Abstract
Background
This retrospective study aims to present and evaluate the long follow-up results of posterior instrumentation without fusion in patients with traumatic thoracic and lumbar fractures.
Methods
45 patients were operated. The mean follow-up period was 147.6 months. Sagittal plane kyphosis (SPK) and anterior wedge angle (AWA) were evaluated in preoperative and follow-up.
Results
SPK and AWA improved significantly in the early postoperative. However, the correction was lost in the 10-year follow-up. The loss of correction was statistically significant in SPK and AWA.
Conclusion
Posterior instrumentation without fusion is still among the most useful in treatment of traumatic thoracolumbar fractures.
Keywords: Lumbar vertebrae, Outcome assessment, Spinal fractures, Thoracic vertebrae
1. Introduction
Conservative treatment is the method of choice for some patients who present with traumatic thoracic and lumbar fractures.1, 2 Although surgical treatment of thoracic and lumbar fractures still remains controversial, posterior decompression and stabilization of the spine is the preferred treatment method for those patients who need a surgical operation.3, 4 Several authors have reported the follow-up results of the posterior instrumentation of traumatic thoracic and lumbar fractures.5, 6 However, there is no series in the literature presenting long-term follow-up results. In addition, presently there is not enough data available for patients treated with fixation and decompression without fusion, although some good clinical outcomes have been reported for short-segment fixation without fusion.7 The present study was designed to evaluate the outcome of thoracolumbar burst fractures managed with posterior fixation, without laminectomy and fusion.
2. Materials and methods
From November 1989 to December 1996, 118 patients with traumatic thoracic and lumbar spine fractures were operated using posterior instrumentation at the Orthopedics and Traumatology Department. Eventually, 45 patients were included in the study because some patients had died or moved to another city and communication was lost with them over the 10-year follow-up period. Thirty patients were male (66.7%), and 15 patients were female (33.3%). Their mean age at the time of surgery was 30.1 years (range, 15–65), and after the 10-year follow-up period, their mean age was 42.4 years (range, 29–79); the mean follow-up period was 147.6 months (range, 128–204). The cause of injury was falling from heights in 24 cases (53.3%), traffic accidents in 19 cases (42.2%), and trauma originating from industrial accidents in two cases (4.4%).
In the study, both Denis and Magerl classifications were used to classify the fractures. According to the Denis classification, 23 patients had burst fractures (type A: 7, type B: 11, type C: 1, type D: 4), 18 had flexion-distraction fractures, and four had fracture-dislocations. There were 19 patients (42.2%) with type A fractures, 18 (40%) with type B type fractures, and eight (17.8%) with type C fractures according to the Magerl classification. Complete spinal cord injury was seen in 36.8% of type A fracture patients, 44.4% of type B, and 75% of type C. Fractures between T4 and L5 were included. Regarding the levels of fractures, there were 25 thoracolumbar fractures (T1 and L1) (55.7%), eight thoracic fractures (17.8%), eight lumbar fractures (17.8%), and four segmental fractures (8.9%).
Complete spinal cord injury was seen in 75% of the thoracic fracture patients, 48% of the thoracolumbar fracture patients, and 25% of the lumbar fracture patients. The American Spinal Injury Association (ASIA) classification was used for functional evaluation, and there were 21 grade A, three grade B, seven grade C, five grade D, and nine grade E cases preoperatively.
All patients underwent posterior instrumentation without fusion. The Harrington distraction system was used as an instrumentation system in seven cases (15.6%) and transpedicular screw fixation was used in 37 cases (84.4%). Four patients were instrumented in two segments, 10 in three segments, 19 in four segments, nine in five segments, and three in six or more segments. Decompression was performed in 11 patients when the canal was severely obliterated by bone fragments. All patients were mobilized postoperatively with thermoplastic thoracolumbar orthosis or a thoracolumbar corset.
