Abstract
Purpose:
To identify risk factors for late presentation in chronic glaucoma.
Materials and Methods:
In a hospital-based case–control study, 312 newly diagnosed consecutive patients with chronic glaucoma were recruited to study in Nikookari Hospital in Tabriz – Iran. Cases were defined as patients presenting with absolute field loss within 5° of fixation or a cup to disc ratio >0.8 in one or both eyes (188 patients). Controls were patients with no absolute field loss within 20° in either eye but otherwise glaucomatous field loss and a cup to disc ratio >0.5 or a difference of 0.2 or greater between the discs (124 patents).
Results:
In logistic regression model, there was a significant association between late presentation and male gender, lower education status, pseudoexfoliative glaucoma, high intraocular pressure (IOP) in the first presentation and no eye exam in last 2 years. Patients with pseudoexfoliative glaucoma had 1.5 times more odd for late presentation (1.52 confidence interval [CI]: 1.14–2.24 P = 0.004). Patients that visited by an ophthalmologist in the last 2 years had 0.5 less likely to present with advanced glaucoma (0.54 CI: 0.32–0.92 P = 0.025). Higher IOP in initial examination was associated with advanced glaucoma. We estimated 1.08 increase in odd (CI: 1.03-1.04 P = 0.001) per increase in 1 mmHg in IOPs above 25 mmHg.
Conclusion:
Our study shows that several risk factors present for late presentation in chronic glaucoma. Our results suggest planning screening programs in high-risk individuals for early detection of glaucoma and prevention of blindness.
Keywords: Advanced glaucoma, late presentation, risk factor
Introduction
Glaucoma is one of the major causes of blindness in the world.[1] Despite new medical and surgical strategies to control intraocular pressure (IOP) glaucoma remains one of the most common causes of blindness.[2] Risk factors for becoming blind from glaucoma have received little attention.
Some studies suggest that late presentation (when glaucomatous visual field defect involves central vision) is a major risk factor for glaucoma blindness;[3,4] however, there are little-published papers on why some people have early stages of glaucoma and others advanced disease at diagnosis. Fraser et al.[1] found an occupational group, high initial IOP, no family history of glaucoma, and method of referral to hospital as risk factors for late presentation of glaucoma. Fraser et al.[5] found African ethics, male gender, age, and high IOP at presentation as a risk factor for advanced disease at diagnosis. Ntim-Amponsah et al.[6] showed that high IOP, age, absence of family history of glaucoma, occupational group, and male sex were associated with late presentation of glaucoma.
This study evaluates possible risk factors for late presentation of glaucoma in East Azerbaijan. To our knowledge, this is the first study looking at the risk factors for the late presentation of chronic glaucoma in Iran.
Materials and Methods
We carried out a hospital-based case-control study. This study was undertaken over 12-months period in Nikookari Eye Center, Tabriz, Iran. Patients with newly diagnosed open-angle glaucoma how referred to glaucoma clinic eligible for the study if they had one of the late or early presentation criteria. Case (late presenting patients) was defined as:
Having field loss within 5° of fixation and visual field defect extension beyond 30° in one or both eyes or
Cup to disk ratio >0.8 when accompanied with visual field loss in the same eye.
And controls were defined as:
No absolute scotoma within 20° of fixation in either eye
And cup to disk ratio >0.5 or difference of cup to disk ratio in two eyes >0.2 when accompanied with typical glaucomatous field defect.
Patients with a history of glaucoma were excluded from the study. All patients assessed by one person (Fallahi) and then, patients interviewed by another investigator that masked to their case or control status. The following information was collected for each patient:
Age, gender, site of inhabitance, level of education, family history of glaucoma, and occupation
Type of glaucoma
Frequency of ophthalmic examination in the last 2 years
Coexisting systemic disease
Presenting IOP
Economical dependence.
For simplifying occupational grouping, standard occupational classification categorized into three groups:
Professional and technical occupations (I and II)
Manual and nonmanual skilled occupations (III and IV)
Partly skilled and nonskilled occupations (V and VI).
Sample size calculated with power 80% and statically significance level of 5% to detect a doubling of odd ratio (OR) in a factor that present in 25% of controls. Overall 140 cases and 140 controls determined as the sample size. The data were analyzed using SPSS version 15 software (inc. Chicago IL USA) to investigate the effect of each study factor on the odds of late presentation. The association between the risk factors and late presentation were assessed by calculating OR for each factor by logistic regression with 95% confidence interval (CI). Factors significant at invariant level were entered to a multivariate model for determining adjusted OR. For continuous variables, Mann–Whitney U-test was used to compare groups. Chi-square analysis and Fisher exact test were used for categorical data analysis.
