Abstract
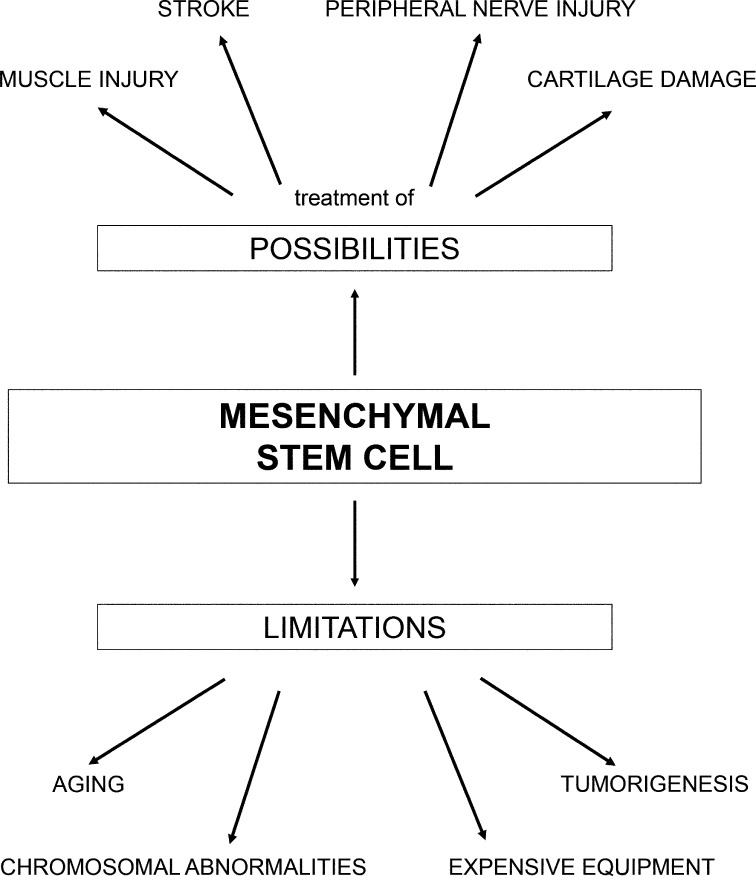
[Purpose] Regenerative medicine and rehabilitation contribute in many ways to a specific plan of care based on a patient’s medical status. The intrinsic self-renewing, multipotent, regenerative, and immunosuppressive properties of mesenchymal stem cells offer great promise in the treatment of numerous autoimmune, degenerative, and graft-versus-host diseases, as well as tissue injuries. As such, mesenchymal stem cells represent a therapeutic fortune in regenerative medicine. The aim of this review is to discuss possibilities, limitations, and future clinical applications of mesenchymal stem cells. [Subjects and Methods] The authors have identified and discussed clinically and scientifically relevant articles from PubMed that have met the inclusion criteria. [Results] Direct treatment of muscle injuries, stroke, damaged peripheral nerves, and cartilage with mesenchymal stem cells has been demonstrated to be effective, with synergies seen between cellular and physical therapies. Over the past few years, several researchers, including us, have shown that there are certain limitations in the use of mesenchymal stem cells. Aging and spontaneous malignant transformation of mesenchymal stem cells significantly affect the functionality of these cells. [Conclusion] Definitive conclusions cannot be made by these studies because limited numbers of patients were included. Studies clarifying these results are expected in the near future.
Key words: Mesenchymal stem cells, Regenerative rehabilitation
INTRODUCTION
Regenerative medicine is a new field of medicine that combines information from several medical areas with the aim to recover the organ function lost due to congenital defects, damage, disease, or age1,2,3,4,5,6,7,8). The four main approaches of regenerative medicine include cell therapy, gene therapy, transplantation, and tissue engineering6, 9,10,11). Previous results from experimental and clinical studies have confirmed the efficacy and safety of these procedures6, 7, 9, 11,12,13). At the same time, they can contribute to the maintenance of homeostasis, with stem cells sustaining long-term tissue regeneration when a biological system has depleted its own self-repair mechanisms and reserves14, 15). The liver and skeletal muscles have shown good regenerative potential. In addition, recent research suggests that self-repair mechanisms exist in all tissues of the body14, 16).