2.1. Imaging and function evaluation
In all cases, preoperative, early postoperative, and 10-year follow-up X-rays were taken and computed tomography (CT) scans were performed. Sagittal plane kyphosis (SPK) and anterior wedge angle (AWA) were evaluated in preoperative, early postoperative, and 10-year follow-up sagittal plane X-rays using Cobb's method (Fig. 1). The anterior wedge angle (AWA) was measured from the endplates of the injury level. Spinal canal diameter was measured on the axial cuts of CT scans at the injury level, preoperatively and postoperatively (X). The calculated vertebral spinal canal diameter (Y) was determined by averaging the spinal canal diameters of the adjacent vertebrae above and below the injury level (Y1 and Y2). The spinal canal narrowing percent (NR) was thus calculated as (Y − X)/Y × 100%. For functional evaluation, the Hannover spine score and the Oswestry disability score were used.
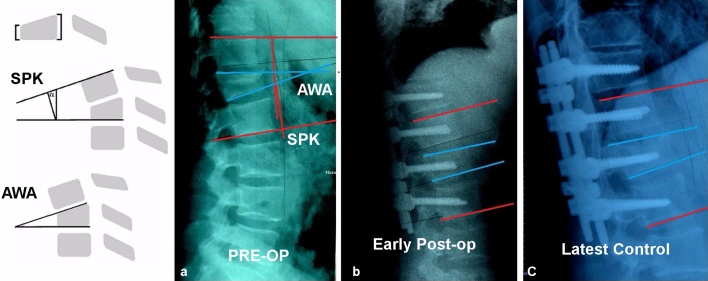
Fig. 1.
L1 fracture ASIA E with anterior column compression treated with pedicle fixation without fusion, preoperatively (a), postoperatively (b), and 10 years after (SPK and AWA measurements).
2.2. Statistical analysis
R 3.2.2. for Windows package program used for statistical analysis. Descriptive statistics are given with mean, standard deviation, median, minimum and maximum values for continuous variables. Shapiro–Wilk test used for test of normality. Wilcoxon test used for comparisons of dependent variables values between two different times one way repeated measures ANOVA used for comparisons of dependent variables values among three different times. After ANOVA for significant variables LSD post hoc test used. For all statistical comparisons with a p value below 0.05 assumed as there is a statistically significance.
3. Results
After the 10-year follow-up period, the ASIA classification for 15 cases was grade A, no case was grade B, three were grade C, 15 were grade D, and 12 were grade E. In the 10-year follow-up period, 27 patients (60%) remained in the preoperative ASIA grade, eight patients (17.8%) improved one grade, seven patients (15.6%) improved two grades, and three patients (6.7%) improved three grades. Overall, a 0.7-grade improvement was seen for the patients.
