Abstract
Objectives
There is little consensus regarding the burden of pain in the UK. The purpose of this review was to synthesise existing data on the prevalence of various chronic pain phenotypes in order to produce accurate and contemporary national estimates.
Design
Major electronic databases were searched for articles published after 1990, reporting population-based prevalence estimates of chronic pain (pain lasting >3 months), chronic widespread pain, fibromyalgia and chronic neuropathic pain. Pooled prevalence estimates were calculated for chronic pain and chronic widespread pain.
Results
Of the 1737 articles generated through our searches, 19 studies matched our inclusion criteria, presenting data from 139 933 adult residents of the UK. The prevalence of chronic pain, derived from 7 studies, ranged from 35.0% to 51.3% (pooled estimate 43.5%, 95% CIs 38.4% to 48.6%). The prevalence of moderate-severely disabling chronic pain (Von Korff grades III/IV), based on 4 studies, ranged from 10.4% to 14.3%. 12 studies stratified chronic pain prevalence by age group, demonstrating a trend towards increasing prevalence with increasing age from 14.3% in 18–25 years old, to 62% in the over 75 age group, although the prevalence of chronic pain in young people (18–39 years old) may be as high as 30%. Reported prevalence estimates were summarised for chronic widespread pain (pooled estimate 14.2%, 95% CI 12.3% to 16.1%; 5 studies), chronic neuropathic pain (8.2% to 8.9%; 2 studies) and fibromyalgia (5.4%; 1 study). Chronic pain was more common in female than male participants, across all measured phenotypes.
Conclusions
Chronic pain affects between one-third and one-half of the population of the UK, corresponding to just under 28 million adults, based on data from the best available published studies. This figure is likely to increase further in line with an ageing population.
Keywords: PAIN MANAGEMENT, EPIDEMIOLOGY
Strengths and limitations of this study.
Adherence to clearly defined and clinically meaningful inclusion criteria.
Use of a risk of bias tool to exclude studies of low quality.
Use of meta-analysis to quantify the current burden of chronic pain and chronic widespread pain in the UK.
Limited number of high-quality studies.
High level of heterogeneity among included studies.
Introduction
Chronic pain, represented by conditions such as low back pain and osteoarthritis, has recently been highlighted as one of the most prominent causes of disability worldwide by the Global Burden of Disease reviews.1 At the same time, national governments have started to recognise that chronic pain represents a major priority and challenge for their public health and healthcare systems through production of national strategies and convening of Pain Summits in countries including the UK, the USA and Australia.2–5 Such initiatives emphasise the importance of accurate population-based estimates of chronic pain in helping to drive and inform policies of prevention and care, needs assessments, and surveillance of the impact of interventions, as has happened for other long-term conditions such as cancer and cardiovascular disease.
Despite several high profile national reports highlighting the significance of chronic pain in the UK,5–8 there is little consensus regarding the burden of pain in this country. One estimate suggests that up to 8 million people in the UK live with chronic pain,5 in keeping with a telephone survey of residents across Europe in which 13% of the UK population reported pain of moderate-to-severe intensity, lasting for a period of >6 months.9 Estimates based on definitions more closely aligned with that of the International Association of the Study of Pain: ‘pain that persists beyond normal tissue healing time, which is assumed to be 3 months’10 have been considerably higher than those quoted from the European telephone survey.7 11 The purpose of this review was to synthesise existing data on the population prevalence of various chronic pain definitions, in order to produce much needed, accurate and contemporary national estimates.
Methods
A protocol for the review was devised in accordance with the PRISMA guidelines12 and registered on PROSPERO (CRD: 42014012993).13 Searches of MEDLINE (inception to 31 May 2015) and EMBASE (1980 to 31 May 2015) electronic databases were performed (via Ovid) for articles reporting the prevalence of chronic pain in the UK. A list of the medical subject headings and free-text terms used are included under online supplementary appendix A. The results were supplemented by a manual search of the bibliographies of the shortlisted review and original study articles. In addition, a number of field experts were approached in order to identify additional viable studies from the grey literature.
bmjopen-2015-010364supp_appendixA.pdf (36.3KB, pdf)
We included all study formats reporting any point or period prevalence estimates, from a general population sample, for the following: (1) chronic pain: defined as pain in one or more body locations, lasting for a period of 3 months or longer; (2) chronic widespread pain: defined in accordance with the American College of Rheumatology (ACR) 1990 guidelines as pain in the axial skeleton and two contralateral limbs, lasting for a period of 3 months or longer;14 (3) fibromyalgia: defined in relation to either the 1990 or 2010 ACR criteria as ‘widespread’ pain, lasting for a period of 3 months or longer, in association with tender points or somatic symptoms as described in their respective protocols;14 15 and (4) neuropathic pain: defined as pain in one or more body locations, lasting for a period of 3 months or longer, with predominantly neuropathic features. Studies presenting data relating exclusively to specified body regions (eg, chronic pelvic pain only, or chronic lower back pain only) were not included in the review, as they would likely underestimate the prevalence of (non-site-specific) chronic pain. Where case–control studies were identified, they had to be nested within a cohort to allow for calculation of prevalence estimates. Studies based in general practices were included if they used the population registers of the practices as a sampling frame of the general population.
In order to provide contemporaneous and representative estimates, studies were excluded if they (1) presented data collected prior to 1990; (2) presented international prevalence estimates, where data from the UK was not independently retrievable; (3) presented data obtained from UK populations that were not deemed to be representative of the general population (eg, estimates of neuropathic pain in patients with diabetes, or chronic pain prevalence within specific migrant populations) or (4) presented data on a study population that had already been included in the analysis. In the case of follow-up studies, estimates from the baseline studies were preferentially included in the review, unless the follow-up study provided data on additional definitions that were not available from the earlier publication.
Two authors (AF and GTJ) screened all the articles by title, and then by abstract. Shortlisted studies were then analysed in greater depth by reference to the full text for assessment of eligibility. Any disagreements regarding the suitability of individual studies were resolved after appraisal by a third author (PC). Data were extracted independently by at least two authors (AF and GTJ or AF and PC), using a collection tool piloted on a small sample of population studies. AF had not been involved in any previously published pain prevalence studies; articles describing studies to which one of the second reviewers (GTJ or PC) had contributed were allocated to the other reviewer for data extraction and quality appraisal. Data were extracted on population characteristics, response rate (where possible adjusted to reflect the viable survey denominator), crude prevalence estimates (number of cases divided by the sample size), age-adjusted and/or sex-adjusted prevalence estimates and, where provided, estimates stratified by age, by gender or by pain severity. Where age-standardised/sex-standardised data were available, these figures were preferentially used in the meta-analysis. Authors were not contacted directly for missing information.
