Abstract
[Purpose] The present literature review was conducted on the use of different measures for the evaluation of balance in patients with Parkinson’s disease. [Materials and Methods] The PubMed, Bireme, SciELO, Lilacs, and PEDro electronic databases were searched for relevant studies. [Results] The searches initially led to the retrieval of 3,623 articles, 540 of which were potentially eligible after limiting the search to clinical trials published in the last five years. A total of 264 duplicates were removed, and 276 articles were excluded based on their titles and abstracts. The full texts of 84 articles were analyzed, and only those with a PEDro score higher than four points (n=25) were included in the review. [Conclusion] Different methods, such as scales, tests, and equipment, are used for the evaluation of balance in patients with Parkinson’s disease. More than one measure has been employed in most studies, and there is no consensus on a single precise measure for the evaluation of balance in this population.
Key words: Parkinson’s disease, Balance, Postural control
INTRODUCTION
Parkinson’s disease (Parkinson’s) is a progressive, chronic, neurodegenerative disease1) stemming from the atrophy of grey matter. It is estimated that 10 million individuals around the world suffer from Parkinson’s, and this figure is expected to double by the year 20302). The prevalence of Parkinson’s ranges from 0.3% among individuals aged less than 60 years to 1% among those aged 60 or older3). The progressive nature of the disease causes both motor and non-motor alterations. The main motor alterations are associated with the risk of falls, which leads to a sedentary lifestyle and the reduction in activities of daily living exerts a negative impact on clinical aspects1,2,3,4,5).
The main clinical manifestations of Parkinson’s are shaking, stiffness, slowness of movement, postural alterations, and stooped gait, leading patients to adopt a flexed posture due to the dominance of pro-gravitational muscles, with forward leaning of the head, the chin tlited toward the thorax, kyphotic thorax, protracted shoulders, the arms rotated internally, and, flexion of the hips, knees, and elbows, which projects the body forward, compromising postural orientation and leading to impaired balance6). All these postural changes, together with other alterations, lead to postural instability, which is considered one of the main characteristics of patients with Parkinson’s. This instability leads to a progressive reduction in both static and dynamic balance, affecting one’s ability to remain standing without support or even sit down.
Researchers believe that postural instability is related to the loss of the capacity to control intentional movements of the center of body mass on the support base during activities that involve the transfer of weight. Many individuals with Parkinson’s demonstrate inadequate interactions among the vestibular, visual, and proprioceptive systems, with consequent changes in the biomechanics of the body7).
The motor rehabilitation process for patients with Parkinson’s is normally directed toward static and functional balance training to provide greater interactions with the surrounding environment through treadmill training8), balance training involving virtual reality programs9), the combination of dance and motor training10), etc. A set of assessment measures to determine the effects of particular interventions has been validated and reported in literature11). Assessment measures are important for analysis of functional changes in all stages of the disease and are particularly sensitive with regard to the evaluation of therapeutic intervention12). The Unified Parkinson’s Disease Rating Scale (UPDRS)13), Berg Balance Scale, Timed Up and Go Test14), Six-Minute Walk Test (6WMT), 10-Meter Walk Test (10MWT)15), and a force plate to determine the center of pressure16) are among the measures used for the evaluation of balance. Moreover, a combination of different measures previously used in controlled clinical trials is often employed.
The aim of the present study was to perform a systematic review of the literature for the analysis of different measures used in the evaluation of balance in patients with Parkinson’s disease.
MATERIALS AND METHODS
The PubMed (National Library of Medicine), BVS Bireme, SciELO, LILACS and PEDro electronic databases were searched for relevant studies addressing balance in patients with Parkinson’s disease. For this purpose, the following combinations of keywords were used: Parkinson’s disease and balance evaluation, Parkinson Disease and balance alterations, Parkinson Disease and balance change, Parkinson Disease and change in balance, Parkinson Disease and Balance Control and Parkinson Disease and Postural Control Balance. The search was limited to randomized controlled, clinical trials published in the previous five years (inclusion criteria).