3.1. Radiological results
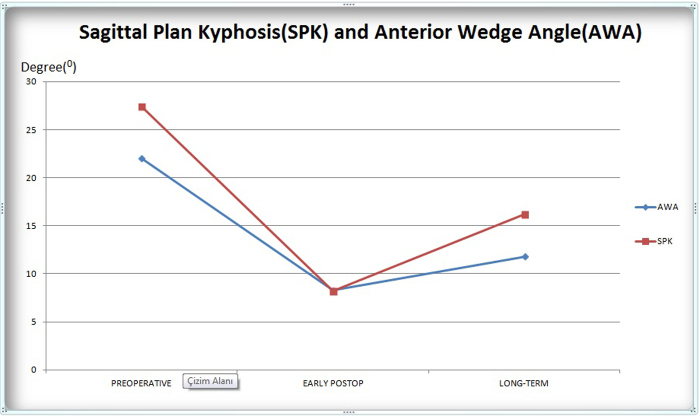
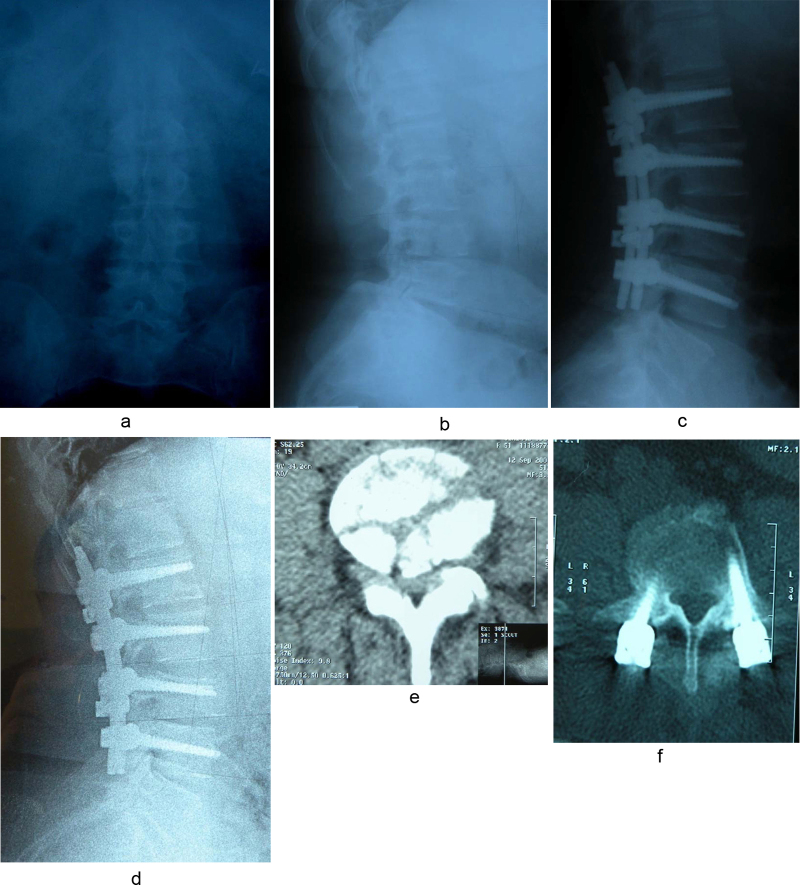
All the changes of the SPK and AWA angles were found statistically significant (p < 0.001). Early and late postoperative values were found significantly increased while significant correction lost was found in late postoperative SPK and AWA angles when compared with early postoperative period (p < 0.001)(Fig. 2). The change in canal narrowing values was statistically significant in preoperative and late postoperative period (p < 0.001). The mean percentage of preoperative narrowed canal diameter was 48.64 ± 14.05% changed to 8.2 ± 4.61% postoperative and the change was found statistically significant (Fig. 3; Table 1).
Fig. 2.
Change in mean SPK and AWA during follow-up period.
Fig. 3.
Comparison of the preoperative (a) and postoperative (b) canal diameter in CT: the average calculated normal canal diameter at the injury level was 18.0 mm. The corresponding preoperative value was 12.6 mm for a spinal canal narrowing percent of 30%. The latest follow-up values showed that the canal diameter was restored, on average, to 16.2 mm at the injury level. On average, the middle sagittal diameter increased 3.6 mm with reduction.
Table 1.
Preoperative, early postoperative, and 10-year follow-up SPK, AWA, and canal narrowing results.
| Patients (n: 45) | Preoperative | Early postoperative | Last control | p |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | ||
| Med (Min–Max) | Med (Min–Max) | Med (Min–Max) | ||
| aSPK (°) | 27.42 ± 9.34 | 8.20 ± 4.69 | 16.26 ± 3.04 | <0.001 |
| 30 (3–46) | 6 (3–20) | 16 (7–37) | ||
| aAWA (°) | 22.04 ± 7.08 | 8.31 ± 4.39 | 11.8 ± 2.98 | <0.001 |
| 24 (10–33) | 7 (2–18) | 11 (9–25) | ||
| bCanal narrowing (%) | 48.64 ± 14.05 | 8.2 ± 4.61 | <0.001 | |
| 48 (20–80) | 16 (0–16) | |||
One way ANOVA on repeated measures.
Wilcoxon test.
