Abstract
Objectives
To estimate the population-level cancer estimates for the Lahore district, which is part of the Punjab Cancer Registry (PCR), Pakistan. The average population per year of Lahore was estimated at 9.8 million in 2010–2012.
Design
A cross-sectional study.
Setting
The Registry has 19 collaborating centres in Lahore that report their data to the Central Office located within a tertiary care cancer treatment facility in Lahore, Pakistan.
Participants
Patients belonging to Lahore, of any age-group, and diagnosed with cancer in 2010–2012, were included in the study. They were followed up between July and October 2015 to determine their vital status.
Outcome measures
Summaries were generated for gender, the basis of diagnosis, diagnoses and deaths. The Age-Standardized Incidence Rates (ASIR) were computed per 100 000 population, by gender and cancer site. Five-year age categories were created from 0–4 until 70–74, followed by 75+ years. Death counts were reported by site.
Results
Between 2010 and 2012, in Lahore, a total of 15 840 new cancers were diagnosed in 43% male patients and 57% female patients; 93.5% were microscopically confirmed and 6.5% non-microscopically. In females, the ASIR was 105.1 and in males, it was 66.7. ASIRs of leading cancers among women were breast 47.6, ovary 4.9 and corpus uteri 3.6, whereas among men they were prostate 6.4, bladder 5.0, and trachea, bronchus and lung 4.6. A total of 5134 deaths were recorded.
Conclusions
In Lahore, the ASIR was higher in women than in men. Among women and men, breast cancer and prostate cancer, respectively, were the leading cancer types. These estimates can be used for health promotion and policymaking in the region.
Keywords: PUBLIC HEALTH, EPIDEMIOLOGY, ONCOLOGY
Strengths and limitations of this study.
This is the first time that the age-standardised incidence rates have been presented for the Lahore district.
A comparison has been made with the incidence rates reported by other registries around the world.
There are follow-up issues related to determining the vital status of the patients, once they are registered as new patients with cancer. Therefore, the limitation of the study is that the vital status of the vast majority of patients could not be determined.
Introduction
In the area of public health research, conducting high-quality population-level studies is hailed as the gold standard, as the outcomes truly represent the disease status of the community on which the studies are being conducted. This includes the practice of population-based cancer registration, which assists in providing statistics and trends on incidence, mortality and survival, as well as information on putative risk factors associated with various diseases within a defined population living in a geographically demarcated area, over a specified period of time. However, cancer registration can only be undertaken if there is appropriate infrastructure to enable it and suitable, well-trained staff to perform the tasks associated with it. Understandably, there is a cost associated with conducting this type of epidemiological work, and in a resource-constrained country like Pakistan, governments are less likely to focus on the area of cancer registration than other areas deemed more immediately critical. Further, there is no legislation in the country that requires healthcare practitioners to report diagnoses of cancer. Moreover, the healthcare delivery in Pakistan is quite complex and is as depicted in figure 1. A large part of the population is served through a mixed system via multiple health providers.1
Figure 1.
Healthcare delivery systems in Pakistan. Image used with permission from Dr. Sania Nishtar from her book titled ‘Choked Pipes’.
The question whether cancer registration is a necessity or a luxury in developing countries has been debated extensively over the years. A paper published in 2008 stated that in low-income countries, cancer registration is urgently needed so as to gauge the cancer burden in the region.2 Given that Pakistan is categorised as a ‘lower-middle income country’ by the World Bank, with its population estimated to be 185.0 million in the year 2014, and the life expectancy at birth being 66 years (65 years for males and 67 years for females), it seems unlikely that registration of all cancer diagnoses will be accurate and complete at the national level in the near future.3 However, there is no denying the fact that knowing the cancer burden in the region helps in projecting regional cancer trends, establishing the required numbers of healthcare facilities to cater to the needs of the patients, training sufficient numbers of healthcare practitioners to manage the conditions, addressing health education, and assisting in developing prevention, early detection and cancer control programmes in the region. Figure 2 is a map of Pakistan showing the provinces of Pakistan and countries adjacent to Pakistan.4 Even though accurate population figures are not available, enthusiastic professionals have, over the years, endeavoured to determine cancer estimates for Pakistan. In the past, the regional registry of the Karachi South district, in the province of Sindh, was established and managed for several years by a dedicated pathologist, Dr. Bhurgri.5 This registry was widely recognised at an international level for its data quality.5 However, owing to the sudden death of Dr. Bhurgri in January 2012, this registry is no longer active. Another registry in Pakistan is the Punjab Cancer Registry (PCR), which was founded collaboratively by a group of health professionals in 2005, pioneered by the administrators of a complete cancer treatment facility in Lahore called the Shaukat Khanum Memorial Cancer Hospital and Research Center (SKMCH and RC).6–9 The PCR, herein, referred to as the Registry, is registered with, and regulated under, the Societies Registration Act, 1860, of the Government of Pakistan.10 It is also a member of the International Association of Cancer Registries, France.11 Online supplementary appendix A shows the list of collaborating centres of the Registry.
Figure 2.
Map of Pakistan showing the provinces and locations of the Lahore and Karachi districts and neighbouring countries.
bmjopen-2016-011828supp_appendixA.pdf (164.5KB, pdf)
The reporting of cancer cases to population-based cancer registries is not required by law in Pakistan. It is in fact a voluntary task undertaken by professionals representing many institutions of the region. When the Registry was established in 2005, a memorandum outlining the structure and governance mechanisms was signed by the stakeholders representing both the government and private laboratories and hospitals of the city. The purpose of establishing the Registry was to determine the cancer estimates in the province of Punjab. Punjab is the most populous province of Pakistan, with a population estimated at 100 M, with 36 administrative districts, of which Lahore is the most populous, with a population of some 10 M.12 13 For about a decade, data have been captured in a systematic and predefined manner, in accordance with the minimum data items required for cancer registries as well as some additional optional data items.6 9 14
In the past, PCR data have been reported to the International Agency for Research on Cancer (IARC) in response to a call for data by the Agency. The data have been used, along with data from Dr Yasmin Bhurgri's paper and the Federal Bureau of Statistics, Pakistan, to provide cancer estimates for Pakistan in the Globocan 2012 report.15
This manuscript provides population-level cancer estimates for the Lahore district, based on cases diagnosed in 2010–2012 and reported to the Registry. This is the first time that the Lahore district population-level data have been computed and are being reported.
Methods
The population denominator
Population-level statistics cannot be computed without the availability of figures for the population under review or the catchment population. In Pakistan, publications describing the population structure are available for the census that was conducted in 1998.12 However, the most recent population census, initiated a year ago, has not yet been completed;16 therefore, accurate figures describing the Pakistani population are not available. As a result, for this study, population estimates are based on population figures determined by using the average annual growth rates provided by the Government of Pakistan.12
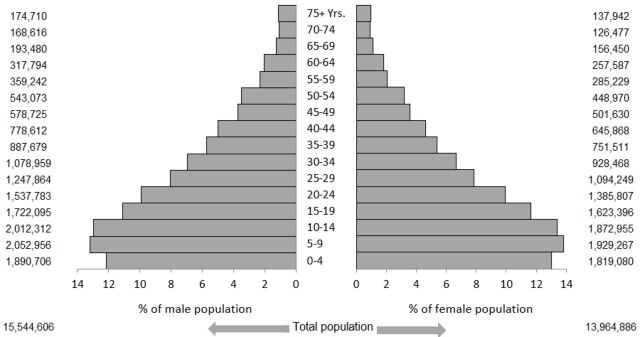
In the years 2010, 2011 and 2012, the population of the Lahore district was estimated at 9 503 871, 9 832 705 and 10 172 916, respectively, computed using an average annual growth rate of 3.46%.12 13 The total area of the Lahore district is 1772 km2, with its average population density being calculated as 5551 persons per square kilometre, in the years under study.12 Figure 3 is a population pyramid showing the combined population distribution of the Lahore district, by age group and gender, for the years 2010–2012. These population estimates were used as the population-at-risk denominator, for calculating the incidence rates for this study.
Figure 3.
Population structure of the Lahore district, 2010–2012, by gender.
Data collection
As routine cancer registration practice, the information is collected on the PCR data collection forms developed collaboratively, following international guidelines on recording cancers (see online supplementary appendix B). The pertinent question on the form states whether a patient is a resident of Lahore or has come to Lahore for diagnosis or treatment only. This has helped to identify the residents of Lahore.
bmjopen-2016-011828supp_appendixB.pdf (194.9KB, pdf)
Each centre is allocated a separate centre identification number. The forms are distributed to, and collected from, each participating centre on a regular basis. Both active and passive methods of data collection are used.14 Registry Staff educate relevant personnel at each centre with regard to data capture and missing information and answer any other queries that arise. At the Cancer Registry and Clinical Data Management unit, only authorised personnel are allowed to enter data from the paper-based forms into the database. The forms collected are stored securely and remain confidential. The information is subsequently entered into the PCR database, developed as part of the computerised Hospital Information System of SKMCH and RC (see online supplementary appendices C-CCC). All authorised Staff members are given specific usernames and passwords to turn the computers on and another username-password to access the system and thence the PCR software. Any form of transmission of the information, including printing and saving it on portable electronic devices, and aspects related to document retention, is strictly regulated by the Governing Council of the Registry and SKMCH and RC, the latter being the sponsor of the Registry. For the cases diagnosed or treated at SKMCH and RC, linkages have been developed with the pathology department and clinics to facilitate data capture.
bmjopen-2016-011828supp_appendixC.pdf (422.6KB, pdf)
For the purpose of recording cancers, the incidence date on the PCR form is defined as the date of cytological/histological confirmation of a malignancy on a pathology report, date of evaluation at an outpatient clinic only or date of clinical investigation(s) as imaging or tumour markers, confirming the diagnosis. A check for multiple primaries is done as per IARC rules.17 In case of duplicate registration identified by checking various combinations of name/age/sex/phone number/address/tumour morphology, the case is registered with the centre where the first diagnosis was made. Edits, for the validity and for the consistency between variables, are also carried out (age/incidence, age/site/histology, site/histology, sex/site, sex/histology, behaviour/site, behaviour/histology, grade/histology and basis of diagnosis/histology). Initially, cancers were coded using the International Classification of Disease for Oncology-Third Edition.18 For this manuscript, cancers were categorised using the International Classification of Diseases, Clinical Modification, 10th revision.19
Data access and follow-up
Release of confidential information is governed by the rules approved by the Registry, and is always without any identifiers.6 For maintaining confidentiality of the information recorded, Staff members are made to sign a confidentiality pledge at the time of employment, which remains in force after cessation of employment with SKMCH and RC. For the purpose of reporting the data to IARC and to determine the vital status, patients diagnosed in the time period 2010–2012 were followed up telephonically between July and October 2015. We were able to establish contact with only 60% of the cases in this way.
Cancers reported
Cancer notifications for the Lahore district have improved with the passage of time, with the cases reported to the Registry going up from 2006 in the year 2005 to 5123 in the year 2015. In chronological order, the numbers reported are as follows: 2006; 2987; 3617; 3990; 5109; 5302; 4949; 5589; 6009; 5943; and 5123. We are still receiving information on cases diagnosed in 2014 and 2015. In recent years, six other districts have been included for the purpose of data collection, with the idea being to include 1–2 contiguous district(s) of Punjab every year in order to expand cancer registration. The data collection form is modified accordingly to ascertain resident status of the patients.6 The approach related to including 1–2 districts on a regular basis has been adopted because the sponsor, SKMCH and RC, is a charitable organisation, and it is logistically not possible to initiate data collection from 36 districts of Punjab simultaneously.
