Abstract
X-linked cerebral creatine deficiency (MIM 300036) is caused by deficiency of the creatine transporter encoded by the SLC6A8 gene. Here we report three patients with this condition from Israel. These unrelated patients were evaluated for global developmental delays and language apraxia. Borderline microcephaly was noted in one of them. Diagnosis was prompted by brain magnetic resonance imaging and spectroscopy which revealed normal white matter distribution, but absence of the creatine peak in all three patients. Biochemical testing indicated normal plasma levels of creatine and guanidinoacetate, but an increased urine creatine/creatinine ratio. The diagnosis was confirmed by demonstrating absent [14]C-creatine transport in fibroblasts. Molecular studies indicated that the first patient is hemizygous for a single nucleotide change substituting a single amino acid (c.619 C > T, p.R207W). Expression studies in HeLa cells confirmed the causative role of the R207W substitution. The second patient had a three base pair deletion in the SLC6A8 gene (c.1222_1224delTTC, p.F408del) as well as a single base change (c.1254 + 1G > A) at a splicing site in the intron-exon junction of exon 8, the latter occurring de novo. The third patient, had a three base pair deletion (c.1006_1008delAAC, p.N336del) previously reported in other patients with creatine transporter deficiency. These three patients are the first reported cases of creatine transporter deficiency in Israel.
Keywords: SLC6A8, Creatine transport, Human fibroblasts, HELA cells, Creatine transporter deficiency, Creatine deficiency
1. Introduction
Creatine is essential for the utilization of ATP at sites of high energy requirement such as muscle, brain and heart [1], [2]. In adult humans, about half of the creatine needed is obtained by dietary intake, mostly from meat and dairy products, and the other half is synthesized in the kidney and liver [3]. Creatine and its phosphorylated form, phosphocreatine, spontaneously break down to creatinine that is excreted in the urine [3]. The loss of creatine (as creatinine) is restored by new enzymatic synthesis and by dietary intake.
Creatine deficiency syndromes are a group of rare diseases that include two autosomal disorders of creatine biosynthesis (arginine: glycine amidinotransferase (AGAT) deficiency, OMIM 612718; and guanidinoacetate methyltransferase (GAMT) deficiency, OMIM 612736) and the X-linked creatine transporter deficiency (OMIM 300352) [4], [5], [6], [7].
The SLC6A8 gene encodes the creatine transporter 1 (CT1 or CRTR), maps to Xq28 and is expressed in most human tissues, with highest levels found in skeletal muscle and kidney [8]. In the brain, the creatine transporter is strongly expressed, especially in the large projection neurons of the brain and spinal cord [9]. Defects in this transporter results in brain creatine deficiency that, in hemizygous males, is characterized by moderate to severe intellectual disability, delays in language and speech, autistic-like behavior, seizures in about 50% of cases, and mid-facial hypoplasia and short stature in some patients [10], [11], [12], [13].
The diagnosis of brain creatine deficiency is suspected based on clinical presentation with usually increased creatine/creatinine ratio and/or reduced brain creatine content by magnetic resonance spectroscopy, and confirmed by measurement of long-term creatine accumulation in fibroblasts and/or DNA sequencing of the SLC6A8 gene [10], [13], [14], [15].
According to the LOVD website (Updated May 02, 2016), there are currently 141 unique DNA variants of the SLC6A8 gene (https://grenada.lumc.nl/LOVD2/vumc/home.php?select_db=SLC6A8). The prevalence of SLC6A8 mutations in males with X-linked intellectual disability is between 1 and 5.4% [10], [12], [16], [17], [18], [19], [20], [21], [22]. In this report, we describe three male patients with creatine transporter deficiency from Israel.
