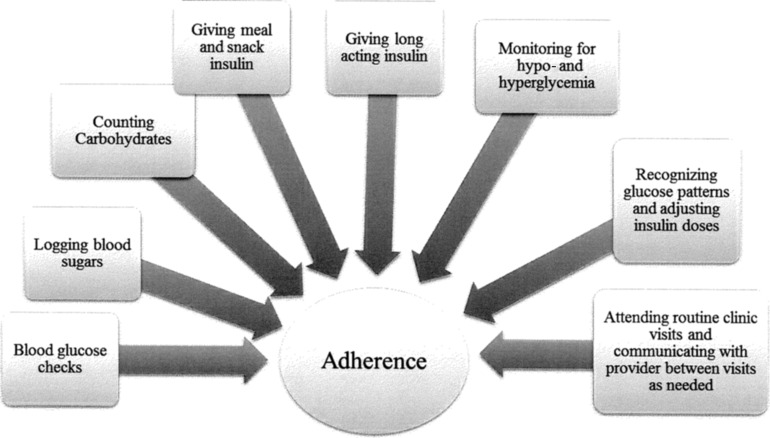
Adherence to the type 1 diabetes (T1D) regimen is notoriously difficult to measure as it includes many components (Fig. 1). Previous studies have relied on self-report or parent-report questionnaires to report on adherence, such as the Self Care Inventory1 or the Self-Management of Diabetes in Adolescents.2 Other studies have used structured interviews, such as the Diabetes Self-Management Profile3 or physician-reported adherence,4 all of which have problems with bias (e.g., social desirability) or insufficient information (i.e., physicians may not be privy to information regarding the patient's diet and activity). Frequency of blood glucose monitoring (BGM), obtained by glucometer downloads, has been accepted as an objective measure of adherence that may be more closely linked with glycemic control,5 but it only captures one aspect of adherence. For example, a patient may check blood glucose frequently, but without using that information to make adjustments to insulin, glycemic control will not be improved. Furthermore, using glucometer data has its own problems—patients (especially adolescents) often forget to bring meters to clinic visits or they may only bring one of several meters (e.g., one at the school nurse's office, one at the other parent's house), resulting in an underestimate of the frequency of BGM. Other problems include difficulty matching up meter data to the appropriate date and time (if date/time is wrong in the meter), dead batteries, and difficulties with software for meter downloads.
FIG. 1.
Type 1 diabetes treatment regimen tasks associated with adherence.
The BOLUS score described by Clements et al.6 is an objective measure of adherence that has the advantage of addressing some of these problems. First, the BOLUS measure captures mealtime insulin administration, which Clements et al. demonstrate is more closely linked to glycemic control than BGM. In their sample, every one-point increase in BOLUS score was associated with a 1.5% decrease in HbA1c level.6 Similarly, a small study conducted in youth with insulin pumps demonstrated that missing one or more meal boluses per week was related to a 0.8% increase in HbA1c.7 Further support for the importance of mealtime dosing was revealed in a large sample, comparing youth in excellent glycemic control with those in poor control, in which those who reported never missing insulin boluses were 24.5 times more likely to be in excellent control than poor control.8 Second, it is unlikely that patients will forget to bring insulin pumps to clinic. Third, the BOLUS is relatively easy to obtain and interpret, making it more likely providers will use it during clinic visits when they are pressed for time.
However, additional research is needed to identify potential problems/pitfalls with the BOLUS measure of adherence. Findings from the Clements et al. article need to be replicated and extended to more diverse samples, as their study sample was 93% white, non-Hispanic. Furthermore, clinical experience suggests that patients may manually calculate their insulin dose, rather than enter the number of carbohydrates consumed into their insulin pump, which would not be captured as a mealtime dose. Similarly, as noted by the authors, adolescents commonly “guesstimate” carbohydrate values, either over- or underestimating carbohydrate grams in a given meal,9 so that the bolus does not match actual intake, making it a less perfect measure of adherence. Another potential pitfall of the BOLUS measure is that adolescents and young adults may eat more erratically, or snack more often than younger children, especially in the evenings. The BOLUS score is determined by assigning 1 point for each meal that is eaten and dosed with insulin between the hours of 6–10am, 11–3pm, and 4–10pm (three total points can be given per day). Thus, if a patient skips breakfast but appropriately gives meal insulin for lunch and dinner, or skips breakfast and then snacks after 11pm, he/she would never receive >2 points per day, giving an appearance of relative nonadherence. Finally, given the rates of disordered eating behavior in adolescents and young adults with T1D—a recent meta-analytic review found these behaviors to be evident in 39.3% of adolescents with T1D10—it is important to consider that some patients may be intentionally withholding insulin. Although the BOLUS score would indicate nonadherence in these patients, the reasoning behind the nonadherence is quite complicated in these cases, and providers should be mindful of the high rates of disordered eating behaviors in this population.
