Abstract
Objective
To determine the situational circumstances associated with bystander interventions to render aid during a medical emergency.
Methods
This study examined 16.2 million Emergency Medical Service (EMS) events contained within the National Emergency Medical Services Information System. The records of patients following a 9-1-1 call for emergency medical assistance were analyzed using logistic regression to determine what factors influenced bystander interventions. The dependent variable of the model was whether or not a bystander intervened.
Results
EMS providers recorded bystander assistance 11% of the time. The logistic regression model correctly predicted bystander intervention occurrence 71.4% of the time. Bystanders were more likely to intervene when the patient was male (aOR = 1.12, 95% CI = 1.12–1.3) and if the patient was older (progressive aOR = 1.10, 1.46 age group 20–29 through age group 60–99). Bystanders were less likely to intervene in rural areas compared to urban areas (aOR = 0.58, 95% CI = 0.58–0.59). The highest likelihood of bystander intervention occurred in a residential institution (aOR = 1.86, 95% CI = 1.85–1.86) and the lowest occurred on a street or a highway (aOR = 0.96, 95% CI = 0.95–0.96). Using death as a reference group, bystanders were most likely to intervene when the patient had cardiac distress/chest pain (aOR = 11.38, 95% CI = 10.93–11.86), followed by allergic reaction (aOR = 7.63, 95% CI = 7.30–7.99), smoke inhalation (aOR = 6.65, 95% CI = 5.98–7.39), and respiration arrest/distress (aOR = 6.43, 95% CI = 6.17–6.70). A traumatic injury was the most commonly recorded known event, and it was also associated with a relatively high level of bystander intervention (aOR = 5.81, 95% CI = 5.58–6.05). The type of injury/illness that prompted the lowest likelihood of bystander assistance was Sexual Assault/Rape (aOR = 1.57, 95% CI = 1.32–1.84) followed by behavioral/psychiatric disorder (aOR = 1.64, 95% CI = 1.57–1.71).
Conclusion
Bystander intervention varies greatly on situational factors and the type of medical emergency. A higher risk of patient death is likely to prompt bystander action. These novel study results can lead to more effective first aid training programs.
Keywords: bystander, EMS, rural, cardiac distress, trauma
Introduction
Experiences throughout the world with mass casualty events and other life-threatening emergencies have highlighted the important role of bystanders. Bystanders are persons at the scene of an event who voluntarily step forward to help, and their early assistance may reduce morbidity and mortality.1 Because bystanders usually outnumber professional rescuers, their involvement may strengthen response to emergency events. Vivid examples of bystander intervention during emergencies are available. After the explosions during the Boston marathon in 2013, a high survival rate was noted, in part, due to the response of bystanders and first responders.2 In a report of 619 survivors of the Haiti earthquake, it was found that 71% of the injured people reported that a “friend, family, or neighbor” had pulled them from the rubble and that less than 1% were rescued from professional rescue forces.3 Another act caught on video shows a group of 10 bystanders in Utah lifting up a 4,000 pound automobile to rescue a motorcyclist who was pinned under a burning car.4
In contrast to these examples, scholars have written about the well-known “bystander effect” in which the likelihood of a person helping others in distress grows smaller when there are more people available to provide help. That is, when an emergency situation occurs, observers are more likely to take action if there are few or no other witnesses. However, much of our knowledge on the bystander effect and helping behaviors comes from artificial means. Academic literature relies heavily on the self-reporting of respondent actions after reading mock written scenarios. Furthermore, much of the published literature relied on the use of undergraduate students as subjects in experiments5–14 or utilized written mock scenarios in other non-academic settings.15–17 Such settings do not permit the analysis of real world situations, nor do they allow an investigator to evaluate other factors. Also, most of these published analyses also suffer from a lack of respondent diversity in terms of age and maturity, because the respondents are often members of an undergraduate student population.
Studies evaluating bystander behavior obtained from natural experiments in real world settings have demonstrated beneficial health outcomes. For example, bystander initiated CPR produced a 27% survival rate compared to a 13% survival rate when CPR was delayed until the arrival of EMS personnel.18 Another CPR study revealed a nearly double rate of survival if the bystander performed CPR instead of waiting for the EMS provider (18.3% vs. 10.9%),19 or a 20% increase in the survival associated with CPR.20 Furthermore, it has been noted that successful resuscitation of drowning victims was most often performed by bystanders.21,22 Bystanders have also been successful in saving lives by reversing opioid poisoning through the administration of naloxone.23 Similarly, the absence of people available to intervene in motor vehicle crashes has been cited as a factor in higher rural fatality rates among car crash victims.24 Although these studies investigate specific diseases or injuries, little amount is known about how often a bystander intervenes across a wide spectrum of medical emergencies or how situational factors may influence bystander intervention in real-world emergencies. The purpose of this study was to identify such factors associated with the rendering of aid in a medical emergency to better understand how to increase bystander interventions. New information gathered from this broader study can help enhance first aid training programs offered to the public.