Mesenchymal stem cells (MSCs) are progenitor cells that have self-renewal and multi-lineage differentiation capabilities along with immunomodulatory activities17), regenerating all of the cell types in the tissue where they are located18). MSCs reside in a specialized physical location known as a niche, which constitutes a three-dimensional microenvironment containing, in addition to the MSCs, neighboring differentiated cell types and the extracellular matrix19). MSCs may express greater plasticity than traditionally attributed, since they can cross lineage barriers and be reprogrammed, adopting the functional phenotypes and expression profiles of cells from other tissues. Consequently, these cells may be useful in regenerative medicine and tissue engineering20,21,22).
Previously it was thought that MSCs are not limited in their application, and that they represent a therapeutic fortune. However, several researchers, including us, have recently demonstrated that this notion is incorrect and that there are certain limitations in the use of MSCs23,24,25). The aim of this review is to discuss the possibilities, limitations, and future clinical applications of MSCs (Table 1).
Table 1. Characteristics of the articles included in this review.
| MSCs in regenerative rehabilitation | Main results | First author, journal, and year of publication (chronology) | Ref. |
|---|---|---|---|
| MSCs in the rehabilitation of damaged muscles | Rejuvenation of the aged skeletal muscle, increased muscle healing after severe injury, slowed muscle tissue degeneration, without significant complications. | McBride TA et al. Mech Ageing Dev, 1995. | 43) |
| Jubrias SA et al. J Appl Physiol, 2001. | 44) | ||
| Dreyer HC et al. Muscle Nerve, 2006. | 42) | ||
| Tanaka S et al. J Phys Ther Sci, 2009. | 45) | ||
| Ambrosio F et al. Tissue Eng Part A, 2010. | 41) | ||
| Tanaka S et al. J Phys Ther Sci, 2015. | 46) | ||
| MSCs in stroke rehabilitation | Formation of synapses and axons and improvement in electrophysiological parameters, clinical improvement on determined by the Stroke Impact Scale and Action Research Arm Test, without significant complications. | Kondziolka D et al. Neurology, 2000. | 47) |
| Nelson PT et al. Am J Pathol, 2002. | 49) | ||
| Kondziolka D et al. J Neurosurg, 2005. | 48) | ||
| Lee JS et al. Stem Cells, 2010. | 50) | ||
| Bhasin A et al. Cerebrovasc Dis Extra, 2011. | 51) | ||
| Honmou O et al. Brain, 2011. | 52) | ||
| Park K et al. J Phys Ther Sci, 2015. | 53) | ||
| MSCs in the rehabilitation of damaged peripheral nerves | Improved axonal organization and increased myelin thickness, better functional recovery and improvement in nerve regeneration, without significant complications. | Salomone R, et al. Muscle Nerve, 2013. | 57) |
| Guo ZY et al. Neural Regen Res, 2015. | 54) | ||
| Wang P et al. Neurosci Lett, 2015. | 55) | ||
| Seyed Foroutan K et al. Trauma Mon, 2015. | 56) | ||
| Lasso JM, et al. J Plast Reconstr Aesthet Surg, 2015. | 58) | ||
| MSCs in the rehabilitation of damaged cartilage | Repair of damaged cartilage, cartilage healing, efficient recovery of function, without significant complications. | Cao L, et al. Biomaterials, 2011. | 61) |
| Johnson K, et al. Science, 2012. | 60) | ||
| Wei X, et al. Acta Pharmacol Sin, 2013. | 59) |
REGENERATIVE REHABILITATION—A NEW FIELD OF MEDICINE
The definition of regenerative rehabilitation can be found on the American Physical Therapy Association website: “Regenerative Rehabilitation is the integration of principles and approaches from rehabilitation and regenerative medicine with the ultimate goal of developing innovative and effective methods that promote the restoration of function through tissue regeneration and repair.”26)
In order to become a functionally vital organ, a regenerated organ must adapt to the existing homeostasis of the entire body. Transplanted organs undergo a number of adaptive processes to resume their potential27, 28). Rehabilitation is crucial to the success of regenerative medicine, and regenerative medicine and rehabilitation can contribute in many ways in patient treatment and care plans. The integration of rehabilitation into regenerative medicine is necessary to achieve an optimal end point.