We should also note that the BOLUS measure is only available from insulin pump downloads, which excludes some of the most high-risk populations. Data from national samples have highlighted racial/ethnic disparities in the use of insulin pumps, with insulin pump use higher in white participants (61%) than black or Hispanic patients (26% and 39%, respectively).11 Furthermore, insurance companies are increasingly requiring documentation of regular BGM (i.e., four times/day) before approving insulin pumps, meaning that those patients who are less adherent are less likely to be prescribed a pump. For patients who do not use insulin pumps, “smart” pens, diabetes apps, and advanced meter technologies are emerging, but these require the user to input blood glucose values and/or carbohydrates, so they do not give reliable and objective evidence of mealtime insulin administration. More work is needed to determine the best measures of adherence for these populations, who may be those at the highest risk for problems with adherence!
Despite these limitations, the BOLUS measure offers promise as a measure of adherence that may be easily interpreted and may provide opportunities for provider-based interventions to improve adherence during clinic visits.12 Ultimately, the BOLUS score would give providers a tool to assess adherence to therapy, focus on the importance of mealtime insulin administration, and potentially improve the glycemic control of their patients using insulin pumps.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.La Greca A: Manual for the Self Care Inventory. Miami, FL: University of Miami, 2004 [Google Scholar]
- 2.Schilling LS, Dixon JK, Knafl KA, et al. : A new self-report measure of self-management of type 1 diabetes for adolescents. Nurs Res 2009;58:228–236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harris MA, Wysocki T, Sadler M, et al. : Validation of a structured interview for the assessment of diabetes self-management. Diabetes Care 2000;23:1301–1304 [DOI] [PubMed] [Google Scholar]
- 4.Kichler JC, Kaugars AS, Maglio K, Alemzadh R: Exploratory analysis of the relationships among different methods of assessing adherence and glycemic control in youth with type 1 diabetes mellitus. Health Psychol 2012;31:35–42 [DOI] [PubMed] [Google Scholar]
- 5.Guilfoyle SM, Crimmons NA, Hood KK: Blood glucose monitoring and glycemic control in adolescents with type 1 diabetes: meter downloads versus self-report. Pediatr Diabetes 2011;12:560–566 [DOI] [PubMed] [Google Scholar]
- 6.Clements MA, DeLurgio SA, Williams DD, et al. : Association of HbA1c to BOLUS scores among youths with type 1 diabetes. Diabetes Technol Ther 2016;18:351–359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burdick J, Chase P, Slover RH, et al. : Missed insulin meal boluses and elevated hemoglobin A1c levels in children receiving insulin pump therapy. Pediatrics 2004;113:e221–e224 [DOI] [PubMed] [Google Scholar]
- 8.Campbell MS, Schatz DA, Chen V, et al. : A contrast between children and adolescents with excellent and poor control: the T1D exchange clinic registry experience. Pediatr Diabetes 2014;15:110–117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spiegel G, Bortsov A, Bishop FK, et al. : Randomized nutrition education intervention to improve carbohydrate counting in adolescents with Type 1 Diabetes study: is more intensive education needed? J Acad Nutr Diet 2012;112:1736–1746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Young V, Eiser C, Johnson B, et al. : Eating problems in adolescents with Type 1 diabetes: a systematic review with meta-analysis. Diabet Med 2013;30:189–198 [DOI] [PubMed] [Google Scholar]
- 11.Willi SM, Miller KM, DiMeglio LA, et al. : Racial-ethnic disparities in management and outcomes among children with type 1 diabetes. Pediatrics 2015;135:424–434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Datye KA, Moore DJ, Russell WE, Jaser SS: A review of adolescent adherence in type 1 diabetes and the untapped potential of diabetes providers to improve outcomes. Curr Diab Rep 2015;15:51. [DOI] [PMC free article] [PubMed] [Google Scholar]