Methods
Data Source
This study used data from the 2012 National EMS Information System (NEMSIS).25 As this is a public-use, de-identified data set, IRB approval was not required. The NEMSIS data contains records from 42 States. This data set contains demographic data, basic 9-1-1 call information, details about the scene of injury or illness, medications administered, and other variables recorded by Emergency Medical Services (EMS). The data set is a non-weighted convenience sample and does not reflect national estimates. The total 2012 NEMSIS data set contained 19.8 million records of EMS events, most prompted by 9-1-1 calls. The NEMSIS data contains 50–70% of all estimated ambulatory events in the United States. As a matter of routine record keeping, EMS providers keep track of scene situational variables, such as weather conditions, traffic conditions, and bystander actions.
Identifying Relevant Records
EMS providers populated the NEMSIS system with information on how bystanders helped the patient before EMS arrived. Bystander assistance ranged widely depending on the nature of the illness or injury. Interventions could include bandages and dressings applied for wound care, administration of home oxygen, resuscitation, or providing nitroglycerin to patients with chest discomfort and counseling and emotional comfort in the case of some injuries, such as sexual assault. No standardized definition was provided for how EMS providers should report bystander assistance. The provider simply queried the patient if they had received any assistance prior to EMS arrival. EMS providers recorded medical interventions such that the treatment facility was aware of what medical interventions took place prior to EMS arrival. Only EMS events prompted by 9-1-1 calls were included in this study. Interfacility transfers were also excluded.
Measurements
The independent variables of the study included demographic (age, gender), clinical (providers impression, primary symptom), and EMS informational variables (EMS certification level and urbanicity). There were four different groups of urbanicity (e.g., Urban, Suburban, Rural, and Wilderness) and was based on an urban influence coding system utilized by the U.S. Department of Agriculture and the Office of Management and Budget. These codes take into account county population size, degree of urbanization, and adjacency to a metropolitan area or areas.
Statistical Analysis
The factors that were associated with bystander decisions were analyzed using a standard logistic regression model without stepwise procedures. The reference group of “obvious death” served as the comparison group to evaluate the odds of bystander intervention on the primary symptom because people usually will not intervene when the person is clearly dead. The dependent variable of the model was whether or not a patient received assistance prior to EMS involvement on the scene. Logistic regression results are presented as adjusted odds ratios (aOR) with 95% confidence intervals. Statistical testing of the descriptive frequency data was not performed because of the large sample size. SAS statistical software version 9.3, University Edition, was used for the data analysis.26
Results
An analysis of bystander interventions using NEMSIS showed that 10.97% (n = 1,775,758) of the EMS events, prompted by an emergency 9-1-1 call, involved bystander help. When gender was known, 9-1-1 calls occurred more often for females (46.64%) than males 40.08%). Emergency services were dispatched most often for the 60–99 age group (38.96%), followed by the 0–19 age group (21.31%), and the remaining age groups (20–29, 30–39, 40–49, and 50–59) showed a progressive increase in call volume (see Table 1).
Table 1.
Bystander sample by disease or injury national emergency medical services information systems: 2012
| Sample Characteristics | ||
|---|---|---|
| Gender | N | Percent |
| Female | 7, 546, 835 | 46.64 |
| Male | 6, 484, 533 | 40.08 |
| Unknown | 2, 149, 022 | 13.28 |
| Age Group | ||
| ages 0–19 | 3, 448, 474 | 21.31 |
| ages 20–29 | 1, 517, 177 | 9.38 |
| ages 30–39 | 1, 279, 222 | 7.91 |
| ages 40–49 | 1, 619, 660 | 10.01 |
| ages 50–59 | 2, 011, 797 | 12.43 |
| ages 60–99 | 6, 304, 060 | 38.96 |
| Provider’s Impression | ||
| Abdominal pain/problems | 855, 830 | 5.29 |
| Airway obstruction | 27, 470 | 0.17 |
| Allergic reaction | 85, 512 | 0.53 |
