the rate of angular changes of the pelvis, hip, knee, and ankle.
For statistical analysis, a one-way factorial analysis of variance (ANOVA) and multiple comparison tests (Fisher’s protected least significant difference, PLSD) were used. The significance value for the risk ratio was set at 5% (p<0.05).
RESULTS
Examination of the pelvic joint in the sagittal plane (Table 1) revealed no significant difference in the anterior-posterior angular change on one-way ANOVA. Examination of the pelvic joint in the frontal plane with regard to pelvic elevation and depression revealed a significant increase in the elevation angle at 0.07–0.1 s in the WSN group and 0.06–0.1 s in the WSA group (p<0.05). Examination of the pelvic joint in the transverse plane with regard to the anterior and posterior rotation angles revealed that the WSN group showed significant posterior rotation at 0.08–0.1 s, whereas the WSA group showed significant anterior rotation at 0.03–0.06 s (p<0.05).
Table 1. Pelvic joint.
| Time (sec) | 0.00 | 0.01 | 0.02 | 0.03 | 0.04 | 0.05 | 0.06 | 0.07 | 0.08 | 0.09 | 0.1 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sagittal plane | WSN (deg/%) | 0.00 | −2.43 | −4.80 | −6.99 | −8.97 | −10.73 | −12.32 | −13.87 | −15.52 | −17.33 | −19.28 |
| WSA (deg/%) | 0.00 | −76.11 | −157.64 | −228.31 | −301.67 | −370.51 | −431.78 | −482.55 | −520.68 | −545.50 | −558.28 | |
| Frontal plane | WSN (deg/%) | 0.00 | −0.82 | −4.88 | −12.31 | −23.04 | −36.74 | −52.87 | −70.65* | −89.18* | −107.47* | −124.59* |
| WSA (deg/%) | 0.00 | 0.35 | −0.09 | −1.33 | −3.63 | −7.29 | −12.43* | −18.82* | −25.88* | −32.87* | −39.40* | |
| Transverse plane | WSN (deg/%) | 0.00 | 3.74 | 5.97 | 6.53 | 5.37 | 2.62 | −1.46 | −6.48 | −11.93* | −17.30* | −22.12* |
| WSA (deg/%) | 0.00 | 12.54 | 22.66 | 29.80* | 33.88* | 34.92* | 32.93* | 27.98 | 20.51 | 10.64 | −0.50 |
*p<0.05; multiple comparison tests (Fisher’s PLSD). Significant differences were observed compared with 0.00 seconds after landing.
Examination of the hip joint in the sagittal plane (Table 2) with regard to flexion and extension revealed a significant increase in the flexion angle at 0.02–0.1 s in the WSN group and at 0.04–0.1 s in the WSA group (p<0.05). Examination of the hip joint in the frontal plane with regard to hip adduction and abduction revealed no significant difference in the adduction angle in the WSN group, but a significant increase in the adduction angle was observed at 0.07–0.1 s in the WSA group (p<0.05). Examination of the hip joint in the transverse plane with regard to internal and external rotation revealed no significant difference when analyzed by one-way ANOVA.
Table 2. Hip joint.
| Time (sec) | 0.00 | 0.01 | 0.02 | 0.03 | 0.04 | 0.05 | 0.06 | 0.07 | 0.08 | 0.09 | 0.1 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sagittal plane | WSN (deg/%) | 0.00 | 2.94 | 7.02* | 12.23* | 18.49* | 25.63* | 33.41* | 41.49* | 49.50* | 57.02* | 63.74* |
| WSA (deg/%) | 0.00 | 1.43 | 4.15 | 7.99 | 12.82* | 18.64* | 25.21* | 32.17* | 39.20* | 46.35* | 53.53* | |
| Frontal plane | WSN (deg/%) | 0.00 | 3.80 | 7.40 | 10.48 | 12.70 | 13.78 | 13.51 | 11.87 | 8.99 | 5.11 | 0.53 |
| WSA (deg/%) | 0.00 | 4.11 | 5.83 | 4.47 | −0.51 | −9.34 | −22.22 | −38.63* | −57.44* | −77.31* | −96.57* | |
| Transverse plane | WSN (deg/%) | 0.00 | −1.30 | −3.68 | −9.07 | −18.99 | −33.26 | −49.65 | −64.73 | −75.58 | −81.18 | −82.23 |
| WSA (deg/%) | 0.00 | −4.66 | −7.83 | −11.67 | −15.38 | −17.68 | −20.64 | −24.38 | −25.26 | −24.89 | −22.99 |
*p<0.05; multiple comparison tests (Fisher’s PLSD). Significant differences were observed compared with 0.00 seconds after landing.