2. Case reports
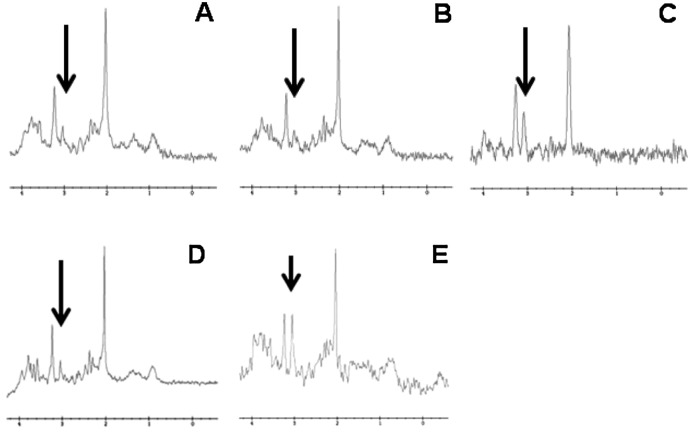
Patient 1 is a male who presented at 10 months of age with global developmental delay. He had failure to thrive, borderline microcephaly and significant hypotonia without dysmorphism. An initial MRI/MRS at 2 years of age identified non- specific changes in the white matter, but the lack of the creatine peak was not correctly identified at that time. A repeated MRI/MRS at 3 years of age demonstrated the lack of the creatine peak (Fig. 1A). Biochemical testing indicated increased urine creatine of 2.9 mmol/mol creatinine (normal 0.006–1.2 mmol/mol creatinine) with normal guanidinoacetate. At 8.5 years of age he has mild to moderate intellectual disability, significant language dyspraxia, and attended a special education school in special educational setting. The mother was low performing and has borderline microcephaly. She completed high school, but it is unknown whether she received a diploma. Her biochemical testing indicated normal urine creatine of 0.089 mmol/mol creatinine (normal range: 0.011–0.24 mmol/mol creatinine) and guanidinoacetate of 29.3 mmol/mol creatinine (normal range: 3–78 mmol/mol creatinine).
Fig. 1.
Magnetic Resonance Spectroscopy (MRS) of the brain in patients with creatine transporter deficiency. A. Patient 1; B. Patient 2; C. Mother pf patient 2; D. Patient 3; E. Normal control. The arrow indicates the creatine peak. Note diminished creatine peak in all patients with creatine transporter deficiency and mildly reduced creatine peak in the mother of patient 2.
Patient 2, a male, was referred at 11 months of age for global developmental delay, axial hypotonia of trunk with hypertonicity of extremities. His MRI at 1.5 years of age was normal, but MRS demonstrated no creatine peak (Fig. 1B). Urine creatine was 3 mmol/mol creatinine (normal 0.006–1 mmol/mol creatinine) with normal guanidinoacetate. At 5.5 years of age, the patient has severe intellectual disability, 5–10 purposeful words, and walks independently with wide-based gait. The mother seemed to have functional and intellectual difficulties (with no microcephaly), but completed high school. It is unclear whether she received a diploma. She did not go through a formal evaluation, but MRS in the mother demonstrated a brain creatine peak lower than normal (Fig. 1C).
Patient 3, a male, presented at one year and 10 months of age with severe motor and language delays. The mother has normal intelligence and is normocephalic. Over time, the child acquired mild microcephaly. At 7.5 years he has speech apraxia, borderline intelligence with significant difference between verbal IQ (VIQ 48) to performance IQ (PIQ 102), and ADHD treated with methylphenidate. Urine creatine was 3 mmol/mol creatinine (normal 0.006–1.2 mmol/mol creatinine) with normal guanidinoacetate and subsequent brain MRS showed the absence of creatine peak (Fig. 1D).
3. Materials and methods
3.1. Biochemical testing
Measurement of plasma and urine guanidinoacetate, creatine and creatinine was performed using gas chromatography mass spectrometry in a hospital laboratory (Sheba Medical Center, Tel Hashomer, Israel) according to standard procedures [23].
3.2. Patients/samples
Fibroblasts from the three pediatric patients as well as the mother of patient 2 and DNA samples from blood of the parents of patient 1 were collected according to an Institutional Review Board -approved protocol. Fibroblasts were cultured in DMEM supplemented with 15% fetal bovine serum and 1% l-glutamine. HELA cells were cultured in DMEM supplemented with 10% fetal bovine serum and 1% l-glutamine.
3.3. Creatine transports
Creatine transport was measured at 37 °C with the cluster-tray method as previously described [22]. Briefly, cells were grown to confluence in 24-well plates (Costar) and depleted of intracellular amino acids by incubation for 60 min in Earle's balanced salt solution containing 5.5 mM d-glucose and supplemented with 0.5% bovine serum albumin. Cells were then incubated with [14]C-creatine 0.1 μCi/ml (Moravek Biochemicals, Brea, CA) containing the indicated concentration of cold creatine (2 μM) for 60 min. Non-saturable creatine transport was measured in the presence of 2 mM unlabeled substrate. The transport reaction was stopped by rapidly washing the cells 4 times with ice-cold 0.1 M MgCl2. Intracellular creatine was extracted from the cells with 0.5 ml of ice-cold ethanol and added to 5 ml of scintillation fluid for counting. Intracellular creatine was normalized for the protein content of each well and intracellular water content and expressed as nmol/ml cell water/h. Saturable creatine transport was calculated by subtracting transport in the presence of excess (2 mM) cold substrate from total transport and values are reported as means ± SE of 3–6 independent determinations.