2010–2012 study
A cross-sectional study was conducted and the Punjab Cancer Registry data were reviewed retrospectively to retrieve information on patients with cancer belonging to the Lahore district and having been diagnosed in 2010–2012. Information was collected on new cancer diagnoses (by histology and gender), the most valid basis of diagnosis as microscopically versus non-microscopically confirmed, multiple primaries and deaths recorded. Five-year age categories were created beginning from 0 to 4 years and ending at 70 to 74 years, with all those above 75 included as 75+. Cases were stratified by year of diagnosis/gender/age group and histology/site.
Data analysis
Counts were determined and ASIRs computed according to 5-year age groups, weighted by the Segi World Standard population.20 ASIRs were expressed per 100 000 population per year, separately for male and female patients. For mortality data, counts were stratified by histology/site. Overall survival interval was computed between the dates of diagnosis and last contact and analysed using the Kaplan-Meier method. Of a total of 15 825 patients registered in the years 2010–2012, survival intervals could not be computed for nearly 43% of the cases. Of these, in the vast majority of cases, no contact could be established with the patients on the phone numbers provided; in some of the cases, the attendants of the patients could only communicate that the patients had died but could not recall their dates of death; in a few cases, the patients died on the day of cancer diagnosis and their intervals were set at naught. Although extensive survival analysis was subsequently done on the 57% of cases on which the duration of survival was available, the survival estimates generated were not considered valid. Therefore, the survival results are not being presented in this manuscript.
Data were analysed using Microsoft Excel, V.2010 and SPSS, V.19. The Institutional Review Board (IRB) of the Shaukat Khanum Memorial Cancer Hospital & Research Center granted exemption from full IRB evaluation.
Results
The total population of the Lahore district in 2010–2012 was estimated to be 29 509 492, with males accounting for 52.7% and females 47.3% (figure 3). The number of cases reported in each of the 3 years under study, 2010, 2011 and 2012, along with their population denominators, were: 5302/9 503 871, 4949/9 832 705 and 5589/10 172 916, respectively. A total of 15 840 cancers were diagnosed in 15 825 patients belonging to the district of Lahore and registered against the corresponding years; 9069 (57.3%) were female and 6771 (42.7%) were male patients. Multiple primary cancers, up to two, were identified in 15 patients (table 1), explaining the discrepancy between the number of cases recorded and the patients registered. Nearly 10% were identified as having been registered twice and were eventually assigned to the centre where the first diagnosis was made, thereby being counted just once. The age range of the patients was 0–106 years. Of all the cancers diagnosed, about 93.5% were microscopically confirmed and 6.5% non-microscopically (table 2). None were registered on the basis of death certificates only. Skin cancer had the highest figure in the microscopically confirmed group (99.6%), whereas liver and intrahepatic bile duct(s) had the highest figure in the non-microscopically confirmed category (69.5%). The ASIR for all sites combined among female patients was 105.1/100 000 women and among male patients, it was 66.7/100 000 men per year. Tables 3–6 show the ASIRs for all the cancers recorded in the Registry, by the year of diagnosis and gender, and the age-specific rates for the 5-year age-group, separately for female and male patients. Among females, the highest ASIRs were recorded for the following sites and malignancies: breast 47.6, ovary 4.9, corpus uteri 3.6, Non-Hodgkin lymphoma (NHL) 3.3, cervix uteri 2.9, and brain and CNS 2.2, whereas in men the highest ASIRs were: prostate 6.4, bladder 5.0, trachea, bronchus and lung 4.6, NHL 4.5, brain and CNS 3.8, and liver 3.7.
Table 1.
Details related to patients having multiple primaries in the Lahore district, 2010–2012
| Serial no. | Gender | Age (years) | Vital status | Multiple sites |
|---|---|---|---|---|
| 1. | Male | 20 | Alive | Colon and brain |
| 2. | Male | 23 | Alive | Larynx and testis |
| 3. | Male | 34 | Dead | Kidney and thyroid |
| 4. | Female | 45 | Alive | Breast and breast |
| 5. | Male | 45 | Alive | Ill-defined and lung |
| 6. | Female | 46 | Alive | Breast and ovary |
| 7. | Male | 55 | Alive | Spinal cord and NHL |
| 8. | Male | 56 | Dead | Brain and unknown primary |
| 9. | Female | 59 | Alive | Breast and liver |
| 10. | Female | 60 | Dead | Breast and breast |
| 11. | Male | 62 | Dead | Rectum and bone |
| 12. | Female | 64 | Alive | Breast and breast |
| 13. | Male | 67 | Dead | Thyroid and stomach |
| 14. | Male | 70 | Dead | Connective tissue and liver |
| 15. | Female | 91 | Dead | Breast and ovary |
NHL, Non-Hodgkin lymphoma.
Table 2.
The basis of diagnosis, categorised as being microscopically and non-microscopically confirmed, 2010–2012, in the Lahore district (N=15 840)
| Basis of diagnosis |
||
|---|---|---|
| Cancer site | Microscopic (per cent) | Non-microscopic (per cent) |
| Lip and oral cavity | 97.0 | 3.0 |
| Oesophagus | 99.1 | 0.9 |
| Stomach | 99.2 | 0.8 |
| Colorectal | 96.9 | 3.1 |
| Liver and intrahep. bile ducts | 30.5 | 69.5 |
| Gall bladder | 92.6 | 7.4 |
| Larynx | 96.6 | 3.4 |
| Bronchus and lung | 94.7 | 5.3 |
| Bone | 97.0 | 3.0 |
| Connective tissue | 94.4 | 5.6 |
| Leukaemia | 92.8 | 7.2 |
| Breast | 95.8 | 4.2 |
| Cervix uteri | 96.8 | 3.2 |
| Corpus uteri | 97.8 | 2.2 |
| Testis | 98.9 | 1.1 |
| Prostate | 97.5 | 2.5 |
| NHL | 95.8 | 4.2 |
| Hodgkin lymphoma | 97.5 | 2.5 |
| Urinary bladder | 97.3 | 2.7 |
| Brain | 96.6 | 3.4 |
| Skin | 99.6 | 0.4 |
| Kidney | 93.4 | 6.6 |
| Thyroid | 97.6 | 2.4 |
| Ovary | 93.7 | 6.3 |
NHL, Non-Hodgkin lymphoma.
Table 3.
Cancer counts and the age-standardised incidence rates of cancers diagnosed in the Lahore district, 2010–2012, according to year of diagnosis
| 2010 |
2011 |
2012 |
|||||
|---|---|---|---|---|---|---|---|
| Site | ICD-10 code | Count | ASIR | Count | ASIR | Count | ASIR |
| Lip | C00 | 13 | 0.2 | 5 | 0.1 | 4 | 0.1 |
| Tongue | C01-C02 | 115 | 2.0 | 92 | 1.5 | 102 | 1.6 |
| Mouth | C03-C06 | 117 | 2.1 | 110 | 1.8 | 115 | 1.9 |
| Salivary glands | C07-C08 | 30 | 0.5 | 32 | 0.5 | 29 | 0.4 |
| Tonsil | C09 | 3 | 0.1 | 3 | 0.1 | 10 | 0.1 |
| Other oropharynx | C10 | 2 | 0.0 | 3 | 0.1 | 1 | 0.0 |
| Nasopharynx | C11 | 13 | 0.2 | 11 | 0.1 | 14 | 0.2 |
| Hypopharynx | C12-C13 | 22 | 0.4 | 12 | 0.2 | 19 | 0.3 |
| Pharynx | C14 | 4 | 0.1 | 3 | 0.0 | 3 | 0.0 |
| Oesophagus | C15 | 76 | 1.4 | 61 | 1.1 | 85 | 1.4 |
| Stomach | C16 | 85 | 1.5 | 86 | 1.4 | 96 | 1.5 |
| Small intestine | C17 | 15 | 0.3 | 15 | 0.3 | 13 | 0.2 |
| Colon | C18 | 148 | 2.6 | 106 | 1.7 | 135 | 2.2 |
| Rectum | C19-C20 | 101 | 1.6 | 89 | 1.4 | 133 | 2.0 |
| Anus | C21 | 21 | 0.4 | 22 | 0.3 | 21 | 0.3 |
| Liver | C22 | 176 | 3.4 | 184 | 3.4 | 145 | 2.6 |
| Gall bladder, etc | C23-C24 | 72 | 1.3 | 76 | 1.4 | 84 | 1.6 |
| Pancreas | C25 | 30 | 0.6 | 30 | 0.6 | 37 | 0.7 |
| Other ill-defined digestive | C26 | 7 | 0.1 | 11 | 0.2 | 12 | 0.2 |
| Nose, sinuses | C30-31 | 17 | 0.3 | 23 | 0.4 | 19 | 0.3 |
| Larynx | C32 | 74 | 1.4 | 55 | 1.0 | 82 | 1.4 |
| Trachea, bronchus and lung | C33-C34 | 162 | 3.2 | 156 | 2.9 | 170 | 3.2 |
| Other thoracic organs | C37-C38 | 14 | 0.2 | 11 | 0.2 | 17 | 0.2 |
| Bone | C40-C41 | 80 | 0.8 | 74 | 0.8 | 80 | 0.8 |
| Melanoma of the skin | C43 | 4 | 0.1 | 11 | 0.2 | 11 | 0.1 |
| Other skin | C44 | 152 | 2.8 | 141 | 2.5 | 174 | 2.9 |
| Connective and soft tissue | C47,C49 | 95 | 1.3 | 95 | 1.2 | 62 | 0.8 |
| Breast | C50 | 1409 | 22.9 | 1339 | 21.4 | 1404 | 21.5 |
| Vulva | C51 | 3 | 0.1 | 7 | 0.2 | 9 | 0.4 |
| Vagina | C52 | 5 | 0.2 | 6 | 0.2 | 5 | 0.2 |
| Cervix uteri | C53 | 86 | 3.1 | 69 | 2.4 | 92 | 3.2 |
| Corpus uteri | C54 | 83 | 3.5 | 84 | 3.3 | 100 | 4.1 |
| Uterus, unspecified | C55 | 34 | 1.3 | 27 | 1.1 | 28 | 1.0 |
| Ovary | C56 | 138 | 4.6 | 124 | 4.1 | 180 | 5.8 |
| Other female genital orgs. | C57 | 5 | 0.2 | 7 | 0.3 | 6 | 0.2 |
| Placenta | C58 | 3 | 0.1 | 2 | 0.0 | 2 | 0.0 |
| Penis | C60 | – | – | 1 | 0.0 | – | – |
| Prostate | C61 | 165 | 6.2 | 193 | 7.1 | 168 | 6.0 |
| Testis | C62 | 31 | 0.7 | 24 | 0.5 | 35 | 0.7 |
| Other male genital organs | C63 | – | – | 3 | 0.1 | 2 | 0.1 |
| Kidney | C64 | 88 | 1.5 | 97 | 1.5 | 89 | 1.4 |
| Renal pelvis | C65 | – | – | – | – | 2 | 0.0 |
| Ureter | C66 | – | – | 1 | 0.0 | 1 | 0.0 |
| Bladder | C67 | 177 | 3.6 | 150 | 2.8 | 223 | 4.0 |
| Other urinary organs | C68 | – | – | 2 | 0.0 | – | – |
| Eye | C69 | 33 | 0.5 | 29 | 0.4 | 35 | 0.4 |
| Brain, nervous system | C70-C72 | 248 | 3.5 | 203 | 2.8 | 234 | 3.0 |
| Thyroid | C73 | 94 | 1.3 | 92 | 1.3 | 110 | 1.5 |
| Adrenal | C74 | 2 | 0.0 | 3 | 0.0 | 6 | 0.1 |
| Hodgkin lymphoma | C81 | 104 | 1.3 | 86 | 1.0 | 92 | 0.9 |
| Non-Hodgkin lymphoma | C82-C88 | 274 | 4.4 | 234 | 3.6 | 262 | 3.9 |
| Multiple myeloma | C90 | 33 | 0.7 | 26 | 0.5 | 30 | 0.5 |
| Lymphoid leukaemia | C91 | 91 | 0.9 | 71 | 0.7 | 157 | 1.4 |
| Myeloid leukaemia | C92-93 | 42 | 0.5 | 31 | 0.4 | 96 | 1.1 |
| Other leukaemias | C95 | 30 | 0.3 | 25 | 0.3 | 45 | 0.4 |
| Leukaemia, unspecified | C94 | 3 | 0.0 | 2 | 0.0 | 3 | 0.0 |
| Other and unspecified | – | 335 | 5.7 | 369 | 6.2 | 393 | 6.4 |
| Benign CNS | – | 138 | 1.9 | 125 | 1.6 | 107 | 1.3 |
| All sites | 5302 | 97.8 | 4949 | 89.1 | 5589 | 96.8 | |
Table 4.