Examination of the knee joint in the sagittal plane (Table 3) with regard to flexion and extension revealed a significant increase in the flexion angle at 0.02–0.1 s in the WSN group and at 0.04–0.1 s in the WSA group (p<0.05). Examination of the knee joint in the frontal plane with regard to varus and valgus angles revealed no significant difference when analyzed by one-way ANOVA. Examination of the knee joint in the transverse plane with regard to internal and external rotation revealed a significant difference in interval rotation at 0.04–0.1 s in the WSN group and at 0.06–0.1 s in the WSA group (p<0.05).
Table 3. Knee joint.
| Time (sec) | 0.00 | 0.01 | 0.02 | 0.03 | 0.04 | 0.05 | 0.06 | 0.07 | 0.08 | 0.09 | 0.1 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sagittal plane | WSN (deg/%) | 0.00 | 25.54 | 56.97* | 92.93* | 131.87* | 172.29* | 212.85* | 252.38* | 289.81* | 324.13* | 354.49* |
| WSA (deg/%) | 0.00 | 20.17 | 47.62 | 79.28 | 114.06* | 150.16* | 185.45* | 219.14* | 251.13* | 281.47* | 310.18* | |
| Frontal plane | WSN (deg/%) | 0.00 | 7.98 | 16.93 | 24.91 | 29.53 | 28.71 | 21.80 | 10.08 | −3.35 | −13.89 | −15.97 |
| WSA (deg/%) | 0.00 | 4.45 | 10.52 | 18.21 | 29.19 | 42.88 | 59.97 | 79.60 | 98.08 | 113.18 | 121.30 | |
| Transverse plane | WSN (deg/%) | 0.00 | −10.00 | −21.87 | −34.96 | −48.50* | −61.70* | −73.87* | −84.49* | −93.34* | −100.49* | −106.17* |
| WSA (deg/%) | 0.00 | −9.89 | −25.88 | −44.17 | −62.05 | −77.31 | −88.61* | −96.11* | −101.20* | −103.89* | −104.66* |
*p<0.05; multiple comparison tests (Fisher’s PLSD). Significant differences were observed compared with 0.00 seconds after landing.
Examination of the ankle joint in the sagittal plane (Table 4) with regard to dorsiflexion and plantar flexion revealed a significant increase in dorsiflexion at 0.01–0.1 s in the WSN group and at 0.02–0.1 s in the WSA group (p<0.05). Examination of the ankle joint in the frontal plane with regard to pronation and supination revealed no significant difference when analyzed by one-way ANOVA. Examination of the ankle joint in the transverse plane with regard to internal and external rotation revealed no significant difference when analyzed by one-way ANOVA.
Table 4. Ankle joint.
| Time (sec) | 0.00 | 0.01 | 0.02 | 0.03 | 0.04 | 0.05 | 0.06 | 0.07 | 0.08 | 0.09 | 0.1 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sagittal plane | WSN (deg/%) | 0.00 | −17.04* | −38.29* | −62.22* | −87.04* | −111.05* | −132.95* | −151.88* | −167.49* | −179.84* | −189.28* |
| WSA (deg/%) | 0.00 | −17.34 | −38.28* | −59.49* | −81.50* | −102.25* | −120.81* | −137.28* | −150.96* | −161.86* | −169.95* | |
| Frontal plane | WSN (deg/%) | 0.00 | −123.31 | −302.48 | −526.60 | −778.31 | −1,041.15 | −1,300.69 | −1,544.82 | −1,766.13 | −1,962.64 | −2,136.62 |
| WSA (deg/%) | 0.00 | −2.17 | −5.68 | −7.83 | −8.95 | −8.76 | −9.05 | −10.36 | −13.23 | −16.03 | −16.76 | |
| Transverse plane | WSN (deg/%) | 0.00 | −33.55 | −86.16 | −156.10 | −238.62 | −328.42 | −419.72 | −506.61 | −584.81 | −652.50 | −709.95 |
| WSA (deg/%) | 0.00 | 12.93 | 45.37 | 97.94 | 164.37 | 235.83 | 301.04 | 353.21 | 390.06 | 415.06 | 433.45 |
*p<0.05; multiple comparison tests (Fisher’s PLSD). Significant differences were observed compared with 0.00 seconds after landing.
DISCUSSION
Movements associated with the induction of lower-extremity injury during sports activities include single-leg landing and cutting maneuvers10). Malalignment is a condition wherein the joint deviates from the neutral position and is a risk factor for injury during such maneuvers. Activities performed with such a deviation could lead to splayfoot or posterior weight shift and hence can increase the risk of injury, depending on the site of weight-bearing along the foot during these activities11).