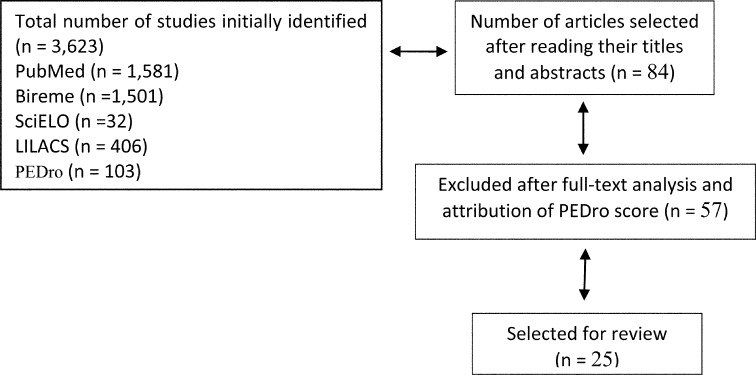
The searches initially led to the retrieval of 3,623 articles, 540 of which were potentially eligible based on the inclusion and exclusion criteria. A total of 264 duplicates were removed, and 276 articles were excluded based on their titles and abstracts. The full texts of 84 articles were analyzed, with the inclusion of only those that met the eligibility criteria and had a PEDro score higher than four points. Thus, 25 studies were selected for the present systematic review (Fig. 1).
Fig. 1.
Flowchart of studies included in the present literature review
RESULTS
Table 1 displays the PEDro scores of the 25 studies that met the eligibility criteria and were included in the present systematic review. Diverse methods for the evaluation of balance in individuals with Parkinson’s were used in studies with different intervention protocols and comparisons between the experimental and control groups (Table 2).
Table 1. Scores of articles included in literature review.
| Reference | Item | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Eligibility | 1- Randomized allocation | 2- Confidential allocation | 3- Similar prognosis | 4- Blinded subjects | 5- Blinded therapists | 6- Blinded evaluators | 7- Key results | 8- Intention to treat analysis | 9- Comparison between groups | 10- Precision and variability | Score | |
| Abud Qutubuddin et al., 201317) | Y | Y | N | Y | N | N | Y | N | N | Y | Y | 5/10 |
| Sara Pires et al., 201418) | Y | Y | N | Y | N | N | Y | Y | N | Y | Y | 6/10 |
| Chirs J., Hass et al., 201219) | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | 6/10 |
| Fuzhong Li et al., 201220) | Y | Y | N | Y | N | N | Y | Y | Y | Y | Y | 7/10 |
| Xia Shen et al., 201521) | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8/10 |
| Natalie E., Allen et al., 201022) | Y | Y | Y | Y | N | N | N | Y | N | Y | Y | 6/10 |
| Emma Stack et al., 201223) | Y | Y | Y | Y | N | N | Y | N | N | N | Y | 5/10 |
| Xian Shen et al., 20148) | Y | Y | Y | Y | N | N | N | Y | Y | Y | Y | 7/10 |
| C., Tassorelli et al., 201424) | Y | Y | Y | Y | Y | Y | N | Y | N | Y | Y | 8/10 |
| Nima Toosizadeh et al., 201425) | Y | Y | Y | Y | Y | N | N | Y | N | Y | Y | 7/10 |
| Alessandro Picelli et al., 201226) | Y | Y | N | Y | N | N | N | Y | N | Y | Y | 5/10 |
| Nicola Smania et al., 201027) | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 10 |
| Mohan Ganesan et al., 201428) | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | 6/10 |
| José Eduardo Pompeu et al., 20129) | Y | Y | N | Y | N | N | Y | Y | N | Y | Y | 6/10 |
| Nan-yong Lee et al., 201510) | Y | Y | N | Y | N | N | N | Y | N | Y | Y | 5/10 |
| Elisa Pelosin et al., 201029) | Y | Y | N | Y | N | N | N | Y | N | Y | Y | 6/10 |
| Atefeh Azarpaikan et al., 201430) | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 10 |
| Giuzeppe Frazzitta et al., 201431) | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 10 |
| Colleen G., Canning et al., 201432) | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 9/10 |
| Margaret Schenkman et al., 201233) | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | 10 |
| Gustavo Christofoletti et al., 201034) | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8/10 |
| Gao Qiang et al., 201435) | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8/10 |
| Serene S Paulo et al., 201436) | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 10 |
| Xia Shen et al., 201237) | Y | Y | Y | Y | N | N | Y | N | Y | Y | Y | 7/10 |
| Ryan P., Duncan et al., 201238) | Y | Y | Y | Y | N | N | Y | N | Y | Y | Y | 7/10 |
Y: yes; N: no
Table 2. Characteristics of the studies included in the present systematic review.