3.2. Clinical results
In functional evaluation, regarding all patients, the mean Hannover score was 74.8 ± 12.48 (range, 35–97). In 30 non-wheelchair patients, the mean Oswestry score was 21.69 ± 13.79% (10–60%). Fifteen patients were immobile or in a wheelchair. Shortcomings of this study are the diversity of instrumentation methods used and the small number of patients with 10-year follow-up.
The back pain of the patients who were operated on measured using visual analogue scale (VAS) score in the 10-year follow-up was zero in 30 patients (66.6%), and the mean VAS score was 1.02 ± 1.36 (0–7). Of these 30 patients, 19 still have implants. There was no statistical correlation between fracture type, fracture level, implant type, implant removal, and VAS score.
3.3. Complications
In a 10-year duration, implants were removed from 16 patients (35.6%). Mean implant removal time was 2.8 years. Implant failure was seen in five of 29 patients; these implants were not removed. Two rod fractures, one screw fracture, one screw distortion, and one nut loosening were seen in these five patients. Short segment stabilization was performed on three of these five patients.
4. Discussion
Surgical treatment of thoracolumbar burst fractures includes direct decompressive procedures combined with fusion. These procedures can be performed anteriorly, posteriorly, or combined anterior–posterior.8 There are also procedures including fixation and indirect reduction without fusion.7 Fixation and indirect reduction without fusion was not considered as standard surgical method because it is believed that this method is not enough strong and stable. However, some studies published good results with this method.7, 9 Moreover, minimally invasive and percutaneous indirect reduction and fixation methods were reported.10, 11 Surgical treatment of burst fractures also includes laminectomy; however, laminectomy may cause instability.12 Additionally, fusion methods may result in adjacent level diseases such as spinal nerve damage.13 Chou et al. divided the surgical treatment of thoracolumbar burst fractures into two groups according to the performance of fusion and followed up these patients for 10 years and found that fusion was not necessary.14
Experimental studies conducted on animals showed that early decompression was useful. After respiratory and hemodynamic stabilization, it is possible to perform surgical procedure in spinal cord injured patients in the first 24 h.15 For thoracolumbar burst fracture patients with neurological deficits, direct decompression before reduction should be considered; however, Yang et al. previously confirmed the immediate improvement of canal diameter achieved by indirect reduction with short segment pedicle screw fixation without fusion within two weeks postoperatively.16 Mouchaty et al. reported neurological improvement in 33.3% of patients with complete neurological deficit (ASIA A) and in 64.7% with incomplete neurological deficit (ASIA A, B, C, and D).17 In the results of the present study, out of 21 patients with complete spinal injury, six improved (28.5%), and of 15 patients with incomplete spinal injury, 12 improved (80%). Neurological status at admission was a reliable prognostic factor according to these studies. Good results were expected in patients with mild or moderate deficits. Neurological improvement is related to initial neurological status.
In radiological evaluation, changes in SPK, AWA and canal diameter were measured. All three measurements are related to the sagittal plane and are also good indicators of developing deformity. Yang et al. stated significant improvement in SPK and AWA for patients with indirect reduction without fusion.18 In the current study, SPK and AWA significantly improved in the early postoperative period. However, the correction obtained by surgery was lost in the 10-year follow-up period. This situation is an important finding of this study. The loss of correction was statistically significant in SPK and AWA. Chou et al. compared patients with fusion and without fusion and found progression in SPK and AWA in both groups. Similar to our findings, they also found significant loss in both groups in long-term follow-up and no difference between two groups.13 The same phenomenon was also reported in loss of correction with either fusion.19, 20 Wang et al. concluded that the collapse of the disc space was the major contributor to the loss of correction,21 or this may be due to loss of height in vertebral corpus. Considering these publications, in long-term follow-up, residual kyphotic deformity may develop in these patients; however, this may not change clinical results negatively. Moreover, these three radiological parameters are related to each other in sagittal plane, and significant improvement in all parameters is supposed. Radiological improvement in all parameters was performed with indirect reduction without fusion by ligamentotaxis in the posterior longitudinal ligament.