| Altered level of consciousness | 588, 563 | 3.64 |
| Behavioral/psychiatric disorder | 531, 293 | 3.28 |
| Diabetic symptoms (hypoglycemia) | 254, 194 | 1.57 |
| Electrocution | 2, 268 | 0.01 |
| Hyperthermia | 74, 220 | 0.46 |
| Hypothermia | 5, 440 | 0.03 |
| Hypovolemia/shock | 70, 309 | 0.43 |
| Inhalation injury (toxic gas) | 6, 026 | 0.04 |
| Obvious death | 65, 188 | 0.40 |
| Poisoning/drug ingestion | 300, 076 | 1.85 |
| Pregnancy/OB delivery | 68, 753 | 0.42 |
| Seizure | 356, 704 | 2.20 |
| Sexual assault/rape | 4, 961 | 0.03 |
| Smoke inhalation | 3, 234 | 0.02 |
| Stings/venomous bites | 8, 897 | 0.05 |
| Stroke/CVA | 179, 090 | 1.11 |
| Syncope/fainting | 526, 765 | 3.26 |
| Traumatic injury | 1, 916, 532 | 11.84 |
| Vaginal hemorrhage | 20, 120 | 0.12 |
| Cardiac distress/Chest Pain | 1, 218, 097 | 7.53 |
| Respiratory Arrest/Distress | 904, 863 | 5.59 |
| Unknown/Other | 8, 105, 985 | 50.10 |
| Primary Symptom | ||
| Bleeding | 430, 028 | 2.66 |
| Breathing Problem | 1, 032, 605 | 6.38 |
| Change in responsiveness | 1, 339, 558 | 8.28 |
| Choking | 24, 337 | 0.15 |
| Death | 120, 695 | 0.75 |
| Device/Equipment Problem | 8, 719 | 0.05 |
| Diarrhea | 47, 472 | 0.29 |
| Drainage/Discharge | 14, 997 | 0.09 |
| Fever | 125, 118 | 0.77 |
| Malaise | 218, 531 | 1.35 |
| Mass/Lesion | 5, 669 | 0.04 |
| Mental/Psych | 488, 872 | 3.02 |
| Nausea/Vomiting | 376, 245 | 2.33 |
| None | 797, 635 | 4.93 |
| Pain | 3, 360, 644 | 20.77 |
| Palpitations | 72, 765 | 0.45 |
| Rash/Itching | 34, 405 | 0.21 |
| Swelling | 99, 515 | 0.62 |
| Transport Only | 184, 316 | 1.14 |
| Unknown/Other | 6, 331, 353 | 39.13 |
| Weakness | 839, 156 | 5.19 |
| Wound | 227, 755 | 1.41 |
| Urbanicity | ||
| Rural | 1, 646, 271 | 10.17 |
| Suburban | 1, 276, 076 | 7.89 |
| Unknown | 220, 619 | 1.36 |
| Urban | 12, 647, 633 | 78.17 |
| Wilderness | 389, 791 | 2.41 |
| Location | ||
| Farm | 15, 677 | 0.10 |
| Home/Residence | 7, 964, 932 | 49.23 |
| Other Location | 659, 287 | 4.07 |
| Place of Recreation or Sport | 143, 716 | 0.89 |
| Public Building (schools, gov. offices) | 603, 074 | 3.73 |
| Residential Institution (Nursing Home, jail/prison) |
2, 389, 976 | 14.77 |
| Street or Highway | 1, 992, 077 | 12.31 |
| Trade or service (business, bars, restaurants, etc.) |
711, 623 | 4.40 |
| Unknown | 1, 700, 028 | 10.51 |
| Level of Service | ||
| EMT-Basic | 1, 223, 114 | 7.56 |
| EMT-Intermediate | 287, 885 | 1.78 |
| EMT-Paramedic | 13, 396, 123 | 82.79 |
| Nurse | 361, 831 | 2.24 |
| Physician | 169, 411 | 1.05 |
| Unknown | 742, 026 | 4.59 |
| Total | 16, 180, 390 | |
Also, the number of options to record a primary symptom is limited in the NEMSIS system. Thus, the number of unknown primary symptoms in the NEMSIS dataset is large (8,105,985 or 50.10%). Among the recorded primary symptoms, the provider’s impression of the illness or injury showed a wide variability call volume by medical emergency. The most common type of known provider impression that EMS responded to was a traumatic injury (1,916,532 or 11.84%) followed by cardiac distress/chest pain (1,218,097 or 7.53%) and respiratory distress (904,863 or 5.59%). The least common type of medical emergency was smoke inhalation (3,234 or 0.02%). When the primary symptom was known or large enough to categorize, the most common primary symptom was pain (3,360,664 or 20.77%) followed by a change in responsiveness (1,339,558 or 8.28%) and breathing problems (1,032,605 or 6.38%).
Situational factors such as the urban/rural designation of the community and the type of EMS service provided varied greatly. The majority of 9-1-1 calls resulted in a dispatch of EMS resources to urban areas (12,647,633 or 78.17%) followed by rural areas (1,646,271 or 10.17%) and suburban areas (1,276,076 or 7.89%). Additionally, specific scene locations also yielded differences in 9-1-1 call volume. Most of the dispatched services were sent to a residence or a person’s home (7,964,932 or 49.23%), followed by a residential institution (nursing home, jail/prison; 2,389,976 or 14.77%), followed by a street or a highway (1,992,077 or 12.31%). Calls involving farm locations were the least common (15,677 or 0.10%) followed by a place of recreation or sport (143,716 or 0.89%). Most of the EMS responses had an EMT-Paramedic dispatched as the highest level of service (13,396,123 or 82.79%) followed by EMT-Basic (1,223,114 or 7.56%).