Cancer counts and age-standardised incidence rates of cancers diagnosed in the Lahore district in 2010–2012, by gender and cancer site/type
| Female |
Male |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Site | ICD-10-code | Count | Per cent | Crude | ASIR | Count | Per cent | Crude | ASIR |
| Lip | C00 | 9 | 0.1 | 0.1 | 0.1 | 13 | 0.2 | 0.1 | 0.1 |
| Tongue | C01-C02 | 129 | 1.4 | 0.9 | 1.7 | 180 | 2.7 | 1.2 | 1.8 |
| Mouth | C03-C06 | 130 | 1.4 | 0.9 | 1.6 | 212 | 3.1 | 1.4 | 2.2 |
| Salivary glands | C07-C08 | 41 | 0.5 | 0.3 | 0.5 | 50 | 0.7 | 0.3 | 0.5 |
| Tonsil | C09 | 8 | 0.1 | 0.1 | 0.1 | 8 | 0.1 | 0.1 | 0.1 |
| Other oropharynx | C10 | – | – | – | – | 6 | 0.1 | 0.0 | 0.1 |
| Nasopharynx | C11 | 19 | 0.2 | 0.1 | 0.2 | 19 | 0.3 | 0.1 | 0.2 |
| Hypopharynx | C12-C13 | 32 | 0.4 | 0.2 | 0.4 | 21 | 0.3 | 0.1 | 0.2 |
| Pharynx | C14 | 5 | 0.1 | 0.0 | 0.1 | 5 | 0.1 | 0.0 | 0.0 |
| Oesophagus | C15 | 95 | 1.0 | 0.7 | 1.2 | 127 | 1.9 | 0.8 | 1.4 |
| Stomach | C16 | 105 | 1.2 | 0.8 | 1.3 | 162 | 2.4 | 1.0 | 1.6 |
| Small intestine | C17 | 17 | 0.2 | 0.1 | 0.2 | 26 | 0.4 | 0.2 | 0.3 |
| Colon | C18 | 159 | 1.8 | 1.1 | 1.9 | 230 | 3.4 | 1.5 | 2.4 |
| Rectum | C19-C20 | 137 | 1.5 | 1.0 | 1.5 | 186 | 2.7 | 1.2 | 1.9 |
| Anus | C21 | 23 | 0.3 | 0.2 | 0.3 | 41 | 0.6 | 0.3 | 0.4 |
| Liver | C22 | 177 | 2.0 | 1.3 | 2.4 | 328 | 4.8 | 2.1 | 3.7 |
| Gall bladder, etc | C23-C24 | 139 | 1.5 | 1.0 | 1.9 | 93 | 1.4 | 0.6 | 1.0 |
| Pancreas | C25 | 40 | 0.4 | 0.3 | 0.5 | 57 | 0.8 | 0.4 | 0.6 |
| Other ill-defined digestive | C26 | 14 | 0.2 | 0.1 | 0.1 | 16 | 0.2 | 0.1 | 0.2 |
| Nose, sinuses | C30-31 | 27 | 0.3 | 0.2 | 0.3 | 32 | 0.5 | 0.2 | 0.3 |
| Larynx | C32 | 28 | 0.3 | 0.2 | 0.3 | 183 | 2.7 | 1.2 | 2.0 |
| Trachea, bronchus and lung | C33-C34 | 92 | 1.0 | 0.7 | 1.2 | 396 | 5.8 | 2.5 | 4.6 |
| Other thoracic organs | C37-C38 | 16 | 0.2 | 0.1 | 0.2 | 26 | 0.4 | 0.2 | 0.2 |
| Bone | C40-C41 | 91 | 1.0 | 0.7 | 0.6 | 143 | 2.1 | 0.9 | 0.9 |
| Melanoma of the skin | C43 | 13 | 0.1 | 0.1 | 0.1 | 13 | 0.2 | 0.1 | 0.1 |
| Other skin | C44 | 196 | 2.2 | 1.4 | 2.7 | 271 | 4.0 | 1.7 | 2.8 |
| Connective and soft tissue | C47,C49 | 108 | 1.2 | 0.8 | 1.0 | 144 | 2.1 | 0.9 | 1.2 |
| Breast | C50 | 4082 | 45.0 | 29.2 | 47.6 | 70 | 1.0 | 0.5 | 0.8 |
| Vulva | C51 | 19 | 0.2 | 0.1 | 0.2 | – | – | – | – |
| Vagina | C52 | 16 | 0.2 | 0.1 | 0.2 | – | – | – | – |
| Cervix uteri | C53 | 247 | 2.7 | 1.8 | 2.9 | – | – | – | – |
| Corpus uteri | C54 | 267 | 2.9 | 1.9 | 3.6 | – | – | – | – |
| Uterus, unspecified | C55 | 89 | 1.0 | 0.6 | 1.1 | – | – | – | – |
| Ovary | C56 | 442 | 4.9 | 3.2 | 4.9 | – | – | – | – |
| Other female genital organs | C57 | 18 | 0.2 | 0.1 | 0.2 | – | – | – | – |
| Placenta | C58 | 7 | 0.1 | 0.1 | 0.0 | – | – | – | – |
| Penis | C60 | – | – | – | – | 1 | 0.0 | 0.0 | 0.0 |
| Prostate | C61 | – | – | – | – | 526 | 7.8 | 3.4 | 6.4 |
| Testis | C62 | – | – | – | – | 90 | 1.3 | 0.6 | 0.6 |
| Other male genital organs | C63 | – | – | – | – | 5 | 0.1 | 0.0 | 0.1 |
| Kidney | C64 | 102 | 1.1 | 0.7 | 1.1 | 172 | 2.5 | 1.1 | 1.7 |
| Renal pelvis | C65 | 1 | 0.0 | 0.0 | 0.0 | 1 | 0.0 | 0.0 | 0.0 |
| Ureter | C66 | 1 | 0.0 | 0.0 | 0.0 | 1 | 0.0 | 0.0 | 0.0 |
| Bladder | C67 | 109 | 1.2 | 0.8 | 1.5 | 441 | 6.5 | 2.8 | 5.0 |
| Other urinary organs | C68 | – | – | – | – | 2 | 0.0 | 0.0 | 0.0 |
| Eye | C69 | 40 | 0.4 | 0.3 | 0.4 | 57 | 0.8 | 0.4 | 0.5 |
| Brain, nervous system | C70-C72 | 227 | 2.5 | 1.6 | 2.2 | 458 | 6.8 | 2.9 | 3.8 |
| Thyroid | C73 | 215 | 2.4 | 1.5 | 2.2 | 81 | 1.2 | 0.5 | 0.7 |
| Adrenal | C74 | 4 | 0.0 | 0.0 | 0.0 | 7 | 0.1 | 0.0 | 0.1 |
| Hodgkin lymphoma | C81 | 80 | 0.9 | 0.6 | 0.7 | 202 | 3.0 | 1.3 | 1.4 |
| Non-Hodgkin lymphoma | C82-C88 | 277 | 3.1 | 2.0 | 3.3 | 493 | 7.3 | 3.2 | 4.5 |
| Multiple myeloma | C90 | 36 | 0.4 | 0.3 | 0.5 | 53 | 0.8 | 0.3 | 0.6 |
| Lymphoid leukaemia | C91 | 112 | 1.2 | 0.8 | 0.7 | 207 | 3.1 | 1.3 | 1.2 |
| Myeloid leukaemia | C92-93 | 62 | 0.7 | 0.4 | 0.5 | 107 | 1.6 | 0.7 | 0.8 |
| Other leukaemias | C94 | 2 | 0.0 | 0.0 | 0.0 | 6 | 0.1 | 0.0 | 0.0 |
| Leukaemia, unspecified | C95 | 40 | 0.4 | 0.3 | 0.3 | 60 | 0.9 | 0.4 | 0.4 |
| Other and unspecified | – | 536 | 5.9 | 3.8 | 6.6 | 561 | 8.3 | 3.6 | 5.7 |
| Benign CNS | – | 188 | 2.1 | 1.3 | 1.8 | 182 | 2.7 | 1.2 | 1.4 |
| All sites | 9069 | 100.0 | 64.9 | 105.1 | 6771 | 100.0 | 43.6 | 66.7 | |
Table 5.