Results
In all 312 subjects were recruited for this study: 188 cases and 124 controls. Table 1 shows the characteristics of the study population. Male gender is more prevalent in the study population (69%). About 74% of the study population was living in the city. The most common diagnosis was pseudoexfoliative glaucoma (44%) followed by primary open-angle glaucoma (POAG) (41%), chronic angle closure glaucoma (CACG) (6%), aphakic glaucoma (4.5%) normal tension glaucoma (4%), and pigmentary glaucoma (0.5%). Twenty-two percent of the population study had a family history of glaucoma in their first degree relatives. Most patients (63%) had no systemic disease. In the study population, 27% of participants had higher educational status, and 70% of them had unskilled or partially skilled occupations.
Table 1.
Characteristics of study population and study factors
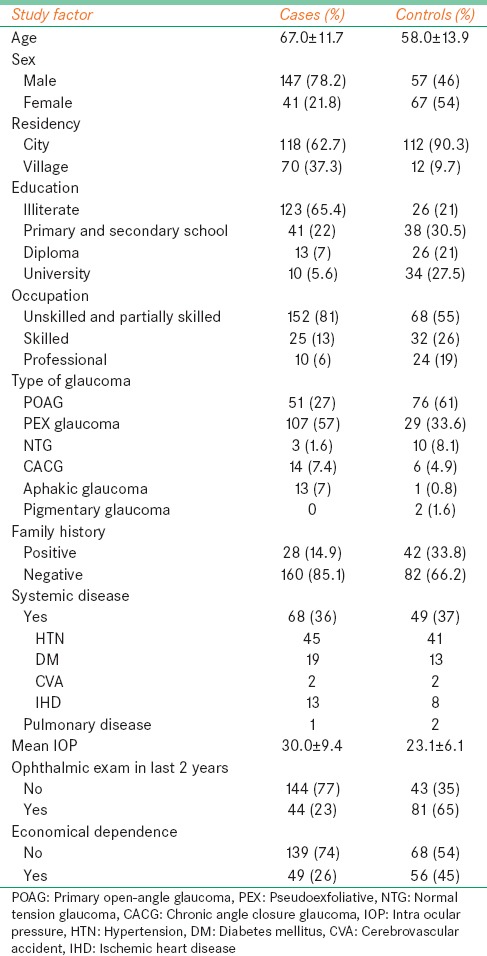
Table 2 shows the estimated effect of each study factor on late presentation. These data provides a strong evidence of an independent association between late presentation and male gender, lower educational status, pseudoexfoliative glaucoma, higher IOP in the first presentation, and no eye exam in last 2 years.
Table 2.
Estimated effect of each study factor on late presentation
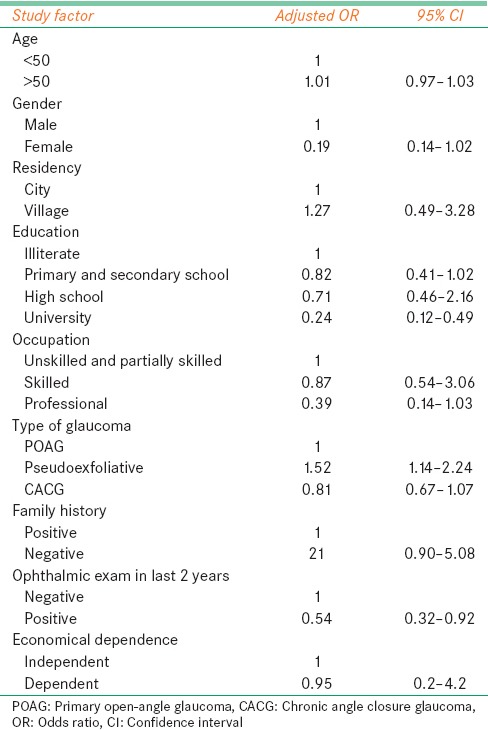
There is a significant association between male gender and late presentation; we estimate a 5 times less odds in female patients for presenting with advanced glaucoma (OR: 0.19 CI: 0.14-1.02, P = 0.034). We estimate a trend of increasing odds for late attendance with decreasing of educational status. Patients with higher educations had 4 times less odds for late presentation as patients who were uneducated (P < 0.0001).