Logistic regression assessed the likelihood of, and the conditions associated with, bystander behavior. There were 1,775,758 instances of recorded assistance and 14,404,632 instances of no help provided. A total of 16,180,390 records were analyzed. The model had a 71.4% concordance rate, indicating that the model correctly predicted bystander intervention a large majority of the time. Using the area under the curve (AUC), c statistic, the logistic regression model was found to be statistically significant (AUC, c statistic = 0.718, cutoff = 0.7).27
Many of the model independent variables correctly predicted bystander intervention behavior (Table 2). By gender, we found that when the patient was a male, others were more likely to assist than if the patient were female (aOR = 1.12, 95% CI = 1.12–1.3). Additionally, the likelihood of a bystander helping progressively increased when the patient was older. Bystander assistance was most likely to occur for the 60–99 age group (aOR = 1.46, 95% CI = 1.45–1.47), followed by the 50–59 age group (aOR = 1.35, 95% CI = 1.34–1.36), and was least likely to occur within the youngest age group, 0–19 age group (aOR = 1.0, reference group).
Table 2.
Likelihood of bystander intervention: situational characteristics that are associated with bystander actions
| Odds Ratio Estimate |
Lower CI | Upper CI | |
|---|---|---|---|
| Gender | |||
| Female | 1.00 | – | – |
| Male | 1.12 | 1.12 | 1.13 |
| Unknown | 0.11 | 0.10 | 0.11 |
| Age | |||
| ages 0–19 | 1.00 | – | – |
| ages 20–29 | 1.10 | 1.09 | 1.11 |
| ages 30–39 | 1.14 | 1.13 | 1.15 |
| ages 40–49 | 1.25 | 1.25 | 1.26 |
| ages 50–59 | 1.35 | 1.34 | 1.36 |
| ages 60–99 | 1.46 | 1.45 | 1.47 |
| Urbanicity | |||
| Urban | 1.00 | ||
| Rural | 0.58 | 0.58 | 0.59 |
| Suburban | 0.91 | 0.91 | 0.92 |
| Wilderness | 0.62 | 0.61 | 0.62 |
| Unknown | 0.78 | 0.77 | 0.79 |
| Incident Location | |||
| Home\Residence | 1.00 | – | – |
| Farm | 1.57 | 1.49 | 1.65 |
| Other Location | 1.21 | 1.20 | 1.22 |
| Place of Recreation or Sport | 1.71 | 1.69 | 1.74 |
| Public Building | 1.00 | 0.99 | 1.01 |
| Residential Institution (Nursing Home, jail/prison) |
1.86 | 1.85 | 1.86 |
| Street or Highway | 0.96 | 0.95 | 0.96 |
| Trade or service (business, bars, restaurants, etc.) |
1.36 | 1.35 | 1.37 |
| Unknown | 2.12 | 2.11 | 2.13 |
| EMS Impression | |||
| Obvious Death | 1.00 | – | – |
| Abdominal pain/problems | 3.78 | 3.63 | 3.94 |
| Airway Obstruction | 4.70 | 4.44 | 4.98 |
| Allergic Reaction | 7.63 | 7.30 | 7.99 |
| Altered level of consciousness | 4.01 | 3.85 | 4.18 |
| Behavioral/psychiatric disorder |
1.64 | 1.57 | 1.71 |
| Diabetic symptoms (hypoglycemia) |
4.10 | 3.93 | 4.28 |
| Electrocution | 4.67 | 4.04 | 5.38 |
| Hyperthermia | 4.10 | 3.91 | 4.30 |
| Hypovolemia/shock | 4.02 | 3.64 | 4.44 |
| Hypothermia | 4.78 | 4.57 | 5.01 |
| Inhalation Injury (toxic gas) | 5.02 | 4.59 | 5.48 |
| Poisoning/drug ingestion | 3.26 | 3.12 | 3.40 |
| Pregnancy. OB Delivery | 3.50 | 3.32 | 3.68 |
| Seizure | 4.05 | 3.89 | 4.23 |
| Sexual assault/rape | 1.57 | 1.32 | 1.84 |
| Smoke inhalation | 6.65 | 5.98 | 7.39 |
| Stings/venomous bites | 3.87 | 3.54 | 4.23 |
| Stroke/CVA | 5.80 | 5.56 | 6.06 |
| Syncope/fainting | 3.35 | 3.21 | 3.49 |
| Traumatic injury | 5.81 | 5.58 | 6.05 |
| Vaginal Hemorrhage | 4.20 | 3.94 | 4.48 |
| Cardiac distress/Chest Pain | 11.38 | 10.93 | 11.86 |
| Respiratory Arrest/Distress | 6.43 | 6.17 | 6.70 |
| Unknown/Other | 4.26 | 4.09 | 4.44 |
| Level of Service | |||
| EMT-Basic | 1.00 | – | – |
| EMT-Intermediate | 0.81 | 0.80 | 0.82 |
| EMT-Paramedic | 0.85 | 0.85 | 0.86 |
| Nurse | 2.15 | 2.13 | 2.17 |
| Physician | 0.31 | 0.31 | 0.32 |
| Unknown | 0.48 | 0.47 | 0.48 |
The location of the illness and/or injury was also associated with bystander behavior. Patients in rural settings were less likely to receive help compared to urban settings (aOR = 0.58, 95% CI = 0.58–0.59) and helping behavior in suburban settings was slightly less likely than what was experienced in urban settings (aOR = 0.91, 95% CI = 0.91–0.92). Helping behavior was most commonly associated with patients in a residential institution (nursing home, jail/prison) (aOR = 1.86, 95% CI = 1.85–1.86), followed by place of recreation or sport (aOR = 1.71, 95% CI = 1.69–1.74). A patient was least likely to receive bystander help if they were sick or injured on a street or highway (aOR = 0.96, 95% CI = 0.95–0.96).