Age-specific and age-standardised incidence rates of cancers diagnosed in the Lahore district, 2010–2012, among females
| Site | Total cases | 0- | 5- | 10- | 15- | 20- | 25- | 30- | 35- | 40- | 45- | 50- | 55- | 60- | 65- | 70- | 75- | Crude | Per cent | ASIR | ICD-10 codes |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lip | 9 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.2 | 0.0 | 1.1 | 0.4 | 0.6 | 1.6 | 0.7 | 0.1 | 0.1 | 0.1 | C00 |
| Tongue | 129 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.1 | 0.2 | 1.2 | 1.4 | 5.4 | 4.7 | 4.9 | 6.6 | 5.8 | 8.7 | 5.1 | 0.9 | 1.4 | 1.7 | C01-C02 |
| Mouth | 130 | 0.0 | 0.0 | 0.0 | 0.2 | 0.2 | 0.3 | 0.2 | 1.5 | 2.9 | 1.6 | 6.0 | 4.6 | 3.5 | 7.0 | 11.1 | 5.1 | 0.9 | 1.4 | 1.6 | C03-C06 |
| Salivary glands | 41 | 0.0 | 0.0 | 0.1 | 0.0 | 0.1 | 0.5 | 0.2 | 0.8 | 0.5 | 0.6 | 1.1 | 0.7 | 2.7 | 1.9 | 0.8 | 0.0 | 0.3 | 0.5 | 0.5 | C07-C08 |
| Tonsil | 8 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.0 | 0.2 | 0.7 | 0.4 | 0.0 | 0.0 | 0.8 | 0.7 | 0.1 | 0.1 | 0.1 | C09 |
| Nasopharynx | 19 | 0.0 | 0.0 | 0.1 | 0.1 | 0.1 | 0.2 | 0.3 | 0.0 | 0.3 | 0.6 | 0.2 | 0.4 | 0.4 | 0.0 | 1.6 | 0.0 | 0.1 | 0.2 | 0.2 | C11 |
| Hypopharynx | 32 | 0.0 | 0.0 | 0.0 | 0.1 | 0.2 | 0.1 | 0.2 | 0.5 | 0.3 | 0.6 | 0.7 | 1.4 | 1.9 | 0.6 | 1.6 | 0.7 | 0.2 | 0.4 | 0.4 | C12-C13 |
| Pharynx | 5 | 0.0 | 0.0 | 0.1 | 0.0 | 0.0 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.4 | 0.0 | 0.0 | 0.8 | 0.7 | 0.0 | 0.1 | 0.1 | C14 |
| Oesophagus | 95 | 0.0 | 0.0 | 0.0 | 0.1 | 0.0 | 0.3 | 0.3 | 0.9 | 1.9 | 4.0 | 1.8 | 2.8 | 5.8 | 4.5 | 4.7 | 3.6 | 0.7 | 1.0 | 1.2 | C15 |
| Stomach | 105 | 0.0 | 0.0 | 0.0 | 0.0 | 0.3 | 0.1 | 1.0 | 1.3 | 2.2 | 3.8 | 2.5 | 3.9 | 2.7 | 8.9 | 0.0 | 3.6 | 0.8 | 1.2 | 1.3 | C16 |
| Small intestine | 17 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.0 | 0.0 | 0.0 | 0.6 | 0.0 | 0.0 | 0.4 | 1.9 | 1.3 | 2.4 | 0.7 | 0.1 | 0.2 | 0.2 | C17 |
| Colon | 159 | 0.0 | 0.0 | 0.1 | 0.3 | 0.1 | 0.7 | 1.3 | 2.0 | 2.0 | 3.4 | 3.3 | 7.0 | 5.0 | 9.6 | 9.5 | 8.0 | 1.1 | 1.8 | 1.9 | C18 |
| Rectum | 137 | 0.0 | 0.0 | 0.1 | 0.2 | 0.9 | 0.9 | 1.4 | 1.2 | 1.7 | 3.0 | 3.1 | 4.2 | 5.0 | 4.5 | 6.3 | 5.1 | 1.0 | 1.5 | 1.5 | C19-C20 |
| Anus | 23 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.0 | 0.3 | 0.1 | 0.9 | 0.6 | 0.2 | 0.0 | 0.8 | 0.6 | 2.4 | 0.7 | 0.2 | 0.3 | 0.3 | C21 |
| Liver | 177 | 0.1 | 0.1 | 0.0 | 0.1 | 0.1 | 0.1 | 0.2 | 0.3 | 1.4 | 4.4 | 6.2 | 11.2 | 12.0 | 16.6 | 8.7 | 5.1 | 1.3 | 2.0 | 2.4 | C22 |
| Gall bladder, etc | 139 | 0.0 | 0.0 | 0.0 | 0.1 | 0.0 | 0.0 | 0.5 | 0.4 | 1.5 | 2.6 | 4.9 | 6.7 | 8.9 | 14.1 | 7.1 | 8.7 | 1.0 | 1.5 | 1.9 | C23-C24 |
| Pancreas | 40 | 0.0 | 0.0 | 0.0 | 0.1 | 0.0 | 0.2 | 0.1 | 0.5 | 0.3 | 0.8 | 0.9 | 2.1 | 0.8 | 5.8 | 2.4 | 1.4 | 0.3 | 0.4 | 0.5 | C25 |
| Other ill-defined digestive | 14 | 0.0 | 0.0 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.0 | 0.0 | 0.0 | 0.9 | 0.0 | 1.2 | 0.0 | 0.8 | 0.0 | 0.1 | 0.2 | 0.1 | C26 |
| Nose, sinuses | 27 | 0.1 | 0.0 | 0.0 | 0.1 | 0.0 | 0.0 | 0.1 | 0.3 | 0.0 | 0.6 | 0.7 | 1.8 | 2.3 | 1.3 | 0.8 | 0.7 | 0.2 | 0.3 | 0.3 | C30-31 |
| Larynx | 28 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.2 | 0.1 | 0.6 | 0.8 | 1.3 | 1.4 | 1.2 | 0.6 | 0.0 | 2.2 | 0.2 | 0.3 | 0.3 | C32 |
| Trachea, bronchus and lung | 92 | 0.0 | 0.0 | 0.1 | 0.2 | 0.1 | 0.1 | 0.5 | 0.4 | 0.9 | 1.4 | 1.8 | 4.6 | 5.4 | 8.3 | 6.3 | 5.8 | 0.7 | 1.0 | 1.2 | C33-C34 |
| Other thoracic organs | 16 | 0.0 | 0.0 | 0.0 | 0.1 | 0.0 | 0.0 | 0.0 | 0.3 | 0.2 | 0.8 | 0.0 | 0.4 | 1.6 | 0.6 | 0.8 | 0.7 | 0.1 | 0.2 | 0.2 | C37-C38 |
| Bone | 91 | 0.2 | 0.5 | 0.9 | 1.4 | 0.9 | 0.3 | 0.4 | 1.3 | 0.3 | 0.6 | 0.4 | 0.4 | 0.0 | 0.0 | 1.6 | 0.0 | 0.7 | 1.0 | 0.6 | C40-C41 |
| Melanoma of the skin | 13 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.1 | 0.3 | 0.2 | 0.4 | 0.4 | 0.7 | 0.0 | 0.0 | 0.8 | 0.7 | 0.1 | 0.1 | 0.1 | C43 |
| Other skin | 196 | 0.1 | 0.0 | 0.0 | 0.1 | 0.1 | 0.3 | 0.2 | 1.3 | 2.9 | 2.2 | 5.1 | 6.3 | 11.3 | 16.6 | 19.0 | 19.6 | 1.4 | 2.2 | 2.7 | C44 |
| Connective and soft tissue | 108 | 0.4 | 0.3 | 0.3 | 0.6 | 0.6 | 0.8 | 0.8 | 1.2 | 1.7 | 1.2 | 1.8 | 1.4 | 1.6 | 3.8 | 2.4 | 2.9 | 0.8 | 1.2 | 1.0 | C47,C49 |
| Breast | 4082 | 0.0 | 0.1 | 0.1 | 0.1 | 3.3 | 14.0 | 32.2 | 55.9 | 86.2 | 126.8 | 130.3 | 158.5 | 154.1 | 157.9 | 124.9 | 92.1 | 29.2 | 45.0 | 47.6 | C50 |
| Vulva | 19 | 0.0 | 0.0 | 0.1 | 0.0 | 0.0 | 0.0 | 0.1 | 0.4 | 0.2 | 0.2 | 0.0 | 1.4 | 0.8 | 0.6 | 0.8 | 2.9 | 0.1 | 0.2 | 0.2 | C51 |
| Vagina | 16 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.2 | 0.0 | 0.1 | 0.3 | 0.8 | 0.2 | 0.7 | 0.4 | 0.0 | 0.8 | 1.4 | 0.1 | 0.2 | 0.2 | C52 |
| Cervix uteri | 247 | 0.0 | 0.0 | 0.0 | 0.0 | 0.2 | 0.4 | 1.3 | 3.9 | 5.7 | 9.4 | 7.1 | 10.5 | 10.1 | 8.3 | 5.5 | 5.1 | 1.8 | 2.7 | 2.9 | C53 |
| Corpus uteri | 267 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.2 | 0.6 | 1.5 | 1.9 | 6.0 | 9.8 | 16.5 | 22.1 | 16.0 | 18.2 | 7.2 | 1.9 | 2.9 | 3.6 | C54 |
| Uterus, unspecified | 89 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.1 | 0.9 | 1.5 | 3.4 | 4.0 | 2.8 | 5.8 | 3.8 | 4.7 | 0.0 | 0.6 | 1.0 | 1.1 | C55 |
| Ovary | 442 | 0.0 | 0.1 | 0.6 | 0.8 | 1.6 | 1.9 | 3.0 | 4.9 | 7.9 | 12.2 | 13.4 | 15.4 | 19.4 | 12.1 | 11.1 | 7.2 | 3.2 | 4.9 | 4.9 | C56 |
| Other female genital organs | 18 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.0 | 0.3 | 0.5 | 0.2 | 0.2 | 0.7 | 2.3 | 0.6 | 0.8 | 0.0 | 0.1 | 0.2 | 0.2 | C57 |
| Placenta | 7 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.1 | 0.3 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.1 | 0.0 | C58 |
| Kidney | 102 | 0.7 | 0.1 | 0.1 | 0.0 | 0.2 | 0.0 | 0.2 | 1.6 | 2.0 | 1.6 | 2.7 | 4.9 | 3.1 | 3.2 | 3.2 | 4.3 | 0.7 | 1.1 | 1.1 | C64 |
| Renal pelvis | 1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.2 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | C65 |
| Ureter | 1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.8 | 0.0 | 0.0 | 0.0 | 0.0 | C66 |
| Bladder | 109 | 0.1 | 0.0 | 0.0 | 0.1 | 0.0 | 0.1 | 0.2 | 1.1 | 1.2 | 1.6 | 2.7 | 4.9 | 5.0 | 8.9 | 10.3 | 10.1 | 0.8 | 1.2 | 1.5 | C67 |
| Eye | 40 | 0.9 | 0.3 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.3 | 0.4 | 0.0 | 0.0 | 0.8 | 4.5 | 0.8 | 2.2 | 0.2 | 0.4 | 0.4 | C69 |
| Brain, nervous system | 227 | 0.3 | 0.7 | 0.6 | 0.9 | 0.9 | 2.0 | 1.4 | 2.5 | 3.3 | 4.4 | 4.9 | 5.3 | 5.0 | 7.7 | 4.0 | 2.9 | 1.6 | 2.5 | 2.2 | C70-C72 |
| Thyroid | 215 | 0.0 | 0.1 | 0.1 | 0.2 | 1.9 | 1.6 | 2.8 | 2.9 | 3.3 | 4.6 | 6.5 | 3.5 | 6.6 | 3.2 | 7.9 | 2.9 | 1.5 | 2.4 | 2.2 | C73 |
| Adrenal | 4 | 0.1 | 0.1 | 0.0 | 0.0 | 0.1 | 0.0 | 0.0 | 0.0 | 0.2 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | C74 |
| Hodgkin lymphoma | 80 | 0.2 | 0.4 | 0.3 | 0.4 | 0.9 | 1.0 | 0.4 | 1.1 | 0.3 | 1.0 | 0.2 | 1.8 | 1.6 | 0.6 | 2.4 | 0.0 | 0.6 | 0.9 | 0.7 | C81 |
| Non-Hodgkin lymphoma | 277 | 0.2 | 0.3 | 0.5 | 0.5 | 0.5 | 0.8 | 0.9 | 2.0 | 3.6 | 5.8 | 7.4 | 12.3 | 10.9 | 14.1 | 13.4 | 18.1 | 2.0 | 3.1 | 3.3 | C82-C88 |
| Multiple myeloma | 36 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.3 | 1.6 | 1.1 | 0.7 | 2.7 | 3.2 | 4.0 | 0.7 | 0.3 | 0.4 | 0.5 | C90 |
| Lymphoid leukaemia | 112 | 2.0 | 1.3 | 1.4 | 0.3 | 0.1 | 0.2 | 0.2 | 0.0 | 0.5 | 0.2 | 0.2 | 0.7 | 1.2 | 0.6 | 0.8 | 0.0 | 0.8 | 1.2 | 0.7 | C91 |
| Myeloid leukaemia | 62 | 0.3 | 0.2 | 0.2 | 0.2 | 0.5 | 0.6 | 0.6 | 0.7 | 0.5 | 0.6 | 1.1 | 1.4 | 0.8 | 0.6 | 1.6 | 0.0 | 0.4 | 0.7 | 0.5 | C92-93 |
| Other leukaemias | 2 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.2 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | C94 |
| Leukaemia, unspecified | 40 | 0.3 | 0.5 | 0.3 | 0.3 | 0.1 | 0.3 | 0.1 | 0.1 | 0.2 | 0.2 | 0.7 | 0.0 | 0.0 | 0.6 | 0.8 | 0.0 | 0.3 | 0.4 | 0.3 | C95 |
| Other and unspecified | 536 | 0.5 | 0.2 | 0.2 | 0.2 | 1.1 | 1.8 | 2.7 | 4.7 | 7.0 | 12.6 | 14.9 | 24.9 | 24.1 | 33.9 | 26.9 | 18.8 | 3.8 | 5.9 | 6.6 | Other and unspecified |
| Benign CNS | 188 | 0.2 | 0.1 | 0.3 | 0.7 | 0.3 | 1.6 | 2.2 | 3.9 | 4.0 | 4.8 | 3.6 | 2.1 | 4.3 | 4.5 | 2.4 | 0.7 | 1.3 | 2.1 | 1.8 | Benign CNS |
| All sites | 9069 | 6.7 | 5.0 | 6.5 | 8.4 | 16.4 | 32.1 | 58.3 | 104.7 | 155.6 | 237.8 | 259.9 | 337.6 | 364.1 | 398.2 | 348.7 | 259.5 | 64.9 | 100.0 | 105.1 | All sites |
Table 6.