The articles were all appraised using a risk of bias tool developed specifically for prevalence studies.16 The tool consists of 10 items addressing the external validity (risk of selection and non-response bias), as well as the internal validity (risk of measurement bias, and bias related to the data analysis) of observational studies in order to generate an overall risk of bias assessment. Studies that were deemed to be at ‘high risk of bias’ by both reviewers were removed from the review.
Estimates for the prevalence of chronic pain and chronic widespread pain that were not restricted to age-specific or gender-specific cohorts were incorporated into a meta-analysis. The SEs for prevalence (p) estimates were derived from the equation  , where n=number of participants with completed data in survey. Data were synthesised using StataSE V.13 for Mac. Studies were weighted according to the prevalence effect size and the inverse of the study variance in order to generate an I2 value, serving as a measure of heterogeneity among the studies. A random effects model was used to generate summary prevalence data, displayed (on forest plots) with 95% CIs. Where number of studies and variation in the characteristics was sufficient (calendar year of survey and geographical location), stratified analysis of the survey prevalence figures was presented.
, where n=number of participants with completed data in survey. Data were synthesised using StataSE V.13 for Mac. Studies were weighted according to the prevalence effect size and the inverse of the study variance in order to generate an I2 value, serving as a measure of heterogeneity among the studies. A random effects model was used to generate summary prevalence data, displayed (on forest plots) with 95% CIs. Where number of studies and variation in the characteristics was sufficient (calendar year of survey and geographical location), stratified analysis of the survey prevalence figures was presented.
Results
After removal of duplicates, our initial search generated 1726 studies. From this cohort 87 full-text articles were reviewed for eligibility assessment; a further 11 articles were identified from the additional searches described in the Methods section. Flow charts of the screening and selection processes are included below under online supplementary appendices B and C.
bmjopen-2015-010364supp_appendixB.pdf (139.3KB, pdf)
bmjopen-2015-010364supp_appendixC.pdf (90.4KB, pdf)
Of the 25 papers shortlisted for detailed analysis, 6 were excluded on the basis of high risk of bias. Articles were mainly excluded due to the use of non-standardised definitions of chronic pain phenotypes17 18 (case definition and period prevalence risk) or from surveying populations that were deemed to be unrepresentative of the general population19–22 (study population and sampling frame risk). A breakdown of the risk of bias scoring, for included and excluded articles is presented under online supplementary appendix D.
bmjopen-2015-010364supp_appendixD.pdf (62.9KB, pdf)
In total, 19 articles were included for synthesis in our review: 13 cross-sectional studies, 4 cohort studies and 2 case–control studies nested in population cohorts. Collectively, the articles present prevalence data on 139 933 residents of the UK; baseline characteristics of included studies are presented in table 1. Meta-analysis was possible for two of the study phenotypes, namely chronic pain and chronic widespread pain.
Table 1.
Overview of all studies included in systematic review
| Study | Study design | Sample source | Sample size | Response rate | Male (n) | Age range (mean) | Prevalence estimates included in systematic review |
Method for data retrieval | Risk of bias | Primary aim | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (Corrected)* | CP | CWP | FM | NeP | CPG | Age | |||||||||
| Beasley et al26 | Cross-sectional | 2 GP practices in UK | 14 680† | – | – | – | ♦ | ♦ | Postal questionnaire | Moderate | To see if the distribution of reported pain sites has any association with a number of potential risk markers | ||||
| Macfarlane et al22 | Cohort | GB birth cohort | 12 069 | 78.0% | 49.4% (3918) | 45 | ♦ | Interview and examination | Moderate | To determine to what extent the reporting of pain in adulthood varies by adult socioeconomic status | |||||
| Gale et al34 | Cohort | GB birth cohort | 11 971 | 78.3% | 49.2% (3399) | 45 (45) | ♦ | Questionnaire | Low | To investigate the relationship between intelligence in childhood and risk of CWP in adulthood | |||||
| Smith et al25 | Cross-sectional | UK RCP OCP study | 11 797 | 85.4% | 0% | – | ♦ | ♦ | Postal questionnaire | Moderate | To examine the prevalence and factors associated with CP among women still in the RCoGP OCP Study | ||||
| Croft et al38 | Case Control nested in Cohort | UK RCP OCP study | 11 797 | 85.4% | (0) | (55) | ♦ | Questionnaire | Low | To identify associations between illness episodes and future pain complaints | |||||
| Jones et al33 | Cohort | GB birth cohort | 10 453 | 89.7% | – | 44–46 (45) | ♦ | Postal questionnaire | Low | To examine whether children with common symptoms experience an increased risk of CWP as adults | |||||
| Torrance et al29 | Cross-sectional | 10 GP practices, 5 locations across England and Scotland | 10 000 | 44.5% (47.0%) | 42.9% (1846) | >18 (53) | ♦ | ♦ | ♦ | ♦ | Postal questionnaire | Moderate | To estimate the proportion of NeP in the population, that is, ‘refractory’ | ||
| Bridges7 | Cross-sectional | Postcodes across England | 8599† | (66.0%) | 44.4% (3817) | 16–100 | ♦ | ♦ | ♦ | Interview | Moderate | ||||
| Vandenkerkhof et al23 | Case–control nested in cohort | UK Birth cohort (England, Scotland and Wales) | 8572† | – | – | 45 (45) | ♦ | ♦ | Postal questionnaire | Moderate | To examine the relationship between diet and lifestyle, and CWP | ||||