After controlling for age, gender, and location influences, a bystander was most likely to intervene when the patient experienced cardiac distress/chest pain (aOR = 11.38, 95% CI = 10.93–11.86), followed by allergic reaction (aOR = 7.63, 95% CI = 7.30–7.99), smoke inhalation (aOR = 6.65, 95% CI = 5.98–7.39), and respiration arrest/distress (aOR = 6.43, 95% CI = 6.17–6.70). Using obvious death as a reference group, the least common type of medical emergency that prompted bystander assistance was sexual assault/rape (aOR = 1.57, 95% CI = 1.32–1.84) and a behavioral/psychiatric disorder (aOR = 1.64, 95% CI = 1.57–1.71). As noted in Table 1, a traumatic injury was the most commonly recorded known event (n = 1,674,304), it was also associated with a high level of bystander intervention (5th highest) (aOR = 5.81, 95%CI = 5.58–6.05).
The level of service provided by EMS was also associated with bystander intervention. For patients where the highest service level was an EMT basic and/or a nurse there was an increase of bystander interventions (aOR = 1.0, reference group, and aOR = 2.15, 95% CI = 2.13–2.17).
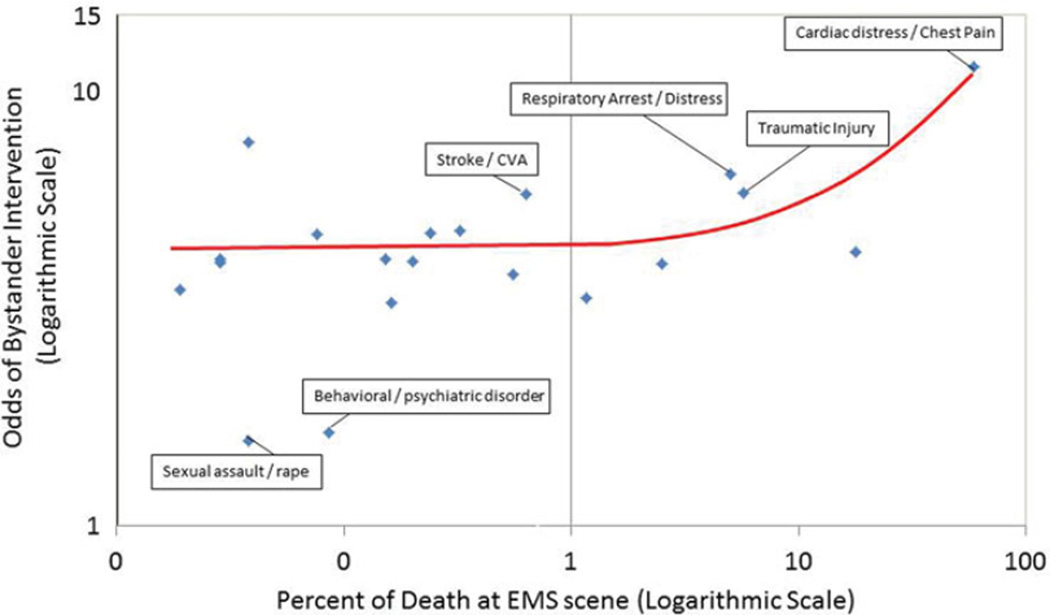
Because the odds of bystander intervention appeared to be higher for more critical and life-threatening situations, an additional analysis was performed. Using the NEMSIS data, we compared percentage of death at the scene to the odds of intervention. Those results are shown in Figure 1. There was a significant correlation between likelihood of death at the scene and the odds that someone would intervene (r = 0.70, p < 0.001).