Age-specific and age-standardised incidence rates of cancers diagnosed in the Lahore district, 2010–2012, amongst males
| Site | Total cases | 0- | 5- | 10- | 15- | 20- | 25- | 30- | 35- | 40- | 45- | 50- | 55- | 60- | 65- | 70- | 75- | Crude | Per cent | ASIR | ICD-10 codes |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lip | 13 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.0 | 0.1 | 0.2 | 0.0 | 0.0 | 0.2 | 0.6 | 1.3 | 0.5 | 0.6 | 0.0 | 0.1 | 0.2 | 0.1 | C00 |
| Tongue | 180 | 0.0 | 0.0 | 0.0 | 0.0 | 0.3 | 0.6 | 0.6 | 2.0 | 3.5 | 3.6 | 4.4 | 5.0 | 7.2 | 6.2 | 9.5 | 2.3 | 1.2 | 2.7 | 1.8 | C01-C02 |
| Mouth | 212 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.2 | 1.2 | 1.1 | 3.0 | 5.4 | 4.8 | 9.7 | 10.1 | 8.8 | 7.7 | 4.0 | 1.4 | 3.1 | 2.2 | C03-C06 |
| Salivary glands | 50 | 0.0 | 0.0 | 0.1 | 0.1 | 0.1 | 0.2 | 0.3 | 0.7 | 0.6 | 0.7 | 0.7 | 1.1 | 1.9 | 1.6 | 3.0 | 1.7 | 0.3 | 0.7 | 0.5 | C07-C08 |
| Tonsil | 8 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.0 | 0.1 | 0.1 | 0.0 | 0.2 | 0.3 | 0.6 | 0.5 | 0.0 | 0.0 | 0.1 | 0.1 | 0.1 | C09 |
| Other oropharynx | 6 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.3 | 0.0 | 0.6 | 0.3 | 0.0 | 0.6 | 0.0 | 0.0 | 0.1 | 0.1 | C10 |
| Nasopharynx | 19 | 0.0 | 0.0 | 0.0 | 0.1 | 0.1 | 0.0 | 0.2 | 0.1 | 0.3 | 0.3 | 0.2 | 0.8 | 1.3 | 0.5 | 0.0 | 0.0 | 0.1 | 0.3 | 0.2 | C11 |
| Hypopharynx | 21 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.1 | 0.1 | 0.3 | 0.0 | 0.6 | 0.3 | 0.9 | 1.0 | 1.2 | 2.9 | 0.1 | 0.3 | 0.2 | C12-C13 |
| Pharynx | 5 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.1 | 0.3 | 0.2 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.0 | C14 |
| Oesophagus | 127 | 0.0 | 0.0 | 0.0 | 0.1 | 0.1 | 0.2 | 0.3 | 0.8 | 0.5 | 3.1 | 3.1 | 4.5 | 5.3 | 6.2 | 9.5 | 6.9 | 0.8 | 1.9 | 1.4 | C15 |
| Stomach | 162 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.8 | 0.9 | 1.4 | 2.2 | 3.8 | 3.3 | 4.7 | 4.4 | 10.3 | 8.3 | 3.4 | 1.0 | 2.4 | 1.6 | C16 |
| Small intestine | 26 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.0 | 0.0 | 0.3 | 0.1 | 0.5 | 0.6 | 0.8 | 0.9 | 0.5 | 1.8 | 2.3 | 0.2 | 0.4 | 0.3 | C17 |
| Colon | 230 | 0.0 | 0.0 | 0.0 | 0.4 | 0.8 | 0.6 | 0.7 | 1.5 | 2.1 | 4.8 | 4.4 | 5.8 | 11.6 | 14.5 | 9.5 | 6.3 | 1.5 | 3.4 | 2.4 | C18 |
| Rectum | 186 | 0.0 | 0.0 | 0.0 | 0.4 | 0.7 | 0.9 | 1.4 | 1.0 | 1.0 | 3.3 | 3.9 | 5.0 | 8.2 | 11.9 | 4.2 | 6.3 | 1.2 | 2.7 | 1.9 | C19-C20 |
| Anus | 41 | 0.0 | 0.0 | 0.0 | 0.1 | 0.1 | 0.1 | 0.5 | 0.0 | 0.6 | 0.5 | 1.3 | 0.8 | 2.2 | 1.6 | 0.6 | 1.1 | 0.3 | 0.6 | 0.4 | C21 |
| Liver | 328 | 0.0 | 0.0 | 0.0 | 0.1 | 0.1 | 0.2 | 0.0 | 1.5 | 1.9 | 5.2 | 10.1 | 17.0 | 14.8 | 24.3 | 17.2 | 14.9 | 2.1 | 4.8 | 3.7 | C22 |
| Gall bladder, etc | 93 | 0.0 | 0.0 | 0.0 | 0.1 | 0.1 | 0.1 | 0.1 | 0.3 | 0.5 | 0.5 | 2.9 | 3.6 | 5.0 | 7.2 | 4.2 | 7.4 | 0.6 | 1.4 | 1.0 | C23-C24 |
| Pancreas | 57 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.0 | 0.1 | 0.0 | 0.8 | 1.4 | 1.3 | 3.1 | 1.3 | 4.7 | 4.7 | 1.1 | 0.4 | 0.8 | 0.6 | C25 |
| Other ill-defined digestive | 16 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.0 | 0.0 | 0.0 | 0.1 | 0.5 | 0.4 | 0.3 | 0.6 | 2.1 | 0.0 | 1.1 | 0.1 | 0.2 | 0.2 | C26 |
| Nose, sinuses | 32 | 0.0 | 0.0 | 0.0 | 0.1 | 0.2 | 0.2 | 0.0 | 0.2 | 0.1 | 0.5 | 0.6 | 1.4 | 0.9 | 1.6 | 2.4 | 0.0 | 0.2 | 0.5 | 0.3 | C30-31 |
| Larynx | 183 | 0.0 | 0.0 | 0.0 | 0.0 | 0.3 | 0.0 | 0.2 | 0.5 | 1.5 | 3.8 | 4.6 | 7.8 | 10.4 | 12.4 | 11.3 | 5.7 | 1.2 | 2.7 | 2.0 | C32 |
| Trachea, bronchus and lung | 396 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.1 | 0.6 | 1.9 | 1.8 | 5.7 | 4.8 | 13.1 | 21.4 | 32.0 | 37.4 | 32.6 | 2.5 | 5.8 | 4.6 | C33-C34 |
| Other thoracic organs | 26 | 0.0 | 0.0 | 0.0 | 0.1 | 0.0 | 0.0 | 0.1 | 0.2 | 0.3 | 0.2 | 1.1 | 0.0 | 0.6 | 0.5 | 1.8 | 2.9 | 0.2 | 0.4 | 0.2 | C37-C38 |
| Bone | 143 | 0.2 | 0.5 | 1.2 | 2.4 | 1.0 | 0.5 | 0.6 | 0.7 | 0.6 | 0.9 | 0.6 | 0.3 | 3.1 | 0.5 | 1.8 | 0.6 | 0.9 | 2.1 | 0.9 | C40-C41 |
| Melanoma of the skin | 13 | 0.0 | 0.0 | 0.0 | 0.1 | 0.0 | 0.1 | 0.1 | 0.1 | 0.0 | 0.0 | 0.0 | 1.1 | 0.0 | 0.5 | 0.0 | 1.7 | 0.1 | 0.2 | 0.1 | C43 |
| Other skin | 271 | 0.1 | 0.1 | 0.1 | 0.2 | 0.3 | 0.9 | 1.6 | 2.0 | 2.3 | 2.8 | 4.1 | 8.6 | 11.3 | 16.5 | 10.1 | 21.2 | 1.7 | 4.0 | 2.8 | C44 |
| Connective and soft tissue | 144 | 0.4 | 0.5 | 0.1 | 0.9 | 0.8 | 1.1 | 0.7 | 1.1 | 0.5 | 2.8 | 1.1 | 2.5 | 2.8 | 3.6 | 4.2 | 2.9 | 0.9 | 2.1 | 1.2 | C47,C49 |
| Breast | 70 | 0.0 | 0.0 | 0.0 | 0.1 | 0.1 | 0.1 | 0.0 | 0.3 | 0.9 | 2.1 | 1.5 | 1.9 | 1.9 | 8.8 | 2.4 | 1.7 | 0.5 | 1.0 | 0.8 | C50 |
| Penis | 1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | C60 |
| Prostate | 526 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.1 | 0.0 | 0.0 | 0.3 | 1.0 | 4.4 | 13.1 | 27.1 | 46.0 | 69.4 | 87.0 | 3.4 | 7.8 | 6.4 | C61 |
| Testis | 90 | 0.2 | 0.0 | 0.0 | 0.5 | 1.1 | 1.2 | 1.2 | 1.1 | 1.0 | 0.7 | 0.6 | 0.3 | 0.3 | 1.6 | 0.6 | 0.6 | 0.6 | 1.3 | 0.6 | C62 |
| Other male genital organs | 5 | 0.1 | 0.0 | 0.0 | 0.0 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 1.0 | 0.6 | 0.0 | 0.0 | 0.1 | 0.1 | C63 |
| Kidney | 172 | 0.6 | 0.2 | 0.0 | 0.1 | 0.1 | 0.2 | 0.3 | 0.9 | 2.7 | 3.3 | 3.3 | 5.6 | 6.3 | 7.2 | 9.5 | 5.7 | 1.1 | 2.5 | 1.7 | C64 |
| Renal pelvis | 1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.3 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | C65 |
| Ureter | 1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.3 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | C66 |
| Bladder | 441 | 0.1 | 0.0 | 0.0 | 0.0 | 0.1 | 0.2 | 0.4 | 1.8 | 2.2 | 5.9 | 7.5 | 19.2 | 23.0 | 30.0 | 29.7 | 42.4 | 2.8 | 6.5 | 5.0 | C67 |
| Other urinary organs | 2 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.6 | 0.0 | 0.0 | 0.0 | C68 |
| Eye | 57 | 1.2 | 0.2 | 0.0 | 0.1 | 0.1 | 0.1 | 0.0 | 0.1 | 0.1 | 0.7 | 0.6 | 0.3 | 1.6 | 2.1 | 2.4 | 1.1 | 0.4 | 0.8 | 0.5 | C69 |
| Brain, nervous system | 458 | 0.7 | 1.0 | 0.7 | 1.2 | 1.6 | 2.9 | 4.5 | 4.4 | 5.0 | 7.3 | 8.8 | 10.6 | 11.3 | 9.8 | 8.3 | 3.4 | 2.9 | 6.8 | 3.8 | C70-C72 |
| Thyroid | 81 | 0.0 | 0.0 | 0.0 | 0.2 | 0.2 | 0.7 | 0.8 | 0.3 | 0.8 | 1.4 | 1.8 | 3.3 | 1.6 | 2.6 | 3.0 | 1.1 | 0.5 | 1.2 | 0.7 | C73 |
| Adrenal | 7 | 0.1 | 0.0 | 0.0 | 0.1 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.2 | 0.0 | 0.3 | 0.0 | 0.0 | 0.6 | 0.0 | 0.0 | 0.1 | 0.1 | C74 |
| Hodgkin lymphoma | 202 | 0.7 | 1.8 | 0.7 | 1.0 | 0.9 | 1.4 | 1.2 | 1.4 | 1.5 | 1.6 | 1.5 | 3.3 | 1.9 | 4.1 | 3.6 | 0.6 | 1.3 | 3.0 | 1.4 | C81 |
| Non-Hodgkin lymphoma | 493 | 0.4 | 1.4 | 1.1 | 1.3 | 2.0 | 1.6 | 2.5 | 2.5 | 4.6 | 5.9 | 10.1 | 11.7 | 18.3 | 18.1 | 16.6 | 14.3 | 3.2 | 7.3 | 4.5 | C82-C88 |
| Multiple myeloma | 53 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.2 | 0.2 | 0.5 | 1.2 | 1.3 | 2.5 | 3.1 | 1.6 | 2.4 | 2.3 | 0.3 | 0.8 | 0.6 | C90 |
| Lymphoid leukaemia | 207 | 3.1 | 2.2 | 2.6 | 0.7 | 0.5 | 0.2 | 0.3 | 0.1 | 0.8 | 0.3 | 0.9 | 0.6 | 0.6 | 2.1 | 0.0 | 1.7 | 1.3 | 3.1 | 1.2 | C91 |
| Myeloid leukaemia | 107 | 0.3 | 0.3 | 0.4 | 0.4 | 0.7 | 0.8 | 0.9 | 1.4 | 1.0 | 1.0 | 0.7 | 1.9 | 1.9 | 2.1 | 0.0 | 0.6 | 0.7 | 1.6 | 0.8 | C92-93 |
| Other leukaemias | 6 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.1 | 0.0 | 0.0 | 0.1 | 0.0 | 0.4 | 0.0 | 0.0 | 0.0 | 0.6 | 0.0 | 0.0 | 0.1 | 0.0 | C94 |
| Leukaemia, unspecified | 60 | 0.5 | 0.4 | 0.7 | 0.2 | 0.5 | 0.2 | 0.3 | 0.1 | 0.3 | 0.3 | 0.2 | 0.3 | 0.6 | 0.0 | 0.6 | 0.0 | 0.4 | 0.9 | 0.4 | C95 |
| Other and unspecified | 561 | 0.3 | 0.1 | 0.6 | 0.9 | 0.4 | 2.0 | 2.6 | 2.9 | 4.8 | 6.0 | 12.2 | 18.7 | 23.9 | 28.4 | 25.5 | 34.9 | 3.6 | 8.3 | 5.7 | Other and unspecified |