Canal narrowing produced by fragments of the vertebral corpus after posterior instrumentation in the long-term follow-up was evaluated by CT. Vornanen et al. found enlargement in canal diameter in all cases using different instrumentation systems.22 Intensive decompression may cause enlargement in canal diameter, independent of the instrumentation system. A reduction of retropulsed fragments in the canal is necessary for neurological improvement according to some authors.23 However, in daily practice, there is no relation between neurological deficit at the beginning and narrowing of canal diameter. Edema, hematoma, and disc fragments are the other causes of neurological deficit. In this series, the narrowed spinal canal diameter was found 48.64 ± 14.05% changed to 8.2 ± 4.61% and this finding statistically significant. This increase is statistically significant and not related to fracture level, fracture type, and the implant used. If there is no neurologic deficit after trauma, extra effort should not be spent in removing bone fragments from the canal. Dai et al. reported no correlation between canal diameter and neurologic deficits at admission and neurological recovery in 87 thoracolumbar fracture patients treated surgically and conservatively.24 These findings are in accordance with other studies in the literature. In this study, at upper levels, a little narrowing after a fracture caused neurological deficits. In the present study, at the cord level, the fractures caused a complete lesion in 75% of cases; at the conus level, they caused complete lesion in 48% of cases; and at the cauda equina level, fractures caused complete lesion in 25% of cases. Thus the level of fracture and narrowing segment is extremely important for developing neurological deficits.
Knop et al. found a Hannover score of 64.4 in the long-term period in 29 thoracolumbar fracture patients treated by posterior instrumentation and fusion.25 Andress et al. found a Hannover score of 81.7 in the long term in burst type thoracolumbar fracture patients who had no neurological deficit.3 The Hannover score was 74.8 (35–97) in our series. The results of all the studies that consider Hannover scores are similar. Nevertheless, no correlation between Hannover score and radiological or computed tomographic findings was found.
In this study, four patients were treated by short segment instrumentation. One of them was revised in the first week postoperative, and another was revised in the first month. In the long-term follow-up period, in three of these four patients, implant insufficiency was detected, and in one of them, kyphotic deformity resembling preoperative deformity was found. One of these patients had an L2 fracture, two had L3 fractures, and one had an L4 fracture. Yang et al., at mid-term follow-up, found sufficient correction by short-segment instrumentation.26 Wang et al. found no difference regarding the loss of correction between fusion and no fusion in the short term in thoracolumbar fractures treated with short-segment instrumentation.27 If it is sufficient, short segment instrumentation may be preferred. It is important to prevent motion of the vertebral column by including the fewest sufficient segments in stabilization.
Spontaneous fusion and facet joint changes are other important issues. Gardner and Armstrong reported no spontaneous fusion and facet joint change in 20 cases instrumented with the Harrington system without fusion.28 Akbarnia et al. reported physiological mobility in dynamic and oblique radiography in 86 joint levels out of 88 levels instrumented without fusion.29 In this study of 45 cases instrumented without fusion, intervertebral fusion was reported in two cases, and posterior fusion was reported in another two cases.
5. Conclusion
Posterior instrumentation without fusion for patients with traumatic thoracic and lumbar fractures is still one of the most useful and preferred procedures. Instability and compression of the spinal cord are the outstanding criteria for deciding on surgical intervention. Early decompression and stabilization of the spine were important factors for improvement with slight or no neurological deficits. Fusion should be included in the operative procedure in limited instances, but it should not be used routinely.
Conflicts of interest
The authors have none to declare.