POSSIBILITIES IN THE APPLICATION OF MSCS TO REGENERATIVE REHABILITATION
Skeletal muscle treatments have integrated regenerative medicine and rehabilitation. Regardless of the cause of injury, muscle injury recovery consists of degeneration, inflammation, regeneration, and fibrosis29, 30). Chronic and severe muscle damage usually only partially heals and scar tissue forms or fibrosis results, while acute and minor injuries heal well in most cases. If a scar lingers, total regeneration of the muscle is impossible. An alternative approach has been introduced by regenerative medicine, which includes the treatment of skeletal muscle injuries by promoting myofiber regeneration and inhibiting the formation of scar tissue. A factor contributing to the formation of scar tissue is transforming growth factor beta 1, TGF-β131, 32); hence, administration of TGF-β1-specific inhibitors has been suggested as an anti-fibrogenic approach33,34,35). In animal models, TGF-β1 antagonists have decreased fibrosis remarkably, while concomitantly improving myofiber regeneration33, 34). The regeneration of myofibers is mostly accomplished by muscle MSCs, or satellite cells (Fig. 1). These cells are concentrated in the myofiber periphery and are activated in response to muscle injury36,37,38). The age-related dysfunction of these muscle stem cells in the elderly leads to an impaired healing response following skeletal muscle injury. Factors circulating in the aged microenvironment force the differentiation of muscle stem cells from a myogenic to a fibrogenic lineage39), resulting in enhanced scar tissue formation. Further compromising regeneration, the profibrogenic switch is accompanied by decreased proliferative capacity of aged muscle stem cells. Therefore, it is logical to propose transplanting young muscle stem cells in order to enhance the regenerative potential of aged skeletal muscles. However, this is not advisable. The transplantation of even embryonic stem cells into an aged environment results in a rapid decline in their regenerative potential40). Rejuvenation of aged skeletal muscles would help transplanted stem cells in the treatment of skeletal muscle injuries. According to a rodent study, running on a treadmill after stem cell transplantation into severely contused muscle increases the myogenic contribution of the donor cells41). Therefore, a synergy between physical and cellular therapies may exist. Thus, muscles capable of producing a contraction may serve as a powerful tool in rejuvenating the regenerative potential of aged muscle. There is plenty of evidence showing that even exercise programs initiated late in life may enhance the ability of muscle healing after severe injury, while concomitantly slowing down tissue degeneration42,43,44,45,46).
Fig. 1.
Mesenchymal stem cells: possibilities and limitations in their application
In addition to application to the recovery of injured muscles, MSCs can be applied in rehabilitation after cerebrovascular insult (Fig. 1). Sixteen years ago Kondziolka et al. published results of the first clinical study of cell therapy for stroke47). Twelve patients, 6 months to 6 years after cerebral infarction onset, were treated by transplantation of immortalized NT2N cells into the subcortical grey matter. These cells were treated with retinoic acid, which led to differentiation into functional neurons. Of note, after transplantation in animal models of stroke, the NT2N cells formed synapses and axons and led to improvements in electrophysiological parameters. However, three patients died before the end of the study. The reasons for death were recurrent stroke, myocardial infarct (MI), and pneumonia. In contrast, no complications48) were observed in the following study that included 14 patients. In these patients, clinical improvement was determined by the Stroke Impact Scale and Action Research Arm Test. However, the drawback of this study was the small number of patients. In addition, one of the treated patients died 27 months after cell transplantation from MI. The autopsy showed that the injected cells survived for at least 2 years after therapy49). In the past few years, several clinical studies of cellular therapy50,51,52,53) have resulted in many publications on the topic. In these and similar studies, MSCs were usually applied intravenously from 5–9 days to 3–12 months after stroke. The transplantations were conducted safely, without significant complications. In spite of this, definitive conclusions from these studies cannot be made since the studies included small numbers of patients.
Direct treatment of damaged peripheral nerves with MSCs has also been demonstrated to be effective. Numerous encouraging animal studies have shown that stem or progenitor cell treatments can rescue some degree of neurological function after injury54,55,56) (Fig. 1). In a rat model of facial nerve injury, MSCs were applied to a transected facial nerve after anastomosis. The results showed that the MSC-treated nerve showed improvements in terms of axonal organization and myelin thickness when compared to nerves that had only been sutured57). In another study, MSCs were injected subepineurally one week after sciatic nerve injury in rabbits. Nerves that were grafted with MSCs showed better functional recovery and improved nerve regeneration58).