3.4. DNA sequencing
DNA was extracted from fibroblast cultures using MagNAPure Compact instrument (Roche Applied Science, Indianapolis, IN). The SLC6A8 gene was sequenced using primers flanking each exon as previously described [16]. Sequence analysis was performed using BigDye v3.1 terminator and an ABI 3130xl (Applied Biosystems). Sequences were analyzed using the Mutation Surveyor software package (Softgenetics, State College, PA, USA).
3.5. HELA cell transfection
HELA cells were transfected using Lipofectamine-2000 (Invitrogen) and selected for 3 weeks with 400 mg/ml of G418 (Invitrogen). Stable transfectants were used for transport experiments.
Site Directed Mutagenesis was performed using QuikChange (Agilent) with a pCMV6-AC-GFP containing the cDNA of SLC6A8 as a template (Origene, RG209828).
4. Results and discussion
4.1. Creatine transport by human fibroblasts
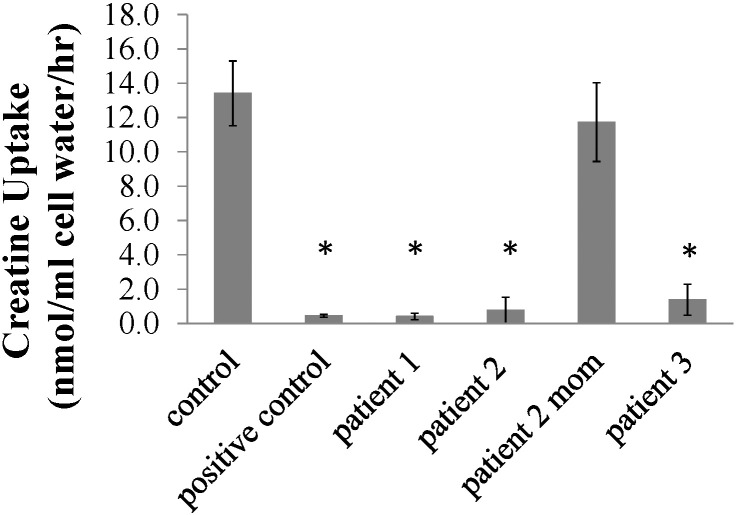
The clinical presentation and the laboratory results of plasma and urine guanidinoacetate, creatine and creatinine measurements suggested a defect in the creatine transporter. For this reason, a skin biopsy was obtained from each patient as well as the mother of the 2nd patient to confirm a defect in cellular creatine transport. Net creatine uptake in cells from all three patients was < 10% of normal fibroblasts (Fig. 2). The fibroblasts from the mother of the second patient had normal creatine uptake (Fig. 2). These latter results show that in a population of cells with random X-inactivation the results of an inactivating mutation might not result in significant changes in creatine transport. A similar phenomenon might happen in the kidney, explaining why urinary creatine excretion is normal in most mothers of patients with X-linked creatine transporter deficiency.
Fig. 2.
Creatine uptake in fibroblasts from normal control and from patients with creatine transporter deficiency. Creatine (2 μM) transport was measured for 1 h. Non-specific uptake, measured in the presence of excess (2 mM) creatine, was subtracted from total uptake to calculate net uptake. Points are averages of triplicates ± SD. *p < 0.01 versus control using analysis of variance.
The mothers of patients 1 and 2 appeared low functioning, but completed normal schooling and had normal social skills. The mother of patient 3 was completely normal, confirming the variability of the effects of mutations in the X-linked transporter gene in females.
4.2. DNA sequencing
Sequencing of the SLC6A8 gene encoding the creatine transporter indicated that patient 1 was hemizygous for c.619 C > T (exon 3), resulting in a single amino acid substitution (p.R207W). His mother was heterozygous for this mutation. This missense mutation has not been previously reported, is predicted to be pathogenic using Polyphen2 and SIFT, and is not listed in the Exac browser in 60,000 normal individuals (http://exac.broadinstitute.org/gene/ENSG00000130821). This variant was submitted to the LOVD SLC6A8 database.
