Abstract
To reduce the high incidence of cervical cancer among Latinas in the United States it is important to understand factors that predict screening behavior. The aim of this study was to test the utility of theory of planned behavior (TPB) in predicting cervical cancer screening among a group of Latinas. A sample of Latinas (N= 614) completed a baseline survey about Pap test attitudes subjective norms, perceived behavioral control, and intention to be screened for cervical cancer. At six-months cervical cancer screening behavior was assessed. Structural equation modeling was used to test the theory. Model fit statistics indicated good model fit (χ2 (48) = 54.32, p-value = .246; CFI = .992; RMSEA = .015; WRMR =.687). Subjective norms (p = .005) and perceived behavioral control (p < .0001) were positively associated with intention to be screened for cervical cancer, and the intention to be screened predicted actual cervical cancer screening (p<.0001). The proportion of variance (R2) in intention accounted for by the predictors was .276 and the R2 in cervical cancer screening accounted for was .130. This study provides support for the use of the theory of planned behavior in predicting cervical cancer screening among Latinas. This knowledge can be used to inform the development of a TPB-based intervention to increase cervical cancer screening among Latinas and reduce the high incidence of cervical cancer in this group of women.
Keywords: cervical cancer screening, Latinas, theory of planned behavior, prevention, women's reproductive health
Screening for cervical cancer and its precursors is primarily responsible for the decreased incidence and mortality of cervical cancer among women in the United States (Barnholtz-Sloan et al., 2009). While the decline in the incidence of cervical cancer is a positive outcome, closer examination of the incidence rates by ethnicity reveal that Latinas shoulder a disproportionate share of the cervical cancer burden. In fact, the overall incidence of cervical cancer in the U.S. is 8.4 per 100,000 women and the incidence among Latinas is 11.1 per 100,000 women (SEER Cancer Statistics Review 2013; Ward, Roncancio, Cano & Plaxe, 2014). The high incidence of cervical cancer among Latinas can be attributed to a reduced likelihood of undergoing cervical cancer screening (Byrd et al., 2004; Boucher & Schenker, 2002; Selvin & Brett, 2003). For example, using Behavioral Risk Factor Surveillance System data from 1993-2010, researchers found that 11.1% of Latinas reported never having undergone screening compared to 5.0% of non-Hispanic white women and 5.8% of black women (Chen et al., 2012). Increasing cervical cancer screening will increase early diagnosis and treatment, thereby decreasing the incidence and mortality rates of cervical cancer among Latinas. In order to increase cervical cancer screening in Latinas it is essential to identify the factors that predict screening.
The Theory of Planned Behavior (TPB), an extension of the Theory of Reasoned Action, is one of the most widely employed social-cognitive theories used to understand the relationship between intentions and behavior (Conner & Armitage, 1998; Ajzen, 1991; Ajzen, 1985; Ajzen & Fishbein, 1980). The TPB was developed to improve the predictive validity of the Theory of Reasoned Action by incorporating perceived behavioral control (Ajzen, 1991). According to the TPB, the intention to perform a behavior directly predicts engaging in that behavior. Intention, in turn, is predicted by an individual’s attitude toward the behavior, subjective norms, and perceived behavioral control. Further, when an individual’s perceived behavioral control reflects the degree of actual control over engaging in a behavior, perceived behavioral control can directly influence engaging in the behavior. The intention to perform the behavior is an indication of the degree to which an individual is ready to perform a given behavior and actually performing the behavior is the observable response to the behavior. Attitude toward the behavior is defined as the degree to which the individual views engaging in the behavior as positive or negative. The subjective norms construct is defined as the perceived social pressure to engage or not engage in the behavior. Finally, perceived behavioral control is defined as the perceived ability to successfully perform the behavior.