Although the exact mechanism by which MSCs repair damaged cartilage is still not known, the ability of these cells to induce proliferation and differentiation of resident progenitor cells or their innate ability to differentiate into chondrocytes may contribute to the repair of damaged cartilage (Fig. 1)59). Transduced MSCs expressing IL-1Ra or antagonists of TNF may both enhance the reparative process through their inherent chondrogenic potential and retard the degradative process in cartilage lesions60). Advances in the fabrication of biodegradable scaffolds that serve as beds for MSC implantation will hopefully lead to better biocompatibility and host tissue integration. In addition, minimal toxicity has been observed in studies using animal models and genetically manipulated stem cells transduced with retroviral and adenoviral vectors61). Thus, future strategies may incorporate the use of MSCs as delivery vehicles for chondrogenic and angiogenic growth factors.
Traditional rehabilitation training programs focus on the whole body and physiological responses to mechanical loading and/or modalities. In contrast, regenerative medicine pays more attention to molecular, cellular, and histological aspects of tissue regeneration. The integration of the two approaches is a great challenge, but would likely have a synergetic impact on tissue regeneration.
LIMITATIONS IN THE APPLICATION OF MSCS TO REGENERATIVE REHABILITATION
The aging process has been shown to alter the immune system, as well as the functionality of stem cells25). The proliferative activity of MSCs significantly decreases during the aging process, which limits their potential for differentiation62). New results have indicated that age-related changes in MSCs should be taken into account whenever these cells are considered for therapy (Fig. 1). Although MSCs from older volunteers had the ability to form colonies, MSCs obtained from young donors formed a larger number of colonies with more cells63). These studies confirmed previous findings in the literature on the impact of aging on the differentiation and therapeutic potential of MSCs.
Tumorigenesis is one of the big obstacles in MSC therapy (Fig. 1). The effect of MSC therapy on the growth or metastasis of existing tumors has not yet been clarified. It is possible that a small number of stem cells may escape and expand in the graft site and form a tumor64). As discussed by Reya et al.65), there is a relationship between stem cells and tumor cells, and normal stem cells could be the targets of transforming mutations. These results were confirmed by Miura et al.66). Their research was focused on investigating murine bone marrow-derived MSCs and their ability to become spontaneously transformed with accumulated chromosomal abnormalities (Fig. 1), i.e., structural and numerical aberrations during passage, to form fibrosarcoma in vivo. The process of transformation was clearly documented, leading to the first report on tumorigenesis of murine bone marrow-derived MSCs. Although the authors did not observe spontaneous immortalization during studies on the same type of stem cells derived from humans, this can be explained by the far more complicated mechanisms that keep human cells more stable.
In another study, Rosland et al.67) demonstrated spontaneous malignant transformation of human MSCs. The procedure for expanding cell lines was carried out independently in two laboratories, showing rates of transformation of 40% and 50%. After malignant transformation, the level of telomerase significantly increased, which is common for human MSCs68,69,70). In summary, the induction of cancer by transplantation and mutational transformation of MSCs cannot yet be excluded71).
Additional aspects related to the practicality of MSC application are their handling and commercialization, which makes it difficult to industrial these processes. It is very important to ensure pure cell lines, not cross-contaminated ones, before MSC therapies can be commercialized. Torsvik et al.72) clearly showed, after facing many problems they did not expect, such as cross-contamination, that all cell lines should be verified by DNA fingerprinting and the use of electronic databases of authenticated DNA profiles. Furthermore, scientific journals, as well as funders of grant proposals, should require such verification of cell lines used in experiments.
In conclusion, to fully and reliably investigate the therapeutic potential of MSCs, it is crucial to use proper equipment and establish efficient and reproducible processes of isolation, cultivation, and differentiation, so as to obtain a homogenous MSC population for use in clinical applications (Fig. 1). This is one of the biggest challenges for achieving greater successes in this field73).