| Torrance et al30 | Cross-sectional | 6 GP practices (Grampian, Leeds, London) | 6000 | 50.0% (52.4%) | 44.4% (1333) | 18–96 (50) | ♦ | ♦ | ♦ | Postal questionnaire | Moderate | To improve the understanding of chronic pain with neuropathic features using epidemiological research | |||
| Elliott et al11 | Cross-sectional | 29 GP practices across Grampian, Scotland | 5036 | 71.6% (82.3%) | 48.3% (1741) | >25 | ♦ | ♦ | Postal questionnaire | Low | To quantify and describe the prevalence and distribution of CP in the community | ||||
| Smith et al*35 | Cross-sectional | 29 GP practices across Grampian, Scotland | 4611 | 78.2% (82.3%) | 48.3% | >25 | ♦ | Postal questionnaire | Moderate | To describe the prevalence and distribution in the community of CP defined as ‘significant’ and ‘severe’ | |||||
| Jones et al41 | Cross-sectional | Grampian NHS register | 4600 | 34.9% (36.3%) | 45.0% | >25 (55) | ♦ | Postal questionnaire | Moderate | To determine the population prevalence of FM | |||||
| Aggarwal et al39 | Cross-sectional | 1 GP practice in Manchester | 4200 | 59.6% (72.0%) | 45% (1035) | 18–75 (Mdn=48) | ♦ | Postal questionnaire | Moderate | To investigate the co-occurrence, in the general population, of syndromes that are frequently unexplained | |||||
| Parsons et al28 | Cross-sectional | 16 GP practices across SE England | 4171 | 60% (62.0%) | 44.0% (1073) | 18–102 (52) | ♦ | ♦ | ♦ | Postal questionnaire | Moderate | To measure the prevalence and troublesomeness of musculoskeletal pain in different body locations and age groups | |||
| Macfarlane et al40 | Cross-sectional | 3 GP practices across NW England | 3950 | 69.9% (80.3%) | 41.1% (1020) | 25–65 (Mdn=54) | ♦ | Postal questionnaire | Moderate | To determine whether the report of pain is influenced by meteorological conditions | |||||
| Macfarlane et al32 | Cross-sectional | 1 GP practice in Manchester | 3004 | 65.0% (75.0%) | 42.8% (835) | 18–65 | ♦ | ♦ | Postal questionnaire | Moderate | To determine whether psychological symptoms and mental disorder are an intrinsic part of the CWP syndrome | ||||
| Mallen et al24 | Cross-sectional | 3 GP practices in North Staffordshire | 2389 | 35.9% (37.0%) | – | 18–25 | ♦ | ♦ | ♦ | Postal questionnaire | Moderate | To establish the prevalence of severely disabling CP in young adults | |||
| Croft et al27 | Cross-sectional | 2 GP practices in Cheshire | 2034 | 66% (75.0%) | 43.0% (572) | 20–85 (Mdn=46) | ♦ | ♦ | ♦ | Postal questionnaire | Moderate | To establish the prevalence of CWP and associated symptoms in a general population sample | |||
*Population sample is a duplicate from Elliot et al;11 therefore, only age-stratified prevalence estimates have been included. Response rates were adjusted to reflect the viable survey denominator.
†n=population responded (denominator not stated).
CP, chronic pain; CPG, chronic pain grade; CWP, chronic widespread pain; FM, fibromyalgia; GP, general practitioner; Mdn, median; n, number; NeP, neuropathic pain; NHS, National Health Service.
Chronic pain
Ten studies presented prevalence data for chronic pain, two of which were from age-restricted cohorts and are therefore excluded from our national synthesis; a UK (England, Scotland and Wales) birth cohort of residents aged 45 years,23 and a survey of 18–25 years old from the North Staffordshire region.24 One study drew participants from a cohort of women previously enrolled in a national study looking at the long-term effects of the contraceptive pill,25 and therefore did not present any pain prevalence data for males. The remaining seven articles reported data on general population samples from various regions across the UK;7 11 26–30 male participants comprised between 41.4% and 49.5% of the survey respondents. Reported prevalence of chronic pain in the UK ranged from 35.0% to 51.3% (table 2; pooled estimate 43.5%, 95% CI 38.4% to 48.5%). A forest plot of the studies included in the meta-analysis, arranged by date order, is presented in figure 1 demonstrating marked variability among the estimates (I2 98.9%, p=0.00). Where gender-specific data were provided, the prevalence was consistently higher in female participants (37.0% to 51.8%) than in male participants (31.0% to 48.9%).
Table 2.
Studies reporting estimates for chronic pain prevalence
| Study | Pain definition | Sample size (response) | Male (n) | Age range (mean) | Prevalence total (95% CI) (n) | Prevalence in males (95% CI) | Prevalence in females (95% CI) |
|---|---|---|---|---|---|---|---|
| Studies excluded from meta-analysis | |||||||
| Smith et al25 | Aches or pains in previous 1/12, lasting >3/12 | 11 797 (85.4%) | 0% | – | – | – | 38.40% |
| Mallen et al24 | Cross-sectional | 2389 (37.0%) | – | 18–25 | 14.3% (119) | ||
| Vandenkerkhof et al23 | Aches or pains in previous 1/12, lasting >3/12 | 8572* | – | 45 (45) | 53.3% (4573) | – | – |
| Studies reporting data from 1990 to 2000 | |||||||
| Croft et al27 | Pain in previous 1/12, lasting >3/12 | 2034 (75.0%) | 43.0% (572) | 20-85 (Mdn=46) | 35.0% | – | – |
| Elliott et al11 | Current pain or discomfort, present for >3/12 | 5036 (82.3%) | 48.3% (1741) | >25 | 46.4† (1817) | 48.9% (37.0% to 61.4%) | 51.8% (41.8% to 61.0%) |
| Studies reporting data from 2001 to 2009 | |||||||
| Torrance et al30 | Current pain or discomfort, present for >3/12 | 6000 (52.4%) | 44.4% (1333) | 18–96 (50) | 48.0% (1420) | – | – |
| Parsons et al28 | Current pain, present for >3/12 | 4171 (62.0%) | 44.0% (1073) | 18–102 (52) | 39.5%‡ (966) | 37.2%‡ | 41.3%‡ |
| Studies reporting data from 2010 to 2015 | |||||||
| Beasley et al26 | Pain lasting >3/12 | – | – | 51.3% (7536) | – | – | |
| Torrance et al29 | Currently troubled by pain or discomfort, present for >3/12 | 10 000 (47.0%) | 42.9% (1846) | >18 (53) | 46.6† (2202) | 45.0%§ | 47.9%§ |
| Bridges7 | Current pain, present for >3/12 | 8599 (66.0%) | 44.4% (3817) | 16–100 | 37.2% (3202) | 31.0% | 37.0% |
*n=population responded (denominator not stated).