Patient 2 had a three base pair deletion (c.1222_1224 del TTC, p.F408del) on exon 8, reported as disease causing 14 times in the LOVD website (http://www.LOVD.nl/SLC6A8), and in the HGMD website (https://portal.biobase-international.com/hgmd/pro/gene.php?gene=SLC6A8) from patients from Italy, USA, Spain, and Eastland Spain [15], [24], [25], [26], [27], [28], [29], [30]. This patient also had a c.1254 + 1 G > A change, possibly affecting splicing, of unknown clinical significance. The mother of this patient had normal creatine uptake and was heterozygous for c.1222_1224delTTC, indicating that the second change on this allele was the result of a de novo mutation.
Patient 3 had a three base pair deletion, c.1006_1008delAAC (p.N336del), reported 20 times previously [10], [12], [31], [32], [33] and shown to cause defective creatine transport [31]. Overexpression of this variant in SLC6A8-deficient fibroblasts did not restore creatine uptake [34]. In addition this patient had an intronic deletion IVS1768-11_1768-9_delCTC which is not expected to cause a splice site problem (reported in LOVD). The mother of this patient was heterozygous for c.1006_1008delAAC plus the intronic IVS1768-11_1768-9_delCTC.
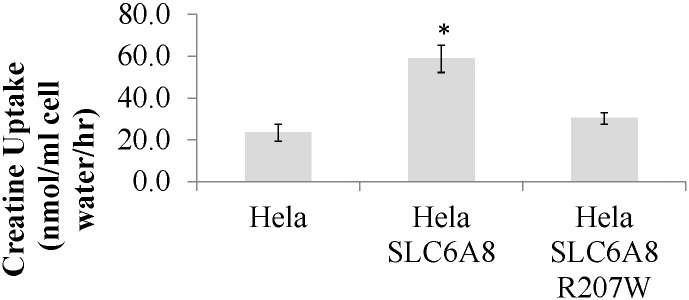
4.3. Creatine uptake
The R207W substitution was introduced in the SLC6A8 cDNA by site-directed mutagenesis and stably transfected into Hela cells. Stably transfected cells were then tested for creatine uptake (Fig. 3). Creatine uptake increased more than twice in SLC6A8- transfected cells as compared to control Hela cells (58.7 versus 23.4 nmol/ml cell/h respectively). Introduction of the R207W substitution did not result in increased creatine transport (30.2 nmol/ml cell/h), confirming that this substitution impaired creatine transporter activity.
Fig. 3.
Creatine transport in Hela cells. Creatine (2 μM) transport was measured for 30 min. Non-specific uptake, measured in the presence of excess (2 mM) creatine, was subtracted from total uptake to calculate net uptake. Points are averages of triplicates ± SD. *p < 0.01 versus Hela using analysis of variance.
In summary, this report describes three patients from Israel with cerebral creatine deficiency with clinical and biochemical diagnosis of X-linked creatine transporter deficiency. The clinical presentation was of global development delay, without specific features. Fibroblasts for these patients had markedly reduced creatine uptake. DNA sequencing of the three patients, identified three different mutations in the SLC6A8 gene, one of which was novel (p.R207W). Expression of this novel p.R207W mutation in HeLa confirmed its causative role in reducing creatine transport.
The two other patients had the two most common mutations (c.1222_1224 del TTC, p.F408del and c.1006_1008delAAC, p.N336del) identified in a global retrospective study of 101 males with X-linked creatine transporter deficiency [10]. This is the first report of these mutations in Israeli patients. Routine measurement of creatine by MRS should be considered in the evaluation of children with global developmental delay.