Acknowledgments
This study was supported by the Serbian Ministry of Science (Grants 175061 and 175092). The authors would like to thank Ms. Sibela Eminovic for English proofreading.
REFERENCES
- 1.Volarevic V, Nurkovic J, Arsenijevic N, et al. : Concise review: therapeutic potential of mesenchymal stem cells for the treatment of acute liver failure and cirrhosis. Stem Cells, 2014, 32: 2818–2823. [DOI] [PubMed] [Google Scholar]
- 2.Syková E, Homola A, Mazanec R, et al. : Autologous bone marrow transplantation in patients with subacute and chronic spinal cord injury. Cell Transplant, 2006, 15: 675–687. [DOI] [PubMed] [Google Scholar]
- 3.Geffner LF, Santacruz P, Izurieta M, et al. : Administration of autologous bone marrow stem cells into spinal cord injury patients via multiple routes is safe and improves their quality of life: comprehensive case studies. Cell Transplant, 2008, 17: 1277–1293. [DOI] [PubMed] [Google Scholar]
- 4.Horwitz EM, Gordon PL, Koo WK, et al. : Isolated allogeneic bone marrow-derived mesenchymal cells engraft and stimulate growth in children with osteogenesis imperfecta: implications for cell therapy of bone. Proc Natl Acad Sci USA, 2002, 99: 8932–8937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Coppi P: Regenerative medicine for congenital malformations. J Pediatr Surg, 2013, 48: 273–280. [DOI] [PubMed] [Google Scholar]
- 6.Atala A, Bauer SB, Soker S, et al. : Tissue-engineered autologous bladders for patients needing cystoplasty. Lancet, 2006, 367: 1241–1246. [DOI] [PubMed] [Google Scholar]
- 7.Schächinger V, Erbs S, Elsässer A, et al. REPAIR-AMI Investigators: Intracoronary bone marrow-derived progenitor cells in acute myocardial infarction. N Engl J Med, 2006, 355: 1210–1221. [DOI] [PubMed] [Google Scholar]
- 8.Binder S, Stanzel BV, Krebs I, et al. : Transplantation of the RPE in AMD. Prog Retin Eye Res, 2007, 26: 516–554. [DOI] [PubMed] [Google Scholar]
- 9.Yaniz-Galende E, Chen J, Chemaly E, et al. : Stem cell factor gene transfer promotes cardiac repair after myocardial infarction via in situ recruitment and expansion of c-kit+ cells. Circ Res, 2012, 111: 1434–1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Christie JD, Edwards LB, Kucheryavaya AY, et al. International Society of Heart and Lung Transplantation: The registry of the International Society for Heart and Lung Transplantation: 29th adult lung and heart-lung transplant report-2012. J Heart Lung Transplant, 2012, 31: 1073–1086. [DOI] [PubMed] [Google Scholar]
- 11.Bainbridge JW, Smith AJ, Barker SS, et al. : Effect of gene therapy on visual function in Leber’s congenital amaurosis. N Engl J Med, 2008, 358: 2231–2239. [DOI] [PubMed] [Google Scholar]
- 12.Hatzistergos KE, Quevedo H, Oskouei BN, et al. : Bone marrow mesenchymal stem cells stimulate cardiac stem cell proliferation and differentiation. Circ Res, 2010, 107: 913–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Oberpenning F, Meng J, Yoo JJ, et al. : De novo reconstitution of a functional mammalian urinary bladder by tissue engineering. Nat Biotechnol, 1999, 17: 149–155. [DOI] [PubMed] [Google Scholar]
- 14.Poss KD, Wilson LG, Keating MT: Heart regeneration in zebrafish. Science, 2002, 298: 2188–2190. [DOI] [PubMed] [Google Scholar]
- 15.Porrello ER, Mahmoud AI, Simpson E, et al. : Transient regenerative potential of the neonatal mouse heart. Science, 2011, 331: 1078–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kajstura J, Rota M, Cappetta D, et al. : Cardiomyogenesis in the aging and failing human heart. Circulation, 2012, 126: 1869–1881. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 17.Nurkovic J, Dolicanin Z, Tutic I, et al. : Adipose tissue mesenchymal stem cells—isolation, cultivation and induced differentiation. Prax Med, 2013, 42: 45–50. [Google Scholar]