In comparison to similar cognitive-motivational theories such as the Health Belief Model and Protection Motivation Theory, empirical evidence suggests that the TPB is a better predictor of intentions and behavior because its constructs exhibit relatively larger effect sizes (Abraham & Sheeran, 2005; Armitage & Conner, 2001; Conner & Armitage, 1998; Conner & Norman, 2005; Norman, Boer & Seydel, 2005 ). Further, a meta-analysis of 185 studies found that the TPB accounted for 39% of the variance in intentions and 27% of the variance in behavior across a broad spectrum of behaviors; which illustrates its wide applicability across behaviors (Armitage & Conner, 2001). The TPB has been found to predict whether or not an individual engages in a wide variety of different health behaviors including exercise, undergoing a health check-up, being screened for breast and colorectal cancers (Armitage & Conner, 2001; Conner & Armitage, 1998; Forbes, Blanchard, Mummery & Courneya, 2014; Godin et al., 2001; Lee, 2011; Steadman & Rutter, 2004; Vallance, Lavallee, Culos-Reed & Trudeau, 2012).
Few studies have employed the full TPB model, to examine cervical cancer screening behavior among Latinas. One study found that the attitude toward the behavior, subjective norms, and perceived behavioral control predicted Latinas’ intentions to be screened for cervical cancer (Roncancio et al., 2013). However, this study did not examine whether the intention to be screened for cervical cancer predicted actual screening behavior. Other researchers have employed some of the model constructs individually and found that they do predict cervical cancer screening in this population (Fernandez-Esquer & Cardenas-Turanzas, 2004; Jennings-Dozier, 1999). However, to our knowledge, there are no longitudinal studies that have tested the utility of the full TPB model to predict both cervical cancer screening intention and behavior among Latinas. Testing the full TPB model is consistent with recommended theory-testing practices (Noar & Zimmerman, 2005) and represents an important contribution to understanding the determinants of cancer screening among Latinas.
The purpose of the current study is to examine the ability of the TPB to predict cervical cancer screening in Latinas. Consistent with the TPB, we hypothesize that attitude, subjective norms and perceived behavioral control will predict cervical cancer screening intentions and that intentions will predict actual screening behavior among Latinas.
METHODS
Participants and Procedure
Data for the present study were collected as part of an intervention trial examining the effectiveness of a lay health worker delivered intervention to increase cervical cancer screening in Latino women (Byrd et al., 2013). Eligible participants were women of Mexican origin ages 21 or older, with no previous history of cancer, no hysterectomy, and no cervical cancer screening within the past three years. The recommendations of the US Preventive Services Task Force, during the study period, were that women over 21 years of age undergo cervical cancer screening at least once every 3 years. Given that the focus of the larger study was on women (over 21 years of age) who were non-compliant with the US Preventive Services Task Force’s recommended screening guidelines, only women who had not undergone cervical cancer screening in the past three years were eligible to be enrolled into the larger study.
Eligible women who agreed to participate (N= 614) were contacted by an interviewer who administered both the informed consent and the survey. The study was conducted in three sites: El Paso, Texas; Houston, Texas; and Yakima Valley, Washington. All three sites used flyer distribution and in-person recruitment. Participants were recruited at a variety of locations including beauty salons, laundromats, jewelry stores, bakeries, schools, community centers, churches and retail stores. Women responded to a survey about Pap test history and attitudes and beliefs about screening and cervical cancer. Development of the survey instrument was informed by qualitative data collected through thirteen focus group interviews conducted with Latino women (N= 84). The focus groups, conducted during the developmental phase of the larger study, explored beliefs about cervical cancer and screening and cultural barriers to having a Pap test. In addition, the focus groups allowed us to hear the women talk about cervical cancer screening in their own words. The language used by the focus group participants was subsequently incorporated into the survey instrument. The survey was then pilot-tested with 50 women from the population of interest to ensure that the items were understandable and appropriate (Byrd, et al., 2012).
Six months following the baseline interview and administration of the educational intervention (to participants randomized to the intervention condition), participants completed a follow-up interview. The primary outcome was cervical cancer screening measured by self-report on the follow-up survey and validated through a review of medical records. All procedures and measures were approved by the University of Texas Health Science Center-Houston Committee for the Protection of Human Subjects and the Fred Hutchinson Cancer Research Center Institutional Review Board.
Measures
Cervical cancer screening behavior
Being screened for cervical cancer was assessed at 6-month follow-up asking whether or not the participant underwent a Pap test after baseline (1= No and 2 = Yes).
Intentions
The intention to be screened for cervical cancer was measured on the baseline survey and was assessed using one item, “Do you plan to have a Pap test within the next 6 months?” with response options: 1= No and 2= Yes.