| Authors and year of publication | Study design | Intervention | Outcomes |
|---|---|---|---|
| Abud Qutubuddin et al., 201317) | Clinical trial | Forced exercise on stationary bike (EG) | 1-UPDRS |
| 2-BBS | |||
| 3-Finger Taping Test | |||
| 4-PDQ-39 | |||
| Sara Pires et al., 201418) | Clinical trial | Combination of musical auditory cues and regular
physical therapy (EG) Regular physical therapy alone (CG) |
1-UPDRS |
| 2-BBS | |||
| 3-TUG | |||
| 4-PDQ-39 | |||
| Chirs J.Hass et al., 201119) | Clinical trial | PRT program (EG) No intervention (CG) |
1-FRT |
| 2-TUG | |||
| 3-UPDRS | |||
| Fuzhong Li et al., 201220) | Clinical trial | Adapted Tai Chi program Tree groups; Tai chi, resistance training, and stretching |
1-Isokinetic dynamometer |
| 2-GAITRite | |||
| 3-FRT | |||
| 4-UPRDS | |||
| 5-TUG | |||
| Fuzhong Li et al., 201220) | Clinical trial | Technology-assisted balance and gait training (EG) Strengthening exercises (CG) |
1-Single-leg stance test |
| Natalie E. Allen et al., 201022) | Clinical trial | Minimally supervised exercise program | 1-Algorithm |
| 2-Coordinated stability test | |||
| 3-Sway meter | |||
| 4-BBS | |||
| 5-FOG Questionnaire | |||
| 6-SPPB | |||
| 7-Short -FES | |||
| 8-PDQ-39 | |||
| Xian Shen et al., 20148) | Clinical trial | Balance and gait training with enhanced feedback
(EG) Lower limb strength training (CG) |
1-ABC |
| 2-Limits-of-stability test | |||
| 3-Single-leg stance test | |||
| C. Tassorelli et al., 201424) | Clinical trial | Injection of botulinum toxin type A + intensive program
(EG) Saline solution + intensive program (CG) |
1-Kinematic analysis of movement |
| 2-EMG | |||
| 3-UPRDS | |||
| 4-VAS | |||
| Nima Toosizadeh et al., 201425) | Clinical trial | Electroacupuncture (EG) Sham treatment (CG) |
1-SF-12 |
| 2-Short-FES | |||
| 3-MMSE | |||
| 4-UPRS | |||
| Alessandro Picelli et al., 201226) | Clinical trial | Robot-assisted treadmill training (EG) Treadmill training alone (CG) |
1-BBS |
| 2-ABC | |||
| 3-TUG | |||
| 4-10MWT | |||
| Nicola Smania et al., 201027) | Clinical trial | Balance training (EG) General physical exercises (CG) |
1-BBS |
| 2-ABC | |||
| 3-Postural transfer test | |||
| 4-COP | |||
| 5-UPRDS | |||
| 6-H&Y | |||
| 7-Staging scale | |||
| 8-GDS | |||
| Mohan Ganesan et al., 201328) | Clinical trial | Tree groups: dopamine, dopamine + conventional treadmill training, dopamine + PWSTT |
1-UPDRS |
| 2-Dynamic posturography | |||
| 3-BBS | |||
| 4-POMA | |||
| José Eduardo Pompeu et al., 20129) | Clinical trial | Training performed with 10 Wii FitTM games (EG) Balance exercises (CG) |
1-UPRS |
| Nam-Yong Lee et al., 201510) | Clinical trial | NDS + FES + Dance (EG) NDS + FES (CG) |
1-BBS |
| 2-Modified Barthel Index | |||
| 3-Beck Depression Inventory | |||
| Elisa Pelosin et al., 201029) | Clinical trial | Physical therapy + strategic video (EG) Physical therapy + video of landscapes (CG) |
1-FOG Questionnaire |
| Atefeh Azarpaikan et al., 201430) | Clinical trial | NFT training period | 1-BBS |
| 2-ECG | |||
| 3-Isokinetic dynamometer | |||
| Giuzeppe Frazzitta et al., 201431) | Clinical trial | Intensive aerobic exercises (EG) Non-intensive exercises (CG) |
1-UPDRS |
| 2-BBS | |||
| 3-6WMT | |||
| Colleen G. Canning et al., 201432) | Clinical trial | Minimally supervised exercises –PD WEBB (EG) Habitual care (CG) |
1-Coordinated balance stability test |
| 2-FOG Questionnaire | |||
| 3-FES-I | |||
| 4-Physical Activity Questionnaire | |||
| 5-SF-12V2 | |||
| 6-SF-6D | |||
| 7-PDQ-39 | |||
| Margaret Schenkman et al., 201233) | Clinical trial | Supervised FBF and AE physical exercise program