†Age-adjusted/gender-adjusted estimate. Three gender estimates were calculated from a smaller data set of 4306 participants.
‡Presented figures have been derived from tabulated data presented in article.
§Gender estimates were calculated from a smaller data set of 4306 participants.
Mdn, median; n, number.
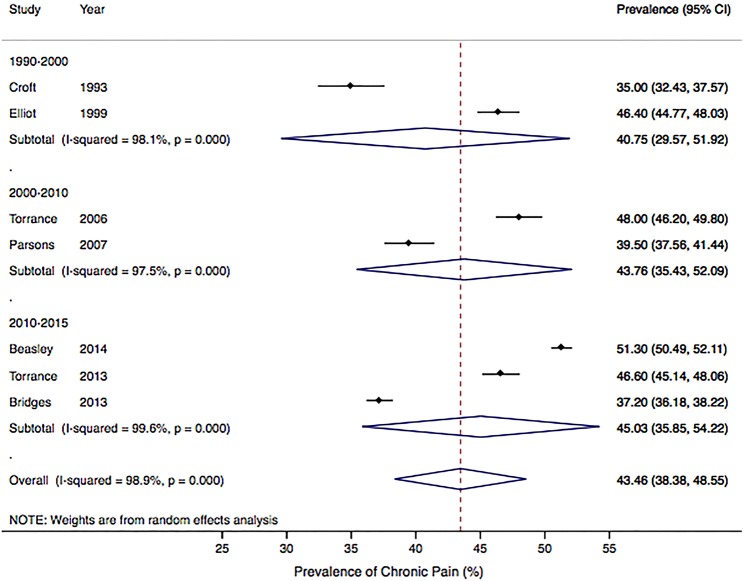
Figure 1.
Pooled estimates for chronic pain prevalence by date of publication.
Exploration of heterogeneity
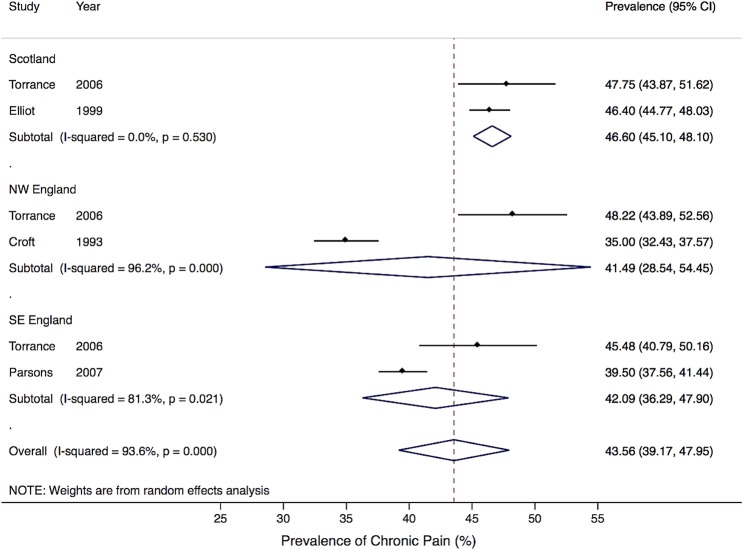
Potential sources of heterogeneity were explored using stratified analysis of the included studies. The gender and age distributions did not really vary enough among the studies to justify different categories; nor was there significant variability in survey methodology. However, pooling of estimates according to publication date suggests an increase in chronic pain prevalence over time: 40.8% (95% CI 29.8% to 51.9%) across studies published between 1990 and 2000; 43.8% (95% CI 35.4% to 52.1%) from studies published between 2000 and 2010; increasing to 45.0% (95% CI 35.8% to 54.2%) from studies published after 2010 (figure 1). Differences were also apparent with geography: three studies included in the chronic pain meta-analysis presented data from distinct geographical locations: Scotland (Grampian),11 SE England27 and NW England (Cheshire);28 one additional study presented stratified estimates for the same areas.30 There was some evidence of geographical variation ranging from 41.5% (95% CI 28.5% to 54.5%) in NW England to 46.6% (95% CI 45.1% to 48.1%) in Scotland (figure 2), although there are too few studies to draw any firm conclusions.
Figure 2.
Pooled estimates for chronic pain prevalence by geographical region.
Chronic pain prevalence by age
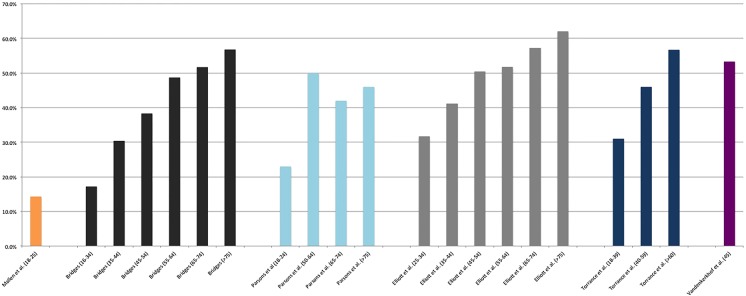
Twelve studies presented data stratified by age groups: chronic pain in seven studies,7 11 23–25 28 29 chronic widespread pain in six studies23 27 31–34 and neuropathic pain in one study.29 Age strata did not overlap precisely across the studies, making synthesis of the data impractical. Within studies, chronic pain prevalence increased steadily with age from a low of 14.3% in 18–25 years old24 to as high as 62% in the over 75 age group.11 A single exception to this trend was observed in one instance where reported pain prevalence among 50–64 years old was higher than that reported in the older age strata.28 Two of the five articles presenting data in the youngest age strata (18–39 years old) reported prevalence estimates >30%.11 29 The data for chronic pain have been tabulated in figure 3. Similar patterns of increasing prevalence with age were demonstrated in studies looking at chronic widespread pain and neuropathic pain, with one single exception where the prevalence of chronic widespread pain in 65–74 years old was lower than the prevalence in the 55–64-year-old bracket; stratification by gender in this study demonstrates that this drop is due to reduced pain reporting by male participants in the 65–74-year-old age bracket.27 The prevalence of chronic widespread pain ranged from 6.8% in 18–32 years old32 to a peak of 21% in the over 75 age group.27 Neuropathic pain prevalence by age was reported in a single study demonstrating increasing pain prevalence: 6.3%, 9.7% and 10.4% in 18–39, 40–59 and over 60 years old, respectively.