Attitudes
Attitudes toward cervical cancer screening was measured using three items. The response scale ranged from 1 (Strongly disagree) to 5 (Strongly agree). The items were, ‘A Pap test is painful.’ ‘Getting a Pap test would only make me worry.’ and ‘It is too embarrassing to have a Pap test.’
Subjective Norms
Subjective norms toward cervical cancer screening were assessed through three items, ‘My family thinks I should have regular Pap tests.’ ‘My closest friend thinks I should have regular Pap tests.’ and ‘My doctor thinks I should have regular Pap tests’. The response scale ranged from 1 (Strongly disagree) to 5 (Strongly agree).
Behavioral Control
Perceived behavioral control over cervical cancer screening was assessed by three items, ‘How sure are you that you can go get your next Pap test?’ ‘How sure are you that you can schedule a Pap test appointment and keep it?’ and ‘How sure are you that you can keep having Pap tests, even if you had to go to a new office in order to get one?’ The response scale ranged from 1 (Not at all sure) to 5 (Completely sure).
Data Analysis
Descriptive statistics were derived using SPSS 20.0 for Windows (Chicago, IL). In general, between 0% and 5.5% of the data on each of the variables were missing. Means, standard deviations, skewness, and kurtosis indices were examined for the variables. All subsequent analyses were conducted using structural equation modeling (SEM) and the software program Mplus version 5.1 (Los Angeles, CA).
General guidelines for determining adequate sample size for testing SEM models consider a sample size of 100-200 to have adequate power (Kline, 2005; Loehlin, 2004). Thus, our sample size of 614 was determined to have sufficient power to test our model. Variance-adjusted least squares estimator (WLSM) was employed to test the model. The fit of the model was evaluated through the examination of several fit indices: 1. Chi-Square (low value and non-significant p-value is desired), 2. the comparative fit index (CFI; values greater than .90 indicate good fit), 3. the weighted root mean square residual (WRMR; values <.90 indicate good fit), and 4. the root-mean-square residual (RMSEA; values ≤.05 indicate good fit).
RESULTS
The mean age of the participants was 43.02 years (SD = 9.77) and the mean number of years of education was 8.33 years (SD= 3.97). Other sample demographics are presented in Table 1. The initial model estimated included the variables: attitude toward screening, subjective norms, and perceived behavioral control, as predictors of the intention to be screened and intention and perceived behavioral control as predictors of cervical cancer screening behavior. In addition, intervention status (i.e., control vs. intervention) and study site as predictors of cervical cancer screening behavior were included in order to control for their effects. Model fit statistics were: χ2 (58) = 149.19, p-value < .001; CFI = .898; RMSEA = .051; WRMR = 1.116. The fit statistics indicated adequate model fit and all of the indicators loaded significantly onto their respective latent variables (attitude, subjective norms, and perceived behavioral control). All path coefficients were significant except for the paths from: 1. study site to cancer screening (p = .310), 2. attitude to intention (p = .295), and 3. perceived behavioral control to cancer screening (p = .099). Given that the model proposed by Ajzen (Ajzen, 1991) includes attitude as a predictor of intention and perceived behavioral control as a predictor of behavior (to the extent that perceived behavioral control reflects actual control) these paths were retained in the model. Given its non-significant association with cancer screening behavior and also the fact that it is not a component of the TPB as described by Ajzen (Ajzen, 1991), study site was removed from the model to maintain parsimony.
Table 1.
Demographic characteristics of the sample (N=614)
| N (%) | |
|---|---|
| Marital Status | |
| Single, never married | 74 (12.1) |
| Married or living with partner | 421 (68.6) |
| Separated, divorced, or widowed | 119 (19.5) |
| Education | |
| Less than high school completed | 423 (84.6) |
| Completed high school | 77 (15.4) |
| Nativity | |
| Foreign born | 538 (87.7) |
| U.S. born | 76 (12.4) |
| Health Insurance | |
| Yes | 111 (18.1) |
| No | 499 (81.3) |
| Unsure | 4 (0.7) |
| Language Spoken | |
| Spanish | 591 (96.3) |
| English | 23 (3.7) |
Frequencies that do not sum to total represent missing data.