(EG) Conventional at-home physical exercise (CG) |
1-CS-PFP |
| 2-FRT | |||
| 3-UPRDRS | |||
| 4-PDQ-39 | |||
| Gustavo Christofoletti et al., 201034) | Clinical trial | Balance and motor function stimulation exercise protocol (EG) | 1-BBS |
| 2-TUG | |||
| Gao Qiang et al., 201435) | Clinical trial | Yang-style Tai Chi exercise protocol (EG) No intervention (CG) |
1-BBS |
| 2-TUG | |||
| 3-UPDRS | |||
| Serene S Paulo et al., 201436) | Clinical trial | Muscle strength training of legs with pneumatic
equipment (EG) Simulated low-intensity exercise (CG) |
1-Muscle strength |
| 2-10MWT | |||
| 3-TUG | |||
| 4- Single-leg stance test | |||
| Xia Shen et al., 201237) | Clinical trial | Training with repetitive steps on preparatory visual
tracks (EG) UM-detook (CG) |
1-UPRDS |
| 2-Limits-of-stability test | |||
| 3-GAITRite | |||
| Ryan P. Duncan et al., 201238) | Clinical trial | Tango dance program (EG) No intervention (CG) |
1-UPRDS |
| 2- Mini BESTest | |||
| 3-FOG Questionnaire | |||
| 4-6WMT | |||
| 5-9HPT | |||
| 6-GAITRite | |||
DISCUSSION
In the context of chronic neurological disorders, efforts are made to diminish physical difficulties and allow affected individuals to perform activities of daily living with the greatest possible efficiency and independence38). Thus, assessment tools and specific measures that address more generic aspects, such as muscle strength, range of motion, functioning, and improvements in quality of life, are needed for individuals with Parkinson’s. It is important for assessment methods to analyze functional changes in all stages of the disease and to be particularly sensitive in the evaluation of therapeutic interventions39).
Among the specific Parkinson’s classification measures used in the studies analyzed, the UPDRS is a validated scale that provides an objective perspective and allows the classification of individuals with Parkinson’s. The UPDRS is also widely used by physiotherapists for the evaluation of balance in clinical practice, as it has specific items for the assessment of this characteristic. The scale was found to be precise and sensitive according to the results of 14 articles analyzed in the present systematic review, the study populations of wich were subject to different intervention protocols40). The scale was validated for the population with Parkinson’s and, in contains items for the assessment of balance. Volpe et al. 41) conducted a study involving 24 patients with Parkinson’s allocated to two groups and assessed balance using the UPDRS. Regarding the motor skills section of the scale, the authors found a significant improvement in the experimental group (dance) in comparison with the control group (conventional physical therapy).
Eleven studies included in the present review used the Berg Balance Scale for the assessment of balance. This scale is composed of 14 tasks that are common in daily living. Each item is scored from 0 to 4 points, with a maximum score of 56 points. The points are based on the time for which a position is held, the distance to which the upper limb is capable of reaching out in front of the body, and the time required to complete each task42). This is a fast, precise assessment tool for detecting changes in balance among individuals with Parkinson’s. In a previous systematic review with meta-analysis, Chih-Hsuan Chou et al. 43) found that a reduction in the gait velocity score on the Berg Balance Scale was correlated with impairment regarding the performance of activities of daily living.