- 18.Volarevic V, Bojic S, Nurkovic J, et al. : Stem cells as new agents for the treatment of infertility: current and future perspectives and challenges. Biomed Res Int, 2014, 2014: 507234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ohlstein B, Kai T, Decotto E, et al. : The stem cell niche: theme and variations. Curr Opin Cell Biol, 2004, 16: 693–699. [DOI] [PubMed] [Google Scholar]
- 20.Schroeder IS: Stem cells: are we ready for therapy? Methods Mol Biol, 2014, 1213: 3–21. [DOI] [PubMed] [Google Scholar]
- 21.Larijani B, Esfahani EN, Amini P, et al. : Stem cell therapy in treatment of different diseases. Acta Med Iran, 2012, 50: 79–96. [PubMed] [Google Scholar]
- 22.Simovic Markovic B, Nikolic A, Gazdic M, et al. : Pharmacological inhibition of Gal-3 in mesenchymal stem cells enhances their capacity to promote alternative activation of macrophages in dextran sulphate sodium-induced colitis. Stem Cells Int, 2016, 2016: 2640746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Senarath-Yapa K, McArdle A, Renda A, et al. : Adipose-derived stem cells: a review of signaling networks governing cell fate and regenerative potential in the context of craniofacial and long bone skeletal repair. Int J Mol Sci, 2014, 15: 9314–9330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim EH, Heo CY: Current applications of adipose-derived stem cells and their future perspectives. World J Stem Cells, 2014, 6: 65–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nurkovic J, Volarevic V, Lako M, et al. : Aging of stem and progenitor cells: mechanisms, impact on the therapeutic potential and rejuvenation. Rejuvenation Res, 2016, 19: 3–12. [DOI] [PubMed] [Google Scholar]
- 26.American Physical Therapy Association: Regenerative rehabilitation. http://www.apta.org/ RegenerativeRehab/. (Accessed May 1, 2014)
- 27.Zheng XX, Sanchez-Fueyo A, Domenig C, et al. : The balance of deletion and regulation in allograft tolerance. Immunol Rev, 2003, 196: 75–84. [DOI] [PubMed] [Google Scholar]
- 28.Scandling JD, Busque S, Dejbakhsh-Jones S, et al. : Tolerance and chimerism after renal and hematopoietic-cell transplantation. N Engl J Med, 2008, 358: 362–368. [DOI] [PubMed] [Google Scholar]
- 29.Huard J, Li Y, Fu FH: Muscle injuries and repair: current trends in research. J Bone Joint Surg Am, 2002, 84-A: 822–832. [PubMed] [Google Scholar]
- 30.Prisk V, Huard J: Muscle injuries and repair: the role of prostaglandins and inflammation. Histol Histopathol, 2003, 18: 1243–1256. [DOI] [PubMed] [Google Scholar]
- 31.Schmid P, Itin P, Cherry G, et al. : Enhanced expression of transforming growth factor-beta type I and type II receptors in wound granulation tissue and hypertrophic scar. Am J Pathol, 1998, 152: 485–493. [PMC free article] [PubMed] [Google Scholar]
- 32.Li Y, Huard J: Differentiation of muscle-derived cells into myofibroblasts in injured skeletal muscle. Am J Pathol, 2002, 161: 895–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chan YS, Li Y, Foster W, et al. : The use of suramin, an antifibrotic agent, to improve muscle recovery after strain injury. Am J Sports Med, 2005, 33: 43–51. [DOI] [PubMed] [Google Scholar]
- 34.Fukushima K, Badlani N, Usas A, et al. : The use of an antifibrosis agent to improve muscle recovery after laceration. Am J Sports Med, 2001, 29: 394–402. [DOI] [PubMed] [Google Scholar]
- 35.Chan YS, Li Y, Foster W, et al. : Antifibrotic effects of suramin in injured skeletal muscle after laceration. J Appl Physiol 1985, 2003, 95: 771–780. [DOI] [PubMed] [Google Scholar]
- 36.Hawke TJ, Garry DJ: Myogenic satellite cells: physiology to molecular biology. J Appl Physiol 1985, 2001, 91: 534–551. [DOI] [PubMed] [Google Scholar]