Figure 3.
Chronic pain prevalence by age strata.
Chronic pain severity
Four articles presented data on chronic pain prevalence in which estimates were stratified according to pain severity,7 28 29 35 using the ‘grading severity of chronic pain’ tool developed by Von Korff et al,36 and validated for use in chronic pain research.37 The data have been reproduced in table 3; the national prevalence of moderately limiting, high disability pain (grade III) ranged from 4.7% to 6.5%, and that of highly limiting, high disability pain (grade IV) from 5.7% to 7.8% of the total population. Combining these two groups, between 10.4% and 14.3% of the population of the UK report severely disabling chronic pain that is either moderately or severely limiting (Von Korff grades III and IV). One article presented data on chronic neuropathic pain severity estimating 1.8% and 2.6% of the population experience grades III and IV chronic neuropathic pain, respectively.29
Table 3.
Studies reporting prevalence estimates for moderate or severe chronic pain
| Study | Pain measure | CPGS grade III (%) | CPGS grade III by gender | CPGS grade IV (95% CI) | CPGS grade IV by gender (95% CI) |
|---|---|---|---|---|---|
| Smith et al35 | Chronic pain | – | – | 6.3% (5.9% to 6.7%) 5.7% (4.9% to 6.5%)* |
M=5.7% (4.6% to 6.8%) F=6.9% (5.7% to 8.1%) |
| Torrance et al29 | Chronic pain | 6.2 | – | 6.0% | – |
| Parsons et al28 | Chronic pain | 6.5 | – | 7.8% | – |
| Bridges7† | Chronic pain | 4.7 | M=3.9% F=5.2% |
7.2% | M=6.5% F =7.7% |
| Torrance et al29 | Neuropathic pain | 1.8 | – | 2.6% | – |
*Estiamtes adjusted to sampling frame.
†Gender-stratified prevalence estimates from Bridges7 have been retrieved by access to the raw data.CPGS, Chronic Pain Grade Scale; F, Female; M, Male.
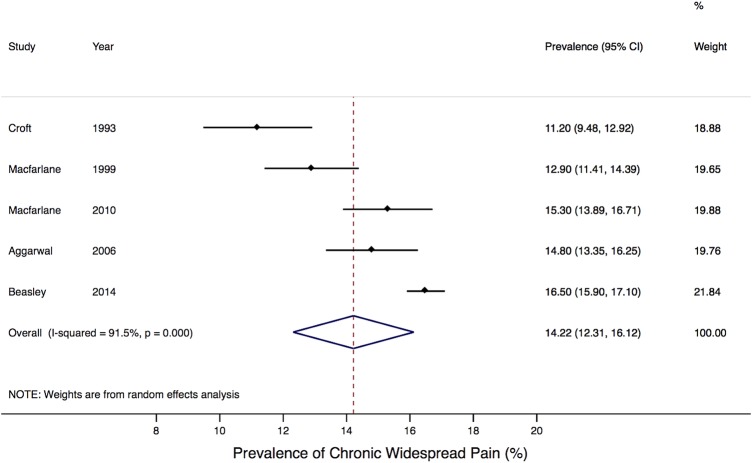
Chronic widespread pain
Ten studies presented prevalence data for chronic widespread pain. Four studies surveying age-restricted birth cohorts of the British population,23 31 33 34 and one study reporting estimates from a gender-restricted cohort38 were excluded from the pooled analysis. The remaining five articles reported data on samples representative of the general population from various regions across the UK.26 27 32 39 40 Prevalence estimates from all 10 studies are reproduced in table 4, and a forest plot demonstrating the variability among study estimates is displayed in figure 4 (I2 91.5%, p=0.00). The reported prevalence of chronic widespread pain ranged from 11.2% to 16.5% (pooled estimate 14.2%, 95% CI 12.3% to 16.1%). Prevalence estimates were again higher in female (12.3% to 17.9%) than in male participants (9.0% to 14.1%).
Table 4.
Studies reporting prevalence estimates for chronic widespread pain
| Study | Pain definition | Sample size | Male (n) | Age range (mean) | Prevalence total (n) | Prevalence in males (%) | Prevalence in females (%) |
|---|---|---|---|---|---|---|---|
| Studies excluded from meta-analysis | |||||||
| Croft et al38 | ACR in the past 1/12 for >3/12 | 11 797 | (0) | (55) | – | – | 12.30 |
| Jones et al33 | ACR in the past 1/12 for >3/12 | 10 453 | – | 44–46 (45) | 12.2% | 11.8 | 12.7 |
| Macfarlane et al22 | ACR in the past 1/12 for >3/12 | 12 069 | 49.4% (3918) | 45 | 11.8% | – | – |
| Vandenkerkhof et al23 | ACR in the past 1/12 for >3/12 | 8572* | – | 45 (45) | 12.3% (1056) | 12.0 | 13.0 |
| Gale et al34 | ACR in the past 1/12 for >3/12 | 11 971 | 49.2% (3399) | 45 (45) | 14.4% (993) | 14.1 | 14.7 |
| Studies included in meta-analysis | |||||||
| Macfarlane et al32 | ACR in the past 1/12 for >3/12 | 3004 | 42.8% (835) | 18–65 | 12.9% (252) | 10.5 | 14.7 |
| Croft et al27 | ACR in the past 1/12 for >3/12 | 2034 | 43.0% (572) | 20–85 (Mdn=46) | 11.2† (164) | 9.40 | 15.60 |
| Aggarwal et al39 | ACR for >3/12 | 4200 | 45% (1035) | 18–75 (Mdn=48) | 14.8% (340) | 9.0 | 17.9 |
| Macfarlane et al40 | ACR in the past 1/12 for >3/12 | 3950 | 41.1% (1020) | 25–65 (Mdn=54) | 15.3% (381) | – | – |
| Beasley et al26 | ACR in the past 1/12 for >3/12 | 14 680* | – | – | 16.5% | – | – |
*n=population responded (denominator not stated).
†Age-adjusted/gender-adjusted estimate.
ACR, American College of Rheumatology; Mdn, median; n, number.
Figure 4.
Pooled estimates for chronic widespread pain prevalence.