The Timed Up and Go Test is used to quantify functional mobility based on the time (in seconds) required to perform the task of standing up from a chair (seat approximately 46 in height and armrests 65 cm in height), walking three meters, turning around, returning to the chair, and sitting down again42). This measure has a specific relationship with gait speed and functional mobility. In the population studied, the Timed Up and Go Test is a good predictor of the risk of falls. Although it was not specifically designed for the assessment of balance, the importance of this measure to the evaluation of dynamic balance related to mobility was evident in the studies analyzed in the present review. In a systematic review with meta-analysis involving 53 studies, Schoene et al. 44) found that the Timed Up and Go Test was a sensitive assessment tool for the evaluation of gait stability and balance in more than 50% of the studies, which is in agreement with the findings of the present systematic review.
A large portion of the studies employed three or more assessment tools, which were always accompanied by tests and equipment. Several studies have addressed the use of assessment measures for the evaluation of balance among individuals with Parkinson’s with the aim of designing interventions that favor an improvement in quality of life and a reduction in the risk of falls. Thus, the studies analyzed evaluated individuals in a complex fashion with functional approaches that were adaptable to the needs of such patients.
The present review shows that a variety of different assessment tools are used for the evaluation of balance in patients with Parkinson’s disease, such as scales, tests, and equipment. The majority of studies employed more than one measure, and there is no consensus regarding a single, precise assessment tool for the evaluation of balance in this population.
Acknowledgments
The authors gratefully acknowledge financial support from the Brazilian National Council for Scientific and Technological Development (CNPq).
REFERENCES
- 1.Uhrbrand A, Stenager E, Pedersen MS, et al. : Parkinson’s disease and intensive exercise therapy—a systematic review and meta-analysis of randomized controlled trials. J Neurol Sci, 2015, 353: 9–19. [DOI] [PubMed] [Google Scholar]
- 2.King LA, Priest KC, Nutt J, et al. : Comorbidity and functional mobility in people with Parkinson’s disease. PM R, 2014, 94: 2152–2157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lenka A, Jhunjhunwala KR, Saini J, et al. : Structural and functional neuroimaging in patients with Parkinson’s disease and visual hallucinations: a critical review. Parkinsonism Relat Disord, 2015, 21: 683–691. [DOI] [PubMed] [Google Scholar]
- 4.Yogev-Seligmann G, Giladi N, Gruendlinger L, et al. : The contribution of postural control and bilateral coordination to the impact of dual tasking on gait. Exp Brain Res, 2013, 226: 81–93. [DOI] [PubMed] [Google Scholar]
- 5.Conradsson D, Lofreguen N, Stahlea A, et al. : The conceptual framework of the novel to balance training in Parkinson’s disease study protocol fartor a randomized controlled trial. BMC Neurol, 2012, 12: 111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Takeuti T, Maki T, Silva CV, et al. : Correlation between balance and incidence of falls in patients with Parkinson’s disease. Neurocienc, 2011, 19: 237–243. [Google Scholar]
- 7.Abe PT, Vitorino DF, Guimarães LH, et al. : Análise do equilíbrio nos pacientes com doença de Parkinson grau leve e moderado através da fotogrametria. Neurocienc, 2004, 12: 2. [Google Scholar]
- 8.Shen X, Mak MK: Balance and gait training with augmented feedback improves balance confidence in people with Parkinson’s disease: a randomized controlled trial. Neurorehabil Neural Repair, 2014, 28: 524–535. [DOI] [PubMed] [Google Scholar]