References
- 1.Altay M., Ozkurt B., Aktekin C.N., Ozturk A.M., Dogan O., Tabak A.Y. Treatment of unstable thoracolumbar junction burst fractures with short- or long-segment posterior fixation in Magerl type a fractures. Eur Spine J. 2007;16:1145–1155. doi: 10.1007/s00586-007-0310-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dai L.Y., Jiang S.D., Wang X.Y., Jiang L.S. A review of the management of thoracolumbar burst fractures. Surg Neurol. 2007;67:221–231. doi: 10.1016/j.surneu.2006.08.081. [DOI] [PubMed] [Google Scholar]
- 3.Andress H.J., Braun H., Helmbelger T., Schürmann M., Hertlein H., Hartl W.H. Long-term results after posterior fixation thoraco-lumbar burst fractures. Injury. 2002;33:357–365. doi: 10.1016/s0020-1383(02)00030-x. [DOI] [PubMed] [Google Scholar]
- 4.Sanderson P.L., Fraser R.D., Hall D.J., Cain C.M., Osti O.L., Potter G.R. Short segment fixation of thoracolumbar burst fractures without fusion. Eur Spine J. 1999;8:495–500. doi: 10.1007/s005860050212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Butt M.F., Farooq M., Mir B., Dhar A.S., Hussain A., Mumtaz M. Management of unstable thoracolumbar spinal injuries by posterior short segment spinal fixation. Int Orthop. 2007;31:259–264. doi: 10.1007/s00264-006-0161-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Muller U., Berlemann U., Sledge J., Schwarzenbach O. Treatment of thoracolumbar burst fractures without neurologic deficit by indirect reduction and posterior instrumentation: bisegmental stabilization with monosegmental fusion. Eur Spine J. 1999;8:284–289. doi: 10.1007/s005860050175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dai L., Jiang L., Jiang S. Posterior short-segment fixation with or without fusion for thoracolumbar burst fractures. A five to seven-year prospective randomized study. J Bone Jt Surg Am. 2009;91:1033–1041. doi: 10.2106/JBJS.H.00510. [DOI] [PubMed] [Google Scholar]
- 8.Singn K., Kim D., Vaccaro A.R. Thoracic and lumbar spinal injuries. In: Herkowitz H., Garfin S., Eismont F., Bell G., Balderston R., editors. Rothman–Simeone the Spine. Saunders Elsevier; Philadelphia: 2006. pp. 1132–1156. [Google Scholar]
- 9.Verlaan J., Diekerhof C., Buskens E. Surgical treatment of traumatic fractures of the thoracic and lumbar spine: a systematic review of the literature on techniques, complications, and outcome. Spine. 2004;29:803–814. doi: 10.1097/01.brs.0000116990.31984.a9. [DOI] [PubMed] [Google Scholar]
- 10.Ringel F., Stoffel M., Stuer C., Meyer B. Minimally invasive transmuscular pedicle screw fixation of the thoracic and lumbar spine. Neurosurgery. 2006;59:361–367. doi: 10.1227/01.NEU.0000223505.07815.74. [DOI] [PubMed] [Google Scholar]
- 11.Charles Y.P., Walter A., Schuller S., Aldakheel D., Steib J.P. Thoracolumbar fracture reduction by percutaneous in situ contouring. Eur Spine J. 2012;21:2214–2221. doi: 10.1007/s00586-012-2306-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roland M., Fairbank J. The Roland–Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine. 2000;25:3115–3124. doi: 10.1097/00007632-200012150-00006. [DOI] [PubMed] [Google Scholar]
- 13.Cheh G., Bridwell K.H., Lenke L.G. Adjacent segment disease following lumbar/thoracolumbar fusion with pedicle screw instrumentation: a minimum 5-year follow-up. Spine. 2007;32:2253–2257. doi: 10.1097/BRS.0b013e31814b2d8e. [DOI] [PubMed] [Google Scholar]
- 14.Chou P.H., Ma H.L., Wang S.T., Liu C.L., Chang M.C., Yu W.K. Fusion may not be a necessary procedure for surgically treated burst fractures of the thoracolumbar and lumbar spines: a follow-up of at least ten years. J Bone Jt Surg Am. 2014;96:1724–1731. doi: 10.2106/JBJS.M.01486. [DOI] [PubMed] [Google Scholar]