Chronic neuropathic pain
Two studies, from the selection presenting data on chronic pain, also screened participants for features predictive of neuropathic pain (defined as a score of 12, or greater, on Leeds Assessment of Neuropathic Symptoms and Signs questionnaire), thereby collectively estimating the prevalence of chronic neuropathic pain among 16 000 residents registered at general practitioner surgeries across England and Scotland: 8.9% and 8.2% in the respective studies.29 30 Estimates for chronic neuropathic pain prevalence were higher in female participants (9.2% to 10.2%) than in males (6.7% to 7.9%).
Fibromyalgia
Owing to the practical restrictions of formally diagnosing a patient with fibromyalgia (requiring a history and examination in order to exclude alternative causes for widespread pain14), only one study41 was able to provide comprehensive data from populations representative of the general population. This study used the modification of the ACR (2010) preliminary diagnostic criteria for fibromyalgia which relies on self-reported pain and somatic symptoms and was developed specifically for epidemiological studies.42 The authors estimated the population prevalence of fibromyalgia to be 5.4% (95% CI 4.7% to 6.1%).41 A small proportion of respondents to the survey (2.4% of the source population) were invited for clinical examinations in order ascertain prevalence rates of fibromyalgia using the conventional diagnostic criteria developed in 1990. These figures were weighted back to the target population in order to generate ‘general population’ estimates, against which the modified research criteria could be compared. However, as the methodology used to generate the latter prevalence estimates was subject to a greater risk of bias, only figures based on the modified criteria, and derived from the source population, have been included in our review.
Discussion
Based on best quality studies of general population samples, the estimated prevalence of chronic pain in the UK is 43%. This equates to just under 28 million people (referencing population statistics from 2013). Chronic pain prevalence rises steadily with increasing age, affecting up to 62% of the population over the age of 75, suggesting that the burden of chronic pain may increase further still, in line with an ageing population, if the incidence remains unaltered. The proportion of patients reporting severe pain was also summarised. Weighted averages for chronic widespread pain suggest that 14.2% of the population may be affected. Between 10.4% and 14.3% of the population report chronic pain that is either moderately or severely limiting (Von Korff grades III and IV), figures that translate into an estimated median of 7.9 million people in the UK population with this category of chronic pain.
The estimate of 43% (28 million people) in the UK with chronic pain is considerably higher than a previously quoted figure of 7.8 million people with ‘chronic pain’5 based on data from the telephone-based pain in Europe survey.9 However, the European survey looked only at moderate-to-severe pain, and figures from that survey are more directly comparable with, and similar to, our summary estimates for moderately or severely limiting chronic pain.
Chronic pain in our review was defined primarily in terms of symptom duration (pain present for a period of 3 months or greater), arguably not reflective of the societal burden of the condition. It may be that a proportion of ‘chronic pain’ reporters are highly functioning individuals with little restriction of day-to-day activity, and limited reliance on health services; many people living with chronic inflammatory or degenerative conditions, in their mildest forms, would fall into this category. However, it is of interest that even in the youngest population age groups, where these conditions are likely to be rare, prevalence estimates for chronic pain are as high as 30% (figure 3), suggesting a greater potential burden on the ‘working’ population than anticipated.
To our knowledge, this is the first study attempting to synthesise prevalence data on chronic pain phenotypes specifically from the UK. In order to strengthen our findings, we have attempted to limit the impact of clinical and methodological heterogeneity by imposing fairly strict selection criteria from the outset of our review, and by remaining selective about the studies that were permitted to enter the meta-analysis. At the expense of sensitivity, our selection criteria generated data comparable enough to allow for synthesis and meta-analysis of the two most prominent pain phenotypes (chronic pain and chronic widespread pain). The tests for statistical heterogeneity among articles included in the meta-analyses still demonstrated substantial variability between studies however (I2 98.9% and 95.2% for chronic pain and chronic widespread pain, respectively). There was limited opportunity to investigate sources of this variability due to the small number of studies included and the lack of recorded characteristics showing variability between studies. A stratified analysis grouped by calendar year of survey suggested this as one potential source of systematic variation between studies, prevalence increasing with time, and one grouping studies by location of study population suggested this as another potential source, but firm conclusions in this regard are limited by the few studies available in which to make robust comparisons, and the marked heterogeneity within the groups. No other stratified analyses by study were possible, but we can speculate that differences in age structure, levels of deprivation and urban/rural differences could also be contributing to differences between study populations, as well as variation in the distribution of known risk factors and confounders. However, without access to individual patient data, and an individual participant data meta-analysis, it is not possible to control fully for these factors.
Another limitation of our review was the quality of the studies available for synthesis. Fewer than half of the 19 included studies were primarily designed to produce prevalence data (table 1), and this was reflected in the variability of reporting of important variables: population denominators and response rates were not always identifiable, in particular where the survey measured multiple outcomes; participant demographics were not always displayed; and there were occasional numerical discrepancies between the data presented in the study abstract, main text and results tables. Six studies were excluded from the review on the grounds of a higher than acceptable risk of bias, three of which provided data that could potentially have been incorporated into our meta-analysis of chronic pain prevalence. We acknowledge that different approaches exist, in terms of whether to, and if so how to, use quality appraisal in systematic literature reviews.43 However, our a priori approach was that quality assessment would be used to select only those studies that met a minimum standard.13
While it is possible that references from the grey literature have been missed, we are reassured that a recent systematic review of all chronic widespread pain surveys44 did not identify any eligible UK papers which had not been included at some stage of out literature search.
Our study indicates how a systematic review of published surveys carried out in one country, with exclusion of studies at high risk of bias, can provide population prevalence estimates for different pain conditions of the sort required by national policy strategies for prevention and care of chronic pain. Despite the high level of heterogeneity between study estimates, the summary figures are comparable with those from international surveys and reviews. For example in the USA, the Institute of Medicine estimated the prevalence of chronic pain in America to be 40%, affecting an estimated 100 million people,3 similar to those of WHO surveys across developed (37%) and developing (41%) countries,45 despite between-country variability, and to the estimate from our review here (43%). Surveys of more severe chronic disabling pain in America,46 Europe9 and elsewhere47 estimate similar prevalence figures to those found here (around 12%). We conclude that our estimates can be used in national and local prevalence calculations of chronic pain prevalence, to inform, for example, planning of community pain services and targets for prevention.