References
- 1.Wallimann T., Wyss M., Brdiczka D., Nicolay K., Eppenberger H.M. Intracellular compartmentation, structure and function of creatine kinase isoenzymes in tissues with high and fluctuating energy demands: the ‘phosphocreatine circuit’ for cellular energy homeostasis. The Biochemical Journal. 1992;281(Pt 1):21–40. doi: 10.1042/bj2810021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wyss M., Kaddurah-Daouk R. Creatine and creatinine metabolism. Physiol. Rev. 2000;80:1107–1213. doi: 10.1152/physrev.2000.80.3.1107. [DOI] [PubMed] [Google Scholar]
- 3.Brosnan J.T., Brosnan M.E. Creatine: endogenous metabolite, dietary, and therapeutic supplement. Annu. Rev. Nutr. 2007;27:241–261. doi: 10.1146/annurev.nutr.27.061406.093621. [DOI] [PubMed] [Google Scholar]
- 4.Leuzzi V. Inborn errors of creatine metabolism and epilepsy: clinical features, diagnosis, and treatment. J. Child Neurol. 2002;17(Suppl. 3):3S89-97. (discussion 83S97) [PubMed] [Google Scholar]
- 5.Stockler S., Schutz P.W., Salomons G.S. Cerebral creatine deficiency syndromes: clinical aspects, treatment and pathophysiology. Subcell. Biochem. 2007;46:149–166. doi: 10.1007/978-1-4020-6486-9_8. [DOI] [PubMed] [Google Scholar]
- 6.Hanna-El-Daher L., Braissant O. Creatine synthesis and exchanges between brain cells: what can be learned from human creatine deficiencies and various experimental models? Amino Acids. 2016 doi: 10.1007/s00726-016-2189-0. [DOI] [PubMed] [Google Scholar]
- 7.Braissant O. Creatine and guanidinoacetate transport at blood-brain and blood-cerebrospinal fluid barriers. J. Inherit. Metab. Dis. 2012;35:655–664. doi: 10.1007/s10545-011-9433-2. [DOI] [PubMed] [Google Scholar]
- 8.Gregor P., Nash S.R., Caron M.G., Seldin M.F., Warren S.T. Assignment of the creatine transporter gene (SLC6A8) to human chromosome Xq28 telomeric to G6PD. Genomics. 1995;25:332–333. doi: 10.1016/0888-7543(95)80155-f. [DOI] [PubMed] [Google Scholar]
- 9.Lowe M.T., Faull R.L., Christie D.L., Waldvogel H.J. Distribution of the creatine transporter throughout the human brain reveals a spectrum of creatine transporter immunoreactivity. J. Comp. Neurol. 2015;523:699–725. doi: 10.1002/cne.23667. [DOI] [PubMed] [Google Scholar]
- 10.van de Kamp J.M., Betsalel O.T., Mercimek-Mahmutoglu S., Abulhoul L., Grunewald S., Anselm I., Azzouz H., Bratkovic D., de Brouwer A., Hamel B., Kleefstra T., Yntema H., Campistol J., Vilaseca M.A., Cheillan D., D'Hooghe M., Diogo L., Garcia P., Valongo C., Fonseca M., Frints S., Wilcken B., von der Haar S., Meijers-Heijboer H.E., Hofstede F., Johnson D., Kant S.G., Lion-Francois L., Pitelet G., Longo N., Maat-Kievit J.A., Monteiro J.P., Munnich A., Muntau A.C., Nassogne M.C., Osaka H., Ounap K., Pinard J.M., Quijano-Roy S., Poggenburg I., Poplawski N., Abdul-Rahman O., Ribes A., Arias A., Yaplito-Lee J., Schulze A., Schwartz C.E., Schwenger S., Soares G., Sznajer Y., Valayannopoulos V., Van Esch H., Waltz S., Wamelink M.M., Pouwels P.J., Errami A., van der Knaap M.S., Jakobs C., Mancini G.M., Salomons G.S. Phenotype and genotype in 101 males with X-linked creatine transporter deficiency. J. Med. Genet. 2013;50:463–472. doi: 10.1136/jmedgenet-2013-101658. [DOI] [PubMed] [Google Scholar]
- 11.Salomons G.S., van Dooren S.J., Verhoeven N.M., Cecil K.M., Ball W.S., Degrauw T.J., Jakobs C. X-linked creatine-transporter gene (SLC6A8) defect: a new creatine-deficiency syndrome. Am. J. Hum. Genet. 2001;68:1497–1500. doi: 10.1086/320595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clark A.J., Rosenberg E.H., Almeida L.S., Wood T.C., Jakobs C., Stevenson R.E., Schwartz C.E., Salomons G.S. X-linked creatine transporter (SLC6A8) mutations in about 1% of males with mental retardation of unknown etiology. Hum. Genet. 2006;119:604–610. doi: 10.1007/s00439-006-0162-9. [DOI] [PubMed] [Google Scholar]