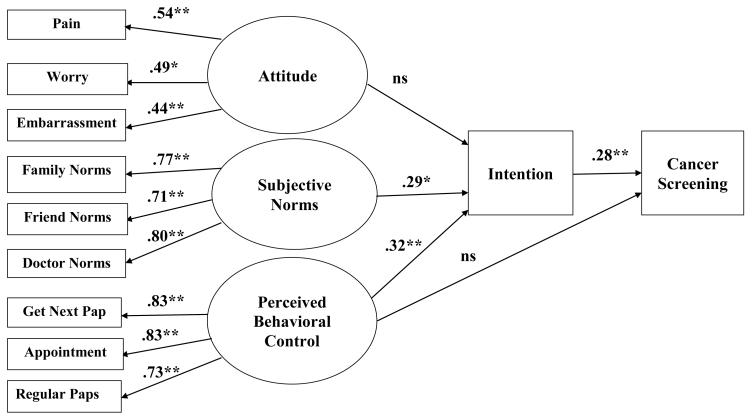
The new model was then estimated. Model fit statistics were: χ2 (48) = 54.32, p-value = .246; CFI = .992; RMSEA = .015; WRMR =.687. The fit indices indicated improved model fit compared to the initial model estimated and all path coefficients were significant except for the path from attitude to intention (p = .245) and the path from perceived behavioral control to cancer screening (p = .086) (see Figure 1). Factor loadings for the indicators of the latent variables attitude, subjective norms, and perceived behavioral control were all significant (see Figure 1). Subjective norms (p = .005) and perceived behavioral control (p < .0001) were positively associated with intention, and intention predicted actual cervical cancer screening (p< .0001). In addition, intervention status was included in the model to control for its effects. Women who received the intervention were more likely to be screened for cervical cancer compared to those who did not (p-value < .0001). Path coefficients are interpreted in the same manner as regression coefficients. For example, each 1 point increase in subjective norms is associated with a .29-point increase in the intention to be screened. The proportion of variance (R2) in intention accounted for by the predictors was .276 and the R2 in cervical cancer screening accounted for by its predictors was .130.
Figure 1.
Structural model of the TPB predicting cervical cancer screening among Latinas. Model fit indices: χ2 (48) = 54.32, p-value= .246; CFI= .992; RMSEA=.015 (.000, .032); WRMR= .069; Intention R2 = .28; Cancer Screening R2 = .13. The model also included Intervention group (i.e., control vs. intervention) as a covariate predicting Cancer Screening to control for its effects (.52, p <.001).
* p-values are significant at < .05; **p-values are significant at ≤ .001; ns= non-significant path
DISCUSSION
The current study examined the utility of TPB in predicting cervical cancer screening in a sample of Latinas who had not been screened in the last three years. One strength of the study was the longitudinal nature of the data which allowed us to examine the relationship between screening intentions and screening behavior. We found support for the TPB in predicting cervical cancer screening in this population. To our knowledge, this is the first study to employ the full TPB to predict both intentions and cervical cancer screening behavior among Latinas.
Our findings are consistent with studies that have employed components of the TPB to predict cervical cancer screening in other female populations (Jennings-Dozier, 1999; Fernbach, 2002; Sheeran & Orbell, 2000) and studies employing the TPB to predict screening intentions in Latinas (Roncancio et al., 2013). We found that perceived behavioral control was the strongest predictor of intention such that women with higher perceived behavioral control expressed greater intentions to be screened for cervical cancer. This suggests the need for interventions to increase Latinas’ sense of control over undergoing screening. Subjective norms was the second strongest predictor of intention in that those women who more strongly endorsed that their family, friends, and doctor expected them to be screened for cervical cancer expressed stronger intention to be screened for cervical cancer. As such, interventions should include messages that strengthen Latinas’ beliefs that people who are important to them expect them to undergo screening. Further, we found that those who expressed the intention to be screened for cervical cancer were more likely to be screened. This indicates that interventions that successfully increase intentions may positively impact screening behavior among Latinas. This should be further explored through the development and implementation of TPB-based interventions for this population. Overall, our findings provide support for the TPB’s predictive ability of Latinas behavior and its potential utility as an intervention to increase cervical cancer screening among Latinas. The next step in this research area is to review the focus group data collected and identify the salient control beliefs and normative beliefs that are associated with perceived behavioral control and subjective norms and develop strategies and messages to increase or reinforce these beliefs in order to increase intentions and screening behavior.