Several studies have assessed video footage at the time of injury and have included a 3D analysis of the knee on single-leg landing12) to establish injury prevention programs. Although all studies suggest that the knee and foot should be aligned during deep knee flexion to absorb the impact of landing13), there is no established method to assess this alignment subjectively or to determine the optimal lower-extremity alignment. In the present study, 3D motion analysis during single-leg landing was used to compare and analyze the manner in which lower-extremity joints behave during the initial 0.1 s of foot contact with the ground, which is the period associated with a high rate of anterior cruciate ligament (ACL) injury.
In the sagittal plane, the WSA group showed a tendency for posterior pelvic tilt with shallow hip and knee flexion and shallow dorsiflexion. As stated in an injury prevention program14) as well as in a study of lower-extremity injury mechanisms by Boden15), this movement pattern represents an inability to utilize deep hip and knee flexion and dorsiflexion in the lower extremity for impact absorption.
Moreover, in the frontal and transverse planes, the WSA group demonstrated anterior rotation at 0.03–0.06 s. Reduced anterior pelvic tilt decreases the ability to absorb impact and can increase mechanical stress on the knees and ankles16).
Increased mechanical stress and impact are compensated for by anterior pelvic rotation. However, the combination of anterior rotation and joint movements in the sagittal plane promotes a posterior shift in the center of mass. To compensate for this posterior weight shift, adduction of the hip joint is observed at 0.07 s.
In the frontal plane, the WSA group showed a tendency for knee valgus. With adduction of the hip joint, the knee deviates medially, resulting in knee valgus. As there was no pronation or supination of the ankle, it can be assumed that the position of the pelvis and movement of the hip led to deviation from the neutral position of the lower extremity, eventually resulting in dynamic valgus. In the transverse plane, internal rotation of the knee joint increased significantly at 0.06 s after initial foot contact with the ground in the WSA group. Kanamori17) indicated that knee valgus and internal rotation increased tensional force in the ACL and that the risk of injury to the ACL increased at 30° flexion with forced knee valgus and internal rotation. In the present study, the entire range of knee rotation, instead of only tibial internal rotation, was assessed. However, due to a combination of hip adduction and internal rotation of the knee, the WSA group was found to exhibit tibial internal rotation.
According to Nagano18), tibial internal rotation is more frequently observed during single-leg landing than during knee valgus, which is consistent with the movement of the joint axis observed in the present study. Hence, prevention of injury during single-leg landing requires tibial rotational control against knee valgus while maintaining deeper flexion in the remaining joints.
Salsich19) suggested the importance of knee pain rehabilitation in patients with a tendency for knee valgus in order to control medial knee shift in the valgus position.
Although muscle strength, range of motion, and sensory input need to be considered in order to prevent lower-extremity injury during single-leg landing and cutting maneuvers, the malalignment demonstrated by the WSA group can also be considered a factor for lower-extremity injury.
Squats should be performed with the lower extremity in the neutral position while each joint functions interdependently. However, when athletes pay increased attention to toe and knee alignment, their attention to pelvic compensation or weight-bearing proprioception from the feet is often disturbed. Hence, optimal alignment is dependent on the subjective judgment of trainers and of the athletes themselves, and malalignment is often overlooked.
The wall squat utilizes corner walls that are perpendicular to each other, which helps to align the toes and knees objectively while maintaining the lower extremity in the neutral position and allowing the individual to receive weight-bearing proprioception from the feet8). Use of the wall squat also aids in the control of common compensation patterns, such as pelvic rotations, dynamic valgus, and weight-bearing deviations in the feet observed in the training environment.
The prevention of lower-extremity injury is vital for maintaining a high performance level and providing athletes with the opportunity to have a longer professional career. Moreover, it also permits recreational-level athletes to enjoy their sports without any pain and thus lead healthier lives. Despite the widespread application of injury prevention programs, there is no established method in the training environment20). The present study sought to emphasize the need for an injury prevention program focused on the lower extremity that can be easily utilized and conducted.