- 13.Longo N., Ardon O., Vanzo R., Schwartz E., Pasquali M. Disorders of creatine transport and metabolism. Am. J. Med. Genet. C: Semin. Med. Genet. 2011;157C:72–78. doi: 10.1002/ajmg.c.30292. [DOI] [PubMed] [Google Scholar]
- 14.Verhoeven N.M., Salomons G.S., Jakobs C. Laboratory diagnosis of defects of creatine biosynthesis and transport. Clin. Chim. Acta. 2005;361:1–9. doi: 10.1016/j.cccn.2005.04.022. [DOI] [PubMed] [Google Scholar]
- 15.Salomons G.S., van Dooren S.J., Verhoeven N.M., Marsden D., Schwartz C., Cecil K.M., DeGrauw T.J., Jakobs C. X-linked creatine transporter defect: an overview. J. Inherit. Metab. Dis. 2003;26:309–318. doi: 10.1023/a:1024405821638. [DOI] [PubMed] [Google Scholar]
- 16.Rosenberg E.H., Almeida L.S., Kleefstra T., deGrauw R.S., Yntema H.G., Bahi N., Moraine C., Ropers H.H., Fryns J.P., deGrauw T.J., Jakobs C., Salomons G.S. High prevalence of SLC6A8 deficiency in X-linked mental retardation. Am. J. Hum. Genet. 2004;75:97–105. doi: 10.1086/422102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Newmeyer A., Cecil K.M., Schapiro M., Clark J.F., Degrauw T.J. Incidence of brain creatine transporter deficiency in males with developmental delay referred for brain magnetic resonance imaging. Journal of Developmental and Behavioral Pediatrics: JDBP. 2005;26:276–282. doi: 10.1097/00004703-200508000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Lion-Francois L., Cheillan D., Pitelet G., Acquaviva-Bourdain C., Bussy G., Cotton F., Guibaud L., Gerard D., Rivier C., Vianey-Saban C., Jakobs C., Salomons G.S., Portes V.d. High frequency of creatine deficiency syndromes in patients with unexplained mental retardation. Neurology. 2006;67:1713–1714. doi: 10.1212/01.wnl.0000239153.39710.81. [DOI] [PubMed] [Google Scholar]
- 19.Arias A., Corbella M., Fons C., Sempere A., Garcia-Villoria J., Ormazabal A., Poo P., Pineda M., Vilaseca M.A., Campistol J., Briones P., Pampols T., Salomons G.S., Ribes A., Artuch R. Creatine transporter deficiency: prevalence among patients with mental retardation and pitfalls in metabolite screening. Clin. Biochem. 2007;40:1328–1331. doi: 10.1016/j.clinbiochem.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 20.Betsalel O.T., van de Kamp J.M., Martinez-Munoz C., Rosenberg E.H., de Brouwer A.P., Pouwels P.J., van der Knaap M.S., Mancini G.M., Jakobs C., Hamel B.C., Salomons G.S. Detection of low-level somatic and germline mosaicism by denaturing high-performance liquid chromatography in a EURO-MRX family with SLC6A8 deficiency. Neurogenetics. 2008;9:183–190. doi: 10.1007/s10048-008-0125-5. [DOI] [PubMed] [Google Scholar]
- 21.Puusepp H., Kall K., Salomons G.S., Talvik I., Mannamaa M., Rein R., Jakobs C., Ounap K. The screening of SLC6A8 deficiency among Estonian families with X-linked mental retardation. J. Inherit. Metab. Dis. 2009 doi: 10.1007/s10545-008-1063-y. [DOI] [PubMed] [Google Scholar]
- 22.Ardon O., di San Filippo C. Amat, Salomons G.S., Longo N. Creatine transporter deficiency in two half-brothers. Am. J. Med. Genet. A. 1979-1983;152A(2010) doi: 10.1002/ajmg.a.33551. [DOI] [PubMed] [Google Scholar]
- 23.Kasumov T., Gruca L.L., Dasarathy S., Kalhan S.C. Simultaneous assay of isotopic enrichment and concentration of guanidinoacetate and creatine by gas chromatography–mass spectrometry. Anal. Biochem. 2009;395:91–99. doi: 10.1016/j.ab.2009.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bizzi A., Bugiani M., Salomons G.S., Hunneman D.H., Moroni I., Estienne M., Danesi U., Jakobs C., Uziel G. X-linked creatine deficiency syndrome: a novel mutation in creatine transporter gene SLC6A8. Ann. Neurol. 2002;52:227–231. doi: 10.1002/ana.10246. [DOI] [PubMed] [Google Scholar]