| Benign CNS | 182 | 0.3 | 0.4 | 0.2 | 0.5 | 0.8 | 2.0 | 1.9 | 2.4 | 2.1 | 3.3 | 3.3 | 1.1 | 3.1 | 1.6 | 3.0 | 0.6 | 1.2 | 2.7 | 1.4 | Benign CNS |
| All sites | 6771 | 9.2 | 9.5 | 9.1 | 12.2 | 14.8 | 20.6 | 27.4 | 38.0 | 53.7 | 93.1 | 118.4 | 194.0 | 255.2 | 337.0 | 329.7 | 328.0 | 43.6 | 100.0 | 66.7 | All sites |
Of the 15 825 patients, death was recorded in 5134 (32.4%) cases by the cut-off date for this study; this included 2726 female and 2408 male patients. Four thousand three hundred and forty-seven patients were still alive (27.5%) at the time of the review, whereas the vital status of 6344 patients (40.1%) could not be determined. Death certificates were available in each record of a hospital death for about 8% of patients (400/5134), representing just one collaborating centre, which is SKMCH and RC. Table 7 displays death counts and proportion by cancer sites. Since the follow-up information was not available for nearly 40% of the patients, the mortality to incidence ratio was not calculated either.
Table 7.
Distribution of deaths recorded (5134 (2726 female and 2408 male patients)), in patients diagnosed with cancer, in the Lahore district, in 2010–2012, according to gender and cancer type (top 10 cancers only)
| Females | Count | Per cent | Males | Count | Per cent |
|---|---|---|---|---|---|
| Breast | 987 | 36 | Brain | 213 | 9 |
| Ovary | 137 | 5 | Bronchus and lung | 207 | 9 |
| Colorectum | 127 | 5 | NHL | 169 | 7 |
| NHL | 109 | 4 | Prostate | 168 | 7 |
| Lip and oral cavity | 106 | 4 | Colorectum | 155 | 6 |
| Brain | 99 | 4 | Lip and oral cavity | 152 | 6 |
| Leukaemia | 87 | 3 | Liver and intrahep. bile ducts | 151 | 6 |
| Liver and intrahep. bile ducts | 85 | 3 | Leukaemia | 144 | 6 |
| Cervix uteri | 65 | 2 | Urinary bladder | 133 | 6 |
| Corpus uteri | 53 | 2 | Stomach | 73 | 3 |
NHL, Non-Hodgkin lymphoma.
Of the deaths recorded, among females, 36% were reported in those who had breast cancer, 5% each in those who had ovarian and colorectal carcinoma, 4% each in NHL, lip and oral cavity, and brain tumour, 3% each in those with leukaemia and liver and intrahepatic bile duct tumours, and 2% each in those who had cancer of the cervix and corpus uteri. In male patients, 9% each were in those who had tumour of the brain and bronchus and lung, 7% each in those with NHL and prostate cancer, 6% each in cancers of the colorectum, lip and oral cavity, liver and intrahepatic bile ducts, bladder, and leukaemia, and 3% in stomach carcinoma.
Discussion
The Registry has been in existence since 2005 but was in an evolving phase in the initial years of its functioning. Therefore, conducting a comparison of the cases recorded over the initial years did not appear to be useful. Further, since there are notification delays and the Registry is still receiving information on cases diagnosed in the most recent years (2014–2015), mainly from one centre, this time period has not been included in the study either. It is hoped that a study conducted at a subsequent stage will cover the 2013–2015 period. For the time period 2010–2012, the results reported for the population of the Lahore district show that, on average, over 5200 new cancer cases were diagnosed every year. The fact that nearly 7% were non-microscopically confirmed cancers, as opposed to nearly 93% that were microscopically confirmed, supports the contention that there was no reliance on the pathology laboratory as the only source of information. These figures are similar to those reported for the Karachi Cancer Registry.5 However, some of the cases diagnosed clinically might not have been reported to the Registry, but we have no way of knowing that at present. The ASIR for all cancers combined was higher among females (105.1) than among males (66.7). These results also include the ASIRs for benign CNS tumours and other/unspecified sites. The ASIRs reported by the Surveillance, Epidemiology, and End Results (SEER) Program of the USA of America (USA) are very high (359.4 for females and 282.6 for males).21 22 These figures represent SEER 18 registries compiling data from all cases diagnosed since 2000 and covering ∼30% of the US population.21 22 The ASIRs published in the CI5-X report for Delhi in India and Riyadh in Saudi Arabia are close to the Lahore district figures, as opposed to the SEER rates; in fact, the ASIRs for females in these three regions are quite similar to one another. It is important to point out that Delhi, located in India, to the east of Lahore, is closer to Lahore than is Karachi located in southern Pakistan. As far as the South Karachi Registry is concerned, on the basis of the last report (1998–2002) released in CI5-IX, it can be seen that the ASIRs for Karachi were relatively high (192.0 for females and 166.6 for males) as compared to those for the Lahore district. Further, in the region of Golestan in Iran (2005–2007), and for Israel, again the ASIRs were high compared to those reported for the Lahore district.19 The SEER Program, Delhi, Iran, and Saudi Arabia, reported the data for the 2003-2007 time period. Table 8 shows a comparison of the ASIRs according to cancer sites, though not all sites, in the aforementioned regions of the world. In women belonging to the Lahore district, the ASIR of breast cancer ranked the highest (47.6) of all the cancers, and was higher than that for Delhi (31.6), but relatively low compared to that reported for the Israeli Jews (89.4). Among men in the Lahore district, the ASIR of prostate cancer was the highest (6.4) of all the cancers, but was lower than that reported for Delhi (10.1) and Riyadh (7.9). Even though breast and prostate cancers were the most common diagnoses in the Lahore district, the point to be noted is that organised screening programmes for early detection of these diseases do not exist in Pakistan. The ASIR of cervical cancer in Lahore was 2.9, but in Delhi it was much higher at 17.7; this is despite the fact that the screening levels are low in the general population of India.23 Of the factors implicated in the aetiology of cervical cancer in the Indian population, the presence of specific oncogenic types of the human papilloma viruses (HPV), namely types 16 and 18, plays an important role in the development of cancer of the cervix. In Pakistan, one population-based study reports HPV positivity to be nearly 2.8% in the general population (25/899) and about 92% in patients with invasive cervical cancer (83/91).24 However, in India, it has been reported that HPV prevalence varies from 7.5% to 16.9% in women without cervical cancer, as opposed to 87.8% to 96.7% among patients with cervical cancer.23 Further, in the latest Globocan report, the ASIR for cancer of the cervix in Pakistan was estimated at 7.9/100 000 females with 5233 cases identified in 2012;15 in the same year, in Saudi Arabia, 241 cases were diagnosed, with the ASIR at 2.7/100 000 women; in contrast to this, in India, 122 844 cervical cancer cases were diagnosed, with a relatively high ASIR of 22.0/100 000 females.15 Since the ASIR is low in the aforementioned Muslim countries compared to a non-Muslim country, circumcision of men may be a plausible explanation in reducing the transmission of HPV infection to their female sexual partners. Circumcision of men is the norm among Muslim males. The role of circumcision has been demonstrated in three separate randomised trials done in Africa.25 Since the incidence of cervical cancer in Pakistan is relatively low and the 5-year prevalence is 15 323, setting up a formal screening programme may have lower yields and therefore a low priority in resource allocation and decision-making in our setting.15
Table 8.