- 9.Pompeu JE, Mendes FA, Silva KG, et al. : Effect of Nintendo Wii™-based motor and cognitive training on activities of daily living in patients with Parkinson’s disease: a randomised clinical trial. Physiotherapy, 2012, 98: 196–204. [DOI] [PubMed] [Google Scholar]
- 10.Lee NY, Lee DK, Song HS: Effect of virtual reality dance exercise on the balance, activities of daily living, and depressive disorder status of Parkinson’s disease patients. J Phys Ther Sci, 2015, 27: 145–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Song CS: Intrarater reliability of action research arm test for individuals with Parkinson’s disease. J Phys Ther Sci, 2012, 24: 1355–1357. [Google Scholar]
- 12.Sampaio RF, Mancini MC, Fonseca ST: Produção científica e atuação profissional: aspectos que limitam essa integração na fisioterapia e na terapia ocupacional. Rev Bras Fisioter, 2002, 6: 3. [Google Scholar]
- 13.Cholewa J, Gorzkowska A, Szepelawy M, et al. : Influence of functional movement rehabilitation on quality of life in people with Parkinson’s disease. J Phys Ther Sci, 2014, 26: 1329–1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bennie S, Bruner K, Dizon A, et al. : Measurements of balance: comparison of the timed ‘Up and Go’ test reach test with the Berg Balance Scale. J Phys Ther Sci, 2003, 15: 93–97. [Google Scholar]
- 15.Henmi O, Shiba Y, Saito T, et al. : Spectral analysis of gait variability of stride interval time series: comparison of young, elderly and Parkinson’s disease patients. J Phys Ther Sci, 2009, 21: 105–111. [Google Scholar]
- 16.Han J, Jung J, Lee J, et al. : Effect of muscle vibration on postural balance of Parkinson’s diseases patients in bipedal quiet standing. J Phys Ther Sci, 2013, 25: 1433–1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Qutubuddin A, Reis T, Alramadhani R, et al. : Parkinson’s disease and forced exercise: a preliminary study. Rehabil Res Pract, 2013, 2013: 375267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pires S, Festas MJ, Soares T, et al. : Pistas auditivas musicais na fisioterapia em grupo de doentes com Parkinson. Investigação original, 2014, 28: 162–166. [Google Scholar]
- 19.Hass CJ, Buckley TA, Pitsikoulis C, et al. : Progressive resistance training improves gait initiation in individuals with Parkinson’s disease. Gait Posture, 2012, 35: 669–673. [DOI] [PubMed] [Google Scholar]
- 20.Li F, Harmer P, Fitzgerald K, et al. : Tai chi and postural stability in patients with Parkinson’s disease. N Engl J Med, 2012, 366: 511–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shen X, Mak MK: Technology-assisted balance and gait training reduces falls in patients with Parkinson’s disease: a randomized controlled trial with 12-month follow-up. Neurorehabil Neural Repair, 2015, 29: 103–111. [DOI] [PubMed] [Google Scholar]
- 22.Allen NE, Canning CG, Sherrington C, et al. : The effects of an exercise program on fall risk factors in people with Parkinson’s disease: a randomized controlled trial. Mov Disord, 2010, 25: 1217–1225. [DOI] [PubMed] [Google Scholar]
- 23.Stack E, Roberts H, Ashburn A: The PIT: SToPP Trial—A Feasibility Randomised Controlled Trial of Home-Based Physiotherapy for People with Parkinson’s Disease Using Video-Based Measures to Preserve Assessor Blinding. Parkinson Disorders, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tassorelli C, De Icco R, Alfonsi E, et al. : Botulinum toxin type A potentiates the effect of neuromotor rehabilitation of Pisa syndrome in Parkinson disease: a placebo controlled study. Parkinsonism Relat Disord, 2014, 20: 1140–1144. [DOI] [PubMed] [Google Scholar]
- 25.Toosizadeh N, Lei H, Schwenk M, et al. : Does integrative medicine enhance balance in aging adults? Proof of concept for the benefit of electroacupuncture therapy in Parkinson’s disease. Gerontology, 2015, 61: 3–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Picelli A, Melotti C, Origano F, et al. : Does robotic gait training improve balance in Parkinson’s disease? A randomized controlled trial. Parkinsonism Relat Disord, 2012, 18: 990–993. [DOI] [PubMed] [Google Scholar]