Figure 1.
Odds of bystander intervention by percentage of death for each category of illness.
Discussion
Using a large database of real-world events documenting helping behavior collected by EMS providers in emergency situations, we examined factors related to helping; several factors emerged. Although bystanders are not always at the scene, the results in this paper help us better understand patterns of intervention when bystanders are present. The findings reveal that bystander assistance to the injured or sick is dependent on the type of medical emergency and is associated with the seriousness of the condition. That is, assistance occurs more often when the risk of death is more likely. Because interventions are dependent on the circumstances at the scene of the emergency scene, this study adds another novel dimension explaining bystander interventions. Even though the nature of the data does not allow us to probe for causal relationships, the factors suggested indicate a need for further exploration and can be used to inform first aid training programs.
Using NEMSIS, we identified a bystander intervention as helping behavior to a patient prior to the arrival of EMS. Using this classification, males were more likely to receive bystander intervention. This is in contrast to earlier work that has found that females are more likely to receive aid.28 However, if the definition of helping behavior is broadened to include calling 9-1-1, the effect of gender in the current data is more nuanced: whereas, males received more direct intervention, more 9-1-1 calls were made for females.
Previous research has found that more help is given in rural environments as compared to urban environments.29 However, with the current study data, more 9-1-1 calls were made within an urban environment, and victims in a rural environment were less likely to receive bystander intervention. Our study did show that bystanders were less likely to engage in helping behaviors when the setting was on a public street or highway and in a public building. Both locations would likely have a high number of people and potential bystanders. Yet, in these settings, bystanders may perceive an intervention to be in a dangerous location or that they may be too busy to stop and provide aid, or diffusion of responsibility may occur. Those specific findings may provide support for the bystander effect made popular published by Latane and Darley, in the 70s.30
Bystander intervention did not occur equally across emergencies. Bystanders intervened more often when there was a higher risk of death, such as when the patient had a traumatic injury or cardiac distress/chest pain and when the symptom was pain or changes in responsiveness. The least amount of helping behavior occurred with sexual assault and behavioral/psychological disorders.
There are two potential explanations for differences in helping behavior across emergency situations. First, bystander knowledge of what type of aid to render may differ across emergencies. For instance, bystanders may be least likely to render aid in the case of sexual assault/rape because they are unsure of what type of intervention is appropriate. In fact, lack of competence was among the first variables proposed by Latane and Darley.30 For instance, people are more likely to perform CPR if they have had training.19 Research in laboratory scenarios has also found that trained individuals (i.e., registered nurses) are more likely to render aid.31 Also, general support for this conclusion was found in a general population survey, where bystanders were more likely to perform CPR if they were young, male, had training, and lived in a rural area.19 Second, the riskiness of the helping behavior is also an important factor. Research has proposed a kind of bystander calculus in the form of an arousal: cost-reward model of helping in which individuals assess both the cost and the benefit of that intervention.32 This bystander calculus occurs by weighing the potential cost of helping (e.g., risk, time) with the potential cost of not helping (e.g., experience of negative emotions such as guilt, negative outcome for the victim). According to this model, when a bystander witnesses someone in need, they experience arousal in response to the victim’s distress. Helping the victim is one way to reduce this arousal. The amount of arousal experienced, and the resulting likelihood of helping, depends on many factors on both sides of the equation. Severe emergencies, for instance are proposed to increase arousal because of the victim’s high level of distress and should, therefore, result in more helping behavior to reduce that arousal.1 However, risk to the self as a result of helping should increase perceptions of potential costs of helping, thereby reducing helping behavior. For instance, Kliegel et al., found that fear of infection influences bystanders’ decisions to provide assistance, with 26% of participants reporting they were negatively influenced by fear of catching an infectious disease.33
The potential benefit of helping someone avoid death appears to be a weighty part of the equation. Our study findings provide support for this. A medical emergency where the patient was in more danger of dying (e.g., cardiac arrest, respiratory distress, and traumatic injury) produced a higher likelihood of intervention. When the emergency was a behavioral\ psychiatric disorder or an assault\rape there was a lower likelihood of intervention. Thus, the bystander was more likely to intervene if the emergency was thought to be an immediate threat to life.
Finally, we found bystander interventions in only 11% of the data analyzed here. Reasons for this number may be the inability of EMS providers to properly record bystander interventions, bystanders not being present at the scene, bystander fear of being sued, or perhaps the aforementioned bystander effect. This is in contrast to recent trends in the literature that have suggested that the bystander effect may be decreasing over time.1 Over-reliance on mock scenarios as a method to gauge bystander behavior may be contributing to this perceived trend. This study makes clear the need to distinguish between real-world emergency situations and contrived or laboratory emergencies.