ASIRs, per 100 000 population per year, for selected cancer sites, in Pakistan, India, Iran, Israel and the USA
| Pakistan | Globocan | Pakistan | India | Iran | Saudi Arabia | Israel | USA | |
|---|---|---|---|---|---|---|---|---|
| Lahore | Pakistan | Karachi | New Delhi | Golestan | Riyadh | Jews | SEER | |
| 2010–2012 | 2012 | 1998–2002 | 2003–2007 | 2005–2007 | 2003–2007 | 2003–2007 | 2003–2007 | |
| Oral cavity and salivary glands-C00-C08 | ||||||||
| Male | 4.6 | 10.5 | 22.5 | 14.0 | 1.7 | 1.6 | 3.3 | 6.9 |
| Female | 3.9 | 9.1 | 20.4 | 4.7 | 1.3 | 1.4 | 2.3 | 3.1 |
| Pharynx-C09-C14 | ||||||||
| Male | 0.6 | 3.8 | 8.2 | 6.6 | 1.0 | 2.4 | 1.5 | 4.4 |
| Female | 0.8 | 1.3 | 3.4 | 1.5 | 0.7 | 1.3 | 0.5 | 1.1 |
| Oesophagus-C15 | ||||||||
| Male | 1.4 | 3.9 | 6.7 | 4.9 | 23.2 | 1.6 | 1.8 | 5.1 |
| Female | 1.2 | 4.4 | 8.6 | 2.9 | 18.8 | 1.3 | 0.9 | 1.2 |
| Stomach-C16 | ||||||||
| Male | 1.6 | 3.8 | 6.0 | 3.2 | 30.4 | 4.4 | 10.0 | 6.6 |
| Female | 1.3 | 2.2 | 3.6 | 1.5 | 12.6 | 2.3 | 5.4 | 3.3 |
| Small intestine-C17 | ||||||||
| Male | 0.3 | – | 0.2 | 0.2 | 1.4 | 0.5 | 1.0 | 1.5 |
| Female | 0.2 | – | 0.4 | 0.1 | 0.9 | 0.3 | 0.7 | 1.1 |
| Colorectum-C18-C21 | ||||||||
| Male | 4.7 | 4.7 | 7.1 | 5.5 | 13.6 | 12.5 | 42.8 | 35.3 |
| Female | 3.7 | 3.3 | 5.2 | 3.7 | 10.4 | 10.6 | 32.6 | 26.5 |
| Liver-C22 | ||||||||
| Male | 3.7 | 4.7 | 5.4 | 2.6 | 3.6 | 3.0 | 3.1 | 7.6 |
| Female | 2.4 | 2.5 | 3.7 | 1.5 | 2.0 | 6.0 | 1.4 | 2.4 |
| Gall bladder-C23-C24 | ||||||||
| Male | 1.0 | 0.9 | 1.3 | 4.0 | 1.2 | 1.2 | 1.7 | 1.7 |
| Female | 1.9 | 2.2 | 4.9 | 8.0 | 1.6 | 2.5 | 1.4 | 1.7 |
| Pancreas-C25 | ||||||||
| Male | 0.6 | 0.5 | 0.9 | 1.9 | 2.8 | 3.2 | 8.6 | 8.2 |
| Female | 0.5 | 0.4 | 0.5 | 1.1 | 1.0 | 1.9 | 6.4 | 6.2 |
| Nose and sinuses-C30-C31 | ||||||||
| Male | 0.3 | – | 0.7 | 0.3 | 0.0 | 0.2 | 0.4 | 0.6 |
| Female | 0.3 | – | 0.4 | 0.2 | 0.2 | 0.2 | 0.3 | 0.4 |
| Larynx-C32 | ||||||||
| Male | 2.0 | 5.0 | 10.7 | 8.0 | 4.1 | 1.7 | 4.1 | 4.3 |
| Female | 0.3 | 0.7 | 1.8 | 1.1 | 1.4 | 0.1 | 0.6 | 0.9 |
| Trachea, bronchus and lung-C33-C34 | ||||||||
| Male | 4.6 | 9.8 | 25.2 | 13.7 | 17.5 | 6.3 | 29.8 | 48.3 |
| Female | 1.2 | 1.7 | 3.6 | 3.6 | 5.6 | 2.2 | 13.4 | 33.8 |
| Bone-C40-C41 | ||||||||
| Male | 0.9 | – | 1.3 | 2.0 | 1.3 | 0.8 | 1.3 | 1.0 |
| Female | 0.6 | – | 1.5 | 1.2 | 1.5 | 0.5 | 1.0 | 0.8 |
| Melanoma of the skin-C43 | ||||||||
| Male | 0.1 | 0.3 | 0.5 | 0.2 | 0.9 | 0.3 | 13.7 | 16.8 |
| Female | 0.1 | 0.2 | 0.3 | 0.2 | 0.7 | 0.4 | 11.2 | 12.0 |
| Skin-C44 | ||||||||
| Male | 2.8 | – | 4.3 | 1.3 | 11.0 | 3.8 | 2.8 | 1.3 |
| Female | 2.7 | – | 4.1 | 1.0 | 7.7 | 3.2 | 1.9 | 1.0 |
| Connective and soft tissue-C47-C49 | ||||||||
| Male | 1.2 | – | 2.4 | 1.5 | 2.1 | 1.3 | 3.2 | 3.0 |
| Female | 1.0 | – | 2.3 | 1.2 | 2.1 | 0.9 | 2.2 | 2.1 |
| Breast-C50 | ||||||||
| Male | 0.8 | – | 1.0 | 1.3 | 0.1 | 0.5 | 1.3 | 0.7 |
| Female | 47.6 | 50.3 | 69.0 | 31.6 | 28.0 | 21.1 | 89.4 | 86.6 |
| Cervix uteri-C53 | ||||||||
| Female | 2.9 | 7.9 | 7.5 | 17.7 | 5.4 | 2.0 | 5.5 | 6.4 |
| Corpus uteri-C54 | ||||||||
| Female | 3.6 | 3.6 | 6.7 | 4.5 | 1.7 | 4.4 | 14.4 | 16.7 |
| Ovary-C56-C57.0-4 | ||||||||
| Female | 5.1 | 5.6 | 8.8 | 8.6 | 6.1 | 3.3 | 9.2 | 9.6 |
| Other female genital organs-C51-C52, C55, C58 | ||||||||
| Female | 1.5 | – | 1.0 | 1.6 | 1.4 | 0.9 | 1.8 | 2.5 |
| Penis-C60 | ||||||||
| Male | – | – | 0.1 | 1.0 | 0.0 | 0.1 | 0.3 | 0.7 |
| Prostate-C61 | ||||||||
| Male | 6.4 | 6.6 | 10.1 | 10.1 | 10.6 | 7.9 | 68.3 | 106.8 |
| Testis-C62 | ||||||||
| Male | 0.6 | 0.9 | 1.2 | 0.6 | 2.3 | 0.6 | 4.7 | 4.9 |
| Kidney, etc -C64, C66, C68 | ||||||||
| Male | 1.7 | 1.7 | 1.9 | 2.7 | 2.2 | 3.8 | 13.9 | 137.0 |
| Female | 1.1 | 0.9 | 0.8 | 1.2 | 1.2 | 2.5 | 6.5 | 7.1 |
| Bladder-C67 | ||||||||
| Male | 5.0 | 5.1 | 9.3 | 6.5 | 8.5 | 5.6 | 25.5 | 20.8 |
| Female | 1.5 | 1.6 | 2.6 | 1.5 | 2.8 | 1.3 | 4.8 | 5.3 |
| Eye-C69 | ||||||||
| Male | 0.5 | – | 0.6 | 0.3 | 0.4 | 0.4 | 0.6 | 0.8 |
| Female | 0.4 | – | 0.3 | 0.2 | 0.2 | 0.2 | 0.4 | 0.6 |
| Brain, CNS-C70-C72 | ||||||||
| Male | 3.8 | 3.4 | 3.3 | 3.8 | 7.8 | 3.5 | 6.7 | 6.4 |
| Female | 2.2 | 2.1 | 2.7 | 2.4 | 5.3 | 2.1 | 5.0 | 4.6 |
| Thyroid-C73 | ||||||||
| Male | 0.7 | 0.7 | 0.7 | 1.1 | 1.2 | 2.5 | 4.8 | 3.9 |
| Female | 2.2 | 2.2 | 2.9 | 2.5 | 3.0 | 10.2 | 14.7 | 12.3 |
| Adrenal and other endocrine-C74-C75 | ||||||||
| Male | 0.1 | – | 0.2 | 0.2 | 0.7 | 0.3 | 0.6 | 0.5 |
| Female | 0.0 | – | 0.3 | 0.2 | 0.4 | 0.2 | 0.5 | 0.4 |
| Hodgkin lymphoma-C81 | ||||||||
| Male | 1.4 | 2.2 | 2.0 | 1.6 | 1.8 | 2.2 | 3.6 | 2.7 |
| Female | 0.7 | 0.8 | 1.0 | 0.7 | 1.1 | 2.0 | 3.4 | 2.2 |
| NHL-C82-C88, C96 | ||||||||
| Male | 4.5 | 5.3 | 7.6 | 5.6 | 7.2 | 8.6 | 17.9 | 15.5 |
| Female | 3.3 | 3.4 | 5.1 | 3.0 | 3.3 | 7.1 | 14.4 | 10.8 |
| Multiple myeloma-C88, C90 | ||||||||
| Male | 0.6 | 0.7 | 1.8 | 2.0 | 2.4 | 1.8 | 4.8 | 4.7 |
| Female | 0.5 | 0.6 | 1.3 | 1.2 | 2.2 | 1.0 | 3.0 | 3.1 |
| Leukaemia-C91-C95 | ||||||||
| Male | 2.4 | 3.3 | 4.8 | 5.6 | 10.8 | 5.7 | 10.6 | 11.1 |
| Female | 1.5 | 2.2 | 4.1 | 3.6 | 7.7 | 4.3 | 6.9 | 7.1 |
| All sites-C00-C96 | ||||||||
| Male | 66.7 | 96.0 | 166.6 | 119.7 | 165.3 | 104.1 | 273.1 | 359.4 |
| Female | 105.1 | 127.7 | 192.0 | 118.4 | 142.0 | 103.9 | 308.5 | 282.6 |
ASIR, The Age-Standardized Incidence Rates; NHL, Non-Hodgkin lymphoma.
As shown in table 8, the ASIRs/100 000 population per year for 10 common cancers in Pakistan, as reported in the Globocan 2012, compared to Lahore, are as follows: In women: breast 50.3, 47.6; lip and oral cavity 9.1, 3.9; cervix uteri 7.9, 2.9; ovary 5.6, 5.1; oesophagus 4.4, 1.2; corpus uteri 3.6, 3.6; NHL 3.4, 3.3; colorectum 3.3, 3.7; liver 2.5, 2.4; and stomach 2.2, 1.3, while among men it was as follows: lip and oral cavity 10.5, 4.6; lung 9.8, 4.6; NHL 5.3, 4.5; prostate 6.6, 6.4; bladder 5.1, 5.0; larynx 5.0, 2.0; colorectum 4.7, 4.7; liver 4.7, 3.7; oesophagus 3.9, 1.4; stomach 3.8, 1.6; and brain and nervous system 3.4, 3.8. The comparison shows that rates are somewhat higher for tobacco-related cancers (lip and oral cavity, lung, larynx and oesophagus) and cervical cancer, though for the latter the rates are still lower than those reported in countries with a high HPV prevalence rate. Since the Globocan 2012 report included data from the Punjab Cancer Registry, Karachi South district, and Dr. Yasmin's paper, the relatively high cancer rates for certain cancers may be attributed to the high consumption of tobacco-related products in that part of Pakistan, in the form of cigarettes and bidi and also of smokeless tobacco as betel quid and niswar.26 Further, Karachi South is one of the 29 districts of the province of Sindh,12 located in the south of the country, and its population was 1.72 M during the period under study. Its last report, published in the CI-5, IX, shows a high incidence rate for tobacco-related cancers.22 Therefore, the dissimilarity in the incidence rates could be attributed to the geographic and lifestyle differences between these two regions. Table 8, depicting the ASIRs, highlights the differences between these two regions and other regions of the world as well.