- 15.Delamarter R.B., Sherman J., Carr J.B. Pathophysiology of spinal cord injury: recovery after immediate and delayed compression. J Bone Jt Surg Am. 1995;77:1042–1049. doi: 10.2106/00004623-199507000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Yang H., Shi J., Liu J. Fluoroscopically-guided indirect posterior reduction and fixation of thoracolumbar burst fractures without fusion. Int Orthop. 2009;33:1329–1334. doi: 10.1007/s00264-008-0626-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mouchaty H., Conti P., Conti R. Assessment of three year experience of a strategy for patient selection and timing of operation in the management of acute thoracic and lumbar spine fractures: a prospective study. Acta Neurochir. 2006;148:1181–1187. doi: 10.1007/s00701-006-0883-5. [DOI] [PubMed] [Google Scholar]
- 18.Yang H., Shi J.H., Ebraheim M. Outcome of thoracolumbar burst fractures treated with indirect reduction and fixation without fusion. Eur Spine J. 2011;20:380–386. doi: 10.1007/s00586-010-1542-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Defino H.L., Canto F.R. Low thoracic and lumbar burst fractures: radiographic and functional outcomes. Eur Spine J. 2007;16:1934–1943. doi: 10.1007/s00586-007-0406-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lakshmanan P., Jones A., Mehta J., Ahuja S., Davies P.R., Howes J.P. Recurrence of kyphosis and its functional implications after surgical stabilization of dorsolumbar unstable burst fractures. Spine J. 2009;9:1003–1009. doi: 10.1016/j.spinee.2009.08.457. [DOI] [PubMed] [Google Scholar]
- 21.Wang X.Y., Dai L.Y., Xu H.Z., Chi Y.L. Kyphosis recurrence after posterior shortsegment fixation in thoracolumbar burst fractures. J Neurosurg Spine. 2008;8:246–254. doi: 10.3171/SPI/2008/8/3/246. [DOI] [PubMed] [Google Scholar]
- 22.Vornanen M.J., Böstman O.M., Myllynen P.J. Reduction of bone retropulsed into the spinal canal in thoracolumbar vertebral body compression burst fractures. A prospective comparative study between Harrington rods and two transpedicular devices. Spine. 1995;20:1699–1703. doi: 10.1097/00007632-199508000-00010. [DOI] [PubMed] [Google Scholar]
- 23.Gertzbein S., Court-Brown C., Marks P. The neurologic outcome following surgery for spinal fractures. Spine. 1998;13:641–644. [PubMed] [Google Scholar]
- 24.Dai L.Y., Wang X.Y., Jiang L.S. Neurologic recovery from thoracolumbar burst fractures: is it predicted by the amount of initial canal encroachment and kyphotic deformity? Surg Neurol. 2007;67:232–238. doi: 10.1016/j.surneu.2006.08.068. [DOI] [PubMed] [Google Scholar]
- 25.Knop C., Fabian F.H., Bastian L. Fate of the transpedicular intervertebral bone graft after posterior stabilization of thoracolumbar fractures. Eur Spine J. 2002;11:251–257. doi: 10.1007/s00586-001-0360-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang H., Liu J., Chen L. Short segment indirect reduction and fixation of thoracolumbar burst fractures without decompression and fusion. Spine J. 2006;6:27S. [Google Scholar]
- 27.Wang S.T., Ma H.L., Liu C.L., Yu W.K., Chang M.C., Chen T.H. Is fusion necessary for surgically treated burst fractures of the thoracolumbar and lumbar spine? Spine. 2006;31:2646–2652. doi: 10.1097/01.brs.0000244555.28310.40. [DOI] [PubMed] [Google Scholar]
- 28.Gardner V.O., Armstrong G.W. Long-term lumbar facet joint changes in spinal fracture patients treated with Harrington rods. Spine. 1990;15:479–484. doi: 10.1097/00007632-199006000-00009. [DOI] [PubMed] [Google Scholar]
- 29.Akbarnia B.A., Crandall D.G., Burkus K., Matthews T. Use of long rods and a short arthrodesis for burst fractures of the thoracolumbar spine. J Bone Jt Surg Am. 1994;76:1629–1635. doi: 10.2106/00004623-199411000-00005. [DOI] [PubMed] [Google Scholar]