Consistent with previous research in college age women (Duffett-Leger et al., 2008), we found attitude toward screening did not predict the intention to be screened. This finding is informative regarding the application of the TPB to this behavior and population since Ajzen (Ajzen, 1991) stated that the relative influence of each component of the TPB can vary depending on the behavior and population in question. In fact, previous research among Latinas has found that reported attitudes toward screening such as feeling that Pap tests are embarrassing do not predict previous cervical cancer screening (Behbakht et al., 2004). Further, in the current study, relatively fewer women expressed negative attitudes or concerns about being screened. The more positive attitudes could be related to the fact that while all of the women in the study were overdue for screening, the majority of them (89.4%) had previously undergone screening. Previous research has found that women who have never been screened for cervical cancer are more likely to endorse the attitudes that Pap tests are painful and/or embarrassing compared to women who have been screened in the past (Byrd et al., 2004). This finding indicates that for women who have previously been screened, interventions based on the TPB might be more effective if they focus on changing perceived behavioral control and subjective norms toward screening. Researchers should further investigate these differences in attitudes toward screening in Latinas who have previously been screened and those who have never been screened as these two groups may require different intervention messages.
In addition, perceived behavioral control did not directly predict screening among the Latinas in our study. According to Ajzen (Ajzen, 1991) this implies that, in this population, perceived behavioral control is not an accurate reflection of the extent to which cervical cancer screening is actually under the women’s control. This is an important finding that suggests the need to further explore and identify factors that increase actual behavioral control. These may include environmental or demographic factors such as a lack of health insurance (Rodriguez et al., 2005), income(Ackerson & Gretebeck, 2007), or knowledge of how to negotiate the healthcare system. Once identified, TPB-based interventions can address these factors and thus increase screening behavior among Latinas.
While this study provides important information, it is not without its limitations. Since this is the first study to examine the utility of the TPB in predicting cervical cancer screening in Latinas, further model testing should be conducted to verify that the model is appropriate for explaining this behavior in Latinas. Also, foreign-born women were overrepresented in the current sample (87.7%) and as such it is possible that the strength and or significance of the TPB predictors could vary among U.S. born Latinas. Finally, the TPB is a cognitive model that assumes that behavioral decisions are both rationally made and primarily under the volitional control of the individual. As illustrated by the current finding that perceived behavioral control did not directly predict screening, it appears that there may be other factors that influence the actual behavioral control these women have over being screened. Identification of these factors will increase the effectiveness of the TPB in both predicting and encouraging screening among Latinas.
This study provides support for the use of theory-based models in predicting cervical cancer screening among Latinas. This knowledge can contribute to the development of a TPB-based intervention to increase screening in Latinas. Given that theory-based interventions are more effective than non-theory-based interventions (Glanz & Bishop, 2010), this is an important line of research to continue in order to reduce cervical cancer-related health disparities in this population.
ACKNOWLEDGEMENTS
Research for this publication was supported by: the Centers for Disease Control and Prevention cooperative agreement U48-DP000057; NIH/NCI grants 1K01CA181437, U54CA153505 & R25T CA57730; and the National Institute on Drug Abuse R25 DA026401.