In conclusion, we have used the best available data to demonstrate that chronic pain affects between one-third and one-half of the population of the UK: a figure that is likely to increase further, with time, in line with an ageing population. Such prevalence data does not itself define need for care or targets for prevention, but reliable information on prevalence will help to drive public health and healthcare policymakers' prioritisation of this important cause of distress and disability in the general population. In the interests of improving the quality and reporting of epidemiological data, we would encourage future population studies to adhere to standardised methods for collecting and presenting observational data, such as the guidance produced by the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) group.48
Acknowledgments
The authors are grateful for the input of Professor Blair Smith (University of Dundee): his counsel early in the project, and his advice and comments regarding the search strategy; and Professor Danielle van der Windt (Keele University) for helpful advice and comments.
Footnotes
Contributors: AF was involved with the study design, data collection, analysis and write-up. He is the guarantor. GTJ and PC assisted with the study design, data collection, analysis and revisions. RML and LJD contributed to the design of the study and revisions to the article.
Funding: The British Pain Society provided financial assistance to AF with the costs of this project. PC was partly supported by an Arthritis Research UK Primary Care Centre grant (reference: 18139).
Competing interests: RML reports personal fees from Grunenthal, grants and personal fees from Napp/Mundipharma, personal fees from Pfizer, personal fees from Astrazeneca, personal fees from BioQuiddity, personal fees from The Medicines Co, outside the submitted work.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Vos T, Flaxman AD, Naghavi M et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2163–96. 10.1016/S0140-6736(12)61729-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Department of Health and Human Services USG. National Pain Strategy: a comprehensive population health strategy for pain, 2015. http://iprcc.nih.gov/docs/DraftHHSNationalPainStrategy.pdf (accessed Feb 2016). [DOI] [PubMed]
- 3.Committee on Advancing Pain Research C, and Education; Board on Health Sciences Policy; Institute of Medicine. Relieving pain in America: a blueprint for transforming prevention, care, education and research, 2011. http://www.nap.edu/catalog/13172/relieving-pain-in-america-a-blueprint-for-transforming-prevention-care (accessed Feb 2016).
- 4.The National Pain Strategy, 2010. http://www.painaustralia.org.au/the-national-pain-strategy/national-pain-strategy.html (accessed Feb 2016).
- 5.Donaldson LJ. Pain: breaking through the barrier. 150 years of the Annual Report of the Chief Medical Officer: on the state of the public health. London, 2008. http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/AnnualReports/DH_096206 [Google Scholar]
- 6.Price C. Putting pain on the agenda: the report of the First English Pain Summit. United Kingdom, 2012. https://www.britishpainsociety.org/static/uploads/resources/files/members_articles_putting_pain_agenda.pdf. [Google Scholar]
- 7.Bridges S. Chronic pain. Health Survey for England, 2011. https://catalogueicnhsuk/publications/public-health/surveys/heal-surv-eng-2011/HSE2011-Ch9-Chronic-Painpdf 2012. https://catalogue.ic.nhs.uk/publications/public-health/surveys/heal-surv-eng-2011/HSE2011-Ch9-Chronic-Pain.pdf [Google Scholar]
- 8.National Pain Audit. Final report 2010–2012. http://www.nationalpainaudit.org/media/files/NationalPainAudit-2012.pdf
- 9.Breivik H, Collett B, Ventafridda V et al. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain 2006;10:287–333. 10.1016/j.ejpain.2005.06.009 [DOI] [PubMed] [Google Scholar]
- 10.[No authors listed]. Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl 1986;3:S1–226. [PubMed] [Google Scholar]
- 11.Elliott AM, Smith BH, Penny KI et al. The epidemiology of chronic pain in the community. Lancet 1999;354:1248–52. 10.1016/S0140-6736(99)03057-3 [DOI] [PubMed] [Google Scholar]
- 12.Liberati A, Altman DG, Tetzlaff J et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fayaz A, Croft P, Langford RM et al. The prevalence of chronic pain in the United Kingdom: protocol for systematic review. http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42014012993. PROSPERO International prospective register of systematic reviews, 2014. [Google Scholar]
- 14.Wolfe F, Clauw DJ, Fitzcharles MA et al. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res 2010;62: 600–10. 10.1002/acr.20140 [DOI] [PubMed] [Google Scholar]
- 15.Wolfe F, Smythe HA, Yunus MB et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum 1990;33:160–72. 10.1002/art.1780330203 [DOI] [PubMed] [Google Scholar]
- 16.Hoy D, Brooks P, Woolf A et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol 2012;65:934–9. 10.1016/j.jclinepi.2011.11.014 [DOI] [PubMed] [Google Scholar]
- 17.Gureje O, Von Korff M, Simon GE et al. Persistent pain and well-being: a World Health Organization study in primary care. JAMA 1998;280:147–51. 10.1001/jama.280.2.147 [DOI] [PubMed] [Google Scholar]
- 18.Gajria C, Murray J, Birger R et al. Identification of patients with neuropathic pain using electronic primary care records. Inform Prim Care 2011;19:83–90. [DOI] [PubMed] [Google Scholar]
- 19.Martin KR, Beasley M, Macfarlane GJ et al. Chronic pain predicts reduced physical activity in a large population cohort study. Arthritis Rheumatol 2014;66:S434. [Google Scholar]
- 20.Nicholl BI, Mackay D, Cullen B et al. Chronic multisite pain in major depression and bipolar disorder: cross-sectional study of 149,611 participants in UK Biobank. BMC Psychiatry 2014;14:2433 10.1186/s12888-014-0350-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bowsher D, Rigge M, Sopp L. Prevalence of chronic pain in the British population: a telephone survey of 1037 households. Pain Clinic 1991;4:223–30. [Google Scholar]