- 37.Fisher BD, Rathgaber M: An overview of muscle regeneration following acute injury. J Phys Ther Sci, 2006, 18: 57–66. [Google Scholar]
- 38.Sato K, Saida K, Yanagawa T, et al. : Differential responses of myogenic C2C12 cells to hypoxia between growth and muscle-induction phases: growth, differentiation and motility. J Phys Ther Sci, 2011, 23: 161–169. [Google Scholar]
- 39.Brack AS, Conboy MJ, Roy S, et al. : Increased Wnt signaling during aging alters muscle stem cell fate and increases fibrosis. Science, 2007, 317: 807–810. [DOI] [PubMed] [Google Scholar]
- 40.Carlson ME, Conboy IM: Loss of stem cell regenerative capacity within aged niches. Aging Cell, 2007, 6: 371–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ambrosio F, Ferrari RJ, Distefano G, et al. : The synergistic effect of treadmill running on stem-cell transplantation to heal injured skeletal muscle. Tissue Eng Part A, 2010, 16: 839–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dreyer HC, Blanco CE, Sattler FR, et al. : Satellite cell numbers in young and older men 24 hours after eccentric exercise. Muscle Nerve, 2006, 33: 242–253. [DOI] [PubMed] [Google Scholar]
- 43.McBride TA, Gorin FA, Carlsen RC: Prolonged recovery and reduced adaptation in aged rat muscle following eccentric exercise. Mech Ageing Dev, 1995, 83: 185–200. [DOI] [PubMed] [Google Scholar]
- 44.Jubrias SA, Esselman PC, Price LB, et al. : Large energetic adaptations of elderly muscle to resistance and endurance training. J Appl Physiol 1985, 2001, 90: 1663–1670. [DOI] [PubMed] [Google Scholar]
- 45.Tanaka S, Miyata T, Fujita T, et al. : Differing responses of satellite cell activity to exercise training in rat skeletal muscle. J Phys Ther Sci, 2009, 21: 141–145. [Google Scholar]
- 46.Tanaka S, Kawahara E, Nakagawa T: Myogenic cell response to muscle contraction with short electrical stimulation. J Phys Ther Sci, 2015, 27: 2349–2352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kondziolka D, Wechsler L, Goldstein S, et al. : Transplantation of cultured human neuronal cells for patients with stroke. Neurology, 2000, 55: 565–569. [DOI] [PubMed] [Google Scholar]
- 48.Kondziolka D, Steinberg GK, Wechsler L, et al. : Neurotransplantation for patients with subcortical motor stroke: a phase 2 randomized trial. J Neurosurg, 2005, 103: 38–45. [DOI] [PubMed] [Google Scholar]
- 49.Nelson PT, Kondziolka D, Wechsler L, et al. : Clonal human (hNT) neuron grafts for stroke therapy: neuropathology in a patient 27 months after implantation. Am J Pathol, 2002, 160: 1201–1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lee JS, Hong JM, Moon GJ, et al. STARTING Collaborators: A long-term follow-up study of intravenous autologous mesenchymal stem cell transplantation in patients with ischemic stroke. Stem Cells, 2010, 28: 1099–1106. [DOI] [PubMed] [Google Scholar]
- 51.Bhasin A, Srivastava MV, Kumaran SS, et al. : Autologous mesenchymal stem cells in chronic stroke. Cerebrovasc Dis Extra, 2011, 1: 93–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Honmou O, Houkin K, Matsunaga T, et al. : Intravenous administration of auto serum-expanded autologous mesenchymal stem cells in stroke. Brain, 2011, 134: 1790–1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Park K, Lee S, Hong Y, et al. : Therapeutic physical exercise in neural injury: friend or foe? J Phys Ther Sci, 2015, 27: 3933–3935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Guo ZY, Sun X, Xu XL, et al. : Human umbilical cord mesenchymal stem cells promote peripheral nerve repair via paracrine mechanisms. Neural Regen Res, 2015, 10: 651–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang P, Zhang Y, Zhao J, et al. : Intramuscular injection of bone marrow mesenchymal stem cells with small gap neurorrhaphy for peripheral nerve repair. Neurosci Lett, 2015, 585: 119–125. [DOI] [PubMed] [Google Scholar]