IOP at initial examination was shown to be significantly associated with the high odds of having advanced glaucoma. We estimated a 1.01 (1.03-1.14) increase in the odds of late presentation per increased 1 mmHg in IOPs above 25 mmHg (P = 0.001).
Patients with pseudoexfoliative glaucoma were estimated to 1.5 times (1.14-2.03) more likely to had advanced glaucoma than patients with POAG and CACG (P = 0.004).
No visit by an ophthalmologist in the last 2 years was shown to be strongly associated with late presentation. Patients who were visited by an ophthalmologist in the last 2 years had 1/2 odds to had advanced glaucoma at diagnosis (OR: 0.54 CI: 0.32-0.92, P = 0.025).
Our data provide a little evidence of association between late presentation, and any of the other factors studied.
Discussion
There have been several studies have estimated that 10-33% of people with glaucoma were severely visual impaired at first examination.[1,2,7] Several studies had shown that advanced glaucoma is a major risk factor for blindness from glaucoma.[3,4,8] The published studies indicate that late presentation of glaucoma is an important and not uncommon risk factor for blindness, this study attempts to elucidate risk factors for late presentation of glaucoma in an Iranian population.
Our study estimates that men are more likely to present in the advanced stages of glaucoma than women of similar age, IOP, education, and type of glaucoma. Natural course of glaucoma in men and women is similar, and the prevalence of glaucoma has no difference in men and women, so the most possible explanation for the earlier presentation of women is that rate of medical and health service use is high in women.
Our study shows that higher IOP's are a risk factor for late presentation of glaucoma. We estimate that patients with presenting IOP > 25 mmHg are at greater risk for late presentation. We estimate 1.1 increases in odds in IOP's above 25 mmHg. This finding is consistent with results of other studies that showed that higher IOPs result in more rapid visual field loss and an increased likelihood of late presentation.[1,2,3,9] This implies a relative necessity to achieve target IOP in a shorter time as possible in patients that presented with higher IOP at presentation.
Our results showed that pseudoexfoliative glaucoma is a major risk factor for late presentation; to the best of our knowledge, this is the first study that identifies pseudoexfoliation as a risk factor for late presentation in glaucoma patients. It is believed that pseudoexfoliative glaucoma was managed more difficult clinically.[10] This may be attributed to the clinical characteristics of pseudoexfoliative glaucoma which associated with higher IOP levels and greater diurnal fluctuation in IOP.[11]
Socioeconomic status was shown to be strongly associated with the risk of late attendance.[1,6,12,13] In our study, socioeconomic statuses were measured by the site of inhabitance, occupational category, education, and economic dependency of them; only level of education was shown to be strongly associated with the risk of late presentation. In the previous studies,[2,6,13] there was a significant association between occupational group and late attendance for open-angle glaucoma in our study. The prevalence of lower occupational class was high in case group (81% vs. 51%) but this difference not at significant level (P = 0.055). This may be due to small sample size in occupational subgroups.
In our study, those with negative family history of glaucoma were found to be two-fold (2.1, CI: 0.9-5.08) more likely to present with advanced glaucoma than those with positive family history but this finding not reaches a significant level at multivariant analysis (P = 0.084). There is growing evidence that suggests that glaucoma is a familial disease.[14] As our study, several studies were shown that positive family history is a protective factor for late presentation in glaucoma.[2,6,13] This may be due to increased awareness that needs for glaucoma screening because information most likely passed on from the other members of family. However, it is possible that these data are incomplete since of the participants may be unaware of their family history of glaucoma. Other studies[15] identify the positive family history of glaucoma as a risk factor for more visual field loss at the time of initial diagnosis.
One reason for late presentation in glaucoma is the infrequency of an eye examination. Fraser et al. showed that the longer since the last eye exam was with more likelihood of presentation with advanced glaucoma.[13] Our study also shows that there was a statistically significant association between the lake of eye exam in the last 2 years and the late presentation of open-angle glaucoma. Whether a patient presents with advanced glaucoma is likely to be a function of the rapidity of visual field deterioration and the frequency of the eye exam. For the assessment of the relative influence of these two risk factors in late attendance, a prospective cohort study must be done.