- 22.Macfarlane GJ, Pye SR, Finn JD et al. Investigating the determinants of international differences in the prevalence of chronic widespread pain: evidence from the European Male Ageing Study. Ann Rheum Dis 2009;68:690–5. 10.1136/ard.2008.089417 [DOI] [PubMed] [Google Scholar]
- 23.Vandenkerkhof EG, Macdonald HM, Jones GT et al. Diet, lifestyle and chronic widespread pain: results from the 1958 British Birth Cohort Study. Pain Res Manag 2011;16:87–92. 10.1155/2011/727094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mallen C, Peat G, Thomas E et al. Severely disabling chronic pain in young adults: prevalence from a population-based postal survey in North Staffordshire. BMC Musculoskelet Disord 2005;6:42 10.1186/1471-2474-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smith BH, Elliott AM, Hannaford PC. Is chronic pain a distinct diagnosis in primary care? Evidence arising from the Royal College of General Practitioners’ Oral Contraception Study. Fam Pract 2004;21:66–74. [DOI] [PubMed] [Google Scholar]
- 26.Beasley M, Macfarlane GJ. Chronic widespread pain versus multi-site pain: does the distribution matter? Arthritis Rheumatol 2014;66:S908–S09. [Google Scholar]
- 27.Croft P, Rigby AS, Boswell R et al. The prevalence of chronic widespread pain in the general population. J Rheumatol 1993;20:710–13. [PubMed] [Google Scholar]
- 28.Parsons S, Breen A, Foster NE et al. Prevalence and comparative troublesomeness by age of musculoskeletal pain in different body locations. Fam Pract 2007;24:308–16. 10.1093/fampra/cmm027 [DOI] [PubMed] [Google Scholar]
- 29.Torrance N, Ferguson JA, Afolabi E et al. Neuropathic pain in the community: more under-treated than refractory? Pain 2013;154: 690–9. 10.1016/j.pain.2012.12.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Torrance N, Smith BH, Bennett MI et al. The epidemiology of chronic pain of predominantly neuropathic origin. Results from a general population survey. J Pain 2006;7:281–9. [DOI] [PubMed] [Google Scholar]
- 31.Macfarlane GJ, Norrie G, Atherton K et al. The influence of socioeconomic status on the reporting of regional and widespread musculoskeletal pain: results from the 1958 British Birth Cohort Study. Ann Rheum Dis 2009;68:1591–5. 10.1136/ard.2008.093088 [DOI] [PubMed] [Google Scholar]
- 32.Macfarlane GJ, Morris S, Hunt IM et al. Chronic widespread pain in the community: the influence of psychological symptoms and mental disorder on healthcare seeking behavior. J Rheumatol 1999;26: 413–19. [PubMed] [Google Scholar]
- 33.Jones GT, Silman AJ, Power C et al. Are common symptoms in childhood associated with chronic widespread body pain in adulthood? Results from the 1958 British Birth Cohort Study. Arthritis Rheum 2007;56:1669–75. [DOI] [PubMed] [Google Scholar]
- 34.Gale CR, Deary IJ, Cooper C et al. Intelligence in childhood and chronic widespread pain in middle age: the National Child Development Survey. Pain 2012;153:2339–44. 10.1016/j.pain.2012.07.027 [DOI] [PubMed] [Google Scholar]
- 35.Smith BH, Elliott AM, Chambers WA et al. The impact of chronic pain in the community. Fam Pract 2001;18:292–9. 10.1093/fampra/18.3.292 [DOI] [PubMed] [Google Scholar]
- 36.Von Korff M, Ormel J, Keefe FJ et al. Grading the severity of chronic pain. Pain 1992;50:133–49. 10.1016/0304-3959(92)90154-4 [DOI] [PubMed] [Google Scholar]
- 37.Smith BH, Penny KI, Purves AM et al. The Chronic Pain Grade questionnaire: validation and reliability in postal research. Pain 1997;71:141–7. 10.1016/S0304-3959(97)03347-2 [DOI] [PubMed] [Google Scholar]
- 38.Croft P, Lewis M, Hannaford P. Is all chronic pain the same? A 25-year follow-up study. Pain 2003;105:309–17. [DOI] [PubMed] [Google Scholar]
- 39.Aggarwal VR, McBeth J, Zakrzewska JM et al. The epidemiology of chronic syndromes that are frequently unexplained: do they have common associated factors? Int J Epidemiol 2006;35:468–76. 10.1093/ije/dyi265 [DOI] [PubMed] [Google Scholar]
- 40.Macfarlane TV, McBeth J, Jones GT et al. Whether the weather influences pain? Results from the EpiFunD study in North West England. Rheumatology 2010;49:1513–20. [DOI] [PubMed] [Google Scholar]
- 41.Jones GT, Atzeni F, Beasley M et al. The prevalence of fibromyalgia in the general population: a comparison of the American College of Rheumatology 1990, 2010, and modified 2010 classification criteria. Int J Epidemiol 2015;67:568–75. 10.1002/art.38905 [DOI] [PubMed] [Google Scholar]
- 42.Wolfe F, Clauw DJ, Fitzcharles MA et al. Fibromyalgia criteria and severity scales for clinical and epidemiological studies: a modification of the ACR Preliminary Diagnostic Criteria for Fibromyalgia. J Rheumatol 2011;38:1113–22. 10.3899/jrheum.100594 [DOI] [PubMed] [Google Scholar]
- 43.Viswanathan M, Ansari MT, Berkman ND et al. AHRQ methods for effective health care. Assessing the risk of bias of individual studies in systematic reviews of health care interventions. Methods guide for effectiveness and comparative effectiveness reviews. Rockville, MD: Agency for Healthcare Research and Quality (US), 2008. [PubMed] [Google Scholar]
- 44.Mansfield KE, Sim J, Jordan JL et al. A systematic review and meta-analysis of the prevalence of chronic widespread pain in the general population. Pain 2016;157:55–64. 10.1097/j.pain.0000000000000314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tsang A, Von Korff M, Lee S et al. Common chronic pain conditions in developed and developing countries: gender and age differences and comorbidity with depression-anxiety disorders. J Pain 2008;9:883–91. 10.1016/j.jpain.2008.05.005 [DOI] [PubMed] [Google Scholar]
- 46.Nahin RL. Estimates of pain prevalence and severity in adults: United States, 2012. J Pain 2015;16:769–80. 10.1016/j.jpain.2015.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Croft PB, Blyth FM, van der Windt D. Chronic pain epidemiology: from aetiology to public health. Oxford, UK: University Press, 2010. [Google Scholar]
- 48.Vandenbroucke JP, von Elm E, Altman DG et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Epidemiology 2007;18:805–35. 10.1097/EDE.0b013e3181577511 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2015-010364supp_appendixA.pdf (36.3KB, pdf)
bmjopen-2015-010364supp_appendixB.pdf (139.3KB, pdf)
bmjopen-2015-010364supp_appendixC.pdf (90.4KB, pdf)
bmjopen-2015-010364supp_appendixD.pdf (62.9KB, pdf)