- 25.de Grauw T.J., Salomons G.S., Cecil K.M., Chuck G., Newmeyer A., Schapiro M.B., Jakobs C. Congenital creatine transporter deficiency. Neuropediatrics. 2002;33:232–238. doi: 10.1055/s-2002-36743. [DOI] [PubMed] [Google Scholar]
- 26.Poo-Arguelles P., Arias A., Vilaseca M.A., Ribes A., Artuch R., Sans-Fito A., Moreno A., Jakobs C., Salomons G. X-linked creatine transporter deficiency in two patients with severe mental retardation and autism. J. Inherit. Metab. Dis. 2006;29:220–223. doi: 10.1007/s10545-006-0212-4. [DOI] [PubMed] [Google Scholar]
- 27.Fons C., Sempere A., Arias A., Lopez-Sala A., Poo P., Pineda M., Mas A., Vilaseca M.A., Salomons G.S., Ribes A., Artuch R., Campistol J. Arginine supplementation in four patients with X-linked creatine transporter defect. J. Inherit. Metab. Dis. 2008;31:724–728. doi: 10.1007/s10545-008-0902-1. [DOI] [PubMed] [Google Scholar]
- 28.Fons C., Sempere A., Sanmarti F.X., Arias A., Poo P., Pineda M., Ribes A., Merinero B., Vilaseca M.A., Salomons G.S., Artuch R., Campistol J. Epilepsy spectrum in cerebral creatine transporter deficiency. Epilepsia. 2009;50:2168–2170. doi: 10.1111/j.1528-1167.2009.02142.x. [DOI] [PubMed] [Google Scholar]
- 29.Fons C., Arias A., Sempere A., Poo P., Pineda M., Mas A., Lopez-Sala A., Garcia-Villoria J., Vilaseca M.A., Ozaez L., Lluch M., Artuch R., Campistol J., Ribes A. Response to creatine analogs in fibroblasts and patients with creatine transporter deficiency. Mol. Genet. Metab. 2010;99:296–299. doi: 10.1016/j.ymgme.2009.10.186. [DOI] [PubMed] [Google Scholar]
- 30.Valayannopoulos V., Boddaert N., Chabli A., Barbier V., Desguerre I., Philippe A., Afenjar A., Mazzuca M., Cheillan D., Munnich A., de Keyzer Y., Jakobs C., Salomons G.S., de Lonlay P. Treatment by oral creatine, l-arginine and l-glycine in six severely affected patients with creatine transporter defect. J. Inherit. Metab. Dis. 2012;35:151–157. doi: 10.1007/s10545-011-9358-9. [DOI] [PubMed] [Google Scholar]
- 31.Battini R., Chilosi A., Mei D., Casarano M., Alessandri M.G., Leuzzi V., Ferretti G., Tosetti M., Bianchi M.C., Cioni G. Mental retardation and verbal dyspraxia in a new patient with de novo creatine transporter (SLC6A8) mutation. Am. J. Med. Genet. A. 2007;143A:1771–1774. doi: 10.1002/ajmg.a.31827. [DOI] [PubMed] [Google Scholar]
- 32.Chilosi A., Leuzzi V., Battini R., Tosetti M., Ferretti G., Comparini A., Casarano M., Moretti E., Alessandri M.G., Bianchi M.C., Cioni G. Treatment with l-arginine improves neuropsychological disorders in a child with creatine transporter defect. Neurocase. 2008;14:151–161. doi: 10.1080/13554790802060821. [DOI] [PubMed] [Google Scholar]
- 33.Chilosi A., Casarano M., Comparini A., Battaglia F.M., Mancardi M.M., Schiaffino C., Tosetti M., Leuzzi V., Battini R., Cioni G. Neuropsychological profile and clinical effects of arginine treatment in children with creatine transport deficiency. Orphanet Journal of Rare Diseases. 2012;7(43) doi: 10.1186/1750-1172-7-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rosenberg E.H., Martinez Munoz C., Betsalel O.T., van Dooren S.J., Fernandez M., Jakobs C., deGrauw T.J., Kleefstra T., Schwartz C.E., Salomons G.S. Functional characterization of missense variants in the creatine transporter gene (SLC6A8): improved diagnostic application. Hum. Mutat. 2007;28:890–896. doi: 10.1002/humu.20532. [DOI] [PubMed] [Google Scholar]