Due to the nature of the data, there are some limitations to this study. Information on the personal characteristics of the bystanders was unavailable. Furthermore, the data are not population based. Although it is an extremely large data set, we do not know if it is representative of U.S. bystander activity. EMS providers may have asked the bystander question in many different ways, leading to different interpretations off what constitutes “aid.” Because the number of bystanders present was not recorded, a direct assessment of the bystander effect could not be made. The primary symptom was missing in many of the cases, and we suspect that the 2.0 version of NEMSIS did not offer enough primary symptoms options for EMS to select. Thus, the other category became very large. Future versions of NEMSIS (i.e. version 3.0) will have more options in the primary symptom field.
Conclusion
As evidenced, by the literature, bystanders can save lives. Bystander intervention in emergency situations involving sickness or injury varies greatly depending on the specific medical emergency, and gender and age of the person needing help. This work also illustrates that bystander intervention is associated with the seriousness of the emergency. This is important in that it addresses the situational factors of the bystander that may help influence the design of future first aid training programs in two ways: (1) by focusing training on more specific life saving techniques consistent with the types and frequencies of injuries and illnesses found in this study, and (2) by developing and encouraging bystander interventions when situations are less life threatening.
The field of bystander interventions would benefit from additional study of the NEMSIS data to extract situation-specific information on the circumstances surrounding the injury/sickness and specific actions taken by bystanders. An analysis of specific bystander actions within specific medical emergencies could further strengthen and inform first aid programs.
Footnotes
Color versions of one or more of the figures in the article can be found online at www.tandfonline.com/ipec.
References
- 1.Fischer P, Krueger JI, Greitemeyer T, et al. The bystander-effect: a meta-analytic review on bystander intervention in dangerous and non-dangerous emergencies. Psychol Bull. 2011;137(4):517–537. doi: 10.1037/a0023304. [DOI] [PubMed] [Google Scholar]
- 2.Walls RM, Zinner MJ. The Boston marathon response: why did it work so well? JAMA. 2013;309(23):2441–2442. doi: 10.1001/jama.2013.5965. [DOI] [PubMed] [Google Scholar]
- 3.Ashkenazi I, McNulty E, Marcus LJ, Dorn BC. The role of bystanders in mass casualty events: lessons from the 2010 Haiti earthquake. J Def Stud Resource Manage. 2012;1:2. [Google Scholar]
- 4.Amateur video posted to YouTube: Flame Throwers: Video of crash victim saved from burning car in Utah. [Accessed February 14, 2015]; Available at: https://www.youtube.com/watch?v=BmzSEYNTkHA. [Google Scholar]
- 5.Clark RD, Word LE. Where is the apathetic bystander? Situational characteristics of the emergency. J Personal Soc Psychol. 1974;29(3):279. [Google Scholar]
- 6.Gottlieb J, Carver CS. Anticipation of future interaction and the bystander effect. J Exper Soc Psychol. 1980;16(3):253–260. [Google Scholar]
- 7.Rutkowski GK, Gruder CL, Romer D. Group cohesiveness, social norms, and bystander intervention. J Personal Soc Psychol. 1983;44(3):545. [Google Scholar]
- 8.Tice DM, Baumeister RF. Masculinity inhibits helping in emergencies: personality does predict the bystander effect. J Personal Soc Psychol. 1985;49(2):420. [Google Scholar]
- 9.Garcia SM, Weaver K, Moskowitz GB, Darley JM. Crowded minds: the implicit bystander effect. J Personal Soc Psychol. 2002;83(4):843. [PubMed] [Google Scholar]
- 10.Karakashian LM, Walter MI, Christopher AN, Lucas T. Fear of negative evaluation affects helping behavior: the bystander effect revisited. N Am J Psychol. 2006;8(1):13–32. [Google Scholar]
- 11.Levine M, Thompson K. Identity, place, and bystander intervention: social categories and helping after natural disasters. J Soc Psychol. 2004;144(3):229–245. doi: 10.3200/SOCP.144.3.229-245. [DOI] [PubMed] [Google Scholar]
- 12.Banyard VL, Moynihan MM, Plante EG. Sexual violence prevention through bystander education: an experimental evaluation. J Comm Psychol. 2007;35(4):463–481. [Google Scholar]