As far as the mortality data in our study are concerned, since the vital status of all the patients could not be recorded, our results have to be interpreted with caution. The highest mortality was recorded in patients diagnosed with breast cancer among females, and among those with brain tumours in males. Owing to the non-availability of the vital status of nearly half of the patients, the survival statistics could not be reported either. Death certificates were available from just one collaborating centre for each record of a hospital death and accounted for nearly 8% of the deaths recorded in the Registry. However, the point to be noted is that the cancer diagnoses were not merely reported from hospitals; rather, they were also reported on patients identified as new cancer cases from different laboratories/collection centres within the district. The establishment of a central death registry in the region could help in collecting the mortality data and determining the cause-specific mortality, along with the survival estimates for the study population. While the Government of Pakistan maintains the National Database Registration Authority with all citizens’ data and biometric information, the capture of death information is variable and typically done at the local government level.27 28 Deaths within hospitals have documented death certificates which get communicated to local government, but the recording of death diagnosis most likely over-reports the final mechanisms of death (‘cardio respiratory failure’), rather than the underlying causes. In view of this, death data and thus survival data have inherent inaccuracies in it.
Conclusion
This is the first time that an attempt has been made to determine and report the population-based cancer statistics for the Lahore district. This collaborative study highlights cancer registration and follow-up issues in a developing country like Pakistan, along with the non-availability of recent, accurate population estimates required as denominators in computation of the incidence rates. On average, 5200 new cases were reported annually in the Lahore district in 2010–2012. Although it is likely that all the cases have not been reported, it is not possible to gauge the extent of under-reporting at this stage. The cancer statistics reported in this manuscript can be used as baseline figures for comparison with studies to be undertaken in the future. These statistics can also assist in exploring, thus highlighting the putative risk factors associated with cancers commonly diagnosed in the region, as part of a health promotion and education programme. Finally, this report can play an important role in developing prevention, early detection and cancer control strategies in the region.
Supplementary Material
Acknowledgments
Clinical and participating investigators: Misbah Masood was responsible for reporting the cancers recorded at the Institute of Nuclear Medicine and Oncology, Lahore; Ghulam Rasool Sial from Ittefaq Hospital, Lahore; Nasir Chughtai from Sheikh Zayed Hospital, Lahore; Omar Rasheed Chughtai from Chughtais Lahore Lab, Lahore; Tanveer Mustafa from Fatima Jinnah Medical University, Lahore; Zeba Aziz and Muhammad Abbas Khokhar from Jinnah Hospital, Lahore; Ghazala Hanif and Alia Ahmad from the Children's Hospital and the Institute of Child Health, Lahore; Rakhshindah Bajwa from the Services Institute of Medical Sciences, Lahore; Sabiha Riaz and Imrana Tanvir from Fatima Memorial College of Medicine and Dentistry, Lahore; Farooq Aziz from Shalamar Medical and Dental College, Lahore; Tazeen Anis from Allama Iqbal Medical College, Lahore; Shahida Niazi from King Edward Medical University, Lahore; and Bilquis A. Suleman from Nawaz Sharif Social Security Hospital, Lahore. Neelam Siddiqui contributed intellectually to the study. Mohammad Tariq Mahmood, Sajid Mushtaq, Asif Loya and Mudassar Hussain did the pathological confirmation of cases at SKMCH and RC, Lahore. Raqib Faraz, Aneel Yousaf, Hina Asif and Adna Atif validated the data, checked for duplication and followed up on the patients; and Ain ul Quader and Kamran Liaqat Ali worked on the comparison of the incidence rates with other regions.
Footnotes
Contributors: FB conceived the idea of the study, designed it, supervised the statistical analysis, did the literature search, interpreted the results, drafted the manuscript and finalised it. She further did the survival analysis for this study. SM did the case-finding, indexing and coding of cases, computed the incidence rates, and created the figures and tables. MAY and FS reviewed the paper critically for important intellectual content, interpretation of the results and final approval of the version to be published.
Competing interests: None declared.
Ethics approval: The Institutional Review Board of the Shaukat Khanum Memorial Cancer Hospital & Research Center, Lahore, Pakistan.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Nishtar S. Chapter 2-Health systems in Pakistan, pp 35-50. In: Nishtar S, ed. Choked pipes: reforming Pakistan's mixed health systems. Karachi: Oxford University Press, 2010:37. Fig 4. [PubMed] [Google Scholar]
- 2.Valsecchi MG, Steliarova-Foucher E. Cancer registration in developing countries: luxury or necessity? Lancet Oncol 2008;9:159–67. 10.1016/S1470-2045(08)70028-7 [DOI] [PubMed] [Google Scholar]
- 3.The World Bank. Washington DC, USA, 2016. http://databank.worldbank.org/data/reports.aspx?source=2&type=metadata&series=EN.POP.DNST# and http://wdi.worldbank.org/table/1.5 (accessed 25 Jan 2015). [Google Scholar]
- 4.Survey of Pakistan (Map). Pakistan 2015. http://www.surveyofpakistan.gov.pk/ (accessed 17 Dec 2015).
- 5.Bhurgri Y. Epidemiology of cancers in Karachi 1995–1999. Karachi: Pharmacia and Upjohn, 2001. [Google Scholar]
- 6.Punjab Cancer Registry. SKMCH & RC, Lahore, Pakistan 2011. http://punjabcancerregistry.org.pk (accessed 16 Dec 2015).
- 7.Shaukat Khanum Memorial Cancer Hospital and Research Center. Lahore, Pakistan, 2015. http://www.shaukatkhanum.org.pk/ (accessed 16 Dec 2015). [DOI] [PubMed] [Google Scholar]
- 8.Badar F. Cancer registration in Pakistan. J Coll Physicians Surg Pak 2013;23:611–12. doi:08.2013/JCPSP.612612 [PubMed] [Google Scholar]
- 9.Badar F, Mahmood S. The state of cancer registration in Pakistan. J Ayub Med Coll Abbottabad 2015;27:507–8. [PubMed] [Google Scholar]
- 10.The Societies Registration Act, 1860 (Act XXI of 1860). Pakistan 2015. http://punjablaws.gov.pk/laws/1.html#_ftn2 (accessed 16 Dec 2016).
- 11.IACR-International Association of Cancer Registries. Lyon, France, 2015. http://www.iacr.com.fr/ (accessed 16 Dec 2015). [Google Scholar]
- 12.Pakistan Bureau of Statistics-Government of Pakistan. Islamabad, Pakistan 2015. http://www.pbs.gov.pk/content/population-census (accessed 16 Dec 2015).
- 13.Census-Publication No. 125-Population Census Organization-Statistics Division, Government of Pakistan, Islamabad (2000). Statistical Tables of 1998 Population and Housing Census. In: ‘1998 District Census Report of Lahore’. Islamabad: Government of Pakistan, 2000:77–305. [Google Scholar]
- 14.MacLennan R. Chapter 6-Items of patient information which may be collected by registries. In: Jensen OM, Parkin DM, MacLennan R, et al., eds. Cancer registration: principles and methods-IARC scientific publications No. 95. Lyon, France: International Agency for Research on Cancer, 1991. http://www.iarc.fr/en/publications/pdfs-online/epi/sp95/SP95.pdf (accessed 16 Feb 2016). [PubMed] [Google Scholar]
- 15.GLOBOCAN 2012: Estimated Cancer Incidence, Mortality, and Prevalence Worldwide in 2012. Lyon, France, 2015. http://globocan.iarc.fr/Default.aspx (accessed 17 Dec 2015). [Google Scholar]
- 16.Census in Pakistan by Wikipedia. Wikimedia foundation. San Francisco, CA, USA, 2016. https://en.wikipedia.org/wiki/Census_in_Pakistan (accessed 22 Jan 2016). [Google Scholar]
- 17.International Association of Cancer Registries, European Network of Cancer Registries, and International Agency for Research on Cancer, working group. Program for multiple primaries- IARC/IACR multiple primary rules. Appendix 3. In: Ferlay J, Burkhard C, Whelan S, et al., eds. Check and conversion programs for cancer registries (IARC/IACR tools for cancer registries). IARC technical report No. 42. Lyon: International Agency for Research on Cancer, 2005:38–45. [Google Scholar]
- 18.National Cancer Institute, Bethesda, MD, Registre des Cancers de I’Isere, Isere, France, Gerhard Domagk Institut fur Pathologie, Munster Universitat, Munster, Germany, Chirurgische Klinik mit Poliklinik der Universitat Erlangen-Nurnberg, Erlangen, Germany, International Agency for Research on Cancer, Lyon, France, Societa Italiana di Cancerologia, Milan, Italy, University of Chicago, Chicago, IL, USA, European Network of Cancer Registries, and International Society of Pediatric Oncology Working Group, contributors. 6th digit code for histologic grading and differentiation. In: Fritz A, Percy C, Jack A, et al., eds. International classification of diseases for oncology. 3rd edn. Geneva: WHO, 2000:31. [Google Scholar]
- 19.Holden K, ed. ICD-10-CM Expert for Hospitals. The complete official code set. Codes valid October 1, 2015 through September 30, 2016. Salt Lake City, UT, USA: Optum360, LLC. 2015.
- 20.Boyle P, Parkin DM. Chapter 11-statistical methods for registries-IARC. In: Jensen OM, Parkin DM, MacLennan R, et al., eds. Cancer registration: principles and methods. Lyon, France: IARC Scientific Publication No. 95. International Agency for Research on Cancer, 1991. https:// http://www.iarc.fr/en/publications/pdfs-online/epi/sp95/SP95.pdf (accessed 16 Feb 2016). [PubMed] [Google Scholar]
- 21.The Surveillance, Epidemiology, and End Results (SEER) Program. NCI, Bethesda, Maryland 2016. http://seer.cancer.gov/registries/terms.html (accessed 4 Feb 2016).
- 22.Cancer Incidence in Five Continents Volumes I to X-IACR; International Agency for Research on Cancer, Lyon, France 2016. http://ci5.iarc.fr/CI5I-X/Pages/table4_sel.aspx (accessed 3 Feb 2016).
- 23.Sreedevi A, Javed R, Dinesh A. Epidemiology of cervical cancer with special focus on India. Int J Womens Health 2015;7:405–14. 10.2147/IJWH.S50001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Raza SA, Franceschi S, Pallardy S, et al. Human papillomavirus infection in women with and without cervical cancer in Karachi, Pakistan. Br J Cancer 2010;102:1657–60. 10.1038/sj.bjc.6605664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Giuliano AR, van der Loeff MF, Nyitray AG. Circumscribed HIV-infected men and HPV transmission. Lancet Infect Dis 2011;11:581–2. 10.1016/S1473-3099(11)70073-1 [DOI] [PubMed] [Google Scholar]
- 26.Imam SZ, Nawaz H, Sepah YJ, et al. Use of smokeless tobacco among groups of Pakistani medical students-a cross-sectional study. BMC Public Health 2007;7:231. 10.1186/1471-2458-7-231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Database and Registration Authority (NADRA). https://www.nadra.gov.pk/ (accessed 26 Apr 2016).
- 28.Local Government and Community Development-Registration of Death. https://lgcd.punjab.gov.pk/FAQ (accessed 26 Apr 2016).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2016-011828supp_appendixA.pdf (164.5KB, pdf)
bmjopen-2016-011828supp_appendixB.pdf (194.9KB, pdf)
bmjopen-2016-011828supp_appendixC.pdf (422.6KB, pdf)