REFERENCES
- 1.Heidt RS, Jr, Sweeterman LM, Carlonas RL, et al. : Avoidance of soccer injuries with preseason conditioning. Am J Sports Med, 2000, 28: 659–662. [DOI] [PubMed] [Google Scholar]
- 2.Hwangbo PN: The effects of squatting with visual feedback on the muscle activation of the vastus medialis oblique and the vastus lateralis in young adults with an increased quadriceps angle. J Phys Ther Sci, 2015, 27: 1507–1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hewett TE, Lindenfeld TN, Riccobene JV, et al. : The effect of neuromuscular training on the incidence of knee injury in female athletes. A prospective study. Am J Sports Med, 1999, 27: 699–706. [DOI] [PubMed] [Google Scholar]
- 4.Yoon SD, Sung DH, Park GD: The effect of active core exercise on fitness and foot pressure in Taekwondo club students. J Phys Ther Sci, 2015, 27: 509–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lloyd DG: Rationale for training programs to reduce anterior cruciate ligament injuries in Australian football. J Orthop Sports Phys Ther, 2001, 31: 645–654, discussion 661. [DOI] [PubMed] [Google Scholar]
- 6.Heo HJ, An DH, Won GY, et al. : EMG analysis of gluteus medius subdivisions during modified unilateral biofeedback exercises for the lower limbs. J Phys Ther Sci, 2013, 25: 85–88. [Google Scholar]
- 7.Kang MH, Jang JH, Yoo WG, et al. : Effects of shoulder flexion loaded by an elastic tubing band on EMG activity of the gluteal muscles during squat exercises. J Phys Ther Sci, 2014, 26: 1787–1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Watanabe M, Matsumoto T, Watarai K, et al. : Assessment of lower extremity alignment using the wall squat. Jpn J Clin Sports Med, 2015, 23: 224–232. [Google Scholar]
- 9.Koga H, Nakamae A, Shima Y, et al. : Mechanisms for noncontact anterior cruciate ligament injuries: knee joint kinematics in 10 injury situations from female team handball and basketball. Am J Sports Med, 2010, 38: 2218–2225. [DOI] [PubMed] [Google Scholar]
- 10.Olsen OE, Myklebust G, Engebretsen L, et al. : Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med, 2004, 32: 1002–1012. [DOI] [PubMed] [Google Scholar]
- 11.Kaufman KR, Brodine SK, Shaffer RA, et al. : The effect of foot structure and range of motion on musculoskeletal overuse injuries. Am J Sports Med, 1999, 27: 585–593. [DOI] [PubMed] [Google Scholar]
- 12.Noehren B, Barrance PJ, Pohl MP, et al. : A comparison of tibiofemoral and patellofemoral alignment during a neutral and valgus single leg squat: an MRI study. Knee, 2012, 19: 380–386. [DOI] [PubMed] [Google Scholar]
- 13.Omi Y, Yun S, Nagatsuma K, et al. : The training effect of the prevention program for anterior cruciate ligament injuries on the kinetics and kinematics of single-leg landing and lower muscular strength in female basketball players. Jpn J Clin Sports Med, 2012, 20: 56–65. [Google Scholar]
- 14.Irmischer BS, Harris C, Pfeiffer RP, et al. : Effects of a knee ligament injury prevention exercise program on impact forces in women. J Strength Cond Res, 2004, 18: 703–707. [DOI] [PubMed] [Google Scholar]
- 15.Boden BP, Dean GS, Feagin JA, Jr, et al. : Mechanisms of anterior cruciate ligament injury. Orthopedics, 2000, 23: 573–578. [DOI] [PubMed] [Google Scholar]
- 16.Sinsurin K, Vachalathiti R, Jalayondeja W, et al. : Different sagittal angles and moments of lower extremity joints during single-leg jump landing among various directions in basketball and volleyball athletes. J Phys Ther Sci, 2013, 25: 1109–1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kanamori A, Zeminski J, Rudy TW, et al. : The effect of axial tibial torque on the function of the anterior cruciate ligament: a biomechanical study of a simulated pivot shift test. Arthroscopy, 2002, 18: 394–398. [DOI] [PubMed] [Google Scholar]
- 18.Nagano Y, Ida H, Akai M, et al. : Gender differences in knee kinematics and muscle activity during single limb drop landing. Knee, 2007, 14: 218–223. [DOI] [PubMed] [Google Scholar]
- 19.Salsich GB, Graci V, Maxam DE: The effects of movement pattern modification on lower extremity kinematics and pain in women with patellofemoral pain. J Orthop Sports Phys Ther, 2012, 42: 1017–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Suzukawa M, Takahashi S, Nagano Y, et al. : Effect of a preventive program on the incidence of lower extremity injuries in junior basketball players. Jpn J Clin Sports Med, 2015, 23: 206–216. [Google Scholar]
- 21.Junzo O: TASCHENATLAS DER ANATOMIE. Bunkodo, 1997, p 225. [Google Scholar]