- 13.Levine M, Crowther S. The responsive bystander: how social group membership and group size can encourage as well as inhibit bystander intervention. J Personal Soc Psychol. 2008;95(6):1429. doi: 10.1037/a0012634. [DOI] [PubMed] [Google Scholar]
- 14.Van Bommel M, Van Prooijen JW, Elffers H, Van Lange PA. Be aware to care: public self-awareness leads to a reversal of the bystander effect. J Exper Soc Psychol. 2012;48(4):926–930. [Google Scholar]
- 15.Fischer P, Greitemeyer T, Pollozek F, Frey D. The unresponsive bystander: are bystanders more responsive in dangerous emergencies? Eur J Soc Psychol. 2006;36(2):267–278. [Google Scholar]
- 16.Shotland RL, Heinold WD. Bystander response to arterial bleeding: helping skills, the decision-making process, and differentiating the helping response. J Personal Soc Psychol. 1985;49(2):347. doi: 10.1037//0022-3514.49.2.347. [DOI] [PubMed] [Google Scholar]
- 17.Chekroun P, Brauer M. The bystander effect and social control behavior: the effect of the presence of others on people’s reactions to norm violations. Eur J Soc Psychol. 2002;32(6):853–867. [Google Scholar]
- 18.Cummins RO, Eisenberg MS, Hallstrom AP, Litwin PE. Survival of out-of-hospital cardiac arrest with early initiation of cardiopulmonary resuscitation. Am J Emerg Med. 1985;3(2):114–119. doi: 10.1016/0735-6757(85)90032-4. [DOI] [PubMed] [Google Scholar]
- 19.Coons SJ, Guy MC. Performing bystander CPR for sudden cardiac arrest: behavioral intentions among the general adult population in Arizona. Resuscitation. 2009;80(3):334–340. doi: 10.1016/j.resuscitation.2008.11.024. [DOI] [PubMed] [Google Scholar]
- 20.Spaite DW, Hanlon T, Criss EA, et al. Prehospital cardiac arrest: the impact of witnessed collapse and bystander CPR in a metropolitan EMS system with short response times. Ann Emerg Med. 1990;19(11):1264–1269. doi: 10.1016/s0196-0644(05)82285-1. [DOI] [PubMed] [Google Scholar]
- 21.Marchant J, Cheng NG, Lam LT, et al. Bystander basic life support: an important link in the chain of survival for children suffering a drowning or near-drowning episode. Med J Australia. 2008;188(8):484. doi: 10.5694/j.1326-5377.2008.tb01725.x. [DOI] [PubMed] [Google Scholar]
- 22.Venema AM, Groothoff JW, Bierens JJ. The role of bystanders during rescue and resuscitation of drowning victims. Resuscitation. 2010;81(4):434–439. doi: 10.1016/j.resuscitation.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 23.Doe-Simkins M, Walley AY, Epstein A, Moyer P. Saved by the nose: bystander-administered intranasal naloxone hydrochloride for opioid overdose. Am J Public Health. 2009;99(5):788. doi: 10.2105/AJPH.2008.146647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brodsky H. The bystander in highway injury accidents. Soc Sci Med. 1984;19(11):1213–1216. doi: 10.1016/0277-9536(84)90373-3. [DOI] [PubMed] [Google Scholar]
- 25.Mann NC, Kane L, Dai M, Jacobson K. Description of the 2012 NEMSIS Public-Release Research Dataset. Prehosp Emerg Care. 2015;19(2):232–240. doi: 10.3109/10903127.2014.959219. [DOI] [PubMed] [Google Scholar]
- 26.SAS Institute, Inc. SAS University Edition, version 9.3. Cary, NC: 2014. [Google Scholar]
- 27.Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd. New York, NY: Wiley; 2000. [Google Scholar]
- 28.Eagly AH, Crowley M. Gender and helping behavior: a meta-analytic review of the social psychological literature. Psychol Bull. 1986;100(3):283. doi: 10.1037/0033-2909.100.3.283. [DOI] [PubMed] [Google Scholar]
- 29.Steblay NM. Helping behavior in rural and urban environments: a meta-analysis. Psychol Bull. 1987;102(3):346. [Google Scholar]
- 30.Latane B, Darley JM. The Unresponsive Bystander: Why Doesn’t He Help? New York, NY: Prentice Hall; 1970. [Google Scholar]
- 31.Tanigawa K, Iwami T, Nishiyama C, Nonogi H, Kawamura T. Are trained individuals more likely to perform bystander CPR? an observational study. Resuscitation. 2011;82(5):523–528. doi: 10.1016/j.resuscitation.2011.01.027. [DOI] [PubMed] [Google Scholar]
- 32.Dovidio JF, Piliavin JA, Gaertner SL, Schroeder DA. The arousal: cost-reward model and the process of intervention: a review of the evidence. In: Clark MS, editor. Review of Personality and Social Psychology. Newbury Park, CA: Sage; 1991. pp. 86–118. [Google Scholar]
- 33.Kliegel A, Scheinecker W, Sterz F, Eisenburger P, Holzer M, Laggner A. The attitudes of cardiac arrest survivors and their family members towards CPR courses. Resuscitation. 2000;47:147–154. doi: 10.1016/s0300-9572(00)00214-8. [DOI] [PubMed] [Google Scholar]