References
- Abraham C, Sheeran P. The health belief model. In: Conner M, Norman P, editors. Predicting Health Behaviour: Research and Practice with Social Cognition Models. Open University Press; Berkshire, England: 2005. pp. 28–80. [Google Scholar]
- Ackerson K, Gretebeck K. Factors influencing cancer screening practices of underserved women. Journal Of The American Academy Of Nurse Practitioners. 2007;19:591–601. doi: 10.1111/j.1745-7599.2007.00268.x. [DOI] [PubMed] [Google Scholar]
- Ajzen I. From Intentions to Actions: A Theory of Planned Behavior. In: Kuhl J, Beckmann J, editors. Action Control. Springer; Berlin Heidelberg: 1985. pp. 11–39. [Google Scholar]
- Ajzen I. The theory of planned behavior. Organizational Behavior & Human Decision Processes. 1991;50:179–211. [Google Scholar]
- Ajzen I, Fishbein M. Understanding Attitudes and Predicting Social Behavior. Englewood Cliffs: Prentice-Hall; Uppper Saddle River, NJ: 1980. [Google Scholar]
- Armitage CJ, Conner M. Efficacy of the Theory of Planned Behaviour: A meta-analytic review. British Journal of Social Psychology. 2001;40:471. doi: 10.1348/014466601164939. [DOI] [PubMed] [Google Scholar]
- Barnholtz-Sloan J, Patel N, Rollison D, Kortepeter K, MacKinnon J, Giuliano A. Incidence trends of invasive cervical cancer in the United States by combined race and ethnicity. Cancer Causes & Control: CCC. 2009;20:1129–1138. doi: 10.1007/s10552-009-9317-z. [DOI] [PubMed] [Google Scholar]
- Behbakht K, Lynch A, Teal S, Degeest K, Massad S. Social and Cultural Barriers to Papanicolaou Test Screening in an Urban Population. Obstetrics & Gynecology. 2004;104:1355–1361. doi: 10.1097/01.AOG.0000143881.53058.81. [DOI] [PubMed] [Google Scholar]
- Boucher F, Schenker MB. Cervical cancer among Hispanic women: assessing the impact on farmworkers. Journal Of Immigrant Health. 2002;4:159–165. doi: 10.1023/A:1015603018296. [DOI] [PubMed] [Google Scholar]
- Byrd TL, Peterson SK, Chavez R, Heckert A. Cervical cancer screening beliefs among young Hispanic women. Preventive Medicine. 2004;38:192. doi: 10.1016/j.ypmed.2003.09.017. [DOI] [PubMed] [Google Scholar]
- Byrd TL, Wilson KM, Smith JL, Heckert A, Orians CE, Vernon SW, et al. Using intervention mapping as a participatory strategy: Development of a cervical cancer screening intervention for Hispanic women. Health Education & Behavior. 2012;39(5):603–611. doi: 10.1177/1090198111426452. [DOI] [PubMed] [Google Scholar]
- Byrd TL, Wilson KM, Smith JL, Coronado G, Vernon SW, Fernandez-Esquer ME, et al. AMIGAS: A multicity, multicomponent cervical cancer prevention trial among Mexican American women. Cancer. 2013;119:1365–1372. doi: 10.1002/cncr.27926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen HY, Kessler C, Mori N, Chauhan SP. Cervical Cancer Screening in the United States, 1993-2010: Characteristics of Women Who Are Never Screened. Journal of Women's Health (15409996) 2012;21:1132–1138. doi: 10.1089/jwh.2011.3418. [DOI] [PubMed] [Google Scholar]
- Conner M, Armitage CJ. Extending the Theory of Planned Behavior: A Review and Avenues for Further Research. Journal of Applied Social Psychology. 1998;28:1429–1464. [Google Scholar]
- Conner M, Norman P. Predicting health behaviour: a social cognition approach. In: Conner M, Norman P, editors. Predicting Health Behaviour: Research and Practice with Social Cognition Models. Open University Press; Berkshire, England: 2005. pp. 1–27. [Google Scholar]
- Duffett-Leger LA, Letourneau NL, Croll JC. Cervical cancer screening practices among university women. JOGNN: Journal of Obstetric, Gynecologic & Neonatal Nursing. 2008;37:572–581. doi: 10.1111/j.1552-6909.2008.00276.x. [DOI] [PubMed] [Google Scholar]
- Fernandez-Esquer ME, Cardenas-Turanzas M. Cervical cancer screening among Latinas recently immigrated to the United States. Preventive Medicine. 2004;38:529–535. doi: 10.1016/j.ypmed.2003.12.009. [DOI] [PubMed] [Google Scholar]