This study is a hospital-based case–control study from a single hospital and has its limitations. One limitation is recalled in the family history of glaucoma and frequency of eye exam; it may produce bias.
Conclusion
Our study showed that certain subgroups of glaucoma were at greater risk for presenting with advanced glaucoma and subsequent blindness. Screening has an important role for reducing advanced disease at diagnosis, but mass public screening is impractical. The most attractive option may be screening of high-risk patients. For detection of risk factors, it needs a prospective and community-based case-control study with higher power to be performed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Fraser S, Bunce C, Wormald R. Risk factors for late presentation in chronic glaucoma. Invest Ophthalmol Vis Sci. 1999;40:2251–7. [PubMed] [Google Scholar]
- 2.Grant WM, Burke JF., Jr Why do some people go blind from glaucoma? Ophthalmology. 1982;89:991–8. doi: 10.1016/s0161-6420(82)34675-8. [DOI] [PubMed] [Google Scholar]
- 3.Jay JL, Murdoch JR. The rate of visual field loss in untreated primary open angle glaucoma. Br J Ophthalmol. 1993;77:176–8. doi: 10.1136/bjo.77.3.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilson R, Walker AM, Dueker DK, Crick RP. Risk factors for rate of progression of glaucomatous visual field loss: A computer-based analysis. Arch Ophthalmol. 1982;100:737–41. doi: 10.1001/archopht.1982.01030030741002. [DOI] [PubMed] [Google Scholar]
- 5.Fraser S, Bunce C, Wormald R. Retrospective analysis of risk factors for late presentation of chronic glaucoma. Br J Ophthalmol. 1999;83:24–8. doi: 10.1136/bjo.83.1.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ntim-Amponsah CT, Amoaku WM, Ewusi RK, Idirisuriya-Khair R, Nyatepe-Coo E, Ofosu-Amaah S. Evaluation of risk factors for advanced glaucoma in Ghanaian patients. Eye (Lond) 2005;19:528–34. doi: 10.1038/sj.eye.6701533. [DOI] [PubMed] [Google Scholar]
- 7.Coffey M, Reidy A, Wormald R, Xian WX, Wright L, Courtney P. Prevalence of glaucoma in the west of Ireland. Br J Ophthalmol. 1993;77:17–21. doi: 10.1136/bjo.77.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen PP. Risk and risk factors for blindness from glaucoma. Curr Opin Ophthalmol. 2004;15:107–11. doi: 10.1097/00055735-200404000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Armaly MF, Krueger DE, Maunder L, Becker B, Hetherington J, Jr, Kolker AE, et al. Biostatistical analysis of the collaborative glaucoma study. I. Summary report of the risk factors for glaucomatous visual-field defects. Arch Ophthalmol. 1980;98:2163–71. doi: 10.1001/archopht.1980.01020041015002. [DOI] [PubMed] [Google Scholar]
- 10.Schlötzer-Schrehardt U, Naumann GO. Ocular and systemic pseudoexfoliation syndrome. Am J Ophthalmol. 2006;141:921–37. doi: 10.1016/j.ajo.2006.01.047. [DOI] [PubMed] [Google Scholar]
- 11.Konstas AG, Stewart WC, Stroman GA, Sine CS. Clinical presentation and initial treatment patterns in patients with exfoliation glaucoma versus primary open-angle glaucoma. Ophthalmic Surg Lasers. 1997;28:111–7. [PubMed] [Google Scholar]
- 12.Eslami Y, Amini H, Zarei R, Fakhrai G, Moghimi S, Mohammadi S, et al. Socioeconomic factors and disease severity at glaucoma presentation. Iran J Ophthalmol. 2011;23:19–26. [Google Scholar]
- 13.Fraser S, Bunce C, Wormald R, Brunner E. Deprivation and late presentation of glaucoma: Case-control study. BMJ. 2001;322:639–43. doi: 10.1136/bmj.322.7287.639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Craig JE, Mackey DA. Glaucoma genetics: Where are we? Where will we go. Curr Opin Ophthalmol. 1999;10:126–34. doi: 10.1097/00055735-199904000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Deva NC, Insull E, Gamble G, Danesh-Meyer HV. Risk factors for first presentation of glaucoma with significant visual field loss. Clin Experiment Ophthalmol. 2008;36:217–21. doi: 10.1111/j.1442-9071.2008.01716.x. [DOI] [PubMed] [Google Scholar]