- 27.Smania N, Corato E, Tinazzi M, et al. : Effect of balance training on postural instability in patients with idiopathic Parkinson’s disease. Neurorehabil Neural Repair, 2010, 24: 826–834. [DOI] [PubMed] [Google Scholar]
- 28.Ganesan M, Sathyaprabha TN, Gupta A, et al. : Effect partial weight supported treadmill gait train balance patients Parkinson. Dis Am Acad Phys Med Rehabil, 2014, 6: 22–33. [DOI] [PubMed] [Google Scholar]
- 29.Pelosin E, Avanzino L, Bove M, et al. : Action observation improves freezing of gait in patients with Parkinson’s disease. Neurorehabil Neural Repair, 2010, 24: 746–752. [DOI] [PubMed] [Google Scholar]
- 30.Azarpaikan A, Torbati HT, Sohrabi M: Neurofeedback and physical balance in Parkinson’s patients. Gait Posture, 2014, 40: 177–181. [DOI] [PubMed] [Google Scholar]
- 31.Frazzitta G, Maestri R, Ghilardi MF, et al. : Intensive rehabilitation increases BDNF serum levels in parkinsonian patients: a randomized study. Neurorehabil Neural Repair, 2014, 28: 163–168. [DOI] [PubMed] [Google Scholar]
- 32.Canning CG, Sherrington C, Lord R, et al. : Exercise for falls prevention in Parkinson disease: a randomized controlled trial. Neurology, 2015, 84: 304–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schenkman M, Hall DA, Barón AE, et al. : Exercise for people in early- or mid-stage Parkinson disease: a 16-month randomized controlled trial. Phys Ther, 2012, 92: 1395–1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Christofoletti G, Freitas RT, Candido ER, et al. : Effectiveness of a physical therapy treatment on static and dynamic balance of subjects with Parkinson’s disease. Fisioterapia Pesquisa, 2010, 17: 259–263. [Google Scholar]
- 35.Gao Q, Leung A, Yang Y, et al. : Effects of Tai Chi on balance and fall prevention in Parkinson’s disease: a randomized controlled trial. Clin Rehabil, 2014, 28: 748–753. [DOI] [PubMed] [Google Scholar]
- 36.Paul SS, Canning CG, Song J, et al. : Leg muscle power is enhanced by training in people with Parkinson’s disease: a randomized controlled trial. Clin Rehabil, 2014, 28: 275–288. [DOI] [PubMed] [Google Scholar]
- 37.Shen X, Mak MK: Repetitive step training with preparatory signals improves stability limits in patients with Parkinson’s disease. J Rehabil Med, 2012, 44: 944–949. [DOI] [PubMed] [Google Scholar]
- 38.Duncan RP, Earhart GM: Randomized controlled trial of community-based dancing to modify disease progression in Parkinson disease. Neurorehabil Neural Repair, 2012, 26: 132–143. [DOI] [PubMed] [Google Scholar]
- 39.Horta W: Escalas clínicas para avaliação de pacientes com doença de parkinson. In: Meneses Ms, Teive HAG. Doença de Parkinson: aspectos clínicos e cirúrgicos. Rio de Janeiro Guanabara Koogan, 1996, pp 83–96. [Google Scholar]
- 40.Schenkman ML, Clark K, Xie T, et al. : Spinal movement and performance of a standing reach task in participants with and without Parkinson disease. Phys Ther, 2001, 81: 1400–1411. [DOI] [PubMed] [Google Scholar]
- 41.Volpe D, Signorini M, Marchetto A, et al. : A comparison of Irish set dancing and exercises for people with Parkinson’s disease: a phase II feasibility study. BMC Geriatr, 2013, 13: 54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Karuka AH, Silva JA, Navega MT: Analysis of agreement of assessment tools of body balance in the elderly. Rev Bras Fisioter, 2011, 15: 460–466. [PubMed] [Google Scholar]
- 43.Chou CH, Hwang CL, Wu YT: Effect of exercise on physical function, daily living activities, and quality of life in the frail older adults: a meta-analysis. Arch Phys Med Rehabil, 2012, 93: 237–244. [DOI] [PubMed] [Google Scholar]
- 44.Schoene D, Wu SM, Mikolaizak AS, et al. : Discriminative ability and predictive validity of the timed up and go test in identifying older people who fall: systematic review and meta-analysis. J Am Geriatr Soc, 2013, 61: 202–208. [DOI] [PubMed] [Google Scholar]