- Fernbach M. The Impact of a Media Campaign on Cervical Screening Knowledge and Self-efficacy. Journal of Health Psychology. 2002;7:85. doi: 10.1177/1359105302007001656. [DOI] [PubMed] [Google Scholar]
- Forbes C, Blanchard C, Mummery W, Courneya K. A comparison of physical activity correlates across breast, prostate and colorectal cancer survivors in Nova Scotia, Canada. Supportive Care in Cancer. 2014;22(4):891–903. doi: 10.1007/s00520-013-2045-7. [DOI] [PubMed] [Google Scholar]
- Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annual Review Of Public Health. 2010;31:399–418. doi: 10.1146/annurev.publhealth.012809.103604. [DOI] [PubMed] [Google Scholar]
- Godin G, Gagne C, Maziade J, Moreault L, Beaulieu D, Morel S. Breast cancer: The intention to have a mammography and a clinical breast examination-application of the theory of planned behavior. Psychology & Health. 2001;16:423. [Google Scholar]
- Jennings-Dozier K. Perceptual determinants of Pap test up-to-date status among minority women. Oncology Nursing Forum. 1999;26:1327–1333. [PubMed] [Google Scholar]
- Kline RB. Principles and Practice of Structural Equation Modeling. The Guilford Press; New York: 2005. [Google Scholar]
- Lee H. The role of descriptive norm withing the theory of planned behavior in predicting Korean Americans' exercise behavior. Psychological Reports. 2011;109(1):208–218. doi: 10.2466/06.07.PR0.109.4.208-218. [DOI] [PubMed] [Google Scholar]
- Loehlin JC. Latent Variables Models. The Guilford Press; New York: 2004. [Google Scholar]
- Noar SM, Zimmerman RS. Health Behavior Theory and Cumulative Knowledge regarding Health Behaviors: Are We Moving in the Right Direction? Health Education Research. 2005;20:275–290. doi: 10.1093/her/cyg113. [DOI] [PubMed] [Google Scholar]
- Norman P, Boer H, Seydel ER. Protection Motivation Theory. In: Conner M, Norman P, editors. Predicting Health Behaviour: Research and Practice with Social Cognition Models. Open University Press; Berkshire, England: 2005. pp. 81–126. [Google Scholar]
- Rodriguez MA, Ward LM, Perez-Stable EJ. Breast and cervical cancer screening: impact of health insurance status, ethnicity, and nativity of Latinas. Annals Of Family Medicine. 2005;3:235–241. doi: 10.1370/afm.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roncancio AM, Ward KK, Fernandez ME. Understanding cervical cancer screening intentions among Latinas using an expanded theory of planned behavior model. Behavioral Medicine (Washington, D.C.) 2013;39:66–72. doi: 10.1080/08964289.2013.799452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SEER Cancer Statistics Review, 1975-2010 [based on November 2012];SEER [On-line] 2013 Available: http://seer.cancer.gov/csr/1975_2010/ SEER data submission, posted to the SEER web site.
- Selvin E, Brett KM. Breast and Cervical Cancer Screening: Sociodemographic Predictors Among White, Black, and Hispanic Women. American Journal of Public Health. 2003;93:618–623. doi: 10.2105/ajph.93.4.618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheeran P, Orbell S. Using implementation intentions to increase attendance for cervical cancer screening. Health Psychology. 2000;19:283–289. doi: 10.1037//0278-6133.19.3.283. [DOI] [PubMed] [Google Scholar]
- Steadman L, Rutter DR. Belief importance and the theory of planned behaviour: Comparing modal and ranked modal beliefs in predicting attendance at breast screening. British Journal of Health Psychology. 2004;9:447–463. doi: 10.1348/1359107042304579. [DOI] [PubMed] [Google Scholar]
- Vallance JK, Lavallee C, Culos-Reed NS, Trudeau MG. Predictors of physical activity among rural and small town breast cancer survivors: An application of the theory of planned behaviour. Psychology, Health & Medicine. 2012;17(6):685–697. doi: 10.1080/13548506.2012.659745. [DOI] [PubMed] [Google Scholar]
- Ward KK, Roncancio AM, Cano MA, Plaxe S. An ecological analysis of the incidence of invasive squamous cell carcinoma of the cervix in Hispanic women in the United States. Ethnicity & Disease. 2014;24(2):243–247. [PMC free article] [PubMed] [Google Scholar]