- 56.Seyed Foroutan K, Khodarahmi A, Alavi H, et al. : Bone marrow mesenchymal stem cell and vein conduit on sciatic nerve repair in rats. Trauma Mon, 2015, 20: e23325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Salomone R, Bento RF, Costa HJ, et al. : Bone marrow stem cells in facial nerve regeneration from isolated stumps. Muscle Nerve, 2013, 48: 423–429. [DOI] [PubMed] [Google Scholar]
- 58.Lasso JM, Pérez Cano R, Castro Y, et al. : Xenotransplantation of human adipose-derived stem cells in the regeneration of a rabbit peripheral nerve. J Plast Reconstr Aesthet Surg, 2015, 68: e189–e197. [DOI] [PubMed] [Google Scholar]
- 59.Wei X, Yang X, Han ZP, et al. : Mesenchymal stem cells: a new trend for cell therapy. Acta Pharmacol Sin, 2013, 34: 747–754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Johnson K, Zhu S, Tremblay MS, et al. : A stem cell-based approach to cartilage repair. Science, 2012, 336: 717–721. [DOI] [PubMed] [Google Scholar]
- 61.Cao L, Yang F, Liu G, et al. : The promotion of cartilage defect repair using adenovirus mediated Sox9 gene transfer of rabbit bone marrow mesenchymal stem cells. Biomaterials, 2011, 32: 3910–3920. [DOI] [PubMed] [Google Scholar]
- 62.Hwang ES: Senescence suppressors: their practical importance in replicative lifespan extension in stem cells. Cell Mol Life Sci, 2014, 71: 4207–4219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Choudhery MS, Badowski M, Muise A, et al. : Donor age negatively impacts adipose tissue-derived mesenchymal stem cell expansion and differentiation. J Transl Med, 2014, 12: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kim SU, de Vellis J: Stem cell-based cell therapy in neurological diseases: a review. J Neurosci Res, 2009, 87: 2183–2200. [DOI] [PubMed] [Google Scholar]
- 65.Reya T, Morrison SJ, Clarke MF, et al. : Stem cells, cancer, and cancer stem cells. Nature, 2001, 414: 105–111. [DOI] [PubMed] [Google Scholar]
- 66.Miura M, Miura Y, Padilla-Nash HM, et al. : Accumulated chromosomal instability in murine bone marrow mesenchymal stem cells leads to malignant transformation. Stem Cells, 2006, 24: 1095–1103. [DOI] [PubMed] [Google Scholar]
- 67.Røsland GV, Svendsen A, Torsvik A, et al. : Long-term cultures of bone marrow-derived human mesenchymal stem cells frequently undergo spontaneous malignant transformation. Cancer Res, 2009, 69: 5331–5339. [DOI] [PubMed] [Google Scholar]
- 68.Parsch D, Fellenberg J, Brümmendorf TH, et al. : Telomere length and telomerase activity during expansion and differentiation of human mesenchymal stem cells and chondrocytes. J Mol Med Berl, 2004, 82: 49–55. [DOI] [PubMed] [Google Scholar]
- 69.Simonsen JL, Rosada C, Serakinci N, et al. : Telomerase expression extends the proliferative life-span and maintains the osteogenic potential of human bone marrow stromal cells. Nat Biotechnol, 2002, 20: 592–596. [DOI] [PubMed] [Google Scholar]
- 70.Zimmermann S, Voss M, Kaiser S, et al. : Lack of telomerase activity in human mesenchymal stem cells. Leukemia, 2003, 17: 1146–1149. [DOI] [PubMed] [Google Scholar]
- 71.Kim WS, Park BS, Sung JH: The wound-healing and antioxidant effects of adipose-derived stem cells. Expert Opin Biol Ther, 2009, 9: 879–887. [DOI] [PubMed] [Google Scholar]
- 72.Torsvik A, Røsland GV, Svendsen A, et al. : Spontaneous malignant transformation of human mesenchymal stem cells reflects cross-contamination: putting the research field on track - letter. Cancer Res, 2010, 70: 6393–6396. [DOI] [PubMed] [Google Scholar]
- 73.Ilic D: Industry highlights: stem cell and regenerative medicine. Regen Med, 2011, 6: 55–60. [DOI] [PubMed] [Google Scholar]